Abstract
Background & objectives:
User charges have been advocated on efficiency grounds despite the widespread criticism about their adverse effect on equity. We assessed the effect of user charges on inpatient hospitalizations rate and equity in Haryana State.
Methods:
The inpatient department (IPD) statistics of the public sector facilities in Yamuna Nagar district where user charges had been introduced were analysed and compared with Rohtak district which did not have user charge between 2000 and 2006. National Sample Survey data of Haryana for the 2004-2005 period were analyzed to compare utilization of public sector facilities for hospitalization, cost of hospitalization, and prevalence of catastrophic out-of-pocket (OOP) expenditure by income quintiles in three districts which had user charges and 17 districts of Haryana which did not levy user charges.
Results:
During 2000 and 2006, hospital admissions declined by 23.8 per cent in Yamuna Nagar district where user charges had been introduced compared to an almost static hospitalization rate in Rohtak district which did not have user charges (P<0.01). Public sector hospital utilization for inpatient services had a pro-rich (concentration index 0.144) distribution in the three districts with user charges and pro-poor (concentration index -0.047) in the 17 districts without user charges. Significantly higher prevalence of catastrophic health expenditure was observed in public sector institutions with user charges (48%) compared to those without user charges (35.4%) (P<0.001).
Interpretation & conclusions:
The findings of our study showed that user charges had a negative influence on hospitalizations in Haryana especially among the poor. Public policies for revenue generation should avoid user charges.
Keywords: Access the health care, demand-side cost sharing, equity, health system research, India, service utilization, user charges
User charges, i.e., where consumer pays part of the total cost of service have been widely experimented by policy makers in both developed and developing countries1. Most Organization for Economic Cooperation and Development (OECD) countries have introduced user charges to counter the demand side moral hazard of risk pooling mechanisms and their association with rising health care expenditures2. On the contrary, their introduction in public sector institutions of developing countries was necessitated by a need to generate resources for providing health care services.
Proponents of user charges have justified their use on grounds of efficiency. It has been argued that introduction of ‘price’ at time of service utilization would discourage unnecessary care and service utilization will be at an efficient level3. The RAND health insurance experiment, a unique natural experiment conducted in the USA to elicit the impact of risk pooling arrangements on service utilization, observed that with the introduction of user charges demand for health service decreases leading in turn to reduction in health care expenditures4. However, the RAND experiment could not establish whether demand reduction was only for ‘unnecessary’ form of medical care, or whether the ‘necessary’ care utilization also decreased. This is the main critique against user charges negating its efficiency arguments. Recent evidence on user charges from developing country context also reinforces the conclusions from RAND study5–8. Moreover, it discourages preventive care service uptake and delays medical care utilization at early stage of disease onset. Both the factors can potentially lead to an overall inefficient impact of user charges.
Another major criticism of user charges has been on grounds of ‘equity’. Some studies on user charges have suggested regressivity of user charges in developing countries6,9. Another OECD multi-country study which used kakwani index as a measure of progressivity for different health financing mechanisms concluded user charges to be a highly regressive means of financing health care10.
Majority of research to document impact of user charges in developing countries has been done in Africa with only a few studies from Asia, particularly India13. The Government of India introduced user charges in public sector hospitals and health centres on a pilot basis as part of its health sector reforms in late 1990s and early 200011. The National Rural Health Mission has also endorsed this strategy to create local resources which would then be utilized locally to improve service availability and quality12.
In this study the impact of user charges was evaluated on the inpatient hospitalization rate in Haryana State. It was also assessed whether the impact of user charges on service utilization was equitable according to income, gender and geographic region, and the vertical equity in out-of-pocket spending at public sector health institutions was ascertained in districts with and without user charges.
Material & Methods
Background: The delegation of the European Commission (EC) in India had entered into a Financing Agreement with the Government of Haryana to support health sector reforms under the Sector Investment Programme (SIP)16. Haryana State implemented the SIP, starting with the constitution of State Sector Reform Cell and Advisory Committee in January 2000.
A State Health and Family Welfare Society at State level, District Health and Family Welfare Society (DHFWS) at district level and a health facility level society (Swasthya Kalyan Samiti, SKS) were constituted. These societies implemented the SIP under the health sector reform process. User charges were introduced at all levels, i.e., in public sector hospitals, community health centres, primary health centres and civil dispensaries in 2001 in three pilot districts namely, Yamuna Nagar, Karnal and Ambala. These charges were levied on out-patient consultation, hospital admission, laboratory tests and other services such as medico-legal services. Preventive services such as vaccination and medicines dispensed were not charged. As per policy, below poverty line patients were exempted from the user charges. The facility level societies (SKS) were delegated powers to use the revenue generated from the user charges locally to improve service availability and quality. Revenue generated from user charges was spent using the prescribed guidelines, which did not include paying any extra monetary incentives to existing staff for extra services. However, extra staff could be contracted to tide over existing shortage in human resources.
