Abstract
Purpose of review
Great progress has been made in recent years in understanding the expanding roles of the vitamin D endocrine system beyond calcemic regulation, including pathophysiological actions in the kidney and the cardiovascular system. The purpose of this review is to update the recent advance regarding the effects of vitamin D and its analogs on the renal and cardiovascular system.
Recent findings
Vitamin D-deficiency is not only widely associated with chronic kidney disease and cardiovascular disease in humans, but may also accelerate the disease progression. Dysregulation of vitamin D metabolism caused by renal insufficiency contributes to the low vitamin D status. Preclinical and clinical studies have demonstrated impressive therapeutic outcome with low-calcemic vitamin D analogs in renal and cardiovascular disease. The mechanism underlying the renal and cardiovascular protection involves regulation of multiple signaling pathways by vitamin D including NF-κB, Wnt/β-catenin and the renin-angiotensin system.
Summary
The renal and cardiovascular protective activity of vitamin D revealed in recent studies has profound clinical implications. Nutritional correction of vitamin D-deficiency and treatment with vitamin D analogs could be therapeutic options for renal and cardiovascular problems. New vitamin D analogs with better renal and cardiovascular therapeutic efficacy are highly desired. More randomized trials are needed to address these issues.
Keywords: Cardiovascular disease, Chronic kidney disease, Renin-angiotensin system, Vitamin D, Vitamin D-deficiency, Vitamin D analogs
Introduction
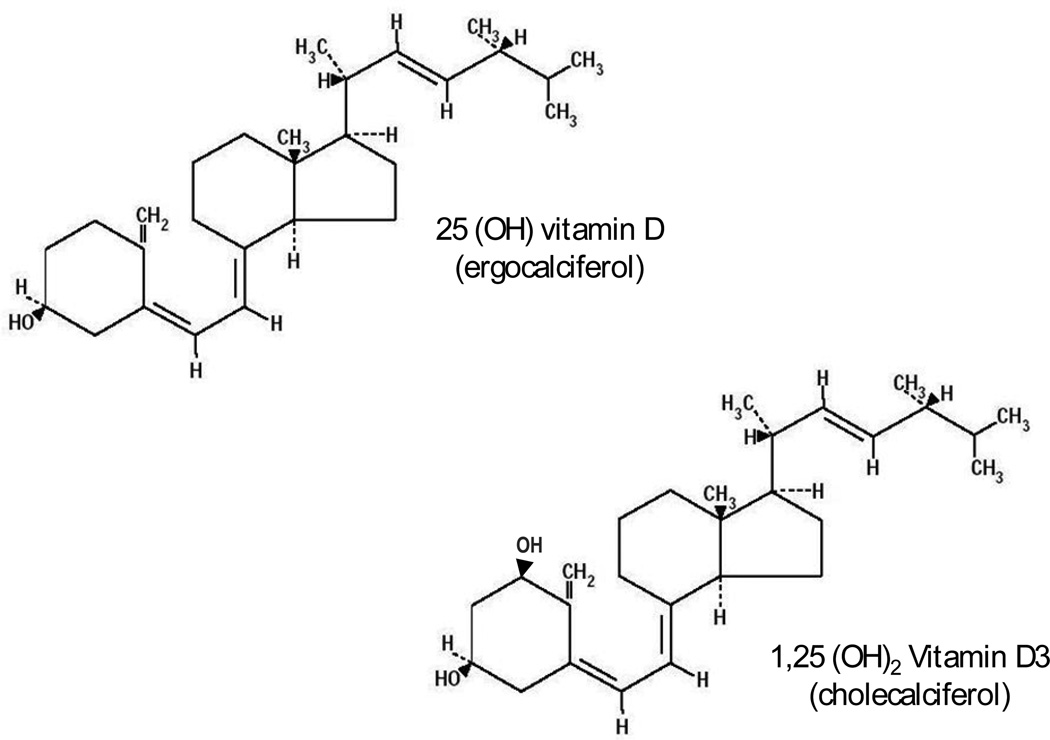
Vitamin D-deficiency (usually defined as serum 25-hydroxyvitamin D levels (25(OH)D) < 20 ng/mL or 50 nmol/L) is an emerging global health problem that is estimated to affect more than one billion people worldwide [1]. The vitamin D endocrine system, with 1,25-dihydroxyvitamin D3 (1,25(OH)2D3) as the most active hormonal metabolite, is a pleiotropic hormonal system (figure 1). As such, vitamin D-deficiency has various adverse consequences [1], including detrimental impact on the renal and cardiovascular system. Studies in recent years have demonstrated strong renal and cardiovascular protective effects of vitamin D and its analogs. Renal and cardiovascular disorders are leading causes of death in humans, thus these findings have profound clinical implications. The main focus of this review is to update the most recent development in the understanding of the renal and cardiovascular effects of vitamin D.
Figure 1.
Although 1,25 (OH) D3 has the greatest affinity for the vitamin D receptor, because of their similar chemical structures and much higher levels, ergocalcifetol is also a physiologically important agonist.
High prevalence of vitamin D-deficiency in chronic kidney disease
High prevalence of vitamin D-deficiency or -insufficiency in patients with chronic kidney disease (CKD) has been well documented in recent epidemiological studies. Low serum 25(OH)D status, particularly low 1,25(OH)2D3 levels, is very common in patients with CKD even at early stages, and the severity of deficiency increases with the progression of kidney disease [2, 3]. Cross-sectional analyses showed that 25(OH)D-deficiency is associated with impaired glomerular filtration rate (GFR) in CKD [4], and 25(OH)D- and 1,25(OH)2D3-deficiency are independently associated with decreased hemoglobin levels and anemia in early CKD [5]. Data from the Third National Health and Nutrition Examination Survey (NHANES III) in the United States revealed a correlation between low serum 25(OH)D (<15–17.8 ng/mL) and the risk of all-cause mortality in the general population [6] and in subjects with CKD who are not undergoing dialysis [7]. Recently data from the Ludwigshafen Risk and Cardiovascular (LURIC) Health Study confirmed that low vitamin D status is associated with all-cause mortality and cardiovascular mortality in CKD patients in Germany [8], and a meta-analysis of 10 prospective studies confirmed that high 25(OH)D levels are associated with significantly improved survival in patients with CKD [9]. Vitamin D-deficiency is closely correlated to kidney disease progression, and the serum vitamin D status is an independent inverse predictor of disease progression and death in CKD patients [10], suggesting that vitamin D-deficiency may in fact accelerate the progression of CKD. On the other hand, numerous retrospective observational studies in the last few years consistently reported reduced mortality in hemodialysis and non-dialysis CKD patients receiving vitamin D or its analog therapy [11]. Whether vitamin D-deficiency is in fact the cause of CKD progression and whether raising vitamin D levels or correcting vitamin D-deficiency indeed ameliorates CKD, however, require large randomized controlled clinical trials to address.
