Abstract
Objective
To examine self-reported rates and disparities in delivery of preventive services to young adults.
Design
Population-based cross-sectional analysis. Multivariate logistic regression was used to examine how age, gender, race/ethnicity, income, insurance, and usual source of care influence the receipt of preventive services.
Setting
2005 and 2007 California Health Interview Surveys (CHIS).
Participants
3670 and 3621 young adults aged 18-26 years who responded to CHIS 2005 and 2007, respectively.
Main Outcome Measures
Self-reported receipt of flu vaccination, STD screening, cholesterol screening, diet counseling, exercise counseling and emotional health screening.
Results
Delivery rates ranged from 16.7% (flu vaccine) to 50.6% (cholesterol screening). Being female and having a usual source of care significantly increased receipt of services, with females more likely to receive STD screening (p<.001), cholesterol screening (p<.01), emotional health screening (p<.001), diet counseling (p<.01) and exercise counseling (p<.05) than males after controlling for age, race/ethnicity, income, insurance and usual source of care. Young adults with a usual source of care were more likely to receive a flu vaccine (p<.05), STD screening (p<.01), cholesterol screening (p<.001), diet counseling (p<.05) and exercise counseling (p<.05) than those without a usual source of care after adjusting for age, race/ethnicity, income, and insurance.
Conclusions
Rates of preventive service delivery are generally low. Greater efforts are needed to develop guidelines for young adults to increase the delivery of preventive care to this age group, and to address the gender and ethnic/racial disparities in preventive services delivery.
Keywords: Young adults, preventive services, primary care
Implications and Contribution
This is the first paper to examine young adult-report of preventive service delivery. Our findings suggest that rates of preventive service delivery are generally low, and having a usual source of care facilitates the receipt of a broad range of preventive care.
Introduction
Young adults, spanning the age of 18 to 26, have received little attention in the preventive health literature. This is despite the fact that the transition to young adulthood is accompanied by higher mortality and morbidity rates than in adolescence, much of which is attributed to preventable factors such as binge drinking, substance use, driving under the influence, weapon possession, risky sexual behaviors, and sedentary lifestyle (1-5). Unhealthy behaviors tend to continue into middle and late adulthood, predisposing individuals to preventable chronic conditions such as cardiovascular and respiratory diseases and diabetes.
Interventions that can alter these unhealthy behaviors may have a significant impact on a young person’s life, and preventive visits are an optimal time to screen and counsel about health risks (6). Yet, the delivery of preventive services to young adults has not received significant attention in both research literature and clinical practice. Although a broad consensus has emerged for clinical guidelines for adolescent preventive services, there are no specific clinical preventive services guidelines that specifically address the young adult age group (6). Young adults have been the age group most likely to be uninsured in the US (7). This challenge can be potentially mitigated by the Patient Protection and Affordable Care Act of 2010 (ACA), which provides unprecedented expansion of health insurance coverage to young adults up to the 26th birthday, including mandatory coverage for preventive services (8, 9). An important conjecture is whether this increase of access will translate to a corresponding increase in utilization of preventive services.
While multiple studies have examined the receipt of preventive care among adolescents and the general adult population (10-13), only two published studies have focused on young adults’ preventive care utilization (14, 15). Both studies utilized provider-reported data from the National Ambulatory Care (NAMCS) and National Hospital Ambulatory Care Surveys (NHAMCS). Findings from these studies indicate that young adults between the ages of 20-29 utilize less ambulatory medical and preventive care than children, adolescents, and older adults (14), and less than one-third (32%) of the visits included some form of preventive counseling. Further, males had fewer visits than females, and Black and Hispanic young adults had fewer visits than other adults (15).
While provider self-report is one important source of information, patient self-report has been shown to be a valuable indicator of utilization and quality of health services both in adult and adolescent literature (16-20). No study has examined the level of preventive care delivery from a young adult-reported perspective. In addition, while previous research has provided information about the influence of demographic characteristics on ambulatory care visits, the influence of demographic variables on the receipt of specific preventive services, such as diet and exercise counseling, are not known. Moreover, while it has been shown that health insurance is a major factor influencing access to health services among young adults (21), it is not known whether other healthcare access factors, such as having a usual source of care, influence the receipt of specific preventive services among young adults.
This study addressed these gaps in the literature through utilizing a large population health survey, the California Health Interview Survey (CHIS), to examine self-reported rates of preventive service delivery and the relationships between demographic and healthcare access factors on the receipt of preventive services among young adults. Specifically, the goals of this study were to: 1) determine the percent of young adults receiving six different preventive services: flu vaccination, sexually-transmitted disease (STD) screening, emotional health screening, cholesterol screening, diet and exercise counseling; and 2) explore how age, gender, race/ethnicity, household income, insurance status, and presence or absence of usual source of care, are related to the frequency of the receipt of each of the preventive services.
