Summary
A study was carried out regarding 213 patients of either gender and all ages who presented with post-burn contractures. The commonest site of contracture was the neck. 92 patients (43.19%) had received their initial burn injury management in general surgery units in tertiary care hospitals compared to 43 patients (20.18%) in district headquarter hospitals. Only 26 patients (12.20%) were managed in plastic surgery/burn wards, and 52 patients (24.41%) received no regular treatment from any hospital. The majority of patients (n=197) had a history of conservative management, with only 16 patients (7.51%) having a split thickness skin graft for part of their initial burns. None of the patients had the appropriate anti-deformity splintage in the affected parts or any physiotherapy during the acute phase of their burns.
Keywords: post-burn contractures, release and reconstruction of post-burn contractures, prevention of post-burn contractures
Abstract
Cette étude décrit 213 patients des deux sexes et de tous les âges qui se sont présentés à cause des contractures dues aux brûlures. Le cou était la partie du corps la plus atteinte comme site de contracture. 92 patients (43,19%) ont reçu leur prise en charge initiale dans une unité de chirurgie générale de l’hôpital pour les soins tertiaires et 43 patients (20,18%) dans les hôpitaux de district. Seulement 26 patients (12,20%) ont été traités en chirurgie plastique tandis que 52 patients (24,41%) n’ont reçu aucun traitement particulier dans aucun hôpital. La majorité des patients (n = 197) ont reçu un traitement conservatif pour les brûlures et seulement 16 patients (7,51%) ont bénéficié d’une greffe cutanée d’épaisseur variable pour une part de leurs lésions. Aucun des patients n’a eu le splintage anti-déformation appropriée ni la physiothérapie nécessaire au cours du traitement dans la phase aiguë des brûlures.
Introduction
Despite advances in the overall management of burn injuries, severe post-burn contractures continue to be a formidable foe for reconstructive surgeons in developing countries like ours (Pakistan). Not only do we have a higher incidence of burn injuries, but we also lack ideal facilities for managing acutely burned patients. These factors are further compounded by ignorance, poverty, and inadequate utilization of available health care facilities. The resultant post-burn contractures are often severe, long standing, and with secondary complications. Management of these problems accounts for up to 50% of a general plastic surgeon’s workload.1-3
Once contractures develop, correction of both functional and aesthetic deformities is indicated. The goal is to ensure complete release of the contracture, resurface the raw area with skin grafts or flaps, and restore cosmesis as much as possible. Contracture release and resurfacing can be effected with local tissue rearrangement such as Z-plasties or transposition flaps. When the contracted tissue is of unacceptable quality, or too irregular, excision of scars is undertaken to achieve the best results. Burn victims often pose a surgical management challenge as extensive scarring may preclude local flap options.4-6
Patients and methods
This prospective observational study was conducted over a period of about four years (Aug. 2007 to October, 2011) at the Department of Plastic Surgery and Burn Care Centre, Pakistan Institute of Medical Sciences (PIMS), Islamabad. The study included all patients of either gender and all ages who presented with post-burn contractures following management of their acute burn injuries. Patients with chemical burns of the eyelids and those who had undergone some surgical intervention for their post-burn contractures at other hospitals were excluded.
Initial assessment and diagnosis were based on a thorough history, a physical examination, and tests. We used a comprehensive pro forma design to record patients’ socio- demographic profile, type of burn injury, total body surface area (TBSA) burned, and the health care facility where acute burn management had been provided. We also recorded whether patients had initially been managed with range of motion (ROM) exercises, whether physiotherapy/ anti-deformity splintage was instituted, whether any surgery had been performed, the time lapse between burn injury and presentation with post-burn contractures, and the site of the contractures.
