Abstract
To determine prevalence and factors associated with intimate partner violence (IPV) among pregnant women seeking antenatal care. This was a cross-sectional study conducted at Kisumu District Hospital, Kenya amongst randomly selected pregnant women. A structured questionnaire was used to collect data. Participants self-reported about their own IPV experience (lifetime, 12 months prior to and during index pregnancy) and associated risk factors. Data were analyzed using Epi-info. The mean age of the 300 participants was 23.7 years. One hundred and ten (37 %) of them experienced at least one form of IPV during pregnancy. Psychological violence was the most common (29 %), followed by sexual (12 %), and then physical (10 %). Women who experienced IPV during pregnancy were more likely to have witnessed maternal abuse in childhood (aOR 2.27, 95 % CI = 1.05–4.89), been in a polygamous union (aOR 2.48, 95 % CI = 1.06–5.8), been multiparous (aOR 1.94, 95 % CI = 1.01–3.32) or had a partner who drank alcohol (aOR 2.32, 95 % CI = 1.21–4.45). Having a partner who attained tertiary education was protective against IPV (aOR 0.37, 95 % CI = 0.16–0.83). We found no association between HIV status and IPV. IPV is common among women seeking antenatal care at Kisumu District Hospital. Health care providers should be alerted to the possibility of IPV during pregnancy in women who witnessed maternal abuse in childhood, are multiparous, polygamous, have a partner who drinks alcohol or has low level education. Screening for IPV, support and referral is urgently needed to help reduce the burden experienced by pregnant women and their unborn babies.
Keywords: Intimate partner violence, Pregnancy, Kenya
Introduction
Women are vulnerable to violence from many different sources, but the World Health Organization multi-country study on women’s health and domestic violence against women of 2005 concludes that most violence against women is perpetrated by an intimate partner [1]. Intimate partner violence (IPV), also called domestic violence, domestic abuse or spouse abuse can be defined as acts of physical aggression, sexual coercion, psychological/emotional abuse or controlling behaviors by a current or former partner or spouse [2] and is recognized as a worldwide problem with serious public health implications. IPV can lead directly to serious injury, disability or death. It can also lead indirectly to mental disorders, substance use, lack of fertility control and personal autonomy. IPV during pregnancy is particularly harmful as it is associated with detrimental outcomes to both the mother and her unborn baby. Women experiencing IPV during pregnancy have higher rates of miscarriage, more complications during pregnancy more sexually transmitted infections (including HIV), and higher prevalence of mental disorders (such as depression, anxiety, sleep disorders and eating disorders) compared to their non-abused peers [3–7].
Worldwide, studies have estimated that between 10 and 71 % of women suffer from IPV in their lifetime [1, 2, 8], and in Kenya, the 2008/2009 demographic health survey report estimated that almost half of the women in Kenya (47 %) suffer from IPV in their life time [9]. However; the prevalence of IPV during pregnancy in Kenya is unknown. Therefore, the following study was conducted to determine the prevalence of IPV among pregnant women seeking antenatal care at a district hospital in Kenya and to learn more about factors associated with IPV among these women.
Methods
Study Population
This study was conducted at Kisumu District Hospital in Nyanza Province, which has a bed capacity of 195, located in the third largest city in Kenya. The subjects in this cross-sectional study were expectant women seeking antenatal care. According to records at the hospital, approximately 600 women access antenatal care services monthly.
Sampling
Systematic random sampling was used to sample the kth mother after a random starting point. All pregnant women irrespective of the trimester and number of visits to the clinic were eligible for the study. In case one declined or was reselected again during a follow up visit, then the next patient in the queue was picked as a replacement. Assuming an IPV prevalence of 10 % [10] and using Cochran’s formula [11], absolute precision of 5 %, and a non response rate of 10 %, the minimum sample size was 152 women. However, the sample size was doubled (N = 300) to increase the precision of the study.
