Abstract
Objective
The paper aims to study the prevalence of depression in epileptic children and adolescents by reviewing the existing literature, looking for any association between depression in these children and their demographic or seizure related factors to highlight the potential risk factors for depression in epileptic children.
Methods
A search of MEDLINE, NLM Gateway, Ovid and EMBASE was carried out to study original English language articles published during the last 15 years, focusing on only epileptic children and adolescents, studying of depression as comorbidity of epilepsy, and describing demographic and epilepsy-related factors associated with depression.
Findings
The 11 articles included in this study have reported data on 1095 epileptic children aged 4-19 years old and showed that the prevalence of depression has continued to be very common in epileptic children and adolescents, ranged from 5.2% to 39.6%. On the whole, the findings did not support the presence of an association between depression and demographic or seizure variables in children.
Conclusion
Pediatricians and other physicians working with epileptic children should have a high index of suspicion for depression as a comorbid condition in children with epilepsy. Early diagnosis and more comprehensive packages of care for depression in epileptic children will enable them to have a better quality of life.
Keywords: Children, Adolescents, Depression, Epilepsy, Seizure Variables
Introduction
Epilepsy is one of the common problems in children. The occurrence of two unprovoked seizures more than 24 hours apart could indicate the presence of an epileptic disorder[1]. Most cases of epilepsy are managed efficiently by medication, and afflicted children have normal IQ and are expected to have a normal life. However, these children need to be carefully monitored for psychopathology and learning disability, as both of these are more common in epileptic children than in the general population[1, 2].
Depression is one of the most common psychiatric disorders in epileptic children[3]. The prevalence of depression in the pediatric population according to the Isle of Wight study was 0.2% in 10 year olds and 2% in 14 year olds[4]. More recent studies have reported higher rates of 1-5 percent among children and adolescents[5]. The prevalence of depression among children with epilepsy in different worldwide studies varies from 23% to 33%[6–9]. Psychosocial risk factors of depression in epilepsy include the fear of seizure, perceived stigma, learned helplessness and pessimistic attribution, and decreased social support. Biological risk factors include family history of mood disorder, left sided focus and focus in temporal or frontal lobe[2].
In recent years, diagnosis of depression has changed due to the refinements in the diagnostic criteria of depression in ICD-10 and DSM-IV. According to these criteria symptoms of depression should persist at least for 2 weeks, with core symptoms being present during most days[5]. The diagnosis of depression in children and adolescents is mainly clinical. However many researchers have used various screening tools and rating scales to diagnose and quantify depression. The aim of this study was to evaluate the prevalence of depression in epileptic children and adolescents by reviewing the existing literature. We also compared the findings of those studies indicating an association between depression in epileptic children and their gender, age, type of epilepsy, duration of epilepsy, age of onset and the number of antiepileptic drugs (AED) used. From a clinical perspective, we attempted to highlight the potential risk factors for depression in epileptic children, with a view to increasing the awareness of clinicians, and improving the diagnosis and management of depression among these patients.
Although there are a number of comprehensive review articles on the subject, most of them date back to at least 6 years ago. On the other hand, the changes in the diagnostic criteria of depression since the introduction of ICD-10 and DSM-IV in the mid-1990s, and the introduction of new generations of AEDs within the past 15 years have had a considerable impact on the clinical presentation, diagnosis and management of depression in epileptic children. The study therefore has intended to review the original articles published in the last 15 years in order to reflect recent changes in the prevalence of depression among children with epilepsy.
Subjects and Methods
A search of MEDLINE, NLM Gateway, Ovid and EMBASE was carried out using the keywords epilepsy, epileptic, depression, depress, child, children, adolescent, psychiatric comorbidity and seizure. The search was limited to English language papers published during the last 15 years. The original articles which studied only epileptic children and adolescents, evaluated depression as the comorbidity of epilepsy, and described demographic and epilepsy-related variables associated with depression in epilepsy, were included in this study.