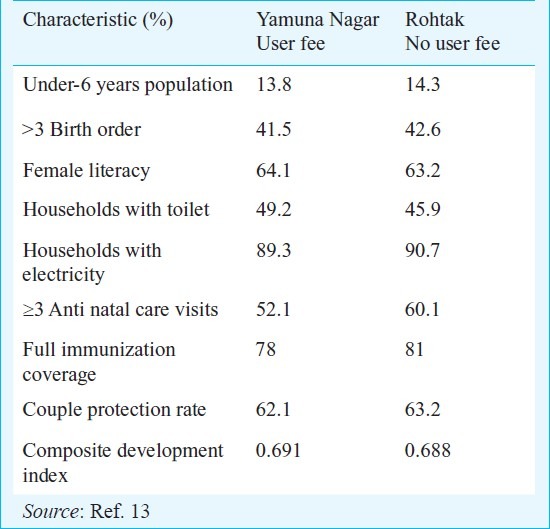
Study design: The district of Yamuna Nagar, one of the three pilot districts, was selected to study the impact of user charges on service utilization. The selection of control district from Haryana State was based on development rank of district. In terms of ranking within Haryana, Yamuna Nagar with a composite index score of 0.691 ranked fourth. Kurukshetra and Rohtak with scores of 0.742 and 0.689, respectively ranked third and fifth (Table I)13. The Rohtak district in Haryana had closest composite index score to Yamuna Nagar. Since it was not a pilot district for health sector reforms, it was chosen as a control district for the present study.
Table I.
Demographic, socio-economic and health service utilization indicators of Yamna Nagar and Rohtak district of Haryana
The present study was conducted during November 2007 to June 2008, when inpatient utilization records from 2000 to 2006 were collected. Pooled data on service utilization at district level were available from 2000 to 2006. From 2003 to 2006, the inpatient data were available disaggregated by health institution, i.e. hospital or health centre. Measles immunization service (MIS) statistics was also analyzed as preventive services were exempted from user charges, any temporal effect on utilization of this service would help in interpreting the time trend of other services. It has been shown that despite the fact that immunizations are delivered mainly in an outreach mode, through community level workers, its utilization shows negative elasticity with price14. Out-patient registers in district hospitals and one community and primary health centre each of Yamuna Nagar and Rohtak were reviewed for past 3 months, to ascertain the extent of patients who were exempted of user charges.
Impact of user charges on equity: Routine MIS data on service utilization did not capture information on health care expenditure or any background socio-economic characteristic of the patients. Data from National Sample Survey (NSS) 60th Round (2004-2005) on Morbidity and Health Care were analyzed to assess vertical equity in financing through out-of-pocket user charges15. This survey recorded detailed out-of-pocket health expenditures (user charges). Monthly household consumption expenditure was also elicited in the survey as an indicator of socio-economic status. Since data were collected for National Sample Survey 60th round during 2003-2004, it provided a unique opportunity to compare three districts where user charges were introduced against other 17 districts which did not have the user charge policy. Since the sample size per district in NSS was inadequate to study effect at district level, pooled data for three pilot districts where user charges were introduced were compared with the remaining 17 districts of Haryana State where user charges were not applied.
Study indicators and analysis: In-patient admission rates per 100,000 population and measles immunization rates were computed on a yearly basis in the selected districts. Rural population was used as denominator for calculating the service utilization rates for the rural health centres; while total district population was used as denominator to compute urban hospital utilization rates which has the entire district as its catchment area. Routine MIS data were used to study the utilization of these services. Census 2001 population and annual growth rate was used to calculate year-wise population of the district and its urban and rural areas according to the gender. Overall utilization of hospital in-patient services and measles vaccination was compared between districts with and without user fee from 2000 to 2006.
Service utilization was stratified according to gender and location of health facility (rural health centres, i.e., primary and community health centres; and urban hospitals) to compare the trend among different groups from 2003 to 2006 and to ascertain inequities in service utilization according to gender (horizontal inequity). Data were analyzed using the SPSS version16. Chi-square test for trend (at 5% significance level) was used to test statistical significance in service utilization rates. Relative per cent change in service utilization was also computed.
