Abstract
Aims
The advanced specialist diploma in ophthalmic pathology was jointly ratified by the Royal College of Pathologists and the Institute of Biomedical Science in 2008. It results in extended roles for suitably qualified Biomedical Scientists (BMSs) in ophthalmic pathology specimen dissection and histological reporting of selected specimens, specifically non-neoplastic corneas. This study aimed to examine the reporting of corneal histology by a BMS training towards this diploma in comparison with a Consultant Ophthalmic Pathologist.
Methods
This report covers a non-interventional, prospective examination of BMS's diagnostic skills. After 6 months training, 50 consecutive corneal cases were reported by the BMS and the same case reported by the consultant ophthalmic pathologist. The BMS's diagnosis was compared with the final consultant's diagnosis. This exercise was then repeated after 24 months of training.
Results
After 6 months, the BMS's diagnoses matched the consultant diagnoses in 44/50 (88%) cases. After 24 months, the BMS's diagnoses matched the consultant diagnoses in 48/50 (96%) of cases.
Conclusions
The results indicate that BMS's reporting of corneal histology is a real and safe possibility. Furthermore, it indicated deficiencies in BMS's diagnostic skills to inform further training/knowledge acquisition.
Keywords: histopathology, cornea, biomedical scientist
Introduction
In recent times, there have been steps towards extended roles in histopathology departments, to allow senior biomedical scientist (BMS) staff to perform certain selected tasks, normally performed by medically trained staff. This reflects the general increase in ‘skill mix' occurring in other areas within the NHS, as recommended in various publications by the Department of Health.1, 2, 3
The example par excellence of an extended role is that of the advanced practitioner in gynaecological cytology. Put in place in 2000/2001 after a working party report by the Royal College of Pathologists (RCPath) into the roles of staff in the National Health Service Cervical Screening Programme (NHSCSP),4, 5, 6 this role allows BMS staff to report abnormal cervical smear samples, give advice on patient management and present cases at multi-disciplinary team meetings. There has also been some work to develop this role to report cervical histology, although this is still at an early stage.7
The Institute of Biomedical Science (IBMS)/RCPath Certificate of Advanced Practice in Ophthalmic Pathology was ratified in 2008, in response to the Report of the Joint Woking Party of the Royal Colleges of Ophthalmologists (RCOphth) and Pathologists (RCPath), concerned with training and BMS manpower in ophthalmic pathology. In England, there are four centrally funded centres for ophthalmic pathology, which together form the National Specialist Ophthalmic Pathology Service. In these centres, consultant pathologists are funded alongside specialist BMS staff, part of whose job description is to undertake the Institute of Biomedical Science/RCPath certificate of advanced practice in ophthalmic pathology. Training is expected to take between 3 and 5 years.
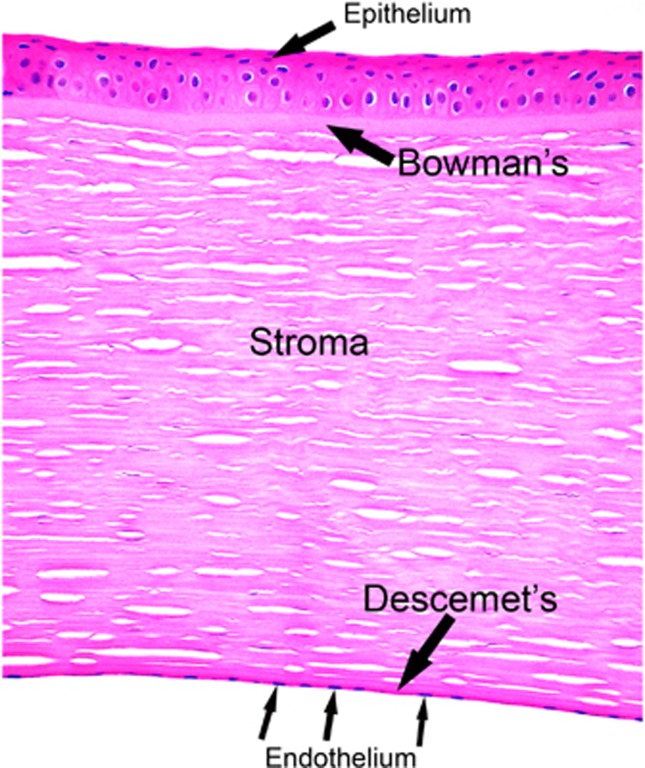
