Abstract
Background
The purpose of this study was to establish the characteristics of patients who are transferred from referring emergency departments (EDs) to two receiving institutions for hand-related emergencies. Our primary hypothesis was that many transferred patients would not require emergent specialty intervention. Our secondary hypotheses were that treatment would differ by day of presentation and type of insurance coverage.
Methods
We searched ED records for all hand-related cases over 1 year. We reviewed charts for demographics and treatment details. The main outcome measures were whether patients were seen by a hand surgeon or underwent surgery within 24 h of transfer.
Results
The study group comprised 296 patients. Ninety-two percent saw a specialty resident, and 48 % saw a hand surgeon. Thirty-nine percent of patients were taken to the operating room within 24 h of presentation. Of patients transferred on the weekends, 48 % saw a hand surgeon versus 61 % of those transferred on weekdays. Similarly, 51 % of patients transferred on a weekday were taken to the OR within 24 h, while 38 % of patients transferred on a weekend were taken to the OR in the same time frame.
Conclusions
More than half of transfers for hand emergencies did not result in examination by a hand surgeon, and nearly two thirds did not require a visit to the OR within 24 h. Patients transferred on the weekend were less likely to see a hand surgeon than those transferred on weekdays. Alternative methods of consultation might allow avoidance of transfer.
Keywords: Hand call, Hand emergency, Inter-hospital transfer
Introduction
Inter-hospital transfer of patients can be costly, inconvenient for patients, and risky. There has been much study of the reasons behind inter-hospital transfers in orthopedic trauma. Several studies have demonstrated a relationship between the transfer of trauma patients and insurance status [1, 3]. Among these, Koval and colleagues found that transferred trauma patients were more likely to be underinsured and admitted during the evening or at night than those patients with similar injuries who were not transferred [7].
There is less information available as to the reasons for inter-hospital transfers for hand emergencies. Hand surgeons at receiving facilities often feel that patients are transferred unnecessarily. A 2010 American Society for Surgery of the Hand member survey revealed that 71 % of hand surgeons surveyed thought their institution received “an excess of unwarranted referrals for hand trauma.” In 2010, Patterson and colleagues found that most of the emergency hand transfers accepted by their level I trauma center did not require the resources of a level I center [11]. Similarly, a recent study by Ozer and colleagues demonstrated that 65 % of patients air-transferred to their institution for replantation did not actually undergo replantation [10].
However, emergency physicians at referring facilities may not have reliable means of accessing a hand specialist other than inter-hospital transfer [8]. Indeed, the Institute of Medicine described the lack of on-call specialist availability “one of the most troubling trends” in emergency care in 2006 [6]. In a recent national survey of emergency department (ED) directors, 80 % reported inadequate access to hand surgeons on call [12]. A similar survey of ED directors in California demonstrated that even as subspecialty call becomes less available, ED to ED transfer is also becoming more difficult [9]. This may make it increasingly difficult for patients with hand emergencies to receive the care they need and for emergency physicians to obtain the consultations they deem necessary for appropriate care.
The goal of this study was to establish the characteristics of patients who are transferred from referring institutions to two level I trauma centers for hand-related emergencies. The primary hypothesis was that many patients transferred would not require emergency care by a hand surgeon. One secondary hypothesis was that those patients not requiring emergency care would be disproportionately represented among transfers taking place on weekends, when referring institutions may have more difficulty accessing specialty care. Another secondary hypothesis was that patients with lower reimbursing insurance would be more likely to be transferred for non-emergent care.
Materials and Methods
We reviewed all ED to ED transfers of adult patients into two level I trauma hospitals for hand-related emergencies during calendar year 2010. Both hospitals maintain databases with information collected at the time of each patient’s registration in the ED. Each transfer record includes a text entry of “chief complaint.” We searched this text field for “hand,” “finger,” “thumb,” “saw,” “bite,” “ampu,” “tendon,” and “tenosynovitis.” With these search terms, we were able to identify 100 % of patients with hand-related emergencies in a sample group of 500 consecutive ED to ED transfers and then applied the algorithm to the entire calendar year.
We manually reviewed the electronic medical record of each subject to ensure that the data listed in the databases were correct, as well as to collect information on demographics and the details of their hospital visit. Specifically, we examined events taking place in our EDs as well as any surgeries, hospital admissions, and later office visits with our hand surgeons.
