Abstract
Background:
There are very few studies from India which have evaluated the prescription pattern for antidepressants by psychiatrists for treatment of depression.
Aim:
To study the psychotropic prescription patterns of patients with first episode depression from diverse settings including teaching institutions in public and private sectors and even privately run psychiatric clinics.
Materials and Methods:
Prescription data of 706 patients with first episode depression, who participated in the IPS multicentric study, were evaluated.
Results:
Escitalopram was the most commonly prescribed antidepressant, comprising 40% of the total prescriptions. This was followed by sertraline (17.6%) and fluoxetine (16.3%). In total, selective serotonin reuptake inhibitors (SSRIs) formed 79.2% of all the prescriptions. Tricyclic antidepressants formed a small part (15.15%) of total prescriptions, with imipramine being the most commonly used tricyclic antidepressant. Serotonin-norepinephrine reuptake inhibitors (venlafaxine, desvenlafaxine and duloxetine) were prescribed to 11.3% of patients with equal share of venlafaxine and duloxetine. About one-sixth (N=104; 14.7%) of the patients were prescribed more than one antidepressant. Nearly three-fourth of the patients (N=523; 74.1%) were prescribed a benzodiazepine, with clonazepam being the most preferred agent, prescribed to nearly half of the participants (49%) and formed nearly two-third of the total benzodiazepine prescriptions (346 out of 523).
Conclusion:
Escitalopram is the most commonly prescribed antidepressant and SSRIs are the most commonly prescribed class of antidepressants. Poly pharmacy in the form of concomitant use of two antidepressants is practiced infrequently. However, benzodiazepines are used quite frequently as the co-prescription.
Keywords: Antidepressants, depression, prescriptions
INTRODUCTION
Antidepressants form part and parcel of management of depression in majority of the cases. Over the years, the number of antidepressants available in India has increased and almost all the antidepressants available across the world are now available in India at an affordable price.
However, there is relative lack of data with respect to the prescription of antidepressants in India.
Very few studies have evaluated the prescription patterns of antidepressants from India. These studies have been invariably limited to only a particular center and there are no studies which have evaluated the prescription patterns across various treatment centers. A retrospective study from North India evaluated the antidepressants prescriptions of 108 patients of depression for the year 1996 and reported imipramine to be the most commonly prescribed antidepressant followed by fluoxetine.[1] Another study evaluated the antidepressant prescription of 100 patients of depression and reported duloxetine to be the most commonly prescribed agent. About one sixth of the patients received more than one antidepressant and most of the patients were co-prescribed benzodiazepines, with clonazepam prescribed in 84% of cases, lorazepam in 73% of cases and nitrazepam in 46% of cases.[2] In a recently published study, first prescriptions given to patients of depressive disorders attending the walk-in-clinic of a tertiary care center were evaluated. This study showed that escitalopram was the most commonly prescribed antidepressant; this was followed by sertraline, paroxetine, and venlafaxine. Among the benzodiazepines, clonazepam was the most commonly prescribed agent; this was followed by lorazepam.[3]
Indian Psychiatric Society took an initiative to carry out a multicentric study which aimed to evaluate functional somatic complaints in patients of depression. This study was spread over 16 centers across the country and provided a unique opportunity to study the prescription patterns of patients with depression. Accordingly, the aim of this paper is to present the data with respect to antidepressant prescriptions of patients with first episode depression.
MATERIALS AND METHODS
This was a multicentric study, funded by the Indian Psychiatric Society, which aimed to assess the typology of functional somatic complaints in patients with depression. Patients were recruited after proper written informed consent and the study was approved by the ethics committees of the Institutes or local ethics committees of the centers where the study was conducted. Patients were recruited across 16 centers, with four centers each in the south zone and east zone, three centers each in the north and west zone and two centers in the central zone of Indian Psychiatric Society. Sixteen centers across the country participated in the study, of which four centers each were in the south zone and east zone, three centers each in the north and west zone and two centers in the central zone of Indian Psychiatric Society. From the east zone the participating centers were at Kolkata, Patna, Tezpur and Guwahati and from north zone the participating centers were at Chandigarh, New Delhi and Ludhiana. The four centers in the south zone were located at Bengaluru, Chennai, Hyderabad and Manipal and the centers in the central zone were at Agra and Lucknow. Centers in the west zone were located at Ahmedabad, Mumbai and Wardha. Of the various centers, four centers were in the centrally funded Institutes with two having general hospital psychiatric units (Chandigarh, New Delhi) and two were in mental hospital set up (Bengaluru and Tezpur). Six centers were in the state Government run Medical Colleges (Ahmedabad, Kolkata, Lucknow, Mumbai, Patna, Guwahati), three centers were in privately run medical colleges (Chennai, Manipal, Wardha), two in privately run clinics (Hyderabad and Ludhiana) and one center was in state funded Mental Hospital (Agra).