Altered vitamin D metabolism in kidney disease
Recent studies provide evidence that dysregulation of vitamin D metabolism is a main cause for vitamin D-deficiency in CKD. The majority of vitamin D in the body comes from de novo synthesis in the skin, catalyzed by ultraviolet light from the sunlight. Once synthesized, vitamin D is quickly converted in the liver to 25(OH)D, the predominant circulating metabolite. In the circulation 25(OH)D complexes with vitamin D binding protein (DBP). Following glomerular filtration the 25(OH)D-DBP complex is reabsorbed via megalin-mediated endocytosis in the proximal tubules [12], where 25(OH)D is converted to 1,25(OH)2D3 by renal 1α-hydroxylase (CYP27B1) [1]. In renal insufficiency, the decline in megalin-mediated endocytotic activity and renal 1α-hydroxylase activity and the loss of 25(OH)D-DBP into the urine because of proteinuria contribute to the development of 25(OH)D and 1,25(OH)2D3 deficiency. This notion is supported by recent experimental data that demonstrate dysregulated vitamin D metabolism in kidney disease. Urinary excretion of DBP was found elevated in type 1 diabetes patients [13], and levels of megalin, DBP and 25(OH)D increased in the urine of type 1 diabetic mice [14]. In Zucker diabetic fatty rats, the expression of megalin and Dab2 was decreased in the kidney and renal reuptake of 25(OH)D-DBP was compromised, accompanied by reduced levels of 25(OH)D and 1,25(OH)2D3 in the serum and elevated urinary excretion of 25(OH)D, 1,25(OH)2D3 and DBP [15]. Moreover, renal 24-hydroxylase (CYP24A1), the catabolic enzyme involved in 25(OH)D and 1,25(OH)2D3 degradation, was found markedly elevated in uremic rats and diseased human kidney biopsies, together with reduction in serum 1,25(OH)2D3 [16]. This suggests that increased CYP24A1 activity also contributes to vitamin D-deficiency in kidney disease.
Another factor that contributes to the low vitamin D status in CKD is fibroblast growth factor (FGF) 23, a major phosphatonin that promotes renal phosphate excretion and suppresses 1,25(OH)2D3 production via inhibition of CYP27B1 and stimulation of CYP24A1 [17]. Circulating FGF23 levels are elevated along with the decline of GFR and the increase in serum creatinine and phosphate levels [18–20]. In advanced CKD persistent phosphate retention due to impaired kidney function greatly induces FGF23, leading to suppression of 1,25(OH)2D3 production. In addition, conventional risk factors such as reduced sunlight exposure and poor dietary vitamin D intake also contribute to vitamin D insufficiency in the CKD population.
Anti-proteinuric activity of vitamin D
Albuminuria is a major risk factor for CKD progression, renal failure, cardiovascular events and death [21], thus reduction of albuminuria is a crucial therapeutic target for CKD. A cross-sectional analysis of the NHANES III data revealed a correlation between vitamin D-insufficiency and increased prevalence of albuminuria in the US adult population [22], suggesting that vitamin D has an intrinsic anti-proteinuric activity. A number of clinical studies have demonstrated therapeutic efficacy of vitamin D analogs to reduce proteinuria. Following an early report that activated vitamin D analog paricalcitol has significant anti-proteinuric activity in CKD [23], two small randomized pilot trials were conducted to evaluate the anti-proteinuric effect of oral paricalcitol treatment in CKD patients (n=24 and n=61, respectively) [24, 25]. These trials showed that paricalcitol significantly reduced albuminuria independent of its effect on hemodynamics or parathyroid hormone suppression. Most recently, a large randomized placebo-controlled clinical trial (the VITAL Study, n=281) confirmed that paricalcitol is able to reduce albuminuria and blood pressure in patients with diabetic nephropathy who were already on renin-angiotensin inhibitor therapy [26]. Together these clinical data provide a strong case to argue for the use of low-calcemic vitamin D analogs as a complementary therapy for treatment of proteinuria. Given the importance of podocytes in the regulation of glomerular filtration, it is speculated that podocytes are important anti-proteinuric target of vitamin D [27].
Renoprotective mechanisms
Recent research with different experimental models of kidney disease has provided good insights into the reno-protective mechanism for vitamin D and its analogs. The reno-protective activity of vitamin D is mediated by the vitamin D receptor (VDR) and appears to act by regulating multiple pathways including the renin-angiotensin system (RAS), NF-κB, Wnt/β-catenin and some key structural proteins (Table 1).
Table 1.
Potential renoprotective actions of 1,25(OH)2 vitamin D
| Suppression of the renin angiotensin system. |
| Reduced NF-κB activation and inflammation. |
| Inhibition of the Wnt/β-catenin pathway. |
| Direct effects on the expression of slit diaphragm proteins |
The renin-angiotensin system
The intrarenal RAS is a major mediator of renal damage. Many pathological conditions such as hyperglycemia, renal insufficiency and vitamin D-deficiency can activate the local RAS in the kidney, leading to increased local concentration of angiotensin (Ang) II, the effector of the RAS cascade that has a broad range of pathogenic activities that promote renal injury [28]. It is well established that the vitamin D hormone is a negative regulator of the RAS by suppressing renin expression [29, 30]. VDR-null mutant mice develop more severe renal damage (e.g. increased albuminuria, glomerulosclerosis and interstitial fibrosis) than wild-type counterparts in diabetic state [31] or under unilateral ureteral obstruction (UUO) [32], because of enhanced activation of the RAS in the kidney. In rats with 5/6 nephrectomy paricalcitol treatment attenuated glomerular and tubulointerstitial damage and reduced blood pressure and proteinuria by blocking the activation of the local RAS in the kidney remnant [33]. Vitamin D analog doxercalciferol modulated high fat-induced renal disease by targeting the RAS and lipid metabolism [34]. Moreover, many studies proved that combination therapy with one vitamin D analog (paricalcitol or doxercalciferol) and one RAS inhibitor (ACE inhibitor or ARB) produced synergistic or additive therapeutic effects in blocking renal damage in experimental models of type 1 and type 2 diabetes mellitus [35–38], UUO [39] and 5/6 nephrectomy [40]. The basis for the enhanced reno-protective efficacy of the combination therapy is the blockade of the compensatory renin induction usually encountered in the use of RAS inhibitors by the vitamin D analog. Inhibition of the renin induction and Ang II accumulation within the kidney leads to significantly better therapeutic outcomes [41]. The combination strategy demonstrated in these preclinical studies explains why vitamin D analogs are still effective in reducing proteinuria in CKD patients who are already on RAS inhibitor therapy [24, 26]. Given that RAS inhibitors are standard of care for CKD and many other diseases, an important implication of the combination therapy is that vitamin D analogs can be used as complementary therapy in many human diseases.
