Abstract
Emphasis on translational research to facilitate progression from the laboratory into the community also creates a dynamic in which ethics and social policy questions and solutions are ever pressing. In response, academic institutions are creating Research Ethics Consultation Services (RECS). All Clinical Translational Science Award institutions were surveyed in early 2010 to determine which institutions have a RECS in operation and what is their composition and function. Of the 46 institutions surveyed, 33 (70%) have a RECS. Only 15 RECS have received any consult requests in the last year. Issues that are common among these relatively nascent services include relationships with institutional oversight committees, balancing requestor concerns about confidentiality with research integrity and human subjects protection priorities, tracking consult data and outcomes, and developing systems for internal evaluation. There is variability in how these issues are approached. It will be important to be attentive to the institutional context to develop an appropriate approach. Further data about the issues raised by requestors and the recommendations provided are necessary to build a community of scholars who can navigate and resolve ethical issues encountered along the translational research pathway. Clin Trans Sci 2013; Volume 6: 40–44
Keywords: ethics, translational research, outcomes research
Introduction
Basic scientists and clinical researchers have sought informal advice from colleagues in bioethics in casual “hallway,” or im promptu, conversations to address challenging ethical issues related to their human subject research from design to implementation to analysis and reporting. These informal interactions have evolved into explicit Research Ethics Consultation Services (RECS) at some academic medical institutions. As Beskow et al.1 noted, research ethics consultants interact with researchers and others in the research enterprise to “provide information; identify, analyze, and/or deliberate about ethical issues; and recommend a course of action.” Cho et al.2 articulated an overarching goal for RECS: to improve the overall quality of research, maximizing benefits and minimizing risks to the social well‐being of individuals and society.
It is not clear how prevalent this new formalized research ethics consultation approach is, nor is it clear how these consultation services are structured. Several research ethics consultants have described their experiences of offering advice to researchers, characterizing their own institutions’ RECS, and have identified important organizational issues that arise in the context of providing consults.3, 4, 5 Organizational issues addressed in this literature include relationships with other organizational programs such as institutional review boards, the confidentiality of the discussions, and the obligations of consultants to the researcher(s) and to the institution. In addition, these institutional descriptions suggest that at this point in time there is neither a consensus on what the best practices are for RECS nor how to best structure such a service in academic research institutions. This is largely due to the fact that there are few empirical data that describe the complete landscape of how these services are evolving. Such data can guide institutions when considering how best to structure such programs and can guide the subsequent empirical research assessing the impact of such programs.
Between 1996 and 2005, a handful of academic medical centers established REC services to meet specific institutional needs. The REC service at the NIH Clinical Center focused on the impact of research on research participants, also functioning as the clinical ethics consult service,6 while the service at the Johns Hopkins Bloomberg School of Public Heath emphasized public health research, including international research.5 The service created at Stanford University included the ethical issues raised by basic science research, and was originally focused largely on the ethical, legal, and social implications (ELSI) of genetic/genomic research (although not exclusive of other types of issues).4 When the National Center for Research Resources initiated the Clinical and Translational Science Award (CTSA) Program in 2005, the request for applications noted the importance of institutional commitments to supporting ethics and many institutions responded with the development of research ethics consultation services.
The CTSA Consortium established the Clinical Research Ethics Key Function Committee (CRE KFC), in which every member of the Consortium has a representative. In April 2010, the CRE KFC Consultation Working Group surveyed the 46 CTSA intuitions that had been awarded to date, to describe the structure and function of research ethics consultation services within the Consortium. The survey included questions about funding, staffing, frequency of consultation requests, program evaluation, relationships with other institutional entities, and policies. We report here the first description of this group of RECS. Our findings about ways which CTSA institutions have developed REC services may serve as models for other universities that may wish to develop similar programs.
