Abstract
A large proportion of emerging adults treated for substance use disorder (SUD) present with symptoms of negative affect and major depressive disorder (MDD). However, little is known regarding how these comorbidities influence important mechanisms of treatment response, such as increases in abstinence self-efficacy (ASE). This study tested the degree to which MDD and/or depressive symptoms interacted with during-treatment changes in ASE and examined these variables' relation to outcome at 3-months post-treatment. Participants (N = 302; 74% male) completed measures at intake, mid-treatment, end-of-treatment, and at 3-month follow-up. ASE was measured with the Alcohol and Drug Use Self-Efficacy (ADUSE) scale; depressive symptoms were assessed with the Brief Symptom Inventory 18 (BSI 18) Depression scale; and current MDD diagnoses were deduced from the Structured Clinical Interview for the DSM-IV. Random coefficient regression analyses focused on during-treatment changes in ASE, with BSI 18 scores and MDD diagnosis included as moderators. At intake, individuals with MDD or high levels of depressive symptoms had significantly lower ASE, particularly in negative affect situations. No evidence for moderation was found: ASE significantly increased during treatment regardless of MDD status. There was a main effect of BSI 18 Depression scores: those with lower BSI 18 scores had lower ASE scores at each time point. MDD and BSI 18 Depression did not predict three-month outcome, but similar to previous findings ASE did predict abstinence status at three months. Treatment-seeking emerging adults with MDD merit particular clinical attention because of their lower reported self-efficacy throughout treatment.
Keywords: Emerging adults, substance use disorder, residential treatment, abstinence self-efficacy, major depressive disorder
“Unless people believe they can produce desired effects by their actions they have little incentive to act or to persevere in the face of difficulties.” (Bandura, 2004, pp. 621–622)
Emerging Adulthood and Substance-Related Risk
The transition to adulthood in the United States can be a time of great change and opportunity, yet it also has a dark side: levels of risky behaviors peak during this developmental period. Eighteen to 25-year-olds are more likely than any other age group to use illicit drugs, drive while under the influence of drugs, and binge drink (Substance Abuse and Mental Health Services Administration [SAMHSA], 2007, 2010). Spanning from 18 to 25 years of age, emerging adulthood in the United States is a period characterized by variation in romantic partners, residence, and employment (Arnett, 2000). It is also a time of lifestyle experimentation that often includes alcohol and drug use. This use does not come without consequences - emerging adulthood confers both the highest risk for the onset of substance use disorders (SUD) and the highest density of psychiatric problems and psychological distress (SAMHSA, 2010).
Increased recognition of the unique risks associated with this specific stage of human development has led to new initiatives to identify how to engage and treat emerging adults with SUD (U.S. Department of Health and Human Services, 2007). Much of this research has centered on interventions to reduce hazardous alcohol consumption among college students, with support found for brief group Motivational Enhancement Therapy, the motivational interviewing-based BASICS program, and personalized normative feedback (LaChance, Feldstein Ewing, Bryan, & Hutchison, 2009; Murphy, Dennhardt, Skidmore, Martins, & McDevitt-Murphy, 2010; Neighbors et al., 2010). However, research on 12-step oriented professional treatment programs or drug use interventions among college students has been limited (Larimer, Kilmer, & Lee, 2005), and clinical research focusing specifically on this age group is scarce; 18 to 25 year olds are grouped with adults in most treatment studies. Furthermore, little is known about how clinical samples of emerging adults respond to interventions targeting alcohol and drug use and whether prevalent co-occurring problems (e.g., psychiatric distress) influence this response.
The Influence of Major Depression on Substance Use Disorder Trajectory
Most emerging adults abandon or decrease heavy drinking and drug use as they enter their late twenties, but the presence of anxiety, hostility, and depression can increase risk for continued problem use into adulthood (Costanzo et al., 2007). Major depressive disorder (MDD) often prevents emerging adults from completing age-related developmental tasks in work, social and educational domains (Zarate, 2009). Moreover, the combination of MDD and SUD can intensify subjective distress and place emerging adults at increased risk for suicide attempts (Rohde, 2009).
