Abstract
Background
Proximal median nerve entrapment (PMNE, or pronator syndrome) at the elbow has traditionally been considered an elusive and rare diagnosis, as it is seldom detectable using electrophysiological techniques. In this paper, the clinical manifestations, physical diagnosis, surgical technique, and results of surgical treatment of PMNE are presented, with accompanying instructional video.
Patients/Methods
During 2011, 44 patients with PMNE were surgically released and followed prospectively, 22 women/22 men, mean age 48.8 (range 25–66). The patients were equally distributed between right/left hands (23/21) and the dominant hand was treated in 56 % of cases. The diagnosis was based on: (1) weakness in median innervated muscles distal to the lacertus fibrosus; (2) pain upon pressure over the median nerve at the level of the lacertus fibrosus; and (3) positive scratch collapse test. A minimally invasive surgical treatment using only local anesthesia with lidocaine–epinephrine and no tourniquet was used, and direct perioperative return of strength in median innervated muscles was seen in all subjects.
Results
The average preoperative quick DASH was 35.4 (range 6.8–77.2); work DASH, 44.3 (6.25–100); and activity DASH, 61.6 (12.5–100). There were 71.1 % patients who completed the 6-month follow-up, and the average postoperative quick DASH was 12.7 (range 0–43.1), which is a statistically significant reduction (p < 0.0001; Student’s paired t test). Similarly, the work and activity DASH was significantly reduced (p < 0.001) to 12.5 (0–75) and 6.25 (0–50), respectively.
Conclusions
PMNE at the level of the lacertus fibrosus should be called lacertus tunnel syndrome to distinguish it from other levels of median nerve entrapment. It is a clinical diagnosis based on three distinct clinical findings: weakness, pain over point of compression, and positive scratch collapse test. Surgical release in local anesthesia allows for a safe, ambulatory, and cost-efficient procedure with low morbidity.
Electronic supplementary material
The online version of this article (doi:10.1007/s11552-012-9483-4) contains supplementary material, which is available to authorized users.
Keywords: Entrapment, Median nerve, Pronator syndrome, Surgery, Wide-awake
Background
The pronator syndrome, or proximal median nerve entrapment (PMNE) at the level of the elbow, was first described in literature in the 1950s [18,22], but unlike its distal counterpart—the carpal tunnel syndrome (CTS)—there are only around 50 publications on the diagnosis and treatment of PMNE, whereas a PubMed search on CTS will result in >7,500 publications. This disparity has led surgeons to claim that PMNE is an “extremely rare diagnosis” [16] and a “diagnosis of belief or disbelief” [15], as objective measurements of PMNE can seldom be retrieved.
In what lies the elusiveness of this diagnosis? In this age of insurance-driven medicine, the dependency on so-called objective measurements, i.e., electromyography (EMG) and nerve conduction studies (NCS), is brought to the forefront of medicine whereas clinical diagnosis and examination is often considered subjective, biased, and unreliable [8]. In the case of PMNE, however, there is a conundrum in that proximal median EMG/NCS often is normal or inconclusive, may simulate CTS [5], and has an unreliable specificity of 30–70 % [3]. The shortcomings of electrodiagnostic studies lies in the fact that a nerve may be compressed and cause symptoms distal to the level of compression due to changes in axonal transport and intraneural circulation [17], but the pressure levels of compression are too low to actually cause axonal injury [7] and thus no visible changes in EMG/NCS. More recently, magnetic resonance imaging (MRI) has been suggested as a potential aid in proximal entrapment diagnosis, but in the case of PMNE, the MRI findings are usually normal until there is evident axonal degeneration and muscle wasting of the forearm [1].
The objective of this manuscript is to revisit the clinical findings and diagnosis of PMNE, as well as describe an in situ approach to surgical decompression of the median nerve at the elbow, with video guidance.
Clinical Diagnosis and Treatment
Already in 1874, Erb emphasized the importance of clinical diagnosis for determination of level of nerve affliction in the upper extremity [2]. Similarly, the earliest publications on PMNE describe the need of thorough physical examination to diagnose the patient [18], in particular the presence of weakness in muscles innervated by the median nerve both in the hand and the forearm. The efficacy (sensitivity and specificity) of manual muscle testing of antagonist muscles to determine levels of focal neuropathies in the upper extremities have been established in randomized, blinded validity studies to 88–93 %, respectively [11,12].