Methods
Our survey consisted of 32 multipart, closed ended questions that were developed by a subcommittee of the CRE KFC Research Ethics Consultation Working Group, to address questions that had emerged at KFC conference calls and national meetings. Survey domains included: consultant staffing, funding, access and utilization, reporting, tracking and evaluation, relationships with other institutional entities, and confidentiality and privacy. To distinguish between formal and informal consultation services respondents were asked to use the two definitions shown in Figure 1 when answering the inclusion question, “Does your institution have a formal research ethics consultation service?” (Figure 1).
Figure 1.
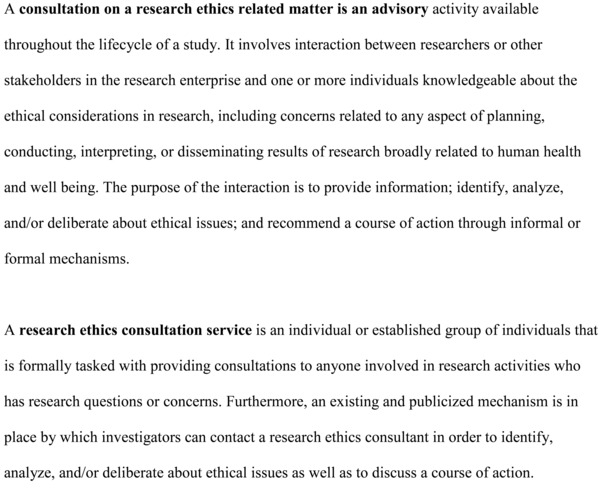
Definitions presented to participants in the introductory instructions of the survey.
All voting members (one per CTSA, N = 46) were contacted via email and asked to complete the survey or to forward it to the person most knowledgeable. To prevent duplication, we asked that only one survey per CTSA be completed. One CTSA has two distinct consult services at separate institutions, increasing our N to 47, and the survey was sent to both institutions. We asked respondents to include their names, institution, and CTSA to allow for targeted follow‐up and assist in achieving 100% response rate. Multiple follow‐up attempts were made by email and phone to encourage recipients to complete the survey. The use of identifiers allowed us to capture all research ethics consultation activities occurring within the CTSA Consortium.
The survey was distributed through REDCap (Research Electronic Data Capture) Survey, a web‐based application hosted developed within the CTSA consortium.7 A basic database software application (Microsoft Excel) was used for data collection and some tabulation. We performed basic descriptive analyses using contingency tables and frequency summations in statistical (STATA) software.8 This study was determined to be exempt from IRB review by the Mayo Clinic IRB.
Results
Each of the 46 CTSA institutions responded to the survey. One CTSA submitted two responses from each of its two RECS. Thirty‐three (70%) institutions had established a consultation service. Although nine of these institutions had initiated a consultation service prior to CTSA funding, only two had been in existence for 6 years or more (Table 1). Two other institutions had plans to establish a REC service within 18 months.
Table 1.
Characteristics of research ethics consult services (n = 33)
| RECS establishment | % (N) |
|---|---|
| <1 year | 18 (6) |
| 1.1–2 years | 15 (5) |
| 3–5 years | 24 (8) |
| 6+ years | 6 (2) |
| Number of core consultants | |
| 1–2 | 30 (10) |
| 3–5 | 58 (19) |
| 6–8 | 12 (4) |
| Committed FTE for consults | |
| 0 | 12 (4) |
| 0.05–0.20 | 36 (12) |
| 0.21–0.50 | 24 (8) |
| >0.51 | 15 (5) |
| Funding source for consult FTE | |
| CTSA | 76 (25) |
| Non‐CTSA grant sources | 21 (7) |
| Fee for service | 12 (4) |
| No explicit funding | 24 (8) |
| Importance of CTSA funding | |
| Very important | 52 (17) |
| Somewhat important | 18 (6) |
| Somewhat unimportant | 15 (5) |
| Not important at all | 12 (4) |
| Number of consultations, past 1 year | |
| 1–4 | 24 (8) |
| 5–10 | 3 (1) |
| 11–15 | 9 (3) |
| 16–25 | 6 (2) |
| 36+ | 3 (1) |
Frequencies for any given item will not necessarily total 33 because some questions allowed multiple responses and all participants did not respond to all questions.
