Abstract
Background:
About 12-24% of children with specific learning disability (SpLD) have co-occurring attention-deficit/hyperactivity disorder (ADHD). According to “parent-proxy reports”, co-occurring “untreated” ADHD adversely impacts the health-related quality of life (HRQoL) of children with newly diagnosed SpLD, especially in their psychosocial functioning.
Aims:
To analyze the impact of “untreated” co-occurring ADHD on the “self-perceived” HRQoL of children with “newly diagnosed” SpLD.
Setting and Design:
Cross-sectional questionnaire-based study in a learning disability clinic situated in a medical college.
Materials and Methods:
From February 2008 to December 2008, 136 consecutive children newly diagnosed as having “SpLD with co-occurring ADHD (SpLD/ADHD)” or “SpLD only” were enrolled. The DISABKIDS chronic generic module (DCGM-37-S (V31)) instrument was used to measure their HRQoL. DCGM-37-S (V31) mean facet and total scores were computed for “SpLD/ADHD” and “SpLD only” children groups and compared using independent samples t-test.
Results:
HRQoL of “SpLD/ADHD” children was significantly better in limitation facet (mean difference: 8.20; 95% confidence interval (CI): 1.75-15.29; P=0.024). Although not statistically significant, the HRQoL of “SpLD/ADHD” children was better in independence, emotion, social inclusion and social exclusion facets; and in total score.
Conclusions:
“SpLD/ADHD” children perceive their physical functioning to be significantly better. Also their perceptions of their psychosocial functioning are better. Contrary to parent-proxy reports, co-occurring “untreated” ADHD does not adversely impact the self-perceived HRQoL of children with “newly diagnosed” SpLD.
Keywords: Attention-deficit/hyperactivity disorder, dyslexia, quality of life, scholastic backwardness, students
INTRODUCTION
Specific learning disability (SpLD) is a group of neurodevelopmental disorders which manifest in childhood as persistent difficulties in learning to efficiently read (“dyslexia”), write (“dysgraphia”), or do simple mathematical calculations (“dyscalculia”) despite normal intelligence, conventional schooling, intact hearing and vision, and adequate motivation and socio-cultural opportunity.[1,2] Up to 5-15% of “seemingly normal” school children have this hidden disability.[1,2] These children present with “academic problems” such as reading slowly and incorrectly, skipping lines while reading aloud, repeatedly making spelling mistakes, illegible handwriting with poor sequencing, and inability to perform even simple mathematics.[1,2]
Children with SpLD invariably fail to achieve school grades at a level that is appropriate for their intelligence.[1,2] Their academic problems often have an adverse impact on their self-image, peer and family relationships, and social interactions.[3] About 12-24% of children with SpLD have another co-occurring neurodevelopmental disorder, namely, attention-deficit/hyperactivity disorder (ADHD) which is characterized by excessive activity, short attention span and impulsivity; and which further impairs their academic and social functioning.[1,2,4]
The health-related quality of life (HRQoL) is a multidimensional measure of the overall condition of a human life, namely: (i) physical, and (ii) psychosocial (psychological and social environment).[5] A detailed Medline search using the key words “quality of life (QoL)” and “(ADHD)” and “dyslexia” failed to retrieve any study which has analyzed the impact of co-occurring “untreated” ADHD on the “self-perceived” HRQoL of children with SpLD. Hence we conducted the present study to address this issue. Our hypothesis was that co-occurring “untreated” ADHD would adversely affect the “self-perceived” HRQoL of children with “newly diagnosed” SpLD.
