Abstract
Colour imaging of fundus tumours has been transformed by the development of digital and confocal scanning laser photography. These advances provide numerous benefits, such as panoramic images, increased contrast, non-contact wide-angle imaging, non-mydriatic photography, and simultaneous angiography. False tumour colour representation can, however, cause serious diagnostic errors. Large choroidal tumours can be totally invisible on angiography. Pseudogrowth can occur because of artefacts caused by different methods of fundus illumination, movement of reference blood vessels, and flattening of Bruch's membrane and sclera when tumour regression occurs. Awareness of these pitfalls should prevent the clinician from misdiagnosing tumours and wrongfully concluding that a tumour has grown.
Keywords: uveal neoplasms, melanoma, naevus, fundus photography, scanning laser ophthalmoscopy, artefacts
Introduction
Fundus photography is almost indispensable in the management of patients with choroidal tumours. Baseline colour pictures are essential for monitoring indeterminate tumours (for example, ‘suspicious naevi'), and for detecting recurrence of tumours after therapy. In recent years, many different fundus cameras have been developed, bringing many benefits such as digital imaging and panoramic photographs. Unlike conventional photography, which captures a comprehensive picture, optically adding all layers and mainly imaging the superficial tissue layer, confocal laser scanning techniques produce tomographic images of the target tissue, focussing on one layer at a time, so that deeper, ‘hidden' layers are seen. The published literature on the pitfalls of colour photography of choroidal tumours is scarce.1 In this article, we describe some of the errors that can occur.
Evolution towards modern colour imaging of uveal tumours
Standard fundus photography captures only up to 60° of the fundus in a single image. Digital imaging with transpupillary illumination has not significantly increased the field of view nor altered visualisation of tumour characteristics. The first wide-angle retinal photograph was produced with the Equator-plus Camera, developed by Pomerantzeff2 in 1975, which imaged almost 150° of the fundus, using a corneal contact device as part of the camera optics and a fibre optic, trans-scleral transilluminator.3 The RetCam is a 120° wide-field digital imaging system, using a handheld video camera with a coaxial light source. It requires clear media so that its application is limited to paediatrics. It has transformed the management of patients with retinoblastoma. In 2002, the Panoret-1000, a wide field (100°), digital, and high-definition fundus camera came on the market.4 As with its Equator-plus predecessor, it uses a specially-designed, corneal contact lens and the same transillumination principle, but the comprehensive colour images are digitally recomposed from the three primary colours (red, green and blue) reflected by the fundus. Even with a pupil diameter as small as 2.5 mm, fundus imaging is possible, as is the case with the more recent, ultra-widefield (200°) Optos camera.5 As the latter uses a confocal scanning laser imaging technology, it has the advantage of being a non-contact camera, also providing simultaneous ultra-widefield fluorescein angiography and autofluorescence. However, the Optomap has the disadvantage of limiting its ultra-wide angle mainly to the horizontal axis, with eyelashes sometimes obscuring fundus details. Moreover, colour images are recomposed with only two reflected monochromatic laser images (red: 633 nm and green: 532 nm), resulting in unnaturally coloured fundus pictures (Figure 1). The newer Spectralis Multicolor6 is also based on confocal scanning laser technology, reconstructing its images with three simultaneously acquired colour laser images reflected in the blue, green and infrared spectrum, and using the same lasers to perform fluorescein and indocyanine green (ICG) angiography. Currently, its viewing angle is limited to 30°. The wide angle version has yet to be brought on the market.
