Abstract
Purpose
The first purpose of this study was to determine the incidence of postoperative nausea and/or vomiting (PONV) 0–48 h after anesthesia at a Japanese cancer center. The second purpose of this study was to collect information on PONV risk factors, independently, in the categories of patient-related, anesthesia-related, and surgery-related factors.
Methods
The frequency of nausea and vomiting was prospectively investigated from 0 to 48 h after anesthesia in 1645 patients (11–94 years of age) at a single medical institution. The occurrence of nausea and vomiting and the use of antiemetics were recorded up to 48 h after anesthesia. Patient-related, anesthesia-related, and surgery-related factors were also recorded and submitted to multiple logistic regression analysis to determine the relationship of these factors to nausea and vomiting.
Results
The incidences of nausea and vomiting from 0 to 24 h after anesthesia were 40 and 22 %, respectively. The incidences 24–48 h after anesthesia were 10 and 3 %, respectively. Female sex, previous history of PONV, prolonged anesthesia, and remifentanil use during surgery were identified as risk factors for both nausea and vomiting. The use of a volatile anesthetic, use of fentanyl during surgery, postoperative use of opioids, nonsmoking status, and drinking alcohol on 4 or fewer days per week were identified as risk factors for nausea alone.
Conclusion
The incidence of and risk factors for PONV at a Japanese cancer center according to this study are comparable to those reported elsewhere.
Keywords: Postoperative nausea and vomiting, PONV, Prospective study, Risk factors, Japan
Introduction
Postoperative nausea and/or vomiting (PONV) is a significant postoperative complication that has been repeatedly investigated in surveys of incidence [1–4]. Many studies have sought to determine risk factors for PONV [1, 3, 5, 6]. Numerous antiemetics have been developed [7–11] and are used for PONV as recommended in various guidelines [12–14]. However, antiemetics such as 5-HT3 receptor antagonists, dexamethasone, and neurokinin-1 (NK1) receptor antagonists are still unapproved for use in Japan. This leaves metoclopramide as the only therapeutic option and deprives Japanese physicians of effective therapies for PONV. The unavailability of new antiemetics is partially attributable to a lack of large-scale studies to investigate the incidence of PONV in this country. Conclusive evidence that PONV is a significant concern in Japan with an incidence essentially no different from that in other countries would substantiate the approval of the new antiemetics, a class of agents widely used elsewhere, for use in Japan.
The first purpose of this study was to determine the incidence of PONV 0–48 h after anesthesia at a Japanese cancer center. The second purpose of this study was to collect information on PONV risk factors, independently, in the categories of patient-related, anesthesia-related, and surgery-related factors.
Subjects, materials, and methods
This study was designed as a prospective cohort study to analyze the incidence of PONV and risk factors for PONV. Following internal ethics committee approval, the study was conducted at a single center from June 15 to September 30, 2010.
Subjects
The subjects of the study were patients with an American Society of Anesthesiologists physical status (ASA PS) of I to III who underwent elective surgery with general or local anesthesia. The following patients were excluded: pregnant women, patients requiring intensive care unit treatment, patients receiving or scheduled to receive a mild or greater emetogenic anticancer drug from 6 days before study entry to 48 h after anesthesia, patients with a symptomatic brain metastasis, patients unable to communicate for a mental reason, and patients for whom any of the following antiemetics were used 48 or fewer hours before the start of anesthesia or during anesthesia: a 5-HT3 receptor antagonist, dexamethasone, phenothiazine drug product, butyrophenone drug product, benzamide drug product, dopamine receptor antagonist, antihistamine, or a NK1 receptor antagonist. Patients for whom none of the exclusion criteria applied and who provided informed consent in writing were included in the study.
Anesthesia and postoperatively used drugs
No preanesthetic premedication drug was administered. Propofol was administered to induce anesthesia; rocuronium or vecuronium was administered as a muscle relaxant; remifentanil, fentanyl, or morphine hydrochloride was administered as an opioid; sevoflurane, propofol, or nitrous oxide was administered for maintenance of anesthesia; and sugammadex sodium or neostigmine was administered to reverse the muscle relaxants. The attending anesthesiologist selected the particular drugs as normal. The prophylactic administration of antiemetics was not allowed except for postoperative rescue. Metoclopramide, which is approved in Japan for PONV, was used as the antiemetic.
Collecting patient data
The attending anesthesiologist recorded patient characteristics on the day before surgery. During anesthesia, the anesthesiologist recorded the disease name, surgery type, anesthesia used, type and dose of any anesthesia-related drugs used, and duration of anesthesia. Following anesthesia, a ward nurse recorded the antiemetic used.
Evaluating nausea and vomiting
We determined that evaluating PONV until 48 h after anesthesia could provide data that would be useful in the future, because NK1 receptor antagonists, the 5-HT3 receptor antagonist palonosetron, and other long-acting drugs have recently been used for treating PONV. PONV was therefore evaluated from 0 to 2, 2 to 24, and 24 to 48 h after anesthesia. PONV was evaluated by an anesthesiologist in the operating room and a nurse in the wards. The evaluator recorded whether nausea was present, and if so, the severity and the number of vomiting or retching episodes. Nausea was defined as a subjective sensation of the desire to vomit by the patient without actual movement of the expelling muscles.
