Abstract
Pain catastrophizing has been described for more than half a century which adversely affects the pain coping behavior and overall prognosis in susceptible individuals when challenged by painful conditions. It is a distinct phenomenon which is characterized by feelings of helplessness, active rumination and excessive magnification of cognitions and feelings toward the painful situation. Susceptible subjects may have certain demographic or psychological predisposition. Various models of pain catastrophizing have been proposed which include attention-bias, schema-activation, communal-coping and appraisal models. Nevertheless, consensus is still lacking as to the true nature and mechanisms for pain catastrophizing. Recent advances in population genomics and noninvasive neuroimaging have helped elucidate the known determinants and neurophysiological correlates behind this potentially disabling behavior.
Keywords: Disability, pain catastrophizing, rehabilitation, review
PAIN CATASTROPHIZING: HISTORY AND DEFINITION
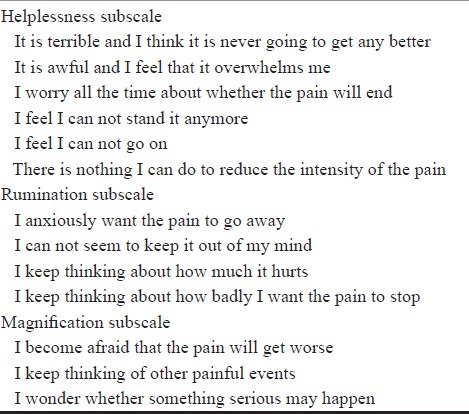
Catastrophizing was first coined by American psychologist Ellis[1] in 1962 and later refined by Beck[2] in 1987 to describe a maladaptive cognitive style originally seen in patients with anxiety and depressive disorders with an irrational negative forecast of future events. Pain is a common negative experience which signifies injury, illness, danger and possible doom. Taken together, pain catastrophizing refers to a set of exaggerated and ruminating negative cognitions and emotions during actual or perceived painful stimulation. One may argue that the earliest record of pain catastrophizing can be found in the classic treatise of Traditional Chinese Medicine, “Ji Gui Yao Lue” (the Essays of the Golden Chamber),[3] written in 200 A.D., which described in details a clinical condition called Zhong Zao, where the patient (often a female) exhibits feelings of worry, repetitive thoughts, helplessness and exaggerated response to pain or stress. In 1889, French writer Guy Maupassant expounded in his work “Sur L’eau” his migrainous attacks as “atrocious torment”, “worst in the world”, “driving one mad”, “scattering one's thoughts”.[4] In 1940's, female Mexican painter Frida Kahlo[5] portrayed her unbearable neuropathic pain and fibromyalgia due to motor vehicle accident with a series of surrealistic paintings centered around the theme of brokenness and hopelessness, vividly depicted in “The broken column” and “Without hope” [Figures 1 and 2]. The earliest work on pain catastrophizing was performed by Spanos et al.[6] in 1979 where individuals reported on their pain experience after a cold pressor task and those with worry, fear and inability to divert attention from pain were classified as pain catastrophisers. Chaves et al.[7] in 1987 studied the thoughts and images of patients which they recalled from a stressful dental procedure and those who tend to exaggerate or magnify the threat value or gravity of the situation were described as catastrophisers. Although the studies by Spanos and Chaves were limited in validity by their use of nonstandardized interview methods, it is worth noting that they formed the blueprints of situational (state) and dispositional (trait) assessments respectively. Rosentiel and Keefe[8] were credited for defining the third domain of pain catastrophizing-helplessness and pessimism about the ability to cope—as they included a six-item subscale in debuting their Coping Strategy Questionnaire (CSQ) in 1983. This led to the subsequent development of the Pain Catastrophizing Scale (PCS) in 1995 by Sullivan et al.[9] which contains thirteen items which are grouped under the three subscales [Table 1]. All items are rated in a 5-point scale, its internal consistency and validity has been demonstrated[10] and has been found to have a high test-retest correlation (r=0.75) across a 6-week period for the same individual. PCS has now been translated to other languages like Chinese,[11], Japanese,[12,13] French,[14] German,[15], Dutch,[16] Spanish,[17] Greek[18] and Catalan[19] and also modified for use in children (PCS-C),[20] adolescents (PCS-Ado)[14] and significant other (PCS-S).[21] Apart from becoming become the reference standard psychometric tool for pain catastrophizing, PCS also defines its three characteristic domains of helplessness, rumination and magnification. Nevertheless, there has been doubt as to the whether PCS can cover the worse-case scenario construct for pain-catastrophizing and suggestion was raised to add in items like “I might end up paralyzed”, “I might become totally disabled”, “I might end up losing my job and not able to support my family”, etc. to increase enhance the validity of PCS scale.[22]
Figure 1.
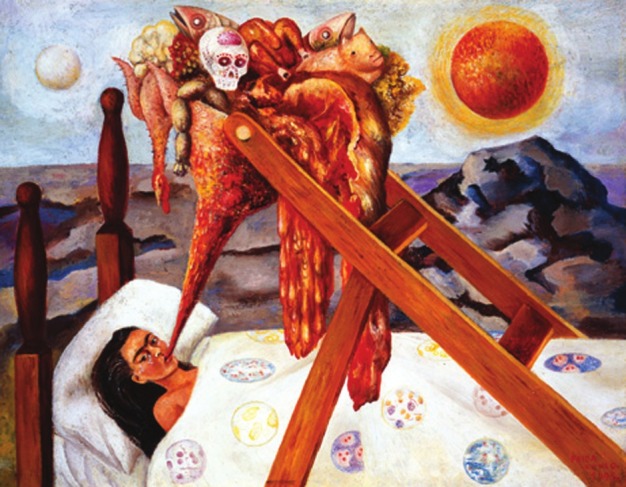
Surrealistic painting titled “Without Hope” where Frida tried to externalize her chronic pain and hopelessness by portraying her bedbound self force-fed with a funnelled mixture of carcasses. Frida Kahlo, “Sin esperanza”, 1945. Oil on Canvas mounted on Masonite, 11”×14”. Collection Museo Dolores Olmedo Patino, Mexico City
Figure 2.
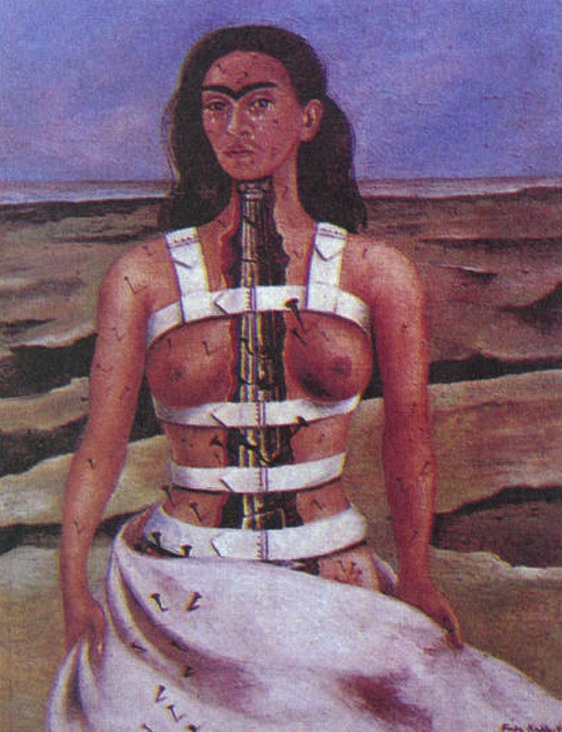
Frida Kahlo's painting “broken column” where she depicted her spine as a broken marble column in the background of multiple nails driven into other parts of her naked body, giving her the continual undignifying pain. She told others “I am disintegration” Frida Kahlo, “La columna rota”, 1944. Oil on canvas mounted on rigid fiber, 16”×12”, Collection Museo Dolores Olmedo Patino, Mexico City
Table 1.
Pain catastrophizing scale
PAIN CATASTROPHIZING AND PHYSICAL DISABILITY
Clinically, pain catastrophizing is a recognized phenomenon which is often considered within the context of depression. There are numerous experiments conducted for the research of pain catastrophizing and they can be broadly divided three categories according to the nature of the subjects: healthy volunteers (e.g., undergraduate students), patients with acute pain (e.g., whiplash injury after motor vehicle accidents) and patients with chronic pain (e.g., fibromyalgia and low back pain). Selected studies with their methodologies, variables and predicted outcome are summarized in Table 2.
Table 2.
Summary of selected clinical studies on pain catastrophizing looking at three research sample groups: Healthy participants, acutely injury and with chronic pain
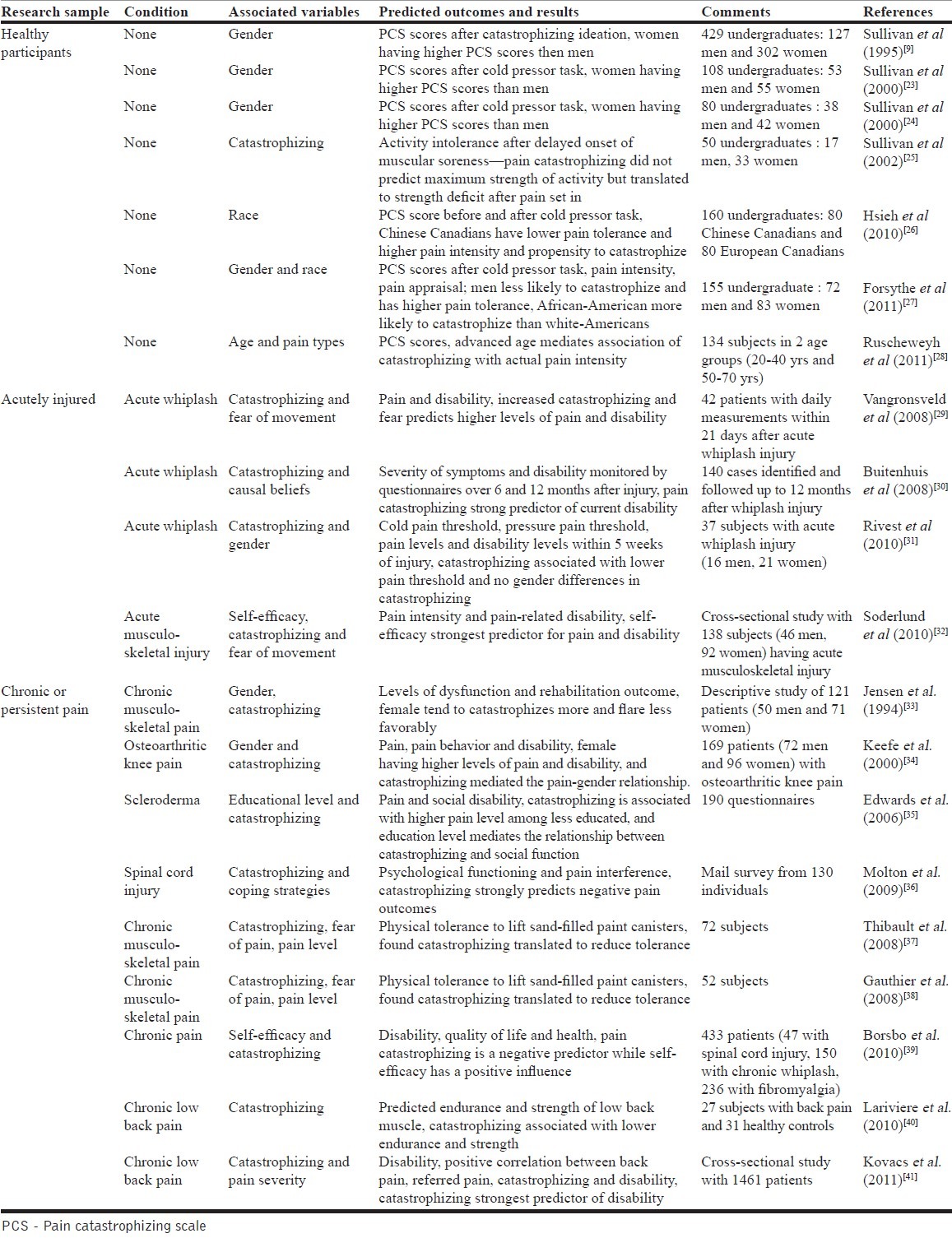
Per se, pain catastrophizing is an independent risk factor for predicting chronicity of pain and poorer prognosis. Van Eijsden-Besseling et al.[42] performed a case-controlled cross-sectional study of work-related upper limb disorders amongst computer workers and found significant correlation of pain catastrophizing with poorer symptoms and prognosis. Bergbom et al.[43] studied the prognostic factors for 297 patients diagnosed with musculoskeletal pain who received various physical therapy within 6 months and found that higher level of pain catastrophizing predicted lack of improvement and continued disability. It is fair to conclude that most studies have consistently highlighted pain catastrophizing as a predictor for physical disability in both acute injury and chronic pain conditions [Table 2].