Patients who needed surgery under general anaesthesia were admitted as in-patients, while those who underwent surgery under local anaesthesia were discharged after 4 hours of observation post-op. The aims of surgical management were to ensure complete release of the contracture, to resurface the raw areas with skin grafts, i.e. split thickness skin grafts (STSG)/full thickness skin grafts (FTSG) or flaps, and to restore normal ROM. We followed the standard management protocol of elective release of mature contractures, according to the standard principles of the reconstructive ladder. In the immediate post-op phase, the released and resurfaced areas were dressed with ties over dressings, and splinted in anti-contracture position. In cases of neck contracture, soft neck collars were applied over tie-over dressings, and neck anti-contracture positioning was ensured by placing a pillow under the shoulder blades with no pillow under the head. Once the wounds healed, a rehabilitation regimen was started, consisting of physiotherapy, ROM exercises, massage, compression garments, and nocturnal neck collars (in cases of neck contracture) for six months. The outcome of surgery was measured in terms of graft take/flap survival, restoration of function, and early recurrence within three months. Graft take was assessed by gross inspection day 5 post-op and graded as Good (if ≥95% graft was taken by the defect surface area), Fair (if 80%-95% graft was taken), and Poor (if <80% graft was taken). The restoration of function was measured by employing a quality grading system comparing the post-operative functional status to the preoperative morbid status. Function was stratified into Poor (no or minimal functional improvement), Satisfactory (modest to near normal functional improvement), and Excellent (completely normal function restored). A followup of three months was set up.
Figs. 1-8 show some of the patients.
Fig. 1. Post-burn neck contracture in a 9-yr-old girl.

Fig. 2. Severe post-burn neck contracture of 7 years’ duration.

Fig. 3. Post-burn neck contracture of 7 months’ duration.

Fig. 4. Post-burn neck and axillary contractures with breast deformity.

Fig. 5. Post-burn axillary contracture.

Fig. 6. Post-burn ankle/foot contracture in a 5-yr-old child.
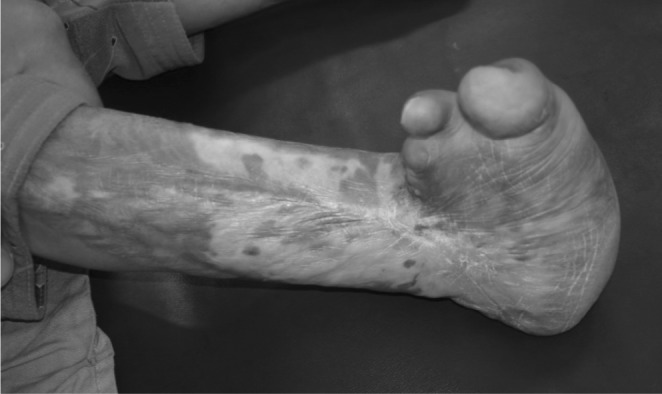
Fig. 7. Crippling post-burn contracture of the hand.

Fig. 8. Fig. 8 - Post-burn contractures of hand, elbow and axilla in a 7-year old child.

Statistical analysis
Data were subjected to statistical analysis using SPSS version 10, and various descriptive statistics were used to calculate frequencies, percentages, means, and standard deviation. Numerical data, such as age, were expressed as mean ± standard deviation, while categorical data, such as the anatomic site of the burns and causes of burns, were expressed as frequencies and percentages.
Results
A total of 213 patients were included in the study. Of these, 143 (67.1%) were males and 70 (32.9%) were females. Ages ranged from 4 to 39 yr. There were 23 children up to the age of 14 yr (10.79%) and 190 adults (89.20%). The mean age of the adults was 23.91 ± 6.13 yr and of the children, 6.52 ± 2.98 yr.
The types of initial burn insults comprised flame burns in 174 cases (81.69%), electrical burns in 21 (9.85%), scalds in 17 (8.45%), and acid burns in 1 (0.47%).
The various causes of burns were domestic accidents with natural gas (n=83, 38.96%), fire accidents in the household (n=67, 31.45%), electrical accidents (n=21, 9.85%), accidents due to leakage of liquefied petroleum gas (LPG) (n=17, 8.45%) from metal cylinders used for household cooking purposes, accidental immersion in hot liquids (n=14, 6.57%), compressed natural gas (CNG) blasts in vehicles (n=7, 3.28%) due to using CNG as automobile fuel contained in cylinders kept inside vehicles, spillage of hot liquids (n=3, 1.40%), and acid burns (n=1, 0.47%).
