Abstract
Background
The purpose of this study was to provide prospective independently analyzed evidence on how patients feel about a carpal tunnel release (CTR) performed under local anesthesia only (no sedation or tourniquet) versus with local anesthesia, intravenous (IV) sedation, and a tourniquet.
Methods
This prospective cohort study compared 100 consecutive CTRs done with only lidocaine and epinephrine in Saint John, New Brunswick to 100 consecutive CTRs done with IV sedation in Davenport, Iowa. Patient perspectives on the anesthesia were captured in a blinded questionnaire 1 week postoperatively.
Results
For subsequent surgery, 93 % of wide awake patients would choose local anesthesia only and 93 % of sedated patients would choose sedation. Wide awake patients spent less time at the hospital (M = 2.6 h) than sedated patients (M = 4.0 h; p < .001). Preoperative blood work, electrocardiograms, and/or chest radiographs were done for 3 % of wide awake patients and 48 % of sedated patients (p < 0.001). Preoperative anxiety levels for wide awake patients were lower than for sedated patients (p = 0.007); postoperative anxiety was similar. There were no anesthesia complications in either group. Narcotics were used by 5 % of unsedated patients and 67 % of sedated patients (p < 0.001). Adequate pain control was reported by 89 % and 90 % of patients, respectively.
Conclusions
The majority of patients from both cohorts liked whichever method of anesthesia they received and would choose it again. However, sedated patients spent more time at the hospital, required more preoperative testing, and reported greater preoperative anxiety.
Keywords: Carpal tunnel syndrome, Carpal tunnel release, Local anesthesia, Wide awake, Intravenous sedation, Patient satisfaction, Patient preference
Introduction
Carpal tunnel syndrome is a common disease process, with an estimated prevalence of 1 to 5 % in the general population [2, 5, 7, 16, 22]. Carpal tunnel release (CTR) is the most common nontraumatic hand surgery performed in North America [2]. The economic burden to the health care system from this condition and its treatment is, therefore, considerable. In Canada, more than 70 % of hand surgeons perform CTRs with surgeon-administered local anesthesia consisting of lidocaine and epinephrine in a clinic setting with field sterility but without the use of a tourniquet, sedation, or a separate anesthesia provider, i.e., wide awake [12, 14]. In contrast, the majority of CTRs performed in the United States are done in the main operating room with a tourniquet, full sterility, sedation, and the assistance of an anesthesia provider.
Those unfamiliar with wide awake hand surgery may be concerned that it would be poorly tolerated. Some patients have the impression that being “asleep” is the most comfortable, pain-free, and “best” method to have surgery. Given the differences in the costs and conveniences of surgery performed with local anesthesia only versus surgery with sedation, we felt it was important to find out how the patients viewed their anesthesia experience. Do patients feel that one type of anesthesia is superior to the other? Is a wide awake CTR painful or associated with elevated anxiety?
The purpose of this study was to compare the patient’s perspective on the anesthesia provided for a CTR: the wide awake approach versus local anesthesia with intravenous (IV) sedation. Our goal was to provide prospective independently analyzed evidence on this subject.