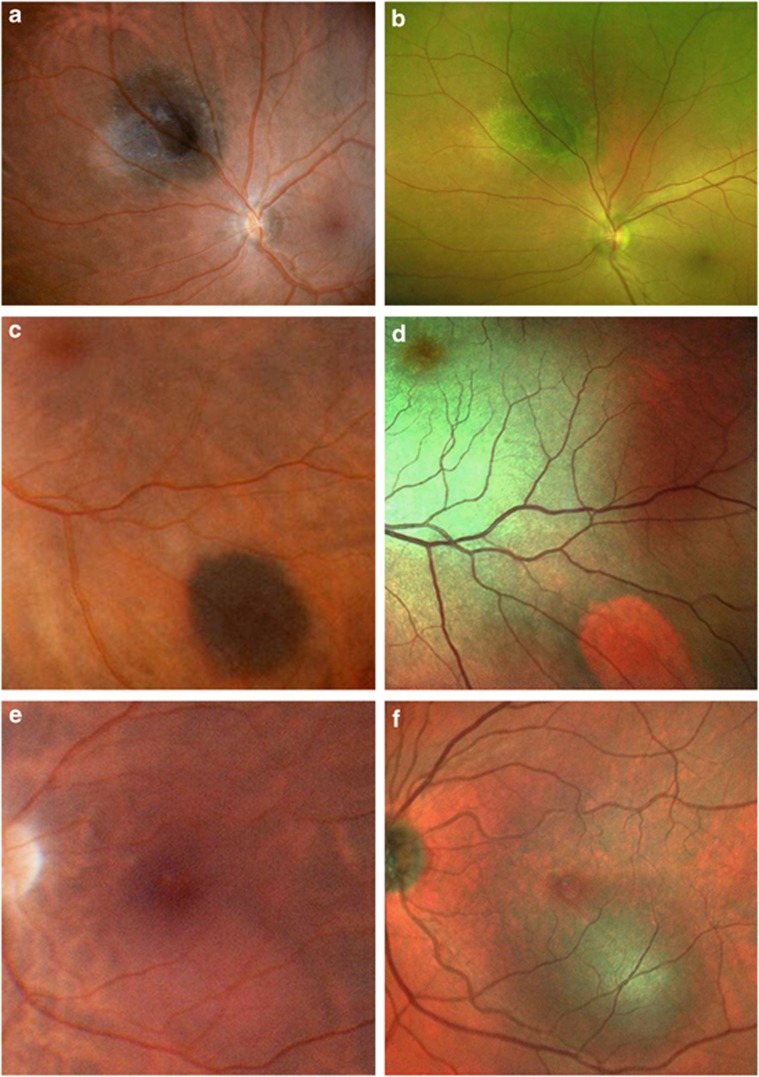
Figure 1.
Different cameras, different colours. Small choroidal melanoma photographed with the Panoret (a) and Optos (b) cameras, the latter producing a false, green colour because it uses only two laser colours. Choroidal naevus imaged with the Panoret (c) and Spectralis Multicolor (d) cameras, the naevus taking an orange-red appearance, suggestive of a haemangioma, with the latter. Circumscribed choroidal haemangioma, inferior to the fovea, imaged using the Panoret (e) and Spectralis Multicolor (f) cameras, the latter misleadingly suggesting a pigmented naevus or melanoma.
Pitfalls of fundus photography
1. Different cameras, different colours
Colour is one of the most important diagnostic features of choroidal tumours. Melanomas tend to be brown, grey, black, or white. Haemangiomas are usually orange-red. Most metastases are white, with the exception of renal and carcinoid secondaries, which can be orange.
Digital cameras use a variety of algorithms to ‘reconstitute' fundus colours, sometimes producing images that do not reflect reality (Figure 1a and b). These false colours can seriously mislead the clinician so that the wrong diagnosis is made (Figure 1c–f). If possible, tumours should be examined ophthalmoscopically without relying entirely on photographs.