Consultant staffing
The number of core consultants participating in a service ranged from 1 to 8 individuals, with 10 having only 1–2 individuals. Every site reported that consultants had only a portion of their salaried effort dedicated to the consultation service. Twenty‐four (73%) of the institutions supported 0.50 or less full time equivalent salary for consultation (Table 1). Most services reported that several areas of expertise were represented on their RECS. Backgrounds of RECS consultants included bioethics (31), medicine (26), humanities (19), law (14), epidemiology/public health (11), biological sciences (9), and social sciences (9).
Funding
When asked about relationships between an institution's RECS and its CTSA, 25 (76%) institutions used CTSA funding to support the consultation service. Among these 25, 19 did not exist prior to the institution's CTSA. Other sources of funding for RECS included non‐CTSA grant sources, fee‐for‐service mechanisms, and general institutional funding sources. Twenty‐three respondents indicated that CTSA funding was either “very” or “somewhat important” for the establishment, implementation, and/or expansion of their research ethics consultation service (Table 1).
Access and utilization
Across all RECS, consultations could be requested by researchers, staff, trainees, and IRB members. Research participants could also request a consult at 20 of 33 (61%) CTSA institutions. Nine (27%) services reported providing consults to individuals or groups not affiliated with their institution such as nonprofit agencies, governmental agencies, and companies or other for‐profit groups.
CTSA institutions reported that principal investigators or other research team staff comprise the majority of those from whom most consults have been requested. Fifteen RECS responded to the question asking how many consults had been provided over the previous year; five providing 11–15 consults and one institution provided more than 36 consults (Table 1).
Communication, tracking, and evaluation
Eighteen services (55%) reported having an electronic system for tracking or recording consultation data elements. Three services always provide formal reports to requestors; 20 do sometimes. Five services always include a disclaimer in the written report stating that consultants are providing nonbinding recommendations; two services sometimes follow this practice. Ten institutions track the outcomes of the consultation (e.g., whether consultees adopted the recommendations provided to her). Only five (16%) have developed evaluation criteria for their services.
Relationships with other institutional entities
Less than half of the services (43%, 20/46) have a relationship with their institution's IRB. In some cases, the IRB refers investigators to the RECS (15) or the consult service works with the IRB in advising researchers (7). At one institution, the IRB serves as the (only) research ethics consultation service. In other cases, members of the RECS service are (or have been) serving as either an IRB member or chairperson at 17 of the services. None of the institutions surveyed had formal policies prohibiting overlapping roles, such as concurrent membership on the IRB and RECS.
Twenty services (43%) have a relationship with their institution's clinical ethics consultation service (CECS). The clinical ethics consultation service refers investigators to the RECS at five institutions and the RECS refers patients/families to the clinical ethics consult service at three institutions. The two services consult with one another at seven institutions (7). At 20 CTSAs, some core consultants serve on both consultation services.
Confidentiality and privacy
Eight services have had requests for “complete” confidentiality before beginning a consult, and 24 had not. When the 24 RECS that had not had requests were asked whether there were certain situations in which they would consider breaking confidentiality, 18 indicated yes: for research misconduct cases (10) or regulatory violations that would trigger formal report to OHRP (13), or a if a research participant's safety was in jeopardy (12). Fourteen RECS have a standardized approach for handling issues of confidentiality and 17 do not. Only six institutions have written confidentiality templates to use to document their agreements of confidentiality.