Materials and Methods
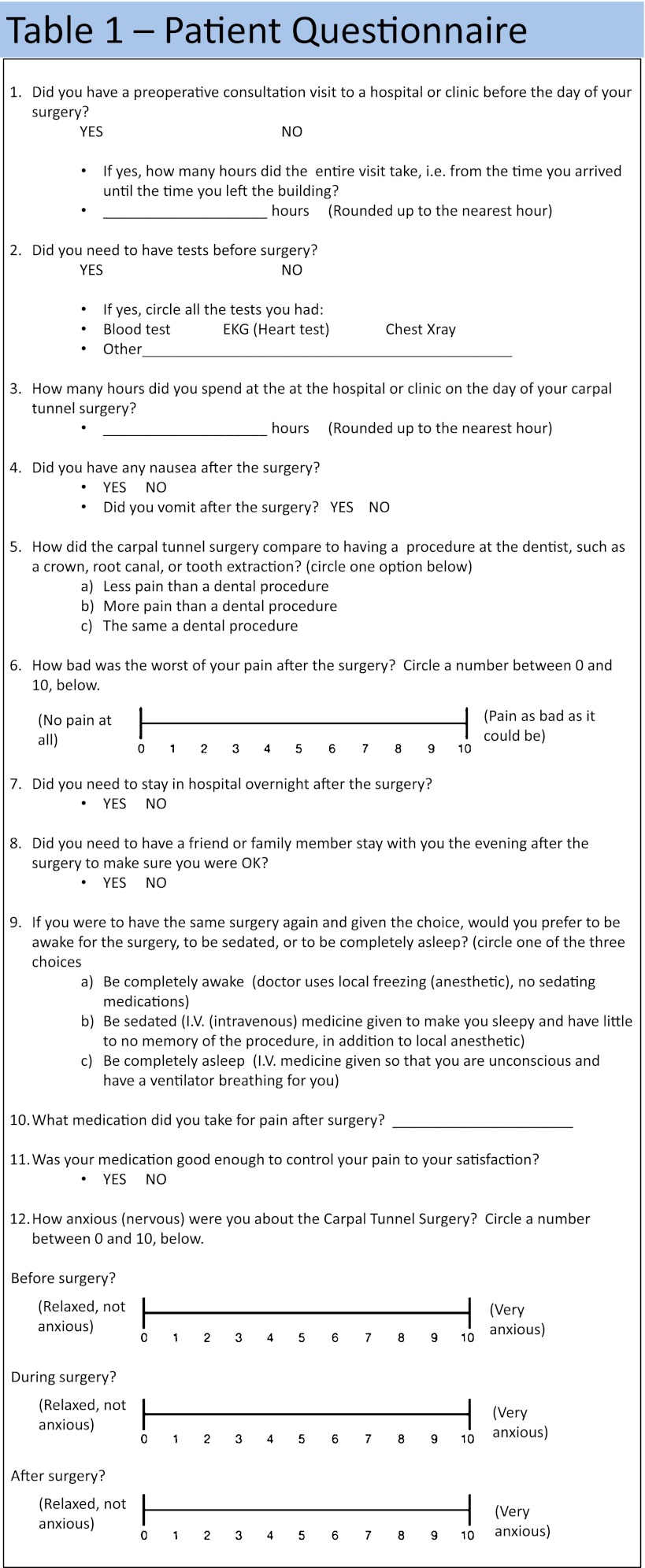
This study was designed as a prospective cohort study of two groups of patients’ attitudes towards the type of anesthesia provided for carpal tunnel surgery. The first group comprised 100 consecutive patients of a single surgeon undergoing an open CTR with only lidocaine and epinephrine (no tourniquet and no sedation) in Saint John, New Brunswick, Canada. The second cohort consisted of 100 consecutive patients of another single surgeon who underwent an endoscopic CTR with local anesthesia (lidocaine), IV sedation, and the use of a tourniquet in Davenport, Iowa, USA. Patient perspectives on the anesthesia experience were captured in a questionnaire completed at their first postoperative visit (Fig. 1). These two anesthesia methods were the standard procedures at each hospital at the time of the study. Postoperative analgesics were prescribed based on the surgeons’ standard practice.
Fig. 1.
Patient questionnaire. The 12-item questionnaire completed by patients 1 week postoperatively
The study was approved by the Ethical Institutional Review Board of both institutions before the study began. All patients were diagnosed with carpal tunnel syndrome based on symptoms and confirmed by clinical exam and/or with electromyography (EMG) or nerve conduction studies. Inclusion criteria were: (1) the patient had a CTR, (2) they attended their first follow up visit, and (3) they were willing and able to understand and complete the postoperative questionnaire. Informed consent to participate in the study was obtained from all subjects. Patients who were not able to attend a postoperative visit or willing to participate in the study were excluded.
At the first postoperative visit, approximately 7 days postsurgery, patients were given a questionnaire to complete. The questionnaire was pilot tested on ten patients before the study and adjustments were made to question syntax and organization so that the questions would be easily understood by the study patients. Patients were made aware that their surgeon would not see their individual responses to the questions and that the results would be collated and tabulated by a third blinded party.
All data were entered into SPSS statistical software for quantitative and statistical analyses. Student’s t tests and chi-squared analysis were used to compare the data between the two groups, for continuous and categorical data, respectively. Significance was defined as p < 0.05.