The TBSA burned in the initial burn injury ranged from 1 to 20%, with a mean of 15.49 ± 4.90%. The smallest TBSA involved was found in cases of isolated burns of the hands or digits secondary to electrical or flame burns while the largest TBSA involved was found in patients with a history of flame burns.
The time lapse between the initial burn injury and presentation ranged from 7 months to 7 years.
Regarding initial management of the burn injury, 92 patients (43.19%) were treated in the general surgery units of tertiary care teaching hospitals, and 43 (20.18%) in district hospitals. Only 26 patients (12.20%) were initially managed in plastic surgery/burn wards, while 52 (24.41%) received no regular treatment from any hospital.
The majority of the patients (n=197) had a history of conservative management while only 16 (7.51%) had undergone STSG for their deep burns.
None of the patients reported a history of appropriate anti-deformity splintage of affected parts or physiotherapy during the acute phase of their burns treatment.
173 patients who needed surgery under general anaesthesia were hospitalized, while 40 patients were managed as outpatients and underwent surgery under local anaesthesia.
Among the body areas affected, the commonest contracture was of the neck (85 cases), followed by axilla (77), fingers/hand (73), elbow (21), knee (15) and ankle/ foot (4). Forty-three patients had more than one contracture. The commonest combination of contractures was neck, axilla, and hand (17 cases), followed by neck and axilla (11), neck and hand (7), axilla and elbow (5), and axilla, elbow, and hand (3).
The operative procedures performed on the patients comprised complete release of contractures followed by resurfacing with skin grafts and flaps. The various resurfacing procedures employed alone or in combination included STSG/FTSG (191 cases), Z-plasties (66), supraclavicular artery flaps (15), abdominal flaps (3) and posterior interreous artery flap (1).
The majority of patients (161 = 84.29%) had a fair graft take, followed by poor take (17 = 8.9%) and good take (13 = 6.80%). All the flaps survived. Functional restoration was satisfactory in all patients. Early recurrence in three months was seen in 8 patients (3.7%): 5 finger contractures, 2 elbow contractures, and 1 neck contracture. Seven out of the 8 patients with early recurrence of contractures were children below 14 years. There was no inhospital mortality in our series.
Discussion
Our study reflects the high frequency of post-burn contractures in our country. To our knowledge, this is the largest local series ever reported on post-burn contractures and it shows the gravity of this largely preventable disability. In developed countries and affluent societies, such disabling conditions have been successfully reduced with improved standards of initial care.7-9
In our patients, we consistently found that in most cases skin grafting for deep burns, exercises/physiotherapy, and anti-deformity positioning during initial burns management injuries were not provided for. All these factors lead to the formation of otherwise avoidable contractures. It is now well established that a burn victim who receives the best initial treatment can expect to heal without any contracture.9,10 Intensive exercise programmes and rehabilitation should be instituted at the very beginning of burns management.7 Early excision and grafting of deep seconddegree and full-thickness burns greatly decrease the frequency and severity of contractures and hypertrophic scarring. Adequately performed anti-deformity positioning also helps to avert the risk of contracture formation.11-13
In our study, most patients were relatively young. The socio-economic implications of such disabling conditions are even more devastating given the economically productive age of the victims. Several published studies have described a similar frequent involvement of younger individuals. 2,14-16
With the exception of neck contractures, in our study all contractures were more frequent among males than females. Most studies have reported a similar incidence of contractures in males.17,18 Telang et al.,14 in their series of 7 neck contractures, reported 5 females and 2 males. However, Paul et al.2 reported equal involvement of the two genders.
Flame burns were the commonest underlying type of burn injury in our study. Flame burns most commonly resulted from accidents due to leakage of natural gas used as domestic fuel for heating/cooking purposes, to clothing catching fire in the kitchen, to accidents with LPG gas cylinders, and to exploding CNG cylinders in vehicles. One frequent underlying cause of domestic gas accidents is the occurrence of unscheduled interruptions in the natural gas supply for households in the winter season. People go to asleep without switching off the gas supply lines of their heaters, but once the gas supply returns it accumulates in the closed room. A gas blast occurs when someone lights a match stick or switches on some electric device in the morning. In our country CNG is widely used to fuel automobiles. Commercial transport vehicles often keep an extra CNG cylinder under the passenger seats, and this is the usual cause of accidental fires in automobiles. All these causes of flame burns are preventable with simple actions based on government commitment and public awareness.