How well does pain catastrophizing translate to physical disability?
Sullivan et al.[25] recruited 50 healthy undergraduates and studied the association between pain catastrophizing and actual physical intolerance by employing the model of exercise-induced delayed onset muscle soreness (DOMS)-where participants were asked to repeat a set of concentric and eccentric contractions against heavy loads until they experienced pain, and to return for similar exercises 48 hours later for measuring any deficit in physical intolerance. The group found that pain catastrophizing did not affect the maximum physical capacity achievable in the first round of exercise, but contributed to reduction in the maximum weight that could be lifted in the second round (i.e., after pain had set in). Also, the relation remained significant after controlling for the level of pain and negative mood, signifying that pain catastrophizing alone translated to physical force deficit. Moreover, they also found that the helplessness subscale of PCS seemed to be the best predictor for disability. However, for subjects with pain, the association of pain catastrophizing with actual performance deficit lacks consensus. Crombez et al.[44] studied 104 subjects with chronic low back pain and measured the association of pain-related fear, actual pain level and pain catastrophizing with performance of a physical task (Trunk-Extension-Flexion). He found that fear of pain, but not pain catastrophizing, is the best predictor of self-reported disability and performance degradation. Similar conclusion was found by Swinkels-Meewisse et al.[45] who recruited 96 subjects with acute low back pain (not more than 4 weeks’ duration) and studied their ability to lift a 7-kg bag repeatedly from the ground in regard to their fear of pain, actual pain levels and pain catastrophizing. However, the Sullivan camp[37] held an opposing view. In his study of 72 subjects with chronic musculoskeletal pain, physical tolerance, communicative pain behaviors (facial and verbal expressions like grimace, grunts, words and sighs) and protective pain behaviors (guarding, holding, touching or rubbing) were studied as the subjects sequentially lifted 18 paint canisters partially filled with sand at three standardized weights. The group found significant associations between pain catastrophizing and physical intolerance and also with both types of pain behaviors. In particular, the group found no association of fear of pain and suggested the reasons to be due to differences in patient population, parameters of tolerance task and pain measurements. In another study aimed to validate the French-Canadian version of the Pain Disability Index (PDI),[38] Sullivan's group adopted an identical protocol of lifting sand-filled paint canisters in 52 subjects with chronic musculoskeletal pain and found association between PDI (which in turn correlated with pain catastrophizing) and reduced performance of canister lifting.
MEASURING PAIN CATASTROPHIZING: SITUATIONAL OR DISPOSITIONAL?
Being a mental set, pain catastrophizing can be assessed in two different ways—either as a reaction measured during or immediately after exposure to a noxious stimulation (situational or state assessment), or, through recall of most negative feelings and cognitions related to painful events (dispositional or trait assessment). Although pain catastrophizing is often conceptualized as a trait which is only manifests with a noxious encounter, it has been argued that dispositional assessment of pain catastrophizing often fail to correlate with actual pain ratings as the recall events(s) may either be too distal in the past or too weak in impact, or the items in the assessment tool are not rigorous enough to capture the variances. On the contrary, it is questionable that by nature of the design of the experiment, situational assessment may only partially cover the three domains of pain catastrophizing—an example being a modified form of PCS (Appendix A of original paper) used by Edwards et al.[46] which seems to have omitted the magnification domain. Studies reported a varying association between the state versus dispositional assessment for pain catastrophizing: Dixon measured PCS score before (dispositional assessment) and after (situational assessment) cold pressor task in healthy subjects and found little correlation between the two;[47] Campbell et al.[48] compared situational versus dispositional PCS across multiple samples of healthy subjects, subjects with short-term pain and with chronic pain and found that except for short-term pain, there is no significant correlation between situational and dispositional pain catastrophizing in healthy subjects and patients chronic pain, and that situational PCS predicts higher pain ratings across all three groups. This calls into question the logic and validity of studies using dispositional type of assessment for pain catastrophizing.
PAIN CATASTROPHIZING: A DISTINCT ENTITY OR REDUNDANT CONSTRUCT?
Implicit in the three domains of pain catastrophizing are negative affect constructs which are shared by a number of conditions like worry, anxiety and in particular, depression.[49–51] The content of items measuring catastrophizing, depression and anxiety in PCS, CSQ and coping-effectiveness scale are also remarkably similar with convergent loading during factor analysis. This led to controversy whether pain catastrophizing is nothing more than a redundant construct or measurement confounds when other negative affect conditions are studied. Hirsh et al. administered the catastrophizing subscale of CSQ (CSQ-CAT) as a dispositional assessment to chronic pain patients and found that after regression analysis, the negative mood components of depression and anxiety were highly associated with pain catastrophizing, which when controlled for, pain catastrophizing has minimal correlation to pain prediction.[49] George et al. conducted a situational measurement in healthy subjects after a cold pressor encounter using CSQ-CAT and Fear of Pain Questionnaire and found that although fear of pain associated with pain catastrophizing strongly, acute pain intensity was only predicted by fear of pain and not pain catastrophizing.[52] This contradicted the findings of an earlier similar study by Sullivan et al.[53] which stated that pain catastrophizing is a better predictor of pain ratings, although one can argue that the conclusions are not directly comparable as Sullivan employed PCS and not CSQ-CAT in his study. Since 1990's, Sullivan's group has been the stronghold in defending the conceptual and operational distinctness of pain catastrophizing from depression as a separate construct in assessing chronic pain.[50] His view is supported by Geisser et al. with his dispositional study in patients with chronic pain, who concluded that catastrophizing is a separate construct that mediates the relationship between depression and the evaluative and affective effects of pain.[54] Keefe et al.[34] found a similar mediating role for catastrophizing amongst osteoarthritis patients between gender, pain, pain behavior and disability after correction for depression. In one dispositional study of subjects with persistent pain due to soft tissue injury, Sullivan et al. found significant correlation of PCS with reported pain intensity and perceived disability, the latter in particular seemed to be independent of the levels of depression or anxiety.[55] Regarding possible overlap with neuroticism, Martin et al.[56] found catastrophizing predicted perceived disability in patients with fibromyalgia independent of neuroticism. Thus said, other researchers still cast doubt over pain catastrophizing as a construct distinct from negative affectivity.[49,52] To add mud to the pond, Tuner et al showed that in chronic pain sufferers, catastrophizing is a strong predictor of pain intensity[57,58] and also in a vice versa manner with a daily process study,[59] and that catastrophizing is a predictor of depression per se.[60] Finally, Mounce et al.[61] performed a dispositional study amongst pain-free subjects who completed nine frequently used psychometric scores which measure pain catastrophizing, negative affect, general trait anxiety, depression and anxiety, fear of illness, pain-specific anxiety, fear of pain, fear of negative evaluation and anxiety sensitivity. Component analysis of all the constructs in these nine scores revealed commonality which can be summarised into three core components: general distress, fear of pain from injury/insult and cognitive intrusion of pain which is shared by depression and pain catastrophizing. Overall evidence for pain catastrophizing as a unique construct distinct from others of negative affectivity is still conflicting, and better research methodologies and tools are needed to enable spectrum analysis of pain-catastrophizing trait in response to standardized painful event, and vice versa. Only then one can better understand the causality (if any) between the trait versus state variables.
DETERMINANTS FOR PAIN CATASTROPHIZING
Gender
So far, both dispositional and situational studies have shown a determinant effect of gender on pain catastrophizing. Sullivan et al. demonstrated significantly higher PCS scores in one study with female as compared to male undergraduates using catastrophizing ideation,[9] and similarly in two another studies using cold pressor tasks,[23,24] with differences observed in the rumination and helplessness subscales, not the magnification subscale. In a study of Swedish patients with chronic musculoskeletal pain, female tend to catastrophizes more readily then male with a less efficient coping strategy.[33] This female predominance in pain catastrophizing is further echoed by Keefe's study with patients suffering from osteoarthritis.[34] The exact mechanisms are still unknown but Goodin et al. suggested that female may possess a lower diffuse noxious inhibitory control neural circuitry which predisposes them to pain catastrophizing.[62] Thus said, Rivest et al. studied patients with acute whiplash injury and found that male sex is more associated with pain catastrophizing,[31] keeping in line with Elklit's findings that men are more prone to anxiety and disability subsequent to whiplash injury.[63] A possible explanation being the preference of the emotion-focused coping strategy by males as compared to the symptom-focused coping strategy by the females.[64]
Age
General consensus is still lacking regarding the effect of advanced age on pain perception, from increased sensitivity[65–69] to reduced perception of both visceral[70] and nonvisceral type of pain.[71] However, one must be aware of the heterogeneity of noxious stimuli and pain assessment used in different studies which inevitable may confound the validity of results. For pain catastrophizing, data on the effects of age is very sparse and after extensive literature search, there is only one recent study by Ruscheweyh et al.[28] which performed a dispositional assessment and found that in younger adults, catastrophizing is associated with emotional response to pain while in older subjects, it is preferentially associated with the actual pain intensity.