MATERIALS AND METHODS
Diagnosis of specific learning disability and attention-deficit/hyperactivity disorder
Each child had been referred to our clinic for assessment of poor school performance and was assessed by a multidisciplinary team comprising of pediatrician, counselor, clinical psychologist, and special educator.[1] Only children above 8 years of age were included in the study as a conclusive diagnosis of SpLD is not made till then.[1,2] Audiometric and ophthalmic examinations were done to rule out non-correctable hearing and visual deficits (of ≥40% disability) as such children do not qualify for a diagnosis of SpLD.[1,2] The pediatrician took a detailed clinical history and did a detailed clinical examination. The socio-demographic characteristics of each child were noted. The modified Kuppuswami's classification was used to determine the family's socio-economic status.[6] The counselor ruled out that emotional problem due to stress at home or at school was not primarily responsible for the child's poor school performance. The clinical psychologist conducted the Wechsler intelligence scale for children-revised (Indian adaptation by Bhatt) to determine that the child's global intelligence quotient score was average or above average (≥85).[7]
Curriculum-based assessment is a recommended method of diagnosing SpLD.[1,8] Employing a locally developed and validated curriculum-based test, the special educator conducted the educational assessment in specific areas of learning, namely, basic learning skills, reading comprehension, oral expression, listening comprehension, written expression, mathematical calculation, and mathematical reasoning.[1,2,8,9] An academic achievement of 2 years below the child's actual school grade placement or chronological age was considered diagnostic of SpLD.[1,2]
The diagnosis of co-occurring ADHD and its co-morbidities, if any, was made by the pediatrician and confirmed by the psychiatrist by ascertaining that the child's specific behaviors met the diagnostic and statistical manual of mental disorders-IV-revised criteria.[10]
Consent and ethical approval
The present study was approved by the scientific and ethics committees of our institution. All parents had signed an informed consent form and all children had given a “written” assent to participate in the study.
Sample size and patient enrolment
It was assumed that 9% of Indian children have SpLD. With a 95% confidence level and 5% confidence interval (CI) the sample size (namely, the number of children that need to be interviewed) was calculated using the standard formula:
![]()
(Z=1.96 (Z value for 95% confidence level); P=0.09 (9% prevalence, expressed as decimal); C=0.05 (CI, expressed as decimal)). The sample size calculated for the present study was 126 children.
However, we included the first consecutive 136 children who could read and understand English and were willing to participate in the study. Thus, the power of analysis for the present study was >95%. No child who could understand and read English refused to participate in the study.
Each child was given the DISABKIDS chronic generic module (DCGM) self-report version (with treatment facet excluded) instrument (its English version), namely the DCGM-37-S (V31), to complete in a quiet secluded room during his/her last visit to our clinic before the diagnosis was informed.[11] Each child completed this self-administered questionnaire in 15 to 25 min without the parent (s) being present. This study was conducted from February 2008 to December 2008.
Measuring self-perceived health-related quality of life with DISABKIDS chronic generic module-37-S (V31)
DCGM-37 is an instrument which has been devised to measure the HRQoL of children and adolescents with any chronic health condition or disability.[11] It has been developed cross-nationally across seven European Union (EU) countries, namely, Austria, France, Greece, Germany, the Netherlands, Sweden, and the United Kingdom.[11] The DCGM-37 has been developed to enable cross-cultural pediatric HRQoL research internationally, namely, in different national and cultural contexts.[11] Its English version can be used in any country for children aged between 8 and 16 years who can read and understand English.[11]
As permitted, in the present study we excluded the treatment facet, as it was not applicable.[11] The DCGM self-report version (with treatment facet excluded) instrument, namely the DCGM-37-S (V31) consists of five facets (or sub-scales; [Table 1]): Independence (autonomy and living without impairments), emotion (emotional worries and concerns), social inclusion (acceptance of others, positive relationships), social exclusion (stigma, feeling left out), and limitation (functional limitations, perceived health). These five facets are additionally associated with three HRQoL domains, denoted, as mental, social, and physical [Table 1]. Each facet consists of six items, except for the emotion facet that has seven items. All 31 items have a 5-point Likert-type response scale with options ranging from 1 (never), to 5 (always). The child uses a 4-week recall period for scoring all 31 items. Each item question is simple and easy to understand. However a child was permitted to take the help of a trained interviewer (Rohini Venkataraman) to read out the question and explain before marking his/her response.[11]
Table 1.