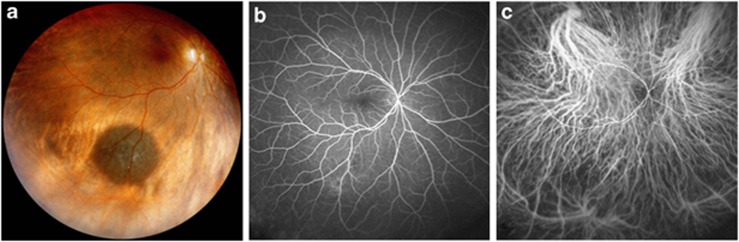
2. Angiography does not reveal every tumour
When deploying angiography for the assessment of a recently discovered choroidal tumour, colour photography might mistakenly be considered as optional, because of its additional cost; however, fluorescein and ICG angiography, although useful, cannot replace colour fundus photography.7 Indeed, angiograms cannot adequately be interpreted without colour photographs. Moreover, when monitoring an indeterminate tumour (for example, ‘suspicious naevus'), a colour fundus picture clearly demonstrating the entire tumour margin is essential. Fluorescein and ICG angiography do not adequately define the tumour extent or may not show the lesion at all (Figure 2).
Figure 2.
The disappearing tumour. A large choroidal naevus, clearly visible on the Panoret picture (a), was examined with fluorescein (b) and ICG (c) angiography (Heidelberg Engineering Spectralis Widefield imaging using a Staurenghi 150° contact lens8), on which the melanocytic tumour does not appear at all.
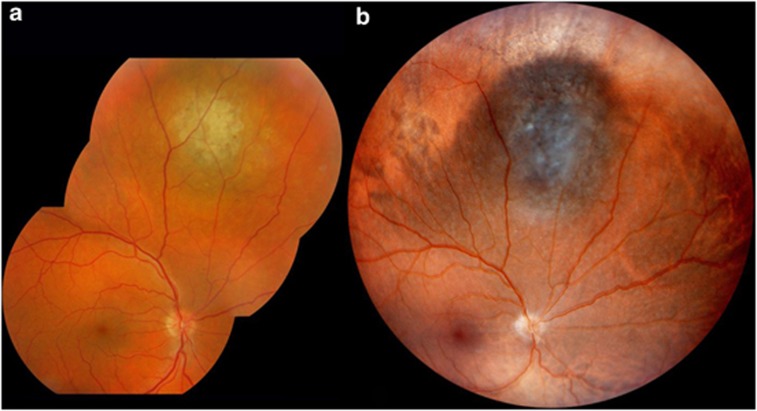
3. Transpupillary illumination underestimates tumour extent
Conventional fundus cameras may not demonstrate the true extent of diffuse tumours. This is because they use transpupillary illumination, which is mostly reflected by the retinal pigment epithelium and inner choroid, so that tapering tumour edges are obscured. Trans-scleral illumination allows more accurate definition of tumour extent, because it provides a better contrast between tumour margins and surrounding tissues (Figure 3). This pitfall should be taken into account when comparing sequential images taken with different methods of fundus illumination.
Figure 3.
Pseudogrowth evoked by trans-scleral illumination. Colour picture of a large naevus in the superior choroid, taken with transpupillary (a, IMAGEnet Topcon camera) and trans-scleral (b, Panoret camera) illumination on the same day. The tumour appears larger and sharper defined on the latter photo.
Eyes with extensive ocular melanocytosis cannot be photographed with transscleral illumination, as the pigmented choroid and sclera block the light from reaching the fundus. In these cases, a scanning laser camera offers the only wide angle alternative to preparing montages of conventional fundus photographs.