In NSSO data monthly per capita consumption expenditure (MPCE) was computed for each household after adjusting for size and composition of the household. Distribution of population according to MPCE was analyzed to calculate quintiles of population with 1st and 5th quintile representing poorest 20 per cent and richest 20 per cent population groups, respectively. Utilization of public sector facilities in each population subgroup according to income quintiles was calculated. Concentration index was computed as a measure of horizontal inequity in service utilization and concentration curve was used to graphically represent service utilization stratified by wealth quintiles17.
Mean out-of-pocket (OOP) expenditure in different MPCE quintiles was assessed for public sectors. Vertical equity was assessed by computing the total OOP health expenditure as per cent of monthly household per capita expenditure for each MPCE quintile in three districts with user charges and 17 districts without user charges in Haryana. Catastrophic health expenditure was computed as any out-of-pocket health expenditure for in-patient admission exceeding 10 per cent of annual consumption expenditure. The study protocol received ethics approval at the London School of Hygiene and Tropical Medicine, UK.
Results
In terms of development ranking within Haryana, Yamuna Nagar with a composite index score of 0.691 ranks fourth, while Rohtak at fifth rank scores 0.689. Both the districts have similar levels of demographic parameters, female literacy, safe drinking water, sanitation, household electrification and coverage of preventive health services (antenatal care, immunization and contraceptive prevalence rate) (Table I).
Overall hospitalization rate declined significantly (P<0.05) in Yamuna Nagar by 23.8 per cent from 1721 per 100,000 population to 1311 per 100,000 population (P<0.0001) (Table II; Fig. 1). The admission rates in Rohtak were almost static during the study period with an insignificant difference of 1.7 per cent, but this was not statistically significant. Admissions in urban hospitals declined in both the districts, however, the decline was significantly higher in Rohtak (9.6%) than in the Yamuna Nagar (4.9%; P<0.01; Table II). On the contrary, admissions at rural health centres declined significantly by 57.2 per cent in Yamuna Nagar compared to an increase of 40.2 per cent in Rohtak between 2003 and 2006 (P<0.001).
Table II.
Health facility wise utilization for indoor admissions in Yamuna Nagar and Rohtak district, Haryana, 2003-2006
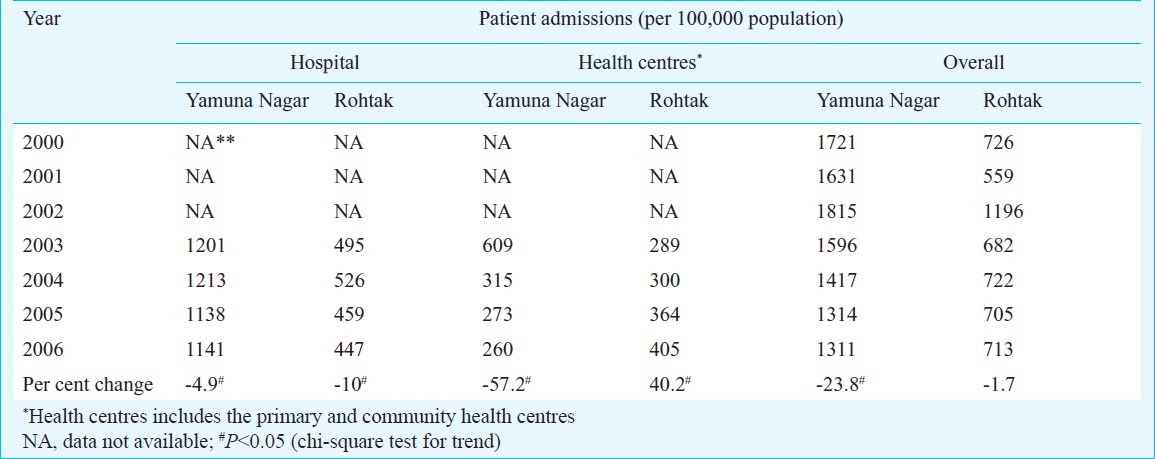
Fig. 1.
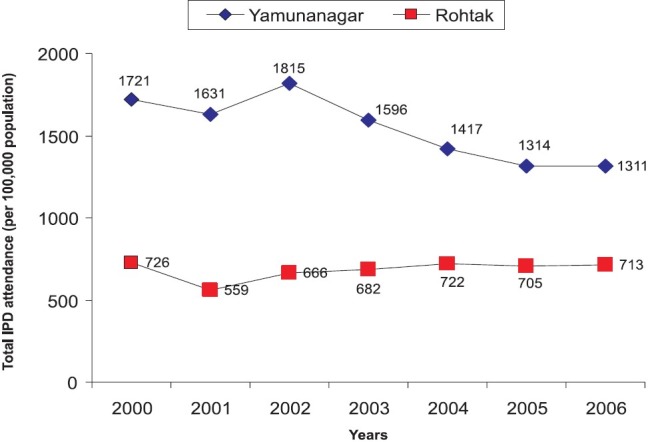
In-patient department (IPD) service utilization rates per 100,000 population in public sector institutions of Yamuna Nagar and Rohtak district, Haryana, 2000-2006.