Race
There is abundant data regarding race differences in the study of pain. Compared to White-Americans, lower pain threshold and tolerance has been documented in African-Americans,[72–75] Hispanic-Americans[76] and South Asians.[26] In context of pain catastrophizing, a higher association has been reported with situational assessment (cold pressor task) in Chinese-Canadians as compared to European-Canadians,[27] and also in African-Americans as compared to White-Americans.[77] Like that for gender, the underlying mechanisms are still unknown.
Genetic susceptibility
Seen as a trait, pain catastrophizing has been associated with specific genotypes. Geroge et al. found that catechol-o-methyltransferase (COMT) diplotype (high versus low activity) modulates pain ratings and pain catastrophizing in shoulder pain,[77,78] where low COMT activity is associated with higher pain ratings and higher tendency for pain catastrophizing. In a similar context, Finan et al. found the val(158)met single nucleotide polymorphism in the COMT gene mediates pain catastrophizing and maladaptive pain coping in fibromyalgia.[79] Neuropeptide S (NPS) is a recently discovered neurotransmitter produced by brainstem neurons which mediates arousal,[80] anxiolytic responses and attenuates contextual fear.[81] Recent data indicated that a adenosine(A) to thymidine(T) single nucleotide polymorphism on the human neuropeptide-S receptor gene (NPSR1) predisposes to catastrophizing in fear reactions.[82] From a cell-signaling perspective, Edwards et al.[83] conducted situational assessment in healthy subjects for pain catastrophizing before and after application of noxious mechanical, heat and cold stimuli, and found that higher levels of pain catastrophizing was associated with enhanced serum interleukin-6 (IL-6) activity. This putative linkage between pain catastrophizing and IL-6 need further research as to whether people with genotype of increased IL-6 activity/production are more prone to pain catastrophizing.
Neurophysiological correlates
Pain catastrophizing is a conglomerate of maladaptive affective and cognitive responses and thanks to the advances in magnetic resonance neuroimaging techniques, in particular functional MRI (fMRI), research data have correlated pain catastrophizing with brain regions responsible for processing of pain, emotions and affect. Seminowicz et al. performed fMRI study on 22 healthy volunteers with electrical stimulation of median nerves and assessed their pain catastrophizing scores. Interesting, at mild levels of pain, pain catastrophizing was associated with increased fMRI activity in the prefrontal, insular, rostral anterior cingulate and parietal cortex. However, with intense pain, there was negative correlation of activity with pain catastrophizing, suggesting a failure of the top-down inhibitory from the cortex. Gracely et al.[84] recruited 29 subjects with fibromyalgia and assessed their pain-catastrophizing scores after blunt stimuli. They found significant association of pain catastrophizing with increased fMRI activities in brain areas related to anticipation of pain (medial frontal cortex, cerebellum), attention to pain (dorsal ACC, dorsolateral prefrontal cortex), emotional aspects of pain (claustrum, closely connected to amygdala) and motor control. Other data have suggested an endogenous alteration of supra-spinal pain-inhibitory versus pain-facilitating pathways, conceptually referred to as the diffuse noxious input controls (DNICs). DNIC is repeatedly measured as pain ratings for a “test” stimulus before and after application of a “conditioning” stimulus, and its response over time is noted. Weissman-Fogel et al found that in healthy subjects pain catastrophizing is associated with a lower DNIC profile,[85] and such findings were replicated by Goodin et al.[62] who also added that female gender also seems to have a lower DNIC. Finally, one recent study by Quartana et al.[86] showed flattening of the morning cortisol profile which was associated with pain catastrophizing irrespective of the actual pain status. This implies a possible endogenous neurohormonal basis for pain catastrophizing as a trait.
Psychosocial variables
Being a negative mental and affective set, pain catastrophizing would in theory be exacerbated by adverse or unstable psychosocial settings. Meredith et al.[87] recruited pain-free subjects and studied the effects of adult attachment styles on emotions, cognitions, pain tolerance, pain intensity and pain catastrophizing during and after a cold pressor task. It was found that adult attachment style mediates the impact of pain intensity on tendency to catastrophize, and insecure attachment leads to higher pain scores and likelihood to pain catastrophizing, while secure attachment was associated with better pain control, lower level of depression and pain catastrophizing. In the same vein but using different methodologies, McWilliams et al.[88] asked university students to complete a battery of psychometric measures including PCS and studied the impact of adult attachment on pain-related fear, pain hypervigilance and pain catastrophizing. It was found that rejection anxiety and beliefs of personal unworthiness associated with fear avoidance while discomfort with intimacy and interpersonal mistrust is linked strongly with pain catastrophizing.
THEORIES FOR PAIN CATASTROPHIZING AND APPROACH ANALYSIS
Attention-bias model
The attention bias models states that pain catastrophizing results of a preferential and dysfunctional bias of attention toward pain and its related cognition and mental processes. Taken for grant as a normal human reaction, any painful stimulus interrupts and demands attention of the subject. Eccleston et al. elaborated a model consisting of seven components (environment, multiple demands from the environment, sensory system, action programs, focal task, threat mediation and moderating factors) to address why and how pain interrupts attention to motivate an urge to escape.[89] He opined that the interruptive function of pain depends on the pain-related characteristics (e.g., threat level of pain) and the environmental demands (e.g., emotional arousal). Authors did mention briefly that pain catastrophizing is a variable of pain characteristics in the interruptive process; hence pain catastrophizers may have their attention maladaptively interrupted to a state of cognitive and behavioral immobilization whenever a painful stimulus occurs. Using a cueing paradigm, Van Damme et al.[90,91] found that subjects who score higher in self-reported pain catastrophizing scores tend to have either exaggerated attentional engagement, retarded attentional disengagement, or both to painful stimuli. Vancleef et al.[92] asked healthy volunteers who had been prescreened with Pain Catastrophizing Scale, the Anxiety Sensitivity Index, and the Injury/illness Sensitivity Index and measure their attentional interference as they perform an auditory discrimination task whilst occasional distracted by low electrocutaneous stimulations. It was found that only pain catastrophizing enhances interference of their attentional ability. In an attempt to tweak attention to modulate pain catastrophizing, Michael et al.[93] subjected volunteers to an initial cold pressor task and then ask them to read out a serious of control, pain-sensory and pain-affect words whilst undergoing a second cold pressor task. As expected, reading affect-related words, but not the other words, led to higher pain catastrophizing in the second task. In a similar line of thought, Quartana et al.[94] recruited subjects with chronic low back pain and manipulated their attention either by distraction or suppression strategies, and found that pain catastrophizing was strongly related to suppression (i.e., enhanced attention) and alleviated by distraction (i.e., reduced attention).
Schema-activation model
Sullivan et al.[9,95] proposed that pain catastrophizers possess s special pain schema which consisted of a distorted cognition with excessively pessimistic beliefs about pain, pain-related experiences and actual ability to cope. When confronted with the minimally noxious stimulus, this schema is activated and heightens the pain experience which eventually over time, translates to a learned expectancy (or self-fulfilled prophecy) regarding the high threat of pain and their own inability of management. This model is strong is explaining the cognitive processes that contribute to pain catastrophizing but do not address the conditions and their interactions that lead to activation of the schema. Also existing methodologies cannot test whether and to what degree the schema has been activated during the pain-catastrophizing process.
Appraisal model
The appraisal model evolves from the transactional model of stress and coping put forward by Lazarus and Folkman. Whenever a pain stressor comes along, the subject initially assess the relevance and levels of harm as the primary appraisal, then continue to contemplate upon the coping options and formulate the beliefs regarding the possibility of success as the secondary appraisal. In the contact of pain catastrophizing, researchers proposed that magnification and rumination domain stems from a dysfunctional focus and evaluation in the primary appraisal stage, while helplessness is a maladaptive and negative secondary appraisal.[96] In a study of professional dancers who are sued to cope with pain due to performance or injury,[97] Anderson et al found that their appraisal of pain did not differ according to the type or severity of pain they experience, except when perceived as a threat, would associate with pain-catastrophizing behavior.
Communal coping model
Advocated by Sullivan et al., the communal coping model states that pain catastrophizing is a behavior strategy of coping where subjects communicate their painful experience to elicit emotional and social support from others, hence reinforcing the pain and illness behavior and subsequently undermining their normal adaptability to cope with the pain itself.[95] Living with a partner or spouse leads to higher probability of catastrophizing for subjects with chronic pain,[98] and the partners or spouse would also perceive higher pain levels from the pain catastrophizers and provide more instrumental support.[99] In a related manner, greater perceived entitlement to pain-related support was more associated with pain catastrophizing.[100] However, such dynamics may be far from pleasant as the expressions of pain by pain catastrophizers, although on one hand solicit support and compassionate proximity, may actually lead to punitive interpersonal responses and relationship conflicts.[99,101–103] Cano et al.[103] recruited married individuals with chronic pain and via hierarchical regression analysis, they found that positive support responses were associated with short period of pain while negative responses with longer pain period. On a broader interpersonal scale, Lackner et al.[104] performed circumplex analysis on interpersonal behavior and proposed that pain-catastrophizing stems from a submissive interpersonal style with high dependency and demand for care and support. Having said, Severeijns et al.[96] queried the need of this communal coping model for pain catastrophizing as according to the appraisal model, the three domains of ruminative thinking, magnification of pain and feeling of helplessness will impinge upon subsequent interpersonal and support mechanisms, hence making the communal coping model redundant.
CAN PAIN MODELS EXPLAIN PAIN CATASTROPHIZING?
Transactional model of stress
First described in 1980's by Lazarus and Folkman,[105] stress is viewed as a relational product between the person and the environment, and stress arises when the individual judges that the environmental demands exceed the individual's own resources.[106] It involves two appraisal processes: the primary appraisal occurs when the individual makes sense of the encounter and determines its nature as challenging, harmful or threatening; the secondary appraisal evaluates the coping resources and decides on what can be done.[107] It has been shown in patients with fibromyalgia, the level of perceived stress has a significant bearing on the symptoms severity and illness impact, lending support to this transactional model which states that when pain (stressor) is initially appraised as way beyond the individual's coping mechanisms, then secondary appraisal as to what can be done will be defective and the individual will felt helpless and pessimistic without a solution and revert to primary appraisal of the stressor in a detrimental feedback loop, resulting in a positive amplification of the pain sensation and gravity of the problem—hence catastrophizing.
