Abstract
Background & objectives:
The ambiguity and variability in existing literature on the magnitude of socio-economic inequality in self-reported morbidities makes it difficult to set priorities in health policy. This study examined three critical research questions: first, how far self-reporting affects measuring socio-economic inequalities in case of obstetric morbidities. Second, does using simple bivariate variations mislead in estimating socio-economic differentials in prevalence of obstetric morbidities? Finally, whether use of sophisticated regression based decomposition results can overcome such problems.
Methods:
The data from National Family Health Survey (NFHS-3; 2005-06) were used, and analyzed by statistical tools such as bivariate estimates and regression based decomposition analysis.
Results:
Bivariate results revealed that self-reported obstetric morbidity data were misleading in measurement of socio-economic differentials, as these failed to show existing socio-economic variations in obstetric morbidities by socio-economic standing of women. However, decomposition analysis showed that the prevalence of obstetric complications was greater among socioeconomically disadvantaged groups.
Interpretation & conclusions:
Based on our findings on measurement of socio-economic inequality in self-reported obstetric morbidity, we conclude that the use of regression based inequality decomposition estimates not only overcomes the problems of measuring socio-economic inequality based on self-reported morbidities, but also increases the validity of such measures.
Keywords: Decomposition analysis, EAG states, India, obstetric morbidity, self-reporting morbidities, socio-economic inequality
Across the world half a million women die of pregnancy related complications1. About a fifth of the births worldwide and a fourth of maternal deaths occur in India, particularly in the Empowered Action Group (EAG) States2. A large number of women suffer from obstetric problems and most of them belong to deprived socio-economic groups3. Obstetric morbidity has a negative effect on women's life4. Obstetric morbidity is one of the major components in larger domain of reproductive morbidity and is defined as “morbidity in pregnant women (regardless of site or duration of the pregnancy) resulting from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes”5. According to biomedical causes more than 70 per cent of maternal deaths are from direct obstetric complications and most of them occur in women with poor socio-economic status5.
In India, very little attention has been given to obstetric morbidity. The reliable information on socio-economic differentials in the incidence and prevalence of obstetric morbidity in India and its States is scarce. The self-reported obstetric morbidity data can be classified into two domains: the first domain of studies indicates that obstetric complications are negatively associated with socio-economic status. Jain and Parasuraman6 in their study based on National Family Health Survey-2 (NFHS-2) data found that socio-economically poor States such as Madhya Pradesh and Bihar have the highest percentage of obstetric morbidity in the country. The extent of obstetric complications decreases with an increase in standard of living and women's education. Another study by Sontakke et al3 based on NFHS - 3 data found that the mean numbers of obstetric morbidity were higher among women in rural areas and with low standard of living in all the selected States.
In contrast, the second domain of studies indicated that obstetric complications are positively associated with socio-economic status, more particularly with literacy levels of women. A study based on District Level Household and Facility Survey (DLHS-2) data revealed that women in the younger age group, better-educated, urban women and those with a higher standard of living have higher prevalence of obstetric morbidity in Odisha7. Narayan8 found that among lower socio-economic group, women's perceptions regarding obstetric morbidity, feeling of low self-esteem, embarrassment, and guilt are some social barriers in reporting and utilizing services for obstetric morbidity. Sen9 compared aggregated self-reported morbidity rates and life expectancy between Kerala and Bihar, with Kerala reporting considerably higher rates of morbidity despite experiencing the highest level of longevity, while Bihar with low levels of longevity reported lower rates of morbidities. The argument was that though Bihar's low life expectancy figures reflected in its disease burden, the meager provision of health services in the State coupled with its high percentage of illiterate population perhaps accounted for its poor perception of illness. Conversely, Kerala, with high levels of literacy and adequate health provision, is better positioned to identify and report self-perceived morbidities. A comparative assessment of these domains of studies presents greater ambiguity and variability in existing literature on the magnitude of socio-economic inequality in obstetric morbidity that makes priority setting in health policy for obstetric morbidity difficult.
