Abstract
Objective
We examined selected survivor characteristics to determine what factors might moderate the response to two psychosocial interventions.
Design
Seventy-one prostate cancer survivors were randomly assigned to either a telephone-delivered health education (THE) intervention or a telephone-delivered interpersonal counseling (TIP-C) intervention.
Measures
Psychological QOL outcomes included depression, negative and positive affect, and perceived stress.
Results
For three of the psychological outcomes (depression, negative affect and stress), there were distinct advantages from participating in THE. For example, more favorable depression outcomes occurred when men were older, had lower prostate specific functioning, were in active chemotherapy, had lower social support from friends and lower cancer knowledge. Participating in the TIP-C provided a more favorable outcome for positive affect when men had higher education, prostate specific functioning, social support from friends and cancer knowledge.
Conclusion
Unique survivor characteristics must be considered when recommending interventions that might improve psychological QOL in prostate cancer survivors. Future research must examine who benefits most and from what components of psychosocial interventions to enable clinicians to recommend appropriate psychosocial care.
Keywords: psychosocial interventions, QOL, prostate cancer, psychological distress
Over 2 million men are currently living with the significant challenges associated with prostate cancer diagnosis and treatment[1]. Prostate cancer and its treatment are associated with psychological and physical side effects that include urinary incontinence, sexual dysfunction, fatigue and psychological distress.[2-4] The incidence of psychological distress, specifically depression and anxiety, has been reported as 16% and 12%, respectively [3], which is higher than population norms for older men. Depression and anxiety are associated with decreased compliance with adjuvant therapy, feelings of nervousness and worry, cognitive and functional impairments and reduced quality of life (QOL) (i.e., decreased psychological, physical, social and spiritual well-being) [5, 6]. High levels of perceived stress have also been associated with high rates of depression and poorer QOL in adults with cancer[7].
Studies of men with prostate cancer have identified the two prominent areas of unmet need: 1) maintenance of psychosocial well-being, such as minimizing psychological distress and improving interpersonal functioning, [8] and 2) meeting informational needs for increased understanding of the illness and its short- and long-term effects [9, 10]. Interventions that target psychological distress and provide information about cancer can help survivors to decrease the uncertainty and related psychological and physical distress associated with cancer[11]. In a review of psychosocial interventions for maintaining and improving QOL in men with prostate cancer, Penedo and Dahn[12] concluded that despite the promising evidence of their effectiveness for reducing psychological distress and improving QOL[13-15], additional research is needed to determine who benefits most and from what components of psychosocial interventions. This call reflects a move away from a one size fits all approach to using a theoretical perspective to examine intervention benefit.
Telephone delivered interventions are an increasingly common component of psychosocial oncology practice. [16, 17] As part of a larger behavioral clinical trial, we developed two telephone–delivered psychosocial interventions (health education and interpersonal counseling) that were designed to target the psychological distress and informational needs of prostate cancer survivors (PCS) and their family members and friends. We found that both interventions were effective in improving multiple dimensions of QOL (psychological distress, and physical, social and spiritual well-being) over the four months course of the investigation.[18] We adapted the stress process model stress process model[19] to guide the study and predict intervention effectiveness on QOL outcomes. The model was originally developed to describe care giving processes for Alzheimer’s patients, and to explain and predict outcomes among cancer patients [20] and informal caregivers of cancer patients. [21-23] The model proposes that contextual characteristics and psychosocial resources can moderate the effect of the interventions on QOL.
In the stress process model, background variables include various demographic variables that describe the patient’s standing in social strata and access to resources. In this investigation, these were indexed by the prostate cancer patients’ age, education and income. The stress process model also indicates that psychosocial resources (e.g., cancer knowledge, social support) and primary stressors (e.g., prostate functioning, symptom distress) will play a major role in maintaining or disrupting QOL and response to psychosocial treatment.[24-26] Both age and education have been reported as influencing QOL and intervention benefit.[25, 26] Younger men with prostate cancer with good sexual functioning before treatment have been reported to experience higher levels of psychological distress following treatment.[26] The combination of younger age and loss of function puts younger men at higher risk for psychological distress than older men with similar prostate specific functionality. Further, Chambers found that following an educational intervention, younger men with higher education reported benefits on important psychological outcomes. Knight [25] and Mishel [24] found that men with less education experienced both greater symptom distress/burden and inability to manage their daily lives due to cancer. Thus, both age and education seem to influence QOL and intervention benefit.
Psychosocial resources are those variables such as social support or cancer knowledge that mediate the relationship between the contextual characteristics and psychosocial distress [23]. Social support is a key resource for cancer survivors and their social network members and lack of support is a cause of psychological distress among PCS.[27] There is clear evidence that social support is beneficial for PCS [28-31] and emotional support provided by family members is associated with reduced anxiety, depression, and hostility.[32] PCS have strong informational needs, and these unmet needs have been linked to poor QOL.[33] Traeger [10], among others[26], found that men with more severe illness perceptions (due to poor knowledge) had poorer emotional well-being. Our preliminary results found that improvements in psychological distress and related physical, social and spiritual well-being occurred when informational support was provided in a structured educational intervention.[18]
Given the benefits of our interventions, the logical next step was to determine for whom the interventions work best. Therefore, the purpose of this paper was to examine what selected factors specified in the stress process model (e.g., age, education, prostate specific functioning, symptom distress and symptom management, social support, cancer knowledge) of the PCS might moderate the response to different interventions designed to improve psychological quality of life (depression, positive and negative affect, and perceived stress). We wanted to answer the question, “who benefits from these two different telephone delivered psychosocial interventions?” to provide clinicians with information for recommending the intervention that might be the most beneficial to prostate cancer survivors.
Methods
Sample
Participants for the larger study were a convenience sample of 71 prostate cancer survivors and their 71 social network members. For the purpose of this paper that focuses on PCS, we have excluded the social network members in all further analysis. Eligibility criteria for the PCS included a diagnosis of prostate cancer, currently undergoing or had completed treatment within the past six months, ability to speak English, no physical or psychological disabilities that would prevent participation in the interventions, and availability of a social network member who was willing to participate in the investigation. Descriptive information about the demographic characteristics of the survivors appears in Table 1. Table 2 lists the illness characteristics of the PCS. The typical participant was in his late 60’s, white, married, retired, and college educated. Treatment included prostatectomy (almost 30%), radiation (56%) and hormone therapy (42%). All of the men listed at least one other chronic illness, with an average of 1.82 (SD = 1.5) illnesses and 4.64 (SD = 3.7) medications. At baseline, there were no significant differences in demographic characteristics between the health education and counseling groups.