The principle is easy: distal to the level of nerve affliction, distinct patterns of muscle weaknesses will be clinically present. In the case of PMNE, these patterns have been determined to primarily correlate to weakness in the flexor pollicis longus (FPL), flexor digitorum profundus II (FDP II), and the flexor carpi radialis (FCR) [19,20].
Symptoms and Clinical Findings
The most common complaints in patients with PMNE at the level of the lacertus fibrosus is a loss of key and tip pinch strength, a loss of fine motor skills and sense of clumsiness (dropping objects), and, rarely, transient paresthesias in the median nerve innervated region of the hand (thumb-radial aspect of ring finger) [10].
Clinically, a symptomatic triad will be evident: (1) the patient will have distinct weakness when manually testing the strength of the muscles innervated by the median nerve distal to the lacertus fibrosus, especially the FPL, FDP II, and FCR (see Video 2); (2) external pressure of the median nerve at the level of the lacertus fibrosus will elicit distinct pain and, at times, a positive Tinel’s sign; and (3) a positive scratch collapse test [6] over the median nerve at the level of the lacertus fibrosus (see Video 1).
Surgical Decompression
Surgical treatment of PMNE has traditionally been associated with a large S-shaped incision to release all potential sites of compression, but carries with it a great disadvantage in the extensive scar tissue that is created.
Our technique has consistently focused on being minimally invasive, releasing the most prominent, and consistently present, constricting structure at the elbow—the lacertus fibrosus. The advent of wide-awake surgery, implying use of local lidocaine–epinephrine infiltration and no tourniquet, has allowed the opportunity to treat these patients with a minor surgical procedure where the return of strength in the median innervated muscles can be appreciated perioperatively.
Anesthesia
The patient is anesthetized 30 min preoperatively using 20–30 ml 1 % lidocaine (10 mg/ml) with epinephrine (5 μg/ml) with 2–3 ml sodium bicarbonate (50 mg/ml) solution added, respectively. Using a 27-in.-gauge needle, the anesthesia is slowly infiltrated from the medial elbow crease and obliquely 4 cm distally and centrally to cover the course of the lacertus fibrosus (Fig. 1). Immediately preoperatively, and after infiltration of the local anesthesia, weakness in FPL and FDP II is again assessed to confirm the diagnosis and rule out the pain block of the anesthetic as a cause of returned muscle strength.
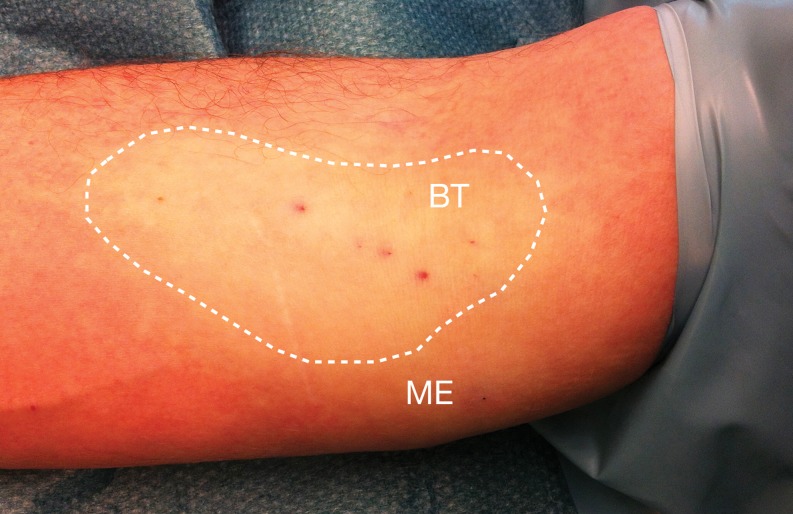
Fig. 1.
Preoperative photo illustrating the area where the infiltration anesthesia was applied to a patient planned for lacertus tunnel release. Thirty milliliters of 1 % lidocaine with epinephrine was administered subcutaneously 30 min preoperatively. The dotted lines mark the area of subcutaneous infiltration, covering the area of the lacertus fibrosus and the medial/central aspect of the elbow and forearm. Skin pallor can be seen as a result of the vasoconstrictive effect from the epinephrine. BT = biceps tendon; ME = medial epicondyle
Surgery (Video 2)
The surgery is performed with the patient awake and no tourniquet. A 2–3-cm transverse incision is placed in the flexion crease of the cubital fossa, from 1 cm medial of the biceps tendon to 2 cm lateral of the medial epicondyle (see Fig. 2a). Careful dissection is made subcutaneously to the pronator teres fascia (Fig. 2b), taking great care to identify and protect branches of the medial antebrachial cutaneous nerve. The pronator teres fascia is incised and followed laterally, allowing exposure of the lacertus fibrosus (Fig. 2c), which is subsequently divided. By retracting the pronator teres muscle medially, the median nerve is readily exposed (Fig. 3d). Any focal adherences to the underlying brachialis muscle may then be released. At this point, the strength of the FPL and FDP II is again tested intraoperatively before the skin is closed, as return of muscle strength is usually immediate after proper release of the nerve (see Video 2). After cauterization, the wound is closed with interrupted sutures, a small soft dressing applied and immediate mobilization encouraged. A load of 1 kg is allowed until suture removal 2 weeks postoperatively. Full load is permitted 4 weeks postoperatively. Patients with no manual labor return to work within 1–2 days postoperatively.
