Abstract
Cells require energy to carry out their functions and they typically use oxidative phosphorylation to generate the needed ATP. Thus, cells have a continuous need for oxygen which they receive by diffusion from the blood through the interstitial fluid. The circulatory system pumps oxygen-rich blood through a network of increasingly minute vessels, the microcirculation. The structure of the microcirculation is such that all cells have at least one nearby capillary for diffusive exchange of oxygen and red blood cells release the oxygen bound to hemoglobin as they traverse capillaries. This review focuses first on the historical development of techniques to measure oxygen at various sites in the microcirculation, including the blood, interstitium and cells. Next, approaches are described as to how these techniques have been employed to make discoveries about different aspects of oxygen transport. Finally, ways in which oxygen might participate in the regulation of blood flow toward matching oxygen supply to oxygen demand is discussed. Overall, the transport of oxygen to the cells of the body is one of the most critical functions of the cardiovascular system and it is in the microcirculation where the final local determinants of oxygen supply, oxygen demand and their regulation are decided.
Keywords: Oxygen transport, red blood cell, hemoglobin, oxygen tension, oxygen saturation, oxygen consumption, phosphorescence quenching, microspectrophotometry, arteriole, capillary, intravital video microscopy
INTRODUCTION
This article is an expanded version of the presentation made on the occasion of the Eugene M. Landis Research Award Lecture of the Microcirculatory Society presented on April 22, 2012 in San Diego, California. The lecture covered highlights of the field of oxygen transport from the perspective of studies focused at the level of the microcirculation over the past four decades. Our current knowledge and understanding of the field of oxygen transport have been shaped by numerous investigators from the disciplines of biochemistry, cell biology, physiology and mathematical modeling. The narrative which follows mentions many of the people who have made important contributions to this field.
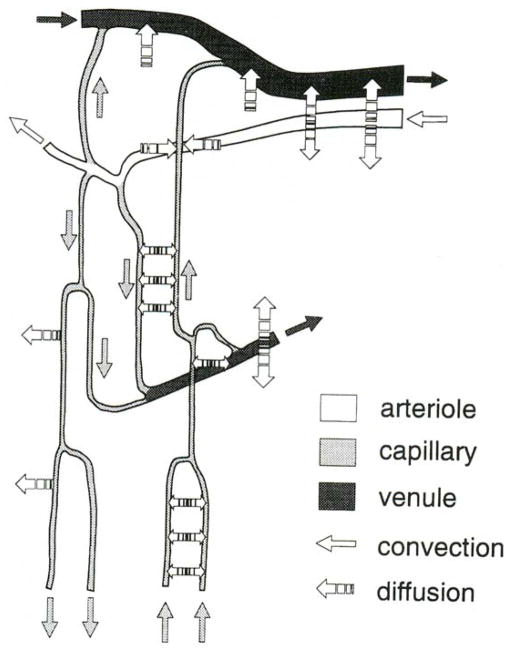
Pathway for oxygen
Since mitochondrial oxidative phosphorylation is the main pathway through which cellular adenosine 5′-triphosphate (ATP) is generated, it is important for an adequate and continuous amount of oxygen to be supplied to these energy-generating organelles. The cardio-respiratory system plays a key role in satisfying this need, especially the part we call the microcirculation. Following the vascular network from the aorta down to the smallest microvessels, the capillaries, each parenchymal cell is in close proximity to at least one capillary, so that passive diffusion ensures an efficient supply of oxygen. As will be discussed in greater detail later, the capillaries are not the only source of oxygen – because of the high permeability of the arteriolar wall to oxygen, the arterioles also represent a major source of oxygen, especially in tissues with low blood flow and oxygen consumption (e.g., resting skeletal muscle). In the peripheral tissues, the pathway for oxygen starts with the release of oxygen from oxyhemoglobin in the red blood cells (RBCs), followed by its passage across the capillary wall, through the interstitium, to the cell and finally into the mitochondria where it is consumed by its reaction with cytochrome c oxidase (190).
As with the study of many aspects of biological systems, there are several different levels of organization or integration, as well as spatial and temporal scales, at which the studies can take place. At the smallest level, the study of oxygen transport can be viewed from a molecular or biochemical perspective in which oxygen and other molecules with which it interacts (e.g., hemoglobin, cytochrome c oxidase) are the focus of attention. The next level involves a cell biological approach in which oxygen interacts with cells and organelles (e.g., mitochondria) within them in such a way that energy is generated to support the activities of the cell. At this level, oxygen can be involved in complicated interacting molecular reaction and signaling networks within and between cells. The microcirculation is positioned in a particularly strategic location, since it represents the interface between the parenchymal cells in a tissue (consumers) and the circulatory system (supplier) which provides nutrients and removes metabolic wastes to support tissue function. Microcirculationists who employ intravital microsopic observation and measurement have a front-row seat to witness the exciting interplay between circulatory and cellular function. This microcirculatory level of integration represents the smallest number of system components that retain the complete integrated function of both the circulatory and cellular systems. The next levels of organization are the organ/tissue level, followed by the integration of all parts of the system into a fully functioning organism. At these last two levels a more “black box” approach is often employed to express the results of experiments or modeling.
Information required in the study of oxygen transport
What information is needed to study oxygen transport in the microcirculation? First, one must know the level of oxygen at several key sites along the pathway. In the blood knowledge of the oxygen tension or PO2 is needed, along with the degree to which the hemoglobin binding sites are saturated with oxygen (hemoglobin oxygen saturation, SO2). The interstitial fluid (ISF) represents the interface between the vascular system which supplies oxygen and the parenchymal cells which consume it. The PO2 in the ISF can be thought of as reporting the balance between oxygen supply and oxygen demand. Thus, when PO2 in the ISF increases, this indicates that the oxygen supply has increased relative to its demand and vice versa. While it would be useful to know the PO2 within the parenchymal cells, currently there are no microcirculatory techniques to provide that key piece of information in real time. However, a recent development is the capability to determine PO2 in the mitochondria, the end user of oxygen for cellular metabolism. Detailed descriptions of these methods and how they work are presented in a subsequent section on how oxygen is measured in the microcirculation.
In addition to information on oxygen levels in and around the microvessels, there are other key data needed for a more complete understanding of oxygen transport. Detailed information about the geometry (i.e., diameter, length and luminal shape) of microvascular networks, as well as their angioarchitecture (i.e., the connections or topology within and between the networks), are needed. Data on microvascular hemodynamics, including RBC velocity, blood flow and hematocrit, are also critical elements in understanding the delivery of oxygen by the blood. Although the individual data mentioned above are interesting and useful in and of themselves, by incorporating these various types of data into a mathematical model of oxygen transport, much more powerful conclusions can be drawn regarding the integrative nature of the oxygen transport system as is pointed out below.
Cellular metabolism
Most cells prefer to make ATP by the process of oxidative phosphorylation in the mitochondria. The idea of different levels of organization can be applied to studies of cellular metabolism. For many years the reductionist approach has been a favored mode of investigation of the metabolic machinery of tissues and cells. This approach has provided much valuable information about the characteristics of the components of organelles, cells and isolated tissues and their involvement in carrying out the processes of cellular metabolism. However, removing these components from their natural chemical environments leaves one to consider how applicable the findings are to the intact tissue in which the circulation and associated parenchymal cells interact to provide that natural chemical setting. Thus, studies on pieces of dissected tissue, isolated cells, isolated mitochondria or purified enzymes of the electron transport chain (e.g., cytochrome c oxidase) must be viewed with caution when attempting to draw conclusions or make predictions about the behavior of intact, perfused systems in regard to their interactions with oxygen and associated molecules. In particular, the PO2 dependence of oxygen consumption for these progressively deconstructed entities appears to vary widely (81, 181, 193, 194). One can reasonably assume that if the precise chemical environment at each level of organization/integration could be accurately reproduced, then there should be common agreement among the different modes of investigation. However, it seems unlikely that we will be able to uncover such precise knowledge anytime in the foreseeable future, so that we must try to design studies which use relatively intact, perfused tissues as are generally available in microcirculatory studies (58). A key element for success in understanding the interactions among the various components which contribute to oxygen transport is also the existence of reliable computational models of the circumstances investigated which include, but are not limited to, realistic microvascular network geometry and topology, anatomic and metabolic data about the parenchymal cells, detailed hemodynamic data of perfusion in the network, and oxygenation data at the various sites referred to above. A number of groups have made great strides in producing such models (68, 136–138, 142, 144, 148–150, 154).
METHODS TO MEASURE OXYGEN IN THE MICROCIRCULATION
Over the years a number of techniques have been developed and used to determine the levels of oxygen at the key sites in the microcirculation referred to above. Some of these methods have been around long enough to have matured, while some have only recently been fully validated, and one is relatively new and awaits further study and validation. There are also methods to measure oxygen at larger scales which will not be addressed in this article.
Oxygen measurements in the blood
Oxygen-sensitive polarographic microcathodes to measure PO2
Oxygen can be measured using polarographic microcathodes, commonly known as oxygen microelectrodes (16). The catalytic surface (usually gold or platinum) at which oxygen is reduced is polarized to −0.7 V and the electrode can be calibrated by placing it in solutions equilibrated with different oxygen tensions covering the range of PO2’s expected to be encountered. The relationship between the small current passing through the electrode circuit and PO2 is linear. The first such electrodes had bare tips of platinum and were subject to stirring artifacts. Whalen (191) recognized the utility of having a recessed tip; such electrodes were insensitive to stirring and also possessed low oxygen consumption. The Whalen-type recessed tip electrode is quite accurate when properly calibrated. Schneiderman and Goldstick (147) carried out a theoretical study of the recessed-tip polarographic microcathode and found that a recess depth of about 10 times the diameter of the tip yielded performance that was virtually identical to that reported years earlier by Whalen et al (191) and thus provided a theoretical basis for the successful application of this type of microelectrode.
Duling and Berne (30) and others (32, 75) have used the Whalen-type recessed-tip oxygen microelectrode with superfusion solutions to determine oxygen levels in the microcirculation. Most of the reported measurements were of perivascular PO2, since penetration of the vessel wall to gain access to flowing blood with sharpened microelectrodes causes damage to the vessel wall, usually leading to platelet aggregation at the site of vascular injury. Also “poisoning” of the catalytic surface by plasma proteins leads to loss of calibration. Electrodes are also adversely affected by prolonged exposure to high PO2. Increased hydroxide ion formation at the catalytic surface raises pH locally and can cause precipitation of Ca or Mg salts there when bicarbonate-buffered superfusion solutions are used. Use of organic pH buffers makes the electrodes much more tolerant to high PO2. It is important to recognize that the electrodes are quite sensitive to temperature (191) and this fact becomes critical in their use with superfusion solutions where significant temperature gradients could be present within the thickness of the solution.
Phosphorescence quenching microscopy (PQM) to measure PO2
Wilson and his colleagues developed the phosphorescence quenching approach to measure PO2 in any location where the phosphor probe could be placed (182, 183). Typically the phosphor footprint is enlarged by binding to a macromolecule (e.g., albumin) or complexing it with polyethylene glycol, so that it is confined to the compartment in which it is introduced, depending on the permeability properties of that space (e.g., confinement to the circulation is expected for the cerebral circulation, but not necessarily for most other vascular beds).
In the so-called “time domain” approach, the phosphor is excited by a brief pulse of light. The excited phosphor can then decay back to the ground state by emitting a photon (phosphorescence) or by transferring energy to nearby oxygen molecules (collisional quenching). The energy transfer to oxygen results in the formation of the reactive species singlet oxygen, which can then react with nearby organic molecules, thereby resulting in the consumption of the original oxygen molecule. The Stern-Volmer equation governs the relationship between rate of phosphorescence decay (k), rate of decay in the absence of oxygen (k0) and PO2: k = k0 + kq PO2, where kq is the quenching coefficient. It is important to recognize that the calibration constants, k0 and kq, are temperature-dependent so that it is imperative that temperature either be controlled or measured as part of the PO2 determinations using PQM (156).
The PQM method (“time domain” approach) was initially implemented in the microcirculation by Torres Filho and Intaglietta (168). The technique was then used extensively by Intaglietta and co-workers for many years to investigate oxygen transport under a variety of conditions (87, 169, 170). Starting in 1996 Golub and co-workers have refined the PQM technique (55–64, 199) so that it now has vastly improved spatial and temporal resolution, in addition to a better appreciation for the contribution of photo-activated oxygen consumption to measurements of PO2, especially in situations where oxygenation at the measurement site is limited by diffusion (e.g., interstitial fluid). Another implementation of the PQM method is called the “frequency domain” approach and was also developed by Wilson and co-workers (183). In this version of the PQM method, the intensity of the excitation light is varied sinusoidally and the PO2 is related to the phase shift between the excitation and phosphorescence signals. A commercial instrument using fine fiber optic light guides (~ 2 mm diameter bundle of optical fibers) is used to supply the excitation light and receive the emitted phosphorescence. This technology has been employed by Poole and his group in microcirculatory studies of the oxygen kinetics associated with muscle contraction (5–7, 134, 135, 145). In this case the Pd-porphyrin phosphor is infused into the circulation and the excitation/emission fiber optic probe is placed over the region to be interrogated. The PO2 values arising from this approach have been called “microvascular PO2” to acknowledge that the value is an approximately volume-weighted admixture of PO2 values from the three compartments – arteriolar, capillary and venular – covered by the 2 mm diameter probe.
Not only is the continued development and refinement of instrumentation and phosphors important for the application of PQM, but the reliable interpretation of the phosphorescence decay curves is key to obtaining accurate measurements of PO2 at various sites (e.g., intravascular, interstitial). For a medium in which the PO2 is uniform, the Stern-Volmer equation can be used to relate the measured phosphorescence lifetime to PO2. However, application of PQM in the microcirculation to determine PO2 under less uniform conditions requires the use of more sophisticated processing of the phosphorescence decay curves. Golub et al (61) presented several different ways for recovering PO2 values under circumstances where the presence of PO2 gradients was certain or at least likely. Other investigators using the PQM method have employed some of these ideas in the analysis of their own data (107, 108, 155). The simplest and probably most practical of these approaches has been the treatment of an unknown distribution of PO2 at the measurement site as a Uniform statistical distribution, in which all PO2 values between a minimum and maximum value are equally represented in the distribution; this appears to be a good approximation in most cases and is simple to implement. Thus, the heterogeneous PO2 is assumed to range from a minimum to a maximum value, Pmin and Pmax, respectively, and the Uniform distribution for this situation is Funiform = 1/2δ, where δ is the half-width of the distribution and δ = (Pmax − Pmin)/2. Since a given PO2 is associated with a specific value of the phosphorescence decay rate, k, according to the Stern-Volmer equation, there is a spectrum of decay rates corresponding to the range of PO2’s at the measurement site. The time course of the phosphorescence decay, I(t), is modified from a monoexponential by a factor dependent on kq and δ and becomes
| [1] |
where I(0) is the phosphorescence intensity at t=0 and M is the mean PO2 at the measurement site or M = (Pmin + Pmax)/2 for the Uniform distribution. Note that when δ→0, the “correction” term becomes unity and the expected monoexponential decay for a uniform PO2 is recovered.