NF-κB activation and inflammation
NF-κB is a family of transcription factors that functions as a master regulator of immune response. NF-κB regulates a wide range of genes involved in inflammation, proliferation and fibrogenesis that are known to play important roles in kidney disease [42]. Vitamin D suppresses NF-κB activation, partly by disrupting DNA binding of NF-κB [43]. Serum vitamin D status is inversely associated with increased renal inflammation in patients with a variety of kidney disorders [44]. Recent investigations showed that paricalcitol protects against kidney damage by blocking NF-κB activity and reducing renal inflammation in experimental models of kidney disease such as UUO [45], cyclosporine-induced nephropathy [46] and gentamicin-induced renal injury [47]. At the molecular level, 1,25(OH)2D3 inhibits the expression of high glucose-induced MCP-1 and angiotensinogen and inflammation-induced PAI-1 by blocking the activation of NF-κB [48–50]. These factors are involved in renal disease progression. For example, MCP-1 induces infiltration of macrophages in the kidney, which release factors that can promote kidney disease progression. Ang II activates NF-κB, whereas NF-κB mediates high glucose induction of angiotensinogen, the substrate of renin for Ang II production. This vicious circle, which enhances the local accumulation of Ang II in diabetic nephropathy, can be disrupted by vitamin D [51].
Wnt/β-catenin pathway
Recent studies implicated that activation of the Wnt/β-catenin pathway induces podocyte injury and albuminuria in adriamycin nephropathy [52]. 1,25(OH)2D3 can block the Wnt/β-catenin pathway by promoting the physical interaction between VDR and β-catenin, thus preventing β-catenin nuclear translocation [53]. The molecular basis underlying liganded VDR and β-catenin interaction has been established [54]. Most recently, paricalcitol was shown to prevent podocyte dysfunction and ameliorate proteinuria by blocking Wnt/β-catenin signaling via VDR-β-catenin interaction [55].
Direct gene regulation
In the glomerular filtration barrier the slit diaphragm functions as the size-selective and charge-selective barrier to protein leakage. A number of proteins involved in the formation of the slit diaphragm are down-regulated in diabetes, and vitamin D therapy blocks the down-regulation [35, 37]. This vitamin D effect may result from direct stimulation on these genes, or secondary to the prevention of podocyte loss. Nephrin, a key slit diaphragm protein produced by podocytes [56], is induced by 1,25(OH)2D3 in podocyte cultures [57]. Most recent work identified a vitamin D response element (VDRE) in the proximal promoter of the nephrin gene that mediates nephrin up-regulation by 1,25(OH)2D3 [58]. This regulation likely accounts for part of the anti-proteinuric mechanism of vitamin D.
Association of vitamin D-deficiency with cardiovascular disease
There is also a growing body of epidemiological evidence that links vitamin D deficiency to cardiovascular disease. By cross-sectional analysis of the NHANES III (1988–1994) and NHANES 2001–2004 databases that are representative of the US adult population, a number of studies consistently demonstrated an association of low serum 25(OH)D levels with high blood pressure [59], increased prevalence of cardiovascular disease [60, 61] and cardiovascular risk factors including hypertension, diabetes, obesity and hyperlipidemia [62]. Prospective studies with cohorts from the Health Professionals’ Follow-Up Study (HPFS) and the Nurses’ Health Study (NHS) also showed an inverse correlation between serum 25(OH)D levels and the risk of incident hypertension [63] and myocardial infarction even after adjusting for factors known to be associated with coronary artery disease [64]. Low serum 25(OH)D is correlated with incident cardiovascular disease in Framingham Offspring Study participants without prior cardiovascular disease [65], and with high blood pressure in Hispanic and African Americans [66]. Vitamin D deficiency is also associated with coronary stenoses, coronary artery calcification and carotid atherosclerosis [67–69]. Moreover, the NHS and HPFS data suggest that higher vitamin D intake reduces the risk of cardiovascular disease in men [70], and a meta-analysis of 17 prospective studies also concludes that vitamin D supplements at moderate to high doses, but not calcium supplement, reduce the risk of cardiovascular disease [71].
Similar correlations are also reported in a variety of patient populations. Prospective analysis of a large electronic medical database demonstrated an association of vitamin D-deficiency with high prevalence of diabetes, hypertension, hyperlipidemia and peripheral vascular disease in a general US healthcare population [72]. Vitamin D-deficiency is associated with heart failure and sudden cardiac death in patients referred for coronary angiography in Europe [73]. A prospective cohort study showed that low serum 25(OH)D levels are associated with increased risk of cardiovascular events in chronic peritoneal dialysis patients in Hong Kong [74]. A meta-analysis of 18 published studies confirms the inverse relationship between blood 25(OH)D levels and hypertension [75]. Together these data indicate that vitamin D-deficiency is an important risk factor for cardiovascular disease.
Cardiovascular protective actions of vitamin D
Cardiovascular disease is common in the CKD population. A significant reduction in cardiovascular mortality was noticed in many retrospective observational studies that reported reduced mortality in CKD patients receiving vitamin D or its analog therapy (see references in [11]), suggesting that vitamin D has strong cardiovascular protective activity. This speculation is supported by animal studies conducted in recent years. In Dahl salt-sensitive rats paricalcitol treatment blocked high salt-induced cardiac hypertrophy [76]. More recent data showed that mono-treatment with paricalcitol or doxercalciferol or combination therapy with these analogs and RAS inhibitors (losartan or enalapril) prevented cardiac hypertrophy in spontaneously hypertensive rats [77] or prevented the progression of existing cardiac hypertrophy in Dahl salt sensitive rats [78]. As described above, the combination therapy blocked the compensatory induction of renin in the kidney and heart [77].