Methods
CHIS design and sampling
We examined data from the 2005 and 2007 CHIS that are available for research purposes in the public use files. While the most recent CHIS data for public use is from 2009, we did not include 2009 data in this analysis because the variables of interest are not available in that year. CHIS, the largest multiethnic, multilinguistic state population health survey in the US, is a random digit dialing survey of the California population that has been conducted every 2 years since 2001. Adults who reside in households are sampled scientifically from every county in the state and interviews are conducted with one randomly selected adult in the household. Data are weighted to compensate for differential probabilities of selection for households to ensure that the sample is representative of the CA population. Detailed description of the sampling methodology can be found in the CHIS 2007 Methodology Series (22). This study was registered with the Committee on Human Research at UCSF under exempt status. All CHIS procedures were approved by the institution review board at UCLA, the State of California, Westat (data collection organization), and the federal Office of the Management of the Budget.
Study participants
Young adults from the age of 18 through 26 years who participated in the CHIS 2005 (n=3670) and CHIS 2007 (n=3621) adult surveys were included in the study. The upper limit of age 26 was used as the ACA extended health insurance coverage to this group effective 2010.
Demographics and health risk profile (Table 1)
Table 1.
Descriptive analysis of the demographic characteristics, health risk profile and self-reported healthcare access among young adults in CHIS 2005 and 2007 (percentage rates).
| CHIS 2005 (N=3,670) Population estimates = 4,529,411 |
CHIS 2007 (N=3,621) Population estimates = 4,679,521 |
|
|---|---|---|
| Age 18-22 23-26 |
57.4% 42.7% |
62.0% 38.0% |
| Gender F |
48.3% | 48.6% |
| Race/Ethnicity White Black Latino Asian Multiracial Native/Alaskan American Pacific Islander |
33.4% 5.8% 45.7% 12.1% 2.0% 0.6% 0.4% |
34.6% 5.9% 41.8% 14.8% 1.9% 0.5% 0.5% |
| Income 0-99% FPL 100-199% FPL 200-299% FPL >300% FPL |
20.0% 22.7% 15.6% 41.7% |
20.8% 19.2% 15.6% 44.4% |
| Currently insured | 70.7% | 74.1% |
| Overweight/Obese | 41.8% | 40.4% |
| Have at least 1 sex partner in the past 12 months* | 73.8% | 74.4% |
| Healthcare access Presence of usual source of care Doctor’s office/HMO/Kaiser Community/Government/Community Hospital Clinic |
70.0% 43.3% 26.7% |
NA NA NA |
Source: AskCHIS. An online search tool to obtain health statistics from CHIS.
NA means the variable is not available for analysis either due the question not asked in that year’s survey or the variable is not in the public use file.
Defined as body mass index >25 based on self-reported weight and height.
Variables in the CHIS dataset that were utilized include: age, gender, race/ethnicity, household income1, insurance status. Other variables include: whether a young adult had at least 1 sex partner in the past 12 months, and whether he/she reported to be overweight/obese. Young adults reported household income as a percent of FPL. They reported insurance status as currently insured versus not currently insured. CHIS reported participants’ overweight/obese status using body mass index (BMI) calculated with self-reported weight and height (kilogram/meter-squared). Using this BMI calculation, young adults were categorized as overweight/obese when BMI is greater than 25 (23).
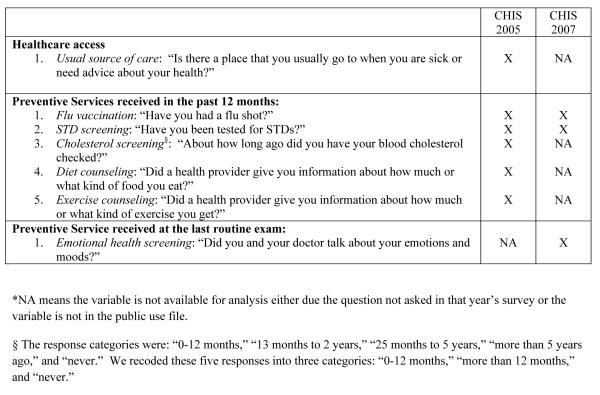
Healthcare access variable (See Figure 1)
Figure 1. Descriptions and sources of the healthcare access and preventive services variables.
*NA means the variable is not available for analysis either due the question not asked in that year’s survey or the variable is not in the public use file.
§ The response categories were: “0-12 months,” “13 months to 2 years,” “25 months to 5 years,” “more than 5 years ago,” and “never.” We recoded these five responses into three categories: “0-12 months,” “more than 12 months,” and “never.”
To broadly assess the level of healthcare access, we examined the self-reported rate of the presence or absence of a usual source of care.
Receipt of preventive services variables (See Figure 1)
The survey queried respondents about the receipt of six preventive services. They are receipt of a flu vaccine, STD screening, cholesterol screening, diet counseling and exercise counseling in the past 12 months. It asked the receipt of emotional health screening at the last routine exam.
Analysis Plan
We performed all statistical analyses using Stata version 11 statistical software package (24). We applied weights provided by the CHIS investigators to generate population frequency estimates of healthcare access and receipt of preventive services. Figure 1 describes the source of each variable. We used a bivariate logistic regression model on each of the preventive service variables by age category, gender, race/ethnicity, income, insurance status, and usual source of care to yield unadjusted odds ratios. We then conducted multivariate logistic regressions for each of the preventive variables with all the demographic and healthcare access variables to yield adjusted odds ratios.