In our study, we operated on contractures which had been developing for at least one year. As a general rule, we do not operate on post-burn contractures during the active phase of healing and scarring because the immature scar is not only highly vascular but also carries a high risk of subsequent re-contracture. The maturity of a scar is determined by gross inspection and palpation. If the scar is no longer hyperaemic but instead soft and supple, it is considered mature. Usually a scar becomes mature in a year. Authoritative publications3,19 have pointed out several exceptions to this general rule of not operating on immature scars, such as incapacitating neck contractures with inability to look forwards, severe microstomia interference with adequate nutrition and orodental hygiene, crippling contractures of the hand, and bilateral knee contractures.
In our study, we managed the majority of the neck contractures with STSGs. Given the recognized limitations of the health care system in a developing country like ours, skin grafts represent the most economical and most commonly performed surgical intervention on these contractures. We prefer to employ thick sheet STSGs, as these have a good take and provide a moderate colour match. We try some over-correction of the defect with graft in order to provide for the inevitable secondary contraction of the skin graft subsequently. The published literature contains reports on the use of skin grafts for contractures.3,20-22
In our study, we employed supraclavicular artery flaps in 15 patients. This flap was used in adult patients when at least one supraclavicular region was unscarred/uninvolved. Compared to skin grafts, the supraclavicular flap provided superior colour and texture match, with the additional advantage of its increase in dimensions over a period of time. Several published series have reported on the superior results of flaps as compared to skin grafts for neck contractures.1,14,23,24 Where microsurgical skills and technologies are available, even free flap transfers are now being attempted to achieve better functional and cosmetic results in patients with neck contractures.25
In our study, we did not use dermal substitutes or tissue expanders. In developed countries these newer adjuncts to surgery are routinely being employed and yield superior results.26-30
Integra is a dermal substitute that has emerged as a novel technique: it has been validated in many studies and has been found particularly useful in large scarred areas (with or without contractures) in any location of the body where tissue expansion and/or flap techniques cannot be employed, either because of the location, paucity of healthy skin, or the large size of the defect.26,31-34 Integra is used to substitute derma, and thin STSG is applied over it, thus providing quality skin cover with minimal donor site morbidity.
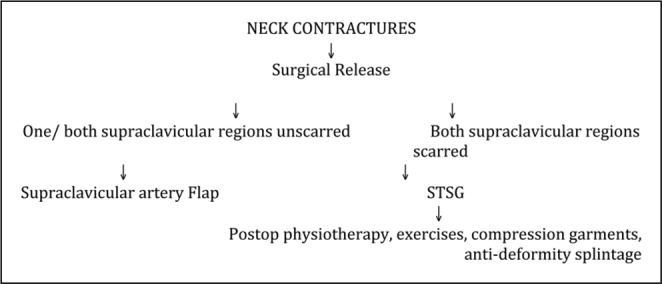
Fig. 9 shows a proposed algorithm for managing neck contractures in settings where ideal infrastructures and sophisticated arsenals of surgical armamentaria such as dermal substitutes etc. are mostly unavailable.
Fig. 9. Management algorithm for neck contractures.
For axillary post-burn contractures, we employed Zplasties, STSGs, or a combination of both. A variety of options have been employed by various researchers for axillary post-burn contractures. The choice of surgical procedure for the reconstruction of post-burn axillary contracture can be made on the basis of the scar contracture pattern and the state of surrounding skin.5,15,35
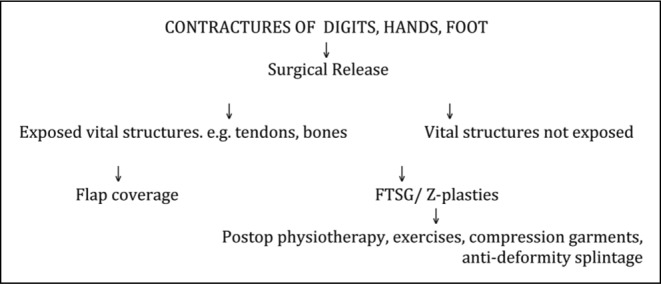
In our study, fingers and hands represented the third commonest site of post-burn contractures. Our findings are consistent with those of other published studies.36,37 Tredget37 observed that in patients with a mean total body surface area burn of 15%, 54% of the patients sustained burns to the hand and upper extremity. In cases of finger contractures, we employed full thickness skin grafts and Zplasties. Fig. 10 shows a proposed algorithm for managing contractures involving digits, hands, and feet.