Self-regulation model
Proposed by Carver et al. in 1982,[108] the self-regulation model states that the human mind will identify goals to modify mentation, volition and tasks performance in face of a challenge or adversity to attain more desirable outcomes.[109] These outcomes include better mental health against the threat of mortality,[110] adherence to law, standards and norms, proactive coping skills[111] especially in poverty,[112,113] maintaining adult attachment relationships and their salvage,[114] academic goals attainment,[115,116] abstinence from substance addiction[117] and also protective effects against disordered eating.[118] Moreover, some researchers consider self-regulation as an adaptive capacity which can be trained up with repeated exercises[119,120] of both the mind and the body, with the added concept that it is a limited resource dependent upon blood sugar[121] and physical stamina. According to this model, self-regulation it is likely to fail with ego depletion,[122,123] which happens when multiple self-regulation activities ended in unattained goals and drained the ego and related limited resources, hence aborting further goal-directed self-regulatory ability on subsequent tasks.[122,123] In the context of pain catastrophizing, the subject encountered the painful experience and identified goals to self-regulate but repeatedly made futile attempts, which then depleted the limited resources of the ego and the physique, hence lapsed into a state of pessimism and helplessness due to goal failure, culminating in an exaggerated response to both the extent of the pain and the gravity of the problem.
Gate control theory and neuromatrix theory
First described by Melzack and Wall in 1965, the gate-control theory[124,125] is an epoch-marking theory in the field of neuroscience which states that pain signals, as primarily mediated by the A-δ and C-fibers, can be modulated by intermediate interneurons which act as gates either to enhance or suppress the pain signal per se. These interneurons may originate at the laminar level or from higher centres of the central nervous system. Crude as it may sound, this gate-control theory pioneered the fundamental concept of modulatory pain pathways by neurons which are not nociceptive by nature. This gate-control theory remained unchallenged in the following 40 years, only to be refined by Melzack himself to the neuromatrix model,[126–128] which incorporated the essential domains of cognition and emotion pari passu with sensory inputs to form a dynamic body-self matrix which in turn generated a neurosignature manifested either as nociception, motor activity or antonomic/immune self-regulatory responses [Figure 3] One important feature of this model is that the neuromatrix is incessant and sensory input is not essential for generation of a neurosignature. This provide an explanation for most, if not all scenarios of chronic and neuropathic pain where noxious sensory input is invariably absent from the equation. In the context of pain catastrophizing, the cognitive and emotional domians of input become so dominating that the neuromatrix outputs become disproportinaland maladaptive.
Figure 3.
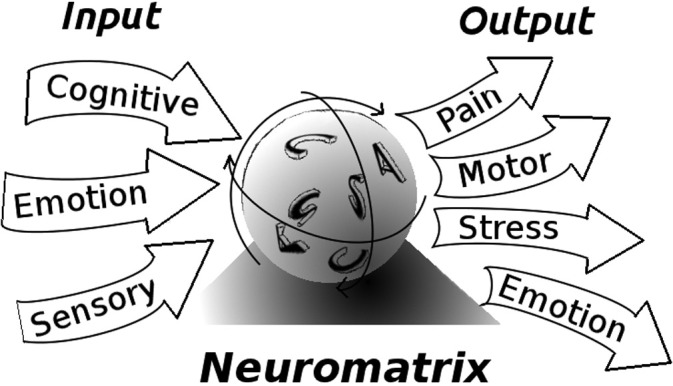
Conceptual diagram of the neuromatrix theory as a refinement of the gate-control theory. Itself visualized as an entity (like an incessant spinning sphere) comprising of the somatosensory (S), cognitive (C)and affective (A) domains, the neuromatrix receives inputs from areas of the brain governing sensation, emotions and cognitions; and in return, churns out a neurosignature (output) which activates various programs for pain recognition, motor response, emotional and stress reactions. (Adapted from Melzack, Evolution of the neuromatrix theory of pain. The Prithvi Raj Lecture: presented at the third World Congress of World Institute of Pain, Barcelona 2004. Pain Pract 2005;5:85-94.)
Conclusions and food for thought
Pain catastrophizing is a specific mindset with direct impact on the subject's behavior, functional ability and quality of living. One questionnaire study on healthy volunteers asking them to reflect on past painful experiences suggest that pain catastrophizing tendency may be pain-type specific and may associate with emotional responses to pain in younger subjects as compared to association with the actual pain intensity in older subjects.[28] On one hand, with its determinants like female sex, Asia/African race, age, certain genotypes and hormonal/neurophysiological phenotypes, pain catastrophizing can be regarded as a trait which will manifest with situational challenge. On the other hand, against a background of chronic pain, pain catastrophizing also function as a variable which can alter the prognosis and level of physical disability. Our understanding of pain catastrophizing may well be summarized as a black-box--we have good knowledge of the inputs and outputs but the processes and mechanisms that constitute the box are still unclear. Moreover, experimental attempt to manipulate the process of pain catastrophizing has concluded without success.[129] Martorella et al. reviewed 51 publications on pain catastrophizing and performed a dimensional conceptual analysis[130] with the conclusion that our present knowledge seems to reach a middle-range theory with a focus on relating pain catastrophizing with two or more concepts aiming for prevention and cure. However, there is still a logical snag: from a philosophical perspective, pain is always an internal subjective sensation which despite numerical or graphical rating, remains a feeling uniquely relating to the individual. When we attempt to use descriptives to represent the feeling in a logical form, it is instantaneously constraint by the lexicographic rules and logic implicit in the words used, which in turn would differ tremendously between different languages. Quoting the logic of famous philosopher Ludwig Wittgenstein: “the limits of my language means the limits of my world” (Tractatus: 5.6) and, “we cannot think what we cannot think; so what we cannot think we cannot say either”(Tractatus: 5.61).[131] Hence, using a reference scoring tool like the PCS to assess the complex mental set of pain catastrophizing will philosophically distort the true nature and limit the boundary of its ramifying affectivity and cognitions. Also trying to describe a mindset that is not experienced or contained in the own self is always a logical and philosophical debate, albeit how scientifically rigorous it would seem.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Ellis A. Reason and emotion in psychotherapy. New York: L. Stuart; 1962. p. 442. [Google Scholar]
- 2.Beck AT. Cognitive therapy of depression. New York: Guilford Press; 1979. p. 425. [Google Scholar]
- 3.Sung YM. Understanding the Ji Gui Yao Lue: A Comprehensive Textbook. Beijing: People's Medical Publishing House; 2010. p. 726. [Google Scholar]
- 4.Maupassant Gd, Riou É. Sur l’eau. Paris: C. Marpon et E. Flammarion; 1888. p. 3. p. l., 246. [Google Scholar]
- 5.Budrys V. Neurological deficits in the life and works of Frida Kahlo. Eur Neurol. 2006;55:4–10. doi: 10.1159/000091136. Epub 2006/01/25. doi: 10.1159/000091136. PubMed PMID: 16432301. [DOI] [PubMed] [Google Scholar]
- 6.Spanos NP, Radtke-Bodorik HL, Ferguson JD, Jones B. The effects of hypnotic susceptibility, suggestions for analgesia, and the utilization of cognitive strategies on the reduction of pain. J Abnorm Psychol. 1979;88:282–92. doi: 10.1037//0021-843x.88.3.282. Epub 1979/06/01. PubMed PMID: 500957. [DOI] [PubMed] [Google Scholar]
- 7.Chaves JF, Brown JM. Spontaneous cognitive strategies for the control of clinical pain and stress. J Behav Med. 1987;10:263–76. doi: 10.1007/BF00846540. Epub 1987/06/01. PubMed PMID: 3612783. [DOI] [PubMed] [Google Scholar]
- 8.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: Relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. Epub 1983/09/01. PubMed PMID: 6226916. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychol Assess. 1995;7:524–32. PubMed PMID: 1996007788. [Google Scholar]
- 10.Osman A, Barrios FX, Kopper BA, Hauptmann W, Jones J, O’Neill E. Factor structure, reliability, and validity of the Pain Catastrophizing Scale. J Behav Med. 1997;20:589–605. doi: 10.1023/a:1025570508954. Epub 1998/01/16 PubMed PMID: 9429990. [DOI] [PubMed] [Google Scholar]
- 11.Yap JC, Lau J, Chen PP, Gin T, Wong T, Chan I, et al. Validation of the Chinese Pain Catastrophizing Scale (HK-PCS) in patients with chronic pain. Pain Med. 2008;9:186–95. doi: 10.1111/j.1526-4637.2007.00307.x. Epub 2008/02/27. doi: 10.1111/j.1526-4637.2007.00307.x. PubMed PMID: 18298701. [DOI] [PubMed] [Google Scholar]
- 12.Matsuoka H, Sakano Y. Assessment of cognitive aspect of pain: Development, reliability, and validation of Japanese version of pain catastrophizing scale. Jpn J Psychosom Med. 2006;47:95–102. [Google Scholar]