Table 1.
Demographic Characteristics of Survivors
| Age (years) | 66.99 (9.6) |
| Race/ethnicity | |
| American Indian/Alaska native | 0 |
| Asian/Pacific Islander | 0 |
| Black | 6 (8.5%) |
| Hispanic | 5 (7.0%) |
| White | 60 (84.5%) |
| Other/Unknown | 0 |
| Marital status | |
| Married | 56 (78.9%) |
| Unmarried | 15 (21.1%) |
| Length of marriage/committee relationship (years) | 32.98 (17.8) |
| Number of children | 2.41 (1.7) |
| Highest level of education | |
| Middle school | 1 (1.4%) |
| High school | 9 (12.7%) |
| Vocational/Technical/Some college | 20 (28.2%) |
| College | 24 (33.8%) |
| Post graduate/Professional degree | 17 (23.9%) |
| Employment status | |
| Unemployed, but seeking employment | 2 (2.8%) |
| Employed part time/full time | 19 (26.8%) |
| Retired | 50 (70.4%) |
| Disabled | 0 |
Table 2.
Prostate Cancer Information for Survivors
| Weeks since diagnosis | 186.77 (257.5) |
| Type of treatment* | |
| Chemotherapy | 10 (14.1%) |
| Radiation | 40 (56.3%) |
| Hormones | 30 (42.3%) |
| Surgery | 30 (42.3%) |
| CAM | 3 (4.2%) |
| Watchful waiting | 7 (9.9%) |
| Type of Surgery* | 57 (80.3%) |
| Biopsy | 21 (29.6%) |
| Complete or radical prostatectomy | 5 (7%) |
| Prostate node dissection | 4 (5.6%) |
| Tumor removal | |
| Stage of cancer # | 11 (15.5%) |
| I | 6 (8.5%) |
| II | 6 (11.3%) |
| III | 8 (11.3%) |
| IV | |
| PSA level | 17.26 (43.6) |
| Gleason score | 6.33 (1.6) |
| Family history of prostate cancer | |
| Yes | 27 (38%) |
| No | 43 (60.6%) |
Note.
Over 100% because survivors had more than one type of treatment.
Stage was unknown by most participants and was dropped from further analyses.
Procedure
Prostate cancer survivors were recruited from regional cancer centers, regional Veterans Affairs Heath Care Centers, cancer support groups, and from research study websites through which interested individuals could volunteer to enroll. After informed consent, PCS and their social network members (i.e., family members or friends) were randomly assigned to one of two 8 week telephone delivered interventions: telephone health education (THE) and telephone interpersonal counseling (TIP-C) described below. Thirty-six men and their social network members were assigned to the TIP-C intervention and 35 men and their social network members were assigned to telephone health education (THE). The interventions were delivered between T1 and T2 of a 3-wave longitudinal study with 8-week intervals. All participants completed baseline (T1) assessments over the telephone that included the instruments described here plus others not relevant to the present report. Participants completed the second (T2) assessment (T1 + 8 weeks) within one week of their final intervention session, and the final assessment (T3) 8 weeks later (T2 + 8weeks). After each assessment, participants were sent a $10 gift card from a local retail merchant to thank them for their time.
At T1, 71 prostate cancer survivors were enrolled and 5 survivors withdrew from the study by T2 (T1-T2 attrition rate = 7%). By T3, an additional 2 participants were lost to follow-up because they declined to complete the T3 assessment (T1-T3 attrition = 10%). The Consort flowchart for this sample is available in the literature.[34] There were no significant differences for demographic or illness characteristics between those that discontinued and those that completed the study.
Interventions
The TIP-C intervention was delivered by two interventionists (one master’s prepared social worker and one master’s prepared nurse; both with oncology expertise). Sessions averaged 31 minutes (SD = 7.0) in duration. The TIP-C intervention was developed from standard interpersonal psychotherapy[35], combined with cancer education, and modified for telephone delivery. The intervention addressed 1) mood and affect management, 2) emotional expression, 3) interpersonal communication and relationships, 4) social support, and 5) cancer information. The TIP-C focuses on enhancing emotional support both through the direct effects of interaction with the interventionist, and mobilizing the survivors’ naturally occurring support. The TIP-C targets social support, and explains how life events and the social environment affect mood, the influence of mood on social functioning, and provides normalization and validation of participants’ experiences and reactions to cancer. TIP-C is designed to improve the quality of the relationships between survivors and other key players in the cancer experience (e.g., family, health care team).
The THE intervention was delivered by two paraprofessionals (non-health students/staff). Sessions averaged 28 minutes (SD = 6.2). Adult educational techniques guided the provision of information. Prior to receiving the intervention, standardized materials developed by the National Cancer Institute were sent to the participants, and these materials were reviewed over the telephone. THE focuses on 1) normal prostate health and prostate cancer, routine tests for the diagnosis and prevention, terminology, 2) treatment, side effects of treatment, and strategies to combat these side effects, 3) lifestyle interventions such as nutrition and physical activity, and 4) referrals and resources. No counseling occurred in the health education and sessions help participants take a more active role in their care by asking more appropriate and relevant questions (i.e. patient activation[36]).
Both interventions had manuals and the intervention content was the same whether the participant was a PCS or social network member. The PCS and his designated social network member were called separately at times convenient to participate in the interventions. The interventionists, who were trained in the intervention for which they were responsible, called each PCS once weekly over 8 weeks. Sessions of both interventions were recorded and reviewed by the first and second authors. After establishing a >90% adherence to the protocols, randomly selected interventions (about 10%) were reviewed, giving feedback to the interveners to maintain fidelity and prevent intervention drift.
Measures
Two sets of measures were used to test the differential effectiveness of the two interventions. The first set included four indicators of psychological QOL (depression, positive and negative affect, and perceived stress).
Psychological Quality of Life
Symptoms of depression were measured using the 20-item Center for Epidemiological Studies-Depression Scale (CES-D) [37]. Scores range from 0 to 60, with higher scores indicating greater depression. The CES-D has strong evidence of satisfactory reliability and validity[38]. Cronbach’s alphas over the 3 measurement times were ≥ .88.
