Abstract
Objective:
The objective was to determine the basic hematological parameters of remunerated blood donors in Benin City and to compare them with those of voluntary donors.
Materials and Methods:
This is a prospective study conducted in a tertiary health facility in Benin City. Pretransfusion samples were obtained from blood bags after gentle mixing and analyzed for hematological parameters. Samples were analyzed using the hematology autoanalyzer MODEL SYSMEX KN21.
Result:
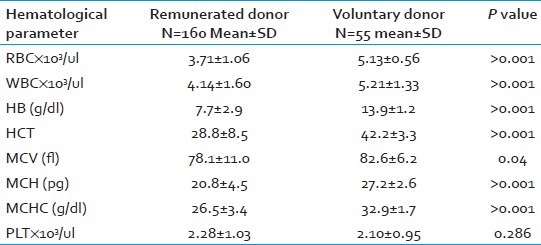
A total of 215 samples were obtained comprising 160 remunerated (paid) and 55 voluntary donor samples. In the paid donors, the mean hemoglobin concentration (Hb) and hematocrit (HCT) 7.7±2.9 and 28.8±8.5 respectively. This was significantly lower than those of voluntary donors who had 13.9±1.2 and 42.2±3.3 with P < 0.001. The mean values of the red cell counts (RBC), white cell counts (WBC), mean cell volume (MCV), mean corpuscular hemoglobin (MCH), and mean corpuscular hemoglobin concentration (MCHC) were significantly lower in paid donors as P-values were < 0.001. MCV was significantly low but not compared to the other parameters as P=0.04. There was no significant difference in the platelet count.
Conclusion:
Paid donors in Benin City have significantly lower hematological parameters than controls.
Keywords: Benin, hematological parameters, remunerated donors, voluntary donors
INTRODUCTION
Blood donors are grouped into voluntary donors, replacement donors, and paid donors. The safest of these is the voluntary donor blood. Blood banking is highly regulated to ensure both donor and recipient safety. The goal of blood banking is to provide adequate and safe blood to recipients at no risk to donors.[1] Baseline hemoglobin of 12 g/dl and 13 g/dl for potential female and male donors' respectively,[2] and a donation interval of 12 weeks minimum have been stipulated in some countries to ensure donor safety.[3] As a way of attaining this goal, voluntary nonremunerated blood donation is encouraged and the World Health Organization (WHO) has set a target of achieving 100% voluntary non remunerated donation by 2020.[4] Nigeria as a member nation of WHO has made little progress with voluntary donor recruitment. Only about 5% of donor bloods used in Nigeria come from voluntary donors; family replacements and paid donors are still the major sources of donor blood procurement.[5–9]
The blood banking system in Nigeria is still poorly developed as a number of centers depend on paid donors whose hematological and infectious status may not determined often times prior to blood donations.
Our aim therefore is to determine the basic hematological parameters of paid blood donors in Benin City compared to voluntary donors.
MATERIALS AND METHODS
This is a prospective cross-sectional study conducted in a tertiary health facility in Benin City, Nigeria. The center has a blood bank unit and utilizes an average of 7,000 units of blood annually. Paid donors are the major source of blood supply through a vendor. Collection by the vendor is usually not supervised by hospital personnel but adheres to routine guidelines for phlebotomy. The vendor brings the units of blood to the hospital in fulfillment of a contractual agreement.
Blood was collected from donor blood bags within 48 h of donation. The blood bag contains 450 ml of donor blood and 63 ml of anticoagulant (citrate phosphate dextrose and adenine). The blood bag was gently rocked to homogenize before sampling. Blood in the donor bag tubing was removed before collecting about 2-3 ml of blood into a plain container to avoid dilution by anticoagulant in EDTA bottle.
