Abstract
Objective
Nocturnal enuresis is a common psychosocial concern for both parents and children. In the present study we have determined the prevalence of nocturnal enuresis in Urmia, Iran children and associated personal and familial factors with this problem.
Methods
A cross sectional epidemiological study for detection of nocturnal enuresis prevalence rate and evaluation of associated familial and personal factors in elementary school children (7-11 years old) from Urmia were investigated. The subjects were selected by cluster sampling method. Chi square test and logistic regression were used in univariate and multivariate respectively.
Findings
Of the 1600 questionnaires distributed, 918 (57%) were completed and included in the final analysis. The rest, which were not filled by parents and also those out of our study age range were excluded. Gender of the subjects was almost equally distributed (48.6% males and 51.4% females). Prevalence of nocturnal enuresis was 18.7% (n = 172) and prevalence of day time incontinence was 5.5% (n=51). There was no significant gender difference between these two groups. Enuretics had crowded families, positive family history, low educational level of parents, jobless father, working mother, single parent, poor school performance, positive history of urinary tract infection (UTI).
Conclusion
Our results with enuresis prevalence and associated factors were comparable to other epidemiological studies from various countries. We found that Iranian families do not pay sufficient attention to their enuretic children.
Keywords: Nocturnal enuresis, Diurnal enuresis, Prevalence, Children
Introduction
Nocturnal enuresis can be defined as any intermittent incontinence while asleep in a child being at least five years old[1]. This disorder is a common, genetically complex and heterogeneous problem among children. This clinical problem is an important concern for family because it leads to considerable emotional distress and concern in affected children, their parents and results in some psychological consequences, such as low self–esteem in children, some other psychological problems and specially low school success[2]. Bed wetting can be diagnosed at 5 year-olds and beyond; clinically, it is generally left untreated until the children are 7-8 years old [3].
Most studies have been investigated to find the etiology of enuresis but most of them have found only risk factors for it because this disorder has a multifactorial etiology [4–6].
We conducted a study to estimate the prevalence of nocturnal enuresis in Urmia, Iran. Different associated familial and personal factors with nocturnal enuresis were also studied.
Subjects and Methods
Urmia is a mountainous city located in northwest Iran with a population of about 500000. A sample of 1600 students, 7-11 years old, representative for the primary school population of Urmia were included in the study. The city was classified into different regions. Every region was considered as a cluster. Seven clusters were selected randomly and two schools (a boys’ and a girls’ school) were selected in each cluster randomly. Finally fourteen schools were selected and questionnaires sent to the parents inviting them to come to school on special day after a week. 1142 (71%) of them came and we explained them our questionnaire; at the end, 974 of them filled the questionnaire completely under our supervision. Revising the questionnaires, we excluded children who were out of our age period range. At last 918 (57%) questionnaires were included in the study.
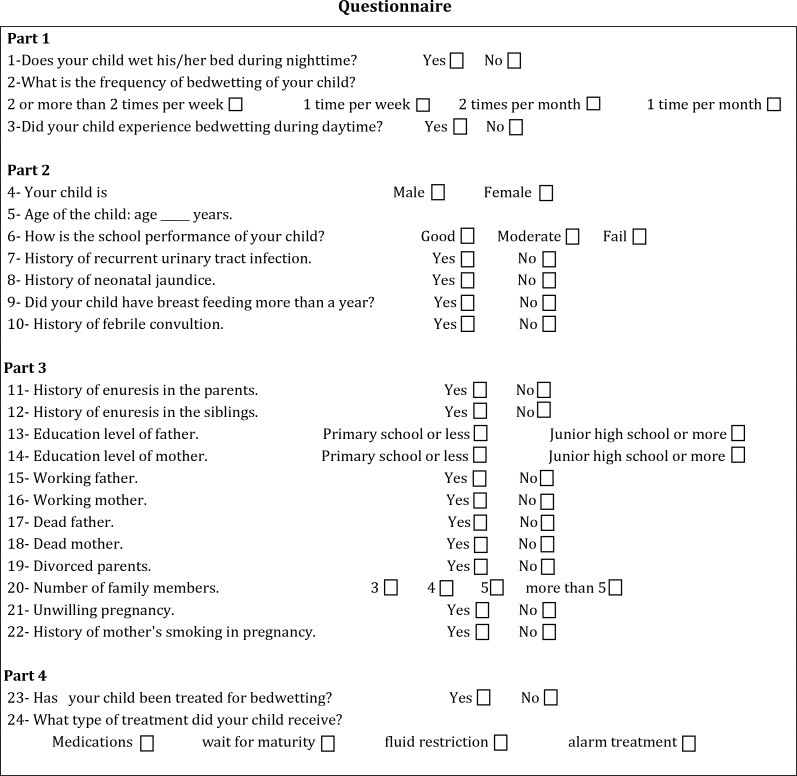
The items of the questionnaire were designed to collect four sections of information about children and their families (Fig. 1). The first section contained questions about the prevalence of enuresis and day time incontinence. Nocturnal enuresis was defined as any intermittent incontinence while asleep in a child being at least five years old, and day time incontinence any intermittent incontinence in day time in the same age range[1]. The second section required information on background data of the child such as age, gender, school performance, history of urinary tract infection (UTI), history of neonatal icterus, breast feeding lasting longer than one year, history of febrile convulsion and birth weight. Educational performance was filled by parents due to elementary education office definition: good, moderate, and fail.