Overall decline in in-patient admissions in Yamuna Nagar was significantly higher among females (21%) as against males (14%, P<0.01). Decline in rural health centre admissions was similar among females (57%) and males (56.2%). However, significantly higher decline in urban hospital admissions was observed for females (7.2%) than in males (1.2%, P=0.01). On the other hand, statistically insignificant decline in urban hospital admissions among males (10.8%) and females (8.7%) was observed in Rohtak district. Measles vaccinations increased from 22452 to 24280 (7.5%) and from 23605 to 25541 (7.6%) between 2001 and 2006 in Yamuna Nagar and Rohtak, respectively.
NSSO data used to analyze vertical equity included data collected from 1400 households, with 245 in the three pilot districts and 1155 in the remaining 17 districts of Haryana. Monthly median household consumption expenditure of respondents in NSS survey from the three districts with user charges  5,269) was similar to those from the remaining 17 districts in the State
5,269) was similar to those from the remaining 17 districts in the State  5,342). All background characteristics of NSS respondents were similarly distributed. Hospitalization rates in districts with and without user charges in Haryana was 27 and 29 per cent, respectively. Hospitalization in public sector institutions showed a pro-rich distribution in districts with user charges (concentration index 0.144, P=0.003) Table III; Fig. 2). Hospitalization in the remaining 17 districts of Haryana had a pro-poor distribution (concentration index -0.047), which was however, statistically insignificant.
5,342). All background characteristics of NSS respondents were similarly distributed. Hospitalization rates in districts with and without user charges in Haryana was 27 and 29 per cent, respectively. Hospitalization in public sector institutions showed a pro-rich distribution in districts with user charges (concentration index 0.144, P=0.003) Table III; Fig. 2). Hospitalization in the remaining 17 districts of Haryana had a pro-poor distribution (concentration index -0.047), which was however, statistically insignificant.
Table III.
Public sector hospitalization and out-of-pocket expenditure characteristics in districts with and without user charges in Haryana, India, 2004-2005
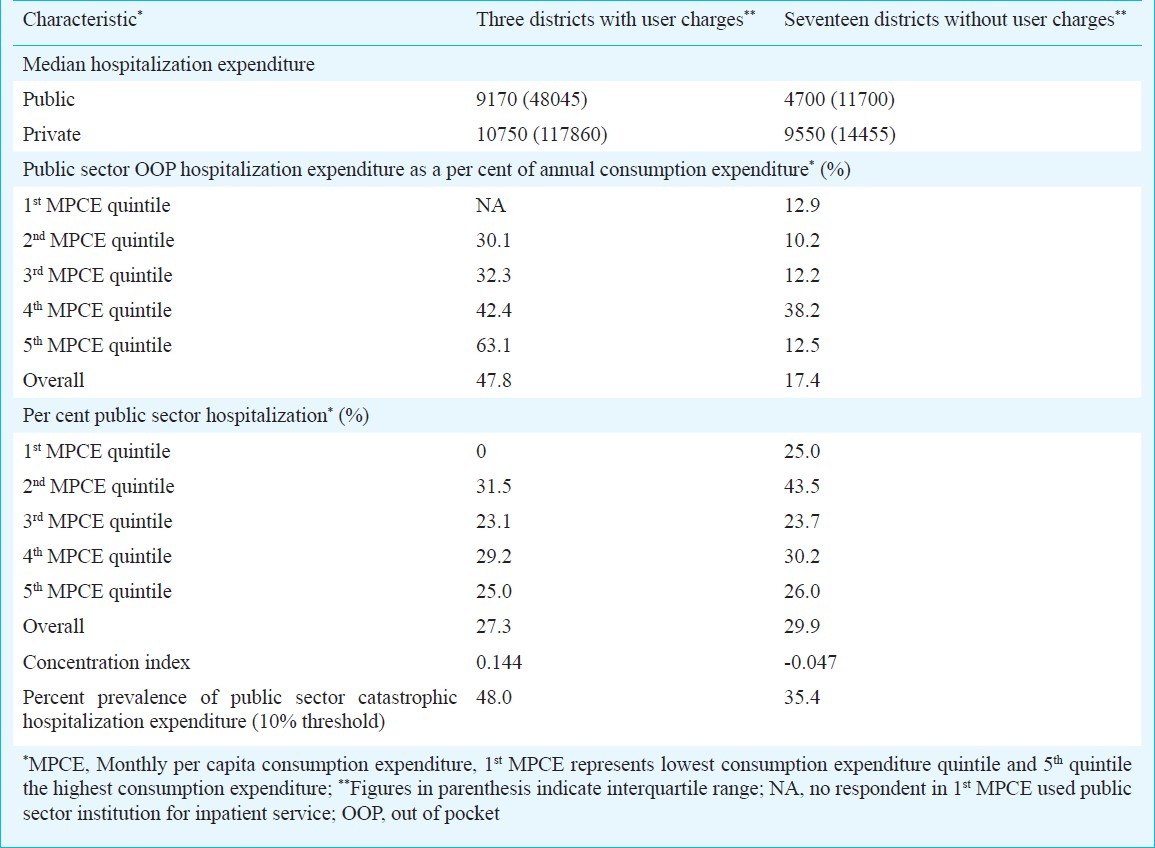
Fig. 2.