Because the 2005 dataset offered a fuller set of independent variables, we conducted both the bivariate and multivariate analyses only on 2005 data except for the variable emotional health screening, which was only available in the 2007 dataset. As current clinical guidelines recommend that health providers monitor blood cholesterol and provide diet and physical activity counseling to overweight/obese patients (25), we adjusted for overweight/obese status for the variables cholesterol screening, diet counseling and exercise counseling. American Indian/Alaskan Native and Pacific Islanders were excluded in the multivariate logistic regressions due to small sample sizes. Using the method provided by the CHIS investigators, estimates that were considered statistically unstable are noted in Tables 2 and 3.
Table 2.
Receipt of flu vaccination, STD screening in the past 12 months and emotional health screening at the last routine exam (percentage rates, odds ratios, adjusted odds ratios, 95% confidence intervals).
| Flu vaccination (2005) N= 3670 Pop est. = 4,529,411 |
STD screening (2005) N=2827 Pop est. =3,329,306 |
Emotional health screening (2007) N=3229 Pop est. = 4,143,427 |
|
|---|---|---|---|
| Overall | 16.7% | 42.2% | 21.5% |
| Age 18-22 (reference) 23-26 OR aOR |
18.6% 14.3% 0.73 (0.59-0.90)† 0.75 (0.61-0.92) a † |
44.6% 39.7% 0.82 (0.68-0.99) ‡ 0.85 (0.69-1.06) a |
20.2% 23.6% 1.22 (0.95-1.58) 1.22 (0.93-1.59)g |
| Gender M (reference) F OR aOR |
18.2% 15.3% 0.81 (0.62-1.06) 0.72 (0.55-0.95) b ‡ |
27.0% 57.5% 3.66 (2.95-4.53) § 3.40 (2.70-4.28) b§ |
16.5% 26.2% 1.80 (1.39-2.32) † 1.74 (1.33-2.27)h § |
| Race/Ethnicity White (reference) Latino OR aOR Black OR aOR Asian OR aOR Multiracial OR aOR |
17.1% 16.3% 0.94 (0.73-1.21) 1.23 (0.84-1.51) c 18.4% 1.09 (0.67-1.78) 1.18 (0.70-1.97) c 18.3% 1.07 (0.74-1.55) 1.08 (0.74-1.57) c 14.1% 0.79 (0.43-1.46) 0.85 (0.45-1.60) c |
44.3% 40.4% 0.85 (0.69-1.06) 1.04 (0.81-1.34) c 59.9% 1.88 (1.19-2.98) † 2.08 (1.24-3.48) c † 28.2% 0.50 (0.33-0.76) † 0.52 (0.34-0.80) c † 53.8% 1.46 (0.86-2.49) 1.59 (0.94-2.72) c |
22.9% 21.9% .94 (0.69-1.28) 0.96 (0.66-1.39)i 22.8% 0.99 (0.57-1.74) 0.97 (0.53-1.76) i 14.2% 0.62 (0.42-0.92) ‡ 0.57 (0.37-0.84) i † 32.9% 1.65 (0.86-3.15) 1.65 (0.86-3.19) i |
| Income 0-99% FPL (reference) 100-199% FPL OR aOR 200-299% FPL OR aOR >300% FPL OR aOR |
12.7% 16.5% 1.36 (0.91-2.03) 1.37 (0.92-2.05) d 19.6% 1.68 (1.21-2.33) † 1.57 (1.11-2.21) d‡ 17.8% 1.49 (1.11-2.01) † 1.36 (0.97-1.91) d |
41.4% 40.5% 0.96 (0.71-1.31) 1.06 (0.75-1.49) d 39.0% 0.90 (0.63-1.29) 0.97 (0.65-1.44) d 44.6% 1.14 (0.85-1.53) 1.27 (0.89-1.82) d |
20.8% 23.1% 1.15 (0.78-1.68) 1.20 (0.81-1.79)j 23.6% 1.18 (0.72-1.93) 1.21 (0.72-2.02) j 20.4% 0.97 (0.65-1.46) 1.05 (0.65-1.68) j |
| Currently insured No (reference) Yes OR aOR |
12.7% 18.5% 1.56 (1.16-2.10) † 1.33 (0.98-1.83) e |
31.7% 46.3% 1.86 (1.48-2.34) § 1.29 (0.97-1.72) e |
17.0% 22.8% 1.44 (1.02-2.02) ‡ 1.39 (0.96-2.03)k |
| Usual source of care No (reference) Yes OR aOR |
12.4% 18.7% 1.63 (1.18-2.24) † 1.52 (1.09-2.12) f ‡ |
30.1% 46.9% 2.05 (1.62-2.58) § 1.54 (1.19-2.01) f † |
NA NA NA NA |
P< 0.001
P< 0.01
P< 0.05
Statistically unstable
Adjusted for gender, race/ethnicity, income, insurance status, usual source of care
Adjusted for age, race/ethnicity, income, insurance status, usual source of care
Adjusted for age, gender, income, insurance status, usual source of care
Adjusted for age, gender, race/ethnicity, insurance status, usual source of care
Adjusted for age, gender, race/ethnicity, income, usual source of care
Adjusted for age, gender, race/ethnicity, income, insurance status
Adjusted for gender, race/ethnicity, income, insurance status
Adjusted for age, race/ethnicity, income, insurance status
Adjusted for age, gender, income, insurance status
Adjusted for age, gender, race/ethnicity, income
Adjusted for age, gender, race/ethnicity, insurance status
Table 3.
