Abstract
Background
Older adults are commonly accompanied to routine medical visits. Whether and how family companion behaviours relate to visit processes is poorly understood.
Objective
To examine family companion behaviours in relation to older adults' medical visit processes.
Design and participants
Observational study of 78 accompanied primary care patients ages 65 and older.
Main outcome measures
Medical visit communication (coded using RIAS), patient verbal activity (as a proportion of visit statements) and visit duration (in min), from audio recordings.
Results
Companions' facilitation of patient involvement was associated with greater patient question asking (P = 0.017) and orienting statements, less passive agreement (P = 0.004) and social talk (P = 0.013) and visits that were 3.4 min longer (P = 0.025). Facilitation of patient understanding was associated with less physician question asking (P = 0.004), visits that were 3.0 min longer (P = 0.031), and lower patient verbal activity (30.3% vs. 36.9% of visit statements; P = 0.028). Facilitation of doctor understanding was associated with greater patient biomedical information giving (P = 0.049). Autonomy detracting behaviours were not associated with visit duration but were associated with lower levels of patient verbal activity (36.3% vs. 29.1% of visit statements; P = 0.041). When companions assumed more behaviours, medical visits were incrementally longer (16.1, 19.5, 21.7 min, corresponding to 0–1, 2–4 and 5+ behaviours; P < 0.001 both contrasts), and patients were less verbally active (35.6%, 33.9%, 27.1% of visit statements; P = 0.09 and P = 0.009, respectively).
Discussion
Behaviours assumed by patients' companions were associated with visit communication, patient verbal activity and visit duration.
Conclusions
Interventions to capitalize on family companions' presence may benefit medical visit processes.
Keywords: doctor–patient–companion communication, patient–provider communication, RIAS, triadic communication
Introduction
Patient engagement in care, reflected by active communication with clinicians and participation in treatment decisions regarding care is central to high‐quality chronic care.1, 2 Advancing patient engagement has emerged as a prominent feature of national policy efforts such as the National Quality Strategy, the Patient Centered Medical Home and the Patient Centered Outcomes Research Institute.3, 4 Developing strategies and the infrastructure to support patient engagement requires awareness that these processes are less straightforward for vulnerable patients such as those who are older, less literate, mentally or cognitively impaired, who have sensory or functional deficits, or who must manage complex treatment regimens.5, 6 Such patients often rely on assistance from family or friends in accessing routine care,7 communicating with their health‐care providers,8 obtaining and processing health information in making treatment decisions9, 10, 11 and adhering to treatment regimens.12
Although family involvement is an articulated dimension of patient‐centred care,13 the connection between family behaviours and patient engagement in medical visit processes is poorly understood.8, 10 Evidence thus far indicates that the more active family members are in physician visits, the more highly satisfied patients are with their usual care provider14, 15 and that patients also participate more actively in decision making.16 What remains unclear is whether or how specific companion behaviours are helpful in engaging patients' participation in medical communication.
This study examines patient engagement in medical dialogue when in the presence of a family companion by drawing from an observational data set of accompanied older adults' primary care physician visits. In a prior analysis of these visits, Clayman et al. used an autonomy framework to describe the kinds of behaviours family companions perform.16 Most behaviours involved enhancement of patient autonomy by facilitating patient involvement in the visit and helping the doctor and patient understand one another. While companions sometimes behaved in ways that detracted from patient autonomy by controlling the patient or attempting to achieve goals of their own, these behaviours occurred less often and never in the absence of the more positive behaviours. Clayman found that when companions facilitated patient involvement, patients were 4½ times more likely to participate actively in medical decision making.
The current analysis extends that work by relating companion behaviours to patient, companion, and physician contribution to medical visit communication, patient engagement in medical visit dialogue and medical visit duration. Of particular interest to this study is whether medical visit duration and patient verbal activity in visit dialogue differs by the nature and type of behaviours the family companions perform.
Methods
Study design and data collection
This study relies on a convenience sample of audio‐taped primary care physician visits collected between August 1998 and July 2000. Physician practice sites included a medical group affiliated with an academic medical centre in New Mexico, a private group practice in a Midwest suburb and an inner city private group practice in the Midwest. Patients of 37 participating physicians and their companions were approached in the waiting room prior to their visit. The scope of the study was explained to patients and family companions (if present), and their interest and eligibility was ascertained. Eligible patients were 65 years or older and identified a participating physician as their usual source of care. Subsequent to consent, patients and companions were administered a short survey prior to the physician visit. Medical visit interactions were video‐recorded. Immediately after the physician visit, a brief survey was again administered to patients. Details describing baseline characteristics of the overall study sample17 and the subset of study participants who were accompanied to their visit by a companion16 have been published.
