Abstract
Background
Rosai-Dorfman disease (RDD) is a rare disease of histiocytic cells, a cause of benign cervical lymphadenopathy (LAP) and massive generalized lymph node enlargement in children and adults. There are also some reports on involvement of other human body organs with or without LAP.
Case Presentation
A 7-month-old infant with chief complaint of generalized massive LAP was referred to our center. RDD was diagnosed according to clinical manifestations and confirmed through histopathologic and immunoreactivity study on the obtained sample by cervical lymph node biopsy.
Conclusion
RDD is not a malignant illness and lymph node enlargement most often decreases in its size happens without special treatment.
Keywords: Rosai-Dorfman Disease, Generalized Lymphadenopathy, Infant, Histiocytosis
Introduction
Rosai-Dorfman disease (RDD) was first introduced in 1969 as sinus histiocytosis with massive lymphadenopathy (SHML)[1]. The patients are most often healthy young adults without a medical background or underlying disease who present with ugly, matted enlarged cervical lymph nodes sometimes associated with fever, polyclonal hypergammaglobulinemia, and an elevated sedimentation rate[2]. Etiology of RDD is not explained exactly, but probably is due to an unknown infectious origin[3]. Histologic findings and immunostaining of protein S-100 positive histiocytes are the choice of final diagnosis and can distinguish it from other disorders of histiocytes that are very important because of different plans of therapy. Spontaneous regression of enlarged nodes and improvement of illness without chemotherapy is common in RDD despite massive and huge lymphadenopathy and expectation of progression of its clinical course.
Reviewing the literature, occurrence of RDD in infants seems to be rare. Due to the rare prevalence of the disease and its multiple manifestations, it is worth presenting a case of RDD with generalized lymphadenopathy.
Case Presentation
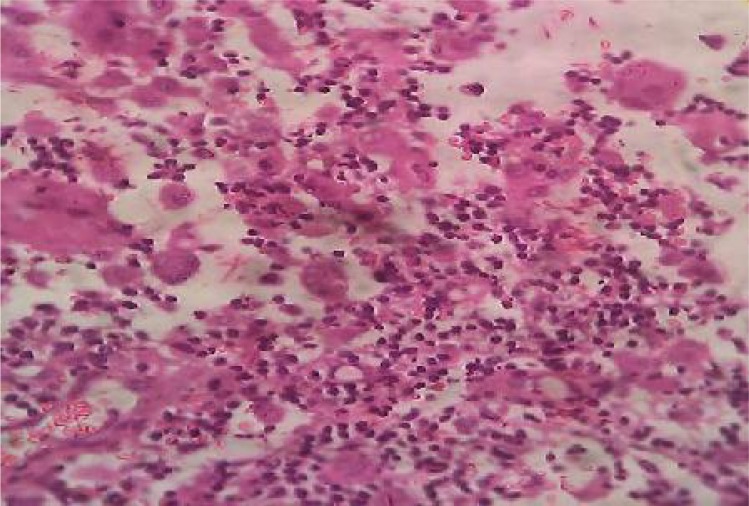
A 7-month-old boy residing in Urmiah, North West Iran, presented with generalized lymphadeno-pathy (LAP) in neck, axilla and groin. He was referred to the Children's Medical Center, the referral pediatric center in Tehran, Iran and admitted to the pediatric infectious disease ward. The patient was a healthy infant till three months ago as his mother noticed a large node on the right side of his neck that had progressive growth and occupied a large portion of cervical area. There was a low grade fever, but no history of upper respiratory tract infection, dyspnea or dysphagia. The child was breastfed and also received supplementary nutrition. Past medical and family history was normal. Clinical examination showed a healthy male infant weighing 8600 gr, length 67 cm and head circumference 45 cm. He had an appearance of bull neck due to bilateral cervical and mandibular LAP. Lymph nodes were discrete, non tender, mobile, matted and about 2 to 6 centimeters in diameter; left axilla and groins also were involved with lymph nodes of almost equal size (Fig 1). Chest x-ray was normal but the skull X-ray showed some lytic lesions in calvarium. The abdominal sonography was normal. White blood cell count 13140/mm3, neutrophils 55.4%, lymphocytes 39.1%, monocytes 4.2%, eosinophils 1.1%, basophils 0.2%, platelets, 530000/mm3, ESR 56 in the first hour. Hemoglobin 10.3 g/dl. Biochemistry, liver function tests and serologic exams for Epstein-Barr virus, cytomegalovirus, HIV, and Toxoplasma gondii, and also the results of diagnostic studies for tuberculosis including tuberculin skin test (TST) were negative. Primary biopsy of cervical lymph node was done. The histologic diagnosis was compatible with RDD by dilated sinusoids filled with histiocytes, signs of emperipolesis of lymphocytes (Fig 2). The neoplastic cells expressed positive immunoreactivity for protein S-100, and CD68 and negative immunoreactivity for CD1a that documented the diagnosis.