Positive and negative affect were assessed with the 20-item Positive and Negative Affect Schedule (PANAS)[39]. Scores range from 10 to 50 on each scale. The PANAS has been used extensively with satisfactory reliability and demonstrated convergent and construct validity[40]. Cronbach’s alphas were ≥.87 for positive affect and ≥ .83 for negative affect over time.
Perceived Stress was assessed with the 10-item Perceived Stress Scale (PSS) [41]that measures subjective appraisals of stress. The PSS has a scale range of 0 – 40. The PSS has demonstrated satisfactory reliability and validity in numerous studies with a Cronbach’s alphas in this study were ≥ .88 over time.
The second set of measures included selected contextual characteristic and psychosocial resource variables that would be predicted by the stress process model to moderate the association between intervention condition and QOL outcomes. These were grouped into the categories of demographic characteristics, illness characteristics and context, and psychosocial resource variables. These potential moderating variables were assessed at baseline only.
Demographic characteristics tested as moderators were age and education. Education was measured through six ordered categories starting with elementary school and ending with post-graduate or professional degree.
Illness characteristics and context were assessed by the stage of cancer (1-4), PSA, and the UCLA Prostate Cancer Index (PCI)[43]. Given the amount of missing self-reported data for stage or PSA, these variables were dropped from further analysis. Participants completed the PCI to assess their prostate specific health related QOL or functioning. This Index has sound psychometric qualities, demonstrating good internal consistency, test-retest reliability, and validity [44]. The reliability of the PCI in this sample was α = .74. Symptom distress and symptom management were each assessed by a one-item scale that ranged from 1-10. Higher scores indicated higher symptom distress and greater abilities to manage one’s symptoms. Participants were asked to respond yes/no to whether they were currently receiving each of the following therapies for their prostate cancer: chemotherapy, radiation, and hormone blocking or if they had ever undergone surgery to treat their prostate cancer.
Psychosocial resources included two measures of the participant’s cognitive or affective background that could have a potential influence on the outcome of the interventions: social support and cancer knowledge. Social support was measured with the 20-item Perceived Social Support-Friend (PSS-FR) scale. The PSS scales have a strong record of psychometric quality, correlating with variables such as degree of relational reciprocity, and intangible and tangible support from Cancer knowledge determined the participant’s general knowledge about prostate cancer with a 14-item index. Respondents answered true or false to statements about biopsies, prostatectomy, routine exams, chemotherapy, radiation, and fatigue. These statements were derived from health education materials about prostate cancer available from the National Cancer Institute.
Statistical Analysis
Level 1 Growth Curve Analyses (GCA)
Multi-Level Modeling (MLM) was performed using SAS PROC MIXED. Individual growth curve parameters were obtained by Maximum Likelihood (ML) estimation, quantifying the systematic changes in scores over time by empirically fitting regression lines for all variables (i.e., psychological QOL) on which repeated measures were obtained. The following growth curve parameters were estimated: (1) the intercept, representing the starting score on each QOL variable prior to experimental treatment, and (2) the natural logarithmic slope, using the unstandardized regression weights, representing the direction and magnitude of average change in scores over time. Because we expected negatively accelerated functions for the growth curves, the slopes were theoretically pre-specified to be curvilinear; a natural logarithmic transformation of time was therefore performed prior to the GCAs. A visual example of the estimate of growth curve slopes appears in Figure 1. An unstructured covariance matrix was specified in the MLM, in which all the variances and covariances among repeated observations were freely estimated and thus permitted to be different from each other.
Figure 1. Example of Raw Data and Estimation of Log Rhythmic Slope.
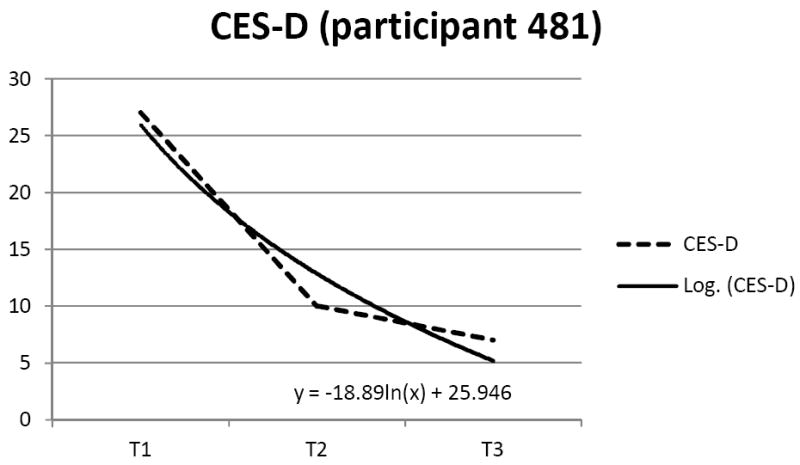
Note. Dashed line represents raw scores on CES-D scale. Solid line represents estimated individual growth curve slope.
Moderation tests
The individual growth curve parameters generated in the Level 1 GCA were subsequently treated as dependent variables in a series of moderated regression analyses. For each analysis, intervention condition (TIP-C or THE) was the independent variable. Each of the potential moderator variables (demographic characteristics, illness characteristics and context, and psychosocial resources) was individually tested to determine if it predicted a differential effectiveness of one intervention over the other. The individual growth curve slopes for each of the four psychological QOL variables were the dependent variables. By analyzing the growth curve slopes, data from all three points of assessment were taken into account because the growth curves represent the trajectory of change from T1 to T3. For all such analyses, the independent and moderator variables were mean centered prior to creating the interaction terms, as recommended by Cohen, Cohen, Aiken, and West (2003) [45]. If a statistically significant interaction was found, this indicated that the moderator variable predicted a differential outcome in terms of individual growth curves for the two intervention conditions. When there were statistically significant interactions found, post hoc conditional regression analyses were conducted at -1SD, the mean, and +1SD for continuous moderator variables, and at two levels (e.g., present/absent) for dichotomous moderator variables. The conditional slopes in these post-hoc analyses were also tested for statistical significance (i.e., significant difference from 0). These tests reflect the differential effectiveness of the two interventions at differing levels of the moderator variable. Where the conditional slope is not significant, there is no statistically significant difference in QOL trajectories (as indexed by the slope) in the two conditions. Significant conditional slopes indicate that the QOL trajectory was significantly different in the two conditions. Because regression is generally underpowered for detecting interactions in all but ideal experimental contexts[46], we implemented this post-hoc deconstruction of interaction effects that were statistically significant at the p < .05 level, as well as those at the p = .05 - .09 significance levels. With the sample size of this investigation, the smallest effect that could be detected for the interaction term at α = .05 and power = .80 would be f2 = .11, which is equivalent to R2Δ = .10 for the interaction effect. Because R2Δ = .10 is a substantial effect, it is possible that there could be somewhat weaker interaction effects that do not exceed the p < .05 threshold for statistical significance, but that may still have some practical implications for identifying superior outcomes in one intervention condition over the other.