Data Collection and Assessments
Data was collected from 26 July to 29 of October 2010. Daily the clients were given a card with a number on reporting to the clinic on a first come first served basis. This number aided the systematic random sampling. An interviewer administered structured questionnaire was used. The questionnaire was translated into Dholuo, the local language, by two translators and was double checked. The instrument was refined after pre-testing in a different location. The questionnaire included variables related to social and demographic characteristics of the pregnant women and their intimate partners, maternal reproductive history and the women’s HIV status. The intimate partner was considered a spouse, companion or boyfriend with whom the woman was having or had a relationship with. Prevalence estimates of IPV were obtained by asking questions about experiencing specific acts [1]. Overall violence refers to ever being exposed to any form of IPV (physical and/or emotional and/or sexual violence). Physical violence refers to being slapped or thrown at something that could hurt, pushed or shoved, hit with a fist or something else that could hurt, kicked, dragged or beaten up, choked or burnt on purpose or had a gun, knife or other weapon used against. Sexual violence refers to being physically forced to have sexual intercourse against her will, having sexual intercourse because she was afraid of what her partner might do, or being forced to do something sexual she found degrading or humiliating. Psychological violence was defined as being insulted or made to feel bad about one self, humiliated or belittled in front of others, intimidated or scared on purpose (for example by a partner yelling and smashing things), or threatened with harm (directly or indirectly in the form of a threat to hurt someone the respondent cares about).
Statistical Analysis
Data were entered, cleaned, stored and analyzed using Epi-Info version 3.5.1. Descriptive analysis of variables was done to describe the social demographic characteristics of these women. Prevalence of women reporting the various forms of IPV in the index pregnancy, 12 months prior to the pregnancy and in their lifetime was sought. Bivariate analysis was done to compare independent factors of women who experienced violence in the index pregnancy, with women who did not. Associations were detected using Chi square (χ2) or Fisher’s exact test. Multiple logistic regression analysis predicting IPV was used to explore the adjusted association of covariates that had a p < 0.1 in bivariate analyses. We ran 2 multiple regression models (one with the marital status variable of married vs. single and the other with the polygamous vs. monogamous variable). We could not include both marital status variables in one regression model since they both represented descriptions of marital status, and in model 2, the single women were dropped since the question about being in a monogamous versus. polygamous marriage did not apply to them. Both models were critical because we wanted to explore the more standard confounding effect of marital status as well as the potential confounding effect of the culturally-specific monogamous vs. polygamous variable. Odds ratio (OR) was used as the measure of association and 95 % CI were computed. A p < 0.05 was regarded as significant.
Ethical Considerations
Approval for scientific and ethical issues was obtained from the Scientific Steering Committee at the Kenya Medical Research Institute and the National Ethical Review Committee respectively. Permission to carry out the study within the hospital was obtained from the Hospital Management Team. Interviews were conducted in private within the health facility, written informed consent was obtained before administration of the questionnaire and the investigator changed the subject of discussion if an interview was interrupted by anyone. There was no identifier on the questionnaire. Victims severely affected by IPV were referred for counseling sessions and medical treatment for those with untreated injuries.
Results
Participants’ Characteristics
Three hundred pregnant women participated with a mean age of 24 years ranging from 14 to 45 years. The majority of participants were married (80.7 %), had completed primary school education (79.7 %) and had a partner who did not consume alcohol (60 %). Among those who had been tested for HIV and were willing to disclose their status (n = 285), 18 % were HIV positive.
Prevalence of IPV
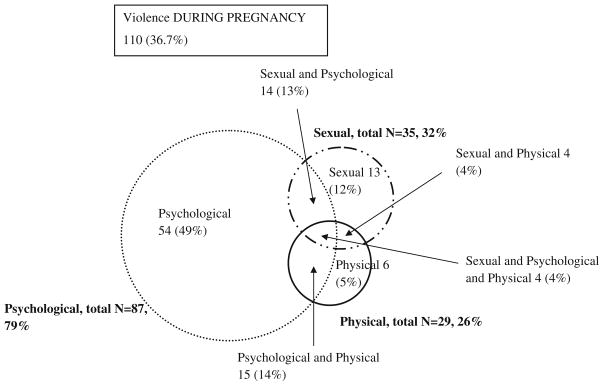
The prevalence of lifetime overall, physical, psychological and sexual IPV was 53, 26, 42 and 15 %, respectively. The prevalence of overall, physical, psychological and sexual IPV within the past 12 months before pregnancy was 52, 25, 40 and 15 %, respectively. Finally, the prevalence of overall, physical, psychological and sexual IPV during pregnancy was 37, 10, 29 and 12 %, respectively. Among the women with a history of IPV during pregnancy (n = 110) 79 % had experienced psychological violence, 32 % sexual violence and 26 % physical violence. Figure 1 illustrates the intersections between the different forms of IPV experienced singly or as a combination by the women during pregnancy. Psychological abuse alone (49 %, n = 54) was the most common form of IPV during pregnancy followed by a combination of physical and psychological abuse (14 %, n = 15), a combination of sexual and psychological abuse (13 %, n = 14) and then sexual abuse alone (13 %, n = 12).