Microspectrophotometry of hemoglobin to measure SO2 and [Hb]
Measurement of hemoglobin oxygen saturation by taking account of differences in the absorption spectra of oxy- and deoxy-hemoglobin, known as oximetry, has been practiced for many years (111). The principles on which oximetry is based were first applied to the in vivo microcirculation to obtain SO2 in single vessels of a network using intravital video microscopy (128, 129). The Beer-Lambert law used widely in spectrophotometry of uniform solutions states that the optical density (OD) or absorbance (A) of a solution at a particular wavelength (λ) is proportional to both the concentration (c) of the substance and the path length of light through the solution (d) so that OD is given by:
| [2] |
where ελ is the extinction coefficient for the substance at the selected wavelength. For an absorbing substance like hemoglobin which can exist in more than one state (e.g., oxyhemoglobin, HbO2, and deoxyhemoglobin, Hb), the Beer-Lambert law can be generalized so that the OD can be expressed as the sum of contributions from the different hemoglobin species in the sample. For the case of a mixture of HbO2 and Hb, the Beer-Lambert law takes on the form
| [3] |
where ελ1 is the extinction coefficient for HbO2 and ελ0 is the extinction coefficient for Hb. By measuring optical density at two wavelengths – λM, where there is a large difference between HbO2 and Hb extinction coefficients, and λI, where the HbO2 and Hb extinction coefficients are equal (i.e., isosbestic wavelength) – one obtains a simple linear relationship between SO2 and the ratio of the two OD’s:
| [4] |
where both the hemoglobin concentration and path length cancel out of the calculation. For hemoglobin inside a RBC, the presence of a membrane separating two solutions of different protein concentration, hemoglobin and plasma, respectively, introduces a difference in refractive index which leads to light scattering at the RBC membrane separating these two phases. The resulting multiple scattering of light was investigated theoretically by Twersky (178) in a series of articles. For wavelength ranges where the absorption peaks are not large (e.g., in the 500 – 600 nm range) the contribution of light scattering depends on hematocrit (H) as Hx(1-H) and is a maximum near normal hematocrit, but is otherwise relatively independent of wavelength. By measuring the optical density at one additional isosbestic wavelength, the contribution of light scattering for that specific condition can be calculated and subtracted from the measured OD to yield SO2 according to Eq. 4, where for whole blood the corrected OD’s are used in place of those for a hemoglobin solution (128, 129). These relationships are explored in more detail in previous publications (119, 120, 126). In addition these same photometric signals were used by Lipowsky et al (102) to determine total hemoglobin concentration, [Hb]T, according to the expression:
| [5] |
where λI is one of the isosbestic wavelengths mentioned above.
Application to arterioles and venules
At the time this technique was introduced for microcirculatory measurements of SO2, it was recognized that the choice of wavelengths for these measurements was not arbitrary, but rather was dictated by the diameters and hematocrits encountered in the microcirculation. For instance, wavelengths in the 500 to 600 nm range are typically used for measurements of vessels in the diameter range from 20 to 100 μm and normal hematocrit (119, 120, 126). The contribution of light scattering to the OD under these conditions is about half of the measured OD. This three-wavelength approach was used in a number of early studies following its introduction. The first applications of this method dealt only with measurements of OD through the centerline of blood vessels, so that the optical path length was the luminal diameter of the vessel. Thus, single values for SO2 and [Hb] were obtained and these were considered to be averages along the light path through the center of the vessel (152, 153). With the advent of improved illumination, imaging and analytical capability, the requirement of one “measuring” wavelength and two isosbestic wavelengths can be relaxed and more powerful instruments to obtain maps of oxygenation in small microvascular networks can be constructed. One such recent multi-wavelength approach is that from Pries’ group (161).
Application to capillaries
Due to the similar size of RBCs and the capillary lumen, RBCs traverse capillaries in single file. Since the product of [Hb] and path length for a single RBC is so small, the amount of light absorbed by hemoglobin at the wavelengths used for larger vessels is too small to yield good contrast between the RBCs and background. However, this problem can be overcome by using wavelengths in the Soret region of the spectrum (about 400 to 450 nm) where hemoglobin absorbs about 10 times the amount of light as for the wavelengths used for larger vessels. Because of the single file flow of RBCs through capillaries, the issue of multiple light scattering by groups of RBCs in larger vessels does not apply for capillaries. RBCs still scatter some light, but the contribution to the measured OD is small and relatively constant (37, 46). Thus, we found empirically that only two wavelengths (e.g., an isosbestic wavelength, 420 nm, and one at which there is a large difference in light absorption by HbO2 and Hb, 431 nm) were necessary to obtain accurate measurements of SO2 for single RBCs. White light from an arc lamp (either xenon or mercury) was used to transilluminate capillaries and the resulting image was duplicated before passing through narrow bandpass interference filters, which selected the two wavelengths and were attached to two sensitive video cameras. The images from the two cameras were then sent to two synchronized video recorders. The images of the RBCs at the two wavelengths were analyzed to obtain the optical density at each wavelength and the SO2 was computed in terms of the ratio of the ODs as in Eq. 4 above. The OD values from each wavelength were used to create space-time images which displayed the OD of a single RBC at different time points as it passed along the capillary (36, 79, 80). This space-time image approach was also used to measure RBC velocity in capillaries, in terms of the displacement of RBCs and plasma gaps along the capillary that occur over a fixed time interval, as well as the lineal density of RBCs (i.e., the number of RBCs per millimeter) in these same capillaries based on automated frame-by-frame analysis of the spatial average of blood optical density over a selected length of capillary. Coincident information on both RBC velocity and lineal density permitted the frame-by-frame calculation of RBC supply rate (number of RBCs per second = RBC velocity × RBC lineal density) in capillaries. In addition, we developed methods to visualize perfusion of capillary networks which provides quantification of functional capillaries, i.e., those perfused with RBCs (78). More recently Fraser et al (52) have extended and refined the application of functional images of capillary networks with great success. They have extracted detailed geometric and other data from in vivo experiments and have used these data to reconstruct realistic networks of capillaries in a skeletal muscle.
Resonance Raman microspectroscopy to measure SO2
The application of resonance Raman microspectroscopy is a relatively new noninvasive technique to measure SO2 in microvessels in vivo (172, 173, 187). The technique offers distinct advantages over other currently used techniques by providing noninvasive and reliable in vivo determinations of SO2 in thin tissues, as well as in solid organs and tissues, which are unsuitable for techniques requiring transillumination.
Oxygen measurements in the interstitial fluid
The measurement of PO2 in the ISF has been carried out by oxygen microelectrodes (see above) and more recently using the phosphorescence quenching approach developed by Wilson and his co-workers (182, 183). The phosphorescent probe is typically bound to albumin or other large macromolecule so that it remains in the ISF when placed there by topical application (59, 60). Any probe which makes its way into the vascular space is quickly washed away by the prevailing blood flow. Thus, PO2 values determined by PQM in the ISF represent oxygen levels in the interfacial space between the vascular system and the parenchymal cells. Oxygen electrodes sample the oxygen field in their catchment volume, consisting of intracellular, interstitial and nearby intravascular compartments (16, 99); this value represents an average over these compartments and is often referred to as “tissue PO2.” Thus, ISF PO2 is a more precisely defined term than tissue PO2 and it is worth noting the distinction between the two.
Measurement of local oxygen consumption
A recent application of the PQM technology is the measurement of local oxygen consumption (VO2) using the rate of disappearance of oxygen at a site when blood flow has been rapidly arrested (64). In this measurement a transparent, inflatable bag made of a gas barrier film is attached to the microscope objective. The bag is positioned so that, when it is rapidly inflated (~0.1 s) to a pressure slightly above systolic pressure, it presses sufficiently on the tissue beneath the objective to arrest blood flow and extrude RBCs from the affected microvessels. The interstitial space of the tissue has previously been loaded with the phosphor by topical application and the disappearance of oxygen is recorded as the time course of PO2 change in the ISF. The local oxygen consumption, VO2, is related to the rate of PO2 decline (dPO2/dt) by
| [6] |
where α is the solubility of oxygen in the ISF. Corrections to account for oxygen consumption by the method itself and oxygen diffusion into the excitation region must be applied in general, although there are practical cases where the oxygen diffusion is small enough to be safely neglected. VO2 can be determined with only a short (~5 s) period of flow arrest followed by a slightly longer period of recovery (~15 s). This allows local VO2 to be determined in a quasi-continuous manner at a rate of three measurements per minute. It is expected that future developments will lead to improved time resolution of VO2 determinations. Alternatively, the time course of the PO2 response to extended flow arrest can be determined to find the oxygen dependence of VO2 (58; see below).
Oxygen measurements in mitochondria
Recent work by Mik et al (107, 108) has shown how PO2 can be evaluated inside mitochondria using the delayed fluorescence of Proto-porphyrin IX, an endogenous probe which can be excited and whose decay to the ground state can be used to determine PO2, in a manner similar to phosphorescence quenching. Indeed, a mathematical description of the analysis of delayed fluorescence decays yields identical equations relating the rate of decay to PO2 (107, 108). Since the mitochondria are the site within all cells for the consumption of oxygen, direct knowledge of the oxygen levels there provide tremendous insight into how oxygen is utilized for cellular energy production.
Related measurements: network geometry, angioarchitecture and microhemodynamics
The study of oxygen transport would not be complete without associated measurements of network geometry, angioarchitecture and microhemodynamics. Accurate measurements of tissue morphometry and of the angioarchitecture of the arteriolar and venular networks can be a tedious process, but this has been accomplished for a number of widely used preparations (42, 104, 141, 167). For capillary networks this procedure has been made less arduous by the introduction and refinement of flow visualization tools which create accurate images of capillaries perfused by RBCs (52, 78). This advance in intravital microscopic imaging has allowed the reconstruction of realistic networks of capillaries in skeletal muscle. Measurements of hemodynamic variables such as RBC velocity and hematocrit in arterioles and venules (146) and similar variables in capillaries (i.e., RBC velocity (179), lineal density of RBCs (38) and RBC supply rate) are critical for an evaluation of convective oxygen flow in the microcirculation, since virtually all of the oxygen carried by blood is located inside the RBCs. Dual-sensor approaches to determine RBC velocity have been used for many years (13, 101, 157, 188). The interpretation of the signals used to calculate velocity in terms of luminal profiles has provided additional insight into the distribution of velocity within microvessels (3, 131). The widespread use of video microscopy as an imaging tool for microcirculatory studies led to the realization of an upper limit on velocity determinations in arterioles and venules (74). Several different ideas have been implemented to overcome the limitations of standard video framing rates such as strobe illumination and shuttering of the video camera (115). With the advent of high framing rate video cameras these tricks are no longer needed, although they remain a cost-effective solution to the more expensive high framing rate option. A recent approach to determining RBC velocity profiles in arterioles using digital camera technology is to use fluorescently-labeled RBCs in an innovative way (1). By selecting an appropriate exposure time, each labeled RBC leaves a bright streak in the image whose length is proportional to the RBC velocity. By measuring a population of streaks and correlating the velocity with luminal position, the profile in RBC velocity can be recovered. This approach has proven to be quite accurate for computing blood flow in microvessels, as well as demonstrating the degree of blunting of the velocity profile as a function of luminal diameter.
COMPUTATIONAL MODELING OF OXYGEN TRANSPORT
Theoretical considerations, including results of computational modeling, have played an important role in the study of oxygen transport. Formulating an informative model requires that the modeler understand the fundamental elements of the system being modeled. In the case of oxygen transport in the microcirculation this includes a deep appreciation of the importance of microvascular network geometry and topology and biophysical principles of blood flow, diffusion and various chemical reactions involving oxygen, and the ability to integrate these sometimes highly technical components into a working model able to make predictions about the outcome of real experiments, interpret the resulting data, compare with previously formulated hypotheses, and guide further experimentation when initial hypotheses require revision. Most models are expressed in terms of systems of time- and space-dependent partial differential equations which describe mass transport of oxygen and other related species (e.g., NO, Hb, Mb). A successful model sets stringent constraints on the involved variables and the quality of the predictions are only as good as the accuracy of the assumptions and values of key input parameters.
August Krogh (94) was the first to present in mathematical terms the basic ideas of what is needed to quantify oxygen transport at the microcirculatory level in the steady state, at least for a single capillary embedded in a tissue of constant oxygen consumption. Krogh’s tissue cylinder model set the stage for almost all subsequent models, and there is a rich history of mathematical modeling deriving from this early start. For instance, Hellums (67, 68) used basic concepts of mass transport to predict that the passage of RBCs through capillaries would result in fluctuations in PO2 or erythrocyte associated transients (EATs), a phenomenon which was observed only recently (4, 56). Popel and his co-workers (54, 136–138, 140) have employed increasingly realistic models of oxygen diffusion and consumption, including hemodynamic features of oxygen transport, EATs, and oxygen transport in arterioles, capillaries and venules. Related work has been carried out on the effects of artificial oxygen carriers or blood substitutes, both hemoglobin-based oxygen carriers, HBOCs (86, 113, 114, 177) and perfluorocarbon emulsions, PFCs (35). Goldman and co-workers have also made recent contributions to modeling oxygen transport in realistic capillary networks (51). Secomb and Pries (141, 142, 148–150) have employed mathematical models of oxygen transport to study the development of microvascular networks, as well as investigate the potential role of different regulatory mechanisms on microvascular blood flow. Two close molecular relatives of oxygen, nitric oxide and superoxide, have also been the subject of extensive modeling efforts in recent years (17, 20–22). All these initiatives have worked together to improve our overall understanding of how oxygen is transported through microvascular networks and how it interacts with the surrounding tissues and other related molecules.
EARLY STUDIES OF OXYGEN TRANSPORT: FROM KROGH TO DULING
Contributions of Krogh to our understanding of oxygen transport
August Krogh is considered by many to be the founder of the field of oxygen transport in the microcirculation. In 1919 Krogh published a series of papers in which he reported morphological and physiological studies pertinent to oxygen transport (93–95). One achievement for which he is well known in the oxygen transport field is formulating a mathematical model, with the help of his colleague Erlang, to describe the diffusion of oxygen from a single capillary into a surrounding cylinder of uniform tissue which consumed the oxygen (94). Although a number of technical revisions have been made to the model, as a conceptual tool in understanding how oxygen is supplied to tissue by the blood, it has had a tremendous and continuing impact in the field. Krogh concluded that generally tissues were well oxygenated and that it took only a small gradient in PO2 to supply an adequate amount of oxygen to parenchymal cells. In this series of papers Krogh also proposed how the diffusion of oxygen to tissues could be regulated under conditions when oxygen demand changed over wide ranges (94, 95). For these seminal contributions to the field Krogh was awarded the Nobel Prize in Physiology or Medicine in 1920.
Several decades of relative silence in the oxygen transport field occurred following Krogh’s groundbreaking work. However, during this time investigators such as Stainsby and Otis (159) performed studies on oxygen transport at the whole tissue level which they then interpreted in terms of the Krogh cylinder model. So, even though the measurements were made at the macroscopic level, clear attempts were made to connect this work to the microscopic level. Other investigators, notably Cain and co-workers (19) and Wagner and co-workers (70, 71, 185) have employed similar approaches with great effect and much has been learned about oxygen transport as a result.