One of the new responsibilities of this post is for a BMS to become proficient in the histopathological reporting of non-neoplastic ophthalmic pathology specimens, exclusively corneas and end-stage eyes. The cornea is a simple anatomical structure with a stereotyped pathological response. Its stratified architecture allows a systematic approach to diagnosing pathological states affecting it (Figure 1). The cornea consists of five layers: the external epithelium that is non-keratinising, non-secretory epithelium and is up to five cells thick. The next layer is Bowman's, which is an acellular, eosinophilic band, thought to represent an anterior condensation of the stroma. The stroma is the thickest part of the cornea and is composed of collagen and fibroblasts (called keratocytes). The inner corneal layers comprise Descemet's layer, which is the basement membrane of the endothelial cell layer.8, 9 The endothelial cell layer contains an active water pump that keeps the stroma in a state of constant dehydration. Any damage or loss of endothelial cells leads to failure of this pump, resulting in oedema of the cornea with visual disturbance.
Figure 1.
H&E showing a normal cornea. The cornea has five layers. The surface epithelium, is composed of stratified squamous, non-keratinising, non-secretory epithelium and is usually up to five cells thick. Bowman's layer is an acellular anterior condensation of the stroma. The stroma is composed of regular arranged collagen, made by the stromal fibroblasts. The clefts appear during normal histological processing. Descemet's membrane is a basement membrane. The endothelial cells secrete Descemet's and possess a water pump that keeps the cornea in a constant state of dehydration.
Materials and methods
After 6 months in post, the BMS reported 50 consecutive, prospective corneal histology cases. These were then reported separately by the consultant pathologist. After 24 months training, the process was repeated on a separate 50 consecutive, prospective cases. These cases were then reported separately by the consultant pathologist. The report given by the Consultant was issued as the final histology report.
After both 6 and 24 months, the 50 cases were first examined by the BMS. The BMS indicated the histological features and diagnosis on a specially designed proforma (Table 1). The same 50 cases were then examined by the consultant, a parallel proforma completed, followed by a joint review of the slides and proformas. In cases where there was a discrepancy in diagnosis, the forms and slides were scrutinised to discover where the BMS had made overcalls or undercalls in histological features that had lead to the incorrect diagnosis. Any histological features noted that were not listed on the proforma could be added by hand.
Table 1. Proforma of histological features used in the study.
| Epithelium |
| Oedema |
| Atrophy |
| Hyperplasia |
| Bullous lifting |
| Subepithelial basement membrane |
| Conjunctivilsation |
| Pannus |
| Ulcer |
| Basal vacuole damage |
| Bowman's |
| Effaced |
| Breaks |
| Stroma |
| Scarring |
| Inflammation: acute; chronic; acute and chronic |
| Deposits (qualify) |
| Vascularisation |
| Implants |
| Thinning |
| Keratocyte cell loss |
| Infective agent: bacteria; fungi; protozoa; other (qualify) |
| Ulcer |
| Non-melt perforation |
| Melt |
| Host–donor interface |
| Band keratopathy |
| Spheroidal droplet keratopathy |
| Lipid keratopathy |
| Descemet's |
| Normal |
| Thin |
| Thickened |
| Ruptured |
| Reduplication |
| Guttae |
| Folds |
| Endothelium |
| Normal |
| Loss |
| Multilayered |
| Contain pigment |
| Deposits |
| Retrocornea |
| Inflammation |
| Fibrosis |
| Attached iris |
| Attached lens |
| Epithelial ingrowth |
Results
After 6 months, in 44/50 (88%) of cases, the BMS's diagnosis matched the consultant's diagnosis; however in 6 cases, (12%), the BMS made an incorrect diagnosis.
After 24 months, in 48/50 (96%) of cases, the BMS's diagnosis matched the consultants diagnosis; however in 2 cases (4%), the BMS made an incorrect diagnosis.