Summary of domains and facets in DISABKIDS chronic generic module-37-S (V31)a: Interpretation of low and high scores[11]
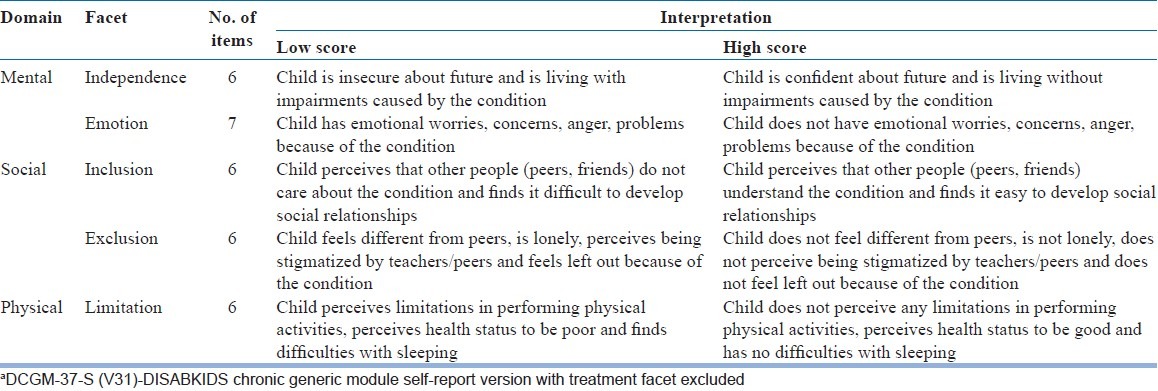
Within each facet, item raw scores were summed and transformed into a score from 0 (worst possible HRQoL) to 100 (best possible HRQoL), by following the standard scoring algorithms of the instrument.[11] The five facet scores were then combined to produce a “general score” for HRQoL, denoted as the DCGM-37-S (V31) total score.[11] The DCGM-37-S (V31) demonstrates good reliability and validity.[11] Internal reliabilities (as measured by Cronbach's alpha) of the five facets range from α = 0.70 to α = 0.87.[11]
Statistical analysis
The data were analyzed using the statistical package for the social sciences program, version 15.0 for Windows (SPSS Ltd., Chicago, USA). The clinical and socio-demographic characteristics of “SpLD/ADHD” and “SpLD only” children groups were compared using the Student's unpaired t-test, Chi-square test or Fischer's exact test (as indicated). Wherever appropriate, with bivariate analysis, the odds ratio (OR) was calculated and 95% CI was estimated around the OR. The DCGM-37-S (V31) mean facet and total scores for “SpLD/ADHD” and “SpLD only” children groups were computed, using SPSS syntax with calculations provided by Professor Monika Bullinger, and compared using independent samples t-test.[10] Statistical significance was considered as P < 0.05 (two-tailed).
Since population norms for Indian children with chronic health problems or disabilities are not available, mean scores of the “SpLD/ADHD” children group were compared, as recommended, with the published EU children norms.[11] These EU norms have been computed from the results of the DISABKIDS field study wherein the HRQoL of 1,152 children and adolescents with seven different chronic conditions or disabilities (namely, asthma, juvenile arthritis, atopic dermatitis, diabetes, cerebral palsy, cystic fibrosis and epilepsy) were measured.