Longitudinal gradient in PO2: Influence of Duling on studies of oxygen transport
Fifty years after Krogh’s work on oxygen transport, Duling and Berne (30) published a classic article describing the first systematic measurements of PO2 in the microcirculation. The study was carried out to determine how PO2 varied along the microvascular network and was a test of Krogh’s tacit assumption that no significant oxygen exchange occurred prior to the capillaries. Duling and Berne reported the unexpected finding that there was a progressive decline in perivascular PO2, the longitudinal gradient in oxygen, in the arterioles of the superfused hamster cheek pouch and cremaster muscle. In this study most of the measurements of PO2 were made on the external surface of the blood vessels, rather than in the flowing blood, due to the acute vascular injury response resulting from penetration of a sharpened electrode through the vessel wall. However, a number of intravascular measurements were made to determine whether there was much difference between intra- and perivascular PO2 values, the transmural gradient in PO2. They showed that there was only a small (1–2 mmHg) difference between these values, indicating that the perivascular PO2 measurements provided an accurate estimate of intravascular oxygen tension and that the arteriolar wall itself did not consume much oxygen. This issue will be discussed in greater detail later in this article. Why did it take so long for Krogh’s ideas to be put to experimental test by direct microcirculatory experiments? Much of the reason must have to do with the fact that such measurements had to await the introduction of new technology (e.g., intravital video microscopy; 11, 82, 192) and the refinement of the technique to measure PO2 in microscopic volumes (191).
APPLICATION OF OPTICAL TECHNIQUES TO STUDY OXYGEN TRANSPORT IN THE MICROCIRCULATION
Introduction of microspectrophotometric measurements of hemoglobin oxygenation: Quantification of oxygen diffusion from arterioles
The loss of oxygen in the arteriolar network reported by Duling and Berne (30) was based on PO2 measurements which directly reflected the amount of oxygen in the dissolved form. Since dissolved oxygen accounts for only a small amount (~2%) of the oxygen contained in blood, it was possible that the large longitudinal gradients in PO2 observed by Duling and Berne represented an insignificant loss of oxygen. Almost all of the oxygen in arterial blood (~98%) is carried in the bound form by hemoglobin in the RBCs. In the terminal vessels of the microcirculation, where the PO2 and SO2 are lower (~ 30 mmHg and 50%, respectively) and where the hematocrit can be considerably lower than in the larger vessels (maybe as low as ~ 10%), the percentage of oxygen in the bound form will be lower or about 92% using the values in this example. Thus, it was necessary to develop a technique to measure the oxygen bound to RBC hemoglobin or hemoglobin oxygen saturation, SO2. This technique was described earlier in this article.
Pittman and Duling (130) applied this technique to make simultaneous measurements of hemoglobin oxygen saturation using microspectrophotometry and of periarteriolar PO2 using recessed-tip oxygen microelectrodes to verify that indeed the pairs of SO2-PO2 values corresponded to expectations from the equilibrium oxygen dissociation curve. The instrumentation used to make the SO2 measurement was upgraded from a rudimentary video-based densitometric approach to one using simultaneous recording of optical density for all three wavelengths using fiber optic light guides, photomultiplier registration of the signals and automated computation of SO2 and [Hb] (31). A similar system was used to implement the dual sensor cross correlation technique to determine RBC velocity (3, 188) and integrated with the SO2, [Hb] and geometric measurements so that all the pertinent variables needed to quantify oxygen transport in single, unbranched vessels of a network could be obtained simultaneously at a given measurement site.
This integrated measurement system was used to add to previous knowledge gained about oxygen transport in the microcirculation. The idea was to collect data using strictly optical methods (i.e., no oxygen electrode measurements requiring the use of a superfusion solution) at upstream and downstream sites in unbranched microvessels (i.e., no convective flow of oxygen into small side branches) throughout the arteriolar and venular networks in a preparation. We were particularly interested in using a skeletal muscle preparation whose metabolic rate could be varied over a wide range through use of muscle contraction. Although the cremaster muscle was a widely used preparation for this purpose, we also desired a muscle that contained a collection of relatively parallel fibers throughout different layers, unlike the cremaster which contained muscle fibers in different layers that were obliquely oriented. The reason for this criterion was a desire to have a preparation more amenable to computational modeling of convective and diffusive oxygen transport. Thus, we developed the hamster retractor muscle preparation, a small superficial muscle used to keep the cheek pouch normally retracted, which satisfied the specified criteria (162). In order to isolate the tissue from the atmosphere, we covered the dissected muscle with a transparent gas barrier film (Saran, polyvinilidene chloride). The chemical composition of Saran was altered in 2005 to make it more environmentally friendly, but at the sacrifice of the gas barrier properties of the previous product. Currently a replacement product possesses the desired gas barrier properties (Krehalon CB-100, Kureha, Japan) by having an extremely low permeability to atmospheric gases, as well as to water vapor.
The first systematic measurements of SO2, [Hb], RBC velocity, v, and luminal diameter, d, were made at paired upstream and downstream sites of unbranched segments in four consecutive branching orders of arterioles in the hamster retractor muscle (96, 97, 165) using the computerized system mentioned above (31). These measurements were combined to compute the convective inflow and outflow from the arteriolar segments as (see Fig. 1):
| [7] |
where CHb is the oxygen binding capacity of Hb (1.34 ml O2/g Hb). The diffusive flow of oxygen from the lumen of the segment, QO2D, was then given by mass balance for oxygen as:
| [8] |
Figure 1.
Schematic diagram of an unbranched segment (length = L) of a microvessel for which the convective inflow and outflow of oxygen (QO2conv) are computed from the variables diameter (d = 2Ri), velocity (v), hemoglobin concentration ([Hb]) and oxygen saturation (SO2) according to Eq. 7. Their difference is equal to the rate of oxygen diffusion (QO2diff) from the segment across the wall of thickness w = Ro − Ri, according to Eq. 8. The oxygen consumption of the wall can be computed from the mass-specific consumption, M, and the volume of the wall. This figure originally appeared in Pittman (124).
Swain and Pittman (165) assumed that the oxygen consumption by the arteriolar wall was negligible, so that QO2D represented the rate at which oxygen diffused across the walls of the arterioles. The results showed that, at progressively downstream sites in the arteriolar network, luminal diameter decreased, as did RBC velocity; [Hb] or Hct was about 80% of systemic; and SO2 declined, while the difference in SO2 between the upstream and downstream sites increased, suggesting that the rate of diffusive loss of oxygen was larger in the smaller arterioles. An unexpected finding was that ~2/3 of the oxygen loss was associated with the arterioles and ~1/3 from the capillaries, a result which may be related to low blood flow and low metabolic rate in the resting retractor muscle. Kuo and Pittman (96, 97) reported similar results with systemic hemodilution (Hct lowered from 50% to 32%) and hemoconcentration (Hct raised from 50% to 65%). The results of these studies confirmed the previous findings of a longitudinal gradient in oxygen (by SO2 rather than PO2 measurements in this case). Subsequently other laboratories (152, 153) found similar results using other tissues in other species, confirming that this result was a rather general one (see Table 1 in ref 124).
The results of these measurements at first appeared to be quite reasonable and expected. Since this was the first time that these variables were measured in a systematic manner, they were subjected to a rigorous analysis using a computational model which included convective and diffusive oxygen transport, as well as consumption by the surrounding tissue. The final conclusion of this analysis was that there appeared to be an order of magnitude discrepancy between oxygen flux from the arterioles and what could be accounted for by oxygen diffusion and consumption in the tissue – calculations based on the experimental results yielded an oxygen flux from the arterioles which was roughly 10 times more than that predicted by computational modeling (139). So far this discrepancy remains an unresolved issue, although some of the assumptions used to compute oxygen flux from the experimental numbers are only approximately correct. The recognition of this order of magnitude discrepancy between experimental results and the theoretical predictions is a testament to the important contributions of computational modeling to this research area (139, 189).
A natural question is “What is the destination of the ‘lost’ oxygen?” Oxygen which diffuses from arterioles can be consumed by neighboring parenchymal cells. It could be taken up by diffusion by other microvessels (e.g., capillaries, venules) in the vicinity of the arteriole. It could also be consumed by the arteriolar wall on its way from the arteriole, although Swain and Pittman (165) assumed that this would be negligible based on the earlier results of a small transmural PO2 gradient by Duling and Berne (30).
Search for the ‘lost’ oxygen: Introduction of phosphorescence quenching measurements of blood and tissue oxygenation
A report by Tsai et al (174) suggested that the last possibility might indeed be a realistic choice. Using the phosphorescence quenching method to measure PO2, they found a large difference in PO2 across the walls of arterioles in the rat mesentery. This large gradient implied that the arteriolar wall consumed oxygen at an enormous rate, almost two orders of magnitude higher than expected. Based on the mitochondrial content of the arteriolar wall, Vadapalli et al (180) calculated the maximum oxygen consumption one would expect to observe for the wall (see Fig. 2). They surveyed the existing literature on oxygen consumption due to endothelial cells, smooth muscle cells, segments of blood vessels and in vivo measurements of consumption by larger vessels and concluded that all these values of oxygen consumption were well within the upper limit calculated, whereas the value of arteriolar wall oxygen consumption reported by Tsai et al (174) was about an order of magnitude higher than the calculated upper limit.
Figure 2.
Compilation of oxygen consumption data for various vascular tissues: endothelial cells, smooth muscle cells (SMC), isolated segments of vessels, large in vivo vessels, and in vivo microvessels (from oxygen flux values computed from measurements similar to those associated with Eqs. 7 and 8). The horizontal line labeled Mmt represents the maximum oxygen consumption expected for these tissues based on their mitochondrial content. The value represented by the open square labeled 1 comes from Tsai et al (168) and the hatched bar on the right side of the plot represents data from numerous studies and reveals the widespread finding of an order of magnitude discrepancy between measured and predicted oxygen flux from microvessels. This figure originally appeared in Vadapalli et al (180). See original article for more details.
Oxygen consumption by phosphorescence measurements of oxygen
A likely explanation of this large discrepancy lies with the phosphorescence quenching method itself. Implementation of the method for microcirculatory measurements carries with it the need for high excitation light intensity and high phosphor concentration in order to obtain a high signal-to-noise ratio. Both of these requirements increase the oxygen consumption by the method, so that care must be taken to optimize other experimental conditions which could elevate oxygen consumption. For instance, at interstitial measurement sites each excitation flash will consume some oxygen and, unless enough time is allowed before the next excitation flash for oxygen to diffuse back into the excited region to replenish the consumed oxygen, the PO2 will fall with each successive flash until a new steady state is achieved in which the rate of oxygen consumption equals the rate of oxygen diffusion into the excited region.
Our measurements indicated that each excitation flash consumes enough oxygen to lower PO2 by about 0.3 mmHg (132). This is considerably larger than the value of 0.02 mmHg reported by Tsai et al (174). However, there was an error in the interpretation of the experiment used by them to arrive at this value, an error which was later corrected (176) giving a value in agreement with that of Pittman et al (132). Since the restoration of PO2 following a flash is governed by the laws of diffusion, this places a constraint on the speed of recovery dictated by the diffusion distance involved and the diffusion coefficient for oxygen, D = 1.04 × 10−5 cm2/s (57). For a circular excitation region of radius R, the time required for about 90% recovery of PO2 is given by T ≈ R2/2D. The radius of the excitation region reported by Tsai et al (174) was 70 μm, so that the characteristic recovery time for their system was about 2.5 s, whereas the flash rate used in their experiments was 30 Hz (for 3 s or 90 flashes). Thus an insufficient amount of time was allowed between flashes for recovery (~0.03 s), so that PO2 fell by about 0.3 mmHg per flash or by about 90 × 0.3 mmHg = 27 mmHg during the 3-sec measurement period. This rather large decrement in PO2 was equal to the reported transmural PO2 difference in the study by Tsai et al (174). A detailed analysis of the consequences of implementing the phosphorescence quenching method by either the “large excitation area” or the “small excitation area” approaches was given by Golub and Pittman (57). Thus, the large transmural gradient in PO2 reported by Tsai et al (174) appears to be the failure to apply a large correction, for the oxygen consumption by the method, to their measurements and so the conclusion that the arteriolar wall is a major sink for oxygen consumption is called into question (63).
Refinements in phosphorescence measurements of oxygen
The measurement technique using phosphorescence quenching has been further refined by using a scanning approach in which PO2 measurements are automatically made over a range of sites in discrete steps so that the same site does not receive multiple excitations over a short time interval (59). This allows one to obtain radial as well as longitudinal profiles of PO2 without the attendant artifact due to oxygen consumption by the method. Recent reports by Golub et al have demonstrated that the transmural gradient in PO2 for arterioles is small (59, 60), only a few mmHg confirming the original report by Duling and Berne (30), and that the rate of loss of oxygen from mesenteric arterioles is not unusually high (63, 133).
Oxygen diffusion from arterioles: Discrepancy between measured and predicted oxygen flux from arterioles
The order of magnitude discrepancy between apparent and predicted oxygen diffusion from arteriolar networks still has not been satisfactorily resolved. Vadapalli et al (180) computed the apparent oxygen flux from arterioles of different branching orders in various tissues and species based on published data in the literature and consistently found that the computed flux from the lumen was about ten times higher than expected. An interesting finding from this analysis is that similar calculations of oxygen flux based on experimental reports from capillaries yielded results that were in agreement with predictions; this difference in the results between arterioles and capillaries might provide a clue as to the nature of the discrepancy when using data from arterioles. One obvious difference between the findings in capillaries and arterioles is that the capillary data were based on measurements involving single RBCs, whereas those from arterioles were based on groups of RBCs with spatial distributions of velocity, hematocrit and oxygenation across the lumen. The photometric measurements for both capillaries and arterioles relied upon detection of light transmitted through the lumen of the microvessel above its centerline. For capillaries this signal was derived from single RBCs, whereas for arterioles the signal was an average weighted by the spatial distribution of the variable in question. In other words, the arteriolar signals depended on an unmeasured and generally unknown distribution of RBC velocity, hematocrit and SO2. Since all the arteriolar data were based on centerline measurements of the selected variables, there was a tacit assumption that the centerline value could be used as a uniform value for the variable in question. The diffusive oxygen flux from arterioles was calculated as the convective inflow minus the convective outflow of oxygen (see Eq. 8 above) and the calculation of these two convective oxygen flows was based on the centerline measurements (see Eq. 7 above). Since the diffusive oxygen flux was calculated as the difference of two large values, relative to the flux itself, and since the discrepancy between calculated and predicted flux was consistently about 10-fold, a possible explanation for the discrepancy is that a systematic error is present whereby the convective oxygen flow at the upstream site is systematically higher than the value at the downstream site by an erroneous amount.
