Abstract
Background & objectives:
Medicines can account for up to 90 per cent of health care spending by poor people. High costs of medicines contribute to decreased access to healthcare. This study was conducted to assess the cost of medicines and their affordability in the private pharmacies in Delhi, India.
Methods:
A survey was conducted to assess the costs of prescribed medicines and treatment of community acquired pneumonia (CAP), with medicines purchased from 27 private pharmacies, in Delhi. Affordability of medicines was assessed by comparing the costs of treatment (medicines) to the monthly per capita expenditure (MPCE) on food, minimum monthly and daily wages for different classes of workers.
Results:
A large variability in the costs of prescriptions was observed (129.37+ 217.99) The cost of treatment of CAP varied from  34.50- 244.75 with azithromycin and
34.50- 244.75 with azithromycin and  72.20- 277.30 with levofloxacin. The percentage of MPCE on food spent for a prescription was 17.64 per cent for urban and 23.4 per cent for rural population. The percentage of MPCE on food spent for treatment of CAP ranged from 10.11 to 13.42 per cent with azithromycin and 13.28 to 17.61 per cent with levofloxacin. The number of days a worker on minimum daily wages would have to work to enable him to purchase his prescription medicines ranged from 1-17 days, depending on the problem. The cost of treatment of CAP required 1-3 days of work by a daily wage earner, depending on the brand of medicine prescribed.
72.20- 277.30 with levofloxacin. The percentage of MPCE on food spent for a prescription was 17.64 per cent for urban and 23.4 per cent for rural population. The percentage of MPCE on food spent for treatment of CAP ranged from 10.11 to 13.42 per cent with azithromycin and 13.28 to 17.61 per cent with levofloxacin. The number of days a worker on minimum daily wages would have to work to enable him to purchase his prescription medicines ranged from 1-17 days, depending on the problem. The cost of treatment of CAP required 1-3 days of work by a daily wage earner, depending on the brand of medicine prescribed.
Interpretation & conclusions:
The findings of our study show that the costs of medicines are highly variable and not affordable for the economically poor in India. Modifications in National Pharmaceutical Policy need to be done urgently.
Keywords: Affordability, costs, drug policy, medicines, private
Sixty per cent (499-649 million) of the population in India does not have regular access to essential medicines. This despite the fact that India produces 8 per cent of the medicines available in the global market in terms of volume and ranks 13th in world production by value1. The private health sector provides majority (80%) of the outpatient health care in India2. Out of pocket expenditure is the main source of health funding and has remained above 90 per cent for more than a decade2. About 60-90 per cent of healthcare spending by poor people is on medicines2,3.
Unlike most other countries, where medicines come under the preview of the Health Ministry, the responsibility for the pharmaceutical sector in India is shared by two ministries, the Department of Chemicals and Petrochemicals under the Ministry of Chemicals and Fertilizers and the Office of Drugs Controller under the Ministry of Health and Family Welfare. The Government's National Pharmaceutical Policy emanates from the Ministry of Chemicals and Fertilizers and is primarily an industrial policy4,5. The main thrust of the Government's pharmaceutical policies has been on the manufacturing and marketing of drugs in the private sector and not much on improving accessibility of essential medicines for the common man. The Government has also decreased the number of medicines under price control from 347 in 1978 to 74 in 19953,4. To compound the problem, there are more than 20,000 medicine formulations in the Indian market3. Many are formulations of unproven efficacy6. It is not humanly possible for even a well informed, health care provider, to be informed about all these formulations. Due to this lack of information, it is the poor patient who has to bear the medical and economic consequences of these formulations.
The Indian health sector has been affected by economic liberalization, structural adjustment reforms by the World Bank and increasing cost of production of pharmaceuticals7. Increasing cost of medicines may be a reason for people not accessing health care. It was assumed that analysis of the costs of prescribed medicines in the private health sector would help us understand how these may affect access to medicines for patients. Hence, the present study was designed with the aims to assess the costs of prescribed medicines and treatment of community acquired preumonia (CAP), and affordability of medicines in the private health sector in Delhi, India.
Material & Methods
This prospective, observational study was conducted in Delhi from July 2006 to December 2007. The study protocol was approved by the Institutional Scientific and Ethical Committee of Maulana Azad Medical College, New Delhi. The methodology adopted was from the World Health Organization's (WHO) manual on indicators for monitoring national drug policies8. This manual contains detailed methodology on how national drug policies can be monitored, both in the public and private health sector. The methodology has been prepared after intense reviews by Harvard School of Public Health and Delphi survey involving 54 experts from International organizations including World bank, European Union, United Nations system, WHO, UNICEF, etc. The indicators were field tested in six countries. The methodology was finalized after reviews both inside and outside the WHO. For assessing affordability indicators from the same and from WHO-Health Action International price survey methodology were adapted to meet our requirements9.