Statistical analysis
The frequencies and percentages of the patient characteristics were calculated in each category, as follows. The median age and age range (minimum–maximum) were calculated along with the mean body weight and standard deviation. The mean opioid dose was calculated along with the standard deviation. For the duration of anesthesia, the lower quartile, median, and upper quartile were calculated. Next, the frequencies and percentages of subjects with nausea, vomiting, and PONV were calculated individually for each surgery type and risk factor at 0–2 h, 2–24 h, 24–48 h, 0–24 h overall, and 0–48 h overall after anesthesia. Logistic univariate regression analysis 0–2 h, 2–24 h, 24–48 h, 0–24 h overall, and 0–48 h overall after anesthesia was conducted to investigate the relationship of the risk factors to nausea, vomiting, and PONV frequency. The regression coefficients, standard errors, odds ratios (ORs), and 95 % confidence intervals (CIs) were calculated along with Wald P values. To avoid the problems of multicollinearity between individual risk factors, the significance of correlations was tested using Spearman’s correlation coefficient, and r values of ≥0.6 were defined as the presence of association. The 13 factors that had no multicollinearity issues and that were considered relevant to PONV were selected from the factors that univariate analysis suggested as being related and were submitted to logistic multivariate regression analysis by the forced-entry method. Adjusted ORs, 95 % CIs, and Wald P values were calculated. Seven of these 13 factors (sex, history of PONV, nonsmoking status, volatile anesthesia vs. total intravenous anesthesia [TIVA], nitrous oxide, reversal of muscle relaxation, and postoperative opioids) were dichotomous. Because the 13 factors did not include local anesthesia, multivariate analysis was performed after excluding the cases of local anesthesia. Remifentanil and fentanyl doses were analyzed as continuous variables, with adjusted ORs calculated every 1000 μg for remifentanil and every 100 μg for fentanyl. The category variables for the remaining 4 factors were as follows. For body mass index (BMI), ≥25 kg/m2 and <25 kg/m2, for duration of anesthesia, >1 h and ≤1 h, for alcohol drinking, on ≤4 days per week and >4 days per week, and for age, ≥50 years and <50 years. In all analyses a P value of less than 0.05 constituted statistical significance. SAS 9.2 (SAS Institute, Cary, NC, USA) was used to perform the statistical analyses.
Results
All 1645 patients undergoing surgery who did not satisfy any of the exclusion criteria were included in the study. The breakdowns for the surgery types were as follows: gynecological surgery (GYN) 273 (17 %), breast surgery 399 (24 %), orthopedic surgery (ORT) 136 (8 %), respiratory surgery (RES) 100 (6 %), abdominal surgery (ABD) 599 (36 %), and otological surgery (OTO) 138 (8 %).
Patient baseline characteristics are shown in (Table 1). A total of 1608 patients (98 %) underwent general anesthesia, and 37 patients (2 %) underwent spinal anesthesia. The duration of anesthesia was 204 min (131–290 min) [median (quartile 1–quartile 3)]. Anesthesia type, drugs used, and postoperative analgesia are presented in detail in Table 2. The median fentanyl dose was 150 μg and the median remifentanil dose was 1500 μg. As postoperative analgesia, an epidural local anesthetic was used in 137 patients (8 %), an epidural opioid was used in 604 patients (37 %), fentanyl intravenous patient-controlled analgesia (IVPCA) was used in 83 patients (5 %), a nonsteroidal anti-inflammatory drug (NSAID) was used in 485 patients (29 %), and additional intravenous opioids (pentazocine or morphine) were used in 125 patients (8 %).
Table 1.
Patient characteristics
| Characteristic | |
|---|---|
| Sex | |
| Female n (%) | 1051 (63.9) |
| Male n (%) | 594 (36.1) |
| Age (years) median (range) | 59 (11–94) |
| −29 n (%) | 71 (4.3) |
| 30–39 n (%) | 154 (9.4) |
| 40–49 n (%) | 320 (19.5) |
| 50–59 n (%) | 303 (18.4) |
| 60–69 n (%) | 450 (27.4) |
| 70– n (%) | 347 (21.1) |
| Weight (kg) mean (SD) | 57.4 (11.0) |
| BMI (kg/m2) mean (SD) | 22.3 (3.4) |
| Nonsmoking status n (%) | 1438 (87.4) |
| Drinking (on ≤4 days per week) | 1265 (76.9) |
| History of PONV n (%) | 135 (8.2) |
| History of motion sickness n (%) | 454 (27.6) |
| ASA PS | |
| I n (%) | 752 (45.7) |
| II n (%) | 881 (53.6) |
| III n (%) | 12 (0.7) |
ASA PS American Society of Anesthesiologists physical status, BMI body mass index, PONV postoperative nausea and/or vomiting
Table 2.