Discussion
Research ethics consultation services are relatively common among CTSA institutions (70%). However, the majority of the services receive only a few requests. This limited utilization may reflect a lack of awareness of the RECS's existence at an institution or a lack of clarity with regard to how RECS is distinct from the types of advice provided by IRBs and clinical ethics services. Consultants should consider offering to present case examples at different departmental seminars. These case examples could be constructed to reflect potential concerns and issues that members of that given department might likely encounter. All institutions receiving NIH and NSF funding must provide a Responsible Conduct of Research curriculum to its NIH and NSF trainees. Consultants could interact with the RCR instructor (in many instances the instructor may be a core consultant on the service!) to provide materials about the RECS and even present during one of the lectures on what the RECS is and what kinds of services it can provide to researchers. The majority (73%) of RECS did not exist prior to their institution receiving a CTSA, suggesting that there may be a quasicausal relationship between NIH's CTSA initiative and the formalization of research ethics consultation services. Many indicated that CTSA funding is used for support, although, there is variability in the amount of FTEs that institutions are dedicating for RECS.
Many RECS have working relationships with IRBs/CECS, including consultants who have multiple roles. This likely reflects the limited availability of research ethics consultants at any particular institution, and multiple approaches to the provision of consultative services. More importantly, this highlights how persons engaged in research ethics activities recognize that there is a role for RECS distinct from the role of IRBs/CECS. IRBs provide oversight and are driven by existing regulations and compliance requirements. Moreover, the purview of IRBs extends only to that research involving human research participants. This leaves out a slice of translational research that embodies important ethical and social policy considerations of researchers: for example, research using de‐identified biological samples, conflict of interest concerns, questions of research integrity, and studies involving human embryonic stem cells and creating chimeras.
Research ethics consultants often are in a position to interact with investigators prior to the IRB submission providing recommendations that can actually enhance the IRB review process and allow the IRB to focus on its primary mission of ensuring the protection of research participants’ rights and safety. No doubt as certain technologies such as whole genome sequencing and regenerative medicine are translated into clinical use, the space of translational ethics will widen and will encompass the expertise of both research and clinical ethics consultants. It will be important to further clarify these differing roles—and the value added by RECS—as these programs become more established.1 The results described here are a first step in better understanding these aspects of RECS delivery.
There do not yet appear to be standardized approaches for structuring RECS, apart from their memberships and users. Key expectations regarding requestor confidentiality have yet to emerge across RECS. When is it appropriate to offer confidentiality for consultations and when is it not, are crucial questions. Taylor and Kass have described an approach that works for their RECS.5 They inform requestors that consult information is routinely shared with other consultants and institutional officials. Other services may keep the identity of a requestor confidential even from other consultants, except when the consultant has serious concerns about harm to self or others. If RECS models are to succeed, they must not only provide quality advice but also build trusting relationships with researchers. The results from this survey demonstrate that some services have developed standard approaches or protocols to addressing the delicate issue of confidentiality; however, most services have not. Similarly, standard approaches to the documentation of consultation requests and/or evaluation of consultation outcomes are not evident. Few RECS have developed and implemented processes for tracking and evaluating their services. Both are essential to provide critical data for quality improvement of these nascent research resources.9
Given the ever increasing integration between research and clinical care, research investigators and ethics consultants are likely to be facing new and challenging questions. Research ethics consultation services can bring a “team‐oriented” approach to identify ways to address the ethical, policy, and social challenges presented by translational and clinical research: when ethics consultants and scientists work together to address questions, multidisciplinary expertise is leveraged.2 McCormick et al.10 reported empirical data suggesting that researchers are willing to utilize such services. Fully engaging researchers in deliberative processes to develop strategies to respond to ethical issues in their human subject research may also prove to benefit the process of research design generally. Further, as new technologies, such as next generation sequencing become more common, complicated issues about how to respond to incidental findings will more common,11 and REC services may be well positioned to provide advice and guidance.12
These collaborative efforts may be increasingly important as emerging informatics capabilities, the rapid pace of technology development, and greater involvement of communities in the research process have made the ethical issues in clinical and translational research more visible and perhaps even more complicated than previously.12, 13, 14, 15, 16 Providing an institutionally supported resource for researchers to obtain advice on ethical issues that researchers might encounter is valuable. Issues may be identified not only be researcher but also by others during grant reviews, IRB reviews, or publication peer review, or FDA reviews.