Fig. 1.
Intersections between the different forms of IPV during the index pregnancy among abused women seeking ANC at Kisumu District Hospital- Kenya
The pattern of psychological violence during the index pregnancy (n = 87) revealed that ‘being insulted or being made to feel bad about oneself was the most common (78 %) form of psychological violence. Being ‘belittled or humiliated in front of other people’ was reported by almost half (43 %) of the abused women, the partner ‘doing things to scare her or intimidated her on purpose’ was reported by 9 % and finally ‘threats to hurt her or someone she cared about’ in 6 % of the cases.
Bivariate Analysis Predicting IPV
Bivariate associations between IPV against women during pregnancy and selected vulnerability factors are presented in Table 1. The woman’s characteristics significantly associated with IPV were being currently/ever married, witnessing maternal abuse in childhood, having given birth two or more times and being in a polygamous partnership. The partners characteristics that predicted IPV were drinking alcohol or being 25 years and over. Having a husband/partner with tertiary education and both parties choosing each other were protective factors significantly associated (p < 0.05) with a history of IPV in pregnancy.
Table 1.
Simple logistic regression comparing characteristics of women who experienced IPV during pregnancy with those who did not among women seeking antenatal care at Kisumu District Hospital in Kenya
| Variable | Abused n (%) | Notabused n (%) | cOR (95% CI) | p value |
|---|---|---|---|---|
| Woman’s age (years) | ||||
| 25 and above | 50 (45.5) | 65 (34.2) | 1.60 (0.99–2.6) | 0.07 |
| Less than 25 | 60 (54.5) | 125 (65.8) | Ref | Ref |
| Marital status | ||||
| Single | 5 (4.5) | 43 (22.6) | Ref | Ref |
| Currently/ever married | 105 (95.5) | 147 (77.4) | 6.14 (2.4–16.0) | <0.005 |
| Family structure (n = 252) | ||||
| Polygamous | 25 (24.3) | 17 (11.6) | 2.99 (1.5–5.8) | <0.005 |
| Monogamous | 78 (75.7) | 130 (88.4) | Ref | Ref |
| Woman’s education level | ||||
| Tertiary and above | 11 (10) | (16.3) | 0.57 (0.3–1.2) | 0.18 |
| Secondary and below | 99 (90) | 159 (83.6) | Ref | Ref |
| Occupation | ||||
| Unemployed | 50 (50.9) | 65 (34.2) | 1.60 (0.99–2.6) | 0.07 |
| Employed | 60 (54.5) | 125 (65.8) | Ref | Ref |
| Witnessed maternal abuse in childhood (n = 245)a | ||||
| Yes | 27 (30.3) | 22 (14.1) | 2.65 (1.4-–5.02) | <0.005 |
| No | 62 (69.7) | 134 (85.9) | Ref | Ref |
| Choice of partner | ||||
| Both choose each other | 82 (74.5) | 161 (84.7) | 0.53 (0.3–0.95) | 0.04 |
| Third party’s choice | 28 (25.5) | 29 (15.3) | Ref | Ref |
| Woman’s alcohol intake | ||||
| Yes | 5 (4.5) | 6 (3.2) | 1.46 (0.4–5.6) | 0.75 |
| No | 105 (95.5) | 184 (96.8) | Ref | Ref |
| Bride price paid (n = 252)b | ||||
| Yes | (52.9) | 83 (56.1) | 0.69 (0.4–1.2) | 0.18 |
| No | 55 (47.1) | 65 (43.9) | Ref | Ref |
| Planned pregnancy | ||||
| Yes | 57 (51.8) | 105 (55.3) | 0.87 (0.5–1.4) | 0.65 |
| No | 53 (48.2) | 85 (44.7) | Ref | Ref |
| Woman HIV status (n = 285)c | ||||
| Positive | 24 (23.1) | 27 (14.9) | 1.71 (0.9–3.3) | 0.08 |
| Negative | 80 (76.9) | 154 (85.1) | Ref | Ref |
| History of abortion | ||||
| Yes | 9 (8.2) | 10 (5.3) | 1.60 (0.6–4.1) | 0.45 |
| No | 101 (91.8) | 180 (94.7) | Ref | Ref |
| Parity | ||||
| Multipara (having given birth 2 or more times) | 56 (50.9) | 54 (28.4) | 2.61(1.6–4.3) | 0.005 |
| Primi/nullipara (having given birth B≤1) | 54 (49.1) | (71.6) | Ref | Ref |
| Partner’s age | ||||