Receipt of cholesterol screening, diet and exercise counseling in the past 12 months (percentage rates, odds ratios, adjusted odds ratios, 95% confidence intervals).
| Cholesterol screening (2005) N=3670 Pop est.= 4,529,411 |
Diet counseling (2005) N=2955 Pop est. = 3,557,718 |
Exercise counseling (2005) N=2955 Pop est.= 3,557,718 |
|
|---|---|---|---|
| Overall | 50.6% | 18.1% | 22.0% |
| Age 18-22 (reference) 23-26 OR aOR |
50.3% 51.1% 1.03 (0.88-1.21) 1.02 (0.86-1.21) a |
17.1% 19.4% 1.16 (0.89-1.52) 1.08 (0.80-1.44)a |
20.1% 24.6% 1.29 (1.00-1.67) 1.22 (0.92-1.61)a |
| Gender Male (reference) Female OR aOR |
45.8% 55.8% 1.50 (1.25-2.26) § 1.39 (1.15-1.68) b † |
15.0% 20.7% 1.49 (1.17-1.89) † 1.49 (1.15-1.94)b † |
19.1% 24.5% 1.37 (1.09-1.74) † 1.38 (1.06-1.80)b‡ |
| Race/Ethnicity White (reference) Latino OR ∥OR Black OR aOR Asian OR aOR Multiracial OR aOR |
44.6% 55.6% 1.57 (1.30-1.91) § 1.87 (1.48-2.36)c§ 56.5% 1.62 (1.10-2.38) ‡ 1.63 (1.08-2.45) c ‡ 43.4% 0.96 (0.73-1.27) 1.06 (0.76-1.43) c 50.4% 1.27 (0.83-1.93) 1.35 (0.90-2.03) c |
12.3% 22.0% 2.01 (1.55-2.62) § 1.91 (1.43-2.57) c § 17.6% 1.52 (0.89-2.61) 1.23 (0.71-2.13) c 20.5% 1.94 (1.18-2.95) ∥ 1.95 (1.25-3.05) c ∥ 16.3% 1.38 (0.73-2.63) 1.26 (0.67-2.38) c |
19.6% 22.6% 1.20 (0.91-1.58) 1.23 (0.91-1.67) c 23.7% 1.28 (0.72-2.26) 1.10 (0.63-1.95) c 25.1% 1.38 (0.87-2.17) 1.54 (0.97-2.43) c 23.7% 1.27 (0.72-2.27) 1.25 (0.72-2.18) c |
| Income 0-99% FPL (reference) 100-199% FPL OR aOR 200-299% FPL OR aOR >300% FPL OR aOR |
55.4% 46.8% 0.71 (0.55-0.92) ‡ 0.74 (0.57-0.96)d ‡ 48.9% 0.77 (0.59-1.01) 0.84 (0.63-1.11) d 51.0% 0.84 (0.66-1.07) 0.99 (0.76-1.29) d |
23.0% 17.2% 0.69 (0.48-1.00) ‡ 0.74 (0.51-1.07) d 22.7% 0.98 (0.69-1.40) 1.12 (0.78-1.61) d 14.5% 0.57 (0.41-0.78) † 0.69 (0.48-1.00) d |
25.9% 17.3% 0.60 (0.40-0.88) ‡ 0.61 (0.41-0.92) d‡ 23.7% 0.89 (0.61-1.30) 0.92 (0.63-1.35) d 21.9% 0.80 (0.60-1.07) 0.84 (0.61-1.16) d |
| Currently insured No (reference) Yes OR aOR |
46.7% 53.4% 1.45 (1.22-1.74) § 1.26 (1.03-1.54)e ‡ |
14.5% 19.2% 1.41 (1.02-1.94) ‡ 1.45 (1.04-2.02) e‡ |
16.0% 23.9% 1.65 (1.16-2.35) † 1.49 (1.02-2.17) e ‡ |
| Usual source of care No (reference) Yes OR aOR |
39.9% 55.2% 1.86 (1.53-2.26) § 1.77 (1.41-2.21)f§ |
13.5% 19.4% 1.54 (1.10-2.15) ‡ 1.52 (1.08-2.13) f ‡ |
15.2% 24.0% 1.77 (1.22-2.57) † 1.59 (1.07-2.38) f ‡ |
| Overweight/obese No (reference) Yes OR aOR |
48.6% 53.4% 1.21 (1.01-1.45) ‡ 1.20 (1.00-1.45)g |
14.5% 23.1% 1.77 (1.37-2.28) § 1.89 (1.44-2.49) g § |
17.7% 28.2% 1.83 (1.46-2.29) § 1.96 (1.53-2.51) g§ |
P< 0.001
P< 0.01
P< 0.05
Statistically unstable
Adjusted for gender, race/ethnicity, income, insurance status, usual source of care, overweight/obese
Adjusted for age, race/ethnicity, income, insurance status, usual source of care, overweight/obese
Adjusted for age, gender, income, insurance status, usual source of care, overweight/obese
Adjusted for age, gender, race/ethnicity, insurance status, usual source of care, overweight/obese
Adjusted for age, gender, race/ethnicity, income, usual source of care, overweight/obese
Adjusted for age, gender, race/ethnicity, income, insurance status, overweight/obese
Adjusted for age, gender, race/ethnicity, income, insurance status, usual source of care
Results
Descriptive Analysis
Table 1 summarizes the demographic characteristics, health risk profile and healthcare access of our sample. Almost two-thirds of young adults were of the younger age group between the ages of 18-22. There were equal proportions of female and male participants. About two-thirds of the participants were non-White, with about 40% having a household income 200% of FPL. Over 70% of young adults were currently insured.