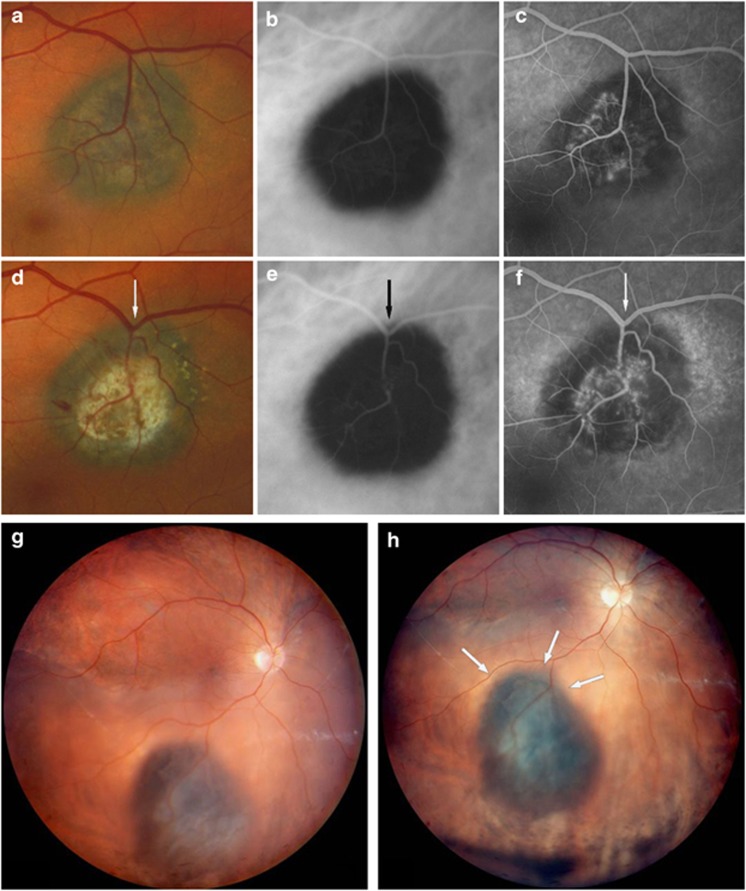
4. Retinal vessels are not always reliable points of reference
Surveillance of fundus tumours involves assessment of the lesion margins, to detect growth or recurrence. This is done by estimating the distance between the tumour borders and ‘stable' points of reference such as retinal blood vessels, choroidal blood vessels and the optic disc. However, retinal vessels can move, as a result of fibrosis (Figure 4a–f), shifting retinal detachment (Figure 4g and h), or when detached retina flattens. These retinal movements can create a false impression of tumour growth or recurrence.
Figure 4.
Dislocated blood vessels simulating pseudogrowth. Small choroidal naevus complicated by choroidal neovascularisation, treated with laser photocoagulation, which has resulted in traction of the retinal vein towards the tumour, mimicking tumour progression. Standard colour photography (a, d), ICG (b, e), and fluorescein (c, f) angiography, before (a–c) and after (d–f) laser therapy. Panoret fundus picture of a dome-shaped choroidal melanoma with secondary retinal detachment at presentation, with the patient lying down (g) and seated upright (h). Both pictures were taken on the same day. Shifting of the serous retinal detachment has moved the retinal vein closer to the superior tumour border (white arrows).
5. The basal diameter of a regressing tumour can increase
A choroidal melanoma is sandwiched between Bruch's membrane and the sclera, both of which are pushed away from each other as tumour growth occurs. Bruch's membrane therefore bulges inwards and, to a lesser extent, the sclera bulges slightly outwards. After radiotherapy, tumour regression eases the pressure off Bruch's membrane and the sclera, both of which resume their original, flatter shape. This flattening has the effect of increasing the basal diameter of regressing tumour, giving a false impression of growth (Figure 5).
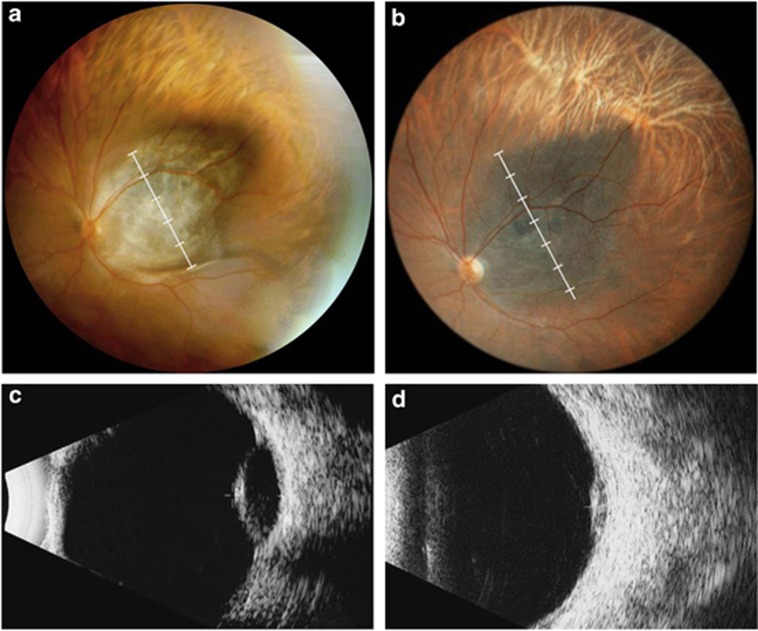
Figure 5.