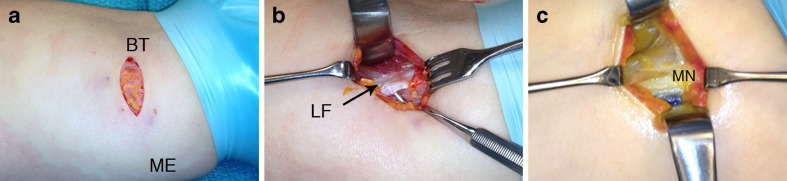
Fig. 2.
Surgical release of the median nerve at the level of the lacertus fibrosus (lacertus tunnel syndrome). a A transverse incision is placed from just medial to the biceps tendon (BT) to just lateral to the medial epicondyle (ME). Following blunt dissection of the subcutaneous tissue, the pronator teres fascia is opened, and the muscle was retracted medially. b The lacertus fibrosus (LF) is carefully isolated (arrow) and divided in its entire length while the median nerve is kept under visual control. c With the pronator teres retracted medially, the median nerve (MN) is easily seen after division of the LF
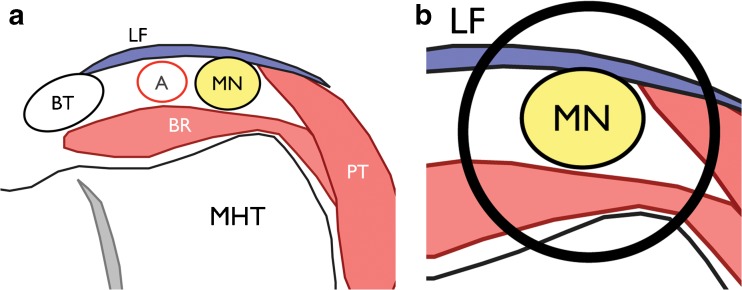
Fig. 3.
a Illustrations of a transverse section of the “lacertus tunnel” at the volar and medial aspect of the elbow, modified from Grant’s Atlas of Anatomy(2). The medial humeral trochlea (MHT) constitutes the bottom of the tunnel; the lateral and medial walls are the brachialis (BR) and pronator teres (PT) muscles, respectively, and the roof is the lacertus fibrosus (LF). MN = median nerve; A = brachial artery; BT = biceps tendon. b zoomed view of the lacertus tunnel
Results
Prospective Follow-Up
Our results of a 5-year retrospective follow-up of 82 patients with PMNE released through surgical decompression has previously been reported [10]. To enhance the objective findings in these patients, we have followed our patients prospectively with quick DASH, including work and activity-related DASH scores, preoperatively and 6 months postoperatively. In addition, the patients answered postoperative questions related to their perceived subjective functions, as recorded using visual analog scales (VAS).
During 2011, 44 patients with PMNE were surgically released and followed prospectively, 22 women/22 men, mean age 48.8 (range 25–66). The patients were equally distributed between right/left hands (23/21), and the dominant hand was treated in 56 % of cases.
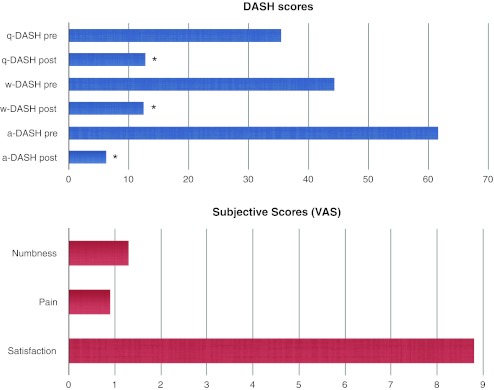
The average preoperative quick DASH was 35.4 (range 6.8–77.2); work DASH, 44.3 (6.25–100); and activity DASH, 61.6 (12.5–100). 71.1 % completed the 6-month follow-up, and the average postoperative quick DASH was 12.7 (range 0–43.1), which is a statistically significant reduction (p < 0.0001; Student’s paired t test). Similarly, the work and activity DASH was significantly reduced (p < 0.001) to 12.5 (0–75) and 6.25 (0–50), respectively.