Fig. 1.
Survey questionnaire
The third section was about data of the children's families such as history of enuresis in parents and siblings, parents’ level of education and employment, divorced or dead parents, total number of family members, unplanned pregnancy and mother's smoking. Educational level of parents was divided into two groups: primary school or less as a low educational level and junior high school or more as a high educational level. Mother's smoking was defined as any smoking in pregnancy. Crowded family was defined as having 5 and more members. The fourth section dealt with treatment of enuresis such as visiting a physician and kind of treatment (medication, alarm treatment, fluid restriction and waiting for maturity). All analyses were performed with SPSS for Windows with P<0.05 considered to indicate significant association. Analyses were done by chi-square test for univariate and multivariate analysis, logistic regression to determine the significant predictive factors for nocturnal enuresis.
Findings
Of the 1600 questionnaires distributed, 918 (57%) were included in analysis. These consisted of 453 boys and 465 girls. The overall prevalence of nocturnal and day time incontinence was 18.7% (n=172) and 5.5% (n=51) respectively (Table 1). The mean age was 8.6 in children with nocturnal enuresis and 9.09 in controls. There was a tendency for a steady decrease in the frequency of nocturnal enuresis with increasing age. There was no statistically significant difference in frequency of nocturnal enuresis in the two genders. Table 2 shows the frequency of nocturnal enuresis related to age and sex. Several familial factors that are related to nocturnal enuresis are shown in Table 3. Crowded families, positive family history, low educational level of the parents, jobless father, working mother and single parent (divorced or widowed) were significantly higher in children with enuresis when compared to non-enuretics. Table 4 represents personal factors which were encountered more in enuretic group. Poor school performance, positive history of UTI, not breast feeding, and low birth weight were significantly higher in enuretics when compared to non-enuretics. Unplanned pregnancy, neonatal icterus, febrile convulsion, mother's smoking did not show any increase in enuretics when compared to non-enuretics. The percentage of children with enuresis attending a physician for treatment was 19.8%. Medication was the most (64.5%) preferred treatment for enuresis, waiting for maturity was the least (6.5%) preferred. Table 5 shows logistic regression test to determine the significant predictive factors for nocturnal enuresis.
Table 1.
Prevalence of enuresis
| Type of Enuresis | Boys n (%) | Girls n (%) | Total n (%) |
|---|---|---|---|
| Nocturnal Enuresis | 95 (20.9) | 77 (16.5) | 172 (18.7) |
| Diurnal Enuresis | 14 (3) | 37 (7.9) | 51 (5.5) |
Table 2.
The frequency of nocturnal enuresis in relation to age and gender
| Age (years) | Boys n/N (%)* | Girls n/N (%)* | Total n/N (%)* |
|---|---|---|---|
| 7 | 30/91 (32.9) | 24/91 (26.3) | 54 (31.3) |
| 8 | 21/91 (23) | 14/95 (14.7) | 35 (20.3) |
| 9 | 17/90 (18.8) | 15/92 (16.3) | 32 (18.6) |
| 10 | 14/97 (14.4) | 14/89 (15.7) | 28 (16.2) |
| 11 | 13/84 (15.4) | 10/98 (10.2) | 23 (13.3) |
| Total | 95/453 (20.9) | 77/465 (16.5) | -- |
n=number of enuretic children; N=total number in each age group
percentage in enuretic children
Table 3.