As described elsewhere, interaction analysis of visit recordings and completed baseline surveys were available for 390 patients, 80 of whom were accompanied to their physician visit by a family companion.18 These data sources were combined with previously described coded information regarding companions' behaviours based on examination of video recordings of these visits.16 Two of the 80 accompanied patients' visits were excluded because video recordings of the visit were not available and behaviours of family companions were not coded. Our final study sample thus comprised 78 distinct patient/family companion dyads with both survey and linked medical visits.
Companion behaviours
Thirteen categories of companion behaviours were defined and coded from videotaped observation of physician visits, as reported elsewhere.16 Companion behaviours were broadly categorized in relation to patient autonomy. Three categories of autonomy enhancing behaviours were identified: (i) facilitating doctor understanding (clarifying or expanding patient history, or introducing medical topics), (ii) facilitating patient understanding (repeating the doctor's explanations or asking the doctor questions) and (iii) facilitating patient involvement (prompting the patient to discuss topics, asking the patient questions or asking the patient to express their opinion). Autonomy detracting behaviours were also identified and these include controlling actions towards the patient (answering for the patient, interrupting the patient repeatedly, discussing their own health or engaging in behaviours such as belittling the patient) as well as alliance building with the doctor (trying to persuade the patient to agree to something the doctor would like or gaining physician agreement for something the companion would like).
In addition to these individual categories of companion behaviours, a summary indicator was constructed to reflect the total number of the 13 specific behaviours assumed by each companion (0 or 1 behaviour; 2–4 behaviours; 5 or more behaviours). Each behaviour within a given category was counted only once.
Interaction analysis
Recordings of medical visit dialogue were coded using the Roter Interaction Analysis System (RIAS), a widely used and well‐validated system for empirically describing medical visit communication.19 The RIAS quantifies aspects of medical visit dialogue by assigning each complete thought to one of thirty‐eight mutually exclusive communication categories. We examined categories of communication as follows: question asking, biomedical information giving, psychosocial information giving, emotional expression, partnership building, positive talk, social talk, negative talk and orientation. For patients and companions, passive agreement (‘hmmm’, ‘ok’, ‘right’) was distinguished from positive talk; for physicians, the parallel category is backchannels, which were included in partnership building. Coding was applied to all dialogue contributed by the patient, physician or companion.
Survey measures
Patient characteristics, including age, gender, race and education were ascertained from a brief survey that was administered just prior to the medical encounter. Health status was measured with the Physical Component Summary (PCS) and Mental Component Summary (MCS) of the Short‐Form 36‐item Health Survey (SF‐36), which was administered to respondents in‐person immediately after the medical encounter.20 Due to sample considerations, physical and mental health function were examined using the median sample value as a cut‐point for stratification (MCS = 53 and PCS = 35). Companion characteristics (age, gender, relationship) were reported by survey immediately prior to the medical encounter.
Analytic approach
Analyses were performed in sas 9.1 (SAS Institute, Cary, NC, USA) with each medical encounter as the unit of analysis. Categories of companion behaviours were examined in relation to patient and companion attributes, communication as measured using RIAS categories, and visit processes. Two visit process measures were examined: (i) visit duration, in min and (ii) patient engagement in medical dialogue, defined as the proportion of patient statements contributed during the visit relative to statements contributed by the companion or physician. Generalized estimating equations (GEE) in conjunction with simple linear or logistic regression were used to assess the statistical significance of these relationships. GEE accounts for within‐physician clustering of patients and is able to accommodate unbalanced numbers of patients per physician.21 An exchangeable correlation structure was assumed in our analyses.
We employed a two stage‐process to describe the statistical significance of the association between family companion behaviours with patient and family companion characteristics, physician visit communication and visit processes. Given the small sample size and large number of comparisons to be investigated, descriptive analyses were initially limited to bivariate relationships. Because companion age and gender were correlated with relationship to patient,16 statistically significant effects from bivariate models (at P < 0.10) were adjusted to account for companion relationship (spouse vs. non‐spouse) to ascertain whether the strength of observed associations were at least partially accounted for by the type of patient–companion relationship. The study was approved by the Johns Hopkins University Bloomberg School of Public Health Institutional Review Board.