Fig. 10. Management algorithm for contractures involving digits, hands and feet.
Limitations of the study
Our study presents some limitations as several of the more modern aspects of contracture management could not be addressed. For instance, we mainly employed STSGs and FTSGs for the resurfacing of released contractures; however, these do not constitute the most ideal choice for resurfacing. They do not provide the best possible colour/texture match, skin elasticity, or ideal cosmesis. There is also a tendency to secondary contractures and late recurrence. Additionally, there is a need for post-operative physiotherapy, splintage, pressure garments, and anti-deformity positioning for several months. When STSGs are employed in combination with dermal substitutes such as Integra and Alloderm, the quality of reconstruction is greatly enhanced, and most of the aforementioned problems are solved. The cost of dermal substitutes is the main barrier to their availability, and thence to their general use in our settings. Tissue expansion is also a useful addition to the armamentarium of reconstructive surgeons in the management of contractures in affluent societies; however, their cost often precludes any widespread use, particularly on poor patients in developing countries. Further well designed studies are suggested to fill the gaps in knowledge and compare skin grafts and local flaps with other sophisticated and modern techniques such as Integra, tissue expansion, and free flaps in reconstructing defects that result from release of contractures.
Our study should prompt other similar local studis and hence allow more meaningful comparison of results in our population in Pakistan.
Recommendations
Given the evidence base, it is clear that burn victims typically face a triple threat in the developing societies:
firstly, there is a higher incidence of more severe burns owing to a lack of preventive strategies, ignorance, poor living conditions, and lack of prehospital care;
secondly, burn victims suffer a second preventable accident when no adequate care of burns is provided, such as early excision and grafting of deep burns, ROM exercises, and physiotherapy/antideformity splintage;
thirdly, surviving burn victims often develop incapacitating contractures and hypertrophic scarring, for which they receive less than ideal management most of the time. Thus burn victims undergo a vicious cycle of suffering.
Our recommendations to address the issues in question are the following: educational programmes should be launched to create mass awareness about prevention of burns, in addition to focusing on adequate initial care in order to avert the subsequent morbidity emanating from pitfalls in early management. As burn management continues to be a largely neglected area of medicine in both public and private sector hospitals, we strongly recommend establishing improved facilities for acute burns management as also for adequate rehabilitation of the survivors. Dedicated, well-trained professionals are needed to ensure proper surgical management of burn patients during the acute phase as well as through the phase of rehabilitation and later reconstruction. We also need to develop national guidelines consistent with our local circumstances. Funding to relevant institutions and better training opportunities for committed professionals from the developing world should also be ensured in order to address these issues more efficiently and abolish the sharp contrast in the quality of care between developing countries and the western world.
Conclusion
Post-burn contractures are relatively commoner among young males. Flame burns are the commonest initial burn insults, and household accidents with natural gas represent the most frequent underlying cause of burn injury. Postburn contractures constitute a formidable sequel of inadequately managed burn injuries in our population. The pitfalls in initial burn care that lead to contractures in our patients include the failure to institute adequate surgical management of deep burns, the lack of physiotherapy/ROM exercises, and failure to provide proper anti-deformity splintage. There is need to revisit the prevalent acute burn care practices and establish focused preventive strategies. Adequately trained and dedicated surgeons should be the cornerstone of such strategies.