Results
There were no losses to follow-up as all of the 100 patients of both groups attended their scheduled postoperative follow up visit and filled out the questionnaire. No patient from either group had any anesthetic-related complications and none required prolonged observation or hospital admission.
The overall time spent at the hospital or clinic on the day of surgery was significantly lower (M = 2.6 h, SD = 1.13) for the wide awake patients (t(194) = 8.895, p < .001) than for the sedated patients (M = 4.0, SD = 1.16). Preoperative testing, such as blood work, an electrocardiogram (EKG), or chest X-ray (excluding nerve testing) was done for 3 % of wide awake patients and 48 % of sedated patients (χ2(1, N = 200) = 53.30, p < .001). Postoperative nausea and/or vomiting (PONV) were reported by 1 % of wide awake and 7 % of sedated patients; this was not significantly different.
Patients’ reported anxiety levels on a visual analog scale (VAS) (0–10) before, during, and after the CTR are shown in Table 1. Sedated patients were not asked to report their intraoperative anxiety. The anxiety levels presurgery for the wide awake patients (M = 2.3, SD = 2.68) were significantly lower (t(197) = 2.716, p = .007) than for sedated patients (M = 3.4, SD = 2.81). The anxiety levels were reduced for both the wide awake (M = 1.5, SD = 2.12) and sedated patients (M = 1.2, SD = 1.85) to comparable levels postoperatively (t(196) = −.953, p = .342).
Table 1.
Perioperative anxiety and postop pain
| Local anesthesia (mean ± SD) | Sedation anesthesia (mean ± SD) | P value | |
|---|---|---|---|
| Preop anxiety | 2.3 ± 2.68 | 3.4 ± 2.81 | 0.007* |
| Intraop anxiety | 2.1 ± 2.49 | – | – |
| Postop anxiety | 1.4 ± 2.12 | 1.2 ± 1.85 | 0.342 |
| Max postop pain | 4.3 ± 2.65 | 4.3 ± 2.70 | 0.895 |
* denotes p<0.05
Patients were asked to compare their CTR experience to a routine procedure at the dentist such as a filling, root canal, or tooth extraction. Wide awake versus sedated patients rated their CTR perioperative pain as less than a routine dental procedure (54 % versus 68 %), about the same as a dental procedure (34 % versus 24 %), and more painful than a dental procedure (12 % versus 8 %), respectively. These differences were not significant (χ2(2, N = 196) = 4.32, p = .12).