To be included in the study the patients were required to fulfill the criteria for Major Depressive Disorder as per DSM-IV, aged between 16-65 years, having symptoms of depression for at least one month. Patients with diagnosis of severe depression with psychotic symptoms, comorbid psychiatric disorders, substance use disorders including heavy smoking, organic brain syndromes and chronic, debilitating physical illnesses like diabetes, hypertension and end stage organ failure were excluded.
Procedure
Patients with a clinical diagnosis of depression and meeting the inclusion and exclusion criteria were approached for participation in the study. They were explained about the nature of the study and patients who agreed to participate and provided informed consent were recruited. The diagnosis of major depressive disorder was confirmed by using Mini International Neuropsychiatric Interview (MINI)[4,5] and the same instrument was used to rule out other psychiatric disorders.
The documentation of clinical profile of the study involved noting down of the prescription given to the patients. The prescription data was extracted for this study.
Statistical analysis
Descriptive analysis in terms of mean and standard deviation with range for continuous variables and frequency with percentage for ordinal and nominal variables was computed. When a patient was prescribed more than one antidepressant then all the antidepressants were included independently while calculating the frequency of a particular agent.
RESULTS
Across the 16 centers, 746 patients were recruited for the study. However, five patients was excluded due to the age of participants being more than 65 years (n=4) and incomplete data (n=1). Of the remaining 741 patients, 35 patients were excluded because of lack of prescription data. Of the 706 patients, 214 patients were from East zone, 140 were from North zone, 116 from South zone, 120 from Central zone and 116 from West zone.
Sociodemographic profile
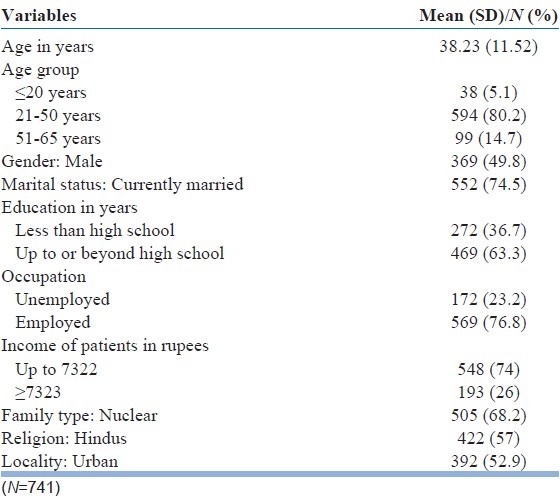
The sociodemographic profile of the study participants (n=746) is shown in Table 1. There was no significant difference in sociodemographic profile of patients included and those excluded from the analysis of prescription patterns. The mean age of the patients was 38.23 years (range16-65), with about 80% of patients in the age group of 21-50 years. There was nearly equal gender distribution. Majority of the participants were married, educated up to or beyond high school level, were employed, were earning less than rupees 7322 and belonged to nuclear families. Majority of the participants were Hindus and about one-fifth of them were Muslims and the rest were from other religious affiliations. There was nearly an equal representation of participants from urban and rural locality.
Table 1.
Sociodemographic profile of study sample
Clinical profile
The mean duration of illness was 25.55 months (SD-43.12; range 1-432 months; Median-12). Most of the patients (56.8%) had moderate to severe depression as per Beck Depression Inventory[6] and a little more than a quarter (26.7%) had very severe depression as assessed by Beck Depression Inventory.