Comorbid MDD is common among adult treatment seekers, with past-year estimates as high as 44% among those with drug use disorders (Grant et al., 2004). The presence of depression predicts an earlier relapse following treatment (Greenfield et al., 1998). The younger an individual, the greater the likelihood of relapse (Dodge, Sindelar, & Sinha, 2005), highlighting the importance of developmental factors as potential moderators of addiction treatment response.
Depression and Abstinence Self-Efficacy
Abstinence self-efficacy (ASE), the confidence to abstain from using alcohol or drugs in different situations, is a consistent predictor of treatment outcome (Adamson, Sellman, & Frampton, 2009; Moos & Moos, 2006). Consequently, enhancing it is seen as a major goal and a mechanism of addiction treatment (Moos & Moos, 2006; Witkiewitz & Marlatt, 2004). Independent of treatment modality, ASE generally increases during treatment (Goldbeck, Myatt, & Aitchison, 1997; McKellar, Ilgen, Moos, & Moos, 2008; Wong et al., 2004), and LaChance and colleagues (2009) found that increases in self-efficacy during a brief group motivational enhancement therapy intervention mediated the intervention’s effect on drinking outcomes in a college student sample.
Twelve-step based treatment does not focus explicitly on increasing ASE during treatment, but attending AA meetings has been associated with higher ASE (Kelly, Magill, & Stout, 2009; Moos, 2008; Morgenstern, Labouvie, McCrady, Kahler, & Frey, 1997). Although ASE is lower among adults with depression, levels of ASE predict treatment outcomes among depressed and non-depressed samples (Dolan, Martin, & Rohsenow, 2008; Gwaltney, Metrik, Kahler, & Shiffman, 2009; Warren, Stein, & Grella, 2007).
Previous research has tended to focus on generalized ASE, with assertions that MDD may dampen (i.e., moderate) the expected during-treatment increase in ASE due to the global feelings of inefficacy that characterize MDD (Maddux & Meier, 1995). However, measures of overall ASE may neglect important between-situation variance in ASE (i.e., high self-efficacy to abstain when offered a glass of wine, but low abstinence self-efficacy when feeling anxious). Following a depressed mood induction, Ralston and Palfai (2010) found that college students reported reduced abstinence self-efficacy in situations related to depression, but no changes in other high risk drinking situations. Understanding situational-specific ASE can be important in preventing relapse to substance use: Ramo and Brown (2008) found that teenagers were five times more likely than adults to relapse in response to a positive emotional state.
The Present Study
While highly prevalent among SUD treatment samples, MDD and depressive symptoms have not been examined in relation to during-treatment changes in ASE. Greater knowledge about the impact of these common comorbidities on the acquisition of ASE will inform and potentially enhance the effectiveness of interventions targeting this clinical sub-group. Using a large, emerging adult residential treatment sample, this study examines changes in drug and alcohol ASE, with specific emphasis on elucidating the influence of depression on during-treatment ASE changes. Additionally, the study examines whether those with depression have situationally-specific deficits in ASE, or whether these deficits are more global.
Specific study hypotheses were that (1) Emerging adults with a diagnosis of current major depression and/or greater current depressive symptoms would have lower overall, and lower negative affect specific, ASE at intake, (2) Major depression would moderate changes in ASE during treatment: increases in ASE would be greater for those without major depression, and depressive symptoms would be negatively related to during treatment ASE changes; and, (3) Major depression and depressive symptoms would predict substance use outcomes, and major depression would moderate the relationship between end-of-treatment ASE and outcome.
Method
Participants
This was a secondary investigation using data from a longitudinal study on emerging adult SUD treatment outcomes and Alcoholics Anonymous (AA) engagement. All participants from the larger study were included in the current study. Study participants were recruited from the Hazelden Center for Youth and Families (HCYF) in Plymouth, MN between October 2006 and April 2008.
HCYF is an addictions treatment program and part of the Hazelden Foundation, a non-profit organization with substance use disorder treatment facilities nationwide. Treatment at HCYF is grounded in the 12-step based Minnesota model of treatment and supplemented with other methods (e.g., cognitive behavioral therapy, motivational interviewing). Separated by gender, key components of the residential program include individual and group therapy, integrated mental health assessment and therapy, individual assignments related to treatment goals and the 12 steps of AA, education through bibliotherapy and daily lectures, and recreational and spiritual care. Patients at HCYF range in age from 14 to 25 years, with a mean age of 18.