There has been a growing concern about the misleading measurement of socio-economic differentials in self-reporting morbidities. According to Sen9, an individual's assessment of their health is directly contingent on their social experience, and this leads to less reporting of illness among socially disadvantaged individuals as they fail to perceive the presence of illness or health deficits. Majority of the poor and illiterate women do not report morbidities and do not go to health facilities as they fail to realize that they have a morbid condition. Manesh and colleagues10 argued that self-reported measures of morbidities are misleading, based on the absence of an observed association. Subramanian et al11 with empirical assessment reveal that self-reported measures of poor health and morbidities from developing countries tend to be viewed with considerable skepticism. However, there is no study, which has empirically tested the validity of self-reported health and morbidity measures in India based on examining the association between socio-economic status (SES) and self-reported morbidity measures with improved measures of socio-economic inequality in health.
Therefore, the present study was aimed to re-assess the problem of measurement of socio-economic inequality in self-reporting of obstetric morbidity in EAG States of India by using improved health inequality measures. In this study, we tested whether the association between self-reported obstetric morbidities and socio-economic status in India follows the expected association or not. The analysis was focused on EAG States namely, Rajasthan, Bihar, Uttar Pradesh, Madhya Pradesh, Odisha, Chhattisgarh, Uttaranchal, and Jharkhand, because these are demographically less developed, have a relatively weaker socio-economic condition and high obstetric morbidity.
Material & Methods
Study place and design: The present study was based on Indian National Family Health Survey-3 (NFHS-3) data conducted in 2005-200612. The survey was coordinated by International Institute for Population Sciences (IIPS) and Macro International under the tutelage of Ministry of Health and Family Welfare (MoHFW), India. The study protocol was approved by the ethics committee of IIPS, Mumbai. The study covered 1,24,385 women in the age group 15-49 yr in India. The urban and rural samples within each State were drawn separately following a multi-stage sampling design. In each State the rural sample was selected in two stages and urban sample in three stages.
Sample selection: This study was focused on currently married women having delivered at least once during the five years preceding the survey in EAG States. The ‘women file’ of NFHS-3 that provides information on specific problems that women experienced during their pregnancies was used. The informed consent of the woman was obtained prior to interview. For the most recent birth in the five years preceding the survey, women were asked whether, at any time during the pregnancy, they had experienced any of the following problems: difficulty with vision during the day light, night blindness, convulsions (not from fever), swelling of legs, body or face, excessive fatigue or vaginal bleeding and if she had excessive vaginal bleeding or very high fever - both symptoms of possible post-partum complications - at any time during the two months after the birth of her most recent child. ‘Pregnancy related problem’ and ‘post pregnancy problem’ were computed separately by using the above information. ‘Any obstetric morbidity’ was computed by using information on both ‘pregnancy related problems’ and ‘post pregnancy problems’.
Statistical analysis: The analysis was performed in three stages. In the first stage, obstetric morbidity was examined using average group differentials by socio-economic and demographic characteristics to assess their association. In the second stage, the concentration indices (CI) were estimated as measures of inequality13. Finally, to overcome the problem of measuring socio-economic inequality in self-reporting obstetric morbidity, sophisticated statistical tool namely regression based inequality decomposition analysis was used. CI of obstetric morbidity was decomposed to find the percentage contribution of different socio-economic predictors to total inequality. The regression based inequality decomposition has an advantage over other statistical tools for measuring socio-economic inequality in obstetric morbidity prevalence. It acts as multi-stage control with mean, marginal effect and CI which takes care of sample distribution along with controlling the effect of other determinants in regression14.