Two hundred and fifty (215) samples were collected from donor bags comprising 160 paid donor samples and 55 voluntary donor samples to serve as control. The voluntary donors are mainly males to allow for even comparison with paid donors who are mainly males. The samples were analyzed immediately using the hematology autoanalyzer MODEL: SYSMEX KN21. Procedures were performed according to the standard operating manuals.
Statistics
Data were analyzed using the statistical Package for Social Sciences (SPSS 16). Comparison of mean values between the two populations was made using Student's t-test for independent variables. P values < 0.05 were considered significant.
RESULTS
A total of 215 samples were analyzed comprising 160 paid donor and 55 voluntary donor samples. The remunerated donor samples had mean values of hemoglobin (Hb) 7.7±2.9, hematocrit (HCT) 28.8±8.5, red blood cell (RBC) count 3.71±1.06, white blood cell (WBC) count 4.14±1.60, RBC mean corpuscular volume (MCV) 78.1±11.0, mean corpuscular hemoglobin (MCH) 20.8±4.5, mean corpuscular hemoglobin concentration (MCHC) 26.5±3.4, and platelet count 2.28±1.03. The control group (voluntary donors) has significantly higher parameters as shown in Table 1. The hemoglobin, white blood cell count, RBC count, HCT, MCH, and MCHC were significantly lower in paid donors as P-values were <0.001. Though the MCV was significantly low but not compared to the other parameters as P = 0.04. There was no significant difference in the platelet count of the two groups.
Table 1.
Hematological parameters in the study population
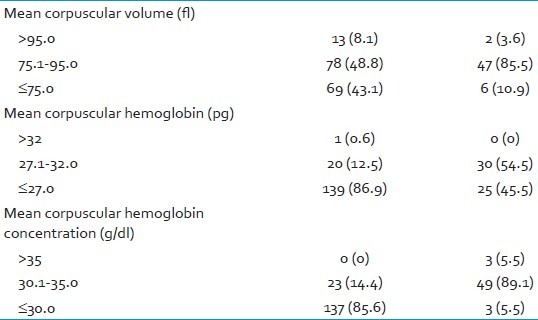
The hemoglobin concentration (Hb) of 91.2% (146/160) of the paid donor blood were ≥12 g/dl while 8.8% (14/160) were >12 g/dl. Among voluntary donors, 92.7% (51/55) had Hb >12 g/dl while 7.3% (4/55) had ≥12 g/dl as in Table 2. The MCV of 43.1% (69/160) of paid donors were ≥75 fl; 8.1% (13/160) had values >95 fl. In the control group, 10.9% (6/55) had MCV ≥75 fl while 3.6% (2/55) had values >95 fl. The MCH of 86.9% (139/160) of the paid donors was ≥27 pg as against 45.5% (25/55) of the control. Majority of the test group had MCHC ≥30 g/dl as against 5.5% (3/55) of the control [Table 3].
Table 2.
Hemoglobin ranges in the study population
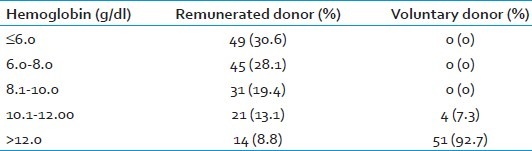
Table 3.
Red cell indices in the study population
DISCUSSION
The dwindling levels of voluntary blood donors has lead to some hospitals relying on the provision of blood of blood by blood vendors in order to maintain the blood transfusion needs of the local community. This study revealed an unacceptably low hemoglobin concentration in remunerated donors. The concomitant reduction in the red cell indices further suggest that the anemia most likely resulted from too frequent blood donation. Remunerated donors are more liable to conceal information regarding frequency of donation and often patronize more than one blood vendors in an attempt to earn more money.
Most donors in this category may have been the high risked group including paid motor drivers, motor boys and drug abusers who are prepared to do anything to maintain their habits. The attitude of not checking their baseline hematocrit by the vendors because of the financial gains further worsens the problem. Good transfusion practice entails measures that protect donors and recipients. The low hemoglobin levels found in this study suggests that donor safety may have been overlooked in an attempt to make blood available to their clients (hospitals).