The literature search resulted in 38 studies that met the criteria to varying extents. Initially, 100 studies were identified that addressed depression in individuals with epilepsy. However, 62 studies were excluded as they focused on depression as comorbidity in adults. Of the 38 studies included, those mentioning depression as only a component of the affective or emotional comorbidity of epilepsy - rather than a distinct condition - were excluded. Of the remaining 20 articles, a further 9 were excluded due to being review articles and meta-analyses, leaving 11 articles for final review. The references of the initially qualifying 38 articles were also reviewed in order to find further relevant studies, yielding no new results.
Findings
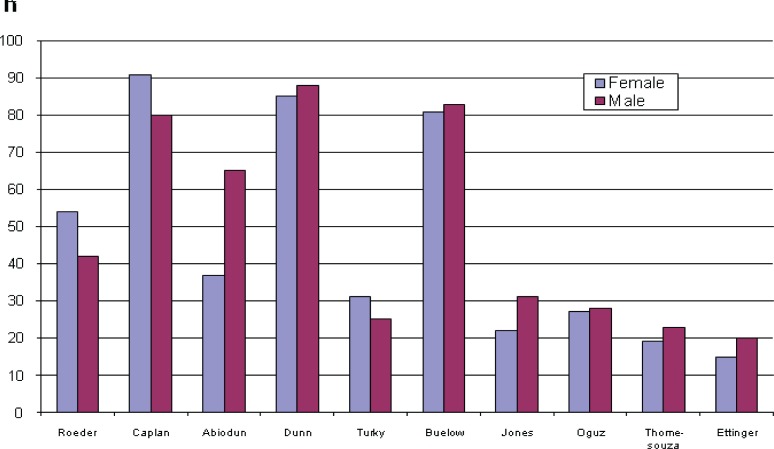
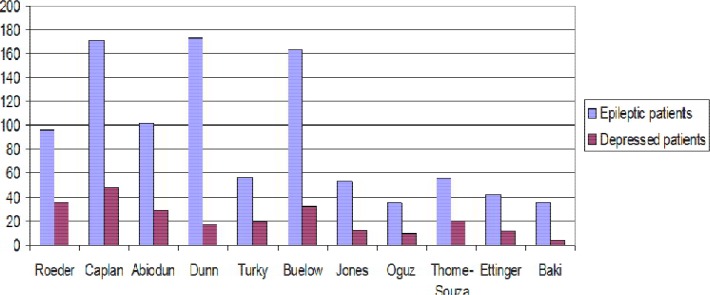
The main 11 articles included in this study reported data on 1095 epileptic children and adolescents aged 4-19 years. All studies were designed as cross-sectional studies, however they were characterized by considerable variability in the population setting and sample sizes (max = 173; min = 35). The number of female and male participants in most studies to be almost similar (Fig 1). Researchers assessed the children by standard measures of depression in child and adolescent according to the Diagnostic and Statistical Manual of Mental Disorders (DSM) or International Classification of Diseases (ICD) criteria. The detailed specific features of the articles are summarized in Table 1. The results are organized into two main categories: firstly the prevalence of depression, and secondly, the factors associated with the development of depression in epilepsy; bearing in mind the interdependence between the two. Prevalence of depression among children with epilepsy: Review of the papers showed that the prevalence of depression among epileptic children and adolescents aged 4-19 years, ranges from 5.2%[10] to 39.6%[11]. The rate of depression in referral centers for epilepsy has been extremely higher in one study[12]. They showed more than 70% of all referred epileptic children have suffered from a psychiatric disorder, with the most common being depression at the rate of 36.4%. Another study[10] showed that most of the depressed children had co-morbidities of disruptive (28%) or anxiety (3.5%) disorders. Children with co-morbid affective/anxiety or disruptive disorders were more likely to suffer from depression than children with only mood disorders. Suicidal ideation among epileptic patients was 20% and 12 times more common in patients with co-morbid anxiety/depressive or disruptive disorders. Interestingly, the rate of depression in epileptic children with or without suicidal ideation was the same[10]. One of the remarkable findings of this review was the results of Turky et al study[11] in 2007. They showed that according to the results of parent-report measures, 39.6% of children with epilepsy were depressed; while based on self-rating scales this rate was 23.1% (Fig. 2).
Fig. 1.
Sample size in 11 studies
Table 1.