All analyses were carried out on STATA 10.1 (STATA crop LP, College Station, Texas, USA) and Microsoft excel program. The following steps were followed for the computation of CI and its decomposition to the related predictors13: (i) The obstetric morbidity variable was regressed against its predictors through an appropriate model for finding the coefficients of the explanatory variable (βk). (ii) Mean of the obstetric morbidity variable and each of its predictor was calculated (μ and Xk). (iii) CI for the obstetric morbidity variable and for the predictors (C and Ck) as well as the generalized CI of error term (GCε) where, yi and μ are the values of the predictors for the ith individual and the determinant mean, respectively were calculated. (iv) The absolute contribution of each predictor was calculated by multiplying the obstetric morbidity variable elasticity with respect to that predictor and its CI ---- (βkXk/μ)Ck(v) The percentage contribution of each determinant was calculated by dividing its absolute contribution by the CI of obstetric morbidity variable (βkXk/μ) Ck/C to quantify the precise contribution of each predictor included in the model to measure the inequality in the obstetric morbidity variable.
CI was computed by using the equation:
![]()
where yi and Ri are, respectively, the health status (measured in terms of prevalence of obstetric morbidity) of the ith woman and the fractional rank of the ith woman (for weighted data) in terms of the index of household economic status; μ is the (weighted) mean of the obstetric morbidity in the sample and covw denotes the weighted covariance. The CI is a refined measure which quantifies the inequalities existing among the advantaged as well as disadvantaged section of the population. Its value varies between -1 and +1. The CI negative values imply that a variable is concentrated among disadvantaged people, while the opposite is true for its positive values. However, when there is perfect equality, the value of CI will be zero.
Decomposition of concentration index: The method proposed by Wagstaff14 was used to decompose socio-economic inequalities in obstetric morbidity into its determinants. For any linear regression model, the health variable of interest i.e. obstetric morbidity, Y, is linked to a set of k socio-economic determinants, Xk. The mathematical equation depicting their relationship is given as follows:
![]()
where ε is an error term. Given the relationship between Yi and Xki the concentration index for Y ‘C’ can be written as
![]()
This equation shows that C is made up of two parts: one is deterministic or explained component and second is residual or unexplained component. The deterministic component explains the inequalities in obstetric morbidity and is equal to the weighted sum of the CI of the predictors, where weights are elasticities (elasticity is a unit free measure of partial association i.e. per cent change in the dependant variable associated with a per cent change in the predictor variable). The residual reflects that part of inequalities which remained unexplained by the selected predictors.
Definition of variables considered for decomposition analysis: A long-standing issue in the literature on health inequality is whether or not all inequalities should be measured or solely those which show some systematic association with indicators of socio-economic standing should be measured15–18. Keeping this in mind the predictor variables were specifically chosen that could systematically explain a major part of inequalities. The decomposition analysis was confined to five critical socio-economic predictors: place of residence, household economic status, women's educational status, religion and caste. All the socio-economic covariates were dichotomized and coded 1 for yes and 0 for otherwise; one was assigned to disadvantaged group. Place of residence was coded as rural/ non rural, economic status as poor/ non poor, education of women as illiterate/ literate, religion as Muslim/ non Muslim and caste as scheduled caste/ tribe (SC/ST)/ non SC/ST. In the study poor included poorest and poorer population and non poor included middle, richer and richest population. Non Muslim included Hindu and other religious groups and non SC/ST included OBCs and other forward castes. Such categorization was done as non Muslim and non SC/ST are assumed socially better off than their counterparts15–17.
Results
NFHS-3 data12 showed huge variation in non-self-reported maternal health indicators such as antenatal care (ANC) and institutional delivery coverage, etc. However, self-reported morbidities such as obstetric morbidities displayed a contrasting picture between EAG States and other Indian States. The obstetric complications did not reveal great variation among EAG States and India as a whole (Table I), though EAG States were weak in terms of socio-economic and health conditions compared with rest of Indian States. The next logical step in this analysis was assessing how self-reported obstetric morbidity varied by socio-economic standing of women.
Table I.