To test whether the idea of a systematic error between upstream and downstream variables could be part of the explanation of the order of magnitude discrepancy between measured and predicted oxygen flux, paired comparisons were made for each variable (i.e., diameter, velocity, hematocrit and SO2) at the upstream and downstream sites for all four branching orders of arterioles, using the four datasets from Kuo and Pittman (96, 97). No significant differences were found between the paired values of diameter, velocity and hematocrit; only SO2 values exhibited a significant difference for 15 out of the 16 paired comparisons (4 arteriolar orders × 4 experimental groups). Thus, except for SO2 there was no evidence to suggest that a systematic difference existed for any of the other variables used in the calculation of diffusive oxygen flux. Additional tests of blood flow and RBC flow conservation were made on the unbranched arteriolar segments used in this study; in each case flow conservation was demonstrated. Since the only measured variable which was different at the upstream and downstream sites was SO2, it makes sense to consider what aspect of the SO2 measurement might play a role in any systematic discrepancy. The centerline (CL) value for SO2 is given by
| [9] |
where the integral is along a vertical line through the center of the vessel, and SO2(r) and H(r) represent the radial variation in oxygen saturation and hematocrit, respectively. Taking into account the radial dependencies of oxygen saturation, hematocrit and RBC velocity, the convective delivery of oxygen in an arteriole is given by
| [10] |
where the integral is taken over the lumen of the arteriole. It is clear that the radial dependence of SO2 enters in a slightly different way in Equations 2 and 3, so that the calculation of QO2C using the centerline values (i.e., Eq. 7) will give a different value whose magnitude will depend on the shape of the profile. Thus, if the SO2 profile has a different shape at the upstream and downstream measurement sites, one would expect the calculated diffusive oxygen flux to be affected. Profiles in SO2 have been measured previously by Ellsworth and Pittman (44), Tateishi et al (166) and Kobayashi et al (90, 91). The general finding in arterioles is that SO2 decreases from the center of the vessel toward the wall, as expected if there is an outward oxygen flux from the blood. Similar findings have also been reported using PQM by Golub and Pittman (55) and Carvalho and Pittman (18). The ultimate resolution of this discrepancy will most likely require a special study which incorporates profiles of all the pertinent variables in Eq. 10. Patel and Pittman (116, 117) presented a theoretical analysis of microspectrophotometry of hemoglobin. Some of these considerations have been presented before (122, 123). Perhaps this mass balance approach for estimating the diffusive flux of oxygen from arterioles is not the best one, since a variable computed as a small difference between two much larger values is highly susceptible to small systematic errors in one or both of the larger numbers.
Oxygen-linked parameters to characterize hamster retractor muscle
In order to make the most effective use of intravital microscopic data on oxygen transport using the hamster retractor muscle, and especially including the data in a comprehensive computational model of oxygen transport, we embarked on a systematic program to determine a number of morphological and biophysical parameters to fully characterize this preparation. Morphological data included detailed geometric information according to histochemical fiber type (163), capillarity (8, 163), mitochondrial density (164) and microvascular network angioarchitecture (42). Biophysical data included the diffusion coefficient for oxygen using a transient approach (9, 10, 43, 105), oxygen consumption in vitro using a Warburg closed chamber approach (163) and analysis of PO2 profiles in excised tissue using oxygen sensitive microelectrodes (34). Myoglobin was also determined for the retractor and several other muscles in the hamster and rat (106). Altogether this collection of data for the hamster retractor muscle represents a valuable database for future studies using this preparation.
Oxygen transport in capillaries
As mentioned earlier in this article, the measurement of hemoglobin oxygen saturation in single capillaries is similar to that in larger vessels, but there are also some significant differences, primarily that measurements need to be made on individual RBCs. This is both a challenge, due to their small size, and a blessing in the sense that the need to measure intravascular profiles of RBC velocity, spatial distribution and SO2 is obviated. Thus, the interpretation of measurements involving capillaries is less tied to intravascular profiles. Ellsworth et al (47) made the first measurements employing the microspectrophotometric technique to measure SO2 in RBCs and discovered the existence and consequences of heterogeneities in oxygen transport at the level of capillary networks. One feature of oxygen transport in capillary networks is that nearby capillaries can interact diffusively anytime there is a PO2 gradient between them. Spatial and temporal heterogeneities in RBC velocity, RBC spacing and SO2, in addition to capillary network connectivity, can give rise to local PO2 gradients which determine the movement of oxygen between capillaries and through the intervening tissue.
These measurements were followed by noting an unexplained gain of oxygen between the entrance and exit of capillaries (45). Further examination of the anatomical arrangement of the capillary network in relation to nearby arterioles revealed that RBCs flowing through capillaries could acquire oxygen by diffusion from arterioles which crossed the path of the capillaries. The reality of this possibility was confirmed by computational modeling carried out by Secomb and Hsu (149).
For over 50 years the intra-luminal resistance to oxygen transport in capillaries was neglected until David Hellums’ seminal paper in 1977 (67). The Krogh model of oxygen diffusion had assumed that all of the resistance to oxygen diffusion was located in the tissue outside the capillaries. Based on Hellums’ calculations, the resistance to oxygen transport was almost evenly divided between the intravascular space and the extravascular space, a revolutionary idea at the time. The reason for this major difference was linked to the particulate nature of blood: the RBCs carried almost all of the oxygen and occupied about half of the blood volume. Due to the similar size of RBCs and capillaries, the RBCs pass through the capillaries in single file, so that there are gaps occupied by plasma with a quite low oxygen solubility separating adjacent RBCs. According to Hellums’ calculations (67) the PO2 in and around the RBCs should be high, while that associated with the intervening plasma gap should be low. A consequence of the alternate passage of RBCs and plasma gaps past a site along a capillary was the prediction of fluctuations in PO2 as RBCs (high PO2) and plasma gaps (low PO2) alternately passed the observation site. These theoretical results were confirmed by more detailed calculations presented by others (49, 50, 72). The predicted fluctuations in PO2 were called “erythrocyte associated transients” or EATs and were a manifestation of the intravascular resistance to oxygen transport. Thus, the presence of EATs indicates that the transport of oxygen from the blood to the tissue is limited by factors, such as RBC spacing and tissue oxygen consumption, which enhance the magnitude of the EATs.
Almost 30 years passed before Hellums’ idea was put to experimental test. As is often the case, a serious test of a prediction must await until the experimental techniques have been refined sufficiently to allow the needed measurements. In the early 1980s our laboratory, and perhaps others, attempted unsuccessfully to detect EATs using recessed-tip oxygen microelectrodes which simply did not have the appropriate response time to observe these rapid transients (Sullivan and Pittman, unpublished). More recently the phosphorescence quenching method has been refined to achieve a sufficient temporal (~100 ms) and spatial (~1 μm) resolution to detect EATs and we have done so in the rat mesentery (56) and rat spinotrapezius muscle (4). Figure 3 gives an example of the scanning approach to PO2 measurements at upstream and downstream sites in a capillary (125) in which EATs are demonstrated at both locations. Lecoq et al (100) have recently confirmed the existence of EATs in another tissue by reporting their observation in the rat olfactory bulb, a tissue with much higher metabolic rate than the mesentery or resting skeletal muscle, using two-photon imaging of oxygen and blood flow.
Figure 3.
Demonstration of erythrocyte-associated transients (EATs) in PO2 at upstream (upper trace) and downstream (lower trace) sites in the same capillary using the scanning PQM approach. The excitation spot switched back and forth between the two sites at a frequency of 100 Hz for 1 sec. There was a systematic difference between PO2 values at the two sites, indicating a longitudinal gradient in PO2 along the capillary. Note also that the magnitude of the fluctuations was larger at the downstream site, as expected for a relatively uniform efflux of oxygen along the capillary and lower oxygen content at the downstream site. This figure originally appeared in Pittman (125).
Other issues in oxygen transport
There are a number of diffusion and kinetic barriers that must be overcome for oxygen to go from its safe harbor on the hemoglobin molecule to its final destination within the mitochondrion where it is consumed. In addition to the obvious physical barriers to oxygen diffusion, such as cell membranes and fluids in the interstitium and cytoplasm, two others in this category which occur between the RBCs in microvessels and the luminal surface of the endothelium are the endothelial surface layer or glycocalyx (143) and the so-called RBC-free layer of plasma (89) between the RBC column and the glycocalyx. The thickness of these barriers can vary according to local time-dependent hemodynamic conditions (88, 143). These physical elements have been included in some computational models of oxygen transport, but no measurements have been reported to indicate their impact on tissue oxygenation. A kinetic barrier to oxygen transport is related to the time needed to release oxygen from hemoglobin in the RBC relative to the residence time of RBCs in capillaries (65). Under conditions of increased RBC flow, such as occurs in skeletal muscle capillaries during exercise hyperemia, RBCs could traverse a capillary too rapidly to allow for the expected release of oxygen. This condition would be exacerbated in cases of rarefaction of the capillary network in hypertension and could be the explanation of the elevated venous SO2 (98) and delayed recovery of venous PO2 (158) observed in the spinotrapezius muscle of spontaneously hypertensive rats.
OXYGEN DEPENDENCE OF RESPIRATION IN SKELETAL MUSCLE
The PO2 dependence of VO2 is an important piece of information in regard to understanding the oxygen needs of cells. By locally arresting blood flow in a tissue and recording the ISF PO2 using PQM until it reaches almost 0 mmHg, it is possible to determine how VO2 depends on PO2. Golub and Pittman (58) showed how VO2 can be calculated as a function of PO2 for the resting rat spinotrapezius muscle from the time course of PO2, following corrections for the oxygen consumption by the method and oxygen diffusion into the excitation region. Using a Michaelis-Menten kinetic model of oxygen consumption by the mitochondria in the resting muscle, and the assumption that the PO2 gradient within the muscle fiber (of arbitrary, but constant, cross section) could be described by a Uniform statistical distribution (an exact result for a circular cross section and uniform oxygen consumption), the PO2 dependence of VO2 was fit to obtain the parameters of maximal (resting) oxygen consumption and Km or P50 for the PO2 dependence (see Fig. 4). This first in situ measurement of oxygen dependence yielded an average value for Km of 10 mmHg, considerably higher than values reported for isolated cells and mitochondria (194). One outcome of the measurements and analysis was that the oxygen dependence varies with the magnitude of the intrafiber PO2 gradient, which in the case of the resting spinotrapezius muscle was about 5 mmHg.
Figure 4.
Typical plot of the oxygen dependence of respiration for the in situ resting rat spinotrapezius muscle. These data points were obtained using Eq. 6 (with corrections as described in ref 55) to compute oxygen consumption and the PO2 values are corresponding interstitial values on the surface of the fibers at the measurement site. The data were partitioned between hypoxic and normoxic regions in the muscle and the resulting curve fits are shown as solid lines. For this muscle Km was 9.4 mmHg and the PO2 difference within the muscle was about 3 mmHg. This figure originally appeared in Golub and Pittman (58). See original article for more details.
NITRIC OXIDE AND ITS CONNECTION TO OXYGEN TRANSPORT
From a molecular point of view, nitric oxide and oxygen are close cousins. Nitric oxide is closely related to the convective oxygen supply through its ability to control arteriolar caliber by its vasorelaxant properties (85, 110), as well as to the oxygen demand through its ability to modulate oxygen consumption (VO2) by the mitochondria in parenchymal cells (15, 22). Thus, NO has the potential to play a major role in oxygen transport and tissue oxygenation. Hemoglobin, the carrier of oxygen in the blood can also interact strongly with NO. For instance, it is thought that the substantial pressor response observed with the infusion of some HBOCs is due to the avid scavenging of NO by cell-free hemoglobin (112). The relative concentrations of NO (10s to 100s of nM), oxygen (10s of μM) and hemoglobin in the RBCs (~20 mM, heme basis) range over several orders of magnitude and this helps to explain the sensitivity of their interactions.
ROLE OF MYOGLOBIN IN OXYGEN TRANSPORT
The presence of the oxygen-carrying protein myoglobin (Mb) appears to be critical for proper functioning of cardiac muscle, as well as oxidative skeletal muscle fibers. The role of myoglobin in muscle has been debated over the years: Is it a readily available reservoir of bound oxygen; is it a facilitator of intracellular oxygen diffusion; or is it possibly a temporary storage depot for NO – or some combination of these functions? The oxygen reservoir function of myoglobin has been around since the work of Millikan (109) and appears to be a widely accepted concept. The idea of myoglobin acting as a facilitator of oxygen transport has been championed over the years, primarily by Wittenberg and coworkers (195, 196). However, due to myoglobin’s large size, doubts have been raised about whether the mobility of Mb inside muscle cells is adequate to allow it to manifest this carrier role to any significant degree (197). Honig and Gayeski (73) employed a cryospectrophotometric method to quantify MbO2 in single, frozen muscle fibers. The initial results of these studies pointed to a relatively flat distribution of MbO2 in single fibers based on a reported spatial resolution of the measurements of ~1 μm. However, a re-evaluation of the spatial resolution question by Voter and Gayeski (184) revealed that the presence of ice crystals in the frozen samples yielded a spatial resolution which was closer to ~120 μm and implied that the intracellular PO2 measurements reported prior to this work were averaged over several muscle fibers and thus would have dampened any PO2 gradients that were present. A new role suggested for Mb has to do with its interactions with nitric oxide (197). Consider the situation in the transition from rest to exercise in an oxidative muscle fiber with a high concentration of Mb. Under resting conditions the muscle fiber should be well-oxygenated, but with the onset of contractions, oxygen will be released from the MbO2 and the deoxygenated Mb will bind free NO in the fiber, thereby lowering NO levels and allowing the mitochondrial oxygen consumption to increase greatly. Thus, Mb acts in a coordinated way as both a local oxygen source and as a NO sink to modulate local oxygen supply and demand. With these several possible roles for Mb, the final verdict regarding the function(s) of Mb awaits further study.
REGULATION OF OXYGEN TRANSPORT
Questions about matching oxygen supply to oxygen demand
Although our laboratory has focused its efforts on the pursuit of measurements involving oxygen transport for many years, the question of whether the oxygen supply to tissues is regulated has always been just a small step away. Is the local supply of oxygen by the circulation matched to its local demand by the tissues (2, 186) and, if so, by what mechanism(s)? What aspect(s) of the oxygen supply is/are regulated? Is it the PO2 at the tissue, cellular or mitochondrial level? Is there a critical oxygen level (58, 171) below which tissue function begins to decrease? Forty years ago the prevailing thought was that blood flow was controlled to yield a fairly constant tissue PO2 (30). But, could it be the rate of oxygen diffusion to the tissue as later suggested by Duling (26, 27, 29)? While it appears that the oxygen supply is well-matched to the oxygen demand, perhaps it is not just the oxygen supply which is being regulated. Why does blood flow, and hence oxygen delivery, increase during active or functional hyperemia and in reactive hyperemia?
Mechanisms of hypoxic vasodilation: Fixed and mobile sensors
A number of mechanisms have been put forward to explain changes in local blood flow in response to various interventions (especially muscle contraction): the myogenic mechanism (24, 83), the metabolic mechanism (24), oxygen-linked ATP release from RBCs (39, 41), NO and prostanoid (e.g., prostacyclin, PGI2) release from the endothelium of arterioles and venules (48, 69, 92, 198) and conducted vasodilatory responses (151) which help integrate these basic mechanisms. The metabolic mechanism has a long and distinguished history and is the standard textbook explanation for most metabolically-linked alterations in blood flow (14), although recent concerns have been voiced as to its ability to adequately account for observed hyperemic responses (84). Undoubtedly there will be additional proposals for mechanisms linked to oxygen which will attempt to explain the matching of oxygen supply and demand. In addition to the ATP release mechanism (39, 41), at least two other regulatory mechanisms involving the RBC as a mobile oxygen sensor have been put forward. Stamler and coworkers (160) have proposed that RBCs carry NO in the form of S-nitroso-Hb (SNOHb), whereby NO is carried in this form at the β93 cysteine of hemoglobin and released in response to the RBC passing through a hypoxic region; this hypothesis remains controversial. Gladwin and co-workers (23) have proposed that hemoglobin possesses nitrite reductase activity and can convert nitrite in the blood into NO inside the RBC, from which it is then released to produce vasodilation of the nearby arteriolar smooth muscle. Because of the strong affinity of free NO to any unliganded heme groups on the hemoglobin, it is difficult to envision how either of these mechanisms involving release of NO from RBCs can be viable. Furthermore, detailed calculations by Chen et al (20, 21) have called into question whether the concentrations of NO produced by either of these mechanisms are sufficient to account for the observed vasodilation. The results of these calculations are related to a current controversy as to the physiological concentration of NO (66). Measurements of NO in the microcirculation using recessed tip microelectrodes by Bohlen and co-workers (12) have consistently shown that NO concentration is in the 100s of nM, whereas Hall and Garthwaite (66), as well as the computational modeling of Chen et al (22), have maintained that the concentration must be in the nM range or below. This almost three order of magnitude discrepancy has yet to be resolved. The endothelium undoubtedly plays an important role in metabolically-linked vasomotor responses through its production and release of molecules such as NO and PGI2 (48, 69, 92, 198). The next chapter describing the oxygen-linked local regulation of blood flow remains to be written and it will not be surprising if it involves the introduction of a new paradigm.