Characteristics of the included papers
| Authors: | Roeder | Caplan | Adewuya | Dunn | Turky | Buelow | Jones | Oguz | Thome-Souza | Ettinger | Baki |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Name of the journal and time of publication | Epilepsia 2009 | Epilepsia 2005 | Epilepsy & Behaviour, 2005 | Dev Med Child Neurol,2009 | Epilepsy & Behaviour, 2008 | Dev Med Child Neurol, 2003 | Dev Med Child Neurol, 2007 | J Child Neurol, 2002 | Epilepsy & Behavior, 2004 | Epilepsia, 1998 | Epilepsy & Behavior, 2004 |
| Region | USA | USA | NIGERIA | USA | UK | USA | USA | Turkey | Brazi | USA | Turkey |
| Sample size | 96 | 171 | 102 | 173 | 56 | 164 | 53 | 35 | 55 | 42 | 35 |
| Gender | Female:54 | F :53% | F:37 | M = 88 | M = 25 | M = 83 | M = 31 | Not included | M = 28 | M = 23 | M = 20 |
| Male:42 | M: 47% | M: 65 | F = 85 | F = 31 | F = 81 | F = 22 | F = 27 | F = 19 | F = 15 | ||
| Age(mean) | 11.3 years (6-17) | 10.3 years (5-16) | 14.46 years (12-18) | 11.7 years (9-14) | 12 years (4-17) | 9-14 years | 11.5 years (8-18) | 12.9years (9-18) | 4-18 years | 7-18 years | 7-19 years |
| Rate of depression | 36.5% | 5.2% | 28.43% | 10% | 39.6% | 20% | 22.6% | 28.6% | 36.4%, | 26% | 12% |
| Correlated factors | longer duration of epilepsy, focal seizure, and poly- therapy | Female gender, older patients, and focal seizure (CPS) | poly-therapy | - | female gender, poor control severity of epilepsy | - | Focal seizure | Longer duration of epilepsy, Polytherapy, olde age. | focal seizure, | - | - |
Fig. 2.
The number of depressed cases among epileptic patients
Demographic and epilepsy related factors and depression prevalence: Regarding demographic factors of samples, only two studies found a correlation between gender and the rate of depression[10, 11]. They indicated that females with epilepsy were more likely to have depression than males. Considering the age as a risk factor for developing depression, three studies have stated the tendency to developing depression is higher in epileptic adolescents and older age groups[9, 10, 12]. Epilepsy-related factors including seizure duration, age of onset, type of epilepsy, and the number of AEDs used by epileptic children were studied by reviewing the eleven studies. Only two studies stated longer duration of epilepsy to be a likely correlated factor for developing depression in children[9, 13]. Four studies in this review showed that focal epilepsy was more significantly associated with depression than generalized epilepsy[10, 12–14]. The association between the development of depression in epileptic children and polytherapy with anti-epileptic drugs was found in three studies[9, 13, 15].
Discussion
Clinical investigations and other research studies during the last two decades have revealed that depression is one of the most frequent psychopathologies among epileptic individuals. Moreover, a number of risk factors and comorbid disorders have been found that may impact the rate of depression in epileptic children. The results of the current study show that the prevalence of depression among epileptic children and adolescents ranges from 5.2%[10] to 39.6%[11]. Caplan et al stated that epileptic children have comorbid psychiatric problems, and the prevalence of comorbid depression and disruptive disorders in these patients is 28.5%[10]. The wide range of prevalence and inconsistency of the results may be related to several factors. Firstly, different methods for assessing depression have been used, e.g. structured or semi-structured interviews, self report scales such as CDI, or parent rated measures such as SDQ or DISC-IV (Table 1).