Selection of outlets: The methodology for sampling and selection of pharmacy outlets was as specified in the WHO manual on indicators for monitoring national drug policies8. The geographical area where the study is to be conducted is divided into units (these may be administrative units) for sampling. A minimum of four geographical units may be selected within the sample frame. Within those geographical units a sample of at least 20 pharmacy units is required. More can be taken. Such a sample is considered acceptable for providing the data needed to calculate indicators with a reasonable level of accuracy in most developing countries.
The sample frame was the city of Delhi with a total area of 1483 km2. It is divided into nine administrative districts10. These were combined to give five zones North (North + North West district), South, East (North East + East districts), West (West + South West districts) and Central (Central + New Delhi districts). The list of retail pharmacies in Delhi was obtained from the Retailers and Distributors Chemist Association of NCT Delhi11. In each zone a list of private pharmacies was compiled and a minimum of five outlets in each zone were selected. The private pharmacies were selected based on the following criteria: (i) the proximity of the private pharmacy to a public health facility, and (ii) the willingness of the pharmacy owner to allow to do the survey. A total of 27 pharmacies were selected, five each from North, South and East zones and six each from West and Central zones. All the pharmacies approached allowed the survey.
Data collection: A minimum of 30 prescriptions each were collected from all the pharmacies. Thirty prescriptions from each health facility were considered sufficient for monitoring prescribing indicators as per the methodology in the WHO manual. The same number was used for assessing costs of a sample of prescriptions. For obtaining the costs of medicines in the prescriptions, the data collector stood inside the pharmacy alongside the pharmacist. The pharmacist handed over the prescription to the data collector for writing and also informed about the costs of the individual medicines prescribed. The data collector wrote details about medicines prescribed and the costs on a structured pre tested proforma. The first 30 prescriptions that were received at the pharmacy on the day of the data collection were recorded.
The cost of medicines in the private sector was evaluated by (i) the total cost of the prescription. This was based on the actual prices at which the medicines were sold in the pharmacy; and (ii) cost of treatment of community acquired pneumonia. For obtaining the cost of a standard treatment of community acquired pneumonia (CAP), the standard treatment schedule as specified in Standard Treatment Guidelines for ambulatory patients was used12. The cost of treatment of pneumonia using tablet azithromycin or levofloxacin with paracetamol was obtained from each pharmacy (27 total) separately. The data collector showed a prescription for treatment of pneumonia using azithromycin or levofloxacin. The costs of the medicines given by the pharmacists were recorded. Then the total cost of treatment of pneumonia was calculated, individually for all 27 pharmacies. The cost of treatment, with the cheapest, most expensive, average and the median cost of the antibiotic and the variation in the cost of treatment of pneumonia due to medicines purchased from the different pharmacies was analyzed.
Affordability: The affordability of medicines in the private sector was assessed by comparing (i) the cost of the general prescriptions and the cost of treatment of pneumonia, as a percentage of monthly per capita consumer expenditure on food (MPCE) and total expenditure for Delhi and all India specifically. The MPCE was taken as specified by the Government of NCT Delhi and the Government of India for the years 2005-2006 and 2006-0713–15. MPCE for both rural and urban population as specified by the national and State Government was used. (ii) The cost of the prescriptions and treatment of pneumonia was compared to the minimum monthly wages earned by different categories of workers; Daily wages earned by unskilled workers, as specified by the Labour ministry, Government of National Capital Territory, Delhi for the year 2006-200716. The Government specifies the minimum wages twice a year and these were used for both the years 2006 and 20079,16.
Both the mean and median costs of prescriptions and treatment of pneumonia using azithromycin and levofloxacin were used for analyzing the percentage expenditure. The percentage difference between the maximum and minimum cost of treatment of pneumonia using azithromycin and levofloxacin was calculated as
![]()
(iii) The number of days a daily wage earner would have to work to procure the cost of treatment of pneumonia was assessed, taking the lowest, maximum, average and median costs of levofloxacin, azithromycin and paracetamol obtained in the survey.
Statistical analysis: The data were analyzed using STATA, version 9.0 (College Station, Texas, USA). Values are expressed as percentage, mean ± standard deviation (SD) and median (range). The inter-zone comparison of costs was done using Kruskal Wallis test.
