Abstract
Objective
Helicobacter pylori is recognized as a major etiological factor in the pathogenesis of gastritis and peptic ulcer disease. H. Pylori eradication has a failure rate of more than 30% in pediatric patients, particularly because of poor compliance, antibiotic resistance and occurrence of side-effects. This study was aimed to determine whether adding the probiotics to a standard anti-H. pylori regimen could minimize the gastrointestinal side-effect prevalence and improve the eradication rate.
Methods
Double-blind randomized placebo controlled study conducted at Children's Medical Center in Tehran, Iran. Sixty six H. pylori positive children were treated with a triple drug treatment protocol (omeprazole+amoxycillin+furazolidon) and randomly allocated to receive either probiotic or placebo. All patients underwent esophagogastroduodendoscopy. H. pylori infection was diagnosed by either rapid urease test (RUT) or histology. H. pylori status was assessed after 4-8 weeks of the completion of treatment with stool H. pylori antigen test. The side effects of the treatment were determined in each group.
Findings
Mean age of patients was 9.09 (range 3-14) years, 44 (65.7%) patients were boys (sex ratio 2:1). All 66 patients completed the course of treatment and follow-up. The rate of H. pylori eradication was significantly higher in probiotic group (P=0.04). In probiotic supplemented children there was a lower rate of nausea/vomiting (P=0.02) and diarrhea (P=0.039) during treatment.
Conclusion
This study showed that probiotics have positive effect on the eradication of H. pylori infection. Adjuvant therapy with probiotic is recommended in order to reduce the frequency of antibiotic induced side-effects during treatment with antibiotics.
Keywords: Children, Probiotic, Endoscopy, Helicobacter Pylori, Eradication
Introduction
H. pylori is a pathogenic Gram-negative spiral bacillus that survives in the acid environment of the stomach. It is a leading cause of chronic gastritis, peptic ulcers, non-ulcer dyspepsia, gastric adenocarcinoma and mucosa-associated lymphoid tissue (MALT) lymphoma. It is estimated that up to 50% of the total world population are infected with H. pylori. The prevalence of H. Pylori infection is currently rising in the developing world[1–4]. One-week triple therapy (two antibiotics for a week and a Proton Pomp Inhibitors (PPI) for 4-8 weeks) represents the current most widely prescribed first-line regimen for H. pylori infection. With current therapeutic regimens, there is a significant failure rate for the eradication of microorganism. The treatment failure rate is known to be much more common in children than in adult patients (more than 30%)[5–11]. Numerous factors are associated with the high prevalence of treatment failure; the most common are poor compliance and antimicrobial resistance due to overuse or misuse of common antibiotics. Frequent occurrence of side effects of antibiotic drugs can lead to the reduced compliance of patients with therapeutic regimens[12, 13].
Adjuvant therapy with probiotics has been studied in recent years. Probiotics are living or attenuated nonpathogenic microorganisms that have a large variety of potential beneficial effects on the health condition. They have the ability to bind to epithelial cells, survive for a long time in the digestive tract, regulate the immune system and influence metabolic reactions.
The most commonly used probiotics that may increase the resistance of gastric barrier and as a result inhibit the growth of H. pylori and its adherence to gastric epithelium are lactobacilli and bifidobacteria species[3, 14–17].
Considering the rarity of a comprehensive survey on the potential role of adjunctive therapy with probiotics for the treatment of childhood H. pylori infection in our country, we aimed, in this study, to assess the effect of probiotic supplementation as a combination of seven species on the childhood H. Pylori infection. In most previous trials only a few species of probiotics are used.
Subjects and Methods
The study was performed at Children's Medical Center in Tehran, Iran, from November 2011 to April 2012. In a randomized double blind clinical trial, sixty six children aged 3-14 years with H. Pylori infection enrolled in this study. The patients were referred to gastroenterology clinic for the evaluation of symptoms and signs including chronic abdominal pain, gastrointestinal bleeding, unexplained frequent vomiting and unexplained iron deficiency anemia.