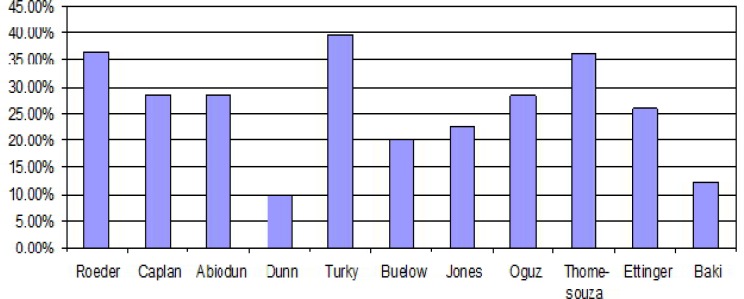
In one study, Turky et al[11] reported the rate of depression according to parent-rated instruments to be 39.6%, whereas in the self report assessments for the same sample it was 23%. This discrepancy could reflect the possibility that some children may not be fully aware of the impact of seizure on their lives. Secondly, different sample sizes - ranging from 35 in some studies[9, 16] to 173 in another[8] - and dissimilar designs of studies, as well as various methods of recruiting of samples could affect the results. Some patients were recruited from community[8] while some others from tertiary or referral centers[12]. Lastly, the time of the study can be important, as the prevalence of depression has increased in parallel with the recent changes in diagnostic criteria of ICD-10 and DMS-IV (Fig. 3). Regarding demo-graphic factors e.g. age and gender of samples, Caplan et al[10] indicated that there has been a tendency for epileptic patients with affective and anxiety disorders to be female (63% vs 43%), however, the correlation was not significant. Turky et al[11] showed that female gender was an independent predictor for depression in epileptic subjects (73.7% vs 26.3%, P=0.04). Although the literature suggests that adolescent girls are athigher risk of depression than boys in general population, this review does not find such an association to be consistent in epileptic children. Some research has shown that psychosocial and behavioral problems are more likely in epileptic girls than boys, especially in adolescents[17]. This seems to be accounted for by girls being more realistic than boys, and boys being usually more optimistic. In adolescents depression and emotional disorders measures are mostly self-rated and based on own perception and self-concept of participants. Therefore, girls may self-score higher than boys on depression assessment.
Fig. 3.
The prevalence of depression in 11 studies
On the whole, this review could not find a correlation between the rate of depression and gender in epileptic individuals.
With regard to age as a risk factor for depression in epileptic children, Caplan et al[10] stated that in epileptic children with anxiety and affective disorders, those with depression were in the older age group; however the relation was not significant. In Oguz et al study[9] depression was significantly more frequent in 12-18 year olds than the 9-11 year old group (P<0.05). Thome-Souze et al[12] showed that depression has been diagnosed in 75% of epileptic adolescents (13-17 years) compared to 25% in epileptic children aged <6 years (P<0.0001). Other studies in this review did not confirm age as a risk factor for depression. Differences between the results of these eleven studies may be related to the use of various measures for depression screening by different researchers. Some studies measured depression using a parent report scale, especially for younger groups. With depressive disorders generally categorized as internalizing conditions, it is likely that parents are not aware of the depressive nature of their children's symptoms. This suggests that children are more accurate reporters of internalizing problems, including depression, than parents.
Seizure-related factors including seizure duration, type of epilepsy, age of onset, and the number of AEDs used by epileptic children were evaluated in all 11 studies, and different results emerged. Considering the duration of epilepsy, Oguz et al[9] indicated that in epileptic children with seizure duration longer than 3 years, depression is more likely to develop (P<0.05). A similar finding by Roeder et al[13] showed that longer duration of epilepsy increased the severity of depressive symptoms. In contrast, Jones et al[14] indicated that children with recent onset epilepsy presented a higher rate of depressive disorders compared to controls (22.6% vs 4%, P=0.01). Some of children with epilepsy (45%) showed some degrees of psychiatric disorders before their first seizure, of which 20.8% had depression. The authors stated that the rate of depression did not differ before and after the presence of seizure, suggesting underlying factors other than chronicity of epilepsy or AEDs may increase the risk of psychopathology. In our review, the association of depression with duration of epilepsy was found to be inconsistent. Several factors including different rating scales and diagnostic measures, different sample sizes and different study designs may have contributed to this discrepancy. Rather uniquely among reviewed studies, Oguz et al divided the cases into two groups according to duration of epilepsy (less than 3 years, and more than 3years), which probably influenced the results and showed a higher rate of depression in the longer duration group.
We could not find any correlation between developing depression and age of onset of seizures in this review. However, studies on population based sample of epileptic children showed that children with early onset epilepsy (<4 years) are more likely to have behavioral problems (P<0.001)[18]. These children did not develope depressive symptoms and their behavioral problems can be explained by long term use of anti-epileptic drugs.
