Abstract
A 76-year-old woman with hepatitis C cirrhosis presented with tarry stools and hematemesis. An endoscopy demonstrated bleeding duodenal varices in the second portion of the duodenum. Contrast-enhanced computed tomography revealed markedly tortuous varices around the wall in the duodenum. Several afferent veins appeared to have developed, and the right ovarian vein draining into the inferior vena cava was detected as an efferent vein. Balloon-occluded retrograde transvenous obliteration (BRTO) of the varices using cyanoacrylate was successfully performed in combination with the temporary occlusion of the portal vein. Although no previous publications have used cyanoacrylate as an embolic agent for BRTO to control bleeding duodenal varices, this strategy can be considered as an alternative procedure to conventional BRTO using ethanolamine oleate when numerous afferent vessels that cannot be embolized are present.
Keywords: Bleeding duodenal varices, Balloon-occluded retrograde transvenous obliteration, Cyanoacrylate, Combination therapy, Temporary portal vein occlusion
INTRODUCTION
Bleeding duodenal varices is a rare complication in patients with portal hypertension, occurring in only 0.4% of these patients, and is often life-threatening because of the difficulty in diagnosis and treatment[1]. Treatment options include a surgical procedure, endoscopic treatment[2], and endovascular treatment, including transjugular intrahepatic portosystemic shunts (TIPS)[3,4] and balloon-occluded retrograde transvenous obliteration (BRTO)[5-10]. Although several studies have reported successful results using BRTO alone[5-8], some difficult cases with large varices or numerous collaterals requiring a combined approach have been reported[7,9], and no previous publications have used cyanoacrylate as an embolic agent for BRTO to control bleeding duodenal varices. We herein report a case with bleeding duodenal varices that were successfully embolized using cyanoacrylate and BRTO in combination with temporary occlusion of the portal vein.
CASE REPORT
A 76-year-old woman with liver cirrhosis secondary to hepatitis C presented with tarry stools and hematemesis. An urgent endoscopy demonstrated bleeding varices in the second portion of the duodenum (Figure 1A). She had no esophageal or gastric varices. Although banding and clipping for the varices was attempted, the bleeding continued and frequent blood transfusions were required. Laboratory findings were as follows: red blood cell, 232 × 104/μL; hemoglobin, 6.8 g/dL; hematocrit, 20.4%; platelets, 96 000/mL; total bilirubin, 1.36 mg/dL; serum albumin, 3.3 g/dL; and prothrombin time, 15.7 s (reference, 11.3 s). Neither ascites nor encephalopathy was observed. Child-Pugh’s classification was graded as B. Contrast-enhanced computed tomography (CT) revealed markedly tortuous varices around the wall in the second and third portion of the duodenum (Figure 1B). Several afferent veins of the varices appeared to have developed, and the right ovarian vein draining into the inferior vena cava was detected as an efferent vein. We planned BRTO to embolize the duodenal varices after obtaining informed consent from the patient.
Figure 1.
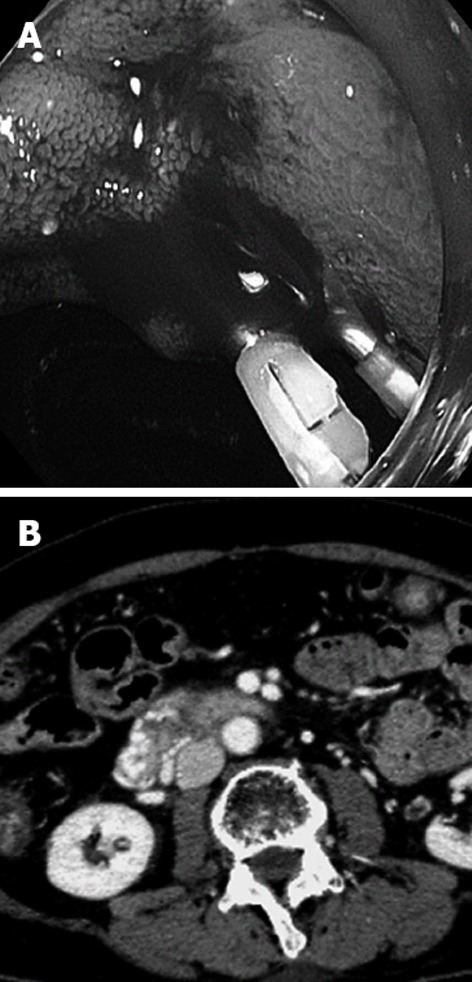
Endoscopy and computed tomography of the duodenum. A: Endoscopy demonstrates bleeding varices in the second portion of the duodenum; B: Contrast-enhanced computed tomography reveals markedly tortuous varices around the wall in the second and third portion of the duodenum.