- 13.Matsuoka H, Himachi M, Furukawa H, Kobayashi S, Shoki H, Motoya R, et al. Cognitive profile of patients with burning mouth syndrome in the Japanese population. Odontology. 2010;98:160–4. doi: 10.1007/s10266-010-0123-6. Epub 2010/07/24. doi: 10.1007/s10266-010-0123-6. PubMed PMID: 20652795. [DOI] [PubMed] [Google Scholar]
- 14.Tremblay I, Beaulieu Y, Bernier A, Crombez G, Laliberte S, Thibault P, et al. Pain Catastrophizing Scale for Francophone Adolescents: A preliminary validation. Pain Res Manag. 2008;13:19–24. doi: 10.1155/2008/845674. Epub 2008/02/28. PubMed PMID: 18301812; PubMed Central PMCID: PMC2670806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meyer K, Sprott H, Mannion AF. Cross-cultural adaptation, reliability, and validity of the German version of the Pain Catastrophizing Scale. J Psychosom Res. 2008;64:469–78. doi: 10.1016/j.jpsychores.2007.12.004. Epub 2008/04/29. doi: 10.1016/j.jpsychores.2007.12.004. PubMed PMID: 18440399. [DOI] [PubMed] [Google Scholar]
- 16.Van Damme S, Crombez G, Bijttebier P, Goubert L, Van Houdenhove B. A confirmatory factor analysis of the Pain Catastrophizing Scale: Invariant factor structure across clinical and non-clinical populations. Pain. 2002;96:319–24. doi: 10.1016/S0304-3959(01)00463-8. Epub 2002/04/26. PubMed PMID: 11973004. [DOI] [PubMed] [Google Scholar]
- 17.Garcia Campayo J, Rodero B, Alda M, Sobradiel N, Montero J, Moreno S. Validation of the Spanish version of the Pain Catastrophizing Scale in fibromyalgia. Med Clin (Barc) 2008;131:487–92. doi: 10.1157/13127277. Epub 2008/11/15. PubMed PMID: 19007576. [DOI] [PubMed] [Google Scholar]
- 18.Papaioannou M, Skapinakis P, Damigos D, Mavreas V, Broumas G, Palgimesi A. The role of catastrophizing in the prediction of postoperative pain. Pain Med. 2009;10:1452–9. doi: 10.1111/j.1526-4637.2009.00730.x. Epub 2009/10/30. doi: 10.1111/j.1526-4637.2009.00730.x. PubMed PMID: 19863742. [DOI] [PubMed] [Google Scholar]
- 19.Miro J, Nieto R, Huguet A. The Catalan version of the Pain Catastrophizing Scale: A useful instrument to assess catastrophic thinking in whiplash patients. J Pain. 2008;9:397–406. doi: 10.1016/j.jpain.2007.12.004. Epub 2008/01/30. doi: 10.1016/j.jpain.2007.12.004. PubMed PMID: 18226964. [DOI] [PubMed] [Google Scholar]
- 20.Crombez G, Bijttebier P, Eccleston C, Mascagni T, Mertens G, Goubert L, et al. The child version of the pain catastrophizing scale (PCS-C): A preliminary validation. Pain. 2003;104:639–46. doi: 10.1016/S0304-3959(03)00121-0. Epub 2003/08/21. PubMed PMID: 12927636. [DOI] [PubMed] [Google Scholar]
- 21.Cano A, Leonard MT, Franz A. The significant other version of the Pain Catastrophizing Scale (PCS-S): Preliminary validation. Pain. 2005;119:26–37. doi: 10.1016/j.pain.2005.09.009. Epub 2005/11/22. doi: 10.1016/j.pain.2005.09.009. PubMed PMID: 16298062; PubMed Central PMCID: PMC2679670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Turner JA, Aaron LA. Pain-related catastrophizing: What is it? Clin J Pain. 2001;17:65–71. doi: 10.1097/00002508-200103000-00009. Epub 2001/04/06. PubMed PMID: 11289090. [DOI] [PubMed] [Google Scholar]
- 23.Sullivan MJ, Tripp DA, Rodgers WM, Stanish W. Catastrophizing and pain perception in sport participants. J Appl Sport Psychol. 2000;12:151–67. PubMed PMID: Peer Reviewed Journal: 2001-00851-003. [Google Scholar]
- 24.Sullivan MJL, Tripp DA, Santor D. Gender differences in pain and pain behavior: The role of catastrophizing. Cognit Ther Res. 2000;24:121–34. PubMed PMID: 2000092641. [Google Scholar]
- 25.Sullivan MJ, Rodgers WM, Wilson PM, Bell GJ, Murray TC, Fraser SN. An experimental investigation of the relation between catastrophizing and activity intolerance. Pain. 2002;100:47–53. doi: 10.1016/s0304-3959(02)00206-3. Epub 2002/11/19. doi: S0304395902002063 [pii]. PubMed PMID: 12435458. [DOI] [PubMed] [Google Scholar]
- 26.Hsieh AY, Tripp DA, Ji LJ, Sullivan MJ. Comparisons of catastrophizing, pain attitudes, and cold-pressor pain experience between chinese and European canadian young adults. J Pain. 2010;11:1187–94. doi: 10.1016/j.jpain.2010.02.015. Epub 2010/05/11. doi: 10.1016/j.jpain.2010.02.015. PubMed PMID: 20452836. [DOI] [PubMed] [Google Scholar]
- 27.Forsythe LP, Thorn B, Day M, Shelby G. Race and sex differences in primary appraisals, catastrophizing, and experimental pain outcomes. J Pain. 2011 doi: 10.1016/j.jpain.2010.11.003. Epub 2011/02/01. doi: 10.1016/j.jpain.2010.11.003. PubMed PMID: 21277836. [DOI] [PubMed] [Google Scholar]
- 28.Ruscheweyh R, Nees F, Marziniak M, Evers S, Flor H, Knecht S. Pain catastrophizing and pain-related emotions: Influence of age and type of pain. Clin J Pain. 2011 doi: 10.1097/AJP.0b013e31820fde1b. Epub 2011/03/04. doi: 10.1097/AJP.0b013e31820fde1b. PubMed PMID: 21368662. [DOI] [PubMed] [Google Scholar]
- 29.Vangronsveld KL, Peters M, Goossens M, Vlaeyen J. The influence of fear of movement and pain catastrophizing on daily pain and disability in individuals with acute whiplash injury: A daily diary study. Pain. 2008;139:449–57. doi: 10.1016/j.pain.2008.05.019. Epub 2008/08/05. doi: 10.1016/j.pain.2008.05.019. PubMed PMID:18674862. [DOI] [PubMed] [Google Scholar]
- 30.Buitenhuis J, de Jong PJ, Jaspers JP, Groothoff JW. Catastrophizing and causal beliefs in whiplash. Spine (Phila Pa 1976) 2008;33:2427–33. doi: 10.1097/BRS.0b013e318183c6ca. discussion 34. Epub 2008/10/17. doi: 10.1097/BRS.0b013e318183c6ca. PubMed PMID:18923318. [DOI] [PubMed] [Google Scholar]
- 31.Rivest K, Cote JN, Dumas JP, Sterling M, De Serres SJ. Relationships between pain thresholds, catastrophizing and gender in acute whiplash injury. Man Ther. 2010;15:154–9. doi: 10.1016/j.math.2009.10.001. Epub 2009/11/07. doi: 10.1016/j.math.2009.10.001. PubMed PMID: 19892580. [DOI] [PubMed] [Google Scholar]
- 32.Soderlund A, Asenlof P. The mediating role of self-efficacy expectations and fear of movement and (re)injury beliefs in two samples of acute pain. Disabil Rehabil. 2010;32:2118–26. doi: 10.3109/09638288.2010.483036. Epub 2010/05/07. doi: 10.3109/09638288.2010.483036. PubMed PMID: 20443673. [DOI] [PubMed] [Google Scholar]
- 33.Jensen I, Nygren A, Gamberale F, Goldie I, Westerholm P. Coping with long-term musculoskeletal pain and its consequences: Is gender a factor? Pain. 1994;57:167–72. doi: 10.1016/0304-3959(94)90220-8. Epub 1994/05/01. PubMed PMID: 8090513. [DOI] [PubMed] [Google Scholar]
- 34.Keefe FJ, Lefebvre JC, Egert JR, Affleck G, Sullivan MJ, Caldwell DS. The relationship of gender to pain, pain behavior, and disability in osteoarthritis patients: The role of catastrophizing. Pain. 2000;87:325–34. doi: 10.1016/S0304-3959(00)00296-7. Epub 2000/08/30. PubMed PMID: 10963912. [DOI] [PubMed] [Google Scholar]
- 35.Edwards RR, Goble L, Kwan A, Kudel I, McGuire L, Heinberg L, et al. Catastrophizing, pain, and social adjustment in scleroderma: Relationships with educational level. Clin J Pain. 2006;22:639–46. doi: 10.1097/01.ajp.0000210918.26159.94. Epub 2006/08/24. doi: 10.1097/01.ajp.0000210918.26159.94. PubMed PMID: 16926580. [DOI] [PubMed] [Google Scholar]
- 36.Molton IR, Stoelb BL, Jensen MP, Ehde DM, Raichle KA, Cardenas DD. Psychosocial factors and adjustment to chronic pain in spinal cord injury: Replication and cross-validation. J Rehabil Res Dev. 2009;46:31–42. doi: 10.1682/jrrd.2008.03.0044. Epub 2009/06/18. PubMed PMID: 19533518; PubMed Central PMCID: PMC2743728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thibault P, Loisel P, Durand MJ, Catchlove R, Sullivan MJ. Psychological predictors of pain expression and activity intolerance in chronic pain patients. Pain. 2008;139:47–54. doi: 10.1016/j.pain.2008.02.029. Epub 2008/04/24. doi: S0304-3959(08)00124-3 [pii] 10.1016/j. pain.2008.02.029 [doi]. PubMed PMID: 18430518. [DOI] [PubMed] [Google Scholar]
- 38.Gauthier N, Thibault P, Adams H, Sullivan MJ. Validation of a French-Canadian version of the Pain Disability Index. Pain Res Manag. 2008;13:327–33. doi: 10.1155/2008/461436. Epub 2008/08/23. PubMed PMID: 18719715; PubMed Central PMCID: PMC2671319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Borsbo B, Gerdle B, Peolsson M. Impact of the interaction between self-efficacy, symptoms and catastrophising on disability, quality of life and health in with chronic pain patients. Disabil Rehabil. 2010;32:1387–96. doi: 10.3109/09638280903419269. Epub 2010/06/02. doi: 10.3109/09638280903419269. PubMed PMID: 20513205. [DOI] [PubMed] [Google Scholar]
- 40.Lariviere C, Bilodeau M, Forget R, Vadeboncoeur R, Mecheri H. Poor back muscle endurance is related to pain catastrophizing in patients with chronic low back pain. Spine (Phila Pa 1976) 2010;35:E1178–86. doi: 10.1097/BRS.0b013e3181e53334. Epub 2010/10/01. doi: 10.1097/BRS.0b013e3181e53334. PubMed PMID: 20881658. [DOI] [PubMed] [Google Scholar]
- 41.Kovacs FM, Seco J, Royuela A, Pena A, Muriel A. The correlation between pain, catastrophizing, and disability in subacute and chronic low back pain: A study in the routine clinical practice of the spanish national health service. Spine (Phila Pa 1976) 2011;36:339–45. Epub 2010/09/09. doi: 10.1097/BRS.0b013e3181cfba29. PubMed PMID: 20823782. doi: 10.1097/BRS.0b013e3181cfba29. [DOI] [PubMed] [Google Scholar]