[11] Effect sizes were computed to explore the clinical importance of differences between the “SpLD/ADHD” children group and the EU norms by dividing their mean difference in scores by the EU children's SD.[11] Cohen's guidelines for the interpretation of effect size (0.2 to <0.5=small, 0.5 to <0.8=medium and ≥0.8=large) were used.[12]
RESULTS
Study children characteristics
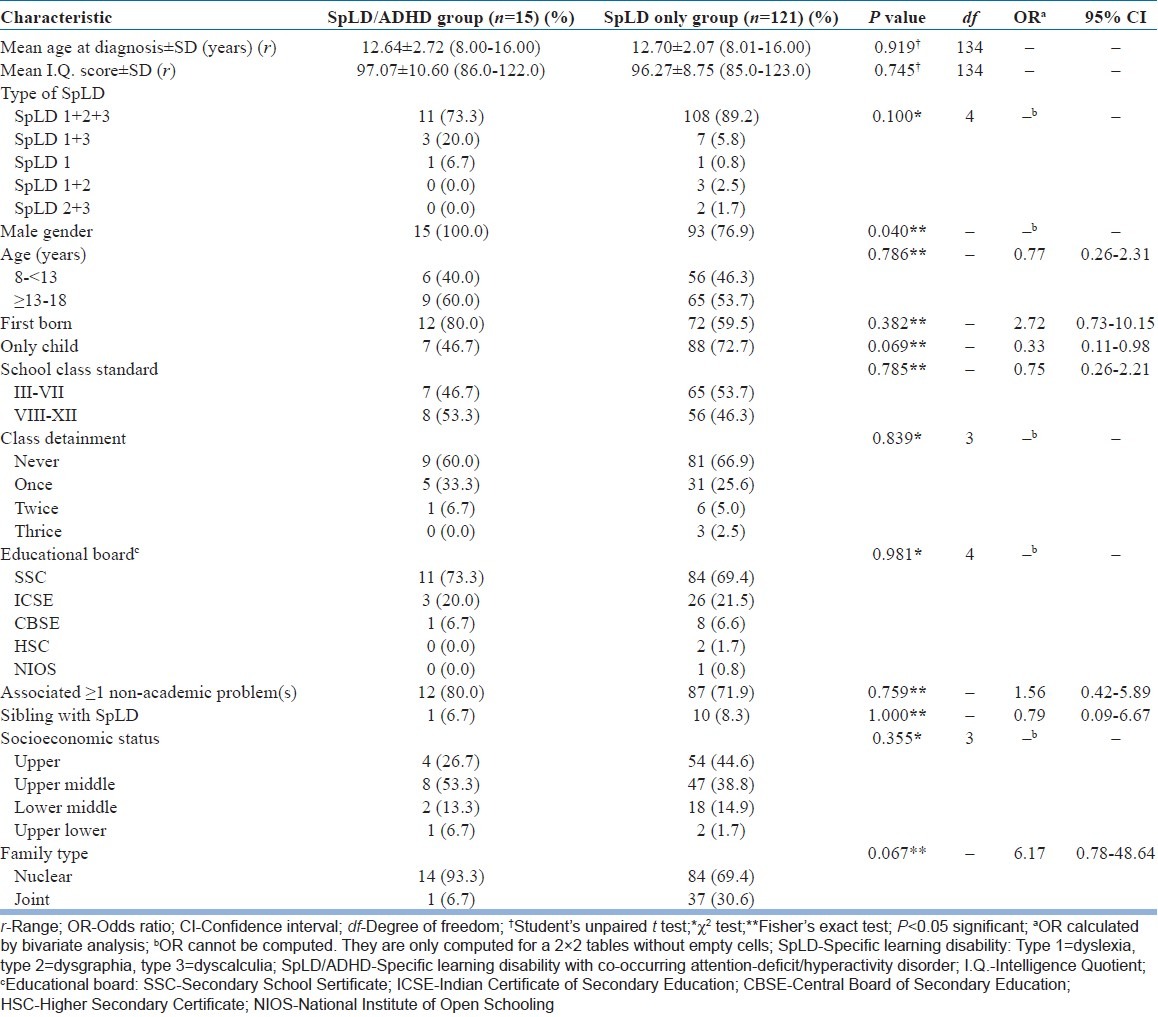
All 136 children with SpLD enrolled in the study were studying in English-medium schools situated in Mumbai [Table 2]. Of these 136 children, 15 (11.0%) had co-occurring ADHD: 5 had ADHD, combined type (ADHD-C); 6 had ADHD, primarily of the inattentive type (ADHD-I); and 4 had ADHD primarily of the hyperactive-impulsive type (ADHD-HI). In both groups majority of children had all three types of SpLD, were boys, were first-born, and were living in nuclear families. In both groups of children majority of parents had reported that they had been told by a teacher or a doctor that their child had associated “non-academic” problem(s), such as, behavioural problems (aggressive behaviour, temper tantrums and stubbornness), anxiety problems, depressive thoughts, or recurrent upper respiratory tract infections [Table 2].
Table 2.
Clinical and socio-demographic characteristics of children
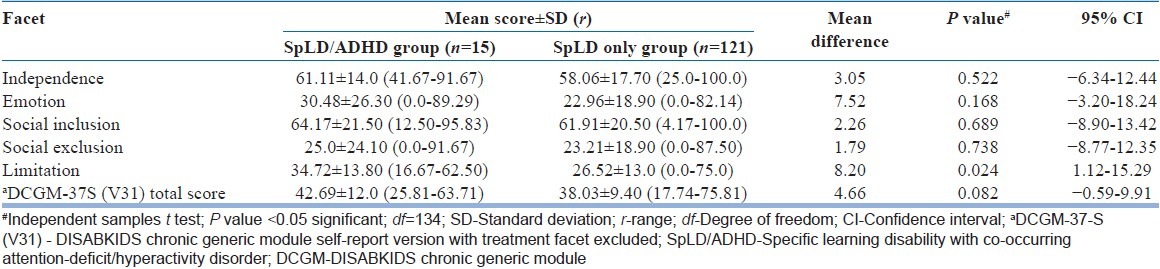
Comparison of health-related quality of life of specific learning disability/attention-deficit/hyperactivity disorder and specific learning disability only children
When comparisons were made in the DCGM-37-S (V31) mean scores of the two groups of children [Table 3], the “SpLD/ADHD” children perceived their physical functioning to be “significantly better” (P=0.024). Although not statistically significant, the “SpLD/ADHD” children perceived their psychosocial functioning and their “overall” functioning to be better than “SpLD only” children [Table 3]. There were no missing data for the DCGM-37-S (V31) items.