Cases where the diagnosis did not agree are summarised below:
After 6 months
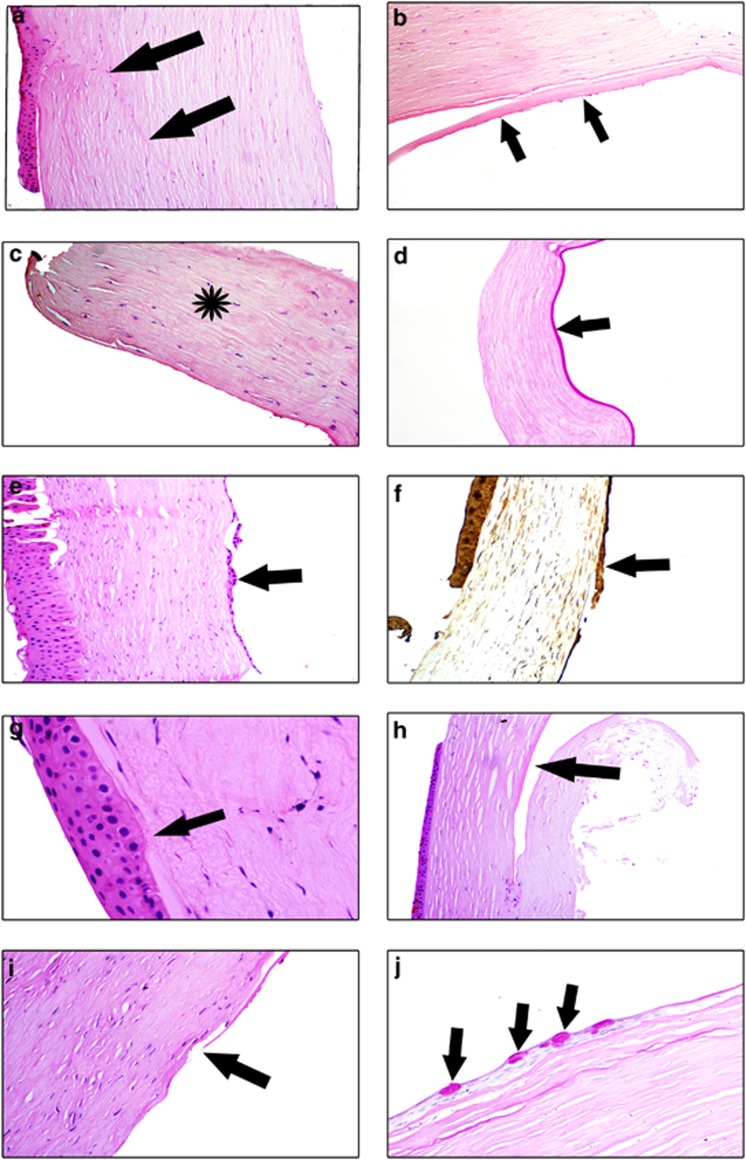
In case 1, the BMS missed a host–donor interface and lack of recognition of loss of endothelial cells, so the diagnosis of graft failure was not possible (Figures 2a and b).
Figure 2.
(a) H&E stain: the black arrow points to the host–donor interface that was missed. (b) H&E stain: this is the same case as (a) and the arrows indicate absence of endothelial cells over the retrocorneal face that were missed. (c) H&E stain: the asterisk is normal corneal stroma. This was interpreted as retrocorneal fibrosis. (d) PAS stain: the same case as (c). The arrow points to a thickened Descemet's layer that was missed. (e) H&E stain: the black arrow points to the epithelial ingrowth that was missed. (f) Immunohistochemistry for Cytokeratin 7. The arrow points to the epithelial ingrowth from the case shown in (e). (g) H&E stain: the arrow points to a break in Bowman's layer that was missed. (h) H&E stain: same case as (g). The arrow points to a space that is the point of insertion of the intrastromal ring (INTAC) prosthesis. (i) H&E stain: the arrow points to a break in Descemet's and the loss of endothelial cells that were both overlooked. (j) PAS stain: Goblet cells on the corneal surface indicating conjunctivilisation. This was missed.