To what extent is oxygen involved in its own regulation?
The final part of this review has to do with what role oxygen itself might play in regulating oxygen transport. It has been known for many years that increasing the oxygen supply to a peripheral tissue usually results in vasoconstriction of the resistance vessels that determine blood flow; decreasing the oxygen supply leads to the opposite response, vasodilation. What is the signal to the vascular smooth muscle that produces these vasomotor responses and from where does it originate? Since it is the vascular smooth muscle whose contractile state is altered in response to the change in oxygen supply to the tissue, it is natural to consider whether the signal derives directly from the smooth muscle itself or rather indirectly from the nearby parenchymal cells which produce a chemical signal resulting in the final vasomotor effect. Thus, is the oxygen sensing mechanism (i.e., “oxygen sensor”) associated with the blood vessel itself, with the parenchymal tissue or with both? Detar and Bohr (25) appeared to have provided the answer that the oxygen sensitivity was located in the smooth muscle. Using contracted rabbit aortic strips, they reported that isometric force produced by the strips gradually decreased as the PO2 of the organ bath in which the strips were suspended was lowered over the full physiological range from about 100 mmHg to about 0 mmHg. Calculations of oxygen diffusion from the bathing medium into such a preparation indicated that the interior of the strip might actually be hypoxic at surface PO2 values much higher than 0 mmHg. Experiments to test this hypothesis were carried out on strips of hog carotid artery with a wide range of thickness (127). It was found that, indeed, diffusion limited the supply of oxygen to the strip and the critical PO2 below which isometric force began to decline was proportional to the square of the thickness of the strip, as predicted by a simple model of oxygen diffusion and consumption (127). By extrapolating the results down to the thickness of an arteriolar wall, the predicted range of oxygen sensitivity of force generation was just a few mmHg, well below the typical PO2 of blood passing through arterioles, leading to the conclusion that it was unlikely vascular smooth muscle possessed the requisite sensitivity to respond directly to changes in oxygen in the microcirculation. The mechanism(s) by which in vitro preparations of conduit arteries respond to changes in bathing solution oxygenation has not been definitively established, but one possibility is the production of a vascular smooth muscle relaxant within the hypoxic core of the preparation and its subsequent diffusion within the smooth muscle tissue (118, 121). Over the past 40 years many studies have been carried out to investigate the oxygen sensitivity of strips, rings and segments of blood vessels, but usually not microvessels, from various organs and various species. It appears that most of these studies did not consider the effects of diffusion limitations on the results due to tissue thickness and unstirred fluid layers, so that the interpretation of many of these studies is not clear-cut.
Some studies of the question of oxygen sensitivity have been carried out on microcirculatory preparations. Duling (28) applied physiological salt solutions with high and low oxygen tensions, by global superfusion or localized spritzing on selected microvessels, to the hamster cheek pouch preparation. As many investigators have since confirmed, superfusion with high PO2 results in vasoconstriction, while that with low PO2 results in vasodilation. Applying such solutions locally to individual vessels did not produce vasomotor responses correlated with the PO2 of the applied solution, leading to the conclusion that individual microvessels did not appear to respond directly to oxygen, whereas some mechanism of oxygen sensing was present at a more global level and most likely involved responses from the parenchymal cells (33). A variation on this approach was employed by Jackson and Duling (77) in which the parenchymal tissue was dissected away from a long arteriole in the superfused hamster cheek pouch. This selected arteriole was not sensitive to localized direct application of solutions with high and low PO2, whereas global changes in PO2 produced the familiar vasomotor responses described above. More recent studies have attempted to identify the location of local oxygen sensing, as well as attribute the vasomotor responses to specific molecules (53, 76, 103). While it is abundantly clear that oxygen is involved somehow in the vasomotor response, the precise manner in which it is involved remains an active area of investigation.
PERSPECTIVE
Almost a century ago August Krogh laid the conceptual foundation on which studies of microcirculatory oxygen transport have been based. During the intervening years, especially in the 1960s and 1970s, there occurred a renaissance in the microcirculation which gave the field new technology and allowed the pursuit of more difficult and penetrating questions, leading to new lines of research. Work over the last 30 years has provided a more complete understanding of where oxygen can move and how it is consumed (see Fig. 5). The mechanism(s) by which oxygen is involved in the local regulation of blood flow remains unclear and is the focus of studies pursuing the matching of oxygen supply to oxygen demand from several different perspectives. The future of this field looks encouraging in terms of providing insights which will lead to new treatments in diseases and pathologies related to the limitation of tissue health and performance brought about by inadequate oxygen supply to tissues. It is expected that studies at the level of the microcirculation will play a significant role in revealing these sought-after insights.
Figure 5.
Schematic diagram of the terminal microvasculature (arterioles, capillaries and venules) depicting the movement of oxygen by convection (arrows within vessels) and diffusion (arrows between vessels). The concept from Krogh’s writings was that diffusive oxygen exchange occurred between neighboring capillaries, but other vessels were not involved in oxygen diffusion. The current view is that the highly diffusible oxygen can move by diffusion between any vessels in close proximity, so long as a PO2 gradient exists between them. Such diffusive exchange is represented in this diagram. The PO2 values in any region are the result of the interactions of local diffusion and consumption as found in numerous computational modeling studies. This figure originally appeared in Ellsworth et al (40).
Acknowledgments
The author expresses his appreciation to Jeff Frisbee, Editor of Microcirculation, for the invitation to prepare this manuscript as an expanded version of remarks presented on the occasion of the 2012 Eugene M. Landis Award of the Microcirculatory Society. The author gratefully acknowledges the contributions of Brian Duling, who introduced him to the field of microcirculation, Aleksander Popel, with whom he has closely collaborated for over 30 years, Mary Ellsworth and Christopher Ellis, who have been outstanding collaborators on many projects, and to Aleksander Golub, without whom the measurement of oxygen in the microcirculation by the phosphorescence quenching technique would not have matured to its present state. All of these individuals have provided unwavering support, inspiration and insight during my personal scientific journey to understand the secrets of the small, but so important, molecule oxygen. In addition, my thanks go out to the many graduate students, postdoctoral scientists and other faculty colleagues whose contributions to our collective research efforts have been a constant source of pride and promise for the future.
The work conducted in our laboratory has been made possible by the generous support of the National Heart, Lung and Blood Institute (grant HL18292), the American Heart Association and the Department of Defense.
Abbreviations used
- RBC
red blood cell
- Hct
hematocrit
- Hb
hemoglobin
- Mb
myoglobin
- PO2
oxygen tension
- SO2
hemoglobin oxygen saturation
- PQM
phosphorescence quenching microscopy
- ATP
adenosine 5′-triphosphate
- ISF
interstitial fluid
- VO2
oxygen consumption
References
- 1.Al-Khazraji BK, Novielli NM, Goldman D, Medeiros PJ, Jackson DN. A simple “streak length method” for quantifying and characterizing red blood cell velocity profiles and blood flow in rat skeletal muscle arterioles. Microcirculation. 2012;19:327–35. doi: 10.1111/j.1549-8719.2012.00165.x. [DOI] [PubMed] [Google Scholar]
- 2.Alders DJ, Groeneveld AB, de Kanter FJ, van Beek JH. Myocardial O2 consumption in porcine left ventricle is heterogeneously distributed in parallel to heterogeneous O2 delivery. Am J Physiol Heart Circ Physiol. 2004;287:H1353–H1361. doi: 10.1152/ajpheart.00338.2003. [DOI] [PubMed] [Google Scholar]
- 3.Baker M, Wayland H. On-line volume flow rate and velocity profile measurement for blood in microvessels. Microvasc Res. 1974;7:131–143. doi: 10.1016/0026-2862(74)90043-0. [DOI] [PubMed] [Google Scholar]
- 4.Barker MC, Golub AS, Pittman RN. Erythrocyte-associated transients in capillary PO2: an isovolemic hemodilution study in the rat spinotrapezius muscle. Am J Physiol Heart Circ Physiol. 2007;292:H2540–H2549. doi: 10.1152/ajpheart.00915.2006. [DOI] [PubMed] [Google Scholar]
- 5.Behnke BJ, Delp MD, McDonough P, Spier SA, Poole DC, Musch TI. Effects of chronic heart failure on microvascular oxygen exchange dynamics in muscles of contrasting fiber type. Cardiovasc Res. 2004;61:325–332. doi: 10.1016/j.cardiores.2003.11.020. [DOI] [PubMed] [Google Scholar]
- 6.Behnke BJ, Barstow TJ, Kindig CA, McDonough P, Musch TI, Poole DC. Dynamics of oxygen uptake following exercise onset in rat skeletal muscle. Respir Physiol & Neurobiol. 2002;133:229–239. doi: 10.1016/s1569-9048(02)00183-0. [DOI] [PubMed] [Google Scholar]
- 7.Behnke BJ, Kindig CA, Musch TI, Koga S, Poole DC. Dynamics of microvascular oxygen pressure across the rest-exercise transition in rat skeletal muscle. Respir Physiol. 2001;126:53–63. doi: 10.1016/s0034-5687(01)00195-5. [DOI] [PubMed] [Google Scholar]
- 8.Bennett RAO, Pittman RN, Sullivan SM. Capillary spatial pattern and muscle fiber geometry in three hamster striated muscles. Amer J Physiol. 1991;260:H579–H585. doi: 10.1152/ajpheart.1991.260.2.H579. [DOI] [PubMed] [Google Scholar]
- 9.Bentley TB, Meng H, Pittman RN. Temperature dependence of oxygen diffusion and consumption in mammalian striated muscle. Am J Physiol. 1993;264:H1825–H1830. doi: 10.1152/ajpheart.1993.264.6.H1825. [DOI] [PubMed] [Google Scholar]
- 10.Bentley TB, Pittman RN. Influence of temperature on oxygen diffusion in hamster retractor muscle. Am J Physiol. 1997;272:H1106–H1112. doi: 10.1152/ajpheart.1997.272.3.H1106. [DOI] [PubMed] [Google Scholar]
- 11.Bloch EH. A quantitative study of the hemodynamics in the living microvascular system. Am J Anat. 1962;110:125–153. doi: 10.1002/aja.1001100204. [DOI] [PubMed] [Google Scholar]
- 12.Bohlen HG. Mechanism of increased vessel wall nitric oxide concentrations during intestinal absorption. Am J Physiol. 1998;275:H542–H550. doi: 10.1152/ajpheart.1998.275.2.H542. [DOI] [PubMed] [Google Scholar]
- 13.Borders JL, Granger HJ. An optical Doppler intravital velocimeter. Microvasc Res. 1984;27:117–127. doi: 10.1016/0026-2862(84)90047-5. [DOI] [PubMed] [Google Scholar]
- 14.Boron WF, Boulpaep EL. Medical Physiology. Philadelphia: Saunders; 2003. [Google Scholar]
- 15.Brown GC. Nitric oxide and mitochondrial respiration. Biochim Biophys Acta. 1999;1411:351–369. doi: 10.1016/s0005-2728(99)00025-0. [DOI] [PubMed] [Google Scholar]
- 16.Buerk DG. Measuring tissue PO2 with microelectrodes. Methods Enzymol. 2004;381:665–690. doi: 10.1016/S0076-6879(04)81043-7. [DOI] [PubMed] [Google Scholar]
- 17.Buerk DG. Mathematical modeling of the interaction between oxygen, nitric oxide and superoxide. Adv Exp Med Biol. 2009;645:7–12. doi: 10.1007/978-0-387-85998-9_2. [DOI] [PubMed] [Google Scholar]
- 18.Carvalho H, Pittman RN. Longitudinal and radial gradients of PO2 in the hamster cheek pouch microcirculation. Microcirculation. 2008;15:215–224. doi: 10.1080/10739680701616175. [DOI] [PubMed] [Google Scholar]
- 19.Chapler CK, Cain SM. The physiologic reserve in oxygen carrying capacity: studies in experimental hemodilution. Can J Physiol Pharmacol. 1986;64:7–12. doi: 10.1139/y86-002. [DOI] [PubMed] [Google Scholar]
- 20.Chen K, Piknova B, Pittman RN, Schechter AN, Popel AS. Nitric oxide from nitrite reduction by hemoglobin in the plasma and erythrocytes. Nitric Oxide. 2008;18:47–60. doi: 10.1016/j.niox.2007.09.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen K, Pittman RN, Popel AS. Vascular smooth muscle NO exposure from intraerythrocytic SNOHb: A mathematical model. Antioxid Redox Signaling. 2007;9:1097–1110. doi: 10.1089/ars.2007.1594. [DOI] [PubMed] [Google Scholar]