At the 6-month follow-up, the patients were asked three questions: (1) persistent numbness in the operated hand? (VAS 0 = no paresthesias, 10 = severe paresthesias); (2) persistent pain in the operated elbow/hand? (VAS 0 = no pain, 10 = extreme pain); and (3) satisfaction with surgery? (VAS 0 = completely dissatisfied, 10 = entirely satisfied). The average 6-month VAS scores were as follows: (1) numbness, VAS 1.3; (2) pain, VAS 0.9; (3) satisfaction, VAS 8.8 (Table 1).
Table 1.
Summary of average pre-/postoperative DASH scores and subjective visual analogue scales (VAS) at 6-month follow-up. The top table (blue) illustrates the preoperative and 6 months postoperative quick DASH (q-DASH), work DASH (w-DASH), and activity DASH (a-DASH), following proximal median nerve release at the level of the lacertus fibrosus. * = significant difference (p < 0.001). The bottom table (red) illustrates the results of subjective visual analog scores (VAS) regarding persistent numbness (0 = no paresthesias, 10 = severe paresthesias); persistent pain (0 = no pain, 10 = extreme pain); and satisfaction with surgery (0 = completely dissatisfied, 10 = entirely satisfied)
Discussion
In this paper, a clinical triad to diagnose PMNE at the level of the lacertus fibrosus is described: weakness in muscles innervated distal to the lacertus fibrosus (FCR, FPL, and FDP II); pain over point of compression (lacertus level); and positive scratch collapse test. The prospective analysis shows a statistically significant postoperative improvement in DASH scores (quick, work, and activity DASH, p < 0.001) as compared to preoperative measurements, as well as a high subjective satisfaction (VAS) with the result of surgery.
Pronator syndrome has traditionally been described as an elusive diagnosis, where all seven possible points of nerve compression from the mid-upper arm to the mid-forearm, should be released through a large S-shaped incision [14]. This surgical technique is technically demanding and, most importantly, associated with a high morbidity as it leaves the patient with severe scarring in the arm.
Two recent publications advocating minimally invasive treatment of pronator syndrome, one open technique [23] and one arthroscopic [13], have challenged the idea of a large incision to treat pronator syndrome. The open technique, as published by Zancolli et al. [23], describe a syndrome where the patient has concomitant carpal tunnel syndrome, weakness in the superficialis muscles (FDS IV) and paresthesia elicited upon compression of the nerve at the level of the superficialis arcade. Both techniques have in common that they primarily release the “fibrous arcade” of the superficialis muscles, located approximately 7 cm distal to the elbow crease. The clinical findings and surgical release thus differ greatly from that described in this manuscript.
In 1945, Sunderland described the internal topography of the radial, median, and ulnar nerves from the axilla to the hand [21]. Based on this original investigation, he concluded: “The nature, extent and peripheral effects of injury sustained by a nerve as the result of trauma are influenced by the funicular pattern at the site of injury.” In an early stage of nerve compression syndrome, there is no actual injury to the nerve, rather ischemic changes and alterations in axonal transport, but the correlation to funicular patterns is still relevant.
Akin to the carpal tunnel, at the level of the lacertus fibrosus, the median nerve passes through a “tunnel,” where the bottom, the lateral wall, and medial wall are the medial trochlea of the humerus, the brachialis, and the pronator muscles, respectively, and the roof is the lacertus fibrosus (Fig. 3). According to Sunderland [21], at this “lacertus tunnel,” the median nerve is organized such that the branches to the pronator teres and FCR are located anteriorly, and the branches to the FPL and FDP II, medially. At the level of the superficialis arcade, on the other hand, the anterior and superficial branches correspond to the FDS and the cutaneous innervation of the hand. These anatomical variations are mirrored in the clinical differences and varying levels of surgical release in the Zancolli publication and the present manuscript, and may be understood as two independent entrapments of the median nerve proximal to the carpal tunnel—one at the level of the superficialis arcade, the other at the level of the lacertus fibrosus. A more distinct and accurate description would thus be to name these the “superficialis syndrome” and “lacertus tunnel syndrome” (LTS), respectively.