Perioperative drugs
| Drug | n (%) | Median ± SD |
|---|---|---|
| General anesthesia (n = 1608) | ||
| Induction | ||
| Propofol | 1608 (100) | |
| Anesthetic maintenance and reversal | ||
| TIVA (propofol) | 294 (18.3) | |
| Volatile anesthetic | 1314 (81.7) | |
| With nitrous oxide | 212 (13.2) | |
| Without nitrous oxide | 1102 (68.5) | |
| With epidural anesthesia | 743 (46.2) | |
| Muscle relaxant use | 1563 (97.2) | |
| Muscle relaxants reversal use | 1128 (70.1) | |
| Neostigmine | 172 (15.2) | |
| Sugammadex | 956 (84.8) | |
| Fentanyl (μg) | 1482 (90.1) | 150.0 ± 166.8 |
| Remifentanil (μg) | 1241 (75.4) | 1500.0 ± 1867.1 |
| Morphine (mg) | 12 (0.73) | 3.0 ± 2.2 |
| 48-h Postoperative analgesics | ||
| Epidural local anesthetic | 137 (8.3) | |
| Opioidsa | 709 (43.1) | |
| NSAIDs | 485 (29.5) | |
TIVA total intravenous anesthesia, NSAIDs nonsteroidal anti-inflammatory drugs
aOpioids include epidural opioids, fentanyl intravenous patient-controlled analgesia, and additional intravenous opioids (morphine, pentazocine)
The incidences of nausea, vomiting, and PONV and the usage of antiemetics are shown in Table 3 according to sex, type of anesthesia, and the type of surgery. The incidences of nausea and vomiting from 0 to 24 h after anesthesia were 40 and 22 %, respectively. Twenty-four percent of the patients used an antiemetic. The incidences of nausea and vomiting from 24 to 48 h after anesthesia were 10 and 3 %, respectively. The incidences of nausea and vomiting over the entire period studied were higher in the female patients. The incidences of nausea and vomiting after local anesthesia tended to be lower than those after general anesthesia, although there were far fewer cases of local anesthesia as compared with general anesthesia. The incidence of PONV from 0 to 48 h after anesthesia was 52 % for GYN, 53 % for BRE, and 46 % for OTO. These figures were higher than the 32 % for ORT, 30 % for RES, and 35 % for ABD. The incidence of PONV from 24 to 48 h after anesthesia was 19 % for GYN, 13 % for RES, and 12 % for ABD, values which were higher than the 3.3 % for BRE, 5.9 % for ORT, and 3.5 % for OTO.
Table 3.
Frequencies of PONV and antiemetic administration in the various periods
| Outcome | Sex | Type of anesthesia | Type of surgery | Total (n = 1645) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male (n = 594) | Female (n = 1051) | GA (n = 1608) | RA (n = 37) | GYN (n = 273) | BRE (n = 399) | ORT (n = 136) | OTO (n = 138) | RES (n = 100) | ABD (n = 599) | ||
| 0–2 h | |||||||||||
| Nausea | 10.6 | 30.1 | 23.5 | 8.1 | 32.6 | 29.1 | 14.0 | 26.2 | 12.0 | 17.7 | 23.0 |
| Vomiting | 4.4 | 12.2 | 9.6 | 0.0 | 11.7 | 10.8 | 5.1 | 14.2 | 3.0 | 8.2 | 9.4 |
| PONV | 10.6 | 30.3 | 23.7 | 8.1 | 32.6 | 29.1 | 14.0 | 27.0 | 12.0 | 17.9 | 23.2 |
| Antiemetics | 4.5 | 15.7 | 12.0 | 0.0 | 19.4 | 14.5 | 5.1 | 17.0 | 1.0 | 8.2 | 11.7 |
| 2–24 h | |||||||||||
| Nausea | 16.7 | 40.1 | 32.4 | 5.4 | 35.5 | 42.1 | 25.0 | 31.9 | 24.0 | 25.4 | 31.6 |
| Vomiting | 8.4 | 21.8 | 17.3 | 5.4 | 15.8 | 23.3 | 12.5 | 18.4 | 15.0 | 14.2 | 17.0 |