An 8-French guiding sheath introducer was inserted into the inferior vena cava via the right internal jugular vein. A 5.2-French, 9-mm cobra-shaped balloon catheter was inserted into the efferent vein through the right ovarian vein, and the balloon was inflated to occlude the efferent vein. Balloon-occluded retrograde venography (BRTV) showed that the dilated efferent vein and the duodenal varices were filled with contrast material, but the contrast material quickly disappeared through several afferent veins (Figure 2A). Because BRTO alone may have failed to achieve adequate sclerosant accumulation because of the leakage into the portal vein, antegrade transhepatic embolization of the afferent veins was attempted.
Figure 2.
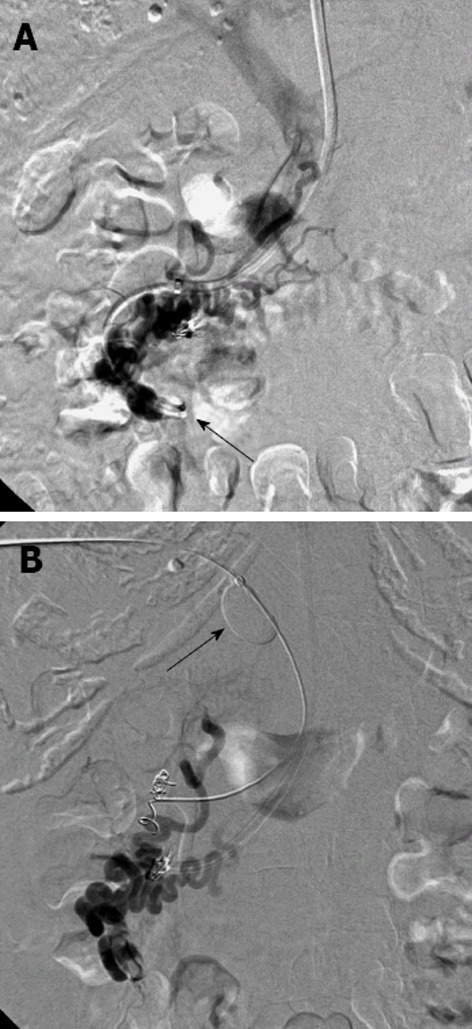
Balloon-occluded retrograde venography. A: Balloon-occluded retrograde venography (BRTV) shows the dilated efferent vein and the duodenal varices, but the contrast material quickly disappears through several afferent veins. Note that the balloon was inflated in the right ovarian vein (arrow); B: BRTV with occlusion of the main portal trunk (arrow) after embolization of one of the afferent veins reveals the complete opacification of the duodenal varices.
A 5-French sheath introducer was inserted through the left lateral portal branch, and one of the afferent veins was embolized using two microcoils (MicroNester coil; Cook, Inc, Bloomington, Indiana, United States). However, several remaining afferent veins could not be embolized, and the contrast material also disappeared through the afferent veins. We then placed a balloon catheter into the main portal trunk to control the hepatopetal flow of the afferent veins. BRTV with occlusion of the main portal trunk revealed the disappearance of the hepatopetal portal flow and complete opacification of the duodenal varices (Figure 2B). A microcatheter was coaxially advanced to the duodenal varices through the retrograde route, and a total of 4 mL of 20% cyanoacrylate with ethiodized oil was injected into the duodenal varices (Figure 3).
Figure 3.

Radiograph after embolization of the duodenal varices demonstrates complete and adequate accumulation of the ethiodized oil in the varices.
The following day, a contrast-enhanced CT examination confirmed the complete accumulation of the ethiodized oil replacement in the duodenal varices (Figure 4) and the patency of either portal vein or systemic circulation. Liver function was preserved after the procedure. Four days after the procedure, an endoscopy showed that hemostasis of the bleeding duodenal varices had been achieved. No evidence of bleeding of the duodenal varices was found on follow-up CT and endoscopy examinations performed four months after the procedure.
Figure 4.