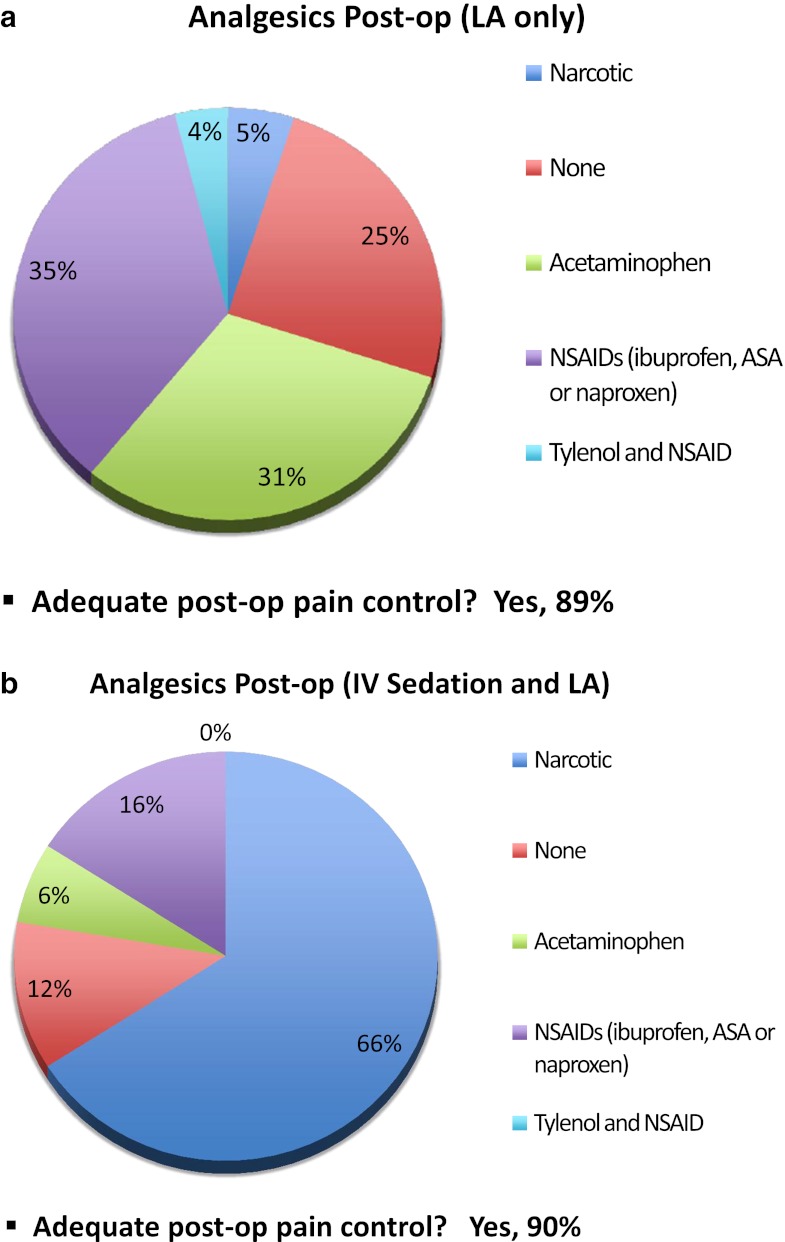
Maximum postoperative pain, reported on a VAS, ranging from 0 to 10, was similar for wide awake (M = 4.3, SD = 2.65) and sedated patients (M = 4.3, SD = 2.70) (t(198) = −.132, p = .895). Figure 2 shows the distribution of analgesic medications used by patients postoperatively. Narcotics were used by 5 % of wide awake patients and 67 % of sedated patients (χ2(1, N = 193) = 80.85, p < .001). Adequate pain control was reported by 89 % and 90 % of patients, respectively.
Fig. 2.
Postoperative analgesics. a Distribution of postoperative analgesic medications used by patients in the wide awake cohort. b Distribution of postoperative analgesic medications used by patients in the IV sedation cohort
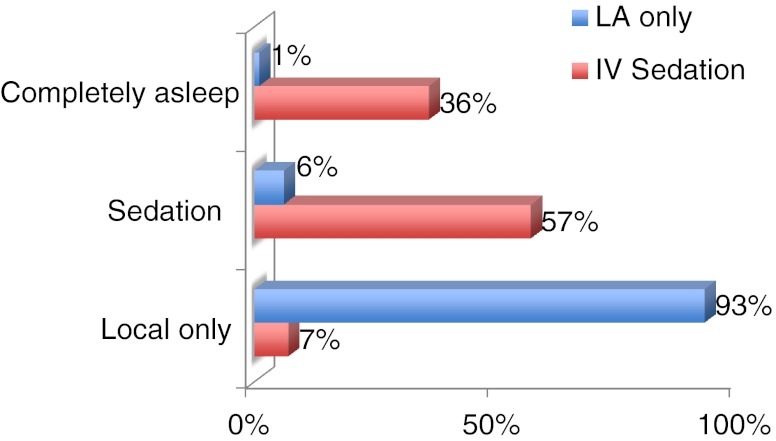
Asked the hypothetical question of having a subsequent CTR, 93 % of wide awake patients would choose local anesthesia only (the same as what they got) if they had the surgery again and 93 % of sedated patients would choose either IV sedation or general anesthesia (Fig. 3).
Fig. 3.
Method of anesthesia of choice for subsequent CTR. Responses of patients from both cohorts, on their method of anesthesia of choice for a hypothetical subsequent carpal tunnel release
Discussion
Our study found that 93 % of patients in both groups would repeat whatever anesthesia they had the first time if they had to have another carpal tunnel operation again in the future. Both cohorts of patients liked whichever type of anesthesia we gave them. It is not surprising that patients will prefer what they know to work well and tend to be more suspicious of the unknown. The results in our wide awake cohort compare well with the results obtained in a level IV German study, which showed that 83 % of their patients would chose the wide awake approach again [8]. These results certainly do not support the concept that “patients need sedation.”