| PONV | 16.7 | 40.2 | 32.5 | 5.4 | 35.5 | 42.1 | 25.0 | 31.9 | 24.0 | 25.7 | 31.7 |
| Antiemetics | 5.4 | 22.6 | 16.8 | 2.7 | 20.1 | 24.6 | 11.8 | 17.7 | 8.0 | 11.4 | 16.4 |
| 24–48 h | |||||||||||
| Nausea | 6.1 | 11.8 | 9.9 | 2.7 | 18.7 | 3.3 | 5.9 | 3.5 | 13.0 | 11.7 | 9.7 |
| Vomiting | 1.5 | 3.5 | 2.8 | 2.7 | 6.6 | 0.8 | 0.7 | 1.4 | 3.0 | 3.2 | 2.8 |
| PONV | 6.1 | 12.1 | 10.1 | 2.7 | 19.4 | 3.3 | 5.9 | 3.5 | 13.0 | 11.9 | 9.9 |
| Antiemetics | 2.2 | 5.7 | 4.6 | 0.0 | 8.8 | 0.8 | 3.7 | 2.8 | 3.0 | 5.7 | 4.4 |
| 0–24 overall | |||||||||||
| Nausea | 21.7 | 51.0 | 41.4 | 10.8 | 48.4 | 52.9 | 31.6 | 45.4 | 28.0 | 31.2 | 40.4 |
| Vomiting | 10.9 | 28.4 | 22.6 | 5.4 | 23.1 | 28.3 | 16.9 | 26.2 | 19.0 | 18.0 | 22.1 |
| PONV | 21.7 | 51.3 | 41.6 | 10.8 | 48.4 | 52.9 | 31.6 | 45.4 | 28.0 | 31.7 | 40.6 |
| Antiemetics | 9.3 | 32.0 | 24.4 | 2.7 | 31.9 | 33.8 | 16.9 | 28.4 | 8.0 | 16.4 | 23.8 |
| 0–48 overall | |||||||||||
| Nausea | 24.1 | 52.6 | 43.3 | 10.8 | 52.0 | 52.9 | 31.6 | 46.1 | 30.0 | 34.2 | 42.3 |
| Vomiting | 11.6 | 29.1 | 23.3 | 5.4 | 24.2 | 28.6 | 16.9 | 27.0 | 20.0 | 19.0 | 22.8 |
| PONV | 24.1 | 53.0 | 43.6 | 10.8 | 52.4 | 52.9 | 31.6 | 46.1 | 30.0 | 34.7 | 42.6 |
| Antiemetics | 10.6 | 33.5 | 25.9 | 2.7 | 34.4 | 34.1 | 19.1 | 29.1 | 10.0 | 18.0 | 25.2 |
GA general anesthesia, RA regional anesthesia, GYN gynecological surgery, BRE breast surgery, ORT orthopedic surgery, RES respiratory surgery, ABD abdominal surgery, OTO otological surgery, PONV postoperative nausea and/or vomiting
The adjusted ORs and CIs of the risk factors for nausea and vomiting 0–48 h after anesthesia are shown in Table 4. Patient-related risk factors for both nausea and vomiting were female sex and history of PONV. Female sex was a particularly strong risk factor, with adjusted ORs (CIs) of 4.1 (3.00–5.62) and 3.65 (2.52–5.30), respectively. Nonsmoking status and drinking alcohol on 4 or fewer days per week were identified as risk factors for nausea alone. Anesthesia-related risk factors for both nausea and vomiting were duration of anesthesia exceeding 1 h and the intraoperative use of remifentanil. The use of a volatile anesthetic (versus propofol), the intraoperative use of fentanyl, and the postoperative use of opioids were identified as risk factors for nausea alone. The results did not show age, BMI, nitrous oxide use, or muscle relaxant antagonists to be correlated with nausea or vomiting.
Table 4.
Adjusted odds ratios of risk factors for nausea and vomiting within the 0–48 h overall period
| Factor | Odds ratio | 95 % CI | P value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Nausea (0–48 h) | ||||
| Sex (female) | 4.10 | 3.00 | 5.62 | <0.0001 |
| Age (≥50 years) | 0.87 | 0.65 | 1.16 | 0.3407 |
| History of PONV | 2.04 | 1.29 | 3.23 | 0.0022 |
| Nonsmoking status | 1.56 | 1.05 | 2.33 | 0.0256 |
| BMI (kg/m2) (≥25) | 1.08 | 0.79 | 1.48 | 0.6394 |
| Drinking (on ≤4 days per week) | 1.39 | 1.02 | 1.92 | 0.0374 |
| Duration of anesthesia (>1 h) | 2.97 | 1.87 | 4.71 | <0.0001 |
| Volatile anesthesia vs. TIVA | 1.61 | 1.14 | 2.22 | 0.0066 |