Prescription patterns
Among the various antidepressants, escitalopram was the most commonly prescribed antidepressant, comprising 40% of the total prescriptions. This was followed by sertraline (17.6%) and fluoxetine (16.3%). Details of other prescriptions are shown in Table 2. In total selective serotonin reuptake inhibitors (SSRIs) formed 79.2% of all the prescriptions. Tricyclic antidepressants (imipramine, amitriptyline, prothiaden, and nortriptyline) formed part of 15.15% of prescriptions, with imipramine being the most commonly used tricyclic antidepressant. Serotonin-norepinephrine reuptake inhibitors (venlafaxine, desvenlafaxine and duloxetine) were prescribed to 11.3% of patients with equal share of venlafaxine and duloxetine. Occasional patients were prescribed mirtazapine, bupropion and trazadone.
Table 2.
Prescription pattern for antidepressants, benzodiazepines and other sedatives
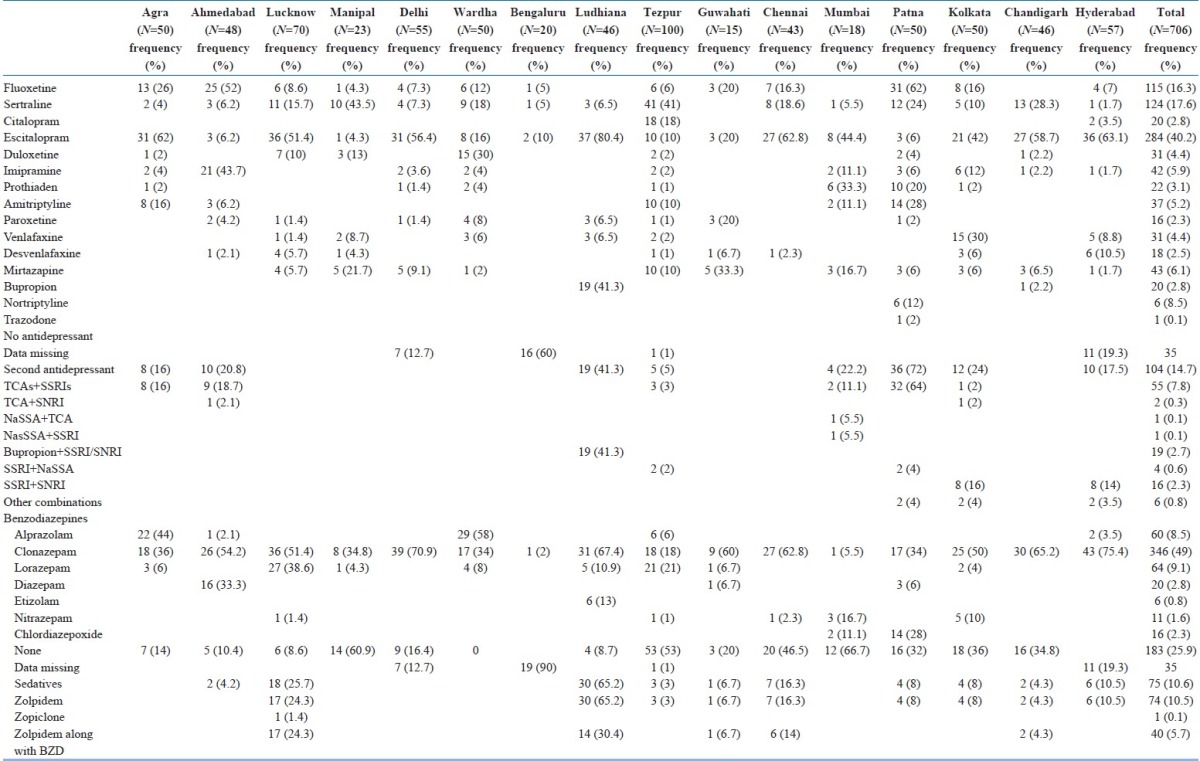
A further look at the prescription across the various centers revealed that escitalopram was the most common agent prescribed in 10 out of the 16 centers [Table 2]. Fluoxetine and sertraline were prescribed most commonly across 2 centers each. Mirtazapine and duloxetine were the most common prescriptions across one center each.