The overall time spent at the hospital for surgery was significantly less for wide awake patients compared to the cohort of patients who received IV sedation during a CTR. Wide awake surgery eliminated the need for preoperative blood work and testing (EKG and/or chest X-ray) for nearly all wide awake patients (97 %). In contrast, 48 % of sedated patients had one or more of the above investigations. These tests are mostly performed because of the sedation, not because of the surgery. Eliminating the need for preoperative testing means that the patient does not need to miss time at work or get a baby sitter to go for those tests on a separate visit prior to surgery.
The need for preoperative testing for surgery with IV sedation clearly raises costs. Sedation-free surgery can easily be performed in a setting outside of a main operating room, which enables further cost savings. Leblanc et al. reported that the use of the main operating room for CTR is nearly four times more expensive and less than half as efficient as a CTR performed in a clinic setting, with the wide awake technique, at a Canadian institution [14]. Chatterjee et al. demonstrated a similar cost and efficiency advantage of performing CTRs in the clinic setting at an American tertiary care institution [3].
Wide awake surgery eliminates the need for an anesthesia provider and postoperative monitoring because only lidocaine and epinephrine are injected. These two drugs have been safely used in dental office procedures in massive numbers throughout the world daily for over 60 years with no monitoring, no IV lines, no preoperative testing, and very few reported adverse events. Patients with comorbidities such as pulmonary, cardiac, multiple medications, or morbid obesity can be better served by lowering the risk level to that of a visit to the dentist office for a minor procedure performed only with lidocaine and epinephrine [18]. Unplanned hospital admissions may also be avoided [6].
There was a low rate of PONV reported in both groups of this study (1 % and 7 %), which were not significantly different at the selected level of significant difference. There were no unplanned hospital admissions or anesthetic-related complications in either cohort. We felt that the wide awake surgery (pure local anesthesia) patients would have a lower risk of postoperative complications such as nausea and vomiting, but this was not the case. The sedated patients had a very low incidence of nausea and vomiting at 7 %. The exact mechanism of PONV is unknown, yet has been reported with much higher incidence in other studies of procedures done with IV sedation [1, 13, 20, 21, 23]. The rate of PONV in a series of 300 consecutive plastic surgery procedures by Marcus et al., performed with sedational anesthetic was 24 % and caused unplanned admissions to hospital in 4 % of patients [17].
Fear of intraoperative anxiety can be a factor that drives unknowing patients away from local anesthesia. Our patients reported that their intraoperative anxiety for the wide awake approach was low (mean of 2.1 out of 10); this was no greater than preoperatively (mean of 2.3). Interestingly, the wide awake patients had significantly less preoperative anxiety. Clearly, this observation has major limitations in that there are many other factors that create anxiety other than the type of anesthesia to be provided. However, it may be that patients who know they will lose control of their faculties (as in sedation or general anesthesia) have some anxiety about that compared to patients who get pure local anesthesia and remain in full control. We also wondered whether fear of pain from local anesthesia would increase anxiety, but it did not appear to do so. It may be that because wide awake surgery (with no tourniquet) has been performed for many years at the hospital in Saint John, many patients have come to view this operation as they would a trip to the dentist. On the other hand, the Iowa population may view this as a “regular operation” with IV medications, loss of consciousness, and the need for a supervised postoperative recovery time. Postoperatively, the anxiety levels were similar between the two groups.
The second factor that can deter unknowing patients from pure local anesthesia is the fear of the pain from the injection. The majority of patients from our study (88 % of wide awake patients and 92 % of sedated patients) rated their CTR as incurring the same or less pain than a routine dental procedure. When local anesthesia is injected properly, patients frequently will only feel pain from the first 27-gauge needle poke [12, 19]. In addition, the techniques of injecting local anesthesia with minimal pain have been shown to be easily learned by medical students and residents [10]. It is noteworthy that many of the patients in the wide awake cohort had their local anesthesia injections performed by medical students and residents.