Regarding the association of depression with the type of seizure, Roeder et al showed that diagnosis of focal seizures was correlated with severe depressive symptoms (P<0.05) in 96 participants[13]. Three other studies stated depression and other psychiatric disorders to be more frequent in children with focal seizure[10, 12, 14]. However, the whole results of our review did not support this association, which may reflect different sample sizes and different ages of participants, as well as various methods of measuring depression used by the researchers.
Finally, a few studies showed the association between depression and the number of antiepileptic drugs. Roeder et al[13] stated that greater number of AEDs was independently associated with severe symptoms of depression, suggesting the number of AEDs to be a risk factor for undetected symptoms of depression. Oguz et al[9] stated that depression was significantly higher in patients receiving more than one AED, compared to monotherpay (P<0.05). There are numerous studies in the literature investigating the effect of AEDs on cognitive function or behavior in elipleptic children, although the results are quite contradictory[19]. Establishing an association between AEDs and the symptoms of depression in epileptic children was found to be fraught with difficulties; due to side effects of AEDs immitating the symptoms of depression or behavioral problems, e.g. sleep problems, change in appetite, concentration difficulties or psychomotor retardation[10]. Plioplys[20] stated that the depressogenic effect of AEDs cannot explain development of depression in children per se; suggesting this effect to be related to the side effects of individual drugs. More specifically, Brent et al[21] showed an association between depression and phenobarbital compared to carbamazepine, and demosntrated a much higher prevalence of major depression (40% vs 4%) in epileptic children treated with phenobarbital. Overall, it seems that the effect of AEDs on the development of depression needs further investigation.
Conclusion
In this study we reviewed the original articles published in the past 15 years on the prevalence of depression in epileptic children and adolescents, and its association with demographic and seizure variables. Our study shows that depression continues to be very common in epileptic children and adolescents, indicating that pediatricians and other physicians working with epileptic children should have a high index of suspicion for this comorbid condition. Clearly, better preventive strategies, early diagnosis and more comprehensive packages of care for depression in children with epilepsy will enable them to have a better quality of life.
The results, on the whole, do not support the presence of an association between depression and age, gender, duration of epilepsy, type of epilepsy, time of onset and the number of AEDs used in children and adolescents, although a few studies found a significant association for depression and some of the above mentioned factors. In the last decade newer generation of AEDs with differing side effect profiles, have been used extensively in children. Some of these new AEDs are now used as anti-depressant or anti-anxiety agents in adults but it is not clear how they affect emotional state of epileptic children. Further studies, in particular randomized clinical trials focusing on particular new AEDs are needed to clarify the ambiguities arising from polypharmacy. Uncertainties due to the changing pattern of coping strategies in children, especially during the pre-pubertal and early pubertal period, could be similarly elucidated by studying specific age sub-groups.