- 42.Van Eijsden-Besseling MD, van Attekum A, de Bie RA, Staal JB. Pain catastrophizing and lower physical fitness in a sample of computer screen workers with early non-specific upper limb disorders: A case-control study. Ind Health. 2010;48:818–23. doi: 10.2486/indhealth.ms1118. Epub 2010/07/10. PubMed PMID: 20616465. [DOI] [PubMed] [Google Scholar]
- 43.Bergbom S, Boersma K, Overmeer T, Linton SJ. Relationship among pain catastrophizing, depressed mood, and outcomes across physical therapy treatments. Phys Ther. 2011 doi: 10.2522/ptj.20100136. Epub 2011/04/01. doi: 10.2522/ptj.20100136. PubMed PMID: 21451092. [DOI] [PubMed] [Google Scholar]
- 44.Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: Evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80:329–39. doi: 10.1016/s0304-3959(98)00229-2. Epub 1999/04/16. PubMed PMID: 10204746. [DOI] [PubMed] [Google Scholar]
- 45.Swinkels-Meewisse IE, Roelofs J, Oostendorp RA, Verbeek AL, Vlaeyen JW. Acute low back pain: Pain-related fear and pain catastrophizing influence physical performance and perceived disability. Pain. 2006;120:36–43. Epub 2005/12/20. doi: 10.1016/j.pain.2005.10.005. PubMed PMID: 16359797. doi: 10.1016/j.pain.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 46.Edwards RR, Smith MT, Stonerock G, Haythornthwaite JA. Pain-related catastrophizing in healthy women is associated with greater temporal summation of and reduced habituation to thermal pain. Clin J Pain. 2006;22:730–7. doi: 10.1097/01.ajp.0000210914.72794.bc. Epub 2006/09/22. doi: 10.1097/01.ajp.0000210914.72794.bc. PubMed PMID: 16988570. [DOI] [PubMed] [Google Scholar]
- 47.Dixon KE, Thorn BE, Ward LC. An evaluation of sex differences in psychological and physiological responses to experimentally-induced pain: A path analytic description. Pain. 2004;112:188–96. doi: 10.1016/j.pain.2004.08.017. Epub 2004/10/21. doi: 10.1016/j. pain.2004.08.017. PubMed PMID: 15494200. [DOI] [PubMed] [Google Scholar]
- 48.Campbell CM, Kronfli T, Buenaver LF, Smith MT, Berna C, Haythornthwaite JA, et al. Situational versus dispositional measurement of catastrophizing: Associations with pain responses in multiple samples. J Pain. 2010;11:443–53 e2. doi: 10.1016/j.jpain.2009.08.009. Epub 2010/05/05. doi: 10.1016/j.jpain.2009.08.009. PubMed PMID: 20439057; PubMed Central PMCID: PMC2898132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hirsh AT, George SZ, Riley JL, 3rd, Robinson ME. An evaluation of the measurement of pain catastrophizing by the coping strategies questionnaire. Eur J Pain. 2007;11:75–81. doi: 10.1016/j.ejpain.2005.12.010. Epub 2006/03/21. doi: 10.1016/j.ejpain.2005.12.010. PubMed PMID: 16545973. [DOI] [PubMed] [Google Scholar]
- 50.Sullivan MJ, D’Eon JL. Relation between catastrophizing and depression in chronic pain patients. J Abnorm Psychol. 1990;99:260–3. doi: 10.1037//0021-843x.99.3.260. Epub 1990/08/01. PubMed PMID: 2145334. [DOI] [PubMed] [Google Scholar]
- 51.Affleck G, Tennen H, Urrows S, Higgins P. Neuroticism and the pain-mood relation in rheumatoid arthritis: Insights from a prospective daily study. J Consult Clin Psychol. 1992;60:119–26. doi: 10.1037//0022-006x.60.1.119. Epub 1992/02/01. PubMed PMID: 1556274. [DOI] [PubMed] [Google Scholar]
- 52.George SZ, Dannecker EA, Robinson ME. Fear of pain, not pain catastrophizing, predicts acute pain intensity, but neither factor predicts tolerance or blood pressure reactivity: An experimental investigation in pain-free individuals. Eur J Pain. 2006;10:457–65. doi: 10.1016/j.ejpain.2005.06.007. Epub 2005/08/13. doi: 10.1016/j. ejpain.2005.06.007. PubMed PMID: 16095935. [DOI] [PubMed] [Google Scholar]
- 53.Sullivan MJ, Thorn B, Rodgers W, Ward LC. Path model of psychological antecedents to pain experience: Experimental and clinical findings. Clin J Pain. 2004;20:164–73. doi: 10.1097/00002508-200405000-00006. Epub 2004/04/22. PubMed PMID: 15100592. [DOI] [PubMed] [Google Scholar]
- 54.Geisser ME, Robinson ME, Keefe FJ, Weiner ML. Catastrophizing, depression and the sensory, affective and evaluative aspects of chronic pain. Pain. 1994;59:79–83. doi: 10.1016/0304-3959(94)90050-7. Epub 1994/10/01. PubMed PMID: 7854806. [DOI] [PubMed] [Google Scholar]
- 55.Sullivan MJ, Stanish W, Waite H, Sullivan M, Tripp DA. Catastrophizing, pain, and disability in patients with soft-tissue injuries. Pain. 1998;77:253–60. doi: 10.1016/S0304-3959(98)00097-9. Epub 1998/11/10. PubMed PMID: 9808350. [DOI] [PubMed] [Google Scholar]
- 56.Martin MY, Bradley LA, Alexander RW, Alarcon GS, Triana-Alexander M, Aaron LA, et al. Coping strategies predict disability in patients with primary fibromyalgia. Pain. 1996;68:45–53. doi: 10.1016/S0304-3959(96)03179-X. Epub 1996/11/01. PubMed PMID: 9251997. [DOI] [PubMed] [Google Scholar]
- 57.Turner JA, Brister H, Huggins K, Mancl L, Aaron LA, Truelove EL. Catastrophizing is associated with clinical examination findings, activity interference, and health care use among patients with temporomandibular disorders. J Orofac Pain. 2005;19:291–300. Epub 2005/11/11. PubMed PMID: 16279480. [PubMed] [Google Scholar]
- 58.Turner JA, Jensen MP, Warms CA, Cardenas DD. Catastrophizing is associated with pain intensity, psychological distress, and pain-related disability among individuals with chronic pain after spinal cord injury. Pain. 2002;98:127–34. doi: 10.1016/s0304-3959(02)00045-3. Epub 2002/07/06. PubMed PMID: 12098624. [DOI] [PubMed] [Google Scholar]
- 59.Turner JA, Mancl L, Aaron LA. Pain-related catastrophizing: A daily process study. Pain. 2004;110:103–11. doi: 10.1016/j.pain.2004.03.014. Epub 2004/07/28. doi: 10.1016/j.pain.2004.03.014. PubMed PMID: 15275757. [DOI] [PubMed] [Google Scholar]
- 60.Turner JA, Jensen MP, Romano JM. Do beliefs, coping, and catastrophizing independently predict functioning in patients with chronic pain? Pain. 2000;85:115–25. doi: 10.1016/s0304-3959(99)00259-6. Epub 2000/02/29. PubMed PMID: 10692610. [DOI] [PubMed] [Google Scholar]
- 61.Mounce C, Keogh E, Eccleston C. A principal components analysis of negative affect-related constructs relevant to pain: Evidence for a three component structure. J Pain. 2010;11:710–7. doi: 10.1016/j.jpain.2009.10.014. Epub 2009/12/18. doi: 10.1016/j.jpain.2009.10.014. PubMed PMID: 20015698. [DOI] [PubMed] [Google Scholar]
- 62.Goodin BR, McGuire L, Allshouse M, Stapleton L, Haythornthwaite JA, Burns N, et al. Associations between catastrophizing and endogenous pain-inhibitory processes: Sex differences. J Pain. 2009;10:180–90. doi: 10.1016/j.jpain.2008.08.012. Epub 2008/11/18. doi:10.1016/j.jpain.2008.08.012. PubMed PMID: 19010738. [DOI] [PubMed] [Google Scholar]
- 63.Elklit A, Jones A. The association between anxiety and chronic pain after whiplash injury: Gender-specific effects. Clin J Pain. 2006;22:487–90. doi: 10.1097/01.ajp.0000208247.18251.bb. Epub 2006/06/15. doi: 10.1097/01.ajp.0000208247.18251.bb. PubMed PMID: 16772804. [DOI] [PubMed] [Google Scholar]
- 64.Jones A, Elklit A. The association between gender, coping style and whiplash related symptoms in sufferers of whiplash associated disorder. Scand J Psychol. 2007;48:75–80. doi: 10.1111/j.1467-9450.2006.00543.x. Epub 2007/01/30. doi: 10.1111/j.1467-9450.2006.00543.x. PubMed PMID: 17257372. [DOI] [PubMed] [Google Scholar]
- 65.Edwards RR, Fillingim RB. Age-associated differences in responses to noxious stimuli. J Gerontol A Biol Sci Med Sci. 2001;56:M180–5. doi: 10.1093/gerona/56.3.m180. Epub 2001/03/17. PubMed PMID: 11253160. [DOI] [PubMed] [Google Scholar]
- 66.Edwards RR, Fillingim RB. Effects of age on temporal summation and habituation of thermal pain: Clinical relevance in healthy older and younger adults. J Pain. 2001;2:307–17. doi: 10.1054/jpai.2001.25525. Epub 2003/11/19. doi: 10.1054/jpai.2001.25525. PubMed PMID: 14622810. [DOI] [PubMed] [Google Scholar]
- 67.Edwards RR, Fillingim RB, Ness TJ. Age-related differences in endogenous pain modulation: A comparison of diffuse noxious inhibitory controls in healthy older and younger adults. Pain. 2003;101:155–65. doi: 10.1016/s0304-3959(02)00324-x. Epub 2003/01/01. PubMed PMID: 12507710. [DOI] [PubMed] [Google Scholar]
- 68.Lariviere M, Goffaux P, Marchand S, Julien N. Changes in pain perception and descending inhibitory controls start at middle age in healthy adults. Clin J Pain. 2007;23:506–10. doi: 10.1097/AJP.0b013e31806a23e8. Epub 2007/06/19. doi: 10.1097/AJP.0b013e31806a23e8. PubMed PMID: 17575490. [DOI] [PubMed] [Google Scholar]
- 69.Riley JL, 3rd, King CD, Wong F, Fillingim RB, Mauderli AP. Lack of endogenous modulation and reduced decay of prolonged heat pain in older adults. Pain. 2010;150:153–60. doi: 10.1016/j.pain.2010.04.020. Epub 2010/06/16. doi: 10.1016/j.pain.2010.04.020. PubMed PMID: 20546997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Moore AR, Clinch D. Underlying mechanisms of impaired visceral pain perception in older people. J Am Geriatr Soc. 2004;52:132–6. doi: 10.1111/j.1532-5415.2004.52023.x. Epub 2003/12/23. PubMed PMID: 14687328. [DOI] [PubMed] [Google Scholar]