For healthcare access, the majority of young adults (70%) reported having a usual source of care.
Receipt of preventive services (See Tables 2 and 3)
Less than a quarter of young adults reported receiving a flu vaccine (16.7%), diet counseling (18.1%) or exercise counseling (22.0%) in the past 12 months (Table 2). About half of young adults reported having STD screening (42.2%) and cholesterol screening (50.6%) in the past 12 months. Less than a quarter (21.5%) of young adults reported emotional health screening at the last routine exam (Table 3).
Receipt of preventive services by demographic and healthcare access factors (See Tables 2 and 3)
The unadjusted bivariate analysis results are presented in Tables 2 and 3. The following summarizes results from the multivariate logistic regression model that was adjusted for age category, gender, race/ethnicity, income, insurance status, and usual source of care.
Age
Young adults between the ages of 23-26 were 25% less likely to receive a flu vaccine than young adults between the ages of 18-22 (p<.01). Age was not a factor in the receipt of cholesterol screening, diet counseling, exercise counseling or emotional health screening.
Gender
Females were more likely than males to receive all preventive services except for flu vaccination. Females were 240% more likely to receive STD screening (p<.001); 39% more likely to receive cholesterol screening (p<.01), 49% more likely to receive diet counseling (p<.01), 38% more likely to receive exercise counseling (p<.05), and 74% more likely to receive emotional health screening (p<.001) than males. However, females were 28% less likely to receive a flu vaccine than males (p<.05).
Race/Ethnicity
The receipt of preventive services differed by race/ethnicity in STD screening, cholesterol screening, diet counseling and emotional health screening, but not in flu vaccination and exercise counseling. Black young adults were roughly 100% more likely to receive STD screening than White young adults (p<.01), while Asian young adults were 48% less likely to receive STD screening than White young adults (p<.01). Latino and Black young adults were 87% (p<.001) and 63% (p<.05) more likely to receive cholesterol screening than White young adults, respectively. Latino young adults were almost 100% more likely to receive diet counseling than White young adults (p<.001). Asian young adults were 43% less likely than White young adults to receive emotional health screening (p<.01).
Household income
Young adults with household income of 200-299% FPL were 57% (p<.05) more likely to receive a flu vaccine than those with household income of 0-99% FPL. In contrast, young adults with income of 100-199% FPL were 26% (p<.05) less likely to receive cholesterol screening and 39% (p<.05) less likely to receive exercise counseling than those with household income of 0-99% FPL. Household income was not a factor in the receipt of STD screening, diet counseling and emotional health screening.
Currently insured
Currently insured young adults were 26% more likely to receive cholesterol screening (p<.05), 45% more likely to receive diet counseling (p<.05), and 49% more likely to receive exercise counseling (p<.05) than uninsured young adults. Health insurance status was not a factor in the receipt of a flu vaccine, STD screening and emotional health screening.
Usual source of care
Young adults with a usual source of care were 52% more likely to receive a flu vaccine (p<.05), 54% more likely to receive STD screening (p<.01), 77% more likely to receive cholesterol screening (p<.001), 52% more likely to receive diet counseling (p<.05) and 59% more likely to receive exercise counseling (p<.05) than those without a usual source of care.
Overweight/obese
Young adults who were overweight/obese were 89% (p<.001) and 96% (p<.001) more likely to receive diet and exercise counseling, respectively, than young adults who were not overweight/obese. Being overweight/obese was not associated with the receipt of cholesterol screening.