Results
Table 3 shows the results of the tests for each moderator variable using the four QOL individual growth curve slopes. For clarity of presentation, only the unstandardized regression coefficient for the interaction term is listed in the table. Post hoc deconstruction of any significant or marginally significant interaction term is indicated immediately below the interaction term, again, in the form of unstandardized regression coefficients. In all analyses the TIP-C condition was dummy coded as 1 and THE as 2. To explain the nature of the interaction effects in more detail, we focus on two specific examples (age and social support) examining the conditional effects at different levels of the moderator. Although we discuss estimates of the effect for participating in each intervention for those at different levels of the moderator variable, this latter information is not included in Table 3.
Table 3.
Demographic, Illness Characteristics, Ill Context Moderators and Psychosocial Resource Moderators of the Effect of Intervention Condition on QOL Outcomes
| Moderator | depression | negative affect | positive affect | perceived stress |
|---|---|---|---|---|
|
| ||||
| Demographic Characteristics | ||||
|
| ||||
| Age | -.20* | -.02 | .12 | -.01 |
| -1SD b = -1.32 | ||||
| M b = -3.27** | ||||
| +1SD b = -5.23*** | ||||
|
| ||||
| education | .06 | .65 | -1.93* | .77a |
| -1SD b = 1.28 | -1SD b = -3.08*** | |||
| M b = -0.69 | M b = -2.29*** | |||
| +1SD b = -2.67* | +1Sd b = -1.50* | |||
|
| ||||
| Illness Characteristics/Context | ||||
|
| ||||
| Prostate Specific Function | .08a | .06 | -.07a | .02 |
| -1SD b = -5.36*** | -1 SD b = 0.90 | |||
| M b = -3.43*** | M b = -0.74 | |||
| +1SD b = -1.51 | +1SD b = -2.38* | |||
|
| ||||
| Chemotherapy | -5.94a | -1.05 | 1.30 | -1.21 |
| no b = -2.69* | ||||
| yes b = -8.63** | ||||
|
| ||||
| symptom distress | -.81 | -.63a | .34 | -.14 |
| -1SD b = -1.70 | ||||
| M b = -3.43*** | ||||
| +1SD b =-4.55*** | ||||
|
| ||||
| symptom management | -.03 | .75* | -.26 | .08 |
| -1SD b = -4.90*** | ||||
| M b = -3.41*** | ||||
| +1SD b = -1.93* | ||||
|
| ||||
| Psychosocial Resources | ||||
|
| ||||
| social support-friends | .50* | .11 | -.49* | .14 |
| -1SD b = -5.80*** | -1SD b = 1.56 | |||
| M b = -3.53*** | M b = -0.63 | |||
| +1SD b = -1.26 | +1SD b = -2.82* | |||
|
| ||||
| cancer knowledge | .59a | .10 | -.47a | .16 |
| -1SD b = -5.40*** | -1SD b = 0.87 | |||
| M b = -3.48*** | M b = -0.66 | |||
| +1SD b= -1.55 | +1SD b= -2.21a | |||
Note. Table values are unstandardized regression coefficients for the interaction term composed of treatment group (dummy coded as TIP-C = 1, THE = 2) × moderator variable. Values in subscript are conditional unstandardized regression coefficients representing the relationship between treatment group and the dependent variable at -1SD, M, and +1SD of the moderator for continuous moderator variables, and at absence (no = 0) or presence (yes = 1) of the moderator for dichotomous moderator variables.
p < .05.
p < .01.
p < .001.
p = .05 - .09.
Our first example illustrates that age was a significant moderator of intervention benefit on depression slopes (Table 3). Because all of the conditional effects are negative, improvements in depression (negative slopes) were always strongest in the THE intervention compared to the TIP-C. Age caused substantial variability in the intervention effect. Among younger men (-1 SD from the mean or 57 years of age) the effect for intervention was not significant. Specific estimates of depression slopes are b = -.45 for younger men in the TIP-C intervention, and b = -1.77 for younger men in the THE intervention. These non-significant conditional slopes document that changes in depression were equivalent for younger men in the two interventions. For men at the mean age (67 years) in our sample, specific estimates of depression slopes were b = -0.10 in the TIP-C and b = -3.38 for men in the THE. This shows that there is an advantage for being in the health education intervention when the man is average aged (67 years) rather than younger (≤ 57 years). Finally, for older men (+1 SD from the mean or 77 years), the estimate of the TIP-C intervention’s effect on depression is b = 0.24 and in the THE condition, it is b = -4.99. Figure 2 illustrates the slopes at the three conditional values of age. As evident in Figure 2, among older men there is a major advantage to being in the educational intervention in improvements in depression, whereas among younger men the differential advantage of one intervention over the other is minimal.
Figure 2. Illustration of Age × Intervention Condition Interaction on CES-D Slopes.