There was a significant difference in the use of narcotics for postoperative analgesia between the two cohorts. Our findings showed equivalent satisfaction in postoperative pain control (89 % and 90 %) between the two groups, despite the difference in narcotic use (5 % for wide awake and 66 % for sedated patients). Tramadol accounted for the majority (84 %) of the narcotics used; hydrocodone (15 %) and codeine (2 %) were also taken. This discrepancy is likely because of a difference in pharmacological standards of practice between the two regions. Postoperative analgesics are selected by the surgeon and not directly associated with the type of anesthesia used during surgery. However, these data demonstrate that adequate postoperative pain control was achieved in the vast majority of patients who took only ibuprofen and/or acetaminophen. This raises the question that the need for opiate-based analgesia post-CTR may be overestimated.
In Canada, most CTRs are now being done safely in minor procedure rooms, within a hospital, clinic, or office with field sterility using the tourniquet-free wide awake approach [14, 15]. One of the main forces that generated wide spread adoption of this approach was the difficulty of getting main operating room time with an anesthesia provider in Canada. However, our experience has taught us that wide awake carpal tunnel surgery is not only well tolerated but also preferred by the vast majority of patients who have been through the experience. In addition, the wide awake approach is now being used for many other operations in hand surgery in Canada [4, 9, 11].
One major limitation of this study is that the two cohorts were treated at different institutions in different countries by different surgeons. Each center treats all patients with either wide awake technique (Saint John) or local anesthesia with IV sedation (Davenport), as their respective standards of practice. Therefore, randomization of patients to one of the methods of anesthesia would have contradicted this standard of practice. Furthermore, there will be some variations in surgical technique, the hospital or clinic environment, and postoperative care that could impact a patient’s overall experience. In addition, the questionnaire used in this study is nonvalidated. These limitations decrease our ability to generalize these results to all patients in all regions. Future studies that randomize patients to local anesthesia only or local anesthesia with IV sedation (and possibly also general anesthesia), a validated questionnaire, and inclusion of a cost analysis would be beneficial.
We have shown that patients generally like whichever form of anesthesia we chose for them for carpal tunnel surgery. We have also shown that pure local anesthesia with lidocaine and epinephrine and no tourniquet can increase patient convenience. The choice of the type of anesthesia given to the patient for carpal tunnel surgery is generally made by the surgeon. Surgeons should consider offering their patients the wide awake approach as one of the alternatives of anesthesia for carpal tunnel surgery.
Acknowledgments
The authors did not receive any funding or grant support. The authors give thanks to Denise Leblanc-Duchin, Jan Lalonde, and Susan MacMichael.
Conflict of interest
None.
References
- 1.Apfel CC, Korttila K, Abdalla M, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med. 2004;350(24):2441–2451. doi: 10.1056/NEJMoa032196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atroshi I, Gummesson C, Johnsson R, et al. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282(2):153–158. doi: 10.1001/jama.282.2.153. [DOI] [PubMed] [Google Scholar]
- 3.Chatterjee A, McCarthy JE, Montagne SA, et al. A cost, profit, and efficiency analysis of performing carpal tunnel surgery in the operating room versus the clinic setting in the United States. Ann Plast Surg. 2011;66(3):245–248. doi: 10.1097/SAP.0b013e3181db7784. [DOI] [PubMed] [Google Scholar]