Fig. 1.
Cervical, axillary and inguinal lymphadenopathy
Fig. 2.
Emperipolesis of lymphocytes
Discussion
In 1969, Rosai and Dorfman introduced the rare cause of lymph noode enlargement in children and young adults. 80% of cases occur under the age 20 years[1, 4]. Male to female ratio is 1.4:1. The etiology of RDD is not defined till now, although some infectious agents such as Epstein-Barr or Herpes virus might be related to its pathogenesis and clinical manifestations[4, 5]. Our patient was a young 7-month-old male infant without a marked infectious disease.
The most frequent clinical presentation in nearly 90% of patients is bilateral, massive and bizarre cervical LAP without pain and tenderness. It has also been described as proconsular or bull neck which resembles the clinical picture in Hodgkin's disease of the neck[6]. Our patient had bull neck that was the most prominent finding without respiratory difficulty or airways obstruction.
Actually, fever, sweating at night, malaise, loss of weight, leukocytosis, neutrophilia, and elevated erythrocyte sedimentation rate are other associated clinical and laboratory findings. Additionally, a polyclonal hypergammaglobulinemia can be seen in 80% and hypochromic or normochromic normocytic anemia is reported in 60% of patients in published articles[7–9].
Massive lymphadenopathy of the cervical neck lymph noodes is a common presentation; however, enlarged lymph noodes in axillary and inguinal areas have been documented in 38% and 44% of cases, respectively. Although these nodes are usually smaller than those in the neck, they might be detected by CT scanning[5, 6, 9]. In our patient axillary and inguinal lymph nodes (measuring 4-6 cm) were more enlarged than cervical lymph nodes.
According to a literature review by Shi et al, involvement of other body organs rather than lymph nodes has been noted in approximately 43% of patients in the registry of RDD.
Merely extranodal involvement without significant LAP is reported in 23% of cases. Body organs most commonly involved are skin, soft tissue, nose and paranasal sinuses (16%); ophthalmic and orbital involvement, ocular adnexa and bone (11%); salivary gland and central nervous system (7%); oral cavity (4%); kidneys, genitourinary and respiratory systems (3%); liver, tonsils (1%); breast, gastrointestinal tract and cardiac involvement (<1%)[10]. In our case there were lytic lesions in skull without involvement of other organs.
RDD is diagnosed by clinicopathologic findings, so fine needle aspiration or an open biopsy is required to obtain a particle of tissue sample[11]. Histologic findings include dilated sinuses of lymph nodes that are filled with numerous big size histiocytes with plenty of pale cytoplasm.
Emperipolesis of histiocytes is a characteristic finding in which lymphocytes that are phagocytized by the histiocytes can move in the cytoplasmic vacuoles. Immunochemistry is positive for protein S-100 and CD68 as well as alpha-1 antichymotrypsin and negative for CD1a. As differential diagnoses should be considered lymphoreticular malignancies such as lymphomas, Hodgkin's disease, malignant histiocytosis and monocytic leukemia, all of which have similar histopathological features. Atypias in cytology and the aggressive clinical course establish the diagnosis in most cases[12].