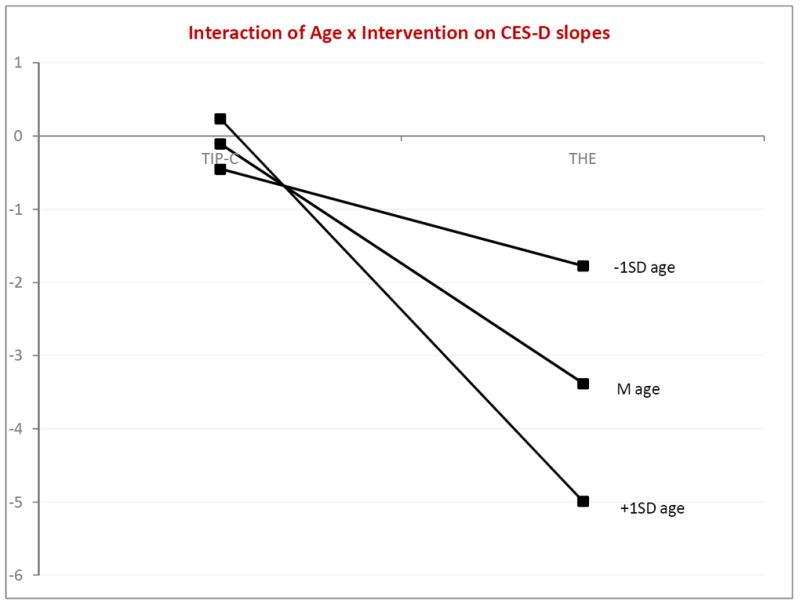
Note. Plotted values represent slopes. Therefore positive values indicate increases in depression over time and negative values indicate decreases in depression over time.
Our second example shows how social support from friends moderated the effect of intervention on positive affect slopes (Table 3). Social support from friends is a particularly remarkable moderator in that it exhibited a disordinal interaction with intervention condition on changes in men’s positive affect over time. Figure 3 plots these slopes at the three conditional values of social support. As illustrated in Figure 3, among men -1 SD from the mean on social support from friends (i.e., low social support), the effect of the intervention was not significant. The average change in positive affect for men in the TIP-C was b = .97 and was b = 2.54 for men in the THE intervention. Positive affect increased for men with low social support in both interventions, but the effect was more pronounced (but not significantly so) among those men in the THE. Among men at the average for social support from friends, the effect of intervention was also not significant, with an average slope of b = 1.40 in the TIP-C intervention and b = .77 in the THE intervention. Both groups of men evidenced increases in positive affect over time, but for men with average social support, the advantage is now for the TIP-C intervention, but not significantly so. Finally, the effect for intervention for men +1 SD from the mean of social support from friends (i.e., high social support) was b = -2.82, p < .05. The average positive affect slopes for these men were b = 1.82 in the TIP-C intervention and b = -1.00 for men in the THE intervention. For men who have high levels of social support from friends, the advantage of being in the TIP-C intervention is truly dramatic. Men in TIP-C had positive slopes for positive affect over time whereas men in THE had negative slopes indicating decreases in positive affect over time.
Figure 3. Illustration of Social Support from Friends × Intervention Condition Interaction on Positive Affect Slopes.
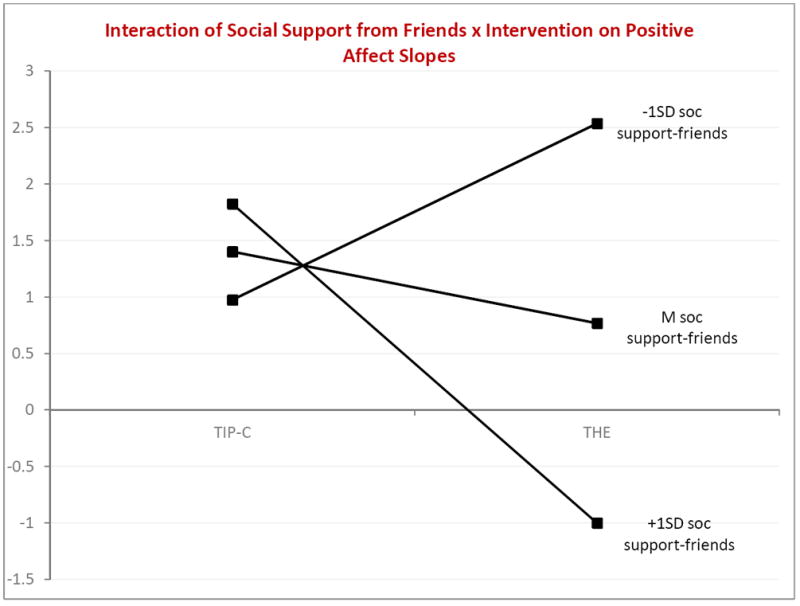
Note. Plotted values represent slopes. Therefore positive values indicate increases in positive affect over time and negative values indicate decreases in positive affect over time.
The results of the moderated regression analyses for the outcome measures are summarized in Table 4. For three of the psychological outcomes (depression, negative affect and stress), there were distinct advantages from participating in THE. More favorable depression outcomes (reduced depression) occurred when men were older, had lower prostate specific functioning, in active chemotherapy, and had lower social support from friends and lower cancer knowledge. For negative affect, more favorable outcomes (reduced negative affect) occurred when the men had higher levels of symptom distress, and lower perceived ability to manage their symptoms. The THE intervention also produced a more favorable outcome (reduced perceived stress) when men had lower education. Participating in the TIP-C provided a more favorable outcome for positive affect (increased positive affect) when men had higher education, prostate specific functioning, social support from friends and cancer knowledge.
Table 4.
Summary of Results of the Effect of the Intervention Condition on Psychological QOL Outcomes
| THE > TIP-C |
|---|
| Depression |
| Older Age, Active Chemotherapy, Lower Prostate Specific Functioning, Lower Social Support from Friends and Lower Cancer Knowledge |
| Negative Affect |
| Higher Symptom Distress and Lower Ability to Manage Symptoms |
| Perceived Stress |
| Lower Education |
| TIP-C > THE |
| Positive Affect |
| Higher Education, Higher Prostate Specific Functioning, Higher Social Support from Friends, and Higher Cancer Knowledge |
Discussion and Conclusions
Although both informational needs and psychosocial distress are paramount issues during survivorship[47], a “one size fits all” approach to meeting the needs of prostate cancer survivors is unlikely to be as effective as interventions more tailored to the unique characteristics of the survivor. This investigation provides evidence that the survivors’ contextual characteristics and psychosocial resources predict differential intervention benefit. Demographic characteristics such as age and education were found to influence effectiveness of the different interventions. Our findings that older men experienced a much more significant reduction in their depression in the health education intervention are consistent with Wong et al.[48] who found older prostate cancer survivors predominantly wanted detailed information. The results of this study show that older men clearly benefitted when they participated in an intervention designed to deliver such information versus one more focused on social relationships and psychological distress. Men with fewer years of formal education also demonstrated substantially decreased stress when they received the information in the health education intervention. This may be due to the fact that these men have less access to informational resources. The qualitative comments from these men supported this assumption. The majority reported that having easy access (i.e., we called them weekly, printed information was mailed to their homes and discussed over the phone) to information about prostate cancer, its treatment, side effects and general health information was the most beneficial part of the intervention.