In case 2, Descemet's thickening was missed with an overcall of retrocorneal fibrosis (Figures 2c and d). This led the BMS to think that the loss of endothelial cells was due to an acute retrocorneal fibrosis rather than a chronic loss of endothelial cells.
In case 3, the BMS missed an epithelial ingrowth and overcalled retrocorneal fibrosis. The BMS instead interpreted the epithelial ingrowth as multi-layering of endothelial cells compatible with a diagnosis of posterior polymorphous dystrophy. The BMS clearly observed abnormality at the retrocorneal face but lacked the knowledge to interpret it safely (Figures 2e and f).
In case 4, the BMS missed breaks/irregularities in Bowman's and the INTAC site in the corneal stroma, leading to a missed diagnosis of an intrastromal ring (INTAC)-treated keratoconus (Figures 2g and h).
With case 5, the BMS missed the ruptured Descemet's and the endothelial cell loss. While keratoconus was mentioned, the hydrops was missed (Figure 2i).
In case 6, the BMS missed cojunctivilisation of the corneal epithelium indicative of limbal stem cell deficiency (Figure 2j).
After 24 months
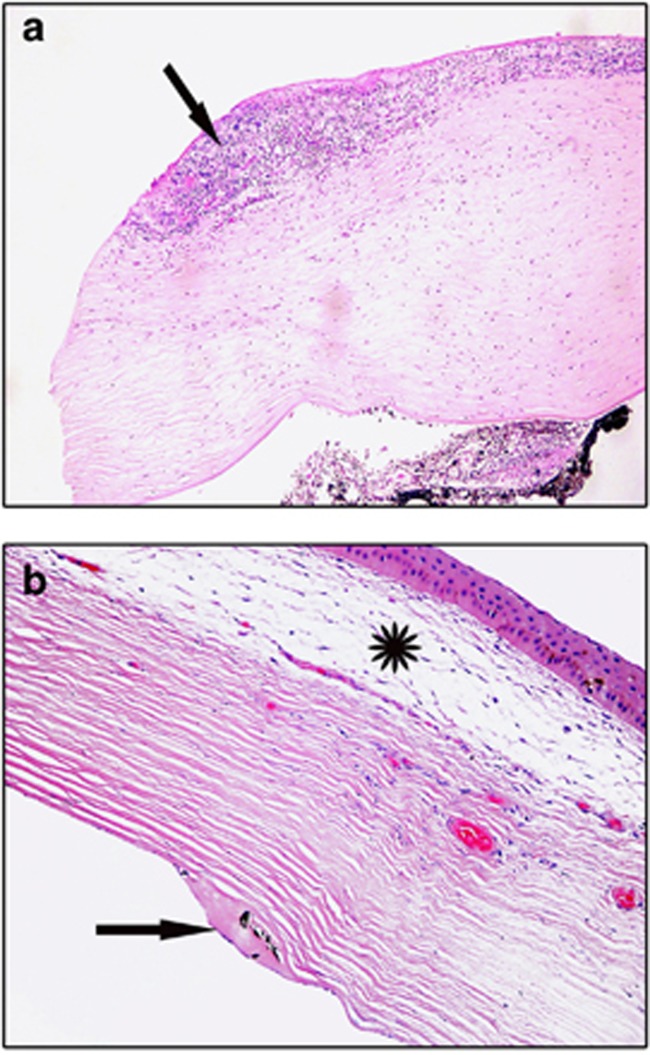
In case 1, the BMS failed to associate the marginal nature of the pathology with the diagnosis of marginal keratitis. The BMS noted all the histological changes but failed to mention the possibility of marginal keratitis in the final report, which may have altered clinical treatment, for example, the exclusion of an autoimmune aetiology by serology/autoantibody studies. (Figure 3)
Figure 3.
(a) The arrow points to the marginal chronic inflammation of the cornea. (b) The asterisk indicates the area of hydrops and the arrow shows the point of Descemet's regeneration post rupture.