The scratch collapse test (SCT) has previously been shown to be a sensitive clinical provocative maneuver in diagnosing peripheral nerve entrapments, with a higher sensitivity than traditional clinical tests, such as Tinel’s and compression tests, in diagnosing carpal tunnel and cubital tunnel syndromes [6], as well as peroneal nerve entrapment [9]. The use of the SCT has also been suggested as an important tool in differentiating between levels of ulnar nerve entrapment at the level of the elbow [4]. Similarly, SCT was an important adjunct in diagnosing LTS, along with specific muscle weakness and pain at the level of entrapment (lacertus tunnel).
In conclusion, proximal median nerve entrapment at the level of the lacertus fibrosus should be referred to as lacertus tunnel syndrome, LTS, to distinguish it from other levels of median nerve entrapment. It is a clinical diagnosis based on three distinct clinical findings: weakness, pain over point of compression, and positive scratch collapse test. Surgical release in local anesthesia allows for a safe, ambulatory, and cost-efficient procedure with low morbidity. Larger, multi-center, and prospective studies are planned to further enhance our understanding of this prevalent, but frequently misunderstood, diagnosis.
Electronic Supplementary Material
The video shows the scratch collapse test in a patient with right-sided lacertus tunnel syndrome. The patient is asked to sustain external rotation of the shoulders with elbows flexed, while the skin over the area of nerve compression is scratched, eliciting a temporary loss of muscle resistance. The healthy left side is compared to the contralateral side where a lacertus tunnel syndrome is present. (MOV 14518 kb)
The video illustrates the preoperative clinical examination of a patient with proximal median nerve entrapment (“lacertus tunnel syndrome”), where the flexor carpi radialis (FCR), flexor pollicis longus (FPL), and flexor digitorum profundus of the index finger (FDP II) are found to be weak, as compared to the healthy arm. The appearance of the arm following infiltration anesthesia, detailed description of the surgical technique and immediate peri-/postoperative return of strength following nerve release is also shown in this instructional video. (MOV 206403 kb)
Acknowledgments
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Andreisek G, Crook DW, Burg D, Marincek B, Weishaupt D. Peripheral neuropathies of the median, radial, and ulnar nerves: MR imaging features. Radiogr: Rev Publ Radiol Soc N Am, Inc. 2006;26(5):1267–1287. doi: 10.1148/rg.265055712. [DOI] [PubMed] [Google Scholar]
- 2.Boyes JH. On the shoulders of giants. Philadelphia: J.B. Lippincott; 1976. [Google Scholar]
- 3.Bridgeman C, Naidu S, Kothari MJ. Clinical and electrophysiological presentation of pronator syndrome. Electromyogr Clin Neurophysiol. 2007;47(2):89–92. [PubMed] [Google Scholar]
- 4.Brown JM, Mokhtee D, Evangelista MS, Mackinnon SE. Scratch collapse test localizes osborne’s band as the point of maximal nerve compression in cubital tunnel syndrome. Hand (N Y). 2010;5(2):141–147. doi: 10.1007/s11552-009-9225-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang MH, Lee YC, Hsieh PF. The real role of forearm mixed nerve conduction velocity in the assessment of proximal forearm conduction slowing in carpal tunnel syndrome. J Clin Neurophysiol. 2008;25(6):373–377. doi: 10.1097/WNP.0b013e31818e7930. [DOI] [PubMed] [Google Scholar]
- 6.Cheng CJ, Mackinnon-Patterson B, Beck JL, Mackinnon SE. Scratch collapse test for evaluation of carpal and cubital tunnel syndrome. J Hand Surg Am. 2008;33(9):1518–1524. doi: 10.1016/j.jhsa.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 7.Dahlin LB, Lundborg G. The neurone and its response to peripheral nerve compression. J Hand Surg Br. 1990;15(1):5–10. doi: 10.1016/0266-7681(90)90040-B. [DOI] [PubMed] [Google Scholar]
- 8.Franklin GM, Glass L, Javaher SP, Kearney RN. Work-related proximal median nerve entrapment (PMNE) diagnosis and treatment. In: Industries WSDoLa, ed. Seattle, Washington 2009:1–11
- 9.Gillenwater J, Cheng J, Mackinnon SE. Evaluation of the scratch collapse test in peroneal nerve compression. Plast Reconstr Surg. 2011;128(4):933–939. doi: 10.1097/PRS.0b013e3181f95c36. [DOI] [PubMed] [Google Scholar]