Although our data suggest emerging interest in establishing such services and variability of approaches, the survey does not provide data about the outcomes or impact of these services on institutions or the research community. Further, little is known about the quality of the advice provided. These are critical questions the authors are addressing. Empirically driven studies include identifying metrics and evaluating the impact of research ethics consultation services on requesters, research projects, and institutions. These will be critical to ensuring the quality of recommendations provided to researchers and providing best practices for creating and maintaining these services.
Another element to addressing these critical questions is identifying the common approaches to analysis and recommendations about ethical concerns and social policy considerations in research. Given the Office of Human Research Protections efforts to revise the current paradigm of involving humans in research and collection, storing, and future use of biological specimens, empirically studying these approaches can inform not just best practices for RECS but also revision of federal policies.
An important step toward enhancing quality of not just recommendations provided but also the nature and scope of the services themselves is a commitment from RECS and their institutions to systematically collect a standard set of data from all consults. The CTSA consortium can provide an infrastructure to further address this goal. In particular, the CRE KFC consultation working group has established a repository to share limited information about consults across participating institutions. This working group has also started a web forum to facilitate discussions about consults. The motivation for developing these tools is to improve the quality of future consultations, by allowing consultants to learn from each other as emerging issues arise at the interface of translational science, community needs, and social policy,1, 9 and to assist those consultants who are establishing new consult services.
Although quality improvement can be facilitated by future data collection both locally and nationally, we offer some current “best practice” recommendations in response to the data collected in this survey. First, particularly when consultants serve multiple roles within the institution, such as the IRBs or CECS, it is important to distinguish between these roles and clarify expectations and obligations that may be role dependent in particular when promoting the service as well as when providing consultations. Second, it is important that the RECS engage in discussions about complementary roles and collaborative relationships, not only with the IRB and CEC, but other groups that may touch on related issues, including responsible conduct of research programs, research subject advocates, ombudsman, human resources, etc. Third, developing standard approaches about confidentiality and limits of confidentiality should involve explicit discussions with the other institutional entities mentioned above. Finally, it will be essential that the approaches developed in responses to these issues be communicated with the potential requestors of consults. Ongoing communication to ensure the local research community is generally aware that a consult service has been established is essential. For example, giving presentations at departmental meetings and other venues about what the service can provide them, and/or showcase a consult with clear benefits to the requestor may be helpful. Over time, and ideally facilitated by the CTSA consortium approaches to sharing collective experiences, research ethics consultation will become a transformative component to the clinical and translational research enterprise that will be valued by researchers and their institutions.
Sources of Funding
The project described was supported in part by UL1RR024150 (J. B. Mc.), UL1RR024989 (R. R. S.), UL1RR025755 (C. R. R.), UL1RR025005 (H. A. T.), UL1RR025014 (B. S. W.), and UL1RR025014–04S1 (J. B. Mc., R. R. S., H. A. T., B. S. W.) from the National Center for Research Resources and National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), through the Clinical and Translational Science Awards Program (CTSA), part of the Roadmap Initiative, Re‐engineering the Clinical Research Enterprise. The manuscript was approved by the CTSA Consortium Publications Committee.
Ethical Approval
A consultation on a research ethics related matter is an advisory activity available throughout the lifecycle of a study. It involves interaction between researchers or other stakeholders in the research enterprise and one or more individuals knowledgeable about the ethical considerations in research, including concerns related to any aspect of planning, conducting, interpreting, or disseminating results of research broadly related to human health and well being. The purpose of the interaction is to provide information; identify, analyze, and/or deliberate about ethical issues; and recommend a course of action through informal or formal mechanisms.
A research ethics consultation service is an individual or established group of individuals that is formally tasked with providing consultations to anyone involved in research activities who has research questions or concerns. Furthermore, an existing and publicized mechanism is in place by which investigators can contact a research ethics consultant in order to identify, analyze, and/or deliberate about ethical issues as well as to discuss a course of action.