| Nitrous oxide | 1.19 | 0.74 | 1.92 | 0.4641 |
| Remifentanil (per 1000 μg) | 1.23 | 1.11 | 1.36 | <0.0001 |
| Fentanyl (per 100 μg) | 1.17 | 1.04 | 1.33 | 0.0103 |
| Reversal of muscle relaxation | 1.29 | 0.97 | 1.73 | 0.0849 |
| Postoperative opioids | 1.38 | 1.03 | 1.83 | 0.0284 |
| Vomiting (0–48 h) | ||||
| Sex (female) | 3.65 | 2.52 | 5.30 | <0.0001 |
| Age (≥50 years) | 1.48 | 1.06 | 2.06 | 0.0214 |
| History of PONV | 1.87 | 1.20 | 2.91 | 0.0056 |
| Nonsmoking status | 1.27 | 0.79 | 2.00 | 0.3177 |
| BMI (kg/m2) (≥25) | 0.81 | 0.57 | 1.16 | 0.2531 |
| Drinking (on ≤4 days per week) | 1.39 | 0.95 | 2.04 | 0.0905 |
| Duration of anesthesia (>1 h) | 1.77 | 1.02 | 3.06 | 0.0426 |
| Volatile anesthesia vs. TIVA | 1.16 | 0.81 | 1.69 | 0.4180 |
| Nitrous oxide | 1.02 | 0.59 | 1.75 | 0.9400 |
| Remifentanil (per 1000 μg) | 1.28 | 1.16 | 1.41 | <0.0001 |
| Fentanyl (per 100 μg) | 1.09 | 0.96 | 1.23 | 0.1917 |
| Reversal of muscle relaxation | 1.25 | 0.89 | 1.74 | 0.1921 |
| Postoperative opioids | 1.21 | 0.89 | 1.65 | 0.2286 |
CI confidence interval, PONV postoperative nausea and/or vomiting, BMI body mass index, TIVA total intravenous anesthesia
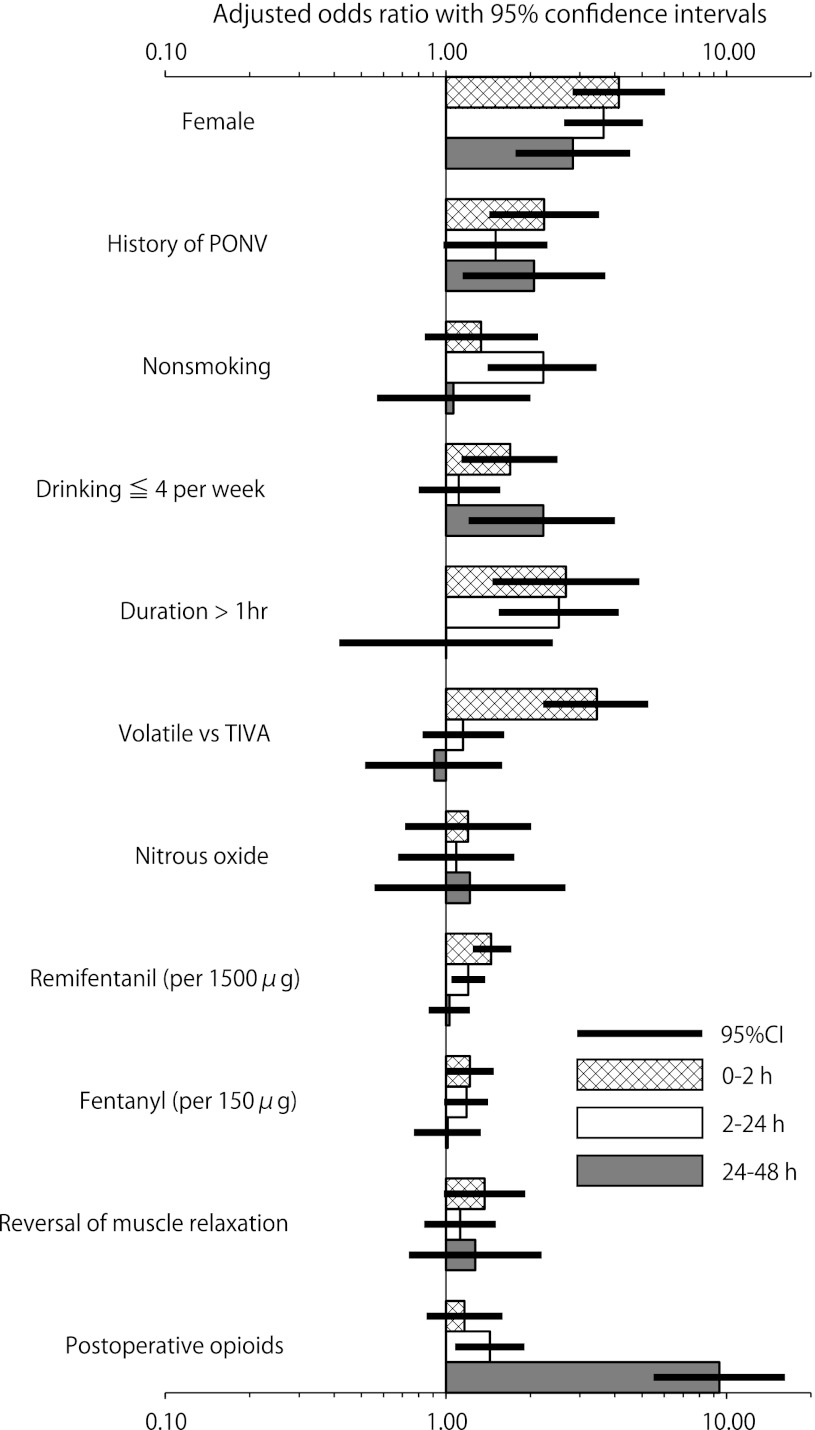
The strengths of the PONV risk factors at 0–2 h, 2–24 h, and 24–48 h after anesthesia are shown in Fig. 1. The use of a volatile anesthesic was highly significant, with an adjusted OR (CI) of 3.45 (2.22–5.26) from 0 to 2 h after anesthesia, but this factor was unrelated to PONV 2–24 h and 24–48 h after anesthesia (P = 0.40, P = 0.73). The use of remifentanil (in 1500 μg increments) was significant, with an adjusted OR (CI) of 1.65 (1.34–2.03) 0–2 h after anesthesia, but its significance decreased to an adjusted OR (CI) of 1.27 (1.06–1.53) 2–24 h after anesthesia and it was insignificant 24–48 h after anesthesia (P = 0.79). The use of fentanyl (in 150 μg increments) was significant, with adjusted ORs (CIs) of 1.28 (1.00–1.63) 0–2 h after anesthesia and 1.23 (0.99–1.54) 2–24 h after anesthesia, but it was insignificant 24–48 h after anesthesia (P = 0.93). The postoperative use of opioids was insignificant 0–2 h after anesthesia (P = 0.33), but was highly significant, with adjusted ORs (CIs) of 1.43 (1.08–1.90) 2–24 h after anesthesia and 9.42 (5.50–16.16) 24–48 h after anesthesia. The effects of female sex and history of PONV, which were risk factors for both nausea and vomiting, were consistent across the time periods studied.
Fig. 1.
Strengths of PONV risk factors at 0–2, 2–24, and 24–48 h after anesthesia. Note that the x axis is log-scale. PONV postoperative nausea and/or vomiting, CI confidence interval, drinking ≤4 per week drinking on ≤4 days per week, duration duration of anesthesia, volatile volatile anesthetic, TIVA total intravenous anesthesia
Discussion
This large-scale study, which was conducted to identify PONV incidence and risk factors, is the first such study to demonstrate the high incidence of PONV in Japan. The study also showed delayed incidencesm from 24 to 48 h after anesthesiam to be relatively high, at 10 % for nausea and 3 % for vomiting.