- 10.Hagert CG, Hagert E. Manual muscle testing—a clinical excamination technique for diagnosing focal neuropathies in the upper extremity. In: Slutsky DJ, editor. Upper extremity nerve repair—tips and techniques: a master skills publicatioN. Rosemont: the American Society for Surgery of the Hand; 2008. pp. 451–466. [Google Scholar]
- 11.Jepsen JR, Laursen LH, Hagert CG, Kreiner S, Larsen AI. Diagnostic accuracy of the neurological upper limb examination II: relation to symptoms of patterns of findings. BMC Neurol. 2006;6:10. doi: 10.1186/1471-2377-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jepsen JR, Laursen LH, Kreiner S, Larsen AI. Neurological examination of the upper limb: a study of construct validity. Open Neurol J. 2009;3:54–63. doi: 10.2174/1874205X00903010054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee AK, Khorsandi M, Nurbhai N, Dang J, Fitzmaurice M, Herron KA. Endoscopically assisted decompression for pronator syndrome. J Hand Surg Am. 2012;37(6):1173–1179. doi: 10.1016/j.jhsa.2012.02.023. [DOI] [PubMed] [Google Scholar]
- 14.Mackinnon SE, Novak CB. Compression neuropathies. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin S, editors. Green’s operative hand surgery, 6th Edition. Vol 1. 6. Philadelphia: Elsevier Churchill Livingston; 2011. pp. 977–1014. [Google Scholar]
- 15.Presciutti S, Rodner CM. Pronator syndrome. J Hand Surg Am. 2011;36(5):907–909. doi: 10.1016/j.jhsa.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 16.Rehak DC. Pronator syndrome. Clin Sports Med. 2001;20(3):531–540. doi: 10.1016/S0278-5919(05)70267-2. [DOI] [PubMed] [Google Scholar]
- 17.Rydevik B, Lundborg G. Permeability of intraneural microvessels and perineurium following acute, graded experimental nerve compression. Scand J Plast Reconstr Surg. 1977;11(3):179–187. doi: 10.3109/02844317709025516. [DOI] [PubMed] [Google Scholar]
- 18.Seyffarth H. Primary myoses in the M. pronator teres as cause of lesion of the N. medianus (the pronator syndrome) Acta psychiatr Neurol Scand Suppl. 1951;74:251–254. [PubMed] [Google Scholar]
- 19.Stal M, Hagert CG, Moritz U. Upper extremity nerve involvement in Swedish female machine milkers. Am J Ind Med. 1998;33(6):551–559. doi: 10.1002/(SICI)1097-0274(199806)33:6<551::AID-AJIM5>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 20.Stal M, Hagert CG, Englund JE. Pronator syndrome: a retrospective study of median nerve entrapment at the elbow in female machine milkers. J Agric Saf Heal. 2004;10(4):247–256. [PubMed] [Google Scholar]
- 21.Sunderland S. The intraneural topography of the radial, median and ulnar nerves. Brain. 1945;68:243–299. doi: 10.1093/brain/68.4.243. [DOI] [PubMed] [Google Scholar]
- 22.Tsai TM, Syed SA. A transverse skin incision approach for decompression of pronator teres syndrome. J Hand Surg Br. 1994;19(1):40–42. doi: 10.1016/0266-7681(94)90047-7. [DOI] [PubMed] [Google Scholar]
- 23.Zancolli ER, Zancolli EP, 3rd, Perrotto CJ. New Mini-invasive decompression for pronator teres syndrome. J Hand Surg Am. 2012;37(8):1706–1710. doi: 10.1016/j.jhsa.2012.05.033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The video shows the scratch collapse test in a patient with right-sided lacertus tunnel syndrome. The patient is asked to sustain external rotation of the shoulders with elbows flexed, while the skin over the area of nerve compression is scratched, eliciting a temporary loss of muscle resistance. The healthy left side is compared to the contralateral side where a lacertus tunnel syndrome is present. (MOV 14518 kb)
The video illustrates the preoperative clinical examination of a patient with proximal median nerve entrapment (“lacertus tunnel syndrome”), where the flexor carpi radialis (FCR), flexor pollicis longus (FPL), and flexor digitorum profundus of the index finger (FDP II) are found to be weak, as compared to the healthy arm. The appearance of the arm following infiltration anesthesia, detailed description of the surgical technique and immediate peri-/postoperative return of strength following nerve release is also shown in this instructional video. (MOV 206403 kb)