Results
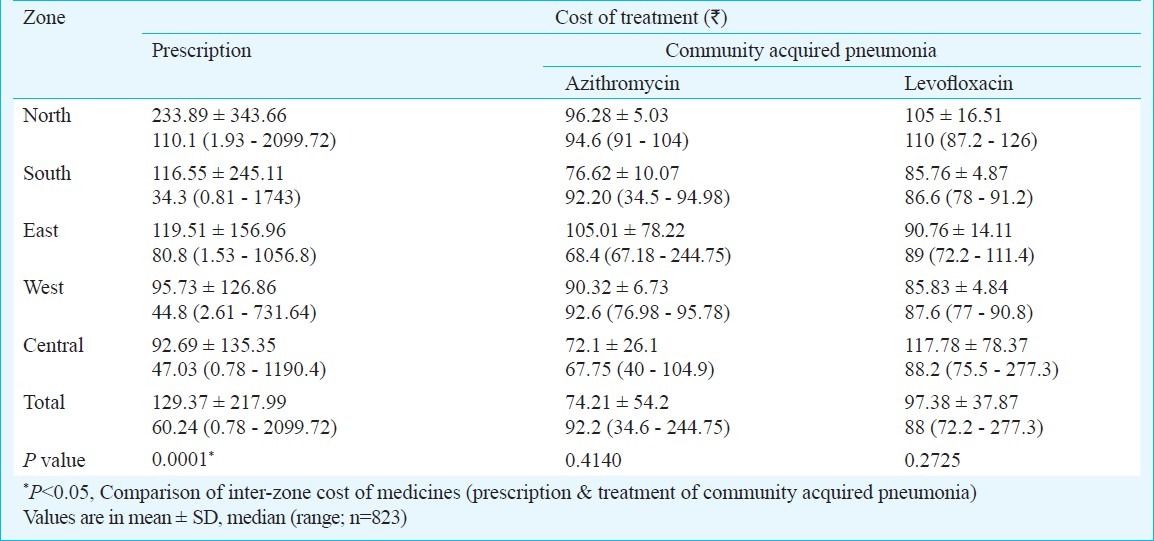
A total of 823 prescriptions were analyzed for costs. The average cost of prescriptions was  129.37 ± 217.99. Both within and inter zone a wide range in the cost of individual prescriptions was observed (Table I). The average cost ranged from
129.37 ± 217.99. Both within and inter zone a wide range in the cost of individual prescriptions was observed (Table I). The average cost ranged from  92.70 ± 135.35 in the Central zone to
92.70 ± 135.35 in the Central zone to  233.90 ± 343.66 in the North zone (P=0.0001). The cost of treatment of CAP using tablet azithromycin or levofloxacin varied from
233.90 ± 343.66 in the North zone (P=0.0001). The cost of treatment of CAP using tablet azithromycin or levofloxacin varied from  34.60 to 244.75 with azithromycin and
34.60 to 244.75 with azithromycin and  72.20 to 277.30 with levofloxacin (Table I).
72.20 to 277.30 with levofloxacin (Table I).
Table I.
Cost of prescription and treatment of community acquired pneumonia in different zones