When interpreting the incidences of PONV in the present study, it must be remembered that the median duration of anesthesia was 204 min, which was longer than that in other studies [1–4]. Furthermore, comparing incidences of PONV among studies may not be feasible because of the difficulty involved with matching patient-, anesthesia-, and surgery-related factors. We believe that another study of PONV incidences in Japan, with matched risk factors is necessary.
PONV incidence is known to be high for certain types of surgeries [2, 15, 16]. The present study showed a high incidence of PONV for GYN, BRE, and OTO. It should be noted that most or all of the patients undergoing these types of surgeries were female. Some investigators claim that the relationship between surgery type and PONV is open to interpretation because patient characteristics and anesthesia-related factors are at play [1, 5, 17, 18]; accordingly, the effect of surgery type was excluded from multivariate regression analysis in the present study.
In the present study, female sex and a history of PONV were identified as risk factors for both nausea and vomiting. Female sex and a history of PONV have previously been identified as important PONV risk factors [2–4, 18]. We also showed that nonsmoking status and drinking alcohol on 4 or fewer days per week were risk factors for nausea alone. Nonsmoking status has previously been shown to increase PONV incidence [19, 20]. Sweeney [20] states that higher levels of drinking may suppress PONV. Our findings validate this prediction.
ASA PS and BMI are reported to affect PONV [2, 3, 21], but these factors were not found to be related to PONV in our study.
Longer durations of anesthesia and the use of volatile anesthetics have been previously reported as risk factors for PONV [22, 23]. The present study showed the risk of PONV to increase with increasing opioid doses during surgery; increasing the remifentanil dose by 1000 μg increased the adjusted OR for nausea by 1.23-fold, while increasing the fentanyl dose by 100 μg increased the OR by 1.17-fold within the 0–48 h overall period. Postoperative opioid use is believed to increase PONV in a dose-dependent manner [24] and was shown in our study to be a risk factor for nausea. The use of nitrous oxide is also thought to be a risk factor for PONV [25–27], but this factor did not have an impact in our study.
The use of 2.5 mg or more neostigmine is a reported risk factor for PONV [28], but our study revealed no relationship between muscle relaxant antagonist use and PONV, possibly because sugammadex was frequently used but neostigmine was not. Although further research is required, because previous univariate analysis of the effects of sugammadex on PONV showed no relationship, it seems that sugammadex may not affect PONV.
Apfel et al. [22] state that volatile anesthetics are a strong risk factor for PONV for up to 2 h after surgery. Stadler et al. [4] disagree with this conclusion, attributing it to the inclusion of a high proportion of children and imbalances in surgery types. Although the present study had a higher proportion of female patients (64 vs. 53 %) than the study of Stadler et al. [4], the proportion of child patients was comparable to the proportion in their study, and our study had no surgery type imbalances such as those in the study of Apfel et al. [22]. We found that the use of volatile anesthetics was a risk factor for nausea, with an adjusted OR of 3.45, only 0–2 h after anesthesia. This strengthens the claim of Apfel et al. [22] and indicates that the impact of volatile anesthetics is very substantial during the early period 0–2 h after anesthesia.
With regard to perioperatively used opioids, our study evaluated the intensity of the effects of not only according to dose but also according to time after anesthesia. Postoperative opioid use, which produces PONV 2 h after anesthesia and beyond, has been shown to be a significant factor for delayed PONV 24 h and beyond. In the present study, the incidence of PONV was relatively high for GYN, RES, and ABD 24–48 h after anesthesia; postoperative epidural opioids and fentanyl IVPCA were used more frequently after these types of surgery than the others. We found that intraoperative remifentanil use had a large impact on PONV 0–2 h after anesthesia. The effects of its use were diminished 2–24 h after anesthesia and were not observed 24 h after anesthesia and beyond. Intraoperative fentanyl use had a comparable impact 0–24 h after anesthesia, but no effects were noted 24 h after anesthesia and beyond. Although our study did not closely compare the significance of the effects of remifentanil and fentanyl by excluding other factors, as in the study by Rama-Maceiras et al. [29], the adjusted ORs show that the times of impact and intensities of PONV differed according to the particular opioid used.
Problematically, the hospital stay of ambulatory surgery patients may be prolonged by PONV attributable to opioid use [13–15]. The findings of the present study suggest that reducing opioid dosage and, particularly, reducing intraoperative fentanyl and postoperative opioid use could be effective for preventing prolonged hospital stays and delayed PONV.
In overall consideration of the results and given the difficulty of controlling patient-related factors in the clinic, controlling anesthesia-related factors appears to be an effective way of reducing the incidence of PONV. It is important to avoid using volatile anesthetics, which are a strong risk factor for nausea during the 2-h period following anesthesia, and to also reduce the use of opioids, which are a risk factor for delayed PONV. However, reducing opioid use has been shown to lead to an increase in anesthetic use [30, 31]; so, using propofol, whose dose Apfel et al. [22] claim is not proportional to PONV, and using local anesthesia and NSAIDs as proposed by Shirakami et al. [32] appear to be viable options for reducing opioid use as much as possible.