Results
Types of behaviours: patient and companion attributes
The 78 older adults comprising our study sample were on average 77.6 years of age and predominantly women (71.8%), white (82.1%) and high school graduates (60.3%; Table 1). Patient attributes were not highly related to companions' behaviours. Companions were more likely to assume autonomy detracting behaviours when accompanying male vs. female patients (59.1% vs. 37.5%) and patients in better, vs. worse physical health (50.0% vs. 38.1%). No other patient attributes were statistically significant in regard to companion behaviours.
Table 1.
Patient and family companion characteristics by family companion behaviours during medical visits
| Patient characteristics | Total sample | Autonomy enhancing – companion facilitates | |||
|---|---|---|---|---|---|
| Doctor understanding | Patient understanding | Patient involvement | Autonomy detracting | ||
| Sample, number (%) | 78 (100.0%) | 65 (83.3%) | 44 (56.4%) | 31 (39.7%) | 34 (43.6%) |
| Mean age (years) | 77.6 | 77.4 | 78.9 | 77.8 | 79.0 |
| Gender | |||||
| Female | 56 (71.8%) | 47 (83.9%) | 32 (57.1%) | 25 (44.6%) | 21 (37.5%) a |
| Male | 22 (28.2%) | 18 (81.8%) | 12 (54.6%) | 6 (27.3%) | 13 (59.1%) a |
| Race | |||||
| White | 64 (82.1%) | 55 (85.9%) | 36 (56.3%) | 27 (42.2%) | 27 (42.2%) |
| Other | 14 (17.9%) | 10 (71.4%) | 8 (57.1%) | 4 (28.6%) | 7 (50.0%) |
| Education | |||||
| <High school | 31 (39.7%) | 26 (83.9%) | 17 (54.8%) | 11 (35.5%) | 13 (41.9%) |
| High school or more | 47 (60.3%) | 39 (83.0%) | 27 (57.5%) | 20 (42.6%) | 21 (44.7%) |
| Mental health function | |||||
| MCS < 53 | 41 (52.6%) | 34 (82.9%) | 23 (56.1%) | 20 (48.8%) | 21 (51.2%) |
| MCS 53+ | 37 (47.4%) | 31 (83.8%) | 21 (56.8%) | 11 (29.7%) | 13 (35.1%) |
| Physical health function | |||||
| PCS < 35 | 42 (53.9%) | 37 (88.1%) | 25 (59.5%) | 18 (42.9%) | 16 (38.1%) a |
| PCS 35+ | 36 (46.2%) | 28 (77.8%) | 19 (52.8%) | 13 (36.1%) | 18 (50.0%) a |
P < 0.05 in regression models that accounted for companion relationship to patient as well as physician clustering.
Autonomy detracting refers to alliance‐building and controlling behaviours towards the patient Short‐Form 36‐Item General Health Survey – MCS, Mental Component Summary Score; PCS, Physical Component Summary Score.
Family companions were on average 59.9 years of age and were predominantly women (61.5%), and spouses (43.6%), or adult children (35.9%); fewer companions were described by ‘other' relationships (17.9%) and they were primarily relatives. Companions who engaged in autonomy enhancing behaviours by facilitating doctor understanding and patient understanding were younger than their counterparts who did not. Female companions more commonly assumed autonomy detracting behaviours than their male counterparts (54.2% vs. 26.7%). Relative to spouses, adult children more commonly facilitated patient understanding (75.0% vs. 44.1%) and involvement (50.0% vs. 26.5%). ‘Other’ companions were more similar in age and behaviours to adult child than spouse companions.
Type of companion behaviours and medical visit communication
We examined patient, companion and doctor communication in relation to the four broad categories of companion behaviours, as displayed in Table 2. Companion facilitation of doctor understanding (by giving the doctor information about the patient's medical history or symptoms (e.g. ‘she fell last week and bruised her arm’)) was significantly associated with both the patient and companion giving the doctor more medical information and the companion expressing more emotion (e.g. ‘I worry about that all the time’) and being less positive in their communication (including jokes and laughter, compliments and approving statements) Companions’ facilitation of patient understanding (by repeating the doctors explanations in simpler terms or by asking the doctor clarifying questions) was not related to any differences in patient communication but was associated with more companion questions, emotional expression and less positive talk. Companions’ facilitation of patient understanding was also associated with fewer questions by the doctor.
Table 2.