Table 3.
Comparison of DISABKIDS chronic generic module-37-S (V31)a facet and total scores of specific learning disability with co-occurring attention-deficit/hyperactivity disorder and specific learning disability only children
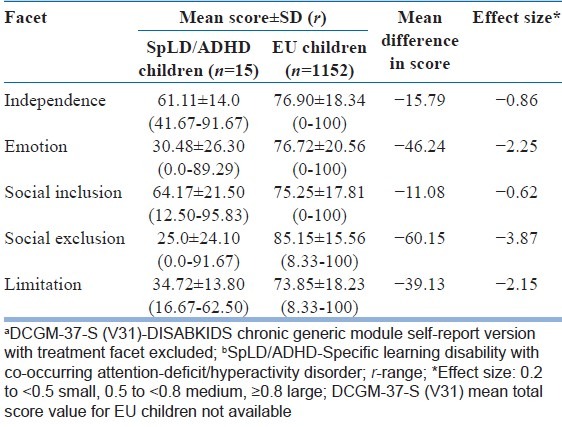
Comparison of health-related quality of life of specific learning disability/attention-deficit/hyperactivity disorder children with EU norms
All the 5 DCGM-37-S (V31) mean facet scores were lower in the “SpLD/ADHD” children when compared with the EU children norms [Table 4]. Effect size results indicated clinically important deficits in HRQoL of “SpLD/ADHD” children in all five facets, namely: ‘large deficits’ in social exclusion, emotion, limitation, and independence; and ‘medium deficit’ in social inclusion [Table 4].
Table 4.
DISABKIDS chronic generic module-37-S (V31)a facet scores of specific learning disability with co-occurring attention-deficit/hyperactivity disorderb children compared with European Union children norms[11]
DISCUSSION
The present study documents that as compared to children with other chronic health conditions/disabilities (such as, asthma, juvenile arthritis, atopic dermatitis, diabetes, cerebral palsy, cystic fibrosis and epilepsy), children with “SpLD/ADHD” have clinically important deficits in their self-perceived psychosocial and physical functioning (social exclusion > emotion > limitation > independence > social inclusion). However, the “self-perceived” HRQoL of “SpLD/ADHD” children is significantly better than the HRQoL of “SpLD only” children in the limitation facet of health; and although not statistically significant, their HRQoL is also better in the other four facets of health, viz., independence, emotion, social inclusion and social exclusion; and in the total score. Our data clearly shows that compared to “SpLD only” children, “SpLD/ADHD” children perceive their physical functioning to be significantly better, viz., (i) they perceive fewer limitations in performing physical activities, (ii) they perceive their health status to be better and (iii) they have lesser difficulties with sleeping. Also, “SpLD/ADHD” children perceive their psychosocial functioning to be better, viz., (i) they have fewer insecurities about their future and about living with impairments caused by their condition; (ii) they have fewer emotional worries, concerns, anger, and problems because of their condition; (iii) fewer of them perceive that their peers and friends do not understand their condition or perceive having difficulties in developing social relationships; and (iv) fewer of them feel different from their peers or feel lonely or perceive being stigmatized by their teachers/peers or being left out because of their condition. In short, compared to “SpLD only” children, “SpLD/ADHD” children perceive their physical, psychosocial and overall HRQoL to be better. Hence, contrary to our hypothesis, the present study reveals that co-occurring “untreated” ADHD does not adversely affect the “self-perceived” HRQoL of children with newly diagnosed SpLD.
To the best of our knowledge, ours is probably the first study that has analyzed the impact of co-occurring “untreated” ADHD on the “self-perceived” HRQoL of children with SpLD and that too utilizing a reliable and validated generic instrument, namely, the DCGM-37-S (V31).