About one-sixth (N=104; 14.7%) of the patients were prescribed more than one antidepressant. Further there was significant variation across centers with half of the centers not resorting to use of two antidepressants concurrently. Of the 104 prescriptions with more than one antidepressant, 55 (52.9% of the total prescriptions of more than one antidepressant) included a combination of a SSRI and a TCA.
Of the 706 patients, nearly three-fourth of them (N=523; 74.1%) were prescribed a benzodiazepine, with clonazepam being the most preferred agent, prescribed to nearly half of the participants (49%) and formed nearly two-third of the total benzodiazepine prescriptions (346 out of 523). Other commonly preferred benzodiazepines were lorazepam (9.1% of all prescriptions and 12.2% of all prescription of benzodiazepines) and alprazolam (8.5% of all prescriptions and 11.5% of all prescription of benzodiazepines).
One-tenth of the participants were prescribed sedatives in the form of zolpidem and zopiclone, with zolpidem being prescribed in 74 out of the 75 prescriptions including these medications. More than half of the patients (40 out of 75) received zolpidem along with the benzodiazepines.
DISCUSSION
Many studies from the Western countries have evaluated the prescription patterns of antidepressants and these have looked into national prescription patterns,[7] prescription patterns in general practice and specialist care,[8] and prescription patterns of antidepressants for outpatients.[9] However, there is lack of national level data with regard to antidepressants prescription from India. Occasional studies have reported the prescription patterns for patients of depression from single center.[1–3] To the best of our knowledge, this is the first multicentric study which has evaluated the antidepressant prescription pattern of psychiatrists, from centers spread across the length and breadth of India.
Results of this study suggest that escitalopram is the most commonly prescribed antidepressant in India and SSRIs are the most commonly prescribed class of antidepressants. Overall nearly 80% of the patients received one or other SSRI. When we compare these findings with the available studies, the recent study from Chandigarh also reported a similar picture.[3] However, the findings are contrary to the other studies from India in which one reported duloxetine[2] and other reported imipramine to be the most commonly prescribed antidepressant.[1] The difference between the findings of the present study and that reported by Trivedi et al .,[2] suggests that prescription pattern of a specific center often does not reflect the national patterns. The significant difference in the choice of antidepressants in the present study from the earlier study done in 1996[1] reflects significant change in the selection of antidepressants and is possibly heavily influenced by the availability of newer antidepressants in the recent years. When we compare the findings of the present study with that with those from other countries, similar trends of prescription of SSRIs have been reported from the West[7,10] and multi-country study from East Asia.[11] However, the percentage of prescription of SSRIs in the present study is higher than that reported in these studies. In the present study SNRIs formed the 11.5% of the total antidepressant prescriptions. Similar findings have also been reported in earlier studies from India[2] and from the West.[7] TCAs formed 15% of all the prescriptions. This finding can be looked in various ways. First, TCAs still retain their place in the management of depression. Second, when we compare this findings with that reported by Chakrabarti and Kulhara[1] from Chandigarh, it can be said that over the years there is change in trend of prescription of antidepressants with significant reduction in the prescription of TCAs. In the present study more than 85% of the patients were prescribed only single antidepressant. This is less than that reported by Trivedi et al .,[2] but significantly higher than that reported by Grover et al .[3]
Current treatment guidelines mostly recommend use of SSRIs as the first line agents in patients of depression.[12] Treatment guidelines discourage concomitant use of two antidepressants to start with.[12] It is heartening to note that most of the patients in the present study were prescribed antidepressants according to the recommendations of the treatment guidelines.
Among the benzodiazepines, clonazepam emerged as the most commonly prescribed benzodiazepine and was prescribed to nearly half of the participants and formed nearly two-third of the total benzodiazepine prescriptions. Similar preference for co-prescription of clonazepam has been reported in earlier studies from India.[2,3] High prescription rates of benzodiazepines in the present study could also be due to higher prevalence of anxiety, autonomic symptoms and sleep disturbance in the patients included in the present study (see other paper of this study Grover et al . in this journal). Another reason for higher rate of prescription of benzodiazepine could be anticipated worsening of anxiety which is commonly seen with use of SSRIs.