Patient, companion, and doctor contribution to communication in relation to categories of family companion behaviours during medical visits
| Autonomy enhancing | Autonomy detracting | |||||||
|---|---|---|---|---|---|---|---|---|
| Facilitate doctor understanding | Facilitate patient understanding | Facilitate patient involvement | Controlling and alliance building | |||||
| n = 65 (83.3%) | n = 44 (56.4%) | n = 31 (39.7%) | n = 34 (43.6%) | |||||
| Patient contribution | Yes | No | Yes | No | Yes | No | Yes | No |
| Question asking | 3.4% | 2.5% | 3.6% | 2.8% | 4.3% a | 2.6% a | 3.1% | 3.4% |
| Biomedical information giving | 43.7% a | 35.3% a | 40.6% | 44.5% | 42.1% | 42.4% | 42.8% | 41.9% |
| Psychosocial information giving | 9.5% | 12.5% | 10.8% | 9.0% | 11.1% | 9.3% | 9.7% | 10.2% |
| Emotional expression | 7.5% | 6.6% | 8.0% | 6.4% | 7.9% | 7.0% | 6.8% | 7.7% |
| Partnership building | 2.4% | 1.4% | 2.3% | 2.2% | 2.6% | 2.0% | 1.9% | 2.6% |
| Passive agreement | 18.4% | 24.4% | 19.1% | 19.7% | 16.2% a | 21.5% a | 18.1% | 20.3% |
| Positive talk | 7.3% | 7.9% | 7.3% | 7.5% | 7.4% | 7.4% | 8.4% | 6.6% |
| Social talk | 2.5% | 5.4% | 2.7% | 3.3% | 1.7% a | 3.8% a | 2.2% | 3.6% |
| Negative talk | 0.6% | 0.7% | 0.6% | 0.7% | 0.4% | 0.8% | 0.7% | 0.5% |
| Orientation | 4.7% | 3.2% | 4.7% | 4.2% | 6.3% a | 3.2% a | 6.2% a | 3.2% a |
| Companion contribution | Yes | No | Yes | No | Yes | No | Yes | No |
| Question asking | 5.5% | 5.6% | 7.6% a | 2.7% a | 5.0% | 5.8% | 6.9% | 4.4% |
| Biomedical information giving | 33.4% a | 15.6% a | 31.0% | 29.8% | 30.8% | 30.2% | 31.7% | 29.5% |
| Psychosocial information giving | 15.6% | 19.7% | 16.9% | 15.4% | 17.1% | 15.7% | 17.3% | 15.5% |
| Emotional expression | 6.7% a | 3.5% a | 7.1% a | 5.0% a | 6.7% | 5.9% | 6.3% | 6.1% |
| Partnership building | 2.2% | 2.8% | 2.5% | 1.9% | 2.6% | 2.0% | 2.4% | 2.1% |
| Passive agreement | 13.8% | 9.5% | 14.4% | 11.5% | 13.0% | 13.1% | 15.4% | 11.4% |
| Positive talk | 15.2% a | 32.3% a | 13.7% a | 23.7% a | 16.5% | 19.0% | 13.1% a | 21.9% a |
| Social talk | 4.0% | 7.2% | 3.3% | 6.2% | 3.7% | 5.1% | 2.6% | 6.1% a |
| Negative talk | 0.6% | 0.7% | 0.5% | 0.8% | 0.4% | 0.7% | 0.5% | 0.7% |
| Orientation | 3.0% | 7.3% | 3.0% | 3.1% | 4.1% a | 2.4% a | 3.8% a | 2.5% a |
| Doctor contribution | ||||||||
| Question asking | 11.0% | 11.0% | 9.9% a | 12.1% a | 11.2% | 10.7% | 10.6% | 11.0% |
| Biomedical Information giving | 33.6% | 31.0% | 33.8% | 32.3% | 33.3% | 33.0% | 34.4% | 32.1% |
| Psychosocial information giving | 3.3% | 4.9% | 3.6% | 3.5% | 4.1% | 3.2% | 4.4% a | 2.9% a |
| Emotional expression | 8.8% | 8.8% | 8.9% | 8.8% | 8.6% | 9.0% | 8.6% | 9.0% |
| Partnership building | 9.2% | 9.7% | 9.3% | 9.1% | 8.9% | 9.5% | 8.8% | 9.5% |
| Positive talk | 19.9% | 19.7% | 20.6% | 19.0% | 19.5% | 20.2% | 19.3% | 20.4% |
| Social talk | 2.5% | 3.3% | 2.3% | 3.0% | 1.8% a | 3.2% a | 2.2% | 3.0% |
| Negative talk | 0.3% | 0.2% | 0.3% | 0.4% | 0.3% | 0.3% | 0.4% | 0.3% |
| Orientation | 11.4% | 12.4% | 11.3% | 11.8% | 12.4% | 10.9% | 11.3% | 11.7% |
P < 0.05 in regression models that accounted for companion relationship to patient and physician clustering.