In the results of therapeutic modalities, no clinical improvement has been reported by administration of antimicrobial or antimyco-bacterium drugs but decreased fever and reduction of lymph node size can be seen by steroid administration. Chemotherapy, radiotherapy, surgery, or immunomodulators are therapeutic policies to treat the patients with massive lymph node enlargement and extranodal involvement with compression of vital organs but among them surgery is more effective[13]. We diagnosed RDD in this case report according to clinical manifestations, histopathologic and immunoreactivity that was positive for protein S-100 and CD68 and negative for CD1a on the obtained sample by biopsy. Corticosteroid and Etoposide were administered by pediatric oncologists resulting in reduction of lymph nodes size and improved general condition of the patients.
Conclusion
RDD must be included as a differential diagnosis in all young patients with chronic generalized lymphadenopathy. The diagnosis of RDD is made by histopathology. RDD is not a malignant illness and lymph noode size most often decreases without special treatment.
References
- 1.Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity. Arch Pathol. 1969;87(1):63–70. [PubMed] [Google Scholar]
- 2.Brown JR, Skarin AT. Clinical mimics of lymphoma. Oncologist. 2004;9(4):406–16. doi: 10.1634/theoncologist.9-4-406. [DOI] [PubMed] [Google Scholar]
- 3.Gupta P, Babyn P. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): a clinicoradiological profile of three cases including two with skeletal disease. Pediatr Radiol. 2008;38(7):721–8. doi: 10.1007/s00247-007-0701-0. quiz 821-2. [DOI] [PubMed] [Google Scholar]
- 4.Khalilzadeh S, Karimi S, Fakharian A, et al. Generalized lymphadenopathy: A case report of Rosai-Dorfman disease. Tanaffos. 2007;6(3):65–7. [Google Scholar]
- 5.Pinto DC, Vidigal Tde A, Castro B, et al. Rosai-Dorfman disease in the differential diagnosis of cervical lymphadenopathy. Braz J Otorhinolaryngol. 2008;74(4):632–5. doi: 10.1016/S1808-8694(15)30616-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McAlister WH, Herman T, Dehner LP. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease) Pediatr Radiol. 1990;20(6):425–32. doi: 10.1007/BF02075199. [DOI] [PubMed] [Google Scholar]
- 7.Murray JC, Rossman SN, Chintagumpala M. Pathological case of the month. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease) Arch Pediatr Adolesc Med. 1995;149(1):57–8. doi: 10.1001/archpedi.1995.02170130059014. [DOI] [PubMed] [Google Scholar]
- 8.Kim M, Provias J, Bernstein M. Rosai-Dorfman disease mimicking multiple meningioma: Case report. Neurosurgery. 1995;36(6):1185–7. doi: 10.1227/00006123-199506000-00019. [DOI] [PubMed] [Google Scholar]
- 9.Sodhi KS, Suri S, Nijhawan R, et al. Rosai-Dorfman disease: unusual cause of diffuse and massive retroperitoneal lymphadenopathy. Br J Radiol. 2005;78(933):845–7. doi: 10.1259/bjr/23127241. [DOI] [PubMed] [Google Scholar]
- 10.Shi SS, Sun YT, Guo L. Rosai-Dorfman disease of lung: a case report and review of the literatures. Chin Med J (Engl) 2009;122(7):873–4. [PubMed] [Google Scholar]
- 11.Duval M, Nguyen VH, Daniel SJ. Rosai-Dorfman disease: an uncommon cause of massive cervical adenopathy in a two-year-old female. Otolaryngol Head Neck Surg. 2009;140(2):274–5. doi: 10.1016/j.otohns.2008.10.041. [DOI] [PubMed] [Google Scholar]
- 12.Pinto DC, Vidigal Tde A, Castro BD, et al. Rosai-Dorfman disease in the differential diagnosis of cervical lymphadenopathy. Braz J Otorhinolaringol. 2008;74(4):632–5. doi: 10.1016/S1808-8694(15)30616-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pulsoni A, Anghel G, Falcucci P, et al. Treatment of sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): report of a case and literature review. Am J Hematol. 2002;69(1):67–71. doi: 10.1002/ajh.10008. [DOI] [PubMed] [Google Scholar]