The sample included 302 participants (73.8% male), reflecting the male to female ratio at the treatment center. Participants were, on average, 20.35 years old (Range = 18–24; SD = 1.58), and spent 25 days in residential treatment (SD = 6.45). Consistent with the racial and ethnic distribution of the surrounding region, 95.3% of the sample was Caucasian. The majority had a H.S. diploma (81.7%), while only 1.7% (n = 5) had completed a bachelor’s or associate’s degree (see Table 1). At treatment intake, 46.1% of the sample was not in school (n = 137), 31.0% were attending college part- or full-time (n = 92), 12.8% were seeking a college degree but not enrolled (n = 38), and 10.1% were in high school (n = 30). The justice system had suggested or mandated treatment for 34 of the participants (11.3%), and in the year before treatment participants had spent an average of 1.56 days (SD = 7.50; range 0–120) in residential SUD treatment or in-patient detoxification programs.
Table 1.
Participant Characteristics at Intake as a Function of Past-Month Depression Status
| MDD (n = 48; 15.8%) (n, %) |
No MDD (n = 254; 84.2%) (n, %) |
Total Sample (N = 302) (n, %) |
|
|---|---|---|---|
| Gender | |||
| Female | 18 (22.8) | 61 (77.2) | 79 (26.2) |
| Male | 30 (13.5) | 193 (86.5) | 223 (73.8) |
| Education | |||
| Did not complete H.S. | 10 (20.0) | 40 (80.0) | 50 (16.6) |
| H.S. Diploma/GED | 38 (15.4) | 208 (84.6) | 246 (81.7) |
| Bachelor’s/Associate’s | 0 (0.0) | 5 (100.0) | 5 (1.7) |
| Justice System Involvement | |||
| Treatment mandated | 4 (11.8) | 30 (88.2) | 34 (11.3) |
| Not mandated | 44 (16.4) | 224 (83.6) | 268 (88.7) |
| Substance Use Disorders | |||
| Alcohol* | 32 (20.8) | 122 (79.2) | 154 (51.0) |
| Cannabis | 24 (18.9) | 103 (81.1) | 127 (42.1) |
| Cocaine | 11 (16.4) | 56 (83.6) | 67 (22.2) |
| Opioid | 9 (12.5) | 63 (87.5) | 72 (23.9) |
| Other Axis I Diagnosis** | |||
| Absent | 16 (8.2) | 179 (91.8) | 195 (64.6) |
| Present | 32 (29.9) | 75 (70.1) | 107 (35.4) |
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Age (years) | 20.50 (1.70) | 20.32 (1.56) | 20.35 (1.58) |
| Length of stay (days) | 25.40 (5.89) | 25.16 (6.56) | 25.20 (6.45) |
| Past-year residential | |||
| SUD treatment or detox (days) | 1.09 (2.63) | 1.65 (8.09) | 1.56 (7.50) |
| Pre-treatment use (out of 90 days) | 67.60 (25.10) | 68.78 (25.33) | 68.59 (25.25) |
| AA Attendance (out of 90 days) | 10.57 (17.79) | 11.16 (20.25) | 11.06 (19.81) |
| Inventory of | |||
| Drug Use Consequences** | 74.28 (20.31) | 63.26 (25.20) | 64.94 (24.80) |
| BSI 18 Depression** | 73.40 (5.69) | 62.80 (10.90) | 64.48 (10.96) |
Note.
p < .05;
p < .01
Procedure
Potential participants were required to be 18 or older, and were approached for recruitment during their first three days of residential treatment. Research assistants spoke with 367 individuals about the study. Of these, 47 (12.8%) declined to participate, citing a lack of interest (n = 15), a desire to avoid follow-ups (n = 8), the study taking too much time (n = 8), preferring to focus on treatment (n = 6), not expecting to finish treatment (n = 5), and other miscellaneous reasons (n = 5). While there was no difference in gender between those who participated versus those who declined, there was a difference in age, t(360) = p <.05; those who declined to participate were younger. The actual age difference between the two groups was slight (mean of 19.79 for non-participants vs. 20.37 for participants).