Inclusion criterion was the presence of H. pylori infection. Exclusion criteria were as follows: 1) consumption of PPIs, H2 receptor antagonists, bismuth compounds and antibiotics in the previous 2 weeks, 2) previous gastric surgery, 3) known allergy to certain antibiotics, 4)glucose-6-phosphate dehydrogenase (G6PD) enzyme deficiency (furazolidone may cause hemolysis and anemia in these deficient patients), and 5) known previous history of renal failure and endocrine, cardiac, or hepatic disease.
Ethics: The research protocol was approved by the medical ethic committee of Tehran University of Medical Sciences and allocated an ethical code. Registration ID of this study in Iranian Registry of Clinical Trials was IRCT201201218793N1. Informed consent was obtained from parents of all patients.
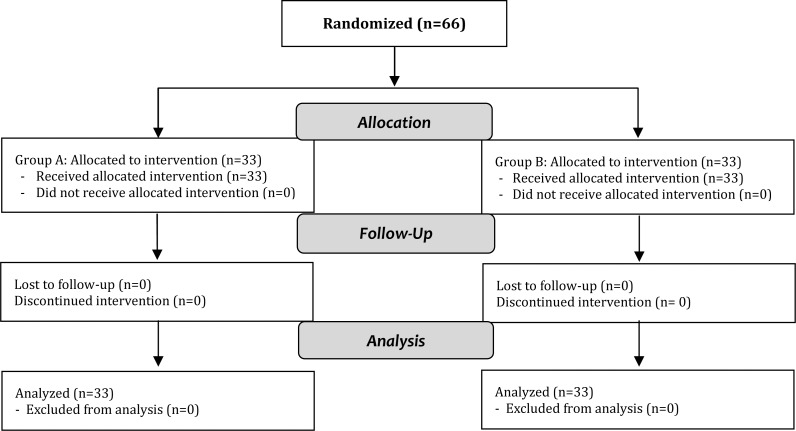
All patients were included for esophagogastroduodenoscopy. H. pylori infection was established by at least one of these criteria: A positive rapid urease test (RUT) or histopathological examination. Upper gastrointestinal endoscopy was carried out after midazolam sedation (0.1 mg/kg). Two pieces of gastric antral biopsy specimens were taken for histology and RUT. Patients were randomly assigned following simple randomization procedures to one of two treatment groups (A: antibiotic+PPI+placebo, B: antibiotic+PPI+ probiotic). Label of drugs was replaced by a new one indicating drug A or B. Contents of sachets were not known to the physician, research fellow, and nurses involved in recording data. All H. pylori positive children in group A were treated with a one-week course of amoxicillin (50 mg/kg/day bid as syrup or capsule) and furazolidone (6 mg/kg/day bid as syrup or tablet), four weeks of omeprazole (1mg/kg/day) plus placebo. Group B received the same antibiotics and PPI plus probiotic preparation 1 sachet/day (restore, 1×109 CFU/1 sachet, Protexin Co, UK). Probiotic combination consisted of strains of Lactobacillus acidophilus, Lactobacillus rhamnosus, Lactobacillus bulgaricus, Lactobacillus casei, Streptococcus thermophilus, Bifidobacterium infantis and Bifidobacterium breve (Fig. 1).
Flow diagram of randomization, allocation, follow-up and analysis
Study design: After endoscopic evaluation and randomization the treatment was started. During the course of treatment and at follow-up, patients were contacted by phone and were asked about the side effects of therapy on a weekly basis. The side effects included diarrhea, nausea/vomiting and abdominal bloating. They had a visit as an outpatient at the middle of therapeutic course. All patients were reinvestigated four to eight weeks after accomplished treatment by stool antigen test for H. pylori. Successful treatment was defined as a negative stool antigen test for H. pylori.
Outcome parameters: Primary outcome measure was the rate of eradication of H. pylori defined as a negative stool antigen test. Secondary outcomes were the rate of side effects during the treatment reported by the patients or parents.
Statistical analysis: The SPSS software version 18 (SPSS Inc., Chicago, IL, USA) was used to appraise the statistical analysis; statistical analytical tests Chi-square or Fisher's exact test and Logistic Regression were used for analyzing data. A P-value of less than 0.05 was considered significant.