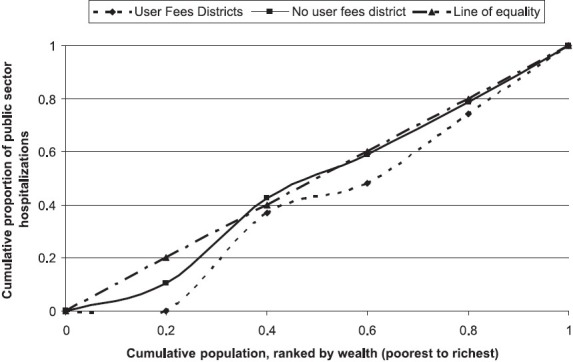
In-patient department (IPD) service utilization rates by wealth quintiles, for Yamuna Nagar and Rohtak districts, Haryana, 2000-2006.
Median inpatient OOP expenditure was almost similar in private hospitals of the three districts with user charges  10,750) and the 17 districts without user charges
10,750) and the 17 districts without user charges  9,550) (Table III). However, median OOP inpatient expenditure in public sector hospitals was almost two times in districts with user charges
9,550) (Table III). However, median OOP inpatient expenditure in public sector hospitals was almost two times in districts with user charges  9,170) as compared to the rest of the state
9,170) as compared to the rest of the state  4,700). Overall, as a per cent of consumption expenditure, households in districts with and without user charges spent 48 and 17 per cent of their consumption expenditure on meeting curative care. According to income quintiles, richer household spent more proportion of their consumption expenditure on health care, thus showing a progressive pattern. Significantly higher proportion of households incurred catastrophic hospitalization expenditure (at 10% threshold) while utilizing public sector facilities in districts with user charges (48.0%) than the remaining 17 districts of the State (35.4%, P<0.01).
4,700). Overall, as a per cent of consumption expenditure, households in districts with and without user charges spent 48 and 17 per cent of their consumption expenditure on meeting curative care. According to income quintiles, richer household spent more proportion of their consumption expenditure on health care, thus showing a progressive pattern. Significantly higher proportion of households incurred catastrophic hospitalization expenditure (at 10% threshold) while utilizing public sector facilities in districts with user charges (48.0%) than the remaining 17 districts of the State (35.4%, P<0.01).
User charge collection in three pilot districts had increased from  0.9 million in 2001 to
0.9 million in 2001 to  5.1 million in 2005. Similarly, the utilization of user charges also increased from 85 per cent in 2001 to 97 per cent in 2005. Majority (69.2%) of this money was spent on minor repairs of buildings and creation of new capital infrastructure. Not much was spent on provision of medicines supply (1.2%) at the health centres/ hospitals. Neither was money spent on paying contractual staff to make services available round the clock. About 5.3 per cent patients had been given exemption from user charges for out-patient care in the past three months.
5.1 million in 2005. Similarly, the utilization of user charges also increased from 85 per cent in 2001 to 97 per cent in 2005. Majority (69.2%) of this money was spent on minor repairs of buildings and creation of new capital infrastructure. Not much was spent on provision of medicines supply (1.2%) at the health centres/ hospitals. Neither was money spent on paying contractual staff to make services available round the clock. About 5.3 per cent patients had been given exemption from user charges for out-patient care in the past three months.