Individuals who gave informed consent were scheduled for a baseline interview within their first seven days of treatment. An independent review board, Schulmann Associates IRB, approved the larger study. Out of the 320 individuals who agreed to participate in the study, 302 (94.4%) completed the baseline interview and were included in the analyses. There were no significant differences in age, gender, or length of stay between those who completed the baseline interview and those who did not.
Participants completed a mid-treatment assessment 14 days into treatment, an end-of-treatment session prior to discharge, and a follow-up interview three months after discharge. The per-session compensation was scaled according to session duration (e.g., $30 for intake, $10 for mid-treatment). Ninety-one percent completed the mid-treatment assessment and 86% completed the end-of-treatment assessment. Participants who completed the end of treatment assessment did not differ from non-completers in gender, length of stay, presence of MDD, intake ADUSE score, or pre-treatment use. Completers were significantly older, t(296) = −2.07, p = .039 (M = 20.40 versus 19.84 for non-completers). Attrition analyses were also conducted for those who completed the three-month follow-up (80.5%; n = 243) versus those who did not, and no significant differences were found.
Measures
Demographics
Treatment attendees provided information about their gender, age, ethnicity, and education as part of the routine intake process.
Recent depressive symptoms
The Brief Symptom Inventory 18 (BSI 18; Derogatis, 2000) was administered at each time point and the six-item Depression subscale provided a continuous measure of depressive symptoms during the previous seven days. The BSI 18 has been normed in community and oncology samples and has acceptable test-retest reliability and internal consistency (Derogatis, 2000).
Substance use consequences
The Inventory of Drug Use Consequences (InDUC-2R; Tonigan & Miller, 2002) was administered at intake to gauge consequences from substance use in the 90 days prior to treatment. Scores on the InDUC-2R can range from 0 to 165 (Tonigan & Miller, 2002). This measure has demonstrated excellent internal consistency in adult samples (α = 0.96; Blanchard, Morgenstern, Morgan, Lobouvie, & Bux, 2003; Gillaspy & Campbell, 2006), and in our sample of emerging adults (α = 0.96).
Major depressive disorder
The Structured Clinical Interview for the DSM-IV (SCID-I/P) is a semi-structured interview for the primary DSM-IV Axis I diagnoses (First, Spitzer, Gibbon, & Williams, 2002). The study had three SCID raters: two had bachelor’s degrees in psychology and one had a PhD in experimental psychology. To prepare for SCID-I/P administration, each of the raters studied the SCID User’s Guide, thoroughly reviewed the SCID, practiced administering the SCID with each other, watched the diagnosis-relevant SCID-101 Didactic Training Series videos, and completed SCID ratings while watching the pre-recorded SCID interviews. SCID interviews were audiotaped during the study, and a random subset of tapes was listened to by a doctoral-level research scientist to ensure adequate diagnostic reliability. No formal inter-rater reliability coefficients were computed.
SUD diagnoses were used to describe the sample, and diagnoses of past-month MDD were used as a dichotomous predictor variable indicating depression present or absent. Those diagnosed with non-current lifetime MDD were not included with this group because lifetime MDD has not been a reliable predictor of SUD treatment outcomes (Bradizza, Stasiewicz, & Paas, 2006; Ramo & Brown, 2008).
When diagnosing MDD using the SCID, studies have found excellent Kappas for joint reliability (0.80 to 0.93), while Kappas for test-retest reliability were fair, ranging from 0.61 to 0.64 (First, Spitzer, Gibbon, & Williams, 1995; Zanarini & Frankenburg, 2001). Several studies have found somewhat lower reliability when using the SCID for comorbid diagnoses among those with substance use disorders (Kranzler et al., 1996), which may result from a discrepancy in determining whether MDD is independent or substance-induced (Grant et al., 2004). Because of this, we utilized the BSI 18 Depression scale as an additional alternative measure of depressive symptoms.
Substance use frequency and AA attendance
The Form-90 instruments were developed for Project MATCH to assess alcohol consumption (Miller & Del Boca, 1994). This family of instruments has shown good test-retest reliability and validity across samples, including adolescents (Rice, 2007; Slesnick & Tonigan, 2004; Tonigan, Miller, & Brown, 1997). The Form-90D is an alternate version of the Form-90 that has demonstrated excellent reliability in measuring illicit drug use (ICCs = 0.75 – 0.82; Westerberg, Tonigan, & Miller, 1998). A modified version of the Form-90D was used to assess days using substances other than nicotine in the 90 days before intake, mandated treatment status, pre-treatment SUD treatment and AA attendance, and abstinence status at follow-up.