Percentage of currently married women* by types of problems reported, EAG states and India, 2005-2006
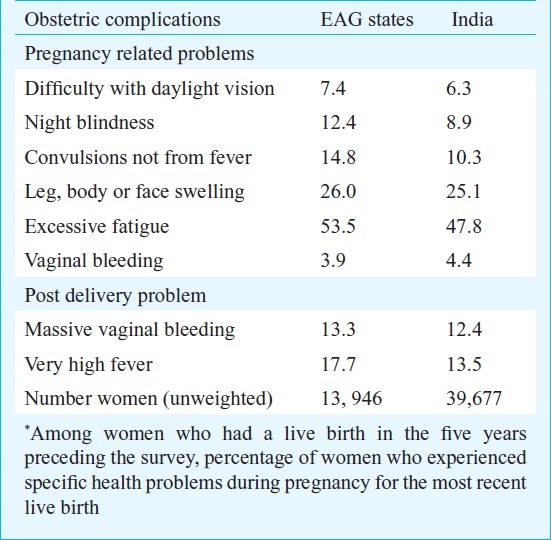
Table II presents the assessment of obstetric complications by socio-economic standing of women for EAG states. The results indicated that for EAG States as a whole, more than 50 per cent of women reported that they suffered from obstetric morbidity. Nearly, a fourth of currently married women reported post pregnancy problems. By women's age, results indicated that women in the younger age group reported maximum obstetric morbidity, which declined slightly with age. The same pattern was observed for pregnancy related and post-pregnancy problems, but with varying levels in percentages of women reporting such problems.
Table II.
Percentage of currently married women* aged 15-49 yr who reported any pre-pregnancy, post-pregnancy and obstetric complications in EAG states, India, 2005-2006
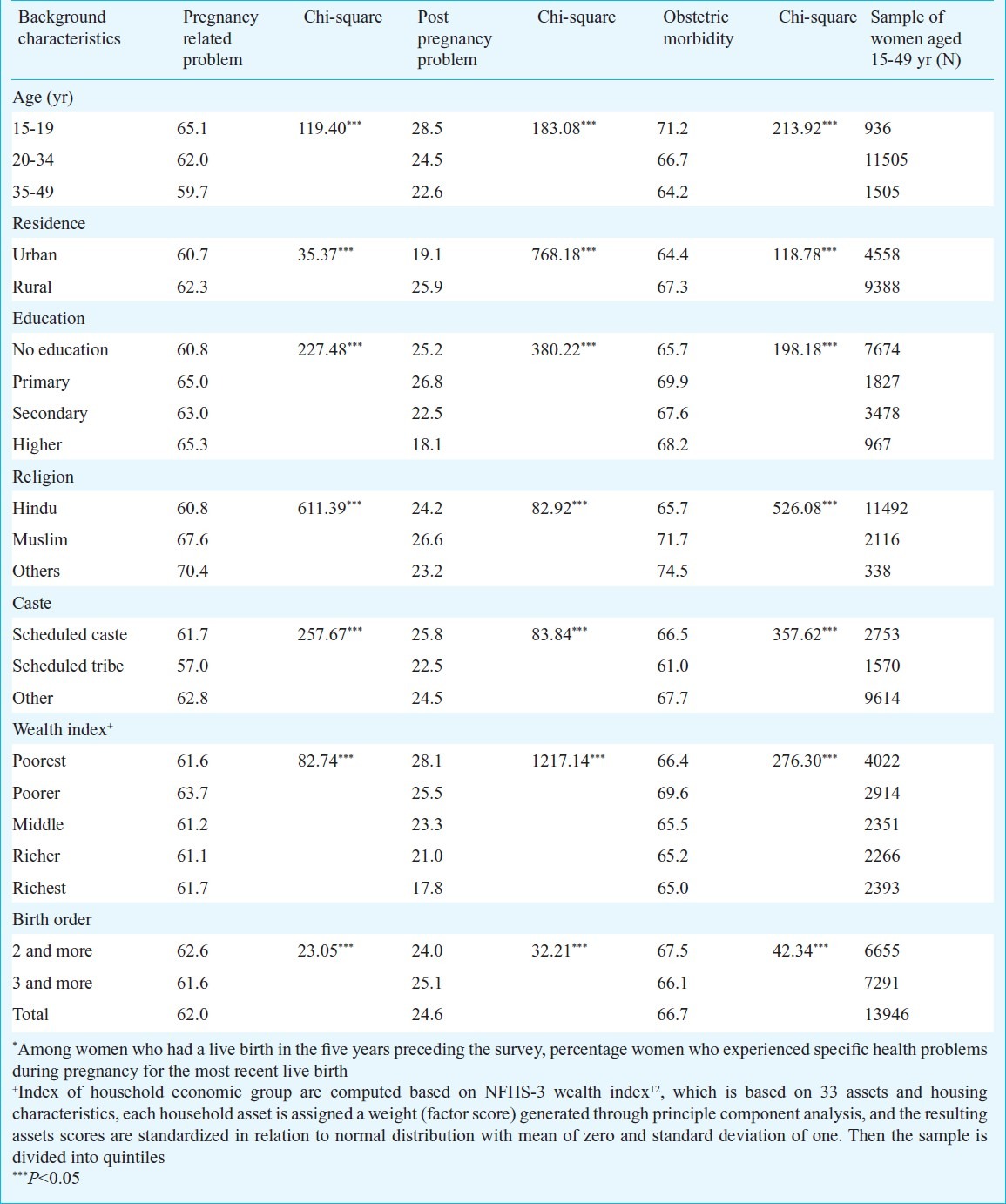
A comparative assessment of average levels of obstetric morbidity by socio-economic characteristics indicated that there was not much difference in the presence of obstetric complications among disadvantaged and advantaged socio-economic groups. Overall, the results indicated a reverse patterns compared with conventional expectations of socio-economic variation in maternal health. This, perhaps, is because with poor socio-economic standing, sometimes woman's own understanding of her health may not be in accordance with the appraisal of medical experts and thus she fails to realize that she is suffering from morbidity and does not report it. However, there could be several other factors which are likely to indicate such unpredictable and unexpected results and could not be captured by bivariate analysis. It is critical to control the bias aroused from socio-economic variations in self-reported morbidities to get correct measurement of socio-economic variation in morbidity prevalence.
To estimate correct socio-economic variation in the prevalence of obstetric morbidity based on self-reported data, regression based decomposition analysis was carried out. Table III presents mean values and CIs of the health variables and selected predictors, along with regression coefficients and percentage contributions to inequality in the prevalence of obstetric morbidity. The column one in the Table represents mean values of health variables and predictors. The results of mean values indicated that 30 per cent of currently married women in EAG States reported that they suffered from any obstetric morbidity. Further, 44 per cent of currently married women belonged to poor household economic status and 54 per cent of them were illiterate. A majority of currently married women belonged to rural area (63%). The next column presents the estimated marginal effects from regression analysis. The marginal effect indicates the direction and degree of association between the selected socio-economic determinants and prevalence of any obstetric morbidity. The results indicated that except illiteracy of women, all other selected socio-economic background characteristics of women were positively associated with obstetric morbidity.
Table III.