Values represent proportion of visit statements contributed by patients (upper panel) and doctors (lower panel).
Companion facilitation of patient involvement (by asking the patient for his/her opinion, prompting the patient to ask questions or discuss concerns) was associated with greater patient question asking, less passive agreement with physician information (statements like ok, hmmm, right) and less social talk (‘I watched the Orioles game last night’) and more orienting statements by both patient and companion (e.g. ‘Doctor, I want to be sure we have enough time to go over what the specialist told me’; ‘I want to ask you a few questions before I leave’). Doctors engaged in less social talk when companions facilitated patient involvement.
Companion use of autonomy detracting behaviours was associated with more patient and companion orienting statements and less positive and social talk by companions. Physicians provided less psychosocial information (e.g. ‘getting out socially can help your mood a lot and keep you connected to things and people you enjoy’) when companions used these type of behaviours.
Type of companion behaviours and medical visit processes
As displayed in Table 3, companion facilitation of patient understanding and patient involvement was associated with significantly longer medical visits (by 3.0 and 3.4 min, respectively). When companions facilitated patient understanding, patients were significantly less verbally active in medical dialogue. Autonomy detracting behaviours were associated with less patient contribution to visit dialogue but were not associated with visit duration.
Table 3.
Types of companions' behaviours in regard to visit duration and patient verbal activity primary care physician visits among accompanied older adults ages 65 and older
| Visit duration (min) | Patient verbal activity (%) | |||||
|---|---|---|---|---|---|---|
| Specific behaviours | No | Yes | B | No | Yes | B |
| Autonomy enhancing | ||||||
| Facilitate doctor understanding | 17.86 | 19.38 | 2.52 | 34.37 | 32.96 | −2.19 |
| Facilitate patient understanding | 17.68 a | 20.24 a | 3.00 a | 36.91 a | 30.32 a | −6.45 a |
| Facilitate patient involvement | 17.43 a | 21.70 a | 3.42 a | 33.16 | 33.25 | −0.30 |
| Autonomy detracting | 18.75 | 19.61 | 1.33 | 36.33 a | 29.14 a | −6.99 a |
P < 0.05 in regression models that accounted for companion relationship to patient and physician clustering.
Patient verbal activity reflects the percentage of total visit statements contributed by the patient, as opposed to the doctor or patients' companion.
Number of companion behaviours and medical visit processes
The greater the number of companion behaviours performed, the longer the visits were and the less verbally active patients were in the visit dialogue. Medical visits were on average 16.1 min in visits during which the companion performed none or just one behaviour, 19.5 min in visits when companions performed 2–4 behaviours (P < 0.001) and 21.7 min in visits during which companions performed more than 5 of the 13 defined behaviours (P < 0.001, in regression models that accounted for companion relationship to patient and physician clustering). When family companions assumed greater numbers of behaviours, patients' contribution to visit dialogue was incrementally diminished. Patients contributed 35.6% of visit statements when companions assumed none or one behaviour, 33.9% of visit statements when companions assumed two to four behaviours (P = 0.100) and 27.1% of visit statements when companions assumed five or more behaviours (P = 0.009). Family companions' activity in the medical visit generally complemented patient contribution to dialogue. When companions assumed greater numbers of behaviours during medical visits, patients contributed less and companions contributed more to visit dialogue (Fig. 1).
Figure 1.
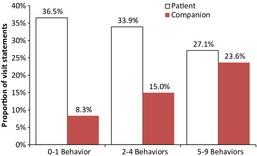
Contribution to visit dialogue by numbers of behaviours assumed by patients' family companion companion behaviours included: clarifying or expanding patient history, introducing medical topics, repeating the doctor's explanations, asking the doctor questions, prompting the patient to discuss topics, asking the patient questions, asking the patient to express their opinion, answering for the patient, interrupting the patient repeatedly, discussing their own health, belittling the patient, trying to persuade the patient to agree to something the doctor would like and gaining physician agreement for something the companion would like.