| 25 and above | 93 (87.7) | 131 (71.6) | 0.84 (1.4–5.8) | <0.005 |
| Less than 25 years | 13(12.3) | 52 (28.4) | Ref | Ref |
| Partner’s education | ||||
| Tertiary and above | 19 (17.3) | 55 (29.1) | 0.5 (0.3–0.9) | 0.03 |
| Secondary and below | 91 (82.7) | 135 (70.9) | Ref | Ref |
| Alcohol intake by partner | ||||
| Yes | 56 (50.9) | 64 (33.7) | 2.04 (1.3-–3.3) | <0.005 |
| No | 54 (49.1) | 126 (66.3) | Ref | Ref |
cOR crude odds ratio, CI confidence interval, ref reference
some women were not willing to disclose their HIV status
some women were not brought up by their parents, others didn’t know if their mothers experienced IPV
the single never married women did not respond to this question
Multiple Logistic Regression Analysis Predicting IPV
Table 2 shows the adjusted odds ratios for all covariates selected from bivariate comparisons. Women who witnessed their own mother’s abuse during their childhood had over two times greater odds of IPV during their index pregnancy than those that did not witness maternal abuse in childhood. Being in a polygamous partnership also resulted in an over two-fold increased odds of IPV compared to being in a monogamous partnership. Finally, women with a partner who drank alcohol had more than twice the odds of experiencing IPV during their pregnancy than women whose partners did not drink alcohol. Other potentially predictive factors related to multiparity and protective factors related to partner’s higher education level need further exploration due to their borderline p values.
Table 2.
Multiple logistic regression analysis of factors associated with IPV during pregnancy among women seeking antenatal care at Kisumu District Hospital-Kenya
| Independent variable | aOR | 95 % CI | p value | aOR | 95 % CI | p value |
|---|---|---|---|---|---|---|
| Witnessed maternal abuse in childhood (yes vs. no) | 2.27 | 1.05–4.89 | 0.04* | 2.51 | 1.13–5.59 | 0.02* |
| Multiparity (having given birth 2 or more times vs. primi/nulliparity) | 1.94 | 1.01–3.81 | 0.05* | 1.78 | 0.89–3.51 | 0.10 |
| Partner with tertiary education (vs. secondary and below) | 0.37 | 0.16–0.83 | 0.02* | 0.44 | 0.19–1.02 | 0.06 |
| Partner who drinks alcohol (Yes vs. No) | 2.32 | 1.21–4.45 | <0.005* | 2.23 | 1.14–4.36 | 0.02* |
| Currently/ever married (vs. single) | 2.18 | 0.49–9.86 | 0.3 | – | – | – |
| Polygamous (vs. monogamous) | – | – | – | 2.48 | 1.06–5.80 | 0.04* |
aOR adjusted odds ratio, CI confidence interval
=significant p values
Controlling for all variables that had p values ≤ 0.1 in the bivariate analysis
Variables with p values <0.05 are considered statistically significant
Discussion
Our study found that almost 4 out of every 10 participants suffered IPV in the hands of an intimate partner during pregnancy, which is consistent with studies done in other African countries. A review of literature of IPV in African countries found IPV prevalence ranging from 2 to 57 % and a meta-analysis yielded an overall prevalence of 15 % (95 % CI = 14–16 %) [12]. The wide-ranging estimates are likely a result of the different types of violence the researchers inquire about, use of different violence measures, and differences in the populations sampled. Additional differences were apparent in the identity of the perpetrator, the points during the pregnancy at which the assessment was administered and the method of administration. Thus if regional prevalence’s are to be determined and compared then a standardized tool should be developed and used universally.