Discussion
Routine MIS service data and NSS (2004-2005) data were used to study the effect of user charges on service utilization with special focus on equity. Two dimensions of health inequities have been explored i.e., horizontal and vertical. Horizontal equity emphasizes treating equals equally, and focuses on equal access for those in equal need. It ensures that provision of health service should be based on the principle of ‘need’ and not on the ‘ability to pay’. Vertical equity highlights the need to treat unequals differently, i.e., rich should pay a higher proportion of their income for accessing health care services compared to the poor. It was found that user charges were associated with a decline in inpatient admissions, which was inequitable from gender and income perspective. Moreover, significantly higher catastrophic OOP hospitalization expenditure in public sector institutions of districts with user charges was noted. No change in utilization was observed for preventive services (measles vaccination), which were free of the user charge.
Present study showed user charges to be associated with reduced admission rates especially among rural population and among women for urban hospital care. It could possibly reflect lower paying abilities of the rural poor, and a gender bias for seeking rather costly form of inpatient care for the females. An alternative explanation to the declining rural hospitalization rates in public sector could be reduction in over-reporting of service utilization performance statistics, after introduction of user charges as user charge collected over a period of time was a proxy for performance.
There are limitations in attributing causal inference to effects associated with user charges. Service utilization or demand for health care is influenced by numerous factors besides the user charges including cost and availability of substitute and complementary services, quality of service, and treatment seeking behaviour18. It is also determined by the health status of population which in turn is determined by demography, socio-economic profile, and other social determinants like safe drinking water and sanitation. Similarly, it would be desirable to study trends in health expenditures using successive rounds of NSS survey. In an ideal scenario a randomized controlled trial (RCT) should have been conducted to derive answers for such operational programmatic questions as addressed in the present study19.
Significantly high out-of-pocket expenditure was found for inpatient hospitalizations in public sector institutions among districts with user charges. This in turn has led to high prevalence of catastrophic health care expenditures. Inpatient OOP spending in districts with user charges showed a progressive pattern. This could possibly be explained by strict implementation of exemptions for the poor. However, only 5 per cent of OPD patients were found to be exempted from user charges, whereas nearly 30 per cent of population is below poverty line. National and State-specific results for other States also show a progressive pattern for OOP spending. Alternatively, the “apparent progressivity” of OOP inpatient spending from our study and overall NSS data could be explained as a result of inability of the poor to access health services15. Thus the poor do not spend altogether for inpatient treatment which is also reflected in non utilization of inpatient care by any household from poorest quintile. This finding is also supported by high unmet need on account of lack of financial resources according to NSS data15. Access to care is positively associated with financial status, especially in developing countries with little scope of risk pooling20,21. In health systems such as in India which are primarily driven by out-of-pocket money, opportunity to access health care is severely constrained by ability to pay22. This is despite abundant evidence of association of higher morbidity and mortality with poor socio-economic status23,24. Our study results indicated that user charges had negative impact in Haryana, however, it would be difficult to generalize this to entire country. Other studies show a mixed impact of user charges on service utilization25–29. Regions where user charges were implemented with relatively greater devolution of powers to use the revenue generated locally to improve service availability and quality; and where exemption mechanisms were functional were able to have a positive impact on service utilization and vice versa. Most of these studies were from Africa29. None of these studies have used a control area to validate their findings whereas in the present study a reference area was used to compare within the same State.
A study which used household survey data in India shows price elasticity for OPD consultation which is not significantly different from zero, implying an insignificant change for OPD care with introduction of user charges30. Further, this study found that price elasticity was indistinguishable from zero at all income levels. However, other studies (Maharashtra, India) have indicated a decline in both OPD and indoor admissions after introduction of user charges, both at overall level and specifically for the poor31. It has been shown that areas which succeed in utilizing extra revenue generated in improving local service availability and quality result in improved service utilization29. This is also substantiated from Maharashtra where declining service utilization was associated with evidence that user fees remained largely un-utilized even when retained by hospital committees at district level35. Without improvements in quality and enforcement of exemptions, it seems reasonable that utilization declined in Maharashtra especially for poor. Utilization of user charges in Haryana was found to be more than 80 per cent in all the years. It was found that the user charge was not utilized to increase availability of medicines or make services available round the clock by recruiting additional staff on contract basis. These factors could have contributed to decline in service utilization despite having extra resources from the user fee.