The cardio-protective mechanism of vitamin D remains to be fully defined. For the effect on cardiac hypertrophy, it is unclear if vitamin D directly acts on the heart via VDR. Although VDR expression was reported increased in hypertrophic heart in mice [79], whether VDR is indeed expressed in cardiomyocytes is controversial [80]. A VDR gene polymorphism is associated with left ventricular mass in patients with late stage CKD [81]. On the other hand, the effect of vitamin D on vascular disease is complex. While 1,25(OH)2D3 can induce vascular calcification in ApoE-null mice [82], it also inhibits foam cell formation, suppresses cholesterol uptake in macrophages from type 2 diabetes patients [83], and decreases atherosclerosis by regulating immune cells [84].
A general and likely mechanism underlying the cardiovascular effects of vitamin D is regulation of the RAS, a cascade that has a profound impact on the cardiovascular system. That 1,25(OH)2D3 functions as a negative regulator of the RAS has long been established. Null mutant mice lacking VDR or Cyp27b1 develop hyperreninemia and cardiac hypertrophy [29, 85]. Overexpression of human VDR in the juxtaglomerular cells suppresses renin expression in transgenic mice [86]. A recent study confirmed that vitamin D analog therapy can significantly suppress plasma renin activity in hemodialysis patients [77]. In healthy humans low vitamin D status may result in up-regulation of the RAS [87]. Data from the large cohort of patients (n>3000) in the LURIC study revealed that both serum 25(OH)D and 1,25(OH)2D3 levels are independently and inversely associated with plasma renin concentration and Ang II levels [88], strongly supporting the concept of vitamin D regulating RAS in humans. Having said that, the therapeutic efficacy of vitamin D and its analogs, either as primary or complementary therapy, in cardiovascular disease needs to be tested by randomized controlled clinical trials. In this regard, the ongoing PRIMO study, a randomized trial that investigates the effect of paricalcitol on the progression of left ventricular hypertrophy in stage 3 and 4 CKD patients (n=227) who are already on RAS inhibitors [89], is highly anticipated. This trial actually assesses the cardiac outcome of the combination of vitamin D analog and RAS inhibitor in humans. Studies like this are needed to fully understand the therapeutic potential of vitamin D and its analogs.
Conclusion
Research in the last few years has greatly advanced our understanding of the renal and cardiovascular effects of vitamin D. The evidence for vitamin D exerting renal and cardiovascular protection is abundant and strong, but the protective mechanism remains to be fully defined. Given the complexity of the disease and the pleiotropic nature of vitamin D activity, the protective effect is expected to be multi-factorial. This notion is supported by the mechanistic insights obtained so far from the experimental cell and animal models. With regard to the renal actions of vitamin D, great progress has been made with a variety of kidney disease models. In comparison, relatively few studies have been conducted to address the role of vitamin D-VDR signaling in vascular disease. An increasing body of epidemiological data has firmly established the correlation or association between low vitamin D status and renal and cardiovascular disease in humans, but clinical studies addressing causative relationship or therapeutic effects remain limited and thus are urgently needed. The prevalence of renal and cardiovascular diseases is increasing, yet disease treatment and management are costly with poor outcome. Better understanding of the renal and cardiovascular actions of vitamin D could stimulate the development of new vitamin D analog drugs for these diseases. One major shortcoming of the current vitamin D analog drugs is the relatively narrow therapeutic window mostly due to the hypercalcemic effect. Therefore, new analog drugs with less calcemic effect and better therapeutic efficacy for renal and cardiovascular diseases are highly desired.
Summary of key points.
Vitamin D-deficiency or insufficiency is associated with renal and cardiovascular disease. A rapidly growing body of evidence has suggested a role of vitamin D in renal and cardiovascular protection.
Vitamin D-deficiency is partly caused by dysregulation of vitamin D metabolism in kidney disease.
Reno-protective actions of vitamin D have been demonstrated in a variety of experimental models of kidney disease. The anti-proteinuric activity of vitamin D and vitamin D analogs is confirmed by randomized clinical trials.
The cardiovascular protective effect of vitamin D is supported by strong epidemiological data. Anti-hypertrophic and anti-atherosclerotic activities of vitamin D and vitamin D analogs have been reported in a number of animal models.
The renal and cardiovascular protective mechanism of vitamin D is multi-factorial and involves multiple regulatory pathways.
Acknowledgements
The author’s work was supported in part by National Institutes of Health grants R01HL085793 and R21 DK073183-01. The author also acknowledges grant support from American Diabetes Association (grant No. 7-05-RA-80), Genzyme Corp. and Abbott Laboratories.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References and recommended reading
* of special interest;
** of outstanding interest
- 1.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 2.Levin A, Bakris GL, Molitch M, et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int. 2007;71:31–38. doi: 10.1038/sj.ki.5002009. [DOI] [PubMed] [Google Scholar]
- 3.Levin A, Le Barbier M, Er L, et al. Incident isolated 1,25(OH)2D3 deficiency is more common than 25(OH)D deficiency in CKD. J Nephrol. 2011 doi: 10.5301/JN.2011.8429. [DOI] [PubMed] [Google Scholar]
- 4.Urena-Torres P, Metzger M, Haymann JP, et al. Association of Kidney Function, Vitamin D Deficiency, and Circulating Markers of Mineral and Bone Disorders in CKD. Am J Kidney Dis. 2011 doi: 10.1053/j.ajkd.2011.04.029. [DOI] [PubMed] [Google Scholar]
- 5.Patel NM, Gutierrez OM, Andress DL, et al. Vitamin D deficiency and anemia in early chronic kidney disease. Kidney Int. 2010;77:715–720. doi: 10.1038/ki.2009.551. [DOI] [PubMed] [Google Scholar]
- 6.Melamed ML, Michos ED, Post W, Astor B. 25-hydroxyvitamin D levels and the risk of mortality in the general population. Arch Intern Med. 2008;168:1629–1637. doi: 10.1001/archinte.168.15.1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehrotra R, Kermah DA, Salusky IB, et al. Chronic kidney disease, hypovitaminosis D, and mortality in the United States. Kidney Int. 2009;76:977–983. doi: 10.1038/ki.2009.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pilz S, Tomaschitz A, Friedl C, et al. Vitamin D status and mortality in chronic kidney disease. Nephrol Dial Transplant. 2011 doi: 10.1093/ndt/gfr076. [DOI] [PubMed] [Google Scholar]
- 9. Pilz S, Iodice S, Zittermann A, et al. Vitamin D Status and Mortality Risk in CKD: A Meta-analysis of Prospective Studies. Am J Kidney Dis. 2011 doi: 10.1053/j.ajkd.2011.03.020.. * This is a meta-analysis of 10 studies with a large sample of patients with CKD that confirms a correlation between low vitamin D status and mortality in CKD.