Family factors related to enuresis
| Factors | Enuretics n (%) | Non-enuretics n (%) | P-value | |
|---|---|---|---|---|
| Educational level of mother | Primary school or less | 108 (62.8) | 298 (39.9) | <0.001 |
| Junior high school or more | 64 (37.2) | 448 (60.1) | ||
| Educational level of father | Primary school or less | 83 (48.3) | 225 (30.2) | <0.001 |
| Junior high school or more | 89 (51.1) | 521 (69.8) | ||
| Working Parents | Mother | 70 (40.6) | 260 (34.8) | 0.03 |
| Father | 143 (83.1) | 671 (89.9) | 0.012 | |
| Family history of enuresis | Mother or father enuretic | 53 (30.8) | 68 (9.1) | <0.001 |
| Mother and father non- enuretic | 119 (69.2) | 678 (90.9) | ||
| Sibling enuretic | 54 (31.4) | 53 (7.1) | <0.001 | |
| Sibling non-enuretic | 118 (68.6) | 693 (92.9) | ||
| Divorce | 22 (12.8) | 56 (7.5) | 0.03 | |
| Parent death | 19 (11) | 48 (6.4) | 0.04 | |
| Family number | 3 | 27 (15.7) | 257 (34.5) | <0.001 |
| 4 | 36 (20.9) | 308 (41.3) | ||
| 5 | 59 (34.3) | 120 (16.1) | ||
| More than 5 | 50 (29.1) | 61 (8.2) | ||
| Unwilling pregnancy | 17 (9.9) | 69 (9.2) | NS | |
| Mother smoking | 13 (7.5) | 50 (6.7) | NS | |
NS: Non-significant
Table 4.
Personal factors that were related to enuresis
| Factors | Enuretics N (%) | Non-enuretics N (%) | P Value | |
|---|---|---|---|---|
| School performance | Good | 62 (36) | 575 (77.1) | <0.001 |
| Moderate | 85 (49.4) | 139 (18.6) | ||
| Fail | 25 (14.5) | 32 (4.3) | ||
| History of UTI | 36 (20.9) | 47 (6.3) | <0.001 | |
| History of neonatal icter | 62 (36) | 243 (32.6) | NS | |
| Not Breast feeding | 48 (27.9) | 128 (17.2) | 0.001 | |
| History of febrile Convulsion | 9 (5.2) | 37 (4.6) | NS | |
| Birth weight | < 2500gr | 74 (43) | 208 (27.9) | <0.001 |
| ≥ 2500gr | 98 (57) | 538 (72.1) | ||
NS: Non-significant; UTI: Urinary tract infection
Table 5.
Multivariate analysis to determine the significant predictive factors for nocturnal enuresis
| Factors | Coefficient Regression | P-value | Odd Ratio | 95% Confidence interval |
|---|---|---|---|---|
| Parents’ history of enuresis | 1.44 | <0.001 | 3.14 | 1.93-5.10 |
| Siblings’ history of enuresis | 1.9 | <0.001 | 6.74 | 4.07-11.14 |
| Not Breast feeding | 1.21 | <0.001 | 3.35 | 2.1-5.35 |
| Positive UTI history | 1.07 | <0.001 | 2.92 | 1.6-4.16 |
| Parent death | 0.79 | 0.001 | 2.2 | 1.1-4.1 |
| Not working father | 0.63 | 0.02 | 1.87 | 1.08-3.25 |
| Working mother | 0.76 | 0.001 | 2.14 | 1.35-3.41 |
| Low educational level of father | 0.55 | <0.001 | 3.14 | 1.93-5.1 |
| Low educational level of mother | 0.95 | <0.001 | 2.6 | 1.72-3.93 |
Discussion
This is a population-based study, which was aimed to detect prevalence and risk factors of nocturnal enuresis in Urmia, a city in northwest Iran. We obtained the prevalence of enuresis in 7-11 year-old children as 18.7%. In previous studies from other provinces, the prevalence of enuresis was reported 7.7%[7] and 6.8%[8] which is lower than ours, but in one province it was reported 17.5%[9] which is similar to our study. Also in children of a rural community in southwestern Nigeria and Turkey it has been reported 17.5%[10, 2]. This is similar to our finding.
It is noticeable that the prevalence of nocturnal enuresis has been reported 8% for Taiwan children[11], and 9.2% for Korean children[12]. This difference might be due to sociocultural variations between the countries and regions. Previous studies demonstrated that the prevalence of enuresis tended to decrease with increasingage[2, 4], similarly in the present study, 31.3% of the children were wetting their bed at age 7 whereas 13.3% of them were wetting their bed at age 11. As nocturnal enuresis is mostly expected to improve spontaneously, its decrease with age is thought to be mostly due to spontaneous improvement[4].