A previous Indian study had analyzed the impact of co-occurring “untreated” ADHD on the “parent-proxy” HRQoL of children with SpLD utilizing another reliable and validated generic instrument, namely, the child health questionnaire-parent form 50 (CHQ-PF50).[13,14] Contrary to our results, the parent-proxy ratings study had documented that the physical functioning of “SpLD/ADHD” children is similar and their psychosocial functioning is significantly poorer, viz., these children are significantly more dissatisfied with their abilities, family and peer relationships, and their overall emotional and social life.[13] The parent-proxy ratings study has also reported that the academic problems of “SpLD/ADHD” children had a significant impact on their parent's emotional health and personal time.[13] It is possible that their own compromised quality of life could have biased the parents to report lower HRQoL scores in the SpLD/ADHD group.[13,15]
It is well known that self-perceived HRQoL of children can vary from their parents-proxy ratings.[11,15] It is possible that their innate attributes of having excessive activity, short attention span and impulsivity made “SpLD/ADHD” children rate their physical and psychosocial functioning and overall HRQoL to be better than “SpLD only” children.
What is the utility of the present study? First; our study has revealed that children with SpLD/ADHD perceive having clinically significant deficits in their social exclusion, emotion, limitation, independence and social inclusion facets of health. The present study highlights the importance of optimally treating children with SpLD/ADHD to improve their HRQoL. Children with SpLD/ADHD need appropriate psychoeducational interventions, namely, remedial education and provisions (accommodations) for their SpLD.[1,4] Also, their ADHD-related symptoms of inattentiveness/hyperactivity/impulsiveness are eminently treatable by behavioral therapy and if necessary, with medications.[16] Second; children with SpLD/ADHD have “more severe” learning problems than children who have SpLD but no ADHD, and also “more severe” attention problems than children who have ADHD but no SpLD.[17] However, children with SpLD/ADHD do not perceive their comorbid ADHD to further adversely affect their HRQoL. Parents of children with SpLD/ADHD often get overwhelmed coping up with their child's dual diagnosis. Pediatricians, psychiatrists and counselors can utilise this important finding to allay parental anxieties and help them in coping up with their child's dual diagnosis. Allaying parental anxieties early would help ensure optimum rehabilitation of these children. Third; in general, there is scanty information available on HRQoL of children having SpLD/ADHD, not only in Indian literature, but also in world literature.[3,13,15,18] We believe that our study results are an important contribution to help reduce this deficit.
The present study has its limitations. First; the mean age of diagnosis in both SpLD/ADHD and SpLD only children groups was about 12.5 years. This situation arises due to the general inadequate awareness about these common neurodevelopmental disorders and reluctance of parents to get their child assessed.[1,4] Hence the present study results may not reflect the impact that untreated comorbid ADHD has on the HRQoL of children in whom SpLD is diagnosed by 8-9 years of age. Second; a significantly more number of children diagnosed with SpLD/ADHD were boys and this could have led to higher HRQoL scores being documented in the SpLD/ADHD group. Boys with chronic health conditions/disabilities are known to document higher scores than girls on the DCGM-37-S (V31).[11] This increased male preponderance in children diagnosed with SpLD/ADHD has also been reported in the “parent-proxy” study.[13] Third; we have not made any attempt to analyze the impact of ADHD subtypes on the self-perceived HRQoL of children with SpLD. In the present study children in both groups had various combinations of subtypes of SpLD [Table 2]. The impact of ADHD sub-types on various SpLD subtypes is too complex and warrants further research. Moreover, results of recent studies of ADHD subtypes have suggested a lack of stability of subtypes over time and thus, question their validity as categorical diagnoses.[19] For similar reasons we did not attempt to assess the severity of either ADHD or SpLD in these children. Fourth; as vernacular (Marathi, Hindi or Gujarati) versions of the DCGM-37-S (V31) instrument are not available, children from the lower socio-economic strata of society who usually attend vernacular medium schools were not represented in our study population. However, our numbers of these children were very small (<10).
We do not believe that these limitations adversely affect the utility of our results. Both due to the limitations as outlined above and the general paucity of data on HRQoL of children having SpLD/ADHD the implications of the present study need to be determined by future studies.