- 10.Ravani P, Malberti F, Tripepi G, et al. Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int. 2009;75:88–95. doi: 10.1038/ki.2008.501. [DOI] [PubMed] [Google Scholar]
- 11. Kovesdy CP. Survival benefits with vitamin D receptor activation: new insights since 2003. Clin J Am Soc Nephrol. 2010;5:1704–1709. doi: 10.2215/CJN.02590310.. ** A nice summary of the recent epidemiological evidence that demonstrates survival benefits of vitamin D and vitamin D analog therapy in CKD populations.
- 12.Nykjaer A, Dragun D, Walther D, et al. An endocytic pathway essential for renal uptake and activation of the steroid 25-(OH) vitamin D3. Cell. 1999;96:507–515. doi: 10.1016/s0092-8674(00)80655-8. [DOI] [PubMed] [Google Scholar]
- 13.Thrailkill KM, Jo CH, Cockrell GE, et al. Enhanced excretion of vitamin D binding protein in type 1 diabetes: a role in vitamin D deficiency? J Clin Endocrinol Metab. 2011;96:142–149. doi: 10.1210/jc.2010-0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fowlkes JL, Bunn RC, Cockrell GE, et al. Dysregulation of the intrarenal vitamin d endocytic pathway in a nephropathy-prone mouse model of type 1 diabetes. Exp Diabetes Res. 2011;2011:269378. doi: 10.1155/2011/269378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Anderson RL, Ternes SB, Strand KA, Rowling MJ. Vitamin D homeostasis is compromised due to increased urinary excretion of the 25-hydroxycholecalciferol-vitamin D-binding protein complex in the Zucker diabetic fatty rat. Am J Physiol Endocrinol Metab. 2010;299:E959–E967. doi: 10.1152/ajpendo.00218.2010.. * This study presents good evidence for impaired vitamin D metabolism that leads to vitamin D deficiency in diabetes.
- 16. Helvig CF, Cuerrier D, Hosfield CM, et al. Dysregulation of renal vitamin D metabolism in the uremic rat. Kidney Int. 2010;78:463–472. doi: 10.1038/ki.2010.168.. * An investigation that suggests that elevated vitamin D catabolism caused by increased CYP24A1 activity contributes to vitamin D-deficiency in advanced kidney disease.
- 17.Shimada T, Hasegawa H, Yamazaki Y, et al. FGF-23 is a potent regulator of vitamin D metabolism and phosphate homeostasis. J Bone Miner Res. 2004;19:429–435. doi: 10.1359/JBMR.0301264. [DOI] [PubMed] [Google Scholar]
- 18.Imanishi Y, Inaba M, Nakatsuka K, et al. FGF-23 in patients with end-stage renal disease on hemodialysis. Kidney Int. 2004;65:1943–1946. doi: 10.1111/j.1523-1755.2004.00604.x. [DOI] [PubMed] [Google Scholar]
- 19.Larsson T, Nisbeth U, Ljunggren O, et al. Circulating concentration of FGF-23 increases as renal function declines in patients with chronic kidney disease, but does not change in response to variation in phosphate intake in healthy volunteers. Kidney Int. 2003;64:2272–2279. doi: 10.1046/j.1523-1755.2003.00328.x. [DOI] [PubMed] [Google Scholar]
- 20.Shigematsu T, Kazama JJ, Yamashita T, et al. Possible involvement of circulating fibroblast growth factor 23 in the development of secondary hyperparathyroidism associated with renal insufficiency. Am J Kidney Dis. 2004;44:250–256. doi: 10.1053/j.ajkd.2004.04.029. [DOI] [PubMed] [Google Scholar]
- 21.Keane WF, Eknoyan G. Proteinuria, albuminuria, risk, assessment, detection, elimination (PARADE): a position paper of the National Kidney Foundation. Am J Kidney Dis. 1999;33:1004–1010. doi: 10.1016/s0272-6386(99)70442-7. [DOI] [PubMed] [Google Scholar]
- 22.de Boer IH, Ioannou GN, Kestenbaum B, et al. 25-Hydroxyvitamin D levels and albuminuria in the Third National Health and Nutrition Examination Survey (NHANES III) Am J Kidney Dis. 2007;50:69–77. doi: 10.1053/j.ajkd.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 23.Agarwal R, Acharya M, Tian J, et al. Antiproteinuric effect of oral paricalcitol in chronic kidney disease. Kidney Int. 2005;68:2823–2828. doi: 10.1111/j.1523-1755.2005.00755.x. [DOI] [PubMed] [Google Scholar]
- 24.Alborzi P, Patel NA, Peterson C, et al. Paricalcitol reduces albuminuria and inflammation in chronic kidney disease: a randomized double-blind pilot trial. Hypertension. 2008;52:249–255. doi: 10.1161/HYPERTENSIONAHA.108.113159. [DOI] [PubMed] [Google Scholar]
- 25.Fishbane S, Chittineni H, Packman M, et al. Oral paricalcitol in the treatment of patients with CKD and proteinuria: a randomized trial. Am J Kidney Dis. 2009;54:647–652. doi: 10.1053/j.ajkd.2009.04.036. [DOI] [PubMed] [Google Scholar]
- 26. de Zeeuw D, Agarwal R, Amdahl M, et al. Selective vitamin D receptor activation with paricalcitol for reduction of albuminuria in patients with type 2 diabetes (VITAL study): a randomised controlled trial. Lancet. 2010;376:1543–1551. doi: 10.1016/S0140-6736(10)61032-X.. ** The first large randomized controlled clinical trial that demonstrates significant therapeutic efficacy of vitamin D analog paricalcitol in the reduction of albuminuria and blood pressure in patients with type 2 diabetes.