References
- 1.Rashid M, Islam MZU, Sarwar SU, et al. The expansile supraclavicular artery flap for release of post-burn neck contractures. J Plast Reconstr Aesthet Surg. 2006;59:1094–101. doi: 10.1016/j.bjps.2005.12.058. [DOI] [PubMed] [Google Scholar]
- 2.Paul AC, Swapan KB, Spronk CA, et al. Postburn contracture treatment: A healthcare project in Bangladesh. Burns. 2008;34:181–4. doi: 10.1016/j.burns.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Goel A, Shrivastava P. Post-burn scars and scar contractures. Indian J Plast Surg. 2010;43:63–71. doi: 10.4103/0970-0358.70724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith FR. Causes of and treatment options for abnormal scar tissue. J Wound Care. 2005;14:49–52. doi: 10.12968/jowc.2005.14.2.26734. [DOI] [PubMed] [Google Scholar]
- 5.Lin TM, Lee SS, Lai CS, et al. Treatment of axillary burn scar contracture using opposite running Y-V-plasty. Burns. 2005;3:894–900. doi: 10.1016/j.burns.2005.04.028. [DOI] [PubMed] [Google Scholar]
- 6.Chapman TT. Burn scar and contracture management. J Trauma. 2007;62(S8) doi: 10.1097/TA.0b013e3180653a8a. [DOI] [PubMed] [Google Scholar]
- 7.Edgar D. Active burn rehabilitation starts at time of injury: An Australian perspective. J Burn Care Res. 2009;30:367–8. doi: 10.1097/BCR.0b013e318198a747. [DOI] [PubMed] [Google Scholar]
- 8.Atiyeh BS, Costagliola M, Hayek SN. Burn prevention mechanisms and outcomes: Pitfalls, failures and successes. Burns. 2009;35:181–93. doi: 10.1016/j.burns.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Schneider JC, Holavanahalli R, Helm P, et al. Contractures in burn injury: Defining the problem. J Burn Care Res. 2006;27:508–14. doi: 10.1097/01.BCR.0000225994.75744.9D. [DOI] [PubMed] [Google Scholar]
- 10.Atiyeh BS, Saba M. Soft tissue reconstruction of the burned hand. Ann Burns Fire Disasters. 1995;8:224–6. [Google Scholar]
- 11.Procter F. Rehabilitation of the burn patient. Indian J Plast Surg. 2010;43:101–13. doi: 10.4103/0970-0358.70730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheridan RL. Burns, rehabilitation and reconstruction. [Serial online, updated Aug 28, 2008.]; [(Cited 2011 Aug 14) (3 screens).]; Available from: http://www.emedicine.medscape.com . [Google Scholar]
- 13.Robson MC. Making the burned hand functional. Clin Plast Surg. 1992;16:663. [PubMed] [Google Scholar]
- 14.Telang P, Jagannathan M, Devale M. A study of the use of the supraclavicular artery flap for resurfacing of head, neck, and upper torso defects. Indian J Plast Surg. 2009;42:4–12. doi: 10.4103/0970-0358.53005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sakr WM, Mageed MA, Mo’ez W, et al. Options for treatment of post burn axillary deformities. Egypt J Plast Reconstr Surg. 2007;31:63–71. [Google Scholar]
- 16.Ullah F, Obaidullah , Tahir M, et al. Management of postburn digital flexion contractures. J Coll Physicians Surg Pak. 2005:15631–3. [PubMed] [Google Scholar]
- 17.El-din SAS, El-din AB, El-shafeey E, et al. Reconstruction of post burn palmar web contractures: A surgical approach. Egypt J Plast Reconstr Surg. 2000;23:29–33. [Google Scholar]
- 18.Emsen IM. A new method in treatment of post-burn and post-traumatic scar contractures: Double opposing Z and V (K-M-N) plasty. Can J Plast Surg. 2010;18:e20–e6. [PMC free article] [PubMed] [Google Scholar]
- 19.Donelane MB. In: “Grabb and Smith’s Plastic Surgery”. 6th ed. Thorne CH, Beasley RW, Aston SJ, Bartlett SP, Gurtner GC, Spear SL, editors. Lippincott Williams and Wilkins; Philadelphia: 2007. Principles of burn reconstruction. pp. 150–61. [Google Scholar]