Pregnancy, although not a disease, is a delicate period when women are expected to be protected from violence. However, some studies have reported that violence appears or escalates during pregnancy [13, 14]. The results of this study showed that a third of the women who reported violence 12 months before pregnancy were not exposed to violence during the pregnancy. There was a significant decrease in all forms of violence during pregnancy except for sexual violence and the majority of the abused women felt that IPV during pregnancy was somewhat less severe and/or less frequent than before the pregnancy. This reaffirms that indeed pregnancy gives some protection from IPV.
Witnessing maternal abuse during childhood was significantly related to IPV during pregnancy even after controlling for confounding covariates. This condition, observed in the present study, may indicate that IPV witnessed in the woman’s childhood may currently be experienced as a “normal” part of life, contributing to her low self-esteem and lack of autonomy to create mechanisms that may help to modify this situation [15]. In addition Kenya is a patriarchal society where violence is recognized as one way of “disciplining” one’s wife, with many women socialized to anticipate this discipline. The gender role socialization (particularly in rural areas) may contribute to the link between witnessing maternal abuse and IPV in pregnancy. Similar findings were reported in Brazil [16].
Partner’s alcohol consumption was also found to be a significant predictor of IPV during pregnancy. This finding has been reported from other studies as well although, the temporal sequence of this association is not clear [12]. Alcohol use can result in household neglect facilitating marital or relationship tension that may result in violence. Alcohol use has also been associated with having multiple sexual partners, an issue that may also lead to conflict [17]. Furthermore, some may intentionally take alcohol to gain courage to engage in selfish deeds such as IPV against their partners.
Polygamy was a third significant predictor of IPV during pregnancy. A plausible explanation for this could be the perceived unequal love among the women or neglect of one or more of the spouses resulting in jealousy and tension in the home and thus fuelling IPV. Another explanation is that it is also possible that men in polygamous relationships experience differential levels of attachment towards their spouses and are more likely to abuse those who have become less favored. Similar findings were reported in a study done in Pakistan [18].
Further research into multiparity and partner’s education is necessary in order to explore their hypothesized effects on IPV during pregnancy. Education as a source of information and also an instrument of change for social norms could fuel the inverse association. This is supported by a study carried out in rural Vietnam [19]. In addition, having delivered two or more times may just demonstrate how women are still dependent on men. Perhaps economic dependence on the abuser is a very real reason for remaining in the relationship. Similar findings were reported in Pakistan [18].
Some factors that have been found to be associated with IPV in other studies were not found in our study. In this study, the woman’s age had no association with IPV. Studies have documented younger age among pregnant women to be associated with increased IPV [20]. The education level of the woman also did not make a difference on exposure to IPV. This finding is consistent with studies conducted in Nigeria [21]. However, studies done elsewhere have shown that women who were less educated had higher odds of abuse during pregnancy than more educated women [22]. Finally, this study found no association between HIV and IPV, which differed from a previous study done in Nairobi, Kenya. The study was on etiology of sexually transmitted infections (STI) among women presenting at an STI clinic in Nairobi and it reported an increased risk of HIV in women reporting physical violence [23]. However, a study done in rural Rwanda similarly reported no association between HIV and IPV [24] and thus further research is needed to shed light on this important issue.
Study Limitations
This study was cross-sectional in design and thus cannot ascribe causation between any of the covariates and IPV. Also this study recruited pregnant women who were seeking antenatal care at a public hospital; to the extent that pregnant women in public facilities differ from those who go to private clinics or those who do not attend antenatal clinic implies that our findings may not be representative of all pregnant women in the study area. In addition since the study was done in one health facility, the results cannot be generalized to the whole country. Previous studies have reported that abused women experience significant barriers to accessing healthcare [25]. Male partners may prevent their female partners from accessing healthcare as a means of control [26]. This may suggest that these women may be under-represented in healthcare settings; conversely authors in previous research have also reported the increased occurrence of illness among women exposed to IPV [27]. These women may, therefore present more often to health care centers than non-abused women with psychosomatic illnesses. For pregnant women in this setting, the antenatal clinic may be one such clinic. While both scenarios are possible, there is no data to substantiate the possibility of one mechanism predominating over the other. Finally it is important to recognize that data were obtained through self-reports; thus there is possibility of inadvertent as well as deliberate misreporting.