Abstinence self-efficacy
The Alcohol and Drug Use Self-Efficacy (ADUSE) scale (Brown et al., 2002) was modified from the Alcohol Abstinence Self-Efficacy scale (DiClemente, Carbonari, Montgomery, & Hughes, 1994) to inquire about both alcohol and drug use. Participants completed this measure at each assessment point. The ADUSE consists of 20 questions rated on a Likert scale from 0 (not at all) to 4 (extremely) that inquire about confidence to avoid drinking or using in different situations. The sum of all 20 items provides an index of overall abstinence self-efficacy. DiClemente and colleagues constructed the Alcohol Abstinence Self-Efficacy Scale from Marlatt and Gordon’s relapse categories (1985). Subscales include Negative Affect, Social/Positive, Physical and Other Concerns, and Craving/Urges situations.
The ADUSE demonstrated excellent reliability at intake, with an overall alpha of 0.94 (20 items, N = 295). Subscales also demonstrated good reliability (α = 0.86 – 0.91). These values are similar to reliability estimates for the Alcohol Abstinence Self-Efficacy Scale (DiClemente et al., 1994). For the ADUSE, we used item means for missing values because individual items varied in their correlation with the total ADUSE score.
Statistical Analyses
All analyses were conducted using SPSS 17.0. Using the three in-treatment assessment points, random coefficient regression was used (RCR; Cohen, Cohen, West, & Aiken, 2003) to model within-subject linear changes in abstinence self-efficacy over the course of treatment, and to assess for variability in those linear changes (Hypothesis 2). Two models were computed for these analyses: one focused on total ADUSE as the dependent variable, the other focused on ADUSE Negative Affect as the dependent variable.
Time was centered at end-of-treatment and coded in weeks. MDD at baseline (coded as 0 = no depression, 1 = depression), and its interaction with time were then added to each model to determine whether there was a main effect of depression on ADUSE scores, and whether depression moderated changes in ADUSE scores over time. A second series of models was estimated, this time with recent depressive symptoms (BSI 18 Depression) as a time-varying covariate. Logistic regression was used to predict substance use (abstinent yes/no) at the three-month follow-up (Hypothesis 3).
Results
Participant Characteristics at Intake
Thirty-five percent of participants met DSM-IV criteria for a current Axis I diagnosis in addition to a substance use disorder (excluding major depressive disorder, and psychotic, somatoform and adjustment disorders). After MDD (15.8%), generalized anxiety disorder (11.3%), social phobia (10.6%), and posttraumatic stress disorder (9.6%) were the most common co-morbid Axis I disorders. All participants met criteria for a substance use disorder, and the most common past-month diagnoses included alcohol use disorder (n = 154; 51.0% of the sample), cannabis use disorder (n = 127; 42.1%), opioid use disorder (n = 72; 23.9%), and cocaine use disorder (n = 67; 22.2%). Consistent with the typical substance use profile of emerging adults, polysubstance use was common, with 51.7% of the sample meeting DSM-IV diagnostic criteria for either polysubstance dependence, or more than one substance use disorder (n = 156).
In the 90 days prior to treatment intake, participants reported using one or more substances an average of 68.59 days (76.2% of pre-treatment period; SD = 25.25) and had a mean score of 64.94 (SD = 24.80) on the InDUC-2R. At intake, mean ADUSE total was 1.96 (SD = 0.87; ‘moderately’ confident to resist use) and mean score on the ADUSE Negative Affect subscale was 1.82 (SD = 1.04). Mean BSI 18 Depression score was 64.48 (SD = 10.96). Those who had been in overnight SUD treatment or detoxification programs in the past year had significantly higher ADUSE total (2.15 vs. 1.90) and Negative Affect scores (2.02 vs. 1.74).