In case 2, the BMS misinterpreted an area of hydropic change and missed a rupture of Descemets in a case of healed infectious keratitis. The diagnosis given by the BMS was that of healed infectious keratitis but with no mention on hydrops. This however would not have altered the clinical management (Figure 3)
Discussion
This study has shown that BMS reporting of corneal pathology is viable. The BMS had been in post for 6 months before participating in the first part of the study. An encouraging diagnostic correlation of 88% after 6 months is a clear indication that the BMS had acquired a high level of histological recognition skills. This then improved to 96% after 24 months. It is worth noting that the BMS have another 18 months in post before the Certificate of Advanced Practice in Ophthalmic Pathology exam will be attempted. As an indication of the breadth of diagnoses reached in the cases examined, the breakdown of all 100 cases is: 21 cases of keratoconus, 20 cases of bullous keratopathy, 14 dystophy cases, 12 cases of graft failure, 10 cases of chronic keratitis, 8 cases of Fuch's endothelial dystrophy, 6 cases of acute keratitis, 3 cases of corneal melt, 3 epithlelial ingrowth cases and 1 case each of Salzmann's degeneration and interstitial keratitis, and 1 case of secondary lipid keratopathy of unknown cause.
The exercise has informed future study for the BMS involved and anyone else who may be thinking of undertaking the Certificate of Advanced Practice in Ophthalmic Pathology. The study has highlighted areas of weakness in the initial stages of training in cornea pathology recognition and interpretation by the BMS and has permitted the consultant supervisor to concentrate on specific targeted areas of the BMS's knowledge deficiency.
Our laboratory receives in the region of 150 corneas per annum and it is anticipated that most of these cases will be reported and signed out by the BMS after appropriate assessments. With this in mind, it is important to consider the external quality assessment of this work. All consultant pathologists are required to participate in an external quality assessment scheme in their chosen histopathological sub-speciality. No such scheme exists for BMS reporting corneal histology yet and this will need to be considered for educational and probity issues.
A deficiency of this study was the lack of participants. Comparisons between different observers would have been much more illuminating, especially as the BMS in this study (AM) has been exclusively trained by one consultant ophthalmic pathologist (HSM). This exercise would also have been improved by the addition of having the cases reported by an external ophthalmic pathologist, as the BMS has been exclusively (to this point) trained by the Consultant in the study.
Overall, the study proved to be a very useful learning tool. The results show that the BMS reporting of corneal histology is a real and safe possibility, although more training is needed for the individual involved, which will be provided by completing the RCPath/IBMS Certificate of Advanced Practice in Ophthalmic Pathology.
The authors declare no conflict of interest.
References
- Department of Health Making the Change: a Strategy for the Professions in Healthcare ScienceDepartment of HealthDH Publications: London; 2001 [Google Scholar]
- Department of Health Modernising Pathology ServicesDepartment of HealthDH Publications: London; 2004 [Google Scholar]
- Lord Carter of Coles Report of the Review of NHS Pathology Services in EnglandDepartment of HealthDH Publications: London; 2006 [Google Scholar]
- Royal College of Pathologists Proposal for the Introduction of Advanced Practitioners into the NHSCSP. Working Party on Professional Roles in Cervical Screening. 2000.
- Smith PA, Hewer EM. Examination for the Certificate in Advanced Practice in Cervical Cytology—the first year's experience. Cytopathology. 2003;14:101–104. doi: 10.1046/j.1365-2303.2003.00052.x. [DOI] [PubMed] [Google Scholar]
- Symonds M. Working as an advanced biomedical science practitioner in cervical cytology. Cytopathology. 2003;14:105–106. doi: 10.1046/j.1365-2303.2003.00043.x. [DOI] [PubMed] [Google Scholar]
- Ellis K, Perunovic B, Dudding N, Smith JHF.Proposal for extending the role of ABMSPS in reporting of cervical loops [abstract] Cytopathology 200718(Suppl 113–18.17250598 [Google Scholar]
- Eagle RC. Eye Pathology an Atlas and Basic Text. WB Saunders Company: Philadelphia; 1999. [Google Scholar]
- Lee WR.Ophthalmic Histopathology2nd ednSpringer-Verlag: London; 2002 [Google Scholar]