No large-scale studies of PONV incidence to support the use of new antiemetics and no evaluations of the efficacy of antiemetics used per consensus guidelines for PONV have been conducted at any Japanese Cancer Center or at any other institution in Japan. Further investigation will be required to determine how PONV incidence, as defined in the present research, can be decreased through prophylaxis with antiemetics. A risk score must be constructed on the basis of the data obtained by this study and evaluated for effectiveness.
Acknowledgments
We express our sincere gratitude to Tetsutaro Hamano of the Hamano Statistical Analysis Center for conducting the statistical analyses and we thank all the kind anesthesiologists and nurses at the Cancer Institute Hospital of the Japanese Foundation for Cancer Research for collecting the study data.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Footnotes
Data from this study were presented in part at The 59th Annual Meeting of the Japanese Society of Anesthesiologists, 2012, Kobe.
References
- 1.Apfel CC, Laara E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology. 1999;91:693–700. doi: 10.1097/00000542-199909000-00022. [DOI] [PubMed] [Google Scholar]
- 2.Cohen MM, Duncan PG, DeBoer DP, Tweed WA. The postoperative interview: assessing risk factors vomiting. Anesth Analg. 1994;78:7–16. doi: 10.1213/00000539-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Koivuranta M, Laara E, Snare L, Alahuhta S. A survey of postoperative nausea and vomiting. Anaesthesia. 1997;52:443–449. doi: 10.1111/j.1365-2044.1997.117-az0113.x. [DOI] [PubMed] [Google Scholar]
- 4.Stadler M, Bardiau F, Seidel L, Albert A, Boogaerts JG. Difference in risk factors for postoperative nausea and vomiting. Anesthesiology. 2003;98:46–52. doi: 10.1097/00000542-200301000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Apfel CC, Roewer N. Risk assessment of postoperative nausea and vomiting. Int Anesthesiol Clin. 2003;41:13–32. doi: 10.1097/00004311-200341040-00004. [DOI] [PubMed] [Google Scholar]
- 6.Gan TJ. Risk factors for postoperative nausea and vomiting. Anesth Analg. 2006;102:1884–1898. doi: 10.1213/01.ANE.0000219597.16143.4D. [DOI] [PubMed] [Google Scholar]
- 7.Diemunsch P, Joshi GP, Brichant JF. Neurokinin-1 receptor antagonists in the prevention of postoperative nausea and vomiting. Br J Anaesth. 2009;103:7–13. doi: 10.1093/bja/aep125. [DOI] [PubMed] [Google Scholar]
- 8.Gan TJ, Apfel CC, Kovac A, Philip BK, Singla N, Minkowitz H, Habib AS, Knighton J, Carides AD, Zhang H, Horgan KJ, Evans JK, Lawson FC. A randomized, double-blind comparison of the NK1 antagonist, aprepitant, versus ondansetron for the prevention of postoperative nausea and vomiting. Anesth Analg. 2007;104:1082–1089. doi: 10.1213/01.ane.0000263277.35140.a3. [DOI] [PubMed] [Google Scholar]
- 9.Gray H. Aprepitant for postoperative nausea and vomiting. Anaesth Intensive Care. 2009;37:135–136. [PubMed] [Google Scholar]
- 10.Henzi I, Walder B, Tramer MR. Dexamethasone for the prevention of postoperative nausea and vomiting: a quantitative systematic review. Anesth Analg. 2000;90:186–194. doi: 10.1097/00000539-200001000-00038. [DOI] [PubMed] [Google Scholar]
- 11.Polati E, Verlato G, Finco G, Mosaner W, Grosso S, Gottin L, Pinaroli AM, Ischia S. Ondansetron versus metoclopramide in the treatment of postoperative nausea and vomiting. Anesth Analg. 1997;85:395–399. doi: 10.1097/00000539-199708000-00027. [DOI] [PubMed] [Google Scholar]
- 12.Gan TJ, Meyer T, Apfel CC, Chung F, Davis PJ, Eubanks S, Kovac A, Philip BK, Sessler DI, Temo J, Tramer MR, Watcha M. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg. 2003;97:62–71. doi: 10.1213/01.ANE.0000068580.00245.95. [DOI] [PubMed] [Google Scholar]
- 13.Gan TJ, Meyer TA, Apfel CC, Chung F, Davis PJ, Habib AS, Hooper VD, Kovac AL, Kranke P, Myles P, Philip BK, Samsa G, Sessler DI, Temo J, Tramer MR, Vander Kolk C, Watcha M. Society for Ambulatory Anesthesia guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2007;105:1615–1628. doi: 10.1213/01.ane.0000295230.55439.f4. [DOI] [PubMed] [Google Scholar]
- 14.McCracken G, Houston P, Lefebvre G. Guideline for the management of postoperative nausea and vomiting. J Obstet Gynaecol Can. 2008;30(600–7):8–16. doi: 10.1016/s1701-2163(16)32895-x. [DOI] [PubMed] [Google Scholar]
- 15.Gan TJ. Postoperative nausea and vomiting—can it be eliminated? JAMA. 2002;287:1233–1236. doi: 10.1001/jama.287.10.1233. [DOI] [PubMed] [Google Scholar]