Though iron studies were not done in this study but other studies have reported a high incidence of iron deficiency anemia in frequent donors.[10–12] Endemicity of parasitic infections such as malaria, malnutrition and helminthic infestations has been reported to contribute to the low red cell indices.[13]
Several studies have reported anemia in blood donors,[14–15] with higher frequencies in Africa than in Western countries.[15–17] Erharbor et al. in a similar study reported that hemoglobin levels are lower in remunerated blood donors than replacement donors in Nigeria.[17] Anemia is the most common reason for donor ineligibility.[18]
It is worthy mentioning that the mean values of the control group is similar to the hematological parameters of the population of other African countries.[19,20]
The implication of this is that a number of the donors may be endangered by these vendors for their financial gains. Secondly the desired increment in hemoglobin of the potential recipients can only be attained by transfusion of several units beyond the expected. The risk of associated transfusion transmissible infections is therefore further increased.
Unemployment with its attendant poverty produces a vicious cycle of anemia. Transfusion requirement and more demand which in turn drive paid donors to donate more often than the required 12 weeks minimum interval further complicates it.
A lack of coordinated blood donation in many health facilities in the country further deepens the reliance on paid donors. The poor quality of donor blood from remunerated donors viz-a-viz low hematocrit and red cell indices found in this study has further reiterated the need for another look at the WHO guidelines on blood donation. While this guideline is arguably the best for donor and patient safety, the precarious health situation in developing countries may necessitate the need to formulate policies that will ensure blood availability to blood banks at all times while preserving donor safety. Blood banks may include a modified replacement donation system in which potential recipients are encouraged to bring donors who are screened for fitness at a particular health facility prior to donation.
The demand for blood is high and far outweighs its supply. This is further worsened by the practice of whole blood transfusion allowing for wastage. Complying with hemoglobin references used in other centers with well-developed blood banking system will further deplete local blood supply. There is need to establish a local reference which must be strictly enforced so as not to endanger donors without depleting blood supply. There is also a need to embark on massive enlightenment campaign to encourage voluntary donors so as to improve qualitative and quantitative blood supply in Nigeria.
CONCLUSION
A significant number of the paid donor population in Benin are anemic (predominantly hypochromic microcytic anemia) and are capable of endangering their lives if they continue in the practice of blood donation without regard to their baseline hemoglobin. There is a need to strictly regulate blood donation practices locally and the activities of donor vendors should be supervised by appropriate agencies if this source of procurement would be allowed to continue. There is also a need to encourage nonremunerated voluntary blood donation practice.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.WHO. Harare: Africa Regional Office; 1998. Regional Blood Safety Initiative. A Regional plan for blood safe. [Google Scholar]
- 2.Marcela C, Clare PF, Taylor JA. 5th ed. Chichester Blackwell Pub; 2005. Clinical blood transfusion in postgraduate haematology; p. 250. Ch. 16. [Google Scholar]