In conclusion, our study established that IPV during pregnancy was a common experience among women seeking antenatal care at Kisumu District Hospital, more common than reported in many other studies, but within the range of reported prevalence from other Sub-Saharan African countries. Therefore, there is a paramount need to include screening for IPV as an integral part of routine antenatal care, train health care providers on how to identify victims of IPV, provide optimal care, and to link IPV survivors with appropriate counseling, legal and social support services. Finally this study examined factors associated with experiencing any type of IPV (psychological and/or physical and/or sexual) during pregnancy. With a larger sample, it would be interesting to examine factors predictive of each of the three types of IPV during women’s pregnancy; in addition further research on male attitudes and beliefs that contribute to IPV should be done if a comprehensive understanding of the problem is to be achieved.
Acknowledgments
We would like to thank the following for their support and contributions: The antenatal clinic staff at Kisumu District Hospital and clients who sought antennal care during the study period, Field Epidemiology and Laboratory Training Program, Kenya (FELTP-K) faculty and administration, Jomo Kenyatta University of Agriculture and Technology (JKUAT), Ministries of Public Health and Sanitation and Medical Services-Kenya and finally the Centers for Disease Control and prevention (CDC) for their financial contribution.
Footnotes
Conflict of interest: The authors state that they have no conflicts of interests.
Contributor Information
Lyndah A. Makayoto, Email: lmakayotto@yahoo.com, Field Epidemiology and Laboratory Training Program, Nairobi, Kenya. Jomo Kenyatta University of Agriculture and Technology, Nairobi, Kenya.
Jared Omolo, Email: jaredom2000@yahoo.com, Field Epidemiology and Laboratory Training Program, Nairobi, Kenya.
Abel M. Kamweya, Email: abelkamweya@yahoo.com, Jomo Kenyatta University of Agriculture and Technology, Nairobi, Kenya.
Valarie S. Harder, Email: vharder@yahoo.com, University of Vermont, 1 South Prospect Street, Burlington, VT 05452, USA.
Joseph Mutai, Email: joemutai@yahoo.com, Kenya Medical Research Institute, Nairobi, Kenya.
References
- 1.World Health Organization. Multi-country study on women’s health and domestic violence against women 2005 [Google Scholar]
- 2.Heise L, Garcia-Moreno C. Violence by intimate partners. In: Krug EG, Dahlberg LL, Mercy JA, et al., editors. World report on violence and health. Geneva: World Health Organization; 2002. pp. 87–121. [Google Scholar]
- 3.Ahmed S, Koenig MA, Stephenson R. Effects of domestic violence on perinatal and early-childhood mortality: Evidence from north India. American Journal of Public Health. 2006;96:1423–1428. doi: 10.2105/AJPH.2005.066316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boy A, Salihu HM. Intimate partner violence and birth outcomes: A systematic review. International Journal of Fertility and Women’s Medicine. 2004;49:159–164. [PubMed] [Google Scholar]
- 5.Campbell JC, Baty ML, Ghandour RM, et al. The intersection of intimate partner violence against women and HIV/ AIDS: A review. International Journal of Injury Control and Safety. 2008;15(4):221–231. doi: 10.1080/17457300802423224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunkle K. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet. 2004;363:1415–1421. doi: 10.1016/S0140-6736(04)16098-4. [DOI] [PubMed] [Google Scholar]
- 7.Plichta SB, Falik M. Prevalence of violence and its implications forwomen’s health. Women’sHealthIssues. 2001;11:244–258. doi: 10.1016/s1049-3867(01)00085-8. [DOI] [PubMed] [Google Scholar]
- 8.Heise L, Ellsberg M, Gottemoeller M. Ending violence against women. Baltimore: Johns Hopkins University Press; 1999. [Google Scholar]
- 9.Kenya National Bureau of Statistics (KNBS) and ICF Macro. Kenya Demographic and Health Survey. Calverton: KNBS and ICF Macro; 2010. [Google Scholar]