The present study also has some limitations. Inability to extract stratified (at the level of area and gender) district level data for past years (2000-2002) was major limitation of the study. Also, routine data were available for only one year prior to intervention. Quality of data is always an issue in studies using routine MIS data. The hospital admission data from the MIS were available from more than 86 per cent of the reporting units over the study period. We compared the hospitalization rate from the MIS data with that from NSSO data. While the NSS data report a public sector hospitalization rate of nearly 800 per 100,000 populations for Haryana15, MIS reported hospitalization rate of 822 and 1084 per 100,000 in the districts with and without user fee, respectively. Use of NSS data also imposed methodological limitations. Consumption expenditure in NSS survey is not differentiated between food and non-food expenditure. It underestimates prevalence of catastrophic expenditure at the WHO recommended 40 per cent cut-off level for non-food expenditure. As an alternative, we used a 10 per cent threshold to project more realistic estimates. At the national level in urban India, spending on food is 63 per cent of the total consumption expenditure for poorest and 35 per cent for the richest quintiles15. In rural areas of Haryana, poorest and richest quintiles spend 65 and 48 per cent expenditure on food, respectively. Hence the results of the present study for catastrophic expenditure may be an underestimate for the poorer income quintiles and vice versa. Similar arguments about current methods for catastrophic expenditures using the cross sectional surveys have been raised elewhere32,33.
We chose to study the impact of user charges in Haryana State as it implemented user charges in a phased manner, providing an opportunity to design a quasi-experimental study to measure the effects. Overall, user charges in Haryana showed adverse impact on health care utilization especially among poor, hence, one should be careful in implementation of policies for demand-side cost sharing in India. Our study shows that high OOP spending especially for inpatient care poses barriers to access for some. At the same time, those who utilize health care face the catastrophic expenditures. The results of our study are generalizable to other parts of the country with similar socio-demographic profiles and health system characteristics. However, since health is a State subject in India, with different context, governance and policies related to implementation of user charges, these factors should be borne in mind when generalizing the findings of this study.
Acknowledgment
The research project was funded by the Indian Association of Preventive and Social Medicine. The authors gratefully acknowledge financial assistance from LSE Health, London School of Economics in obtaining NSSO data. We would like to acknowledge support of Haryana Health Department, Dr P.K. Singh, Dr Shivinder Singh and Dr J.C. Bansal in data extraction.
References
- 1.Thomson S, Foubister T, Mossialos E. Financing health care in European Union challenges and policy responses. London: WHO Regional Office for Europe; 2009. [Google Scholar]
- 2.Robinson R. User charges for health care. In: Mossialos E, Dixon A, Figueras J, Kutzin J, editors. Funding health care: Options for Europe. Buckingham: Open University Press; 2002. [Google Scholar]
- 3.Kutzin J. The appropriate role for patient cost sharing. In: Saltman R, Figueras J, Sakellarides C, editors. Critical challenges for health care reform in Europe. Buckingham: Open University Press; 1998. [Google Scholar]
- 4.Manning W, Newhouse J, Duan N, Keeler E, Leibowitz A. Health insurance and the demand for medical care: Evidence from a Randomized Experiment. Am Econ Rev. 1987;77:251–77. [PubMed] [Google Scholar]
- 5.Van Damme W, Meessen B, Por I, Kober K. Catastrophic health expenditure. Lancet. 2003;362:996. doi: 10.1016/S0140-6736(03)14375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.James CD, Hanson K, McPake B, Balabanova D, Gwatkin D, Hopwood I, et al. To retain or remove user fees?: reflections on the current debate in low- and middle-income countries. Appl Health Econ Health Policy. 2006;5:137–53. doi: 10.2165/00148365-200605030-00001. [DOI] [PubMed] [Google Scholar]
- 7.McIntyre D, Thiede M, Dahlgren G, Whitehead M. What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts? Soc Sci Med. 2006;62:858–65. doi: 10.1016/j.socscimed.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Leive A, Xu K. Coping with out-of-pocket health payments: empirical evidence from 15 African countries. Bull World Health Organ. 2008;86:849–56. doi: 10.2471/BLT.07.049403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lagarde M, Palmer N. The impact of user fees on health service utilization in low- and middle-income countries: how strong is the evidence? Bull World Health Organ. 2008;86:839–48. doi: 10.2471/BLT.07.049197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wagstaff A, van Doorslaer E, van der Burg H, Calonge S, Christiansen T, Citoni G, et al. Equity in the finance of health care: some further international comparisons. J Health Econ. 1999;18:263–90. doi: 10.1016/s0167-6296(98)00044-7. [DOI] [PubMed] [Google Scholar]