Discussion
Our findings linking companion behaviours with visit communication are noteworthy in the light of recent policy efforts, which advocate ‘patient engagement’ as an indicator of high‐quality care.1, 2 We found that companion facilitation of patient involvement was associated with more task‐focused exchange, especially by the patient; patients asked more questions and engaged in less social chit‐chat and were less likely to passively accept physician information. Patients and companions also made more orienting statements indicating that they both were more pro‐active in directing the course of the visit by introducing new topics or agenda items. Doctors were similarly more task‐focused in these instances evidenced by limited social talk on their part. As a consequence, these visits were somewhat longer, but we would argue also more patient‐engaged and productive.
Other companion behaviours also affected communication in various ways. Facilitation of doctor understanding was associated with both the patient and companion providing the doctor more information about the patient's medical problem and the companion expressing more emotion and less passive and light‐hearted exchange with the physician. These behaviours did not have an impact on visit length or patient engagement in the dialogue. Interestingly, the companion's facilitation of patient understanding was not associated with any specific patient behaviours but was related to less patient contribution to the visit dialogue and more companion task‐focused exchange, including more questions, expressions of emotion and less positive talk. It appears that in this instance, the companion did the ‘communication work’ for the patient; the patient contribution to the medical dialogue diminished in proportion to the increase in companion verbal activity. In some respects, it appears that the companion also did some of the ‘communication work’ for the physician as well, as evidenced by fewer physician questions.
Autonomy detracting behaviours were related to more patient and companion orienting statements, less positive and social talk on the part of the companion, and more psychosocial information giving on the part of the doctor. These type of behaviours were unrelated to visit duration but were associated with less patient activity in the visit dialogue. Autonomy detracting behaviours were more commonly assumed by companions of patients who were men and in better physical health. We cannot comment on the reasons such behaviours were assumed, although the range of potential reasons spans the nature of their relationship interpersonal conflict, companion concerns regarding the adequacy of disclosure or discussion of patient – or companion – health issues, as well as deferential attitudes towards the medical enterprise or concern that relevant information be imparted in the allotted visit time.
That few patient characteristics were associated with the behaviours assumed by their companion during medical visits merits comment. Specifically, family companions who were younger, women and adult children (vs. spouses) were more likely to engage in both autonomy enhancing and autonomy detracting behaviours than their counterparts. These results are consistent with reports suggesting that working age adults are more consumerist in communicating with health professionals relative to older adults22 and indicate that this relationship holds true when in the role of patient as well as when accompanying a parent to a medical visit.
The fact that visit duration was associated with both the number and type of companion behaviours is of practical relevance to physician practices and policy‐makers. Visit duration is indicative of resource use (from the physician perspective) and the opportunity for information exchange (from the patient and family companion perspective). It is therefore particularly noteworthy that although visits were incrementally longer when companions performed more behaviours, the strength of the relationship was more pronounced for autonomy enhancing behaviours with potential benefits of prompting patient involvement and facilitating patient and doctor understanding. Prior work indicates that family companions' behaviours are associated with patient engagement in medical decision making16 and satisfaction with care,14, 15 but this is the first analysis to demonstrate a relationship between specific companion behaviours and visit duration.
That patient verbal activity was more limited when companions assumed greater numbers of behaviours suggests that patients and companions' participation in physician visit communication complement one other. Person‐ and family‐centred care, including involvement in decisions about health care, joint development of treatment goals and longitudinal plans of care, and the patient and family experience have emerged as core concepts to be promulgated through national and international quality efforts.4, 23 We believe that operationalization of these concepts will further our understanding of how patients and families negotiate, perceive and prefer the roles they assume in health‐care delivery processes.
As in any study, our findings are subject to limitations. Most notably, this is a correlational study of a relatively small convenience sample. Therefore, we cannot draw any conclusions regarding causal pathways. Although study data were collected in three different clinical sites and included a relatively large number of physicians, we cannot determine the extent to which observed family companion behaviours are broadly representative of those employed by companions of older primary care patients. Nevertheless, an analysis of questions related to patient's report of companion roles in visits15 confirm that the kinds of companion behaviours described in this study are similarly recognized by some 39% of Medicare beneficiaries.
We were unable to construct multivariate regression models to comprehensively account for correlation between patient characteristics and family behaviours that may have been influential to visit processes because of small sample. Our analyses did not ascertain what precipitated companion behaviours and whether they were self‐initiated or motivated by patient or physician statements. The study is based on a cross‐sectional sample of medical visits that were limited to a single physician visit, as are almost all medical communication studies, and no conclusions can be drawn about how companion behaviours may change over time.