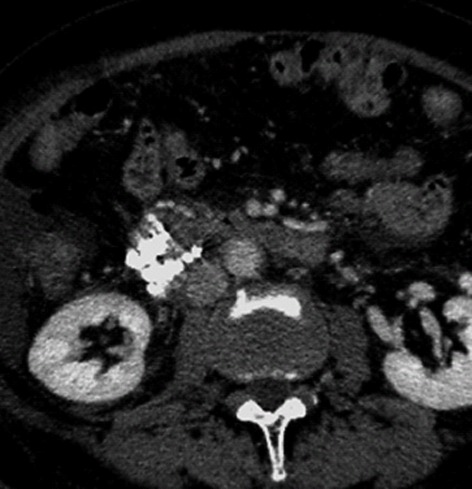
Contrast-enhanced computed tomography after embolization of the duodenal varices shows the complete accumulation of ethiodized oil in the varices.
DISCUSSION
BRTO is an established endovascular treatment for gastric varices[11] but has only been described for the treatment of bleeding duodenal varices in a few reports with limited numbers of clinical patients[5-10]. The advantages of BRTO over TIPS for duodenal varices are that it can completely embolize targeted varices and that it does not reduce portal flow, avoiding further exacerbation of hepatic function and encephalopathy without a significant mortality rate[4,8]. However unlike gastric varices, successful treatment with BRTO alone for duodenal varices is not always feasible and often require combined therapies with an endoscopic or anterograde transhepatic approach, as significant communications or complex hemodynamics between the efferent and afferent veins often complicate treatment and necessitate combined therapy[7,9].
In the present case, some of the afferent veins may have enabled collateral hepatopetal flow during balloon occlusion of the afferent vein, and pressure among the duodenal varices varied, resulting in insufficient filling with the contrast material. At first, coil embolization was attempted via a transhepatic portal venous approach, as reported by previous investigators[5,7-9], but not all the afferent veins could be embolized because of the difficulty in catheterizing the tortuous vessels. Second, we performed temporary balloon occlusion of the portal vein. This method was effective because a change in the hemodynamics of the duodenal varices occurred. Temporary occlusion of the main portal trunk may increase the pressure of hepatopetal flow, and the direction of flow in the afferent veins changes from hepatopetal to hepatofugal. This mechanism is similar to that of temporary balloon occlusion of the splenic artery during BRTO for gastric varices to control the portal pressure gradient[12].
In our case, we used cyanoacrylate, not ethanolamine oleate, as a sclerosant. Every investigator has used ethanolamine oleate as the most suitable sclerosant during BRTO for duodenal varices[5-10]. However, ethanolamine oleate was not suitable in our case, because it requires several hours to achieve full effort and may increase the risk of portal venous thrombosis under temporary portal venous balloon occlusion. On the other hand, cyanoacrylate rapidly solidifies with fast polymerization upon exposure to an ionic solution[13], and we believe that this was the best way of minimizing the duration of portal venous occlusion. The potential shortcomings of cyanoacrylate are adhesion to the balloon catheter system or inadvertent embolization upon balloon removal. This should be kept in mind as a note of caution whenever attempting to use cyanoacrylate. To prevent this complication, it would be advantageous to ensure that a microcatheter is advanced to the targeted duodenal varices and only duodenal varices are embolized, with minimal volume of cyanoacrylate.
Endoscopic injection sclerotherapy using cyanoacrylate has been performed as an effective measure[2], but it has the drawback of perforation, tissue injury, and unclear visualization because of massive hemorrhage. Moreover, endoscopic injection of cyanoacrylate also carries a risk of embolism of either portal vein or systemic circulation[14]. Endovascular injection of cyanoacrylate can prevent untargeted embolization such as portal vein or pulmonary artery, confirming the hemodynamics of the duodenal varices using contrast material.
Bleeding duodenal varices is a rare condition that is difficult to diagnose and is potentially life-threatening. BRTO using cyanoacrylate was successfully performed for control of bleeding duodenal varices in the present case. This is an alternative procedure to conventional BRTO using ethanolamine oleate when insufficient filling of the varices with sclerosant occurs and several afferent vessels cannot be adequately embolized.