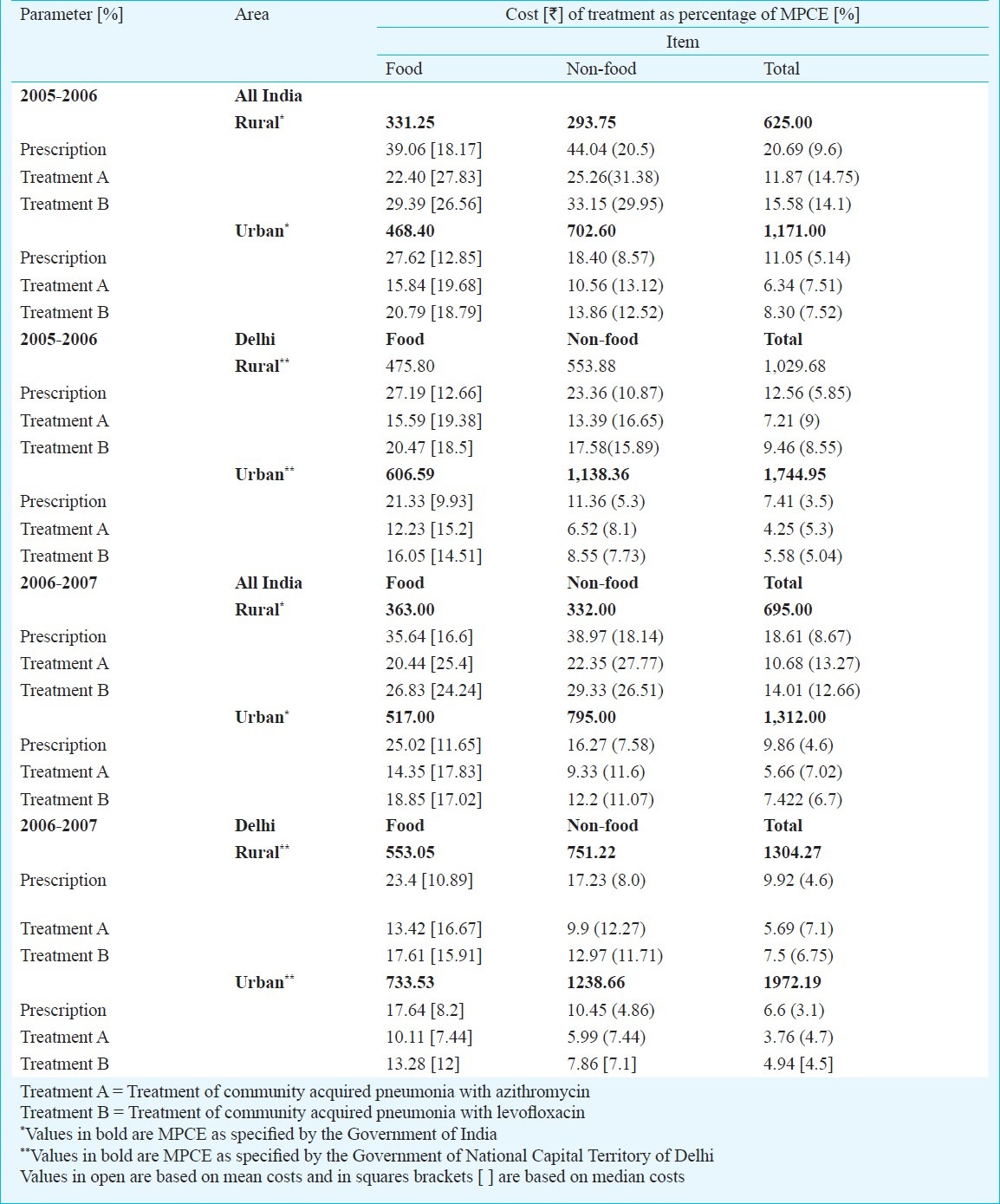
Prescriptions: The percentage of the MPCE on food spent on the average cost of prescription ranged between 17.64-23.4 per cent (2006-2007, Delhi) and 25.02-35.64 per cent (2006-2007, All India). The percentage of MPCE of the median costs of the prescriptions, spent on the prescription ranged from 8.2-10.89 per cent (Delhi) and 11.65-16.59 per cent (All India) (Table II).
Table II.
Cost of prescriptions & treatment of community acquired pneumonia as a percentage of monthly per capita expenditure [MPCE] on food, non-food & total expenditure: All India, Delhi 2005-2006, 2006-2007
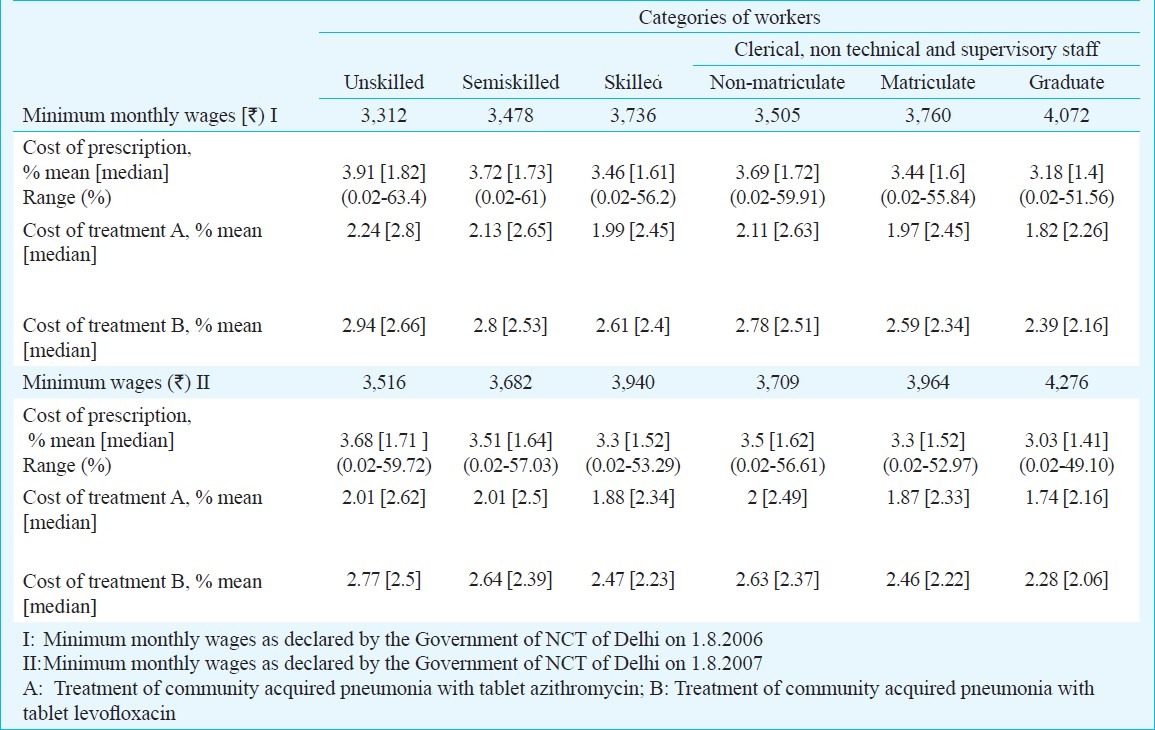
The percentage of minimum monthly wages spent on purchase of the average cost of prescription medicines ranged from 3.03 to 3.91 per cent depending on the skill of the worker and the year and 1.41-1.82 per cent of the median cost of prescription medicines (Table III). The number of days a daily wage earner would have to work, to enable himself to procure the prescription medicine ranged from 1-17.