- 22.Chen K, Pittman RN, Popel AS. Nitric oxide in the vasculature: Where does it come from, and where does it go? A quantitative perspective. Antioxid Redox Signaling. 2008;10:1185–1198. doi: 10.1089/ars.2007.1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Crawford JH, Isbell TS, Huang Z, Shiva S, Chacko BK, Schechter AN, Darley-Usmar VM, Kerby JD, Lang JD, Jr, Kraus D, Ho C, Gladwin MT, Patel RP. Hypoxia, red blood cells, and nitrite regulate NO-dependent hypoxic vasodilation. Blood. 2006;107:566–574. doi: 10.1182/blood-2005-07-2668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davis MJ, Hill MA, Kuo L. Local regulation of microvascular perfusion. In: Tuma RF, Duran WN, Ley K, editors. Handbook of physiology: Microcirculation. 2. San Diego, CA: Elsevier; 2008. pp. 161–284. [Google Scholar]
- 25.Detar R, Bohr DF. Oxygen and vascular smooth muscle contraction. Am J Physiol. 1968;214:241–244. doi: 10.1152/ajplegacy.1968.214.2.241. [DOI] [PubMed] [Google Scholar]
- 26.Duling BR. Microvascular responses to alterations in oxygen tension. Circ Res. 1972;31:481–489. doi: 10.1161/01.res.31.4.481. [DOI] [PubMed] [Google Scholar]
- 27.Duling BR. Changes in microvascular diameter and oxygen tension induced by carbon dioxide. Circ Res. 1973;32:370–376. doi: 10.1161/01.res.32.3.370. [DOI] [PubMed] [Google Scholar]
- 28.Duling BR. Oxygen sensitivity of vascular smooth muscle. II. In vivo studies. Am J Physiol. 1974;227:42–49. doi: 10.1152/ajplegacy.1974.227.1.42. [DOI] [PubMed] [Google Scholar]
- 29.Duling BR. Oxygen, metabolism and microcirculatory control. In: Kaley G, Altura BM, editors. Microcirculation. II. Baltimore: Univ Park Press; 1978. pp. 401–429. [Google Scholar]
- 30.Duling BR, Berne RM. Longitudinal gradients in periarteriolar oxygen tension. A possible mechanism for the participation of oxygen in local regulation of blood flow. Circ Res. 1970;27:669–678. doi: 10.1161/01.res.27.5.669. [DOI] [PubMed] [Google Scholar]
- 31.Duling BR, Damon DN, Donaldson SR, Pittman RN. A computerized system for densitometric analysis of the microcirculation. J Appl Physiol. 1983;55:642–651. doi: 10.1152/jappl.1983.55.2.642. [DOI] [PubMed] [Google Scholar]
- 32.Duling BR, Kuschinsky W, Wahl M. Measurements of the perivascular PO2 in the vicinity of the pial vessels of the cat. Pflugers Arch. 1979;383:29–34. doi: 10.1007/BF00584471. [DOI] [PubMed] [Google Scholar]
- 33.Duling BR, Pittman RN. Oxygen tension: dependent or independent variable in local control of blood flow? Fed Proc. 1975;34:2012–2019. [PubMed] [Google Scholar]
- 34.Dutta A, Wang L, Meng H, Pittman RN, Popel AS. Oxygen tension profiles in isolated hamster retractor muscle at different temperatures. Microvasc Res. 1996;51:288–302. doi: 10.1006/mvre.1996.0028. [DOI] [PubMed] [Google Scholar]
- 35.Eggleton CD, Roy TK, Popel AS. Predictions of capillary oxygen transport in the presence of fluorocarbon additives. Am J Physiol. 1998;275:H2250–H2257. doi: 10.1152/ajpheart.1998.275.6.H2250. [DOI] [PubMed] [Google Scholar]
- 36.Ellis CG, Ellsworth ML, Pittman RN. Application of image analysis for evaluation of red blood cell dynamics in capillaries. Microvasc Res. 1992;44:214–225. doi: 10.1016/0026-2862(92)90081-y. [DOI] [PubMed] [Google Scholar]
- 37.Ellis CG, Ellsworth ML, Pittman RN. Determination of red blood cell oxygenation in vivo by dual video densitometric image analysis. Am J Physiol. 1990;258:H1216–H1223. doi: 10.1152/ajpheart.1990.258.4.H1216. [DOI] [PubMed] [Google Scholar]
- 38.Ellis CG, Fraser S, Hamilton G, Groom AC. Measurement of the lineal density of red blood cells in capillaries in vivo, using a computerized frame-by-frame analysis of video images. Microvasc Res. 1984;27:1–13. doi: 10.1016/0026-2862(84)90037-2. [DOI] [PubMed] [Google Scholar]
- 39.Ellsworth ML, Ellis CG, Goldman D, Stephenson AH, Dietrich HH, Sprague RS. Erythrocytes: oxygen sensors and modulators of vascular tone. Physiology (Bethesda) 2009;24:107–116. doi: 10.1152/physiol.00038.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ellsworth ML, Ellis CG, Popel AS, Pittman RN. Role of microvessels in oxygen supply to tissue. Physiology. 1994;9:119–123. doi: 10.1152/physiologyonline.1994.9.3.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ellsworth ML, Forrester T, Ellis CG, Dietrich HH. The erythrocyte as a regulator of vascular tone. Am J Physiol. 1995;269:H2155–2161. doi: 10.1152/ajpheart.1995.269.6.H2155. [DOI] [PubMed] [Google Scholar]
- 42.Ellsworth ML, Liu A, Dawant B, Popel AS, Pittman RN. Analysis of vascular pattern and dimensions in arteriolar networks of the retractor muscle in young hamsters. Microvasc Res. 1987;34:168–183. doi: 10.1016/0026-2862(87)90051-3. [DOI] [PubMed] [Google Scholar]
- 43.Ellsworth ML, Pittman RN. Heterogeneity of oxygen diffusion through hamster striated muscles. Am J Physiol. 1984;246:H161–167. doi: 10.1152/ajpheart.1984.246.2.H161. [DOI] [PubMed] [Google Scholar]
- 44.Ellsworth ML, Pittman RN. Evaluation of photometric methods for quantifying convective mass transport in microvessels. Am J Physiol. 1986;251:H869–H879. doi: 10.1152/ajpheart.1986.251.4.H869. [DOI] [PubMed] [Google Scholar]
- 45.Ellsworth ML, Pittman RN. Arterioles supply oxygen to capillaries by diffusion as well as by convection. Am J Physiol. 1990;258:H1240–1243. doi: 10.1152/ajpheart.1990.258.4.H1240. [DOI] [PubMed] [Google Scholar]
- 46.Ellsworth ML, Pittman RN, Ellis CG. Measurement of hemoglobin oxygen saturation in capillaries. Amer J Physiol. 1987;252:H1031–H1040. doi: 10.1152/ajpheart.1987.252.5.H1031. [DOI] [PubMed] [Google Scholar]
- 47.Ellsworth ML, Popel AS, Pittman RN. Assessment and impact of heterogeneities of convective oxygen transport parameters in capillaries of striated muscle: experimental and theoretical. Microvasc Res. 1988;35:341–362. doi: 10.1016/0026-2862(88)90089-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Falcone JC, Bohlen HG. EDRF from rat intestine and skeletal muscle venules causes dilation of arterioles. Am J Physiol. 1990;258:H1515–H1523. doi: 10.1152/ajpheart.1990.258.5.H1515. [DOI] [PubMed] [Google Scholar]
- 49.Federspiel WJ, Popel AS. A theoretical analysis of the effect of the particulate nature of blood on oxygen release in capillaries. Microvasc Res. 1986;32:164–189. doi: 10.1016/0026-2862(86)90052-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Federspiel WJ, Sarelius IH. An examination of the contribution of red cell spacing to the uniformity of oxygen flux at the capillary wall. Microvasc Res. 1984;27:273–285. doi: 10.1016/0026-2862(84)90059-1. [DOI] [PubMed] [Google Scholar]
- 51.Fraser GM, Goldman D, Ellis CG. Microvascular flow modeling using in vivo hemodynamic measurements in reconstructed 3D capillary networks. Microcirculation. 2012;19:510–520. doi: 10.1111/j.1549-8719.2012.00178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fraser GM, Milkovich S, Goldman D, Ellis CG. Mapping 3-D functional capillary geometry in rat skeletal muscle in vivo. Am J Physiol Heart Circ Physiol. 2012;302:H654–H664. doi: 10.1152/ajpheart.01185.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Frisbee JC, Roman RJ, Krishna UM, Falck JR, Lombard JH. Relative contributions of cyclooxygenase- and cytochrome P450 omega-hydroxylase-dependent pathways to hypoxic dilation of skeletal muscle resistance arteries. J Vasc Res. 2001;38:305–314. doi: 10.1159/000051061. [DOI] [PubMed] [Google Scholar]
- 54.Goldman D, Popel AS. A computational study of the effect of vasomotion on oxygen transport from capillary networks. J Theor Biol. 2001;209:189–199. doi: 10.1006/jtbi.2000.2254. [DOI] [PubMed] [Google Scholar]
- 55.Golub AS, Pittman RN. Recovery of radial PO2 profiles from phosphorescence quenching measurements in microvessels. Comp Biochem Physiol A Mol Integr Physiol. 2002;132:169–176. doi: 10.1016/s1095-6433(01)00544-x. [DOI] [PubMed] [Google Scholar]
- 56.Golub AS, Pittman RN. Erythrocyte-associated transients in PO2 revealed in capillaries of rat mesentery. Am J Physiol Heart Circ Physiol. 2005;288:H2735–H2743. doi: 10.1152/ajpheart.00711.2004. [DOI] [PubMed] [Google Scholar]
- 57.Golub AS, Pittman RN. PO2 measurements in the microcirculation using phosphorescence quenching microscopy at high magnification. Am J Physiol Heart Circ Physiol. 2008;294:H2905–H2916. doi: 10.1152/ajpheart.01347.2007. [DOI] [PubMed] [Google Scholar]
- 58.Golub AS, Pittman RN. Oxygen dependence of respiration in rat spinotrapezius muscle in situ. Am J Physiol Heart Circ Physiol. 2012;303:H47–H56. doi: 10.1152/ajpheart.00131.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Golub AS, Barker MC, Pittman RN. PO2 profiles near arterioles and tissue oxygen consumption in the rat mesentery. Am J Physiol Heart Circ Physiol. 2007;293:H1097–H1106. doi: 10.1152/ajpheart.00077.2007. [DOI] [PubMed] [Google Scholar]
- 60.Golub AS, Barker MC, Pittman RN. Microvascular oxygen tension in the rat mesentery. Am J Physiol Heart Circ Physiol. 2008;294:H21–H28. doi: 10.1152/ajpheart.00861.2007. [DOI] [PubMed] [Google Scholar]
- 61.Golub AS, Popel AS, Zheng L, Pittman RN. Analysis of phosphorescence in heterogeneous systems using distributions of quencher concentration. Biophys J. 1997;73:452–465. doi: 10.1016/S0006-3495(97)78084-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Golub AS, Popel AS, Zheng L, Pittman RN. Analysis of phosphorescence decay in heterogeneous systems: consequences of finite excitation flash duration. Photochem Photobiol. 1999;69:624–632. [PubMed] [Google Scholar]
- 63.Golub AS, Song BK, Pittman RN. The rate of oxygen loss from mesenteric arterioles is not unusually high. Am J Physiol Heart Circ Physiol. 2011;301:H737–H745. doi: 10.1152/ajpheart.00353.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Golub AS, Tevald MA, Pittman RN. Phosphorescence quenching micro-respirometry of skeletal muscle in situ. Am J Physiol Heart Circ Physiol. 2011;300:H135–H143. doi: 10.1152/ajpheart.00626.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gutierrez G. The rate of oxygen release and its effect on capillary O2 tension: a mathematical analysis. Respir Physiol. 1986;63:79–96. doi: 10.1016/0034-5687(86)90032-0. [DOI] [PubMed] [Google Scholar]
- 66.Hall CN, Garthwaite J. What is the real physiological NO concentration in vivo? Nitric Oxide. 2009;21:92–103. doi: 10.1016/j.niox.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hellums JD. The resistance to oxygen transport in the capillaries relative to that in the surrounding tissue. Microvasc Res. 1977;13:131–136. doi: 10.1016/0026-2862(77)90122-4. [DOI] [PubMed] [Google Scholar]
- 68.Hellums JD, Nair PK, Huang NS, Ohshima N. Simulation of intraluminal gas transport processes in the microcirculation. Ann Biomed Eng. 1996;24:1–24. doi: 10.1007/BF02770991. [DOI] [PubMed] [Google Scholar]
- 69.Hester RL. Uptake of metabolites by postcapillary venules: Mechanism for the control of arteriolar diameter. Microvasc Res. 1993;46:254–261. doi: 10.1006/mvre.1993.1050. [DOI] [PubMed] [Google Scholar]
- 70.Hogan MC, Bebout DE, Wagner PD. Effect of hemoglobin concentration on maximal O2 uptake in canine gastrocnemius muscle in situ. J Appl Physiol. 1991;70:1105–1112. doi: 10.1152/jappl.1991.70.3.1105. [DOI] [PubMed] [Google Scholar]
- 71.Hogan MC, Willford DC, Keipert PE, Faithfull NS, Wagner PD. Increased plasma O2 solubility improves O2 uptake of in situ dog muscle working maximally. J Appl Physiol. 1992;73:2470–2475. doi: 10.1152/jappl.1992.73.6.2470. [DOI] [PubMed] [Google Scholar]
- 72.Homer LD, Weathersby PK, Kiesow LA. Oxygen gradients between red blood cells in the microcirculation. Microvasc Res. 1981;22:308–323. doi: 10.1016/0026-2862(81)90099-6. [DOI] [PubMed] [Google Scholar]
- 73.Honig CR, Gayeski TE. Comparison of intracellular PO2 and conditions for blood-tissue O2 transport in heart and working red skeletal muscle. Adv Exp Med Biol. 1987;215:309–321. doi: 10.1007/978-1-4684-7433-6_36. [DOI] [PubMed] [Google Scholar]
- 74.Intaglietta M, Tompkins WR, Richardson DR. Velocity measurements in the microvasculature of the cat omentum by on-line method. Microvasc Res. 1970;2:462–473. doi: 10.1016/0026-2862(70)90039-7. [DOI] [PubMed] [Google Scholar]
- 75.Ivanov KP, Derry AN, Vovenko EP, Samoilov MO, Semionov DG. Direct measurements of oxygen tension at the surface of arterioles, capillaries and venules of the cerebral cortex. Pflugers Arch. 1982;393:118–120. doi: 10.1007/BF00582403. [DOI] [PubMed] [Google Scholar]
- 76.Jackson WF. Arteriolar oxygen reactivity: where is the sensor? Am J Physiol. 1987;253:H1120–1126. doi: 10.1152/ajpheart.1987.253.5.H1120. [DOI] [PubMed] [Google Scholar]
- 77.Jackson WF, Duling BR. The oxygen sensitivity of hamster cheek pouch arterioles. In vitro and in situ studies. Circ Res. 1983;53:515–525. doi: 10.1161/01.res.53.4.515. [DOI] [PubMed] [Google Scholar]
- 78.Japee SA, Ellis CG, Pittman RN. Flow visualization tools for image analysis of capillary networks. Microcirculation. 2004;11:39–54. doi: 10.1080/10739680490266171. [DOI] [PubMed] [Google Scholar]
- 79.Japee SA, Pittman RN, Ellis CG. A new video image analysis system to study red blood cell dynamics and oxygenation in capillary networks. Microcirculation. 2005;12:489–506. doi: 10.1080/10739680591003332. [DOI] [PubMed] [Google Scholar]