- 16.Sonner JM, Hynson JM, Clark O, Katz JA. Nausea and vomiting following thyroid and parathyroid surgery. J Clin Anesth. 1997;9:398–402. doi: 10.1016/S0952-8180(97)00069-X. [DOI] [PubMed] [Google Scholar]
- 17.Apfel CC, Greim CA, Haubitz I, Goepfert C, Usadel J, Sefrin P, Roewer N. A risk score to predict the probability of postoperative vomiting in adults. Acta Anaesthesiol Scand. 1998;42:495–501. doi: 10.1111/j.1399-6576.1998.tb05157.x. [DOI] [PubMed] [Google Scholar]
- 18.Junger A, Hartmann B, Benson M, Schindler E, Dietrich G, Jost A, Beye-Basse A, Hempelmannn G. The use of an anesthesia information management system for prediction of antiemetic rescue treatment at the postanesthesia care unit. Anesth Analg. 2001;92:1203–1209. doi: 10.1097/00000539-200105000-00023. [DOI] [PubMed] [Google Scholar]
- 19.Chimbira W, Sweeney BP. The effect of smoking on postoperative nausea and vomiting. Anaesthesia. 2000;55:540–544. doi: 10.1046/j.1365-2044.2000.01474.x. [DOI] [PubMed] [Google Scholar]
- 20.Sweeney BP. Why does smoking protect against PONV? Br J Anaesth. 2002;89:810–813. doi: 10.1093/bja/aef269. [DOI] [PubMed] [Google Scholar]
- 21.Watcha MF, White PF. Postoperative nausea and vomiting. Its etiology, treatment, and prevention. Anesthesiology. 1992;77:162–184. doi: 10.1097/00000542-199207000-00023. [DOI] [PubMed] [Google Scholar]
- 22.Apfel CC, Kranke P, Katz MH, Goepfert C, Papenfuss T, Rauch S, Heineck R, Greim CA, Roewer N. Volatile anaesthetics may be the main cause of early but not delayed postoperative vomiting: a randomized controlled trial of factorial design. Br J Anaesth. 2002;88:659–668. doi: 10.1093/bja/88.5.659. [DOI] [PubMed] [Google Scholar]
- 23.Sinclair DR, Chung F, Mezei G. Can postoperative nausea and vomiting be predicted? Anesthesiology. 1999;91:109–118. doi: 10.1097/00000542-199907000-00018. [DOI] [PubMed] [Google Scholar]
- 24.Roberts GW, Bekker TB, Carlsen HH, Moffatt CH, Slattery PJ, McClure AF. Postoperative nausea and vomiting are strongly influenced by postoperative opioid use in a dose-related manner. Anesth Analg. 2005;101:1343–1348. doi: 10.1213/01.ANE.0000180204.64588.EC. [DOI] [PubMed] [Google Scholar]
- 25.Apfel CC, Korttila K, Abdalla M, Kerger H, Turan A, Vedder I, Zernak C, Danner K, Jokela R, Pocock SJ, Trenkler S, Kredel M, Biedler A, Sessler DI, Roewer N. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med. 2004;350:2441–2451. doi: 10.1056/NEJMoa032196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Divatia JV, Vaidya JS, Badwe RA, Hawaldar RW. Omission of nitrous oxide during anesthesia reduces the incidence of postoperative nausea and vomiting. A meta-analysis. Anesthesiology. 1996;85:1055–1062. doi: 10.1097/00000542-199611000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Leslie K, Myles PS, Chan MT, Paech MJ, Peyton P, Forbes A, McKenzie D. Risk factors for severe postoperative nausea and vomiting in a randomized trial of nitrous oxide-based vs nitrous oxide-free anaesthesia. Br J Anaesth. 2008;101:498–505. doi: 10.1093/bja/aen230. [DOI] [PubMed] [Google Scholar]
- 28.Tramer MR, Fuchs-Buder T. Omitting antagonism of neuromuscular block: effect on postoperative nausea and vomiting and risk of residual paralysis. A systematic review. Br J Anaesth. 1999;82:379–386. doi: 10.1093/bja/82.3.379. [DOI] [PubMed] [Google Scholar]
- 29.Rama-Maceiras P, Ferreira TA, Molins N, Sanduende Y, Bautista AP, Rey T. Less postoperative nausea and vomiting after propofol + remifentanil versus propofol + fentanyl anaesthesia during plastic surgery. Acta Anaesthesiol Scand. 2005;49:305–311. doi: 10.1111/j.1399-6576.2005.00650.x. [DOI] [PubMed] [Google Scholar]
- 30.Katoh T, Ikeda K. The effects of fentanyl on sevoflurane requirements for loss of consciousness and skin incision. Anesthesiology. 1998;88:18–24. doi: 10.1097/00000542-199801000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Katoh T, Kobayashi S, Suzuki A, Iwamoto T, Bito H, Ikeda K. The effect of fentanyl on sevoflurane requirements for somatic and sympathetic responses to surgical incision. Anesthesiology. 1999;90:398–405. doi: 10.1097/00000542-199902000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Shirakami G, Teratani Y, Segawa H, Matsuura S, Shichino T, Fukuda K. Omission of fentanyl during sevoflurane anesthesia decreases the incidences of postoperative nausea and vomiting and accelerates postanesthesia recovery in major breast cancer surgery. J Anesth. 2006;20:188–195. doi: 10.1007/s00540-006-0413-x. [DOI] [PubMed] [Google Scholar]