Table III.
Cost of prescription and treatment of community acquired pneumonia [mean and [median] costs) as a percentage of minimum monthly wages of different categories of workers
The percentage of the MPCE (2006-2007) on food, spent on average cost of treatment of pneumonia using azithromycin was between 10.11-13.42 (2006-2007, Delhi) and 14.35-20.44 per cent (2006-2007, All India). It was 13.28-17.61 per cent (2006-2007, Delhi) and 18.85-26.83 per cent (2006-2007, All India) with levofloxacin (Table II). The percentage of the MPCE on food, non food and total expenditure spent on prescription medicines and for treatment of pneumonia was maximum amongst the rural population, both for Delhi and All India comparison.
The cost of treatment of pneumonia as a percentage of the minimum monthly wages, was 1.74 to 2.24 per cent with azithromycin and 2.28 to 2.94 per cent with levofloxacin depending on the year (Table III).
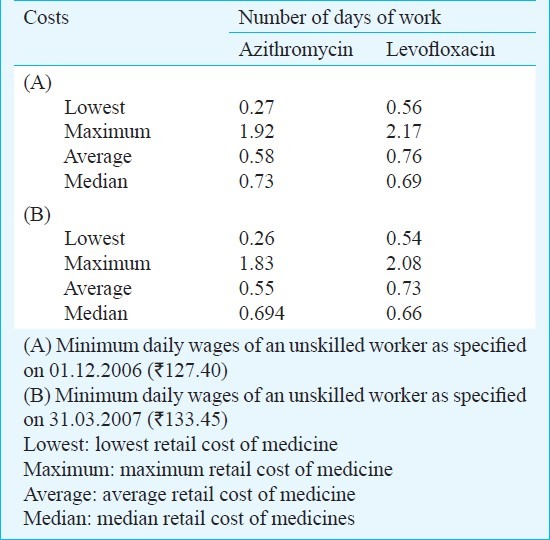
The percentage of MPCE or daily wages that would be spent for procuring the prescription medicines and treatment of pneumonia with levofloxacin was lesser when calculated as a percentage of median costs than mean costs. However, it was more as percentage of median costs for azithromycin. When the cost of treatment of pneumonia was compared with the daily wages of the lowest paid, unskilled worker in the city, it was observed that a worker would have to work for one to three days to afford the treatment of pneumonia with azithromycin or levofloxacin depending on the nature and brand of the antibiotic prescribed. The brand determines the cost of the medicines purchased i.e. lowest, maximum or average cost. This was observed over both the years 2006 and 2007 (Table IV). The percentage difference between the maximum and minimum costs of treatment of pneumonia with different brands of azithromycin was 607.31 per cent and with levofloxacin was 284.07 per cent.
Table IV.
Number of days of work required to afford the cost of treatment of community acquired pneumonia by an unskilled worker on daily wages
Discussion
Medicines form a substantial portion of out of pocket spending on health by households in India. The private health sector provides 81 per cent of outpatient and 45 per cent of inpatient care in India, as public health facilities providing free or subsidized care, are inadequate in number and infra structure17. Affordability of medicines thus, is a major issue determining access to medicines, as social insurance especially for people in the unorganized sector is lacking. Delhi has a large population of over 18 million of which 32.82 per cent (4.55 million) are workers (cultivators, agricultural labourers, household industrial workers, other workers)18. A large proportion of Delhi's population comprises of migratory population from other States and rural population (6.82%, 9.44 lakhs). The number of people employed is 5.43 million, of whom only 0.83 million are in the organized sector. Thus only a few people have social insurance based on organized employment sources.