Findings
A total of 66 children with H. pylori infection were recruited in the study and randomized into two groups. All 66 patients completed the treatment protocol combined of amoxicillin, furazolidone and omeprazole plus placebo in group A and probiotic in group B. No patient discontinued the treatment and there were no losses to follow-up.
The patient group consisted of 44 (65.7%) males, the male to female ratio was 2:1. Their mean age was 9.09±3.12 years (range 3 to 14 years). Both groups demonstrated improvement in clinical symptoms after treatment. The group treated with the combination of probiotic and standard therapeutic regimen showed more significant eradication rate (Odds Ratio 4.37, Confidence interval: 1.07–17.62, P=0.04)(Table 1).
Table 1.
Comparison of the proportion of patients in two groups with successful eradication
| Stool Antigen | Probiotic+Antibiotic | Placebo+Antibiotic | P. Value |
|---|---|---|---|
| Negative (eradicated) | 30 (90.09%) | 23 (69.69%) | 0.04 |
| Positive (not eradicated) | 3 (9.09%) | 10 (30.30%) |
We found that children receiving probiotic suffered less frequently diarrhea and nausea/vomiting during eradicating treatment; these discrepancies were statistically significant. The difference in the prevalence of abdominal bloating was not significant between the two groups (Table 2). In a subgroup of patients who developed side effects, the symptoms were not severe enough to stop the treatment.
Table 2.
Comparison of the adverse effects during treatment in two enrolled groups
| Side effect | Probiotic+Antibiotic | Placebo+Antibiotic | P. value |
|---|---|---|---|
| Nausea/vomitting (%) | 2 (6.06%) | 9 (27.27%) | 0.02 |
| Diarrhea (%) | 2 (6.06%) | 8 (24.24%) | 0.04 |
| Abdominal bloating (%) | 3 (9.09%) | 4 (12.12%) | 1 |
Table 3 represents the clinical characteristics and endoscopic findings of the studied patients. These percentages are calculated for all enrolled children before randomization and allocation.
Table 3.
Clinical characteristics and endoscopic findings of patients enrolled in the study
| Complaints | Number/percent | Endoscopic Finding | Number/percent |
|---|---|---|---|
| Abdominal pain (%) | 43 (65.15%) | Antral nodularity | 57 (86.36%) |
| Gastrointestinal bleeding (%) | 14 (21.21%) | Gastric erythema | 16 (24.24%) |
| Vomiting (%) | 15 (22.72%) | Duodenal ulcer | 14 (21.21%) |
| Iron deficiency anemia (%) | 4 (6.06%) | Gastric ulcer | 1 (1.51%) |
Discussion
In this randomized, placebo-controlled double blind study, children on H. pylori eradication therapy receiving seven strains of probiotic in addition to the standard triple regimen where compared with patients on the same triple regimen receiving placebo. The findings reported a significant reduction of the treatment complication and improved therapeutic outcome.
New investigations have provided evidence suggesting that probiotics modulate H. pylori colonization of the gastric epithelial cells. It is increasingly known that alterations in the intestinal microflora have an important role for the development of complication and patient's intolerance during anti-H. pylori treatment. Probiotic supplementation could reduce the nondesirable complications of antibiotics and as a result, maximize the success of therapy[18, 19].
Many studies have documented the effectiveness of prophylactic probiotics in association with antibiotics in the modification of H. pylori eradication rate and the antibiotic-associated gastrointestinal side-effects during eradication therapy[5, 20–24]. Certain probiotics such as Lactobacillus strains are known to interfere with the activity of H. pylori by inhibiting its adherence to gastric epithelium and inactivating its main virulence factor, urease enzyme[25, 26].
Park SK et al concluded that combining first line anti H. pylori therapy with probiotic species, composed of Bacillus subtilis and Streptococcus faecium reduced side effects, improved patient's tolerance and enhanced the eradication rate of H. pylori[27]. Similar results were reported by Bekar O et al from Turkey, who investigated the effect of combining standard triple anti H. pylori therapy with kefir, a fermented milk derived product containing probiotics[28]. The results of these two studies confirm our findings. In another study, supplementation of Lactobacillus and Bifidobacterium strains resulted in the modification of stool microflora and enhanced H. pylori clearance[29].