- 3.Djalali M, Neyestani TR, Bateni J, Siassi F. The effect of repeated blood donations on the iron status of Iranian blood donors attending the Iranian blood transfusion organization. Int J Vitam Nutr Res. 2006;76:132–7. doi: 10.1024/0300-9831.76.3.132. [DOI] [PubMed] [Google Scholar]
- 4.Blood safety and donation: Fact sheet No. 279, 2008 June. [Last accessed on 2012 May 16]. Available from: http://www.who.int/mediacentre/factsheets/fs279/en/
- 5.Ahmed SG, Hassan AW, Obi SO. The pattern of blood donations in North East Nigeria. Nig J Surg Res. 1999;1:76–81. [Google Scholar]
- 6.Bashawri LA. Pattern of blood procurement, ordering and utilization in a University Hospital in Eastern Saudi Arabia. Saudi Med J. 2002;23:555–61. [PubMed] [Google Scholar]
- 7.Ahmed SG, Umar BA, Ibrahim UA, Saidu AT, Jolayemi B. Dynamics of blood donation and donor categories in Birnin Kudu, Nigeria. Nig J Basic Clin Sci. 2004;1:66–70. [Google Scholar]
- 8.Ahmed SG, Hassan AW. Viral Infectivity Markers in Donor blood- A Retrospective Study of Three Donor Categories. Nig J Surg Res. 2000;2:75–80. [Google Scholar]
- 9.Ahmed SG. Laboratory strategic defence initiative against transfusion of human immune deficiency virus in blood and blood products. Nig Postgrad Med J. 2003;10:254–9. [PubMed] [Google Scholar]
- 10.Mittal R, Marwaha N, Basu S, Mohan H, Ravi Kumar A. Evaluation of iron stores in blood donors by serum ferritin. Indian J Med Res. 2006;124:641–6. [PubMed] [Google Scholar]
- 11.Jeremiah ZA, Koate BB. Anaemia, iron deficiency and iron deficiency anaemia among blood donors in Port Harcourt, Nigeria. Blood Transfus. 2010;8:113–7. doi: 10.2450/2009.0113-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jeremiah ZA, Koate BB. Reference percentiles of haematological and biochemical iron values of blood donors in Port Harcourt, Nigeria. Hematology. 2009;14:366–70. doi: 10.1179/102453309X12473408860622. [DOI] [PubMed] [Google Scholar]
- 13.De Maeyer E, Adiels-Tegman M. The prevalence of anaemia in the world. World Health Stat Q. 1985;38:302–16. [PubMed] [Google Scholar]
- 14.Adediran IA, Fesogun RB, Oyekunle AA. Haematological parameters in prospective Nigerian blood donors rejected on account of anaemia and/or microfilaria infestation. Nig J Med. 2005;14:45–50. doi: 10.4314/njm.v14i1.37134. [DOI] [PubMed] [Google Scholar]
- 15.Tayou Tagny C, Monny Lobe M, Mbanya D. Evaluation of two methods for haemoglobin measurement in Cameroonian blood donors. Transfus Clin Biol. 2006;13:331–4. doi: 10.1016/j.tracli.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 16.Rajab JA, Muchina WP, Orinda DA, Scott CS. Blood donor haematology parameters in two regions of Kenya. East Afr Med J. 2005;82:123–7. doi: 10.4314/eamj.v82i3.9268. [DOI] [PubMed] [Google Scholar]
- 17.Erhabor O, Ok O, Awah I, Uko KE, Charles AT. The prevalence of Plasmodium parasitaemia among donors in the Niger delta of Nigeria. Trop Doct. 2007;37:32–4. doi: 10.1258/004947507779951998. [DOI] [PubMed] [Google Scholar]
- 18.Gomez-Simon A, Navarro-Nuwez L, Perez-Ceballos E, Lozano ML, Candela MJ, Cascales A, et al. Evaluation of four rapid methods for haemoglobin screening of whole blood donors in mobile collection settings. Transfus Apher Sci. 2007;36:235–42. doi: 10.1016/j.transci.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 19.Adetifa IM, Hill PC, Jeffries DJ, Jackson-Sillah D, Ibanga HB, Bah G, et al. “Haematological values from a Gambian cohort-possible reference range for a West African population”. Int J Lab Hematol. 2009;31:615–22. doi: 10.1111/j.1751-553X.2008.01087.x. [DOI] [PubMed] [Google Scholar]
- 20.Saathoff E, Schneider P, Kleinfeldt V, Geis S, Haule D, Maboko L, et al. “Laboratory reference values for healthy adults from southern Tanzania”. Trop Med Intern Health. 2008;13:612–25. doi: 10.1111/j.1365-3156.2008.02047.x. [DOI] [PubMed] [Google Scholar]