Effects and contribution of predictor variables based on decomposition analysis for currently married women for obstetric morbidity in EAG states, 2005-2006
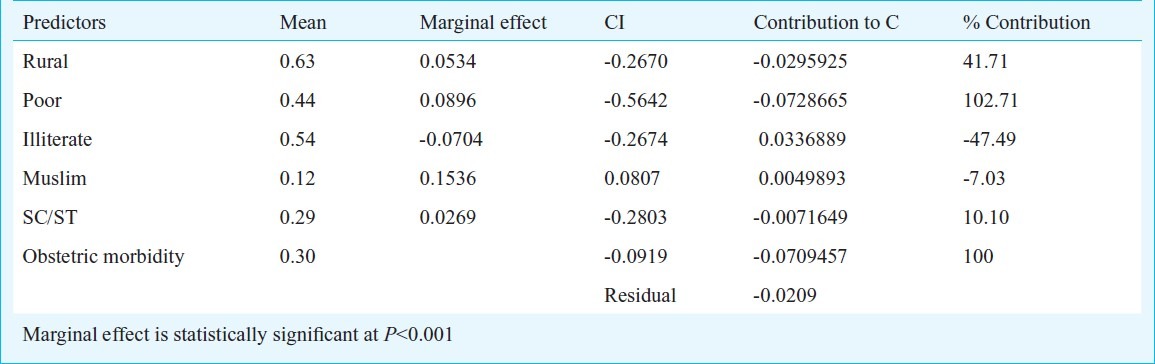
The two last columns present the decomposition estimates of socio-economic inequalities in self-reporting of obstetric morbidity. Decomposition estimates revealed that the model explained a major part of the inequalities (-0.0709 of -0.0919) in reporting of obstetric morbidity. Contrast, with simple bivariate analysis, the decomposition results demonstrated that inequalities were more among the disadvantaged socio-economic groups of society than their counterparts. Poor household economic status of women made the largest contribution, however, illiteracy seemed to be contributing in a direction against conventional belief that obstetric complications are more among illiterate than literate women. This could be because of differences in the awareness levels of literate and illiterate women, which affect the reporting of the morbidity and hence, the results. Being Muslim women contributed negatively to total inequality. Living in rural areas contributed about 40 per cent of the total inequalities in obstetric morbidity prevalence. Furthermore, the results indicated that belonging to SC/ST was also modestly contributing to total inequality in prevalence of obstetric morbidity.
The decomposition outcomes demonstrated that most of the inequalities were explained by the poor household economic status, illiteracy of women (irrespective of direction of contribution) and residing in rural areas. Moreover, the very small value of the residual (unexplained part i.e. -0.02) demonstrated that the selection of predictors was justified and that socio-economic standing of women played a key role in inequalities in prevalence of obstetric morbidity among currently married women in EAG States.
Discussion
Results suggested that self-reporting data of obstetric morbidity potentially misled the measurement of socio-economic differentials with simple bivariate estimates, as these failed to bring out the true socio-economic variation in prevalence of obstetric complications among women of EAG States. However, the application of regression based inequality decomposition analysis helped in overcoming the self-reporting bias. Decomposition results revealed that primarily, the inequalities in obstetric prevalence arose from poverty, education and residing in rural areas. However, the direction of contribution of education to the incidence of obstetric morbidity was negative. The logical explanation for this is that education of women makes about 50 per cent difference in prevalence of obstetric morbidity irrespective of its direction of association. Using regression based decomposition analysis technique not only provides expected pattern of variation but also gives better validated measures compared with earlier methods of estimating socio-economic inequalities in health.
To conclude, our analyses show that estimation of socio-economic differentials in prevalence of self-reported morbidities (obstetric morbidity in our case) is likely to be misleading. Therefore, it is important to use sophisticated regression based decomposition analyses for estimating socio-economic inequalities in self-reported morbidities. The use of regression based inequality decomposition analyses not only overcomes the reporting bias in self-reported morbidities but also increases the validity of results based on self-reported morbidities. However, more coherent elucidations of the results are needed when to infer these findings for health policy interventions, for instance, if a decomposition analysis is showing illiteracy status of women as a negative contribution that gives a number of intriguing insights: one, education is a key determinant of bias in self-reporting obstetric morbidity. Second, improvement of education is important for improving knowledge about the problem of obstetric morbidity, which helps in seeking timely health care. Lastly, education helps in reporting the problem accurately, which helps in the measurement of the magnitude of problem.
Acknowledgment
Authors acknowledge the organizers of Global Health Metric Evaluation (GHME): Controversies, Accountability and Innovations Conference, Seattle, Washington, USA, Institute for Health Metric Evaluation (IHME), The LANCET, Harvard School of public health, University of Washington and University of Queensland for meaningful discussions.
References
- 1.World Health Organization. Maternal mortality in 2005, estimates developed by WHO, UNICEF, UNFPA and the World Bank. 2005. [accessed on January 20, 2011]. Available from: http://www.who.int/reproductivehealth .