Conflict of Interest
None
References
- 1.Johnston MV. Seizure in childhood. In: Vaughan VC, Behrman RE, editors. Nelson Textbook of Pediatrics. 18th ed. Philadelphia: Saunders; 2007. pp. 2457–75. [Google Scholar]
- 2.Gelder M, Harrison P, Cowen P. Shorter Oxford Textbook of Psychiatry. 5th ed. Oxford: Oxford University Press; 2006. [Google Scholar]
- 3.Kanner AM, Dunn DW. Diagnosis and management of depression and psychosis in children and adolescents with epilepsy. J Child Neurol. 2004;19(1):565–72. doi: 10.1177/088307380401900108. [DOI] [PubMed] [Google Scholar]
- 4.Harrington R. Affective disorders. In: Rutter M, Taylor E, editors. Child and Adolescent Psychiatry. 4th ed. Oxford: Blackwell; 2004. [Google Scholar]
- 5.Goodman R, Scott S. Child Psychiatry. 2nd ed. Oxford: Blackwell; 2005. [Google Scholar]
- 6.Ettinger A, Weisbrot D, Nolan E, et al. Symptoms of depression and anxiety in pediatric epilepsy patients. Epilepsia. 1998;39(6):595–9. doi: 10.1111/j.1528-1157.1998.tb01427.x. [DOI] [PubMed] [Google Scholar]
- 7.Rafie H, Alwasha MJ, Hussein B, et al. Symptoms of anxiety and depression among adolescents with seizures in Irbid, Northern Jordan. Seizure. 2000;9(6):412–6. doi: 10.1053/seiz.2000.0427. [DOI] [PubMed] [Google Scholar]
- 8.Dunn D, Austin J, Perkins S. Prevalence of psychopathology in childhood epilepsy: categorical and dimensional measures. Dev Med Child Neurol. 2009;51(5):364–72. doi: 10.1111/j.1469-8749.2008.03172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oguz A, Kurul S, Dirik E, et al. Relationship of epilepsy-related factors to anxiety and depression scores in epileptic children. J Child Neurol. 2002;17(1):37–40. doi: 10.1177/088307380201700109. [DOI] [PubMed] [Google Scholar]
- 10.Caplan R, Siddarth P, Gurbani S, et al. Depression and anxiety disorders in pediatric epilepsy. Epilepsia. 2005;46(5):720–30. doi: 10.1111/j.1528-1167.2005.43604.x. [DOI] [PubMed] [Google Scholar]
- 11.Turky A, Beavis JM, Thapar AK, Kerr MP. Psychopathology in children and adolescents with epilepsy: An investigation of predictive variables. Epilepsy Behav. 2008;12(1):136–44. doi: 10.1016/j.yebeh.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Thome-Souza S, Kuczynski E, Assumpção F, et al. Which factors may play a pivotal role on determining the type of psychiatric disorder in children and adolescents with epilepsy? Epilepsy Behav. 2004;5(6):988–94. doi: 10.1016/j.yebeh.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 13.Roeder R, Roeder K, Asano E, et al. Depression and mental health help-seeking behaviors in a predominantly African American population of children and adolescents with epilepsy. Epilepsia. 2009;50(8):1943–52. doi: 10.1111/j.1528-1167.2009.02046.x. [DOI] [PubMed] [Google Scholar]
- 14.Jones J, Watson R, Sheth R, et al. Psychiatric comorbidity in children with new onset epilepsy. Dev Med Child Neurol. 2007;49(7):493–7. doi: 10.1111/j.1469-8749.2007.00493.x. [DOI] [PubMed] [Google Scholar]
- 15.Adewuya AO, Ola BA. Prevalence of and risk factors for anxiety and depressive disorders in Nigerian adolescents with epilepsy. Epilepsy Behar. 2005;6(3):342–7. doi: 10.1016/j.yebeh.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 16.Baki O, Erdogan A, Kantarci O, et al. Anxiety and depression in children with epilepsy and their mothers. Epilepsy Behav. 2004;5(6):958–64. doi: 10.1016/j.yebeh.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 17.Austin JK, Dunn DW, Huster GA. Childhood Epilepsy and Asthma: changes in behaviour problems related to gender and changes in condition severity. Epilepsia. 2000;41(5):615–23. doi: 10.1111/j.1528-1157.2000.tb00217.x. [DOI] [PubMed] [Google Scholar]
- 18.Høie B, Sommerfelt K, Waaler P, et al. Psychosocial problems and seizure-related factors in children with epilepsy. Devel Med Child Neurol. 2006;48(3):213–6. doi: 10.1017/S0012162206000454. [DOI] [PubMed] [Google Scholar]
- 19.Bourgeois BF. Antiepileptic drugs, learning, and behavior in childhood epilepsy. Epilepsia. 1998;39(9):913–21. doi: 10.1111/j.1528-1157.1998.tb01440.x. [DOI] [PubMed] [Google Scholar]
- 20.Plioplys S. Depression in children and adolescents with epilepsy. Epilepsy Behav. 2003;4(3):39–45. doi: 10.1016/j.yebeh.2003.08.016. [DOI] [PubMed] [Google Scholar]
- 21.Brent DA, Crumrine PK, Varma RR, et al. Phenobarbital treatment and major depressive disorder in children with epilepsy. Pediatrics. 1987;80(6):909–17. [PubMed] [Google Scholar]