To conclude, present study suggests that escitalopram is the most commonly prescribed antidepressant and SSRIs are the most commonly prescribed class of antidepressants. Poly pharmacy in the form of concomitant use of two antidepressants is practiced infrequently. However, benzodiazepines are used quite frequently as the co-prescription.
The findings of the present study must be interpreted in the light of limitations of the present study. This study was limited to patients of depression without any comorbid conditions (both physical and psychological). Further, the study excluded patients of depression with psychotic symptoms, elderly depressed patients and patients in the child and adolescent age group. Although this study analyzed prescriptions of 700 depressed subjects, yet this sample size can be considered as relatively inadequate for national purposes. Hence, future studies should evaluate larger sample of patients and should include patients of depression of all age groups, with all kind of comorbidities.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chakrabarti S, Kulhara P. Patterns of antidepressant prescriptions: I acute phase treatments. Indian J Psychiatry. 2000;42:21–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Trivedi JK, Dhyani M, Sareen H, Yadav VS, Rai SB. Anti-depressant drug prescription pattern for depression at a tertiary health care center of Northern India. Med Pract Rev. 2010;1:16–8. [Google Scholar]
- 3.Grover S, Kumar V, Avasthi A, Kulhara P. An audit of first prescription of new patients attending a psychiatry walk-in-clinic in north India. Indian J Pharmacol. 2012;44:319–25. doi: 10.4103/0253-7613.96302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lecrubier Y, Sheehan D, Weiller E, Amorim P, Bonora I, Sheehan K, et al. The Mini International Neuropsychiatric Interview (MINI)-a short diagnostic structured interview: Reliability and validity according to CIDI. Eur Psychiatry. 1997;12:224–31. [Google Scholar]
- 5.Amorim P, Lecrubier Y, Weiller E, Hergueta T, Sheehan D. DSM-III-R psychotic disorders: Procedural validity of the Mini International Neuropsychiatric Interview (MINI). Concordance and causes for discordance with the CIDI. Eur Psychiatry. 1998;13:26–34. doi: 10.1016/S0924-9338(97)86748-X. [DOI] [PubMed] [Google Scholar]
- 6.Beck AT, Ward C, Mendelson M. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 7.Bauer M, Monz BU, Montejo AL, Quail D, Dantchev N, Demyttenaere K, et al. Prescribing patterns of antidepressants in Europe: Results from the Factors Influencing Depression Endpoints Research (FINDER) study. Eur Psychiatry. 2008;23:66–73. doi: 10.1016/j.eurpsy.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Kjosavik SR, Hunskaar S, Aarsland D, Ruths S. Initial prescription of antipsychotics and antidepressants in general practice and specialist care in Norway. Acta Psychiatr Scand. 2011;123:459–65. doi: 10.1111/j.1600-0447.2011.01697.x. [DOI] [PubMed] [Google Scholar]
- 9.Nakao M, Takeuchi T, Yano E. Prescription of benzodiazepines and antidepressants to outpatients attending a Japanese university hospital. Int J Clin Pharmacol Ther. 2007;45:30–5. doi: 10.5414/cpp45030. [DOI] [PubMed] [Google Scholar]
- 10.Lako IM, Taxis K, Bruggeman R, Knegtering H, Burger H, Wiersma D, et al. The course of depressive symptoms and prescribing patterns of antidepressants in schizophrenia in a one-year follow-up study. Eur Psychiatry. 2012;27:240–4. doi: 10.1016/j.eurpsy.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Uchida N, Chong MY, Tan CH, Nagai H, Tanaka M, Lee MS, et al. International study on antidepressant prescription pattern at 20 teaching hospitals and major psychiatric institutions in East Asia: Analysis of 1898 cases from China, Japan, Korea, Singapore and Taiwan. Psychiatry Clin Neurosci. 2007;61:522–8. doi: 10.1111/j.1440-1819.2007.01702.x. [DOI] [PubMed] [Google Scholar]
- 12.Practice guideline for the treatment of patients with major depressive disorder. 3rd ed. Arlington (VA): American Psychiatric Association (APA); 2010. American Psychiatric Association (APA) [Google Scholar]