Acknowledgments
The authors would like to thank Dr. Laura Beskow for her contributions to the survey design, Ms. Lisa Linn for her assistance with final manuscript preparation, and Ms. Marguerite Robinson for thoughtful comments and suggestions.
All authors contributed to study and survey. J.B.M. and A.L.O. collected and analyzed the data; J.B.M. drafted the manuscript; and R.R.S., A.L.O., C.R.R., H.A.T., and B.S.W. made significant contributions to writing the final document.
References
- 1. Beskow L, Grady C, Iitis AS, Sadler JZ, Wilfond BS. Points to consider: the research ethics consultation service and the IRB. IRB: Ethics Hum Res. 2009; 31: 1–9. [PMC free article] [PubMed] [Google Scholar]
- 2. Cho MK, Tobin SL, Greely HT, McCormick J, Boyce A, Magnus D. Strangers at the benchside: research ethics consultation. Am J Bioeth. 2008; 8: 4–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. de Melo‐Martín I, Palmer LI, Fins JJ. Viewpoint: developing a research ethics consultation service to foster responsive and responsible clinical research. Acad Med. 2007; 82: 900–904. [DOI] [PubMed] [Google Scholar]
- 4. Cho MK, Tobin SL, Greely HT, McCormick J, Boyce A, Magnus D. Research ethics consultation: the Stanford experience. IRB: Ethics Hum Res. 2008; 30: 1–6. 5. [PMC free article] [PubMed] [Google Scholar]
- 5. Taylor HA, Kass NE. Research ethics consultation at the Johns Hopkins Bloomberg School of Public Health. IRB: Ethics Hum Res. 2009; 31: 9–14. 6. [PMC free article] [PubMed] [Google Scholar]
- 6. DuVal G, Gensler G, Danis M. Ethical dilemmas encountered by clinical researchers. J Clin Ethics. 2005; 16: 267–276. 7. [PubMed] [Google Scholar]
- 7. Harris PA, Taylor R, Thielke R, Payne P, Gonzalez N, Conde J G. Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42: 337–381. 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stata 10.0. StataCorp LP; College Station, Texas. [Google Scholar]
- 9. Kelley M, Fryer‐Edwards K, Fullerton SM, Gallagher TH, Wilfond B. Sharing data and experience: using the clinical and translational science award “moral community” to improve research ethics consultation. Am J Bioeth. 2008; 8: 4–13. [DOI] [PubMed] [Google Scholar]
- 10. McCormick JB, Boyce AM, Cho MK. Biomedical scientists’ perceptions of ethical and social implications: is there a role for research ethics consultation. PLoS ONE. 2009; 4: e4659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bemmels HR, Wolf SM, Van Ness B. Mapping the inputs, analyses, and outputs of biobank research systems to identify sources of incidental findings and individual research results for potential return to participants. Genet Med. 2012; 4: 385–392. 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Havard M, Cho MK, Magnus D. Triggers for research ethics consultation. Sci Transl Med. 2012; 4: 118. 13. [DOI] [PubMed] [Google Scholar]
- 13. Boyer BB., Dillard D, Woodahl EL, Whitener R, Thummel KE, Burke W. Ethical issues in developing pharmacogenetic research partnerships with American indigenous communities. Clin Pharmacol Ther. 2011; 89: 343–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Greely HT. The uneasy ethical and legal underpinnings of large‐scale genomic biobanks. Ann Rev Genomics Hum Genet. 2007; 8: 343–364. [DOI] [PubMed] [Google Scholar]
- 15. Aalta‐Setala K, Conklin BR, Lo B. Obtaining consent for future research with induced pluripotent cells: opportunities and challenges. PLoS Biol. 2009; 7: e42. 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Illes J, Kirschen M, Edwards E, Stanford LR, Bandettini P, Cho M, Ford PJ, Glover GH, Kulynych J, Macklin R, et al. Incidental findings in brain imaging research. Science. 2006; 311: 783–784. [DOI] [PMC free article] [PubMed] [Google Scholar]