In a randomized trial by Hurduc et al, it was concluded that supplementation of Saccharomyces boulardi to the standard triple drug regimen resulted in a 12% nonsignificant increased therapeutic effect on H. pylori but reduction in the incidence of side effects was significant[30]. The significance of difference in the rate of adverse effects between two groups and higher eradication rate in our survey was in accordance with this study although the latter was statistically significant in our patients.
It is reported that Bifidobacterium bifidum could significantly reduce the rate of gastrointestinal complaints in H. pylori positive patients and modify the activity of organism in the gastric mucusa[31].
To our knowledge, there is only one relevant study in Iranian children with a small sample sizereporting that supplementation with probiotics, could improve drug compliance and reduce side effects without a change in the eradication rate of H. pylori[32]. The profile of adverse effects were similar to our results but this was not true for the eradication rate.
A number of studies have shown no significant discrepancies in the success of H. pylori eradication treatment between the groups receiving probiotics and the peers on placebo[5, 33]. The wide variety and controversial results in previous studies may be attributed to the differences in study design, patient groups, different therapeutic regimens, probiotic dose, and probiotic species.
In our study the rate of H. pylori eradication was significantly higher in patients who received probiotics. In probiotic supplemented children there was a meaningfully lower rate of nausea/vomiting and diarrhea during treatment.
Conclusion
According to the findings of this clinical trial, probiotic supplementation during the treatment for H. pylori eradication, may positively affect antibiotic-related symptoms and treatment success. Further large, randomized, double-blind, placebo-controlled clinical trials must be conducted with minimal variability in study designs, to appropriately evaluate the efficacy of specific probiotic strains in comparison to placebo.
Acknowledgment
This study was approved by Research Committee of Tehran University of Medical Sciences. Registration ID of this study in Iranian Registry of Clinical Trials was IRCT201201218793N1.
Our special thanks go to Mrs. Parizad, Mrs. Madadie, Mrs. Tafreshie and Mrs. Khanjani, proficient nurses of Children's Medical Center Endoscopy Unit for their cooperation.
Conflict of Interest
None
References
- 1.Kusters JG, van Vliet AH, Kuipers EJ. Pathogenesis of Helicobacter pylori infection. Clin Microbiol Rev. 2006;19(3):449–90. doi: 10.1128/CMR.00054-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Imrie C, Rowland M, Bourke B, et al. Is Helicobacter pylori infection in childhood a risk factor for gastric cancer? Pediatrics. 2001;107(2):373–80. doi: 10.1542/peds.107.2.373. [DOI] [PubMed] [Google Scholar]
- 3.Du MQ, Isaccson PG. Gastric MALT lymphoma: from aetiology to treatment. Lancet Oncol. 2002;3(2):97–104. doi: 10.1016/s1470-2045(02)00651-4. [DOI] [PubMed] [Google Scholar]
- 4.Jafar Soltani, Jalil Amirzadeh, Soheila Nahedi, Sirous Shahsavari. Prevalence of helicobacter pylori infection in children, a population-based cross-sectional study in west of Iran. Iran J Pediatr. 2013;23(1):13–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Lionetti E, Miniello VL, Castellaneta SP, et al. Lactobacillus reuteri therapy to reduce side-effects during anti-Helicobacter pylori treatment in children: a randomized placebo controlled trial. Aliment Pharmacol Ther. 2006;24(10):1461–8. doi: 10.1111/j.1365-2036.2006.03145.x. [DOI] [PubMed] [Google Scholar]