In the present study, there was no statistically significant difference in prevalence of nocturnal enuresis between boys and girls (20.9% versus 16.5%). This result is also similar to most reports in the literature[13, 14]. Although in some literature the prevalence of enuresis was more common in boys than in girls [2, 5, 10, 11, 13, 15–20]. The present study showed that some familial factors were significantly associated with nocturnal enuresis.
Enuresis was more frequent among children with positive family history and this is consistent with the literature[2, 4, 5, 11, 20–22]. Some studies have reported parents of enuretics had low educational level[2, 19, 22]. We saw low educational level of fathers in 48.3% and 62.8% in mothers. Working mothers were found to have more enuretic children than housewives. Jobless fathers were seen in 83.1% of enuretics. This was thought to be creating stress in their children. Similar results were seen in school age children in northwest Turkey and Istanbul[4, 13]. Crowded family was another associated familial factor in enuretics. Also increased number of siblings was an effective factor in Turkish children[2] and children in Istanbul[13]. The present results also showed that single parent (divorced or parent death) is an important factor associated with enuresis. Our results correspond with those of the studies in Taiwan and Turkey[2, 11].
The personal factors encountered more in enuretics were: poor school performance, positive history of UTI, not breast feeding, and low birth weight. In our study poor school performance was comparable with other epidemiologic studies from various countries with poor school performance [2, 4, 21, 23]. According to our findings, history of recurrent UTI was significantly associated with enuresis. 20.9% enuretics had positive history of UTI which is similar to that in Turkish and European children[2, 21].
Beside other factors, the role of not breast feeding and low birth weight were found to be important in 27.9% and 43% of the enuretics compared with 17.2% and 27.9% non-enuretics. According to our findings unplanned pregnancy, neonatal icterus, febrile convulsion, or mother's smoking was not increased in enuretics when compared to non-enuretics. In the present study 19.8% (n=13) of the children were seen by a physician similar to that of 17.2% in Turkey[2]. In our study, the most commonly used methods for treatment were medication (64.5%). Also in Turkey[2] the most preferred treatment was medication (59.5%). In contrast, these results were not supported by studies from northwest Turkey[4]. Here only 19.8% of the cases used medication.
As a limitation to the study we did not consider the severity of enuresis and related factors. Furthermore, it is recommended that our findings should be confirmed by further studies with attention to severity factors related to enuresis.
Conclusion
In summary, the prevalence of enuresis in Urmia was similar to studies in other countries having similar socioeconomic status. Our results represented enuresis associated with a lot of personal and familial factors which were comparable to other epidemiologic studies from various countries.
Acknowledgment
This study has been approved and supported by Urmia Medical University.
Conflict of Interest
None
References
- 1.Nevéus T, von Gontard A, Hoebeke P, et al. The standardization of terminology of lower urinary tract function in children and adolescents: report from the standardization committee of the international children's continence society. J Urol. 2006;176(1):314–24. doi: 10.1016/S0022-5347(06)00305-3. [DOI] [PubMed] [Google Scholar]
- 2.Ozden C. L, Ozdal O, Altinova S, et al. Prevalence and Associated Factors of Enuresis in Turkish Children. International Braz J Urol. 2007;33(2):216–22. doi: 10.1590/s1677-55382007000200013. [DOI] [PubMed] [Google Scholar]
- 3.Logan A C, Lesperance F. Primary nocturnal enuresis: omega-3 fatty acids may be of therapeutic value. Med Hypotheses. 2005;64(6):1188–91. doi: 10.1016/j.mehy.2004.11.030. [DOI] [PubMed] [Google Scholar]
- 4.Unalacak M, Söğüt A, Aktunç E, Demircan N, AltIn R. Enuresis nocturnal prevalence and risk factors among school age children in northwest turkey. Eur J Gen Med. 2004;1(3):21–5. [Google Scholar]