ACKNOWLEDGMENTS
The authors would like to thank our Dean Dr. Sandhya Kamath for granting us permission to publish this study; all the children and parents who participated in this study; Dr. Nilesh Shah, Professor and Head of Psychiatry for his help in confirming the diagnosis of the attention-deficit hyperactivity disorder; and Professor D. P. Singh, Department of Research Methodology, Tata Institute of Social Sciences, Deonar, Mumbai, for his help in the statistical analysis of the data. We also thank Professor Monika Bullinger, DISABKIDS Project Coordinator, Department of Medical Psychology, University Hospital of Hamburg-Eppendorf, Hamburg, Germany for providing us the DISABKIDS manual free of cost and granting us permission to use the DCGM-37-S instrument. The material in this publication is the result of use of the DCGM-37-S instrument and the assistance of the EUROPEAN DISABKIDS GROUP is gratefully acknowledged.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Karande S, Kulkarni M. Specific learning disability: The invisible handicap. Indian Pediatr. 2005;42:315–9. [PubMed] [Google Scholar]
- 2.Shaywitz SE. Dyslexia. N Engl J Med. 1998;338:307–12. doi: 10.1056/NEJM199801293380507. [DOI] [PubMed] [Google Scholar]
- 3.Karande S, Bhosrekar K, Kulkarni M, Thakker A. Health-related quality of life of children with newly diagnosed specific learning disability. J Trop Pediatr. 2009;55:160–9. doi: 10.1093/tropej/fmn099. [DOI] [PubMed] [Google Scholar]
- 4.Karande S, Satam N, Kulkarni M, Sholapurwala R, Chitre A, Shah N. Clinical and psychoeducational profile of children with specific learning disability and co-occurring attention-deficit hyperactivity disorder. Indian J Med Sci. 2007;61:639–47. [PubMed] [Google Scholar]
- 5.The World Health Organization Quality of Life assessment (WHOQOL) Position paper from the World Health Organization. Soc Sci Med. 1995;41:1403–9. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- 6.Mishra D, Singh HP. Kuppuswamy's socioeconomic status scale - A revision. Indian J Pediatr. 2003;70:273–4. doi: 10.1007/BF02725598. [DOI] [PubMed] [Google Scholar]
- 7.Bhatt MC. Adaptation of the Wechsler intelligence scale for children for Gujarati population [PhD dissertation] Ahmedabad (Gujarat): University of Gujarat; 1971. [Google Scholar]
- 8.Deno SL, Fuchs LS, Marston D, Shinn M. Using curriculum-based measurement to establish growth standards for students with learning disabilities. School Psych Rev. 2001;30:507–24. [Google Scholar]
- 9.Sholapurwala RF. Curriculum Based Test for Educational Evaluation of Learning Disability. 1st ed. Mumbai: Jenaz Printers; 2010. [Google Scholar]
- 10.Diagnostic and Statistical Manual of Mental Disorders. 4th ed Revised. Washington, DC: American Psychiatric Association; 2000. American Psychiatric Association. [Google Scholar]
- 11.The DISABKIDS Questionnaires: Quality of Life Questionnaires for Children with Chronic Conditions. 1st ed. Lengerich: Pabst Science Publishers; 2006. The European DISABKIDS Group. [Google Scholar]
- 12.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale (NJ): Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 13.Karande S, Bhosrekar K. Impact of attention.deficit/ hyperactivity disorder on health.related quality.of.life of specific learning disability children. Indian J Pediatr. 2009;76:1119–24. doi: 10.1007/s12098-009-0240-9. [DOI] [PubMed] [Google Scholar]
- 14.Landgraf JM, Abetz L, Ware JE. Child Health Questionnaire (CHQ): A User's Manual. 2nd ed. Boston, MA: Health Act; 1999. [Google Scholar]
- 15.Eiser C, Jenney M. Measuring quality of life. Arch Dis Child. 2007;92:348–50. doi: 10.1136/adc.2005.086405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. The MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD. Arch Gen Psychiatry. 1999;56:1073–86. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- 17.Mayes SD, Calhoun SL, Crowell EW. Learning disabilities and ADHD: Overlapping spectrumn disorders. J Learn Disabil. 2000;33:417–24. doi: 10.1177/002221940003300502. [DOI] [PubMed] [Google Scholar]
- 18.Srivastava A, Sreejayan K, Joseph AM, Sharma PS. Indian research on comorbidities. Indian J Psychiatry. 2010;52:S246–9. doi: 10.4103/0019-5545.69240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Solanto MV, Alvir J. Reliability of DSM-IV symptom ratings of ADHD: Implications for DSM-V. J Atten Disord. 2009;13:107–16. doi: 10.1177/1087054708322994. [DOI] [PubMed] [Google Scholar]