- 4.Farhangkhoee H, Lalonde J, Lalonde DH. Wide-awake trapeziectomy: video detailing local anesthetic injection and surgery. Hand (N Y) 2011;6(4):466. doi: 10.1007/s11552-011-9367-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gelfman R, Melton LJ, 3rd, Yawn BP, et al. Long-term trends in carpal tunnel syndrome. Neurology. 2009;72(1):33–41. doi: 10.1212/01.wnl.0000338533.88960.b9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gold BS, Kitz DS, Lecky JH, et al. Unanticipated admission to the hospital following ambulatory surgery. JAMA. 1989;262(21):3008–3010. doi: 10.1001/jama.1989.03430210050028. [DOI] [PubMed] [Google Scholar]
- 7.Jenkins PJ, Duckworth AD, Watts AC, et al. The outcome of carpal tunnel decompression in patients with diabetes mellitus. J Bone Joint Surg Br. 2012;94(6):811–814. doi: 10.1302/0301-620X.94B6.29174. [DOI] [PubMed] [Google Scholar]
- 8.Koegst WH, Wolfle O, Thoele K, et al. The “Wide Awake Approach” in hand surgery: a comfortable anaesthesia method without a tourniquet. Handchir Mikrochir Plast Chir. 2011;43(3):175–180. doi: 10.1055/s-0031-1280762. [DOI] [PubMed] [Google Scholar]
- 9.Lalonde DH. Wide-awake flexor tendon repair. Plast Reconstr Surg. 2009;123(2):623–625. doi: 10.1097/PRS.0b013e318195664c. [DOI] [PubMed] [Google Scholar]
- 10.Lalonde DH. “Hole-in-one” local anesthesia for wide-awake carpal tunnel surgery. Plast Reconstr Surg. 2010;126(5):1642–1644. doi: 10.1097/PRS.0b013e3181f1c0ef. [DOI] [PubMed] [Google Scholar]
- 11.Lalonde DH. Reconstruction of the hand with wide awake surgery. Clin Plast Surg. 2011;38(4):761–769. doi: 10.1016/j.cps.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 12.Lalonde D, Bell M, Benoit P, et al. A multicenter prospective study of 3,110 consecutive cases of elective epinephrine use in the fingers and hand: the Dalhousie Project clinical phase. J Hand Surg Am. 2005;30(5):1061–1067. doi: 10.1016/j.jhsa.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 13.Le TP, Gan TJ. Update on the management of postoperative nausea and vomiting and postdischarge nausea and vomiting in ambulatory surgery. Anesthesiol Clin. 2010;28(2):225–249. doi: 10.1016/j.anclin.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Leblanc MR, Lalonde J, Lalonde DH. A detailed cost and efficiency analysis of performing carpal tunnel surgery in the main operating room versus the ambulatory setting in Canada. Hand (N Y) 2007;2(4):173–178. doi: 10.1007/s11552-007-9043-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leblanc MR, Lalonde DH, Thoma A, et al. Is main operating room sterility really necessary in carpal tunnel surgery? A multicenter prospective study of minor procedure room field sterility surgery. Hand (N Y) 2011;6(1):60–63. doi: 10.1007/s11552-010-9301-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luckhaupt SE, Dahlhamer JM, Ward BW, et al. Prevalence and work-relatedness of carpal tunnel syndrome in the working population, United States, 2010 National Health Interview Survey. Am J Ind Med. 2012. [DOI] [PMC free article] [PubMed]
- 17.Marcus JR, Tyrone JW, Few JW, et al. Optimization of conscious sedation in plastic surgery. Plast Reconstr Surg. 1999;104(5):1338–1345. doi: 10.1097/00006534-199910000-00015. [DOI] [PubMed] [Google Scholar]
- 18.McAlister FA, Bertsch K, Man J, et al. Incidence of and risk factors for pulmonary complications after nonthoracic surgery. Am J Respir Crit Care Med. 2005;171(5):514–517. doi: 10.1164/rccm.200408-1069OC. [DOI] [PubMed] [Google Scholar]
- 19.Mustoe TA, Buck DW, 2nd, Lalonde DH. The safe management of anesthesia, sedation, and pain in plastic surgery. Plast Reconstr Surg. 2010;126(4):165e–176e. doi: 10.1097/PRS.0b013e3181ebe5e9. [DOI] [PubMed] [Google Scholar]
- 20.Myles PS, Williams DL, Hendrata M, et al. Patient satisfaction after anaesthesia and surgery: results of a prospective survey of 10,811 patients. Br J Anaesth. 2000;84(1):6–10. doi: 10.1093/oxfordjournals.bja.a013383. [DOI] [PubMed] [Google Scholar]
- 21.Steely RL, Collins DR, Jr, Cohen BE, et al. Postoperative nausea and vomiting in the plastic surgery patient. Aesthet Plast Surg. 2004;28(1):29–32. doi: 10.1007/s00266-004-3015-8. [DOI] [PubMed] [Google Scholar]
- 22.Tanaka S, Wild DK, Seligman PJ, et al. The US prevalence of self-reported carpal tunnel syndrome: 1988 National Health Interview Survey data. Am J Public Health. 1994;84(11):1846–1848. doi: 10.2105/AJPH.84.11.1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Williams KS. Postoperative nausea and vomiting. Surg Clin North Am. 2005;85(6):1229–1241. doi: 10.1016/j.suc.2005.09.005. [DOI] [PubMed] [Google Scholar]