Of note, and consistent with the literature[4, 26], prostate specific functioning influenced intervention benefit. Our sample was mostly older men who reported below average to average prostate specific function prior to treatment as well as active chemotherapy. Depression decreased significantly more for men with below average or average prostate specific functioning and in active chemotherapy in the THE versus the TIP-C intervention. It appears that the information delivered in the THE intervention is associated with more positive outcomes for men who are simultaneously grappling with the major insults to physical well-being that are represented by lower specific prostate functioning and active chemotherapy. Physiological challenges in these older men appear to be best met with straightforward health related information.
Similar to other studies related to illness severity [51-53], men with higher symptom distress and lower abilities to manage their symptoms did better when the intervention focused on health education (e.g, reduced negative affect). Again, perhaps the information shared helped manage those symptoms, which had primary importance to the PCS and his QOL.
Psychosocial resources predicted a differential response to the interventions. Social support plays an important role in maintaining psychological QOL in prostate cancer survivors.[49] In this study we found that social support from friends[50] rather than family played a significant role in the differential effectiveness of the interventions. This may be due in part to the fact that the social support from friends is often viewed as voluntary, whereas social support from family is viewed by many as obligatory. Therefore, for some people, social support from friends may be viewed as a more valuable commodity. Also, it is likely that for many survivors, social support from friends may be coming from age and gender matched peers who are in a good position to empathize and perhaps even share their own experiences with prostate health related issues. Some of our sample reported no one other than their spouses for social support. In this investigation, men with lower social support from friends benefitted more when in the health education intervention. This may be because many men with prostate cancer share information with each other. A man with lower social support from friends might therefore particularly benefit from an intervention that effectively replaces the informal peer information exchange that may be lacking. Also, because the TIP-C intervention focuses more on roles and relationships, this type of intervention might be a more salient for people who are more extensively embedded in their social network.
Men with lower cancer knowledge also had better improvements in outcomes in the health education intervention. Presumably, the THE delivers the information that these men lack but may want[26, 48] as they go through cancer treatment and survivorship. Our findings suggest that perhaps a two step approach to improving QOL in PCS is needed. First, we need to meet the unmet informational needs before tackling psychosocial well-being issues, such as improving interpersonal functioning.
It is evident that on balance most of the significant moderators further enhanced the salutary effects of the health education. This is consistent with related findings in the literature showing that far more prostate cancer survivors are interested in receiving informational services than psychosocial services and that informational support can help to reduce psychological distress[54]. At the same time it is important to realize that most of the significant moderators only played a role in 1 or 2 of the psychological QOL outcomes. For many of the psychological QOL variables, the predicted moderating variables were not associated with a differential effectiveness between the two interventions.
Survivor characteristics such as older age, lower education, lower specific prostate functioning, lower social support from friends and initially lower cancer knowledge were all associated with better outcomes if the PCS was received the health education intervention. In contrast, and with all other things being equal, men with higher levels of education, social support from friends, or prostate specific functioning had better psychological QOL trajectories when participating in an interpersonal counseling intervention.
Interpretations of this study’s findings are limited by several issues. The analyses were based on a relatively small white, well educated sample. This limits both statistical power and the generalizability to the larger population of prostate cancer survivors. Also, the average participant in this investigation was several years beyond the initial diagnosis. It is possible that the different interventions might be more or less effective at different times during the survivorship trajectory and that would be worth investigating in a larger sample.
Our findings documented that men with prostate cancer benefitted from the psychosocial interventions. For the older, less well educated and less well functioning men in the domains of social support, cancer knowledge and prostate functioning, the benefits of supplying health education to prevent potential reductions in psychological QOL were clear. The advantage to the telephone delivery is that clinicians will be able to document not only that their patients received the information about prostate cancer and general health topics, but demonstrated an understanding during the discussions on the telephone.
In conclusion, Penedo and Dahn[12] deduced in their review of interventions for prostate cancer that the evidence supports that cancer survivors benefit significantly from psychosocial interventions, and our findings provide support for this conclusion. However, they further observed that “additional research is needed to improve the understanding of who benefits most and from what components of psychosocial interventions” (p. 532). This research provides some insight into who benefits from what intervention. However, future research conducted to further examine who benefits from different interventions, based on different survivor characteristics, will enable clinicians to recommend effective interventions that will improve the QOL for prostate cancer survivors.
Acknowledgments
Funding for this R21 study (R21CA113409) was provided by the National Cancer Institute to Terry Badger. We gratefully thank our recruitment sites: Arizona Cancer Center, Veteran’s Affairs Health Care Systems in Phoenix and Tucson. This material is the result of work supported with the resources and the use of facilities at the Veterans Affairs Health Care Systems in Phoenix and Tucson. We thank our research staff, Maria Figueroa, Xochitl Gaxiola, Jeannine Thomas, Jen Riech, and Karina Othon-Tapia.
Footnotes
Disclaimer: The contents of this publication do not represent the views of the Department of Veterans Affairs or the United States Government.
Contributor Information
Terry A. Badger, The University of Arizona, College of Nursing, 1305 N. Martin, Tucson, AZ 85721, Office: 520-626-6058 FAX:520-626-7891 tbadger@nursing.arizona.edu.
Chris Segrin, The University of Arizona, Department of Communication.
Aurelio J Figueredo, The University of Arizona, Department of Psychology.
Joanne Harrington, Division of Hematology and Oncology, Phoenix Veterans’ Affairs Health Care System, Phoenix, AZ.
Kate Sheppard, The University of Arizona, College of Nursing.
Stacey Passalacqua, James Madison University, School of Communication Studies, Harrisonburg, Virginia 22807.
Alice Pasvogel, The University of Arizona, College of Nursing.
Maria Bishop, Arizona Cancer Center and Southern Arizona Veterans’ Affairs Health Care System, Tucson, AZ.