- 27.Li YC. Podocytes as target of vitamin D. Current Diabetes Reviews. 2010 doi: 10.2174/157339911794273964. in press. [DOI] [PubMed] [Google Scholar]
- 28.Carey RM, Siragy HM. The intrarenal renin-angiotensin system and diabetic nephropathy. Trends Endocrinol Metab. 2003;14:274–281. doi: 10.1016/s1043-2760(03)00111-5. [DOI] [PubMed] [Google Scholar]
- 29.Li YC, Kong J, Wei M, et al. 1,25-Dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest. 2002;110:229–238. doi: 10.1172/JCI15219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yuan W, Pan W, Kong J, et al. 1,25-Dihydroxyvitamin D3 Suppresses Renin Gene Transcription by Blocking the Activity of the Cyclic AMP Response Element in the Renin Gene Promoter. J Biol Chem. 2007;282:29821–29830. doi: 10.1074/jbc.M705495200. [DOI] [PubMed] [Google Scholar]
- 31.Zhang Z, Sun L, Wang Y, et al. Renoprotective role of the vitamin D receptor in diabetic nephropathy. Kidney Int. 2008;73:163–171. doi: 10.1038/sj.ki.5002572. [DOI] [PubMed] [Google Scholar]
- 32. Zhang Y, Kong J, Deb DK, et al. Vitamin D receptor attenuates renal fibrosis by suppressing the renin-angiotensin system. J Am Soc Nephrol. 2010;21:966–973. doi: 10.1681/ASN.2009080872.. * This study provides good evidence demonstrating that vitamin D-VDR signaling suppresses renal fibrosis by targeting the renin-angiotensin system.
- 33.Freundlich M, Quiroz Y, Zhang Z, et al. Suppression of renin-angiotensin gene expression in the kidney by paricalcitol. Kidney Int. 2008;74:1394–1402. doi: 10.1038/ki.2008.408. [DOI] [PubMed] [Google Scholar]
- 34.Wang XX, Jiang T, Shen Y, et al. Vitamin D receptor agonist doxercalciferol modulates dietary fat-induced renal disease and renal lipid metabolism. Am J Physiol Renal Physiol. 2011;300:F801–F810. doi: 10.1152/ajprenal.00338.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang Z, Zhang Y, Ning G, et al. Combination therapy with AT1 blocker and vitamin D analog markedly ameliorates diabetic nephropathy: blockade of compensatory renin increase. Proc Natl Acad Sci U S A. 2008;105:15896–15901. doi: 10.1073/pnas.0803751105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Deb DK, Sun T, Wong KE, et al. Combined vitamin D analog and AT1 receptor antagonist synergistically block the development of kidney disease in a model of type 2 diabetes. Kidney Int. 2010;77:1000–1009. doi: 10.1038/ki.2010.22. [DOI] [PubMed] [Google Scholar]
- 37.Zhang Y, DK D, Kong J, et al. Long-Term Therapeutic Effect of Vitamin D Analog Doxercalciferol on Diabetic Nephropathy: Strong Synergism with AT1 Receptor Antagonist. American Journal of Physiology Renal Physiology. 2009;297:F791–F801. doi: 10.1152/ajprenal.00247.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ohara I, Tanimoto M, Gohda T, et al. Effect of combination therapy with angiotensin receptor blocker and 1,25-dihydroxyvitamin D(3) in type 2 diabetic nephropathy in KK-A(y)/Ta mice. Nephron Exp Nephrol. 2011;117:e124–e132. doi: 10.1159/000320284. [DOI] [PubMed] [Google Scholar]
- 39.Tan X, He W, Liu Y. Combination therapy with paricalcitol and trandolapril reduces renal fibrosis in obstructive nephropathy. Kidney Int. 2009;76:1248–1257. doi: 10.1038/ki.2009.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mizobuchi M, Morrissey J, Finch JL, et al. Combination therapy with an angiotensin-converting enzyme inhibitor and a vitamin D analog suppresses the progression of renal insufficiency in uremic rats. J Am Soc Nephrol. 2007;18:1796–1806. doi: 10.1681/ASN.2006091028. [DOI] [PubMed] [Google Scholar]
- 41.Li YC. Renoprotective effects of vitamin D analogs. Kidney Int. 2010;78:134–19. doi: 10.1038/ki.2009.175. [DOI] [PubMed] [Google Scholar]
- 42.Guijarro C, Egido J. Transcription factor-kappa B (NF-kappa B) and renal disease. Kidney Int. 2001;59:415–424. doi: 10.1046/j.1523-1755.2001.059002415.x. [DOI] [PubMed] [Google Scholar]
- 43.Sun J, Kong J, Duan Y, et al. Increased NF-{kappa}B activity in fibroblasts lacking the vitamin D receptor. Am J Physiol Endocrinol Metab. 2006;291:E315–E322. doi: 10.1152/ajpendo.00590.2005. [DOI] [PubMed] [Google Scholar]
- 44.Zehnder D, Quinkler M, Eardley KS, et al. Reduction of the vitamin D hormonal system in kidney disease is associated with increased renal inflammation. Kidney Int. 2008;74:1343–1353. doi: 10.1038/ki.2008.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tan X, Wen X, Liu Y. Paricalcitol inhibits renal inflammation by promoting vitamin D receptor-mediated sequestration of NF-kappaB signaling. J Am Soc Nephrol. 2008;19:1741–1752. doi: 10.1681/ASN.2007060666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Park JW, Bae EH, Kim IJ, et al. Paricalcitol attenuates cyclosporine-induced kidney injury in rats. Kidney Int. 2010;77:1076–1085. doi: 10.1038/ki.2010.69. [DOI] [PubMed] [Google Scholar]
- 47.Park JW, Bae EH, Kim IJ, et al. Renoprotective effects of paricalcitol on gentamicin-induced kidney injury in rats. Am J Physiol Renal Physiol. 2010;298:F301–F313. doi: 10.1152/ajprenal.00471.2009. [DOI] [PubMed] [Google Scholar]
- 48.Deb DK, Chen Y, Zhang Z, et al. 1,25-Dihydroxyvitamin D3 suppresses high glucose-induced angiotensinogen expression in kidney cells by blocking the NF-{kappa}B pathway. Am J Physiol Renal Physiol. 2009;296:F1212–F1218. doi: 10.1152/ajprenal.00002.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang Z, Yuan W, Sun L, et al. 1,25-Dihydroxyvitamin D(3) targeting of NF-kappaB suppresses high glucose-induced MCP-1 expression in mesangial cells. Kidney Int. 2007;72:193–201. doi: 10.1038/sj.ki.5002296. [DOI] [PubMed] [Google Scholar]
- 50.Chen Y, Kong J, Sun T, et al. 1,25-Dihydroxyvitamin D(3) suppresses inflammation-induced expression of plasminogen activator inhibitor-1 by blocking nuclear factor-kappaB activation. Arch Biochem Biophys. 2011;507:241–247. doi: 10.1016/j.abb.2010.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li YC. Renoprotective effects of vitamin D analogs. Kidney Int. 2009;78:134–139. doi: 10.1038/ki.2009.175. [DOI] [PubMed] [Google Scholar]
- 52.Dai C, Stolz DB, Kiss LP, et al. Wnt/beta-catenin signaling promotes podocyte dysfunction and albuminuria. J Am Soc Nephrol. 2009;20:1997–2008. doi: 10.1681/ASN.2009010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Palmer HG, Gonzalez-Sancho JM, Espada J, et al. Vitamin D(3) promotes the differentiation of colon carcinoma cells by the induction of E-cadherin and the inhibition of beta-catenin signaling. J Cell Biol. 2001;154:369–387. doi: 10.1083/jcb.200102028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shah S, Islam MN, Dakshanamurthy S, et al. The molecular basis of vitamin D receptor and beta-catenin crossregulation. Mol Cell. 2006;21:799–809. doi: 10.1016/j.molcel.2006.01.037. [DOI] [PubMed] [Google Scholar]
- 55. He W, Kang YS, Dai C, Liu Y. Blockade of Wnt/beta-catenin signaling by paricalcitol ameliorates proteinuria and kidney injury. J Am Soc Nephrol. 2011;22:90–103. doi: 10.1681/ASN.2009121236.. * A well-described study that shows vitamin D analog paricalcitol targets the Wnt/β-catenin signaling pathway in podocytes in preventing proteinuria.