We excluded patients who were transferred for evaluation by a service other than hand surgery, such as hand burns, which are seen by the burn surgery service at our institutions. Second, we excluded patients who were referred from an outpatient setting, rather than transferred from another ED. We categorized each subject’s insurance status and then divided these into “higher reimbursing” (private insurance, Workers’ Compensation, Medicare) and “lower reimbursing” (Medicaid, charity and welfare programs, self-pay). We were unable to determine whether a specialist had been consulted at the referring institution prior to transfer of the patient.
Our two main outcome measures were whether the patient was seen by a resident or a hand surgeon on the day of transfer and whether the patient underwent a procedure in the operating room on the day of transfer. We defined “hand surgeon” as either a fellow or an attending in hand surgery, as our fellows have independent admitting and operating privileges.
We tested associations using odds ratios and the chi-squared test. The modified Wald method was used to calculate confidence intervals. This study was approved by the IRB.
Results
The database of hospital 1 contained 415 records. Of these, we excluded 111 as referrals for other services, 112 as not being true ED to ED transfers, and 42 patients under the age of 18. This left 150 included patients. The database of hospital 2 contained 189 records, 36 of which we excluded as referrals for other services, 4 for not being transfers, and 3 for being less than 18 years of age. This left 146 patients in the hospital 2 database, and a total of 296 patients overall.
Patient demographics were similar between the two hospitals. The majority of patients were male non-Hispanic whites. Most were transferred via ambulance (Table 1).
Table 1.
Patient demographics
| Number (%) | |
|---|---|
| Age in years, mean (SD) | 45.4 (15.4) |
| Male | 240 (81) |
| Female | 56 (19) |
| White | 235 (79) |
| Black | 10 (3) |
| Hispanic | 37 (13) |
| Other | 14 (5) |
| Higher reimbursing insurance | 215 (73) |
| Lower reimbursing insurance | 81 (27) |
| Transferred on weekend | 135 (46) |
| Transferred on weekday | 161 (54) |
| Method of transport | |
| Ambulance | 216 (73) |
| Private car | 16 (5) |
| Helicopter | 6 (2) |
| Unknown | 58 (20) |
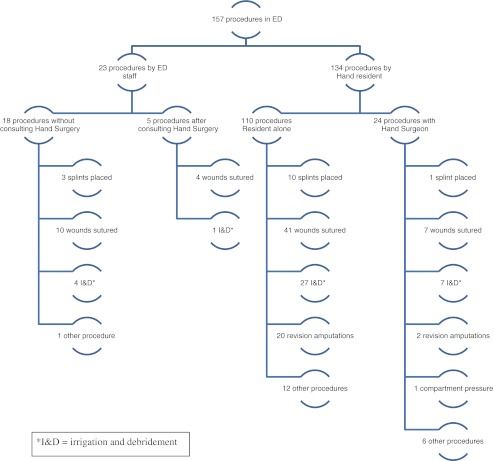
At the referring hospitals’ EDs, patients generally received interventions consistent with initial stabilization, while procedures tended to be performed in the receiving ED. Almost all patients were seen by a resident from the Orthopaedic Surgery or Plastic Surgery service during their visit to our EDs, while 55 % were also seen by a hand surgeon in the ED (Table 2). Fifty-three percent of patients underwent a procedure in the receiving EDs. Details of those procedures can be found in Fig. 1. Of these patients, 38 (24 %) underwent a procedure in the ED and later underwent surgery in the OR.
Table 2.
Components of ED visits
| Referring EDs | Receiving EDs | |
|---|---|---|
| Number (%, 95 % CI) | Number (%, 95 % CI) | |
| IV antibiotics | 221 (75, 69.4–79.3) | 92 (31, 26.1–36.6) |
| Tetanus booster | 146 (49, 43.7–55.0) | 25 (8, 5.7–12.2) |
| Plain radiographs | 184 (62, 56.5–67.5) | 175 (59, 53.4–64.6) |
| CT/MRI | 2 (1, 0.0–2.6) | 1 (0.3, 0.0–2.1) |
| Seen by resident in receiving ED | – | 272 (92, 88.2–94.5) |
| Seen by hand surgeon in receiving ED | – | 141 (48, 42.0–53.3) |
Fig. 1.
Procedures performed during ED visits
At disposition from our EDs, 40 % of patients were discharged to home, 52 % were admitted to the hospital, and 8 % were admitted to the ED Observation Unit (specifically designated for hospital stays less than 24 h duration). Thirty-nine percent of patients were taken to the operating room within 24 h of presentation on an emergency basis. Sixteen percent of patients went to the operating room on a subacute basis (generally within 1 week of presentation), and 45 % of patients never underwent surgery in the operating room. Operative interventions performed are described in Table 3.