Discussion
Using a large self-reported population dataset, we found that young adults received low rates of preventive services (16.7-50.6%); however, having a usual source of care led to the receipt of a wider range of preventive services regardless of insurance status. This is consistent with findings from studies in the pediatric and adult population, where the presence of usual source of care plays an important role in improving access to health education and counseling (10-13) (26). Usual source of care is a component of the medical home concept that is widely used to improve quality of care for transition-aged adolescents (27, 28). The results from this study suggest that as uninsured young adults gain access to health insurance through ACA, it will be important to connect them to a regular and known source of care.
Young females were more likely to receive preventive services than young males, except for flu vaccination. The largest disparity between males and females was in STD screening. This likely reflects the female-focused Center for Disease Control and Prevention and U. S. Preventive Services Task Force recommendations on chlamydia and gonorrhea screening guidelines (29-30). It may also be that young males, unlike females, do not have reproductive health needs that prompt them to visit their health providers regularly (31). Our findings support recent work on male adolescent health and suggest that greater effort should also be focused on increasing the use of preventive care among young men (32-33).
Age and household income were not strongly associated with the receipt of preventive services. The age of the young adult mattered only in the receipt of a flu vaccine for which the younger age group was more likely to receive flu vaccine than the older group. Since the younger age group includes young adults of college-age, their higher uptake could be related to the college environment, potentially receiving encouragement via school campaigns, such as posters, advertisements in student newspapers, and college health. It is also possible that a higher percentage of this younger age group continues to seek care at a pediatric medical home where delivery of immunizations is a key scope of practice based on current guidelines (34-35). For household income, young adults with lower income were more likely to receive cholesterol screening, diet counseling and exercise counseling than those with higher income. These findings are similar to those found for nutrition counseling among adolescents (36), suggesting that health providers might perceive low income young adults as having less access to health services, good nutrition and adequate exercise.
This was the first study to examine factors that influence the receipt of three key preventive interventions to improve cardiovascular health in young adults: Cholesterol screening, diet counseling, and exercise counseling. The rate of cholesterol screening was 2-3 times higher than diet counseling and exercise counseling. This likely reflects the practice of universal cholesterol screening in adults above the age of 20 every 5 years according to current guidelines (25, 30), while there is insufficient evidence to recommend for or against routine behavioral counseling to promote a healthy diet or physical activity in primary care settings (30).
We found that racial/ethnic minority young adults were more likely to receive cholesterol screening and diet counseling than Whites, even after adjusting for overweight/obese status. This is consistent with a previous finding with adolescents, with Blacks and Latinos more likely to receive nutrition counseling than Whites (36). Clinicians may perceive that minority patients are more likely to require screening, either because of perceived elevated risk levels or an assumption of less access to alternative resources for preventive health services (36). Black young adults also reported higher STD screening rates than did White young adults. As the incidence of STD is highest among Black young adults (37), it may be appropriate that Black young adults were more likely than White young adults to report higher rates of screening.
Consistent with findings from a previous study of emotional health screening using CHIS adolescent data (38), we found that female young adults were more likely to report receiving emotional health screening than males. While the prevalence of major depressive disorder in female young adults is twice of male young adults (39), it is unclear whether female young adults are more likely to initiate a discussion about their emotions, or health providers are more likely to screen females for emotional distress.
Limitations
Although CHIS is the largest state population health survey, the data is cross-sectional and limits our ability to establish causality. As CHIS surveys adults who reside in households, this data does not reflect the receipt of preventive services among young adults who live in college dormitories or on military bases. In addition, while patient report has been shown to be a valid indicator of service delivery (16-20), self-report data is an individual’s “estimate” of past events, which may be biased by the way an individual recalls events (40). The interpretation of the variable usual source of care is imperfect in that we do not know whether it means a health provider, a health clinic or frequent visits with a particular provider or clinic.
Finally, the emotional health screening variable has a non-specific time-frame as it assessed whether young adults received screening “at the last routine exam”.
Conclusions
Young adults have high prevalence of risk behavior, morbidity and mortality, but low utilization of preventive care. Our findings indicate that beyond access to health insurance, having a usual source of care facilitates the receipt of a broad range of preventive care. The ACA enables a greater number of young adults to obtain health insurance and preventive services; however, while multiple professional organizations have established guidelines in many of the preventive areas, there are no uniformly endorsed preventive guidelines to inform the care of this age group (6). Efforts are needed to develop guidelines for young adults to increase the delivery of preventive care to this age group, and to address the gender and ethnic/racial disparities in preventive services delivery.
Acknowledgement
The development of this paper was supported by grants from the Maternal and Child Health Bureau, Health Resources and Services Administration, U.S. Department of Health and Human Services (U45MC 00002 & U45MC 00023). Dr. Lau was primarily responsible for the conceptualization of the study and the writing of the manuscript, and the analysis and interpretation of data. Dr. Ozer was primarily responsible for the conceptualization of the study the editing and critical revision of the manuscript, and the interpretation of the data. Drs. Irwin and Adams contributed to the conceptualization of the study, analysis and interpretation of data, and revision of the manuscript.