Despite these limitations, our findings raise important issues with regard to the patient–family–physician relationship for research, practice and policy. From a research standpoint, this study suggests that broader quality of care measures that encompass measures of both patient and family engagement in communication and care processes may be useful and could potentially contribute to the notion that effective ‘self‐management' might well involve members of patients broader social network. Furthermore, a health system or policy perspective that values treatment adherence as a primary goal might look to how the involvement of family members in older patient visits may improve patient's ability to follow therapeutic recommendations and improve patient outcomes.
Although patient preferences for companion involvement may vary by socio‐demographic characteristics or the nature of interpersonal relationships, preferences may also vary by the types and severity of their conditions. It is plausible, for instance, that patients may welcome family involvement in some aspects of care, while preferring privacy in communicating with health‐care professionals about potentially stigmatizing conditions (e.g. incontinence, sexual dysfunction, mental illness or memory impairment). The role of family for patients with cognitive impairment or severe mental health issues is likely to differ from that of older adults with physical deficits and chronic medical conditions such as diabetes.24
The construct of ‘shared decision making' has been recently advocated as requiring expansion to reflect its ‘inter‐professional' nature, with family involvement as a defined dimension,9, 10, 11 although specificity around how to do so has been scant in shared decision‐making research.25 The Agency for Healthcare Research and Quality has advanced a webcast ‘Healthcare 411' with a public service announcement declaring it helpful to ‘bring a friend or family member to doctor appointments.' http://healthcare411.ahrq.gov/videocast.aspx?id = 691 Results from this study contribute empirical information to these discussions by validating that medical visit decision‐making10, 11, 26 and patient self‐management27 transpire within a broader context that may include trusted family or significant others. The incorporation of family in conceptualizing the patient–provider partnership and as a contributing party to health‐care processes reflects the real‐world context of health‐care communication and medical decision making9, 28, 29 with implications for the design of decision‐support and chronic care innovations that are responsive to the circumstances and concerns of older adults.
Acknowledgements
This study was supported by National Institute of Mental Health grant K01MH082885 ‘Optimizing Family Involvement in Late‐Life Depression Care’ (JLW). The sponsor of this research was not involved in its study concept or design, recruitment of subjects or acquisition of data, data analysis or interpretation, or in the preparation of this manuscript. The original research that funded the collection of these data was supported by NIA Grant #R44‐AG15737 to Mary Ann Cook (jvcradiology@charter.net)
References
- 1. Fowler FJ Jr, Levin CA, Sepucha KR. Informing and involving patients to improve the quality of medical decisions. Health Affairs (Millwood), 2011; 30: 699–706. [DOI] [PubMed] [Google Scholar]
- 2. IOM . Crossing the Quality Chasm. A New Health System for the 21st Century. Washington, DC: National Academy Press, 2001. [PubMed] [Google Scholar]
- 3. Scholle S, Torda P, Peikes D, Han E, Genevro J. Engaging Patients and Families in the Medical Home. Rockville, MD: Agency for Healthcare Research and Quality, 2010. AHRQ Publication No. 10‐0083‐EF. [Google Scholar]
- 4. Partnership NP . Priorities for the National Quality Strategy, 2011. Available at: http://www.qualityforum.org/Setting_Priorities/NPP/National_Priorities_Partnership.aspx. accessed 5 September 2011.