Table 3.
Operative interventions
| Number (%) | |
|---|---|
| Repair of combined injury | 54 (33) |
| Attempted revascularization/replant | 27 (16) |
| Irrigation and debridement infection | 26 (16) |
| Exploration of penetrating wound | 14 (9) |
| Skin flap or graft | 7 (4) |
| Repair of closed fracture | 6 (4) |
| Repair of fingertip injury | 6 (4) |
| Repair of open fracture | 5 (3) |
| Isolated nerve repair | 4 (2) |
| Fasciotomy | 3 (2) |
| Other | 12 (7) |
| Total | 164 |
Of patients transferred on the weekends (Friday, Saturday, or Sunday), 48 % saw a hand surgeon at the receiving centers on the day of transfer versus 61 % of those transferred on weekdays (odds ratio = 0.60, 95 % CI 0.38–0.95). There was no difference in likelihood of seeing a hand surgeon on the day of transfer between patients with higher reimbursing insurance versus lower reimbursing insurance. Similarly, 51 % of patients transferred on a weekday were taken to the OR within 24 h, while only 38 % of patients transferred on a weekend were taken to the OR in the same time frame (odds ratio 0.57, 95 % CI 0.36–0.91). Again, there was no difference in likelihood of having surgery within 24 h of transfer between patients with higher reimbursing insurance and lower reimbursing insurance.
Discussion
We found that 48 % of patients transferred emergently for hand surgery consultation saw an attending hand surgeon within 24 h, and 39 % were taken to the operating room within 24 h. This low percentage does not mean these transfers were unwarranted, as the vast majority of transferred patients (92 %) received a consultation by a resident in hand surgery, and 53 % of transferred patients underwent some type of procedure in the receiving EDs. Additionally, we do not know precisely how often the hand surgeon was contacted by the resident.
Given the low percentage of patients who were taken to surgery within 24 h, our results do indicate that patients may be transferred for reasons other than the need for emergent surgery. However, unlike prior investigations into reasons for ED transfers, ours did not find any differences among our patients based on insurance status. Less than 13 % of the patients in this study were completely uninsured. We did find that transferred patients were less likely to see a hand surgeon and go to the OR on weekends versus weekdays. Given the shortage of available specialists discussed earlier, it seems likely that referring emergency physicians have more trouble finding local hand surgeons on the weekends and so transfer patients of lower acuity. However, it also may be that hand surgeons at the receiving institutions are less willing to come into the ED and/or perform surgery on the weekends. In either case, this practice variability is unlikely to be related to characteristics of the presenting emergency and, thus, may represent an opportunity for quality improvement.
One method that has the potential to address this difference and to decrease transfer of low-acuity patients would be to develop telemedicine systems that allow generalists to get advice from hand surgeons about whether to initiate a transfer. If hand surgeons could be connected virtually to the transferring ED, they may be able to guide the ED through appropriate emergency care and arrange urgent follow-up while avoiding transfer. In 1997, Buntic and colleagues proposed a protocol of using the digital transmission of photographs and radiographs to identify replantation candidates [2]. Nearly 15 years later, this innovative idea is technologically viable and yet rarely practiced. A recent study by Hsieh and colleagues examined the same question with more modern technology [5]. In their study, a hand surgeon first viewed photographs of the hand injuries and created a triage plan for the patient (conservative management, primary closure, or attempted replantation). The same surgeon then saw the patient in person. They found that the in-person examination altered the triage plan in 15 % of patients.
Telephone consultations with specialists are already routine practice in some areas with limited access to hand specialists [8]. We suggest that in many cases, a telephone consultation in combination with a digital photograph transmitted by e-mail or text message could fulfill the needs of the patient and emergency physician while improving overall efficiency. However, issues of the security of health information transmitted electronically, physician liability, and lack of a method of reimbursement for such consultations all present potential obstacles.
In terms of security, data transmitted electronically could either be de-identified or encrypted, both methods commonly used in transmission of research data currently. To protect physician liability, we suggest a customized consent form. Reimbursement for remote consultation is more challenging, but there is precedent in the field of telemedicine. Some surgeons may choose to perform these consultations without reimbursement as a routine part of call. Others, such as those operating within a larger hospital system, may be able to set a standardized fee for remote consultation. As practice environments vary, so too will the approach to reimbursement.