Large variation in costs of medicines was observed. In India the pricing policy for medicines in existence in the country, is a major reason for the price variation3,4,6. The prices of all medicines not under price control have been left to the market forces6. The maximum allowable post manufacturing expense (MAPE) permitted for medicines under price control is 100 per cent and ceiling prices have been fixed for these6. For the other medicines, there is no restriction on the MAPE, resulting in large and variable prices. The variation in prices of the same medicine but sold under different brands is large and may range from 25-3400 per cent19. In a study, when the price differentials between the highest and lowest selling prices and the maximum retail price (MRP) were calculated, a price differential of 32.7 per cent among retail stores selling the same brand of the medicine was observed and the differential was as high as 120 per cent for amoxycillin20. Retail margins of medicines in India are estimated as about 25 per cent20. Differences in wholesale prices, retail mark ups, both formal and informal and taxes can all result in variability in drug prices for the consumer3,20,21.
For assessing affordability of medicines an indicator (OT3) from the WHO manual was adopted which compares the average retail price of standard treatment of pneumonia to the average retail price of a basket of food8. We have instead compared the cost of treatment of pneumonia to MPCE on food and other costs. The MPCE is calculated based on standardized sample surveys by the Government within the whole country and in each State. The costs were compared as a percentage of MPCE at the Delhi State and All India level. The costs of prescriptions and pneumonia accounted for a significant proportion of the MPCE on food and total costs. It has been seen that rural India spends 77 per cent of their expenditure on health on medicines while urban India spends around 70 per cent of the same on medicines3. The share of medicines in out of pocket expenditure on health in Delhi for rural population is 61.83 per cent and for urban is 72.7 per cent3. Even as a percentage of the minimum wages earned a significant percentage of the wages would be spent on the cost of medicines.
One of the best ways of studying the impact of medicine prices on the cost of health care for patients is to compare the cost of treatment with people's actual incomes9. The daily wage of the lowest paid unskilled government worker was compared to the cost of treatment of CAP and general prescription. Although this parameter is often used for chronic conditions, we adapted it for an acute condition. The number of days a daily wage earner would have to work to procure the cost of treatment of pneumonia, depended on the brand of the medicine prescribed or dispensed by the pharmacist. Thus, the importance of generic prescribing becomes relevant for the poor patient3.
The percentage of MPCE on food spent for purchasing medicines was more for the national (All India) averages than for Delhi State. Delhi has a higher per capita income18. This does not reflect the average national incomes in India. Thus, comparison of medicine prices with All India averages of MPCE gives a better estimate of affordability for all. However, the calculated values with All India MPCEs in this study may be considered an approximation, since the costs of medicines were only obtained in Delhi. The ideal way would have been to compare with costs of medicines obtained through an All India sample survey of pharmacies.
The cost of medicine may be lesser than in other countries but relative to the purchasing power of the average citizen the costs are high22. It has also been observed that populations with lower MPCE reported with illness and sought treatment to a lesser extent. The poor also had a lower probability of obtaining medicines when they were ill than the richer groups23.
A widening gap between the Pharmaceutical Price index and All Commodity Price Index has been observed25. The existing monopolistic market structure of the pharmaceutical industry, market segmentation, existence of large scale differentiation through brand names without having significant variation in the chemical contents, aggressive advertising, sales promotion and asymmetry of information about medicine prices, which decreases both prescriber and consumer choices have reduced the relevance of price competition in the market resulting in heterogeneity in prices of the same product24.
A wide variation in medicine prices may result in prescribing of those brands which are more costly. The burden of such prescribing has to be borne by the patient. It was observed that depending on the brand of antibiotic prescribed, a daily wage earner might have to work for one to three days to purchase the medicine for treatment of an acute condition (pneumonia). For a 41.6 per cent of the 1 billion population living below the International poverty line of US $ 1.25 per day (purchasing power parity in nominal terms  21.6 in urban and
21.6 in urban and  14.3 in rural) this may be a large amount and difficult to acquire28. Further, many people in low and middle income countries earn less than the wages of the lowest paid government worker26.
14.3 in rural) this may be a large amount and difficult to acquire28. Further, many people in low and middle income countries earn less than the wages of the lowest paid government worker26.
The Consumer Price Index ( CPI, general) in India has been steadily increasing since 2006 (from 127 in 2006 to 185 in 2010). The consumer price index number for medical care has also been increasing from 126 (December, 2006) to 156 ( December, 2010). The inflation rate based on CPI has also fluctuated from 5 to 16 over the last five years. The Wholesale price index has increased from 199 in March 2006 to 257.5 in March 201127. All these indicate that cost of living including medical care has increased.