- 56.Ruotsalainen V, Ljungberg P, Wartiovaara J, et al. Nephrin is specifically located at the slit diaphragm of glomerular podocytes. Proc Natl Acad Sci U S A. 1999;96:7962–7967. doi: 10.1073/pnas.96.14.7962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Takano Y, Yamauchi K, Hiramatsu N, et al. Recovery and maintenance of nephrin expression in cultured podocytes and identification of HGF as a repressor of nephrin. Am J Physiol Renal Physiol. 2007;292:F1573–F1582. doi: 10.1152/ajprenal.00423.2006. [DOI] [PubMed] [Google Scholar]
- 58. Deb DK, Wang Y, Zhang Z, et al. Molecular mechanism underlying 1,25-dihydroxyvitamin D regulation of nephrin gene expression. J Biol Chem. 2011 doi: 10.1074/jbc.M111.269118.. ** A mechanistic study that demonstrates how 1,25-dihydroxyvitamin D up-regulates nephrin gene transcription. This evidence suggests that vitamin D prevents proteinuria by maintaining the integrity of the slit diaphragm.
- 59.Scragg R, Sowers M, Bell C. Serum 25-hydroxyvitamin D, ethnicity, and blood pressure in the Third National Health and Nutrition Examination Survey. Am J Hypertens. 2007;20:713–719. doi: 10.1016/j.amjhyper.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 60.Kim DH, Sabour S, Sagar UN, et al. Prevalence of hypovitaminosis D in cardiovascular diseases (from the National Health and Nutrition Examination Survey 2001 to 2004) Am J Cardiol. 2008;102:1540–1544. doi: 10.1016/j.amjcard.2008.06.067. [DOI] [PubMed] [Google Scholar]
- 61.Kendrick J, Targher G, Smits G, Chonchol M. 25-Hydroxyvitamin D deficiency is independently associated with cardiovascular disease in the Third National Health and Nutrition Examination Survey. Atherosclerosis. 2009;205:255–260. doi: 10.1016/j.atherosclerosis.2008.10.033. [DOI] [PubMed] [Google Scholar]
- 62.Martins D, Wolf M, Pan D, et al. Prevalence of cardiovascular risk factors and the serum levels of 25-hydroxyvitamin D in the United States: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2007;167:1159–1165. doi: 10.1001/archinte.167.11.1159. [DOI] [PubMed] [Google Scholar]
- 63.Forman JP, Giovannucci E, Holmes MD, et al. Plasma 25-hydroxyvitamin D levels and risk of incident hypertension. Hypertension. 2007;49:1063–1069. doi: 10.1161/HYPERTENSIONAHA.107.087288. [DOI] [PubMed] [Google Scholar]
- 64.Giovannucci E, Liu Y, Hollis BW, Rimm EB. 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Arch Intern Med. 2008;168:1174–1180. doi: 10.1001/archinte.168.11.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang TJ, Pencina MJ, Booth SL, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117:503–511. doi: 10.1161/CIRCULATIONAHA.107.706127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schmitz KJ, Skinner HG, Bautista LE, et al. Association of 25-hydroxyvitamin D with blood pressure in predominantly 25-hydroxyvitamin D deficient Hispanic and African Americans. Am J Hypertens. 2009;22:867–870. doi: 10.1038/ajh.2009.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lai H, Fishman EK, Gerstainblith G, et al. Vitamin D deficiency is associated with significant coronary stenoses in asymptomatic African American chronic cocain users. Int. J. Cardiol. 2011 doi: 10.1016/j.ijcard.2011.01.032. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Reis JP, von Muhlen D, Michos ED, et al. Serum vitamin D, parathyroid hormone levels, and carotid atherosclerosis. Atherosclerosis. 2009;207:585–590. doi: 10.1016/j.atherosclerosis.2009.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.de Boer IH, Kestenbaum B, Shoben AB, et al. 25-hydroxyvitamin D levels inversely associate with risk for developing coronary artery calcification. J Am Soc Nephrol. 2009;20:1805–1812. doi: 10.1681/ASN.2008111157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sun Q, Shi L, Rimm EB, et al. Vitamin D intake and risk of cardiovascular disease in US men and women. Am J Clin Nutr. 2011;94:534–542. doi: 10.3945/ajcn.110.008763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Wang L, Manson JE, Song Y, Sesso HD. Systematic review: Vitamin D and calcium supplementation in prevention of cardiovascular events. Ann Intern Med. 2010;152:315–323. doi: 10.7326/0003-4819-152-5-201003020-00010.. * This meta-analysis of 17 studies suggests that vitamin D supplements at moderate to high doses, but no calcium supplements, reduce the risk of cardiovascular disease.