Abbreviations
- ACA
Patient Protection and Affordable Care Act of 2010
- AMA
American Medical Association
- AAP
American Academy of Pediatrics
- NAMCS
National Ambulatory Medical Care Survey
- NHAMCS
National Hospital Ambulatory Care Survey
- STD
sexually-transmitted disease
- CHIS
California Health Interview Survey
- FPL
Federal poverty level
- BMI
Body mass index
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Household income was reported as a percent of the federal poverty level, which was $19,350 and $20,650 for a four-person family in 2005 and 2007, respectively.
Contributor Information
Josephine S. Lau, University of California, San Francisco.
Sally H. Adams, University of California, San Francisco.
Charles E. Irwin, Jr., University of California, San Francisco.
Elizabeth M. Ozer, University of California, San Francisco.
References
- 1.Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Arch Gen Psychiatry. 2009 Jul;66(7):764–72. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harris KM, Gordon-Larsen P, Chantala K, Udry JR. Longitudinal trends in race/ethnic disparities in leading health indicators from adolescence to young adulthood. Arch Pediatr Adolesc Med. 2006 Jan;160(1):74–81. doi: 10.1001/archpedi.160.1.74. [DOI] [PubMed] [Google Scholar]
- 3.McCracken M, Jiles R, Blanck HM. Health behaviors of the young adult U.S. population: Behavioral risk factor surveillance system, 2003. Prev Chronic Dis. 2007 Apr;4(2):A25. [PMC free article] [PubMed] [Google Scholar]
- 4.Mulye TP, Park MJ, Nelson CD, Adams SH, Irwin CE, Jr, Brindis CD. Trends in adolescent and young adult health in the United States. J Adolesc Health. 2009 Jul;45(1):8–24. doi: 10.1016/j.jadohealth.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 5.Park MJ, Brindis CD, Chang F, Irwin CE., Jr A midcourse review of the healthy people 2010: 21 critical health objectives for adolescents and young adults. J Adolesc Health. 2008 Apr;42(4):329–34. doi: 10.1016/j.jadohealth.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 6.Ozer EM, Urquhart J, Brindis C, Park J, Irwin CE., Jr Young adult preventive health guidelines: There but can’t be found. Arch Pediatr Adolesc Med. 2011 doi: 10.1001/archpediatrics.2011.794. In press. [DOI] [PubMed] [Google Scholar]
- 7.Nicholson JL, Collins SR, Mahato B, Gould E, Scheon C, Rustgi S. Rite of passage? Why young adults become uninsured and how new policies can help, 2009 update. The Commonwealth Fund. 2009 Aug; [PubMed] [Google Scholar]
- 8.English A. The Patient Protection and Affordable Care Act of 2010: How does it help adolescents and young adults. National Adolescent Health Information and Innovation Center; Center for Adolescent Health and the Law; and San Francisco, CA: 2010. Chapel Hill, NC. [Google Scholar]
- 9.Koh HK, Sebelius KG. Promoting prevention through the Affordable Care Act. N Engl J Med. 2010 Sep 30;363(14):1296–9. doi: 10.1056/NEJMp1008560. [DOI] [PubMed] [Google Scholar]
- 10.Brown DW, Giles WH, Greenlund KJ, Croft JB. Disparities in cholesterol screening: Falling short of a national health objective. Prev Med. 2001 Dec;33(6):517–22. doi: 10.1006/pmed.2001.0928. [DOI] [PubMed] [Google Scholar]
- 11.Corbie-Smith G, Flagg EW, Doyle JP, O’Brien MA. Influence of usual source of care on differences by race/ethnicity in receipt of preventive services. J Gen Intern Med. 2002 Jun;17(6):458–64. doi: 10.1046/j.1525-1497.2002.10733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: Insurance status and usual source of care. Am J Public Health. 2003 May;93(5):786–91. doi: 10.2105/ajph.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Finkelstein MM. Preventive screening. What factors influence testing? Can Fam Physician. 2002 Sep;48:1494–501. [PMC free article] [PubMed] [Google Scholar]
- 14.Callahan ST, Cooper WO. Changes in ambulatory health care use during the transition to young adulthood. J Adolesc Health. 2010 May;46(5):407–13. doi: 10.1016/j.jadohealth.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 15.Fortuna RJ, Robbins BW, Halterman JS. Ambulatory care among young adults in the United States. Ann Intern Med. 2009 Sep 15;151(6):379–85. doi: 10.7326/0003-4819-151-6-200909150-00002. [DOI] [PubMed] [Google Scholar]
- 16.Haddock CK, Poston WS, Pyle SA, Klesges RC, Vander Weg MW, Peterson A, et al. The validity of self-rated health as a measure of health status among young military personnel: Evidence from a cross-sectional survey. Health Qual Life Outcomes. 2006 Aug 29;4:57. doi: 10.1186/1477-7525-4-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klein JD, Allan MJ, Elster AB, Stevens D, Cox C, Hedberg VA, et al. Improving adolescent preventive care in community health centers. Pediatrics. 2001 Feb;107(2):318–27. doi: 10.1542/peds.107.2.318. [DOI] [PubMed] [Google Scholar]
- 18.Roberts RO, Bergstralh EJ, Schmidt L, Jacobsen SJ. Comparison of self-reported and medical record health care utilization measures. J Clin Epidemiol. 1996 Sep;49(9):989–95. doi: 10.1016/0895-4356(96)00143-6. [DOI] [PubMed] [Google Scholar]
- 19.Ozer EM, Adams SH, Lustig JL, Millstein SG, Camfield K, El-Diwany S, et al. Can it be done? Implementing adolescent clinical preventive services. Health Serv Res. 2001 Dec;36(6 Pt 2):150–65. [PMC free article] [PubMed] [Google Scholar]
- 20.Ozer EM, Adams SH, Lustig JL, Gee S, Garber AK, Gardner LR, et al. Increasing the screening and counseling of adolescents for risky health behaviors: A primary care intervention. Pediatrics. 2005 Apr;115(4):960–8. doi: 10.1542/peds.2004-0520. [DOI] [PubMed] [Google Scholar]
- 21.Callahan ST, Cooper WO. Uninsurance and health care access among young adults in the United States. Pediatrics. 2005 Jul;116(1):88–95. doi: 10.1542/peds.2004-1449. [DOI] [PubMed] [Google Scholar]
- 22.California Health Interview Survey. Methodology series: Report 4. 2009 Mar; [Google Scholar]
- 23.Center for Disease Control and Prevention [Accessed May 10, 2011];Overweight and obesity website. Available at: http://www.cdc.gov/obesity.