- 5. Katon W. The comorbidity of diabetes mellitus and depression. American Journal of Medicine, 2008; 121: S8–S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self‐management of chronic disease in primary care. Journal of the American Medical Association, 2002; 288: 2469–2475. [DOI] [PubMed] [Google Scholar]
- 7. IOM . Retooling for an Aging America: Building the Health Care Workforce. Washington, DC: The National Academies Press, 2008. [PubMed] [Google Scholar]
- 8. Wolff J, Roter D. Family presence in routine medical visits: A meta‐analytical review. Social Science and Medicine, 2011; 72: 823–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Morton R, Tong A, Howard K, Snelling P, Webster A. The views of patients and carers in treatment decision making for chronic kidney disease: systematic review and thematic synthesis of qualitative studies. British Medical Journal, 2010; 340: c112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stacey D, Legare F, Pouliot S, Kryworuchko J, Dunn S. Shared decision making models to inform an interprofessional perspective on decision making: a theory analysis. Patient Education and Counseling, 2010; 80: 164–172. [DOI] [PubMed] [Google Scholar]
- 11. Price EL, Bereknyei S, Kuby A, Levinson W, Braddock CH 3rd. New elements for informed decision making: A qualitative study of older adults' views. Patient Education and Counseling, 2012; 86: 335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. DiMatteo M. Social support and patient adherence to medical treatment: a meta‐analysis. Health Psychology, 2004; 23: 207–218. [DOI] [PubMed] [Google Scholar]
- 13. Gerteis M, Edgman‐Levitan S, Daley J. Through the Patient's Eyes. Understanding and Promoting Patient‐Centered Care. San Francisco, CA: Jossey‐Bass, 1993. [Google Scholar]
- 14. Street R, Gordon H. Companion participation in cancer consultations. Psycho‐oncology, 2008; 17: 244–251. [DOI] [PubMed] [Google Scholar]
- 15. Wolff J, Roter D. Hidden in plain sight: Medical visit companions as a quality of care resource for vulnerable older adults. Archives of Internal Medicine, 2008; 168: 1409–1415. [DOI] [PubMed] [Google Scholar]
- 16. Clayman M, Roter D, Wissow L, Bandeen‐Roche K. Autonomy‐related behaviors of patient companions and their effect on decision‐making activity in geriatric primary care visits. Social Science and Medicine, 2005; 60: 1583–1591. [DOI] [PubMed] [Google Scholar]
- 17. Teresi J, Ramirez M, Ocepek‐Welikson K, Cook M. The development and psychometric analyses of ADEPT: an instrument for assessing the interactions between doctors and their elderly patients. Annals of Behavioral Medicine, 2005; 30: 225–242. [DOI] [PubMed] [Google Scholar]
- 18. Wolff J, Roter D. Older Adults' Mental Health Function and Patient‐Centered Care: Does Family Companion Presence Help or Hinder Communication? Journal of General Internal Medicine, 2012; 27: 661–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Roter D, Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Education and Counseling, 2002; 46: 243–251. [DOI] [PubMed] [Google Scholar]
- 20. Ware J Jr, Snow K, Kosinski M, Gandek B. SF‐36 Health Survey Manual and Interpretation Guide. 1993.
- 21. Zeger S, Liang K. Longitudinal data analysis for discrete and continuous outcomes. Biometrics, 1986; 42: 121–130. [PubMed] [Google Scholar]
- 22. Adelman R, Greene M, Ory M. Communication between older patients and their physicians. Clinics in Geriatric Medicine, 2000; 16: 1–24, vii. [DOI] [PubMed] [Google Scholar]
- 23. O'Flynn N, Staniszewska S. National Institute for H, Clinical Excellence. Guideline development G. Improving the experience of care for people using NHS services: summary of NICE guidance. British Medical Journal, 2012; 344: d6422. [DOI] [PubMed] [Google Scholar]
- 24. Rabins PV, Black BS. Ethical issues in geriatric psychiatry. International Review of Psychiatry, 2010; 22: 267–273. [DOI] [PubMed] [Google Scholar]
- 25. Galvin K, Clayman M. Whose Future Is It? Ethical Family Decision Making in the Oncofertility Context In: Woodruff T, Zoloth L, Campo‐Engelstein L, Rodriguez S. (eds) Oncofertility: Reflections From the Humanities and Social Sciences. New York, NY: Springer, 2010: 429–445. [Google Scholar]
- 26. Legare F, Stacey D, Pouliot S et al Interprofessionalism and shared decision‐making in primary care: a stepwise approach towards a new model. Journal of Interprofessional Care, 2011; 25: 18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Battersby M, Von Korff M, Schaefer J et al Twelve evidence‐based principles for implementing self‐management support in primary care. Joint Commission Journal on Quality and Patient Safety, 2010; 36: 561–570. [DOI] [PubMed] [Google Scholar]
- 28. Fraenkel L, McGraw S. Participation in medical decision making: the patients' perspective. Medical Decision Making, 2007; 27: 533–538. [DOI] [PubMed] [Google Scholar]
- 29. Schafer C, Putnik K, Dietl B, Leiberich P, Loew T, Kolbl O. Medical decision‐making of the patient in the context of the family: results of a survey. Supportive Care in Cancer, 2006; 14: 952–959. [DOI] [PubMed] [Google Scholar]