- 72. Anderson JL, May HT, Horne BD, et al. Relation of vitamin D deficiency to cardiovascular risk factors, disease status, and incident events in a general healthcare population. Am J Cardiol. 2010;106:963–968. doi: 10.1016/j.amjcard.2010.05.027.. * This is an epidemiological study with a large sample size that confirms a high prevalence of vitamin D deficiency in the general healthcare population and an association between vitamin D levels and prevalent and incident cardiovascular risk factors and outcomes.
- 73.Pilz S, Marz W, Wellnitz B, et al. Association of vitamin D deficiency with heart failure and sudden cardiac death in a large cross-sectional study of patients referred for coronary angiography. J Clin Endocrinol Metab. 2008;93:3927–3935. doi: 10.1210/jc.2008-0784. [DOI] [PubMed] [Google Scholar]
- 74.Wang AY, Lam CW, Sanderson JE, et al. Serum 25-hydroxyvitamin D status and cardiovascular outcomes in chronic peritoneal dialysis patients: a 3-y prospective cohort study. Am J Clin Nutr. 2008;87:1631–1638. doi: 10.1093/ajcn/87.6.1631. [DOI] [PubMed] [Google Scholar]
- 75. Burgaz A, Orsini N, Larsson SC, Wolk A. Blood 25-hydroxyvitamin D concentration and hypertension: a meta-analysis. J Hypertens. 2010 doi: 10.1097/HJH.0b013e32834320f9.. * A meta-analysis of 18 studies that confirms the association of low vitamin D status with hypertension in humans.
- 76.Bodyak N, Ayus JC, Achinger S, et al. Activated vitamin D attenuates left ventricular abnormalities induced by dietary sodium in Dahl salt-sensitive animals. Proc Natl Acad Sci U S A. 2007;104:16810–16815. doi: 10.1073/pnas.0611202104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Kong J, Kim GH, Wei M, et al. Therapeutic effects of vitamin D analogs on cardiac hypertrophy in spontaneously hypertensive rats. Am J Pathol. 2010;177:622–631. doi: 10.2353/ajpath.2010.091292.. ** This is a first study that demonstrates enhanced therapeutic efficacy with combination therapy of vitamin D analog and RAS inhibitor in the inhibition of cardiac hypertrophy. The data confirm previous finding that blockade of the compensatory renin induction improves therapeutic efficacy.
- 78.Bae S, Yalamarti B, Ke Q, et al. Preventing progression of cardiac hypertrophy and development of heart failure by paricalcitol therapy in rats. Cardiovasc Res. 2011 doi: 10.1093/cvr/cvr133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chen S, Glenn DJ, Ni W, et al. Expression of the vitamin d receptor is increased in the hypertrophic heart. Hypertension. 2008;52:1106–1112. doi: 10.1161/HYPERTENSIONAHA.108.119602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang Y, DeLuca HF. Is the vitamin d receptor found in muscle? Endocrinology. 2011;152:354–363. doi: 10.1210/en.2010-1109. [DOI] [PubMed] [Google Scholar]
- 81.Testa A, Mallamaci F, Benedetto FA, et al. Vitamin D receptor (VDR) gene polymorphism is associated with left ventricular (LV) mass and predicts left ventricular hypertrophy (LVH) progression in end-stage renal disease (ESRD) patients. J Bone Miner Res. 2010;25:313–319. doi: 10.1359/jbmr.090717. [DOI] [PubMed] [Google Scholar]
- 82.Becker LE, Koleganova N, Piecha G, et al. Effect of paricalcitol and calcitriol on aortic wall remodeling in uninephrectomized ApoE knockout mice. Am J Physiol Renal Physiol. 2011;300:F772–F782. doi: 10.1152/ajprenal.00042.2010. [DOI] [PubMed] [Google Scholar]
- 83. Oh J, Weng S, Felton SK, et al. 1,25(OH)2 vitamin d inhibits foam cell formation and suppresses macrophage cholesterol uptake in patients with type 2 diabetes mellitus. Circulation. 2009;120:687–698. doi: 10.1161/CIRCULATIONAHA.109.856070.. * First study that reports inhibitory effect of 1,25-dihydroxyvitamin D on cholesterol influx and foam cell formation in type 2 diabetes patients.
- 84. Takeda M, Yamashita T, Sasaki N, et al. Oral administration of an active form of vitamin D3 (calcitriol) decreases atherosclerosis in mice by inducing regulatory T cells and immature dendritic cells with tolerogenic functions. Arterioscler Thromb Vasc Biol. 2010;30:2495–2503. doi: 10.1161/ATVBAHA.110.215459.. ** This paper reports anti-atherosclerotic effects of 1,25-dihydroxyvitamin D in a widely used mouse model of atherosclerosis.
- 85.Zhou C, Lu F, Cao K, et al. Calcium-independent and 1,25(OH)2D3-dependent regulation of the renin-angiotensin system in 1alpha-hydroxylase knockout mice. Kidney Int. 2008;74:170–179. doi: 10.1038/ki.2008.101. [DOI] [PubMed] [Google Scholar]
- 86.Kong J, Qiao G, Zhang Z, et al. Targeted vitamin D receptor expression in juxtaglomerular cells suppresses renin expression independent of parathyroid hormone and calcium. Kidney Int. 2008;74:1577–1581. doi: 10.1038/ki.2008.452. [DOI] [PubMed] [Google Scholar]
- 87.Forman JP, Williams JS, Fisher ND. Plasma 25-hydroxyvitamin D and regulation of the renin-angiotensin system in humans. Hypertension. 2010;55:1283–1288. doi: 10.1161/HYPERTENSIONAHA.109.148619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Tomaschitz A, Pilz S, Ritz E, et al. Independent association between 1,25-dihydroxyvitamin D, 25-hydroxyvitamin D and the renin-angiotensin system: The Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Clin Chim Acta. 2010;411:1354–1360. doi: 10.1016/j.cca.2010.05.037.. ** This is the first large epidemiological study that demonstrates an inverse correlation between the vitamin D status and the status of the renin-angiotensin system in a large cohort of human subjects. These findings support the data from animal studies that establish the vitamin D hormone as a negative regulator of the renin-angiotensin system.
- 89.Thadhani R, Appelbaum E, Chang Y, et al. Vitamin D receptor activation and left ventricular hypertrophy in advanced kidney disease. Am J Nephrol. 2011;33:139–149. doi: 10.1159/000323551. [DOI] [PubMed] [Google Scholar]