- 80.Japee SA, Pittman RN, Ellis CG. Automated method for tracking individual red blood cells within capillaries to compute velocity and oxygen saturation. Microcirculation. 2005;12:507–515. doi: 10.1080/10739680591003341. [DOI] [PubMed] [Google Scholar]
- 81.Jobsis FF. Basic processes in cellular respiration. In: Fenn WO, Rahn H, editors. Handbook of Physiology. Vol. 1. Washington, DC: Am Physiol Soc; 1964. pp. 63–124. sec 3. [Google Scholar]
- 82.Johnson PC. Renaissance in the microcirculation. Circ Res. 1972;31:817–823. doi: 10.1161/01.res.31.6.817. [DOI] [PubMed] [Google Scholar]
- 83.Johnson PC. The myogenic response. In: Bohr DF, Somlyo AP, Sparks HV Jr, editors. Handbook of Physiology; The Cardiovascular System; Vascular Smooth Muscle. Bethesda, MD: American Physiological Society; 1980. pp. 409–442. [Google Scholar]
- 84.Joyner MJ, Wilkins BW. Exercise hyperaemia: is anything obligatory but the hyperaemia? J Physiol. 2007;583:855–860. doi: 10.1113/jphysiol.2007.135889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kashiwagi S, Kajimura M, Yoshimura Y, Suematsu M. Nonendothelial source of nitric oxide in arterioles but not in venules: alternative source revealed in vivo by diaminofluorescein microfluorography. Circ Res. 2002;91:e55–64. doi: 10.1161/01.res.0000047529.26278.4d. [DOI] [PubMed] [Google Scholar]
- 86.Kavdia M, Pittman RN, Popel AS. Theoretical analysis of blood substitute affinity and cooperativity effects on organ oxygen transport. J Appl Physiol. 2002;93:2122–2128. doi: 10.1152/japplphysiol.00676.2002. [DOI] [PubMed] [Google Scholar]
- 87.Kerger H, Torres Filho IP, Rivas M, Winslow RM, Intaglietta M. Systemic and subcutaneous microvascular oxygen tension in conscious Syrian golden hamsters. Am J Physiol. 1995;268:H802–H810. doi: 10.1152/ajpheart.1995.268.2.H802. [DOI] [PubMed] [Google Scholar]
- 88.Kim S, Kong RL, Popel AS, Intaglietta M, Johnson PC. Temporal and spatial variations of cell-free layer width in arterioles. Am J Physiol Heart Circ Physiol. 2007;293:H1526–H1535. doi: 10.1152/ajpheart.01090.2006. [DOI] [PubMed] [Google Scholar]
- 89.Kim S, Ong PK, Yalcin O, Intaglietta M, Johnson PC. The cell-free layer in microvascular blood flow. Biorheology. 2009;46:181–189. doi: 10.3233/BIR-2009-0530. [DOI] [PubMed] [Google Scholar]
- 90.Kobayashi H, Takizawa N. Oxygen saturation and pH changes in cremaster microvessels of the rat. Am J Physiol. 1996;270:H1453–H1461. doi: 10.1152/ajpheart.1996.270.4.H1453. [DOI] [PubMed] [Google Scholar]
- 91.Kobayashi H, Takizawa N. Imaging of oxygen transfer among microvessels of rat cremaster muscle. Circulation. 2002;105:1713–1719. doi: 10.1161/01.cir.0000013783.63773.8f. [DOI] [PubMed] [Google Scholar]
- 92.Koller A, Dornyei G, Kaley G. Flow-induced responses in skeletal muscle venules: Modulation by nitric oxide and prostaglandins. Am J Physiol. 1998;275:H831–H836. doi: 10.1152/ajpheart.1998.275.3.H831. [DOI] [PubMed] [Google Scholar]
- 93.Krogh A. The rate of diffusion of gases through animal tissues with some remarks on the coefficient of invasion. J Physiol. 1919;52:391–408. doi: 10.1113/jphysiol.1919.sp001838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Krogh A. The number and distribution of capillaries in muscles with calculations of the oxygen pressure head necessary for supplying the tissue. J Physiol. 1919;52:409–415. doi: 10.1113/jphysiol.1919.sp001839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Krogh A. The Anatomy and Physiology of Capillaries. New York: Hafner Publishing; 1959. [Google Scholar]
- 96.Kuo L, Pittman RN. Effect of hemodilution on oxygen transport in arteriolar networks of hamster striated muscle. Am J Physiol. 1988;254:H331–339. doi: 10.1152/ajpheart.1988.254.2.H331. [DOI] [PubMed] [Google Scholar]
- 97.Kuo L, Pittman RN. Influence of hemoconcentration on arteriolar oxygen transport in hamster striated muscle. Am J Physiol. 1990;259:H1694–1702. doi: 10.1152/ajpheart.1990.259.6.H1694. [DOI] [PubMed] [Google Scholar]
- 98.Lash JM, Bohlen HG. Excess oxygen delivery during muscle contractions in spontaneously hypertensive rats. J Appl Physiol. 1995;78:101–111. doi: 10.1152/jappl.1995.78.1.101. [DOI] [PubMed] [Google Scholar]
- 99.Lash JM, Bohlen HG. Perivascular and tissue PO2 in contracting rat spinotrapezius muscle. Am J Physiol. 1987;252:H1192–1202. doi: 10.1152/ajpheart.1987.252.6.H1192. [DOI] [PubMed] [Google Scholar]
- 100.Lecoq J, Parpaleix A, Roussakis E, Ducros M, Houssen YG, Vinogradov SA, Charpak S. Simultaneous two-photon imaging of oxygen and blood flow in deep cerebral vessels. Nat Med. 2011;17:893–898. doi: 10.1038/nm.2394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lipowsky HH, Zweifach BW. Application of the “two-slit” photometric technique to the measurement of microvascular volumetric flow rates. Microvasc Res. 1978;15:93–101. doi: 10.1016/0026-2862(78)90009-2. [DOI] [PubMed] [Google Scholar]
- 102.Lipowsky HH, Usami S, Chien S, Pittman RN. Hematocrit determination in small bore tubes by differential spectrophotometry. Microvasc Res. 1982;24:42–55. doi: 10.1016/0026-2862(82)90041-3. [DOI] [PubMed] [Google Scholar]
- 103.Lombard JH, Liu Y, Fredricks KT, Bizub DM, Roman RJ, Rusch NJ. Electrical and mechanical responses of rat middle cerebral arteries to reduced PO2 and prostacyclin. Am J Physiol. 1999;276:H509–H516. doi: 10.1152/ajpheart.1999.276.2.H509. [DOI] [PubMed] [Google Scholar]
- 104.Mathieu-Costello O, Ellis CG, Potter RF, MacDonald IC, Groom AC. Muscle capillary-to-fiber perimeter ratio: morphometry. Am J Physiol. 1991;261:H1617–H1625. doi: 10.1152/ajpheart.1991.261.5.H1617. [DOI] [PubMed] [Google Scholar]
- 105.Meng H, Bentley TB, Pittman RN. Oxygen diffusion in hamster striated muscle: comparison of in vitro and near in vivo conditions. Am J Physiol. 1992;263:H35–39. doi: 10.1152/ajpheart.1992.263.1.H35. [DOI] [PubMed] [Google Scholar]
- 106.Meng H, Bentley TB, Pittman RN. Myoglobin content of hamster skeletal muscles. J Appl Physiol. 1993;74:2194–2197. doi: 10.1152/jappl.1993.74.5.2194. [DOI] [PubMed] [Google Scholar]
- 107.Mik EG, Stap J, Sinaasappel M, Beek JF, Aten JA, van Leeuwen TG, Ince C. Mitochondrial PO2 measured by delayed fluorescence of endogenous protoporphyrin IX. Nat Methods. 2006;3:939–945. doi: 10.1038/nmeth940. [DOI] [PubMed] [Google Scholar]
- 108.Mik EG, Johannes T, Zuurbier CJ, Heinen A, Houben-Weerts JH, Balestra GM, Stap J, Beek JF, Ince C. In vivo mitochondrial oxygen tension measured by a delayed fluorescence lifetime technique. Biophys J. 2008;95:3977–3990. doi: 10.1529/biophysj.107.126094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Millikan GA. The kinetics of blood pigments: haemocyanin and haemoglobin. J Physiol. 1933;79:158–179. doi: 10.1113/jphysiol.1933.sp003037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nase GP, Tuttle J, Bohlen HG. Reduced perivascular PO2 increases nitric oxide release from endothelial cells. Am J Physiol Heart Circ Physiol. 2003;285:H507–H515. doi: 10.1152/ajpheart.00759.2002. [DOI] [PubMed] [Google Scholar]
- 111.Nilsson NJ. Oximetry. Physiol Rev. 1960;40:1–26. doi: 10.1152/physrev.1960.40.1.1. [DOI] [PubMed] [Google Scholar]
- 112.Olson JS, Foley EW, Rogge C, Tsai AL, Doyle MP, Lemon DD. NO scavenging and the hypertensive effect of hemoglobin-based blood substitutes. Free Radic Biol Med. 2004;36:685–697. doi: 10.1016/j.freeradbiomed.2003.11.030. [DOI] [PubMed] [Google Scholar]
- 113.Page TC, Light WR, Hellums JD. Prediction of microcirculatory oxygen transport by erythrocyte/hemoglobin solution mixtures. Microvasc Res. 1998;56:113–126. doi: 10.1006/mvre.1998.2088. [DOI] [PubMed] [Google Scholar]
- 114.Page TC, Light WR, McKay CB, Hellums JD. Oxygen transport by erythrocyte/hemoglobin solution mixtures in an in vitro capillary as a model of hemoglobin-based oxygen carrier performance. Microvasc Res. 1998;55:54–64. doi: 10.1006/mvre.1997.2055. [DOI] [PubMed] [Google Scholar]
- 115.Parthasarathi AA, Japee SA, Pittman RN. Determination of red blood cell velocity by video shuttering and image analysis. Annals of Biomed Eng. 1999;27:313–325. doi: 10.1114/1.144. [DOI] [PubMed] [Google Scholar]
- 116.Patel S, Pittman RN. Mathematical analysis of hemoglobin spectrophotometry in microvessels. Microvasc Res. 2001;62:63–73. doi: 10.1006/mvre.2001.2310. [DOI] [PubMed] [Google Scholar]
- 117.Patel S, Pittman RN. Impact of microscope numerical aperture on microspectrophotometric measurements of hemoglobin in microvessels. Microvasc Res. 2002;64:198–206. doi: 10.1006/mvre.2002.2416. [DOI] [PubMed] [Google Scholar]
- 118.Pittman RN. Influence of oxygen lack on vascular smooth muscle contraction. In: Vanhoutte PM, Leusen I, editors. Vasodilatation. New York: Raven Press; 1981. pp. 183–193. [Google Scholar]
- 119.Pittman RN. In vivo photometric analysis of hemoglobin. Ann Biomed Eng. 1986;14:119–137. doi: 10.1007/BF02584263. [DOI] [PubMed] [Google Scholar]
- 120.Pittman RN. Microvessel blood oxygen measurement techniques. In: Baker CH, Nastuk WL, editors. Microvascular Technology. Orlando, Florida: Academic Press; 1986. pp. 367–389. [Google Scholar]
- 121.Pittman RN. Interaction between oxygen and the blood vessel wall. Can J Cardiol. 1986;2:124–131. [PubMed] [Google Scholar]
- 122.Pittman RN. Influence of microvascular architecture on oxygen exchange in skeletal muscle. Microcirculation. 1995;2:1–18. doi: 10.3109/10739689509146755. [DOI] [PubMed] [Google Scholar]
- 123.Pittman RN. Oxygen supply to contracting skeletal muscle at the microcirculatory level: Diffusion vs. convection. Acta Physiol Scand. 2000;168:593–602. doi: 10.1046/j.1365-201x.2000.00710.x. [DOI] [PubMed] [Google Scholar]
- 124.Pittman RN. Oxygen transport and exchange in the microcirculation. Microcirculation. 2005;12:59–70. doi: 10.1080/10739680590895064. [DOI] [PubMed] [Google Scholar]
- 125.Pittman RN. Oxygen gradients in the microcirculation. Acta Physiologica. 2011;202:311–322. doi: 10.1111/j.1748-1716.2010.02232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Pittman RN. Regulation of tissue oxygenation. San Rafael, CA: Morgan & Claypool Life Sciences; 2011. [PubMed] [Google Scholar]
- 127.Pittman RN, Duling BR. Oxygen sensitivity of vascular smooth muscle. I. In vitro studies. Microvasc Res. 1973;6:202–211. doi: 10.1016/0026-2862(73)90020-4. [DOI] [PubMed] [Google Scholar]
- 128.Pittman RN, Duling BR. A new method for the measurement of percent oxyhemoglobin. J Appl Physiol. 1975;38:315–320. doi: 10.1152/jappl.1975.38.2.315. [DOI] [PubMed] [Google Scholar]
- 129.Pittman RN, Duling BR. Measurement of percent oxyhemoglobin in the microvasculature. J Appl Physiol. 1975;38:321–327. doi: 10.1152/jappl.1975.38.2.321. [DOI] [PubMed] [Google Scholar]
- 130.Pittman RN, Duling BR. Effects of altered carbon dioxide tension on hemoglobin oxygenation in hamster cheek pouch microvessels. Microvasc Res. 1977;13:211–224. doi: 10.1016/0026-2862(77)90086-3. [DOI] [PubMed] [Google Scholar]
- 131.Pittman RN, Ellsworth ML. Estimation of red cell flow in microvessels: consequences of the Baker-Wayland spatial averaging model. Microvasc Res. 1986;32:371–388. doi: 10.1016/0026-2862(86)90072-5. [DOI] [PubMed] [Google Scholar]
- 132.Pittman RN, Golub AS, Popel AS, Zheng L. Interpretation of phosphorescence quenching measurements made in the presence of oxygen gradients. Adv Exp Med Biol. 1998;454:375–383. doi: 10.1007/978-1-4615-4863-8_45. [DOI] [PubMed] [Google Scholar]
- 133.Pittman RN, Golub AS, Schleicher WF. Rate of decrease of PO2 from an arteriole with arrested flow. Adv Exp Med Biol. 2005;566:257–262. doi: 10.1007/0-387-26206-7_34. [DOI] [PubMed] [Google Scholar]
- 134.Poole DC, Copp SW, Hirai DM, Musch TI. Dynamics of muscle microcirculatory and blood-myocyte O2 flux during contractions. Acta Physiol (Oxf) 2011;202:293–310. doi: 10.1111/j.1748-1716.2010.02246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Poole DC, Kindig CA, Behnke BJ. Effects of emphysema on diaphragm microvascular oxygen pressure. Am J Respir Crit Care Med. 2001;163:1081–1086. doi: 10.1164/ajrccm.163.5.2008065. [DOI] [PubMed] [Google Scholar]
- 136.Popel AS. Theory of oxygen transport to tissue. Crit Rev Biomed Eng. 1989;17:257–321. [PMC free article] [PubMed] [Google Scholar]
- 137.Popel AS, Goldman D, Vadapalli A. Modeling of oxygen diffusion from the blood vessels to intracellular organelles. Adv Exp Med Biol. 2003;530:485–495. doi: 10.1007/978-1-4615-0075-9_46. [DOI] [PubMed] [Google Scholar]
- 138.Popel AS, Gross JF. Analysis of oxygen diffusion from arteriolar networks. Am J Physiol. 1979;237:H681–689. doi: 10.1152/ajpheart.1979.237.6.H681. [DOI] [PubMed] [Google Scholar]
- 139.Popel AS, Pittman RN, Ellsworth ML. Rate of oxygen loss from arterioles is an order of magnitude higher than expected. Am J Physiol. 1989;256:H921–924. doi: 10.1152/ajpheart.1989.256.3.H921. [DOI] [PubMed] [Google Scholar]
- 140.Popel AS, Pries AR, Slaaf DW. Microcirculation Physiome Project. J Vasc Res. 1999;36:253–255. doi: 10.1159/000025649. [DOI] [PubMed] [Google Scholar]
- 141.Pries AR, Secomb TW, Gaehtgens P. Structure and hemodynamics of microvascular networks: heterogeneity and correlations. Am J Physiol. 1995;269:H1713–H1722. doi: 10.1152/ajpheart.1995.269.5.H1713. [DOI] [PubMed] [Google Scholar]