References
- 1.ACS. Cancer Facts & Figures, 2011. American Cancer Society; Atlanta, GA: 2011. [Google Scholar]
- 2.Danjoux C, Gardner S, Fitch M. Prospective evaluation of fatigue during a course of curative radiotherapy for localised prostate cancer. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2007;15(10):1169–1176. doi: 10.1007/s00520-007-0229-8. [DOI] [PubMed] [Google Scholar]
- 3.Sharpley CF, Christie DR. An analysis of the psychometric profile and frequency of anxiety and depression in Australian men with prostate cancer. Psycho-oncology. 2007;16(7):660–667. doi: 10.1002/pon.1118. [DOI] [PubMed] [Google Scholar]
- 4.Namiki SYA. Health-related quality of life in men with localized prostate cancer. International Journal of Urology. 2010;17:125–158. doi: 10.1111/j.1442-2042.2009.02437.x. [DOI] [PubMed] [Google Scholar]
- 5.Jacobsen PB, Jim HS. Psychosocial interventions for anxiety and depression in adult cancer patients: achievements and challenges. CA: a cancer journal for clinicians. 2008;58(4):214–230. doi: 10.3322/CA.2008.0003. [DOI] [PubMed] [Google Scholar]
- 6.Korfage IJ, et al. Anxiety and depression after prostate cancer diagnosis and treatment: 5-year follow-up. British journal of cancer. 2006;94(8):1093–1098. doi: 10.1038/sj.bjc.6603057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faul LA, Jim HS, Williams C, Loftus L, Jacobsen PB. Relationship of stress managment skills to psychological distress and quality of life in adults with cancer. Psycho Oncology. 2010;19(1):102–109. doi: 10.1002/pon.1547. [DOI] [PubMed] [Google Scholar]
- 8.Ezer H, Ricard N, Bouchard L, Souhami L, Saad F, Aprikian A, Taguchi Y. Adaptation of wives of prostate cancer following diagnosis and 3 months after treatment: A test of the family adaptation theory. International Journal of Nursing Studies. 2006;43:827–838. doi: 10.1016/j.ijnurstu.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Docherty A, Brothwell CP, Symons M. The impact of inadequate knowledge on patient and spouse experience of prostate cancer. Cancer nursing. 2007;30:58–63. doi: 10.1097/00002820-200701000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Traeger L, Penedo FJ, Gonzalez JS, Dahn JR, Lechner SC, Schneiderman N, Antoni MH. Illness perceptions and emotional well-being in men treated for localized prostate cancer. Journal of psychsomatic Research. 2009;67:389–397. doi: 10.1016/j.jpsychores.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 11.Bailey J, D E, Wallace M, Mishel MH. Watching, waiting and uncertainty in prostate cancer. Journal of clinical nursing. 2007;16:734–741. doi: 10.1111/j.1365-2702.2005.01545.x. [DOI] [PubMed] [Google Scholar]
- 12.Penedo FJ, Dahn JR. Prostate cancer and QOL: Impact of treatment, disease burden and psychosocial interventions. Expert Review of Pharmacoeconomics & Outcomes Research. 2004;4:525–535. doi: 10.1586/14737167.4.5.525. [DOI] [PubMed] [Google Scholar]
- 13.Penedo FJ, et al. A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: development of stress management skills improves quality of life and benefit finding. Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine. 2006;31(3):261–270. doi: 10.1207/s15324796abm3103_8. [DOI] [PubMed] [Google Scholar]
- 14.Penedo FJ, et al. Cognitive behavioral stress management intervention improves quality of life in Spanish monolingual hispanic men treated for localized prostate cancer: results of a randomized controlled trial. International Journal of Behavioral Medicine. 2007;14(3):164–172. doi: 10.1007/BF03000188. [DOI] [PubMed] [Google Scholar]
- 15.Livingston P, White VM, Hayman J, Mauseli E, Dunn SM, Hill D. The psychological impact of a specialist referral and telephone intervention on male cancer patients: a randomised controlled trial. Psycho Oncology. 2010;19:617–627. doi: 10.1002/pon.1609. [DOI] [PubMed] [Google Scholar]
- 16.Marcus A, et al. Telephone counseling in psychosocial oncology: A report from the Cancer Information and Counseling Line. Patient Education and Counseling. 2002;46(4):267–275. doi: 10.1016/s0738-3991(01)00163-x. [DOI] [PubMed] [Google Scholar]
- 17.Secura KW, Budin W, Garfing E. Telephone social support and education for adaptation to prostate cancer: A pilot study. Oncology Nursing Forum. 2004;31:335–338. doi: 10.1188/04.ONF.335-338. [DOI] [PubMed] [Google Scholar]
- 18.Badger T, Segrin C, Figueredo AJ, Harrington J, Sheppard K, Passalacqua S, Pasvogel A, Bishop M. Psychosocial Interventions to improve quality of life among prostate cancer survivors and their partners. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2011;20(6):833–844. doi: 10.1007/s11136-010-9822-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pearlin LI, et al. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30(5):583–94. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 20.Judge KS, Menne HL, Whitlatch CJ. Stress process model for individuals with dementia. Gerontologist. 2010;50(3):294–302. doi: 10.1093/geront/gnp162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gaugler JE, et al. Cancer caregiving and subjective stress: a multi-site, multi-dimensional analysis. Psychooncology. 2005;14(9):771–85. doi: 10.1002/pon.916. [DOI] [PubMed] [Google Scholar]
- 22.Gaugler JE, et al. The proliferation of primary cancer caregiving stress to secondary stress. Cancer Nurs. 2008;31(2):116–23. doi: 10.1097/01.NCC.0000305700.05250.9d. quiz 124-5. [DOI] [PubMed] [Google Scholar]
- 23.Gaugler JE, et al. Family cancer caregiving and negative outcomes: the direct and mediational effects of psychosocial resources. J Fam Nurs. 2009;15(4):417–44. doi: 10.1177/1074840709347111. [DOI] [PubMed] [Google Scholar]
- 24.Mishel MH, Germino BB, Belyea M, Stewart JL, Bailey DE, Jr, Mohler J, Robertson C. Moderators of an uncertainty management intervention. Nursing research. 2003;52(2):89–97. doi: 10.1097/00006199-200303000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Knight SJ, Latina DM, Hart SL, Sadetsky N, Kane CJ, DuChane J, Carroll PR. Education predicts quality of life among men with prostate cancer cared for in the Department of Veterans Affairs. Cancer. 2007;109(9):1769–1776. doi: 10.1002/cncr.22597. [DOI] [PubMed] [Google Scholar]