- 11.MOHFW. A handbook for the State Investment Programme Managers & ECTA facilitators & consultants. New Delhi: Ministry of Health & Family Welfare. Government of India and European Commission; 2000. Sector Investment Programme (supported by EC) [Google Scholar]
- 12.National Rural Health Mission: Implemenatation Guidelines. New Delhi: Ministry of Health and Family Welfare, Government of India; 2005. MOHFW. [Google Scholar]
- 13.Ram F, Shekhar C. Ranking and mapping of districts based on socio-economic and demographic indicators. Mumbai: International Institute of Population Sciences; 2006. [Google Scholar]
- 14.England S, Kaddar M, Nigan A, Pinto M. Practice and policies on user fees for immunization in developing countries. Geneva: World Health Organization; 2001. [Google Scholar]
- 15.Morbidity, Health Care and the Condition of the Aged. NSS 60th Round (January-June 2004) New Delhi: National Sample Survey Organization, Ministry of Statistics and Programme Implementation, Government of India; 2006. NSSO. [Google Scholar]
- 16.SPSS for Windows, version 13.0. Chicago: SPSS Inc; 2004. SPSS Inc. [Google Scholar]
- 17.O’Donnell O, Van Doorslaer E, Wagstaff A, Lindelow M. Analyzing health equity using household survey data a guide to techniques and their implementation. Washington, DC: The World Bank; 2008. [Google Scholar]
- 18.The influence of financial participation of population on the demand for health care: an analytical tool for countries in greatest need. Geneva: World Health Organization; 1994. WHO. [Google Scholar]
- 19.Prinja S, Gupta M, Singh A, Kumar R. Effectiveness of planning and management interventions for improving age-appropriate immunization in rural India. Bull World Health Organ. 2010;88:97–103. doi: 10.2471/BLT.08.059543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pannarunothai S, Mills A. The poor pay more: health-related inequality in Thailand. Soc Sci Med. 1997;44:1781–90. doi: 10.1016/s0277-9536(96)00287-0. [DOI] [PubMed] [Google Scholar]
- 21.Pillai RK, Williams SV, Glick HA, Polsky D, Berlin JA, Lowe RA. Factors affecting decisions to seek treatment for sick children in Kerala, India. Soc Sci Med. 2003;57:783–90. doi: 10.1016/s0277-9536(02)00448-3. [DOI] [PubMed] [Google Scholar]
- 22.Sekhri N, Savedoff W. Private health insurance: implications for developing countries. Bull World Health Organ. 2005;83:127–34. [PMC free article] [PubMed] [Google Scholar]
- 23.National Family health Survey 3. Mumbai: International Institute of Population Sciences and ORG Macro; 2006. IIPS. [Google Scholar]
- 24.Sample Registration Survey Bulletin. New Delhi: Registrar General of India; 2006. SRS. [Google Scholar]
- 25.Nyonator F, Kutzin J. Health for some? The effects of user fees in the Volta Region of Ghana. Health Policy Plan. 1999;14:329–41. doi: 10.1093/heapol/14.4.329. [DOI] [PubMed] [Google Scholar]
- 26.Collins D, Quick J, Musau S, Kraushaar D, Hussein I. The fall and rise of cost sharing in Kenya: the impact of phased implementation. Health Policy Plan. 1996;11:52–63. doi: 10.1093/heapol/11.1.52. [DOI] [PubMed] [Google Scholar]
- 27.Bodart G, Servais G, Mohamed Y, Schmidt-Ehry B. The influence of health sector reform and external assistance in Burkina Faso. Health Policy Plan. 2001;16:74–86. doi: 10.1093/heapol/16.1.74. [DOI] [PubMed] [Google Scholar]
- 28.Mbugua JK, Bloom GH, Segall M. Impact of user charges on vulnerable groups: the case of Kibwezi in rural Kenya. Soc Sci Med. 1995;41:829–35. doi: 10.1016/0277-9536(94)00400-n. [DOI] [PubMed] [Google Scholar]
- 29.Building on the user fee experience: The African case. Geneva: World Health Organization; 2003. WHO. [Google Scholar]
- 30.Gupta I, Dasgupta P. Demand for curative health care in rural India: Choosing between private, public and no care. New Delhi: Institute for Economic Growth; 2000. Discussion paper no 14/2000. [Google Scholar]
- 31.Mahal A, Veerabharaiah N. User charges in India's health care sector: An assessment. In: Lal PG, editor. NCMH background papers: Financing and delivery of health care services in India. New Delhi: National Commission on Macroeconomics and Health, Ministry of Health and Family Welfare, Government of India; 2005. [Google Scholar]
- 32.Prinja S, Kanavos P, Kumar R. Health care inequities in north India: Role of public sector in universalizing health care. Indian J Med Res. 2012;136:421–31. [PMC free article] [PubMed] [Google Scholar]
- 33.Prinja S, Verma R. Estimating catastrophic health expenditures: need for improved methodology and interpretation. Indian J Community Med. 2011;36:239–40. doi: 10.4103/0970-0218.86531. [DOI] [PMC free article] [PubMed] [Google Scholar]