- 71.Gibson SJ, Helme RD. Age-related differences in pain perception and report. Clin Geriatr Med. 2001;17:433–56. doi: 10.1016/s0749-0690(05)70079-3. v-vi. Epub 2001/07/19. PubMed PMID: 11459714. [DOI] [PubMed] [Google Scholar]
- 72.Rahim-Williams FB, Riley JL, 3rd, Herrera D, Campbell CM, Hastie BA, Fillingim RB. Ethnic identity predicts experimental pain sensitivity in African Americans and Hispanics. Pain. 2007;129:177–84. doi: 10.1016/j.pain.2006.12.016. Epub 2007/02/14. doi: 10.1016/j.pain.2006.12.016. PubMed PMID: 17296267; PubMed Central PMCID: PMC1925263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Edwards RR, Fillingim RB. Ethnic differences in thermal pain responses. Psychosom Med. 1999;61:346–54. doi: 10.1097/00006842-199905000-00014. Epub 1999/06/15. PubMed PMID: 10367615. [DOI] [PubMed] [Google Scholar]
- 74.Chapman WP, Jones CM. Variations in cutaneous and visceral pain sensitivity in normal subjects. J Clin Invest. 1944;23:81–91. doi: 10.1172/JCI101475. Epub 1944/01/01. doi: 10.1172/JCI101475 [doi]. PubMed PMID: 16695086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Edwards RR, Doleys DM, Fillingim RB, Lowery D. Ethnic differences in pain tolerance: Clinical implications in a chronic pain population. Psychosom Med. 2001;63:316–23. doi: 10.1097/00006842-200103000-00018. Epub 2001/04/09. PubMed PMID: 11292281. [DOI] [PubMed] [Google Scholar]
- 76.Watson PJ, Latif RK, Rowbotham DJ. Ethnic differences in thermal pain responses: A comparison of South Asian and White British healthy males. Pain. 2005;118:194–200. doi: 10.1016/j.pain.2005.08.010. Epub 2005/10/06. doi: 10.1016/j.pain.2005.08.010. PubMed PMID: 16202529. [DOI] [PubMed] [Google Scholar]
- 77.George SZ, Dover GC, Wallace MR, Sack BK, Herbstman DM, Aydog E, et al. Biopsychosocial influence on exercise-induced delayed onset muscle soreness at the shoulder: Pain catastrophizing and catechol-o-methyltransferase (COMT) diplotype predict pain ratings. Clin J Pain. 2008;24:793–801. doi: 10.1097/AJP.0b013e31817bcb65. Epub 2008/10/22. doi: 10.1097/AJP.0b013e31817bcb65 [doi] 00002508-200811000-00007 [pii]. PubMed PMID: 18936597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.George SZ, Wallace MR, Wright TW, Moser MW, Greenfield WH, 3rd, Sack BK, et al. Evidence for a biopsychosocial influence on shoulder pain: Pain catastrophizing and catechol-O-methyltransferase (COMT) diplotype predict clinical pain ratings. Pain. 2008;136:53–61. doi: 10.1016/j.pain.2007.06.019. Epub 2007/08/10. doi: S0304-3959(07)00346-6 [pii] 10.1016/j.pain.2007.06.019 [doi]. PubMed PMID: 17686583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Finan PH, Zautra AJ, Davis MC, Lemery-Chalfant K, Covault J, Tennen H. COMT moderates the relation of daily maladaptive coping and pain in fibromyalgia. Pain. 2011;152:300–7. doi: 10.1016/j.pain.2010.10.024. Epub 2010/12/07. doi: S0304-3959(10)00651- 2 [pii] 10.1016/j.pain.2010.10.024. PubMed PMID: 21130573; PubMed Central PMCID: PMC3053137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Reinscheid RK, Xu YL, Civelli O. Neuropeptide S: A new player in the modulation of arousal and anxiety. Mol Interv. 2005;5:42–6. doi: 10.1124/mi5.1.8. Epub 2005/02/26. doi: 5/1/42 [pii] 10.1124/mi5.1.8. PubMed PMID: 15731503. [DOI] [PubMed] [Google Scholar]
- 81.Pape HC, Jungling K, Seidenbecher T, Lesting J, Reinscheid RK. Neuropeptide S: A transmitter system in the brain regulating fear and anxiety. Neuropharmacology. 2010;58:29–34. doi: 10.1016/j.neuropharm.2009.06.001. Epub 2009/06/16. doi: S0028-3908(09)00155- 5 [pii] 10.1016/j.neuropharm.2009.06.001. PubMed PMID: 19523478; PubMed Central PMCID: PMC2784192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Raczka KA, Gartmann N, Mechias ML, Reif A, Buchel C, Deckert J, et al. A neuropeptide S receptor variant associated with overinterpretation of fear reactions: A potential neurogenetic basis for catastrophizing. Mol Psychiatry. 2010;15:1045–67-74. doi: 10.1038/mp.2010.79. Epub 2010/07/16. doi: mp201079 [pii] 10.1038/mp.2010.79. PubMed PMID: 20628342. [DOI] [PubMed] [Google Scholar]
- 83.Edwards RR, Kronfli T, Haythornthwaite JA, Smith MT, McGuire L, Page GG. Association of catastrophizing with interleukin-6 responses to acute pain. Pain. 2008;140:135–44. doi: 10.1016/j.pain.2008.07.024. Epub 2008/09/10. doi: 10.1016/j.pain.2008.07.024. PubMed PMID: 18778895; PubMed Central PMCID: PMC2659503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gracely RH, Geisser ME, Giesecke T, Grant MA, Petzke F, Williams DA, et al. Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain. 2004;127(Pt 4):835–43. doi: 10.1093/brain/awh098. Epub 2004/02/13. doi: 10.1093/brain/awh098. PubMed PMID: 14960499. [DOI] [PubMed] [Google Scholar]
- 85.Weissman-Fogel I, Sprecher E, Pud D. Effects of catastrophizing on pain perception and pain modulation. Exp Brain Res. 2008;186:79–85. doi: 10.1007/s00221-007-1206-7. Epub 2007/11/22. doi: 10.1007/s00221-007-1206-7. PubMed PMID: 18030455. [DOI] [PubMed] [Google Scholar]
- 86.Quartana PJ, Buenaver LF, Edwards RR, Klick B, Haythornthwaite JA, Smith MT. Pain catastrophizing and salivary cortisol responses to laboratory pain testing in temporomandibular disorder and healthy participants. J Pain. 2010;11:186–94. doi: 10.1016/j.jpain.2009.07.008. Epub 2009/10/27. doi: 10.1016/j.jpain.2009.07.008. PubMed PMID: 19853521; PubMed Central PMCID: PMC2821973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Meredith PJ, Strong J, Feeney JA. The relationship of adult attachment to emotion, catastrophizing, control, threshold and tolerance, in experimentally-induced pain. Pain. 2006;120:44–52. doi: 10.1016/j.pain.2005.10.008. Epub 2005/12/20. doi: 10.1016/j.pain.2005.10.008. PubMed PMID: 16359795. [DOI] [PubMed] [Google Scholar]
- 88.McWilliams LA, Asmundson GJ. The relationship of adult attachment dimensions to pain-related fear, hypervigilance, and catastrophizing. Pain. 2007;127:27–34. doi: 10.1016/j.pain.2006.07.020. Epub 2006/09/12. doi: 10.1016/j.pain.2006.07.020. PubMed PMID: 16963183. [DOI] [PubMed] [Google Scholar]
- 89.Eccleston C, Crombez G. Pain demands attention: A cognitive-affective model of the interruptive function of pain. Psychol Bull. 1999;125:356–66. doi: 10.1037/0033-2909.125.3.356. Epub 1999/06/01. PubMed PMID: 10349356. [DOI] [PubMed] [Google Scholar]
- 90.Van Damme S, Crombez G, Eccleston C. Retarded disengagement from pain cues: The effects of pain catastrophizing and pain expectancy. Pain. 2002;100:111–8. doi: 10.1016/s0304-3959(02)00290-7. Epub 2002/11/19. PubMed PMID: 12435464. [DOI] [PubMed] [Google Scholar]
- 91.Van Damme S, Crombez G, Eccleston C. Disengagement from pain: The role of catastrophic thinking about pain. Pain. 2004;107:70–6. doi: 10.1016/j.pain.2003.09.023. Epub 2004/01/13. PubMed PMID: 14715391. [DOI] [PubMed] [Google Scholar]
- 92.Vancleef LM, Peters ML. Pain catastrophizing, but not injury/illness sensitivity or anxiety sensitivity, enhances attentional interference by pain. J Pain. 2006;7:23–30. doi: 10.1016/j.jpain.2005.04.003. Epub 2006/01/18. doi: 10.1016/j.jpain.2005.04.003. PubMed PMID:16414550. [DOI] [PubMed] [Google Scholar]
- 93.Michael ES, Burns JW. Catastrophizing and pain sensitivity among chronic pain patients: Moderating effects of sensory and affect focus. Ann Behav Med. 2004;27:185–94. doi: 10.1207/s15324796abm2703_6. Epub 2004/06/09. doi: 10.1207/s15324796abm2703_6. PubMed PMID: 15184094. [DOI] [PubMed] [Google Scholar]
- 94.Quartana PJ, Burns JW, Lofland KR. Attentional strategy moderates effects of pain catastrophizing on symptom-specific physiological responses in chronic low back pain patients. J Behav Med. 2007;30:221–31. doi: 10.1007/s10865-007-9101-z. Epub 2007/04/20. doi: 10.1007/s10865-007-9101-z. PubMed PMID: 17443402. [DOI] [PubMed] [Google Scholar]
- 95.Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17:52–64. doi: 10.1097/00002508-200103000-00008. Epub 2001/04/06. PubMed PMID: 11289089. [DOI] [PubMed] [Google Scholar]
- 96.Severeijns R, Vlaeyen JW, van den Hout MA. Do we need a communal coping model of pain catastrophizing? An alternative explanation. Pain. 2004;111:226–9. doi: 10.1016/j.pain.2004.07.024. Epub 2004/09/15. doi: 10.1016/j.pain.2004.07.024. PubMed PMID:15363864. [DOI] [PubMed] [Google Scholar]
- 97.Anderson R, Hanrahan SJ. Dancing in pain: pain appraisal and coping in dancers. J Dance Med Sci. 2008;12:9–16. Epub 2008/01/01. PubMed PMID: 19618573. [PubMed] [Google Scholar]
- 98.Giardino ND, Jensen MP, Turner JA, Ehde DM, Cardenas DD. Social environment moderates the association between catastrophizing and pain among persons with a spinal cord injury. Pain. 2003;106:19–25. doi: 10.1016/s0304-3959(03)00226-4. Epub 2003/10/29. PubMed PMID:14581106. [DOI] [PubMed] [Google Scholar]
- 99.Keefe FJ, Lipkus I, Lefebvre JC, Hurwitz H, Clipp E, Smith J, et al. The social context of gastrointestinal cancer pain: A preliminary study examining the relation of patient pain catastrophizing to patient perceptions of social support and caregiver stress and negative responses. Pain. 2003;103:151–6. doi: 10.1016/s0304-3959(02)00447-5. Epub 2003/05/17. PubMed PMID: 12749969. [DOI] [PubMed] [Google Scholar]