Regressing tumour, increasing basal diameter. Dome-shaped choroidal melanoma, before (a) and two years after (b) proton therapy (Panoret camera). While the tumour thickness has decreased from 5.8 mm (c) to 2.0 mm (d) on B-scan ultrasonography, the apparent tumour diameter has increased by at least one disc diameter (compare white rulers), because of inward flattening of the underlying sclera.
Conclusions
The development of digital and confocal scanning laser technology has provided many benefits, which include wide angle photography, increased contrast, non-contact imaging, non-mydriatic fundus photography, and simultaneous angiography. However, there are many pitfalls. Grey tumours may appear green, and orange tumours may look brown or white. False colour can result in serious misdiagnosis so that the wrong treatment is administered. Apparent tumour extent can vary considerably according to whether photographs are taken with trans-pupillary or trans-scleral illumination. Misleading impressions of tumour growth can arise because reference points move or because Bruch's membrane and sclera flatten with tumour regression. Clinicians should be aware of the limitations of fundus cameras when using colour photography to diagnose and monitor choroidal tumours.
Acknowledgments
We would like to thank Dr Line Chamot, Prof Bertil Damato and Mr Marc Curchod for their critical review of this paper, as well as the whole photographic team of the Jules–Gonin Eye Hospital for their relentless efforts to produce high quality pictures, all the while adopting the latest technologies.
The authors declare no conflict of interest.
Footnotes
This paper was presented at the Cambridge Ophthalmological Symposium 2012
References
- Johnson RN, McDonald HR, Ai E, Jumper JM. Camera artifacts producing the false impression of growth of choroidal melanocytic lesions. Am J Ophthalmol. 2003;135:711–713. doi: 10.1016/s0002-9394(02)02159-1. [DOI] [PubMed] [Google Scholar]
- Pomerantzeff O. Equator-plus camera. Invest Ophthalmol. 1975;14 (5:401–406. [PubMed] [Google Scholar]
- Ducrey N, Pomerantzeff O, Schepens CL, Delori FC, Schneider J. Clinical trials with the Equator-Plus camera. Am J Ophthalmol. 1977;84 (6:840–846. doi: 10.1016/0002-9394(77)90507-4. [DOI] [PubMed] [Google Scholar]
- Walsh JB, Garcia JPS, Nieto JC, Rosen RB, Garcia PT, Fradin S.Wide-Angle Digital Fundus Photography: Panoret 1000 vs RetCam 120 Invest Ophthalmol Vis Sci 200243E-Abstract4370 [Google Scholar]
- Optomap Product descriptionAvailable at: http://www.optos.com/en-GB/Professionals/Ophthalmology/Product-description/ . Accessed 20 October 2012.
- Spectralis Multicolor Scanning Laser Imaging Available at: http://www.heidelbergengineering.com/international/products/spectralis/imaging-modes/multicolor/ . Accessed 20 October2012
- Meyer K, Augsburger JJ. Independent diagnostic value of fluorescein angiography in the evaluation of intraocular tumors. Graefes Arch Clin Exp Ophthalmol. 1999;237:489–494. doi: 10.1007/s004170050267. [DOI] [PubMed] [Google Scholar]
- Staurenghi G, Viola F, Mainster MA, Graham RD, Harrington PG. Scanning laser ophthalmoscopy and angiography with a wide-field contact lens system. Arch Ophthalmol. 2005;123:244–252. doi: 10.1001/archopht.123.2.244. [DOI] [PubMed] [Google Scholar]