- 24.StataCorp . Stata statistical software: Release 11. StataCorp LP; College Station, TX: 2009. [Google Scholar]
- 25.National Cholesterol Education Program. National Heart, Lung, and Blood Institute. National Institute of Health; 2001. Third report of the expert panel on detection, evaluation, and treatment of the high blood cholesterol in adults (adult treatment panel III) Report No.: 01-3670. [Google Scholar]
- 26.Devoe JE, Tillotson CJ, Wallace LS, Lesko SE, Pandhi N. Is health insurance enough? A usual source of care may be more important to ensure a child receives preventive health counseling. Matern Child Health J. 2011 Mar 4; doi: 10.1007/s10995-011-0762-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cooley WC, Sagerman PJ. American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians, Transitions Clinical Report Authoring Group. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011 Jul;128(1):182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- 28.Strickland BB, Singh GK, Kogan MD, Mann MY, van Dyck PC, Newacheck PW. Access to the medical home: New findings from the 2005-2006 national survey of children with special health care needs. Pediatrics. 2009 Jun;123(6):e996–1004. doi: 10.1542/peds.2008-2504. [DOI] [PubMed] [Google Scholar]
- 29.Sexually transmitted diseases treatment guidelines. Centers for Disease Control and Prevention; Atlanta: U.S.: 2010. [Google Scholar]
- 30.Recommendations. U.S. Preventive Services Task Force; [Accessed May 10, 2011]. Available at: http://www.uspreventiveservicestaskforce.org/recommendations.htm. [Google Scholar]
- 31.Irwin CE., Jr Young adults are worse off than adolescents. J Adolesc Health. 2010 May;46(5):405–6. doi: 10.1016/j.jadohealth.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 32.Marcell AV, Ford CA, Pleck JH, Sonenstein FL. Masculine beliefs, parental communication, and male adolescents’ health care use. Pediatrics. 2007 Apr;119(4):e966–75. doi: 10.1542/peds.2006-1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marcell AV, Klein JD, Fischer I, Allan MJ, Kokotailo PK. Male adolescent use of health care services: Where are the boys? J Adolesc Health. 2002 Jan;30(1):35–43. doi: 10.1016/s1054-139x(01)00319-6. [DOI] [PubMed] [Google Scholar]
- 34. [Accessed May 10, 2011];Advisory committee for immunization practices (ACIP) general recommendations on immunizations. Available from: http://www.cdc.gov/vaccines/pubs/ACIP-list.htm.
- 35.Hagan JF, Shaw J, Duncan P. Bright futures: Guidelines for health supervision of infants, children and adolescents. 2008 [Google Scholar]
- 36.Adams SH, Husting S, Zahnd E, Ozer EM. Adolescent preventive services: Rates and disparities in preventive health topics covered during routine medical care in a California sample. J Adolesc Health. 2009 Jun;44(6):536–45. doi: 10.1016/j.jadohealth.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sexually transmitted disease surveillance. Centers for Disease Control and Prevention; Atlanta: U.S.: 2009. [Google Scholar]
- 38.Ozer EM, Zahnd EG, Adams SH, Husting SR, Wibbelsman CJ, Norman KP, et al. Are adolescents being screened for emotional distress in primary care? J Adolesc Health. 2009 Jun;44(6):520–7. doi: 10.1016/j.jadohealth.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 39.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005 Jun;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 40.Kimberlin CL, Winterstein AG. Validity and reliability of measurement instruments used in research. Am J Health Syst Pharm. 2008 Dec 1;65(23):2276–84. doi: 10.2146/ajhp070364. [DOI] [PubMed] [Google Scholar]