Ways to make medicines more affordable in India include: (i) Availability of unbiased information on the quality and comparative prices of all medicines available in the country. It has been seen that physicians could provide better services and reduce medicine costs if information about medicine prices was readily available28. At present the National Pharmaceutical Pricing Authority in India fixes prices for medicines under price control only and these are available. The number of medicines under price control in India are very few and many are not used commonly. (ii) Changes in medical pharmacology and pharmacy curriculum to include sensitization of medical graduates and pharmacists on basic aspects of pricing of medicines and their cost effectiveness are needed. At present this is not being done. (iii) Increasing consumer awareness about medicines, their prices and reasons for the same. (iv) Promotion of use of generics through educating health professionals and implementing of medicine policies that make generic substitution compulsory26. A lack of trust in the quality control of generic companies exists among physicians. (v) If market forces continue to fail to bring down medicine prices, regulating medicine prices needs to considered3,26. A larger number of drugs included in the National Essential Drug list (EDL) may be put under price control with adequate incentives for the manufacturers. At present only 44 drugs from the national EDL are under price control and many of these are of little clinical utility3.
The National Health Policy 2002 has realized that the supply of medicines by the States has been inadequate, resulting in poor utilization of public health facilities by the patients5. The Policy as well as the XIth Five Year Plan have both envisaged providing essential medicines under Central Government funding to improve access to essential medicines5,29.
Perhaps the National Pharmaceutical Policy of the country needs to incorporate the priority components established by WHO for national drug policies30. At present the pharmaceutical policy does not have the relevant structures in place to ensure that the poor have access to medicines. Dichotomy between the pharmaceutical policy and the health needs of the country is a major cause of the variable and high medicine prices.
In conclusion, high cost of medicines in India makes treatment less affordable for the poor segments of the population. Modifications in Pharmaceutical Policy changes at the national and State level are urgently required to improve affordability and hence access to medicines for the people.
References
- 1.The world medicines situation. Geneva: 2004. World Health Organization. WHO/EDM/PAR/2004.5. [Google Scholar]
- 2.World Health Statistics. Geneva: 2009. [accessed on December 6]. World Health Organization. Available from: http://www.who.int/entity/whosis/whostat/EN_WHS09_Full.pdf . [Google Scholar]
- 3.Sakthivel S. Byword editorial consultants. Access to essential drugs and medicines. In: Lal PG, editor. National Commission on Macroeconomics and Health. New Delhi: Ministry of Health &; 2005. pp. 185–210. [Google Scholar]
- 4.Government of India. Draft National Pharmaceutical Policy 2006, Part A. Delhi. [accessed on December 6, 2009]. Available from: http://chemicals.nic.in/npp_circulation_latest.pdf .
- 5.Government of India. National Health Policy (India) 2002. Delhi. [accessed on December 6, 2009]. Available from: http://www.mohfw.nic.in/NRHM/Documents/National_Health policy_2002.pdf .
- 6.Government of India. Drug Policy 1986. Delhi. [accessed on December 6, 2009]. Available from: http://nppaindia.nic.in/Dp1986mod.htm .
- 7.Sakthivel S. How effective is India's Drug Price control regime? [accessed on February 14, 2010]. Available from: http://www.hsph.harvard.edu/research/takemi/files/RP256.pdf .
- 8.Jakobowicz PB, Rainhorn JD, Reich MR, editors. Indicators for monitoring national drug policies: a practical manual. Geneva: World Health Organization; 1994. WHO/DAP/9412. [Google Scholar]
- 9.World Health Organization and Health Action International. Background report prepared for the WHO Planning Meeting on the Global initiative for treatment of chronic diseases. Cairo (Egypt): WHO Regional office for the Eastern Mediterranean and Health Action International; 2005. [accessed on December 6, 2009]. Price availability and affordability. An international comparison of chronic disease medicines. Available from: http://www.haiweb.org/medicine prices . [Google Scholar]
- 10.Delhi statistical handbook. New Delhi: Government of India Press; 2006. Government of National Capital Territory Delhi. Directorate of Economics & Statistics. [Google Scholar]
- 11.List of Pharmaceuticals, Retailers and whole sellers in Delhi, India [document on the internet] [accessed on March 6, 2006]. Available from: http://www.indiacom.com/yellowpages/pharmaceuticals-retailersandwholesellers/Delhi Pharmaceuticals-retailersandwholesellers in Delhi, India .