- 100.Cano A, Leong L, Heller JB, Lutz JR. Perceived entitlement to pain-related support and pain catastrophizing: Associations with perceived and observed support. Pain. 2009;147(1- 3):249–54. doi: 10.1016/j.pain.2009.09.023. Epub 2009/10/16. doi: 10.1016/j. pain.2009.09.023. PubMed PMID: 19828251; PubMed Central PMCID: PMC2787815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Boothby JL, Thorn BE, Overduin LY, Ward LC. Catastrophizing and perceived partner responses to pain. Pain. 2004;109:500–6. doi: 10.1016/j.pain.2004.02.030. Epub 2004/05/26. doi: 10.1016/j.pain.2004.02.030. PubMed PMID: 15157712. [DOI] [PubMed] [Google Scholar]
- 102.Buenaver LF, Edwards RR, Haythornthwaite JA. Pain-related catastrophizing and perceived social responses: Inter-relationships in the context of chronic pain. Pain. 2007;127:234–42. doi: 10.1016/j.pain.2006.08.018. Epub 2006/10/03. doi: 10.1016/j.pain.2006.08.018. PubMed PMID: 17011706; PubMed Central PMCID: PMC1866270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cano A. Pain catastrophizing and social support in married individuals with chronic pain: The moderating role of pain duration. Pain. 2004;110:656–64. doi: 10.1016/j.pain.2004.05.004. Epub 2004/08/04. doi: 10.1016/j.pain.2004.05.004. PubMed PMID: 15288406; PubMed Central PMCID: PMC2396732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lackner JM, Gurtman MB. Pain catastrophizing and interpersonal problems: A circumplex analysis of the communal coping model. Pain. 2004;110:597–604. doi: 10.1016/j.pain.2004.04.011. Epub 2004/08/04. doi: 10.1016/j.pain.2004.04.011. PubMed PMID:15288400. [DOI] [PubMed] [Google Scholar]
- 105.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer Pub. Co; 1984. p. xiii. 445. [Google Scholar]
- 106.Dewe P. Determinants of coping: Some alternative explanations and measurement issues. Psychol Rep. 2001;88(3 Pt 1):832–4. doi: 10.2466/pr0.2001.88.3.832. Epub 2001/08/18. PubMed PMID: 11508028. [DOI] [PubMed] [Google Scholar]
- 107.Folkman S. An approach to the measurement of coping. Journal of Occupational Behaviour. 1982;3:95–107. [Google Scholar]
- 108.Carver CS, Scheier MF. Control theory: A useful conceptual framework for personality-social, clinical, and health psychology. Psychol Bull. 1982;92:111–35. Epub 1982/07/01. PubMed PMID: 7134324. [PubMed] [Google Scholar]
- 109.Muraven M, Baumeister RF. Self-regulation and depletion of limited resources: Does self-control resemble a muscle? Psychol Bull. 2000;126:247–59. doi: 10.1037/0033-2909.126.2.247. Epub 2000/04/05. PubMed PMID: 10748642. [DOI] [PubMed] [Google Scholar]
- 110.Gailliot MT, Schmeichel BJ, Baumeister RF. Self-regulatory processes defend against the threat of death: Effects of self-control depletion and trait self-control on thoughts and fears of dying. J Pers Soc Psychol. 2006;91:49–62. doi: 10.1037/0022-3514.91.1.49. Epub 2006/07/13. doi: 10.1037/0022-3514.91.1.49. PubMed PMID: 16834479. [DOI] [PubMed] [Google Scholar]
- 111.Aspinwall LG, Taylor SE. A stitch in time: Self-regulation and proactive coping. Psychol Bull. 1997;121:417–36. doi: 10.1037/0033-2909.121.3.417. Epub 1997/05/01. PubMed PMID: 9136643. [DOI] [PubMed] [Google Scholar]
- 112.Buckner JC, Mezzacappa E, Beardslee WR. Characteristics of resilient youths living in poverty: The role of self-regulatory processes. Dev Psychopathol. 2003;15:139–62. doi: 10.1017/s0954579403000087. Epub 2003/07/10. PubMed PMID: 12848439. [DOI] [PubMed] [Google Scholar]
- 113.Buckner JC, Mezzacappa E, Beardslee WR. Self-regulation and its relations to adaptive functioning in low income youths. Am J Orthopsychiatry. 2009;79:19–30. doi: 10.1037/a0014796. Epub 2009/03/18. doi: 10.1037/a0014796. PubMed PMID: 19290722. [DOI] [PubMed] [Google Scholar]
- 114.Sbarra DA, Hazan C. Coregulation, dysregulation, self-regulation: An integrative analysis and empirical agenda for understanding adult attachment, separation, loss, and recovery. Pers Soc Psychol Rev. 2008;12:141–67. doi: 10.1177/1088868308315702. Epub 2008/05/06. doi: 10.1177/1088868308315702. PubMed PMID: 18453476. [DOI] [PubMed] [Google Scholar]
- 115.Weed K, Keogh D, Borkowski JG, Whitman T, Noria CW. Self-Regulation mediates the relationship between learner typology and achievement in at - risk children. Learn Individ Differ. 2011;21:96–108. doi: 10.1016/j.lindif.2010.10.006. Epub 2011/02/01. doi: 10.1016/j.lindif.2010.10.006. PubMed PMID: 21278904; PubMed Central PMCID: PMC3026284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Duckworth AL, Seligman ME. Self-discipline outdoes IQ in predicting academic performance of adolescents. Psychol Sci. 2005;16:939–44. doi: 10.1111/j.1467-9280.2005.01641.x. Epub 2005/11/30. doi: 10.1111/j.1467-9280.2005.01641.x. PubMed PMID: 16313657. [DOI] [PubMed] [Google Scholar]
- 117.Ferrari JR, Stevens EB, Jason LA. The relationship of self-control and abstinence maintenance: An exploratory analysis of self-regulation. J Groups Addict Recover. 2009;4:32–41. doi: 10.1080/15560350802712371. Epub 2009/01/01. doi: 10.1080/15560350802712371. PubMed PMID: 20689650; PubMed Central PMCID: PMC2916178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Scoffier S, Paquet Y, d’Arripe-Longueville F. Effect of locus of control on disordered eating in athletes: The mediational role of self-regulation of eating attitudes. Eat Behav. 2010;11:164–9. doi: 10.1016/j.eatbeh.2010.02.002. Epub 2010/05/04. doi: 10.1016/j.eatbeh.2010.02.002. PubMed PMID: 20434063. [DOI] [PubMed] [Google Scholar]
- 119.Muraven M, Baumeister RF, Tice DM. Longitudinal improvement of self-regulation through practice: Building self-control strength through repeated exercise. J Soc Psychol. 1999;139:446–57. doi: 10.1080/00224549909598404. Epub 1999/08/24. PubMed PMID: 10457761. [DOI] [PubMed] [Google Scholar]
- 120.Baumeister RF, Gailliot M, DeWall CN, Oaten M. Self-regulation and personality: How interventions increase regulatory success, and how depletion moderates the effects of traits on behavior. J Pers. 2006;74:1773–801. doi: 10.1111/j.1467-6494.2006.00428.x. Epub 2006/11/07. doi: 10.1111/j.1467-6494.2006.00428.x. PubMed PMID: 17083666. [DOI] [PubMed] [Google Scholar]
- 121.Gailliot MT, Baumeister RF, DeWall CN, Maner JK, Plant EA, Tice DM, et al. Self-control relies on glucose as a limited energy source: Willpower is more than a metaphor. J Pers Soc Psychol. 2007;92:325–36. doi: 10.1037/0022-3514.92.2.325. Epub 2007/02/07. doi: 10.1037/0022-3514.92.2.325. PubMed PMID: 17279852. [DOI] [PubMed] [Google Scholar]
- 122.Baumeister RF. Ego depletion and self-regulation failure: A resource model of self-control. Alcohol Clin Exp Res. 2003;27:281–4. doi: 10.1097/01.ALC.0000060879.61384.A4. Epub 2003/02/27. doi: 10.1097/01.ALC.0000060879.61384.A4. PubMed PMID: 12605077. [DOI] [PubMed] [Google Scholar]
- 123.Baumeister RF, Bratslavsky E, Muraven M, Tice DM. Ego depletion: Is the active self a limited resource? J Pers Soc Psychol. 1998;74:1252–65. doi: 10.1037//0022-3514.74.5.1252. Epub 1998/05/26. PubMed PMID:9599441. [DOI] [PubMed] [Google Scholar]
- 124.Melzack R, Wall PD. Pain mechanisms: A new theory. Science. 1965;150:971–9. doi: 10.1126/science.150.3699.971. Epub 1965/11/19. PubMed PMID: 5320816. [DOI] [PubMed] [Google Scholar]
- 125.Britton NF, Skevington SM. A mathematical model of the gate control theory of pain. J Theor Biol. 1989;137:91–105. doi: 10.1016/s0022-5193(89)80151-1. Epub 1989/03/07. PubMed PMID: 2593677. [DOI] [PubMed] [Google Scholar]
- 126.Melzack R. From the gate to the neuromatrix. Pain. 1999;(Suppl 6):S121–6. doi: 10.1016/S0304-3959(99)00145-1. Epub 1999/09/24. PubMed PMID:10491980. [DOI] [PubMed] [Google Scholar]
- 127.Melzack R. Evolution of the neuromatrix theory of pain. The Prithvi Raj Lecture: Presented at the third World Congress of World Institute of Pain, Barcelona 2004. Pain Pract. 2004;5:85–94. doi: 10.1111/j.1533-2500.2005.05203.x. Epub 2006/12/21. doi: PPR5203 [pii] 10.1111/j.1533-2500.2005.05203.x [doi]. PubMed PMID:17177754. [DOI] [PubMed] [Google Scholar]
- 128.Melzack R. Pain and the neuromatrix in the brain. J Dent Educ. 2001;65:1378–82. Epub 2002/01/10. PubMed PMID:11780656. [PubMed] [Google Scholar]
- 129.Bialosky JE, Hirsh AT, Robinson ME, George SZ. Manipulation of pain catastrophizing: An experimental study of healthy participants. J Pain Res. 2008;1:35–41. Epub 2008/01/01. PubMed PMID: 21197286; PubMed Central PMCID: PMC3004615. [PMC free article] [PubMed] [Google Scholar]
- 130.Martorella G, Cote J, Choiniere M. Pain catastrophizing: A dimensional concept analysis. J Adv Nurs. 2008;63:417–26. doi: 10.1111/j.1365-2648.2008.04699.x. Epub 2008/08/30. doi: 10.1111/j.1365-2648.2008.04699.x. PubMed PMID: 18727769. [DOI] [PubMed] [Google Scholar]
- 131.Wittgenstein L, Pears D, McGuinness B. Tractatus logico-philosophicus. London New York: Routledge; 2001. p. xxv. 106. [Google Scholar]