- 142.Pries AR, Secomb TW. Microcirculatory network structures and models. Ann Biomed Eng. 2000;28:916–921. doi: 10.1114/1.1308495. [DOI] [PubMed] [Google Scholar]
- 143.Pries AR, Secomb TW, Gaehtgens P. The endothelial surface layer. Pflugers Arch. 2000;440:653–666. doi: 10.1007/s004240000307. [DOI] [PubMed] [Google Scholar]
- 144.Roy TK, Pries AR, Secomb TW. Theoretical comparison of wall-derived and erythrocyte-derived mechanisms for metabolic flow regulation in heterogeneous microvascular networks. Am J Physiol Heart Circ Physiol. 2012;302:H1945–H1952. doi: 10.1152/ajpheart.01176.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Russell JA, Kindig CA, Behnke BJ, Poole DC, Musch TI. Effects of aging on capillary geometry and hemodynamics in rat spinotrapezius muscle. Am J Physiol Heart Circ Physiol. 2003;285:H251–H258. doi: 10.1152/ajpheart.01086.2002. [DOI] [PubMed] [Google Scholar]
- 146.Sarelius IH, Duling BR. Direct measurement of microvessel hematocrit, red cell flux, velocity, and transit time. Am J Physiol. 1982;243:H1018–1026. doi: 10.1152/ajpheart.1982.243.6.H1018. [DOI] [PubMed] [Google Scholar]
- 147.Schneiderman G, Goldstick TK. Oxygen electrode design criteria and performance characteristics: recessed cathode. J Appl Physiol. 1978;45:145–154. doi: 10.1152/jappl.1978.45.1.145. [DOI] [PubMed] [Google Scholar]
- 148.Secomb TW, Beard DA, Frisbee JC, Smith NP, Pries AR. The role of theoretical modeling in microcirculation research. Microcirculation. 2008;15:693–698. doi: 10.1080/10739680802349734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Secomb TW, Hsu R. Simulation of O2 transport in skeletal muscle: diffusive exchange between arterioles and capillaries. Am J Physiol. 1994;267:H1214–H1221. doi: 10.1152/ajpheart.1994.267.3.H1214. [DOI] [PubMed] [Google Scholar]
- 150.Secomb TW, Hsu R, Dewhirst MW. Synergistic effects of hyperoxic gas breathing and reduced oxygen consumption on tumor oxygenation: a theoretical model. Int J Radiat Oncol Biol Phys. 2004;59:572–578. doi: 10.1016/j.ijrobp.2004.01.039. [DOI] [PubMed] [Google Scholar]
- 151.Segal SS. Regulation of blood flow in the microcirculation. Microcirculation. 2005;12:33–45. doi: 10.1080/10739680590895028. [DOI] [PubMed] [Google Scholar]
- 152.Seiyama A, Chen SS, Imai T, Kosaka H, Shiga T. Assessment of rate of O2 release from single hepatic sinusoids of rats. Am J Physiol. 1994;267:H944–H951. doi: 10.1152/ajpheart.1994.267.3.H944. [DOI] [PubMed] [Google Scholar]
- 153.Seiyama A, Kosaka H, Shiga T. Effect of ACh and calmodulin inhibitor on O2 transfer from exocrine pancreatic microvessels of rats. Am J Physiol. 1996;271:H1–H7. doi: 10.1152/ajpheart.1996.271.1.H1. [DOI] [PubMed] [Google Scholar]
- 154.Sharan M, Vovenko EP, Vadapalli A, Popel AS, Pittman RN. Experimental and theoretical studies of oxygen gradients in rat pial microvessels. J Cereb Blood Flow Metab. 2008;28:1597–1604. doi: 10.1038/jcbfm.2008.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Shibata M, Ichioka S, Ando J, Kamiya A. Microvascular and interstitial PO2 measurements in rat skeletal muscle by phosphorescence quenching. J Appl Physiol. 2001;91:321–327. doi: 10.1152/jappl.2001.91.1.321. [DOI] [PubMed] [Google Scholar]
- 156.Sinaasappel M, Ince C. Calibration of Pd-porphyrin phosphorescence for oxygen concentration measurements in vivo. J Appl Physiol. 1996;81:2297–2303. doi: 10.1152/jappl.1996.81.5.2297. [DOI] [PubMed] [Google Scholar]
- 157.Slaaf DW, Jeurens TJ, Tangelder GJ, Reneman RS, Arts T. Methods to measure blood flow velocity of red blood cells in vivo at the microscopic level. Ann Biomed Eng. 1986;14:175–186. doi: 10.1007/BF02584268. [DOI] [PubMed] [Google Scholar]
- 158.Smith LM, Barbee RW, Ward KR, Pittman RN. Prolonged reduction of tissue PO2 in the spinotrapezius muscle of spontaneously hypertensive rats following contraction. Am J Physiol Heart Circ Physiol. 2004;287:H401–H407. doi: 10.1152/ajpheart.00980.2002. [DOI] [PubMed] [Google Scholar]
- 159.Stainsby WN, Otis AB. Blood flow, blood oxygen tension, oxygen uptake, and oxygen transport in skeletal muscle. Am J Physiol. 1964;206:858–866. doi: 10.1152/ajplegacy.1964.206.4.858. [DOI] [PubMed] [Google Scholar]
- 160.Stamler JS, Jia L, Eu JP, McMahon TJ, Demchenko IT, Bonaventura J, Gernert K, Piantadosi CA. Blood flow regulation by S-nitrosohemoglobin in the physiological oxygen gradient. Science. 1997;276:2034–2037. doi: 10.1126/science.276.5321.2034. [DOI] [PubMed] [Google Scholar]
- 161.Styp-Rekowska B, Disassa NM, Reglin B, Ulm L, Kuppe H, Secomb TW, Pries AR. An imaging spectroscopy approach for measurement of oxygen saturation and hematocrit during intravital microscopy. Microcirculation. 2007;14:207–221. doi: 10.1080/10739680601139302. [DOI] [PubMed] [Google Scholar]
- 162.Sullivan SM, Pittman RN. Hamster retractor muscle: a new preparation for intravital microscopy. Microvasc Res. 1982;23:329–335. doi: 10.1016/s0026-2862(82)80005-8. [DOI] [PubMed] [Google Scholar]
- 163.Sullivan SM, Pittman RN. In vitro O2 uptake and histochemical fiber type of resting hamster muscles. J Appl Physiol. 1984;57:246–253. doi: 10.1152/jappl.1984.57.1.246. [DOI] [PubMed] [Google Scholar]
- 164.Sullivan SM, Pittman RN. Relationship between mitochondrial volume density and capillarity in hamster muscles. Am J Physiol. 1987;252:H149–H155. doi: 10.1152/ajpheart.1987.252.1.H149. [DOI] [PubMed] [Google Scholar]
- 165.Swain DP, Pittman RN. Oxygen exchange in the microcirculation of hamster retractor muscle. Am J Physiol. 1989;256:H247–H255. doi: 10.1152/ajpheart.1989.256.1.H247. [DOI] [PubMed] [Google Scholar]
- 166.Tateishi N, Suzuki Y, Tanaka J, Maeda N. Imaging of oxygen saturation and distribution of erythrocytes in microvessels. Microcirculation. 1997;4:403–412. doi: 10.3109/10739689709146804. [DOI] [PubMed] [Google Scholar]
- 167.Torres Filho IP, Cyrino FZ, Popel AS, Bouskela E, Johnson PC. Morphometric analysis of the anastomosing arteriolar network in cat sartorius muscle. Int J Microcirc Clin Exp. 1994;14:3–13. doi: 10.1159/000178200. [DOI] [PubMed] [Google Scholar]
- 168.Torres Filho IP, Intaglietta M. Microvessel PO2 measurements by phosphorescence decay method. Am J Physiol. 1993;265:H1434–H1438. doi: 10.1152/ajpheart.1993.265.4.H1434. [DOI] [PubMed] [Google Scholar]
- 169.Torres Filho IP, Kerger H, Intaglietta M. pO2 measurements in arteriolar networks. Microvasc Res. 1996;51:202–212. doi: 10.1006/mvre.1996.0021. [DOI] [PubMed] [Google Scholar]
- 170.Torres Filho IP, Leunig M, Yuan F, Intaglietta M, Jain RK. Noninvasive measurement of microvascular and interstitial oxygen profiles in a human tumor in SCID mice. Proc Natl Acad Sci USA. 1994;91:2081–2085. doi: 10.1073/pnas.91.6.2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Torres Filho IP, Spiess BD, Pittman RN, Barbee RW, Ward KR. Experimental analysis of critical oxygen delivery. Am J Physiol Heart Circ Physiol. 2005;288:H1071–H1079. doi: 10.1152/ajpheart.00884.2004. [DOI] [PubMed] [Google Scholar]
- 172.Torres Filho IP, Terner J, Pittman RN, Proffitt E, Ward KR. Measurement of hemoglobin oxygen saturation using Raman microspectroscopy and 532 nm excitation. J Appl Physiol. 2008;104:1809–1817. doi: 10.1152/japplphysiol.00025.2008. [DOI] [PubMed] [Google Scholar]
- 173.Torres Filho IP, Terner J, Pittman RN, Somera LG, III, Ward KR. Hemoglobin oxygen saturation measurements using resonance Raman intravital microscopy. Am J Physiol Heart Circ Physiol. 2005;289:H488–H495. doi: 10.1152/ajpheart.01171.2004. [DOI] [PubMed] [Google Scholar]
- 174.Tsai AG, Friesenecker B, Mazzoni MC, Kerger H, Buerk DG, Johnson PC, Intaglietta M. Microvascular and tissue oxygen gradients in the rat mesentery. Proc Natl Acad Sci USA. 1998;95:6590–6595. doi: 10.1073/pnas.95.12.6590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Tsai AG, Johnson PC, Intaglietta M. Oxygen gradients in the microcirculation. Physiol Rev. 2003;83:933–963. doi: 10.1152/physrev.00034.2002. [DOI] [PubMed] [Google Scholar]
- 176.Tsai AG, Cabrales P, Johnson PC, Intaglietta M, Golub AS, Pittman RN. Effect of oxygen consumption by measuring method on PO2 transients associated with the passage of erythrocytes in capillaries of rat mesentery. Am J Physiol Heart Circ Physiol. 2005;289:H1777–H1779. doi: 10.1152/ajpheart.00503.2005. [DOI] [PubMed] [Google Scholar]
- 177.Tsoukias NM, Goldman D, Vadapalli A, Pittman RN, Popel AS. A computational model of oxygen delivery by hemoglobin-based oxygen carriers in three-dimensional microvascular networks. J Theor Biol. 2007;248:657–674. doi: 10.1016/j.jtbi.2007.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Twersky V. Absorption and multiple scattering by biological suspensions. J Opt Soc Am. 1970;60:1084–1093. doi: 10.1364/josa.60.001084. [DOI] [PubMed] [Google Scholar]
- 179.Tyml K, Sherebrin MH. A method for on-line measurements of red cell velocity in microvessels using computerized frame-by-frame analysis of television images. Microvasc Res. 1980;20:1–8. doi: 10.1016/0026-2862(80)90014-x. [DOI] [PubMed] [Google Scholar]
- 180.Vadapalli A, Pittman RN, Popel AS. Estimating oxygen transport resistance of the microvascular wall. Am J Physiol Heart Circ Physiol. 2000;279:H657–H671. doi: 10.1152/ajpheart.2000.279.2.H657. [DOI] [PubMed] [Google Scholar]
- 181.Vanderkooi JM, Erecińska M, Silver IA. Oxygen in mammalian tissue: methods of measurement and affinities of various reactions. Am J Physiol. 1991;260:C1131–1150. doi: 10.1152/ajpcell.1991.260.6.C1131. [DOI] [PubMed] [Google Scholar]
- 182.Vanderkooi JM, Maniara G, Green TJ, Wilson DF. An optical method for measurement of dioxygen concentration based upon quenching of phosphorescence. J Biol Chem. 1987;262:5476–5482. [PubMed] [Google Scholar]
- 183.Vinogradov SA, Fernandez-Seara MA, Dupan BW, Wilson DF. A method for measuring oxygen distributions in tissue using frequency domain phosphorometry. Comp Biochem Physiol A Mol Integr Physiol. 2002;132:147–52. doi: 10.1016/s1095-6433(01)00541-4. [DOI] [PubMed] [Google Scholar]
- 184.Voter WA, Gayeski TE. Determination of myoglobin saturation of frozen specimens using a reflecting cryospectrophotometer. Am J Physiol. 1995;269:H1328–H1341. doi: 10.1152/ajpheart.1995.269.4.H1328. [DOI] [PubMed] [Google Scholar]
- 185.Wagner PD. Muscle O2 transport and O2 dependent control of metabolism. Med Sci Sports Exerc. 1995;27:47–53. [PubMed] [Google Scholar]
- 186.Walley KR. Heterogeneity of oxygen delivery impairs oxygen extraction by peripheral tissues: theory. J Appl Physiol. 1996;81:885–894. doi: 10.1152/jappl.1996.81.2.885. [DOI] [PubMed] [Google Scholar]
- 187.Ward KR, Torres Filho IP, Barbee RW, Torres L, Tiba MH, Reynolds PS, Pittman RN, Ivatury RR, Terner J. Resonance Raman spectroscopy: A new technology for tissue oxygenation monitoring. Crit Care Med. 2006;34:792–799. doi: 10.1097/01.ccm.0000201898.43135.3f. [DOI] [PubMed] [Google Scholar]
- 188.Wayland H, Johnson PC. Erythrocyte velocity measurement in microvessels by a two-slit photometric method. J Appl Physiol. 1967;22:333–337. doi: 10.1152/jappl.1967.22.2.333. [DOI] [PubMed] [Google Scholar]
- 189.Weerappuli DPV, Pittman RN, Popel AS. Effect of convection in capillaries on oxygen removal from arterioles in striated muscle. J Theor Biol. 1990;147:275–288. doi: 10.1016/s0022-5193(05)80057-8. [DOI] [PubMed] [Google Scholar]
- 190.Weibel ER. The Pathway for Oxygen. Cambridge, MA: Harvard University Press; 1984. [Google Scholar]
- 191.Whalen WJ, Riley J, Nair P. A microelectrode for measuring intracellular PO2. J Appl Physiol. 1967;23:798–801. doi: 10.1152/jappl.1967.23.5.798. [DOI] [PubMed] [Google Scholar]
- 192.Wiederhielm CA. Continuous recording of arteriolar dimensions with a television microscope. J Appl Physiol. 1963;18:1041–1042. doi: 10.1152/jappl.1963.18.5.1041. [DOI] [PubMed] [Google Scholar]
- 193.Wilson DF. Quantifying the role of oxygen pressure in tissue function. Am J Physiol Heart Circ Physiol. 2008;294:H11–H13. doi: 10.1152/ajpheart.01293.2007. [DOI] [PubMed] [Google Scholar]
- 194.Wilson DF, Erecińska M, Drown C, Silver IA. The oxygen dependence of cellular energy metabolism. Arch Biochem Biophys. 1979;195:485–493. doi: 10.1016/0003-9861(79)90375-8. [DOI] [PubMed] [Google Scholar]
- 195.Wittenberg BA, Wittenberg JB. Transport of oxygen in muscle. Annu Rev Physiol. 1989;51:857–878. doi: 10.1146/annurev.ph.51.030189.004233. [DOI] [PubMed] [Google Scholar]
- 196.Wittenberg JB. Myoglobin-facilitated oxygen diffusion: role of myoglobin in oxygen entry into muscle. Physiol Rev. 1970;50:559–636. doi: 10.1152/physrev.1970.50.4.559. [DOI] [PubMed] [Google Scholar]
- 197.Wittenberg JB, Wittenberg BA. Myoglobin function reassessed. J Exp Biol. 2003;206:2011–2020. doi: 10.1242/jeb.00243. [DOI] [PubMed] [Google Scholar]
- 198.Xiang L, Naik JS, Hester RL. Functional vasodilation in the rat spinotrapezius muscle: Role of nitric oxide, prostanoids and epoxyeicosatrienoic acids. Clin Exp Pharmacol Physiol. 2008;35:617–624. doi: 10.1111/j.1440-1681.2007.04864.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Zheng L, Golub AS, Pittman RN. Determination of PO2 and its heterogeneity in single capillaries. Am J Physiol. 1996;271:H365–H372. doi: 10.1152/ajpheart.1996.271.1.H365. [DOI] [PubMed] [Google Scholar]