- 6.Oderda G, Marinello D, Lerro P, et al. Dual vs. triple therapy for childhood Helicobacter pylori gastritis: a double blind randomized multicentre trial. Helicobacter. 2004;9(4):293–301. doi: 10.1111/j.1083-4389.2004.00242.x. [DOI] [PubMed] [Google Scholar]
- 7.Gessner BD, Bruce MG, Parkinson AJ, et al. A randomized trial of triple therapy for pediatric Helicobacter pylori infection and risk factors for treatment failure in a population with a high prevalence of infection. Clin Infect Dis. 2005;41(9):1261–8. doi: 10.1086/496925. [DOI] [PubMed] [Google Scholar]
- 8.Hasan SR, Vahid V, Reza PM, et al. Short-duration furazolidone therapy in combination with amoxicillin, bismuth subcitrate, and omeprazole for eradication of Helicobacter pylori. Saudi J Gastroenterol. 2010;16(1):14–8. doi: 10.4103/1319-3767.58762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehri N, Kambiz E, Ahmad K, et al. The efficacy of a 1-week triple therapy for eradication of Helicobacter pylori infection in children. Arab J Gastroenterol. 2011;12(1):37–9. doi: 10.1016/j.ajg.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 10.Misiewicz JJ. Management of Helicobacter pylori-related disorders. Eur J Gastroenterol Hepatol. 2012;9(Suppl 1):S17–20. [PubMed] [Google Scholar]
- 11.Gerrits MM, van Vilet AH, Kuipers EJ, et al. Helicobacter pylori and antimicrobial resistance: molecular mechanisms and clinical implications. Lancet Infect Dis. 2006;6(11):699–709. doi: 10.1016/S1473-3099(06)70627-2. [DOI] [PubMed] [Google Scholar]
- 12.Najafi M, Sobhani M, Khodadad A, Farahmand F, Motamed F. Reinfection Rate after Successful Helicobacter pylori Eradication in Children. Iran J Pediatr. 2010;20(1):58–62. [PMC free article] [PubMed] [Google Scholar]
- 13.Szajewska H, Setty M, Mrukowicz J, et al. Probiotics in gastrointestinal diseases in children: hard and not-so-hard evidence of efficacy. J Pediatr Gastroenterol Nutr. 2006;42(5):454–75. doi: 10.1097/01.mpg.0000221913.88511.72. [DOI] [PubMed] [Google Scholar]
- 14.Imase K, Tanaka A, Tokunaga K, et al. Lactobacillus reuteri tablets suppress Helicobacter pylori infection - a double-blind randomized placebo-controlled cross-over clinical study. Kansenshogaku Zasshi. 2007;81(4):387–93. doi: 10.11150/kansenshogakuzasshi1970.81.387. [DOI] [PubMed] [Google Scholar]
- 15.Wang KY, Li SN, Liu CS, et al. Effects of ingesting Lactobacillus- and Bifidobacterium-containing yogurt in subjects with colonized Helicobacter pylori. Am J Clin Nutr. 2004;80(3):737–41. doi: 10.1093/ajcn/80.3.737. [DOI] [PubMed] [Google Scholar]
- 16.Nista EC, Candelli M, Cremonini F, et al. Bacillus clausii therapy to reduce side-effects of anti-Helicobacter pylori treatment: randomized, double-blind, placebo controlled trial. Aliment Pharmacol Ther. 2004;20(10):1181–8. doi: 10.1111/j.1365-2036.2004.02274.x. [DOI] [PubMed] [Google Scholar]
- 17.Hamilton-Miller JM. The role of probiotics in the treatment and prevention of Helicobacter pylori infection. Int J Antimicrob Agents. 2003;22(4):360–6. doi: 10.1016/s0924-8579(03)00153-5. [DOI] [PubMed] [Google Scholar]
- 18.Gotteland M, Andrews M, Toledo M, et al. Modulation of Helicobacter pylori colonization with cranberry juice and Lactobacillus johnsonii La1 in children. Nutrition. 2008;24(5):421–6. doi: 10.1016/j.nut.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 19.Gotteland M, Cruchet S, Brunser O. Can the amount of Helicobacter pylori in the stomach be kept low through probiotic intake? Am J Clin Nutr. 2005;81(4):939–40. doi: 10.1093/ajcn/81.4.939. [DOI] [PubMed] [Google Scholar]