- 10.Rwanda Demographic Health Survey. 2005 Institut National de la Statistique Ministére des Finances et de la Planification Économique Kigali. Rwanda an ORC Macro Calverton; Mary-land USA: 2006. p. FR183. [Google Scholar]
- 11.Cochran WG. Sampling Techniques. 2. New York: Wiley; 1963. [Google Scholar]
- 12.Shamu S, Abrahams N, Temmerman M, et al. A systematic review of african studies on intimate partner violence against pregnant women: prevalence and risk factors. PLoS One. 2011;6(3):e17591. doi: 10.1371/journal.pone.0017591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenberg ML, Mercy JA, Hammond WR. Assaultive violence. In: Wallace RB, Doebbeling BN, editors. Maxcy-Rosenau-Last Public Health and Preventive Medicine. 14. Stamford: Appleton and Lange; 1998. pp. 1226–1238. [Google Scholar]
- 14.Kerstin EE, Högberg U. Violence against pregnant women will remain hidden as long as no direct questions are asked. Midwifery. 2002;18:268–278. doi: 10.1054/midw.2002.0318. [DOI] [PubMed] [Google Scholar]
- 15.Durand JG, Schraiber LB. Violência na gestação entre usuárias de serviços públicos de saúde da Grande São Paulo: Prevalência e Fatores Associados. Revista Brasileira de Epidemiologia. 2007;10(3):310–322. [Google Scholar]
- 16.Schraiber LB, D’Oliveira AF, Couto MT. Violência e súade: estudos científicos recentes. Revista de Saúde Pública. 2006;40:112–120. doi: 10.1590/s0034-89102006000400016. [DOI] [PubMed] [Google Scholar]
- 17.Weiser SD, Leiter K, Heisler M, et al. A population-based study on alcohol and high-risk sexual behaviors in Botswana. PLoS Med. 2006;3:e392. doi: 10.1371/journal.pmed.0030392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karmaliani R, Irfan F, Bann CM, et al. Domestic violence prior to and during pregnancy among Pakistani women. Acta Obstetricia et Gynacologica Scandinavica. 2008;87(11):1194–1201. doi: 10.1080/00016340802460263. [DOI] [PubMed] [Google Scholar]
- 19.Vung ND, Ostergren PO, Krantz G. Intimate partner violence against women in rural Vietnam—Different socio-demographic factors are associated with different forms of violence: need for new intervention guidelines? BMC Public Health. 2008;8:55. doi: 10.1186/1471-2458-8-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dunn LL, Oths KS. Prenatal predictors of intimate partner abuse. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2004;33:54–63. doi: 10.1177/0884217503261080. [DOI] [PubMed] [Google Scholar]
- 21.Ezechi OC, Kalu BK, Ezechi LO, et al. Prevalence and pattern of domestic violence against pregnant Nigeria women. Journal of Obstetrics and Gynecology. 2004;24:652–656. doi: 10.1080/01443610400007901. [DOI] [PubMed] [Google Scholar]
- 22.Khurram N, Hyder A. Violence against pregnant women in developing countries: review of evidence. European Journal of Public Health. 2003;13:105–107. doi: 10.1093/eurpub/13.2.105. [DOI] [PubMed] [Google Scholar]
- 23.Fonck K, Leye E, Kidula N, et al. Increased risk of HIV in women experiencing physical partner violence in Nairobi. Kenya AIDS and behavior. 2005;9(3):335–339. doi: 10.1007/s10461-005-9007-0. [DOI] [PubMed] [Google Scholar]
- 24.Ntaganira J, Muula AS, Siziya S, et al. Factors associated with intimate partner violence among pregnant rural women in Rwanda. Rural and Remote Health. 2009;9:1153. online. Available from: http://www.rrh.org.au. [PubMed] [Google Scholar]
- 25.Wilson KS, Silberberg MR, Brown AJ, et al. Health needs and barriers to healthcare of women who have experienced intimate partner violence. Journal of Womens Health (Larchmt) 2007;16:1485–1498. doi: 10.1089/jwh.2007.0385. [DOI] [PubMed] [Google Scholar]
- 26.Nicolaidis C. Partner interference with health care: do we want one more piece of a complex puzzle? Journal of General Internal Medicine. 2007;22:1216–1217. doi: 10.1007/s11606-007-0262-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lipsky S, Holt VL, Easterling TR, et al. Police-reported intimate partner violence during pregnancy and the risk of antenatal hospitalization. Maternal and Child Health Journal. 2004;8:55–63. doi: 10.1023/b:maci.0000025727.68281.aa. [DOI] [PubMed] [Google Scholar]