Table 1 displays demographic information separated by intake depression status. Participants were considered “depressed” if they met DSM-IV criteria for past-month MDD (n = 48). Chi-square tests were conducted to test for differences on categorical outcomes and t-tests were conducted to test for differences on continuous variables. Rates of concurrent Axis I diagnosis were significantly different, χ2 (1, N = 302) = 24.34, p < .001, such that more participants with MDD had another Axis I diagnosis than did those without MDD. The results for alcohol use disorder were also significant, χ2 (1, N = 302) = 5.61, p = .019; individuals with MDD were more likely to have a current alcohol use disorder than those without MDD. Significant differences were also found for the InDUC-2R and BSI 18 Depression subscale (see Table 1), in that participants with MDD reported more consequences from their substance use and more depressive symptoms in the week before treatment.
Relationship of Depression to Self-Efficacy at Intake
Intake scores on the BSI 18 Depression subscale were significantly and positively related to MDD status, r(302) = .35, p < .001, however only the ADUSE Negative Affect scale was significantly associated with MDD status, r(294) = −.17, p =.003 (see Table 2). On the whole, participants reporting more past week depressive symptoms on the BSI 18 reported significantly lower ADUSE scores in a number of situations, except for those related to Physical and Other Concerns (see Table 2).
Table 2.
Correlations between Abstinence Self-Efficacy and Depression Indicators at Intake (N = 294)
| Major Depressive Disorder | BSI 18 Depression Scale | |
|---|---|---|
| Alcohol and Drug Use | ||
| Self-Efficacy Scale | ||
| Total Score | −.11 | −.22*** |
| Negative Affect | −.17** | −.26*** |
| Physical/Other Concerns | −.02 | −.11 |
| Cravings/Urges | −.08 | −.23*** |
| Social/Positive | −.10 | −.15** |
Note.
p < .01;
p < .001
Changes in Self-Efficacy During Treatment
Change over Time
Mean total ADUSE scores were 1.96 (SD = 0.87) at intake, 2.40 (SD = 0.86) at mid-treatment, and 2.52 (SD = 0.85) at end-of-treatment. Mean ADUSE Negative Affect scores were 1.82 (SD = 1.04) at intake, 2.20 (SD = 1.02) at mid-treatment, and 2.38 (SD = 1.00) at end-of-treatment. Random coefficient regression of within-subject linear changes showed a significant effect of time for ADUSE total (γ = .14, SE = .01, p < .001) and ADUSE Negative Affect, (γ = .14, SE = .02, p < .001), indicating that, on average, ADUSE scores increased significantly during treatment. Analysis of the variance components revealed significant variability in the ADUSE total slope and intercept (see Table 3), as well as a significant correlation between end-of-treatment ADUSE and changes over time. Individuals who ended treatment with higher overall abstinence self-efficacy experienced a greater increase in ADUSE scores over time. Significant variability was also present in the ADUSE Negative Affect slope and intercept, and there was a significant correlation between end-of-treatment values and changes in negative affect ASE over time (see Table 3).