Footnotes
P- Reviewer Rerknimitr R S- Editor Jiang L L- Editor O’Neill M E- Editor Li JY
References
- 1.Hashizume M, Tanoue K, Ohta M, Ueno K, Sugimachi K, Kashiwagi M, Sueishi K. Vascular anatomy of duodenal varices: angiographic and histopathological assessments. Am J Gastroenterol. 1993;88:1942–1945. [PubMed] [Google Scholar]
- 2.Kang HY, Lee WK, Kim YH, Kwon BW, Kang MS, Kim SB, Song IH. Ruptured duodenal varices arising from the main portal vein successfully treated with endoscopic injection sclerotherapy: a case report. Korean J Hepatol. 2011;17:152–156. doi: 10.3350/kjhep.2011.17.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lopera JE, Arthurs B, Scheuerman C, Sandoz C, Petersosn S, Castaneda-Zuniga W. Bleeding duodenal: varices treatment by TIPS and transcatheter embolization. Cardiovasc Intervent Radiol. 2008;31:431–434. doi: 10.1007/s00270-004-0161-y. [DOI] [PubMed] [Google Scholar]
- 4.Kim MJ, Jang BK, Chung WJ, Hwang JS, Kim YH. Duodenal variceal bleeding after balloon-occluded retrograde transverse obliteration: treatment with transjugular intrahepatic portosystemic shunt. World J Gastroenterol. 2012;18:2877–2880. doi: 10.3748/wjg.v18.i22.2877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haruta I, Isobe Y, Ueno E, Toda J, Mitsunaga A, Noguchi S, Kimura T, Shimizu K, Yamauchi K, Hayashi N. Balloon-occluded retrograde transvenous obliteration (BRTO), a promising nonsurgical therapy for ectopic varices: a case report of successful treatment of duodenal varices by BRTO. Am J Gastroenterol. 1996;91:2594–2597. [PubMed] [Google Scholar]
- 6.Ohta M, Yasumori K, Saku M, Saitsu H, Muranaka T, Yoshida K. Successful treatment of bleeding duodenal varices by balloon-occluded retrograde transvenous obliteration: a transjugular venous approach. Surgery. 1999;126:581–583. [PubMed] [Google Scholar]
- 7.Ota K, Okazaki M, Higashihara H, Kokawa H, Shirai Z, Anan A, Kitamura Y, Shijo H. Combination of transileocolic vein obliteration and balloon-occluded retrograde transvenous obliteration is effective for ruptured duodenal varices. J Gastroenterol. 1999;34:694–699. doi: 10.1007/s005350050321. [DOI] [PubMed] [Google Scholar]
- 8.Sonomura T, Horihata K, Yamahara K, Dozaiku T, Toyonaga T, Hiroka T, Sato M. Ruptured duodenal varices successfully treated with balloon-occluded retrograde transvenous obliteration: usefulness of microcatheters. AJR Am J Roentgenol. 2003;181:725–727. doi: 10.2214/ajr.181.3.1810725. [DOI] [PubMed] [Google Scholar]
- 9.Zamora CA, Sugimoto K, Tsurusaki M, Izaki K, Fukuda T, Matsumoto S, Kuwata Y, Kawasaki R, Taniguchi T, Hirota S, et al. Endovascular obliteration of bleeding duodenal varices in patients with liver cirrhosis. Eur Radiol. 2006;16:73–79. doi: 10.1007/s00330-005-2781-2. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka O, Ohno K, Ohno T, Tomioka H, Shimizu S, Yamagami T, Nishimura T. Should balloon-occluded retrograde transvenous obliteration be the first-line interventional radiologic treatment for bleeding duodenal varices? A case report and review of the literature. Acta Radiol. 2008;49:32–36. doi: 10.1080/02841850701633049. [DOI] [PubMed] [Google Scholar]
- 11.Fukuda T, Hirota S, Sugimoto K, Matsumoto S, Zamora CA, Sugimura K. “Downgrading” of gastric varices with multiple collateral veins in balloon-occluded retrograde transvenous obliteration. J Vasc Interv Radiol. 2005;16:1379–1383. doi: 10.1097/01.RVI.0000175336.05823.eb. [DOI] [PubMed] [Google Scholar]
- 12.Kiyosue H, Tanoue S, Kondo Y, Maruno M, Takaji R, Matsuoto S, Ueda S, Mori H. Balloon-occluded retrograde transvenous obliteration of complex gastric varices assisted by temporary balloon occlusion of the splenic artery. J Vasc Interv Radiol. 2011;22:1045–1048. doi: 10.1016/j.jvir.2010.12.028. [DOI] [PubMed] [Google Scholar]
- 13.Pollak JS, White RI. The use of cyanoacrylate adhesives in peripheral embolization. J Vasc Interv Radiol. 2001;12:907–913. doi: 10.1016/s1051-0443(07)61568-1. [DOI] [PubMed] [Google Scholar]
- 14.Miyakoda K, Takedatsu H, Emori K, Inoue H, Toyonaga A, Mitsuyama K, Tsuruta O, Sata M. N-butyl-2-cyanoacrylate (histoacryl) glue in the right atrium after endoscopic injection for a ruptured duodenal varix: complication of histoacryl injection. Dig Endosc. 2012;24:192. doi: 10.1111/j.1443-1661.2011.01185.x. [DOI] [PubMed] [Google Scholar]