- 26.Chambers SK, Ferguson M, Gardiner RA, Aitken J, Occhipinti S. Intervening to improve psychological outcomes for men with prostate cancer. Psycho Oncology. 2012 doi: 10.1002/pon.3095. [DOI] [PubMed] [Google Scholar]
- 27.Manne S, et al. Cancer-related communication, relationship intimacy, and psychological distress among couples coping with localized prostate cancer. J Cancer Surviv. 2010;4(1):74–85. doi: 10.1007/s11764-009-0109-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou ES, et al. Perceived stress mediates the effects of social support on health-related quality of life among men treated for localized prostate cancer. J Psychosom Res. 2010;69(6):587–90. doi: 10.1016/j.jpsychores.2010.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arora NK, et al. Perceived helpfulness and impact of social support provided by family, friends, and health care providers to women newly diagnosed with breast cancer. Psychooncology. 2007;16(5):474–86. doi: 10.1002/pon.1084. [DOI] [PubMed] [Google Scholar]
- 30.Helgeson VS, Cohen S. Social support and adjustment to cancer: reconciling descriptive, correlational, and intervention research. Health Psychol. 1996;15(2):135–48. doi: 10.1037//0278-6133.15.2.135. [DOI] [PubMed] [Google Scholar]
- 31.Zhou ES, et al. Longitudinal effects of social support and adaptive coping on the emotional well-being of survivors of localized prostate cancer. J Support Oncol. 2010;8(5):196–201. doi: 10.1016/j.suponc.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gotcher DF. Interpersonal communication and psychosocial adjustment. Journal of Psychosocial Oncology. 1992;10:21–39. [Google Scholar]
- 33.Kezia E, Rees CE. Information needs and information-seeking behaviors of men with prostate cancer and their partners. Cancer Nursing. 2002;25:35–41. doi: 10.1097/00002820-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Badger TA, S C, Figueredo AJ, Harrington J, Sheppard K, Passalacqua S, Pasvogel A, Bishop M. Psychosocial interventions to improve quality of life in prostate cancer survivors and their intimate or family partners. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2011 doi: 10.1007/s11136-010-9822-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weissman MM, Markowitz JC, Klerman GL. Comprehensive guide to interpersonal psychotherapy. New York: Basic Books; 2000. [Google Scholar]
- 36.Hendren S, Griggs JJ, Epstein RM, et al. Study protocol: A randomized controlled trial of patient navigation-activation to reduce cancer health disparities. BMC Cancer. 2010;10 doi: 10.1186/1471-2407-10-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 38.Badger TA, Segrin C, Dorros SM, Meek P, Lopez AM. Depression and anxiety in women with breast cancer and their partners. Nursing research. 2007;56:44–53. doi: 10.1097/00006199-200701000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Watson D, Clark LL, Tellegan A. Development and validation of brief measures of positive and negative affect: the PANAS sclae. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 40.Manne S, Schnoll R. Measuring cancer survivors’ psychological distress and well-being: A factor analytic assessment of the Mental Health Inventory. Psychological Assessment. 2001;13:99–109. [PubMed] [Google Scholar]
- 41.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of health and social behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 42.Procidano ME, Heller K. Measures of perceived social support from friends and from family: three validation studies. American Journal of Community Psychology. 1983;11(1):1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- 43.Litwin MS, Hays RD, Fink A, et al. The UCLA Prostate Cancer Index: Development, reliability and validity of a health related quality of life measure. Medical Care. 1998;36:1002–1012. doi: 10.1097/00005650-199807000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Karakiewicz PI, Kattan MW, et al. Cross-cultural validation of the UCLA prostate cancer index. Urology. 2003;61(2):302–307. doi: 10.1016/s0090-4295(02)02245-8. [DOI] [PubMed] [Google Scholar]
- 45.Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Hillsdale: Erlbaum; 2003. [Google Scholar]
- 46.McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychological Bulletin. 1993;114:376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- 47.McDowell ME, Occhipinti S, Ferguson M, Dunn J, Chambers SK. Predictors of change in unmet supportive care needs in cancer. Psycho Oncology. 2010;19:508–516. doi: 10.1002/pon.1604. [DOI] [PubMed] [Google Scholar]
- 48.Wong F, Stewart DE, Dancey J, Meana M, McAndrews MP, Bunston T, Cheung AM. Men with prostate cancer: influence of psychological factors on informational needs and decision making. Journal of Psychosomatic Research. 2000;49:13–18. doi: 10.1016/s0022-3999(99)00109-9. [DOI] [PubMed] [Google Scholar]
- 49.IOM. Cancer Care for the whole patient: Meeting psychosocial health needs. The National Academies Press; Washington, D.C: 2007. [PubMed] [Google Scholar]
- 50.Northouse LL, et al. Living with prostate cancer: patients’ and spouses’ psychosocial status and quality of life. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2007;25(27):4171–4177. doi: 10.1200/JCO.2006.09.6503. [DOI] [PubMed] [Google Scholar]
- 51.Given C, et al. Does a symptom management intervention affect depression among cancer patients: results from a clinical trial. Psycho-oncology. 2004;13(11):818–830. doi: 10.1002/pon.807. [DOI] [PubMed] [Google Scholar]
- 52.Given B. Cancer-related fatigue: a brief overview of current nursing perspectives and experiences. Clinical journal of oncology nursing. 2008;12(5 Suppl):7–9. doi: 10.1188/08.CJON.S2.7-9. [DOI] [PubMed] [Google Scholar]
- 53.Given B, et al. The impact of providing symptom management assistance on caregiver reaction: results of a randomized trial. Journal of pain and symptom management. 2006;32(5):433–443. doi: 10.1016/j.jpainsymman.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 54.Davison BJ, Goldenberg SL, Gleave MF, Degner LF. Provision of individualized information ot men and their partners to facitlitate treatment decision making in prostate cancer. Oncology nursing forum. 2003;30(1):107–114. doi: 10.1188/03.ONF.107-114. [DOI] [PubMed] [Google Scholar]