- 20.Harrison CA, MacNeil S. The mechanism of skin graft contraction: An update on current research and potential future therapies. Burns. 2008;34:153–63. doi: 10.1016/j.burns.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 21.Iwuagwa FC, Wilson D, Bailie F. The use of skin grafts in burn contracture release: A 10-year review. Plast Reconstr Surg. 1999;103:1198–204. doi: 10.1097/00006534-199904040-00015. [DOI] [PubMed] [Google Scholar]
- 22.Rudulph R, Ballantyne DL. In: “Plastic Surgery”. McCarthy JG, editor. WB Saunders Co; Philadelphia: 1990. Skin Grafts. pp. 221–74. [Google Scholar]
- 23.Pallua N, Machens HG, Liebau J, et al. Treatment of mentosternal contractures by flap-plasty. Chirurg. 1996;67:850–95. doi: 10.1007/pl00002529. [DOI] [PubMed] [Google Scholar]
- 24.Aufricht G. Evaluation of pedicle flaps versus skin grafts in reconstruction of surface defects and scar contractures of the chin, cheeks, and neck. Surgery. 1994;15:75. [Google Scholar]
- 25.Tsai FC, Mardini S, Chen DJ, et al. The classification and treatment algorithm for post-burn cervical contractures reconstructed with free flaps. Burns. 2006;32:626–33. doi: 10.1016/j.burns.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 26.Kritikos O, Tsoutsos D, Papadopoulos S, et al. The use of artificial skin in plastic surgery and burns. Acta. 2006;48 [PubMed] [Google Scholar]
- 27.MacLennan SE, Corcoran JF, Naele HW. Tissue expansion in head and neck burn reconstruction. Clin Plast Surg. 2000;27:121–32. [PubMed] [Google Scholar]
- 28.Masser MR. Tissue expansion: A reconstructive revolution or a cornucopia of complications. Br J Plast Surg. 1990;43:344–8. doi: 10.1016/0007-1226(90)90085-e. [DOI] [PubMed] [Google Scholar]
- 29.Zellwege G, Kunzi W. Tissue expanders in reconstruction of burn sequelae. Ann Plast Surg. 1991;26:380–8. doi: 10.1097/00000637-199104000-00014. [DOI] [PubMed] [Google Scholar]
- 30.Abdel-Razek EM. Expanded supraclavicular artery island flap for post-burn neck reconstruction. Ann Burns Fire Disasters. 1999;12:107–15. [Google Scholar]
- 31.Stiefel D, Schiestl C, Meuli M. Integra artificial skin for burn scar revision in adolescents and children. Burns. 2010;36:114–20. doi: 10.1016/j.burns.2009.02.023. [DOI] [PubMed] [Google Scholar]
- 32.Soejima K, Nozaki M, Sasaki K, et al. Reconstruction of burn deformity using artificial dermis combined with thin split skin grafting. Burns. 1997;23:501–4. doi: 10.1016/s0305-4179(97)88485-9. [DOI] [PubMed] [Google Scholar]
- 33.Haertsch P. Reconstructive surgery using an artificial dermis (Integra). J Plast Reconstr Aesthet Surg. 2002;55:262–3. doi: 10.1054/bjps.2002.3845. [DOI] [PubMed] [Google Scholar]
- 34.Hunt JA, Moisidis E, Haertsch P. Initial experience of Integra in the treatment of post-burn anterior cervical neck contractures. J Plast Reconstr Aesthet Surg. 2002;53:652–8. doi: 10.1054/bjps.2000.3436. [DOI] [PubMed] [Google Scholar]
- 35.Coban YK. Moderate axillary postburn contracture release using the VM-plasty. Burns. 2007;33:133–4. doi: 10.1016/j.burns.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 36.Schneider JC, Holavanahalli R, Helm P, et al. Contractures in burn injury, part II: Investigating joints of the hand. J Burn Care Res. 2008;29:606–13. doi: 10.1097/BCR.0b013e31817db8e1. [DOI] [PubMed] [Google Scholar]
- 37.Tredget E. Management of the acutely burned upper extremity. Hand Clin. 2000;16:187–202. [PubMed] [Google Scholar]