- 20.de Bortoli N, Leonardi G, Ciancia E, et al. Helicobacter pylori eradication: a randomized prospective study of triple therapy versus triple therapy plus lactoferrin and probiotics. Am J Gastroenterol. 2007;102(5):951–6. doi: 10.1111/j.1572-0241.2007.01085.x. [DOI] [PubMed] [Google Scholar]
- 21.Song MJ, Park DI, Park JH, et al. The effect of probiotics and mucoprotective agents on PPI-based triple therapy for eradication of Helicobacter pylori. Helicobacter. 2010;15(3):206–13. doi: 10.1111/j.1523-5378.2010.00751.x. [DOI] [PubMed] [Google Scholar]
- 22.Sýkora J, Valecková K, Amlerová J, et al. Effects of a specially designed fermented milk product containing probiotic Lactobacillus casei DN-114 001 and the eradication of H. pylori in children: a prospective randomized double-blind study. J Clin Gastroenterol. 2005;39(8):692–8. doi: 10.1097/01.mcg.0000173855.77191.44. [DOI] [PubMed] [Google Scholar]
- 23.Sullivan A, Nord CE. Probiotics and gastrointestinal diseases. J Intern Med. 2005;257(1):78–92. doi: 10.1111/j.1365-2796.2004.01410.x. [DOI] [PubMed] [Google Scholar]
- 24.Cruchet S, Obregon MC, Salazar G, et al. Effect of the ingestion of a dietary product containing Lactobacillus johnsonii La1 on Helicobacter pylori colonization in children. Nutrition. 2003;19(9):716–21. doi: 10.1016/s0899-9007(03)00109-6. [DOI] [PubMed] [Google Scholar]
- 25.Lou JG, Chen J, Huang XL, Zhao ZY. Changes in the intestinal microflora of children with Helicobacter pylori infection and after Helicobacter pylori eradication therapy. Chin Med J (Engl) 2007;120(10):929–31. [PubMed] [Google Scholar]
- 26.Huebner ES, Surawicz CM. Probiotics in the prevention and treatment of gastrointestinal infections. Gastroenterol Clin North Am. 2006;35(2):355–65. doi: 10.1016/j.gtc.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 27.Park SK, Park DI, Choi JS, et al. The effect of probiotics on Helicobacter pylori eradication. Hepatogastroenterology. 2007;54(79):2032–6. [PubMed] [Google Scholar]
- 28.Bekar O, Yilmaz Y, Gulten M. Kefir improves the efficacy and tolerability of triple therapy in eradicating Helicobacter pylori. J Med Food. 2011;14(4):344–7. doi: 10.1089/jmf.2010.0099. [DOI] [PubMed] [Google Scholar]
- 29.Sheu BS, Wu JJ, Lo CY, et al. Impact of supplement with Lactobacillus- and Bifidobacterium-containing yogurt on triple therapy for Helicobacter pylori eradication. Aliment Pharmacol Ther. 2002;16(9):1669–75. doi: 10.1046/j.1365-2036.2002.01335.x. [DOI] [PubMed] [Google Scholar]
- 30.Hurduc V, Plesca D, Dragomir D, et al. A randomized, open trial evaluating the effect of Saccharomyces boulardii on the eradication rate of Helicobacter pylori infection in children. Acta Paediatr. 2009;98(1):127–31. doi: 10.1111/j.1651-2227.2008.00977.x. [DOI] [PubMed] [Google Scholar]
- 31.Miki K, Urita Y, Ishikawa F, et al. Effect of Bifidobacterium bifidum fermented milk on Helicobacter pylori and serum pepsinogen levels in humans. J Dairy Sci. 2007;90(6):2630–40. doi: 10.3168/jds.2006-803. [DOI] [PubMed] [Google Scholar]
- 32.Saneeyan H, Layegh S, Rahimi H. Effectivness of probiotic on treatment of Helicobacter pylori infection in children. J Isf Med Sch. 2011;29(146):882–9. [In Persian] [Google Scholar]
- 33.Goldman CG, Barrado DA, Balcarce N, et al. Effect of a probiotic food as an adjuvant to triple therapy for eradication of Helicobacter pylori infection in children. Nutrition. 2006;22(10):984–8. doi: 10.1016/j.nut.2006.06.008. [DOI] [PubMed] [Google Scholar]