This study has limitations. Our data are limited to one region of the country, and referral patterns may be different in other areas. Massachusetts is distinct in its universal health insurance mandate, and further study is required to evaluate the effect of this mandate on our results. During this time period, Massachusetts had the lowest percentage of uninsured patients in the USA [4]. The lack of a relationship of transferred patients to insurance status may differ in other geographic areas. In both hospitals studied here, patients are accepted for transfer directly by emergency physicians, whereas hand surgeons in other systems may have more direct contact with their referring institutions. Additionally, our study is retrospective, and therefore, we cannot speculate beyond what is included in the medical records. Finally, our study is biased in that we did not evaluate patients who presented to referring institutions with a hand emergency and were not transferred.
We conclude that in this study, more than half of the patients transferred for hand emergencies did not receive an emergency consultation with a hand surgeon and did not undergo emergent surgery. Many patients could benefit from remote consultation prior to, or instead of, inter-hospital transfer. Further study is required to establish the safety and efficacy of such consultations.
Acknowledgments
Conflict of interest
The authors have no conflicts of interest, commercial associations, or intent of financial gain regarding this research.
References
- 1.Archdeacon MT, Simon PM, Wyrick JD. The influence of insurance status on the transfer of femoral fracture patients to a Level-I trauma center. J Bone Joint Surg. 2007;89:2625–2631. doi: 10.2106/JBJS.F.01499. [DOI] [PubMed] [Google Scholar]
- 2.Buntic RF, Siko PP, Buncke GM, et al. Using the internet for rapid exchange of photographs and x-ray images to evaluate potential extremity replantation candidates. J Trauma. 1997;43:342–344. doi: 10.1097/00005373-199708000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Goldfarb CA, Borrelli J, Lu M, et al. A prospective evaluation of patients with isolated orthopedic injuries transferred to a Level I trauma center. J Orthop Trauma. 2006;20:613–617. doi: 10.1097/01.bot.0000249415.47871.e5. [DOI] [PubMed] [Google Scholar]
- 4.Health Reform in Massachusetts: expanding access to health insurance coverage. Assessing the results. Blue Cross Blue Shield of Massachusetts Foundation. 2011. Available at: http://bluecrossmafoundation.org/health-reform/~/media/d0dda3d667be49d58539821f74c723c7.pdf. Accessed 6 Aug 2012.
- 5.Hsieh C, Tsai H, Yin J, et al. Teleconsultation with the mobile camera-phone in digital soft-tissue injury: a feasibility study. Plast Reconstr Surg. 2004;114:1776–1782. doi: 10.1097/01.PRS.0000142402.07896.21. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine: committee on the future of emergency care in the United States health system. Hospital-based Emergency Care at the Breaking Point. Washington DC: The National Academies Press; 2006.
- 7.Koval KJ, Tingey CW, Spratt KF. Are patients being transferred to Level-I trauma centers for reasons other than medical necessity? J Bone Joint Surg. 2006;88A:2124–2132. doi: 10.2106/JBJS.F.00245. [DOI] [PubMed] [Google Scholar]
- 8.Labs JD. Standard of care for hand trauma: where should we be going? Hand. 2008;3:197–202. doi: 10.1007/s11552-008-9117-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Menchine MD, Baraff LJ. On-call specialists and higher level of care transfers in California emergency departments. Acad Emerg Med. 2008;15:329–336. doi: 10.1111/j.1553-2712.2008.00071.x. [DOI] [PubMed] [Google Scholar]
- 10.Ozer K, Kramer W, Gillani S, et al. Replantation versus revision of amputated fingers in patients air-transported to a Level 1 trauma center. J Hand Surg. 2010;35A:936–940. doi: 10.1016/j.jhsa.2010.02.031. [DOI] [PubMed] [Google Scholar]
- 11.Patterson JM, Boyer MI, Ricci WM, et al. Hand trauma: a prospective evaluation of patients transferred to a level I trauma center. Am J Orthop. 2010;39:196–200. [PubMed] [Google Scholar]
- 12.Rao MB, Lerro C, Gross CP. The shortage of on-call surgical specialist coverage: a national survey of emergency department directors. Acad Emerg Med. 2010;17:1374–1382. doi: 10.1111/j.1553-2712.2010.00927.x. [DOI] [PubMed] [Google Scholar]