- 2.Ramasubban R, Jejeebhoy S. Women's reproductive health in India. New Delhi: Rawat Publications; 2000. [Google Scholar]
- 3.Sontakke P, Reshmi R, Sebastian D. Obstetric morbidity among currently married women in selected States of India. Indian J Fam Welfare. 2009;55:17–26. [Google Scholar]
- 4.Turan J, Jonson K, Polan M. Experiences of women seeking medical care for obstetric fistula in Eritrea: Implications for prevention, treatment, and social reintegration. Global Public Health. 2007;2:64–77. doi: 10.1080/17441690600648728. [DOI] [PubMed] [Google Scholar]
- 5.Measuring reproductive morbidity: Report of a technical working group. Geneva: WHO; 1989. World Health Organization. [Google Scholar]
- 6.Jain R, Parsuraman S. Maternal morbidity and utilization of antenatal care services: A study of Madhya Pradesh and Bihar. In: Roy TK, Guruswami M, Arokiasamy P, editors. Population, health and development in India. Jaipur: Rawat Publication; 2002. [Google Scholar]
- 7.Sahu H. Mumbai: International Institute for Population Sciences; 2004. [accessed on December 12, 2010]. Safe delivery and reproductive (Obstetric) morbidity in Orissa: exploring their possible relationship based on DLHS-RCH. Available from: http://www.iipsindia.org/library-htm . [Google Scholar]
- 8.Narayan K. Issues on obstetric morbidity: Finding from community based research. Paper presented at workshop on reproductive health in India: New evidences and issues, Pune, India. 2000. [accessed on December 20, 2010]. Available from: http://www.iywg.org/popline/issues-obstetric-morbidity-findings-community-basedresearch .
- 9.Sen A. Health: perception versus observation. BMJ. 2002;324:860–1. doi: 10.1136/bmj.324.7342.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manesh AO, Sheldon TA, Pickett KE, Carr-Hill R. Accuracy of child morbidity data in demographic and health surveys. Int J Epidemiol. 2008;37:194–200. doi: 10.1093/ije/dym202. [DOI] [PubMed] [Google Scholar]
- 11.Subramanian SV, Subramanyam MA, Selvaraj S, Kawachi I. Are self reports of health and morbidities in developing countries misleading. Evidence from India? Soc Sci Med. 2009;68:260–5. doi: 10.1016/j.socscimed.2008.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Family Health Survey (2005-06) Mumbai, India: International Institute for Population Sciences; 2006. IIPS and Macro Internationals. [Google Scholar]
- 13.Hosseinpoor AR, Doorslaer VE, Speybroeck N, Naghavi M, Mohammad K, Majdzadeh R, et al. Decomposing socioeconomic inequality in infant mortality in Iran. Int J Epidemiol. 2006;35:1211–9. doi: 10.1093/ije/dyl164. [DOI] [PubMed] [Google Scholar]
- 14.Wagstaff A. Inequality aversion, health inequalities and health achievements. J Health Econ. 2002;21:627–41. doi: 10.1016/s0167-6296(02)00006-1. [DOI] [PubMed] [Google Scholar]
- 15.Arokiasamy P, Pradhan J. Measuring wealth-based health inequality among Indian children: the importance of equity vs efficiency. Health Policy Planning. 2011;26:429–40. doi: 10.1093/heapol/czq075. [DOI] [PubMed] [Google Scholar]
- 16.Joe W, Mishra US, Navaneetham K. Inequalities in childhood malnutrition in India: some evidence on group disparities. J Hum Dev Capabil. 2009;10:417–39. [Google Scholar]
- 17.Pradhan J, Arokiasamy P. Socio-economic inequalities in child survival in India: a decomposition analysis. Health Policy. 2010;98:114–20. doi: 10.1016/j.healthpol.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 18.Wagstaff A. Poverty and health sector inequalities. Bull World Health Organ. 2002;80:97–105. [PMC free article] [PubMed] [Google Scholar]