- 12.Sharma S, Sethi GR, Sachdev GK, Gupta U, Gulati RK, editors. Standard treatment guidelines. A manual for medical therapeutics. 2nd ed. New Delhi: BPL Publications Pvt; 2005. [Google Scholar]
- 13.National Sample Survey Organization (NSSO) Household consumer expenditure in India NSS, 63rd Round, July 2006-June 2007. Report No. 527 (63/1.0/1) New Delhi: NSSO Government of India; 2008. Ministry of Statistics and Programme Implementation (Government of India) [Google Scholar]
- 14.National Sample Survey 62nd Round (State sample), July 2005-June 2006. New Delhi: Government of NCT Delhi; 2007. Directorate of Economics & Statistics. Government of National Capital Territory of Delhi) [Google Scholar]
- 15.National Sample Survey 63rd Round (State sample). July 2006-June 2007. New Delhi: Government of NCT Delhi; 2008. Directorate of Economics ' Statistics (Government of National Capital Territory of Delhi) [Google Scholar]
- 16.Government of National Capital Territory of Delhi. Labour Department. Minimum monthly wage rates. [accessed on December 6, 2009]. Available from: http://www.delhi.gov.in/wcm/connect/doit_labour/labourHome/Minimum+Wages/Rates+at++a+glance .
- 17.Rao KS, Nundy M, Dua AS. National Commission on Macroeconomics and Health. Financing and delivery of health care services in India. New Delhi: Ministry of Health & Family Welfare, Government of India; 2005. Delivery of health services in the private sector; pp. 89–104. [Google Scholar]
- 18.Government of National capital Territory of Delhi. Economic Survey of Delhi 2008-09. [accessed on February 10, 2010]. Available from: http://www.delhiplanning.nic.in/Economics%Survey/ES2008-09.htm .
- 19.Roy V, Rewari Ambiguous drug pricing. A physician's dilemma. Indian J Pharmacol. 1998;30:404–7. [Google Scholar]
- 20.Godwin SK, Varatharajan D. Drug price differentials across different retail market settings. Health Administrator. 2006;19:41–7. [Google Scholar]
- 21.More equitable pricing for essential drugs: What do we mean and what are the issues? Hosbjor (Norway): Background paper for differential pricing and financing of essential drugs; 2001. [accessed on December 20, 2009]. World Health Organization/ World Trade Organization. Available from: http://www.wto.org/english/tratop_e/trips_e/who_background_e.pdf . [Google Scholar]
- 22.Gonzales AG. The drugs don’t work: access to medicines in the developing world. ICFAI J Health care Law. 2007;5:41–74. [Google Scholar]
- 23.Makinen M, Waters H, Rauch M, Almagambetova N, Bitran R, Gilson L, et al. Inequalities in health care use and expenditures: empirical data from eight developing countries and countries in transition. Bull World Health Organ. 2000;78:55–65. [PMC free article] [PubMed] [Google Scholar]
- 24.Monaghan MJ, Monaghan MS. Do market components account for higher US prescription prices. Ann Pharmacother. 1996;30:1489–94. doi: 10.1177/106002809603001219. [DOI] [PubMed] [Google Scholar]
- 25.World Bank. New Gobal poverty estimates - what it means for India. [accessed on July 30, 2011]. Available from: http:://www.worldbank.org.in/WBSITE/EXTERNAL/COUNTRIES/SOUTHASIAEXT/INDIAEXTN10,,content PK141137~pagepiPK:141127~thesitePK12 .
- 26.Mendis S, Fukino K, Cameron A, Laing R, Filipe A, Jr, Khatib O, et al. The availability and affordability of selected essential medicines for chronic diseases in six low and middle income countries. Bull World Health Organ. 2007;85:279–88. doi: 10.2471/BLT.06.033647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reserve Bank of India. Handbook of Statistics on Indian Economy. [accessed on July 25, 2011]. Available from: http://www.rbi.org.in/scripts/AnnualPublications.aspx?head=Handbook%20of%20Statistics%20on%20Indian%20Economy .
- 28.Frazier LM, Brown JT, Divine GW, Fleming GR, Philips NM, Siegal WC, et al. Can physicians education lower the cost of prescription drugs? A prospective controlled trial. Ann Intern Med. 1991;115:116–21. doi: 10.7326/0003-4819-115-2-116. [DOI] [PubMed] [Google Scholar]
- 29.Eleventh Five Year Plan 2007-2012. II. Delhi: Oxford University Press; 2007. Social sector. Planning Commission, Government of India; pp. 57–127. [Google Scholar]
- 30.How to develop and implement a national drug policy WHO Policy perspectives on medicine, No.6. Geneva: WHO; 2002. World Health Organization. [Google Scholar]