- 5.De Sousa A, Kapoor H, Jagtap J, et al. Prevalence and factors affecting enuresis among primary school children. Indian J Urol. 2007;23(4):354–7. doi: 10.4103/0970-1591.36703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howe AC, Walker CE. Behavioral management of toilet training, enuresis and encopresis. Pediatr Clin North Am. 1992;39(3):413–32. doi: 10.1016/s0031-3955(16)38336-5. [DOI] [PubMed] [Google Scholar]
- 7.Azhir A, Frajzadegan Z, Adibi A, et al. An epidemiological study of enuresis among primary school children in Isfahan, Iran. Saudi Med J. 2006;27(10):1572–7. [PubMed] [Google Scholar]
- 8.Safarinejad MR. Prevalence of nocturnal enuresis, risk factors, associated familial factors and urinary pathology among school children in Iran. J Pediatr Urol. 2007;3(6):443–52. doi: 10.1016/j.jpurol.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 9.Ghahramani M, Basirymoghadam M, Ghahramani A. Nocturnal Enuresis and its impact on Growth. Iran J Pediatr. 2008;18(2):167–70. [Google Scholar]
- 10.Osungbade KO, Oshiname FO. Prevalence and perception of nocturnal enuresis in children of a rural community in southwest Nigeria. Trop Doct. 2003;3(4):234–6. doi: 10.1177/004947550303300416. [DOI] [PubMed] [Google Scholar]
- 11.Chang P, Chen WJ, Tsai WY, et al. An epidemiological study of nocturnal enuresis in Taiwanese children. BJU Int. 2001;87(7):678–81. doi: 10.1046/j.1464-410x.2001.02161.x. [DOI] [PubMed] [Google Scholar]
- 12.Lee SD, Sohn DW, Lee JZ, et al. An epidemiological study of enuresis in Korean children. BJU Int. 2000;85(7):869–73. doi: 10.1046/j.1464-410x.2000.00617.x. [DOI] [PubMed] [Google Scholar]
- 13.Gur E, Turhan P, Can G, et al. Enuresis: Prevalence, risk factors and urinary pathology among school children in Istanbul, Turkey. Pediatr Int. 2004;46(1):58–63. doi: 10.1111/j.1442-200X.2004.01824.x. [DOI] [PubMed] [Google Scholar]
- 14.Ozkan KU, Garipardic M, Toktamis A, et al. Enuresis prevalence and accompanying factors in schoolchildren: A questionnaire study from southeast Anatolia. Urol Int. 2004;73(2):149–55. doi: 10.1159/000079696. [DOI] [PubMed] [Google Scholar]
- 15.Serel TA, Akhan G, Koyuncuoğlu HR, et al. Epidemiology of enuresis in Turkish Children. Scand J Urol Nephrol. 1997;31(6):537–9. doi: 10.3109/00365599709030658. [DOI] [PubMed] [Google Scholar]
- 16.Oge O, Kocak I, Gemalmaz H. Enuresis: point prevalence and associated factors among Turkish children. Turk J Pediatr. 2001;43(1):38–43. [PubMed] [Google Scholar]
- 17.Marugan de Miguelsanz JM, Lapena Lopez de Armentia S, et al. An epidemiological analysis of the sequence of bladder control and nocturnal Enuresis prevalence in the children of the province of leÓn. An ESP Pediatr. 1996;44(6):561–7. [PubMed] [Google Scholar]
- 18.Butler RJ, Golding J, Northstone K. ALSPAC Study Team: Nocturnal enuresis at 7.5 years old: prevalence and analysis of clinical signs. BJU Int. 2005;96(3):404–10. doi: 10.1111/j.1464-410X.2005.05640.x. [DOI] [PubMed] [Google Scholar]
- 19.Cher TW, Lin GJ, Hsu KH. Prevalence of nocturnal enuresis and associated familial factors in primary school children in Taiwan. J Urol. 2002;168(3):1142–6. doi: 10.1016/S0022-5347(05)64612-5. [DOI] [PubMed] [Google Scholar]
- 20.Wei Wang Q, Guo Wen J, Kui Song D, et al. Bed-wetting in Chinese children: Epidemiology and predictive factors. Neurourol Urodyn. 2007;26(4):512–7. doi: 10.1002/nau.20373. [DOI] [PubMed] [Google Scholar]
- 21.Inan M, Tokuc B, Y. Aydiner C, et al. Personal characteristics of enuretic children: an epidemiological study from south-east Europe. Urol Int. 2008;81(1):47–53. doi: 10.1159/000137640. [DOI] [PubMed] [Google Scholar]
- 22.Tai HL, Chang YJ, Chang SC, Chen GD, Chang CP, Chou MC. The epidemiology and factors associated with nocturnal enuresis and its severity in primary school children in Taiwan. Acta Paediatr. 2007;96(2):242–5. doi: 10.1111/j.1651-2227.2007.00025.x. [DOI] [PubMed] [Google Scholar]
- 23.Chang SSY, Ng CFN, Wong SN. Hong Kong Childhood Enuresis Study Group: behavioural problems in children and parenting stress associated with primary nocturnal enuresis in Hong Kong. Acta Paediatr. 2002;91(4):475–9. doi: 10.1080/080352502317371742. [DOI] [PubMed] [Google Scholar]