Table 3.
Covariance Estimates for Between-Subjects Effects of Time on In-Treatment ASE
| Total Abstinence Self-Efficacy (N = 302) | |||||
|---|---|---|---|---|---|
| Variance Component | Parameter | Estimate | SE | Z Value | p |
| Intercept Variability | τ11 | 0.54 | 0.03 | 11.52 | < .001 |
| Slope/Intercept Correlation | τ21 | 0.06 | 0.02 | 3.65 | < .001 |
| Slope Variability | τ22 | 0.02 | 0.01 | 3.86 | < .001 |
| Negative Affect Abstinence Self-Efficacy (N = 302) | |||||
| Variance Component | Parameter | Estimate | SE | Z Value | p |
| Intercept Variability | τ11 | 0.71 | 0.10 | 11.59 | < .001 |
| Slope/Intercept Correlation | τ21 | 0.06 | 0.02 | 2.75 | < .01 |
| Slope Variability | τ22 | 0.02 | 0.01 | 2.84 | < .01 |
MDD as a moderator
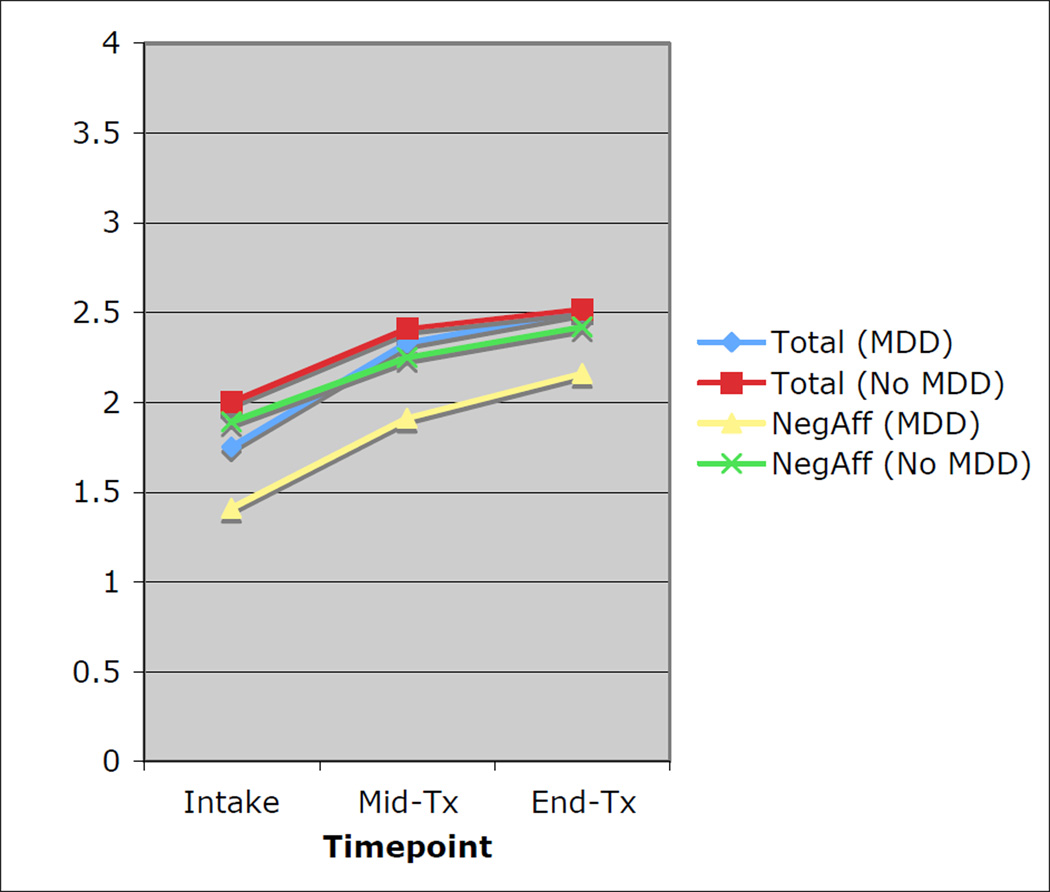
Next, depression status at intake and its interaction with time were added to each model. The linear changes in the total ADUSE score remained significant, but the main effect of MDD status on Total ADUSE and the interaction between MDD and time were non-significant (see Figure 1). Similar results were found for ADUSE Negative Affect. Those with baseline depression had similar increases in ADUSE scores overall and in negative affect situations during treatment, and at end-of-treatment did not differ in their scores on the Total ADUSE or the Negative Affect subscale (see Figure 1). Adding pre-treatment consequences from substance use (InDUC-2R), alcohol use disorder diagnosis, and presence of another psychiatric disorder as covariates did not change the direction of these findings.
Figure 1.
Changes in abstinence self-efficacy during treatment as a function of intake depression. Note. MDD = Major depressive disorder; NegAff = Alcohol and Drug Use Self-Efficacy Negative Affect scale.
Impact of BSI 18 Depression on during treatment changes in abstinence self-efficacy
Mean scores on the BSI 18 Depression subscale during treatment were 64.48 (SD = 10.96) at intake, 55.98 (SD = 9.97) at mid-treatment, and 53.88 (SD = 9.33) at end of treatment. Because BSI 18 Depression scores were obtained at each in-treatment interview, they were treated as a time-varying covariate in both models. When controlling for intake InDUC-2R scores, alcohol use disorder diagnosis, and other psychiatric disorders, the main effect of BSI 18 Depression on the total ADUSE score was significant, γ = −0.02, SE = .003, p < .001, as was the main effect of BSI 18 Depression on ADUSE Negative Affect, γ = −0.02, SE = .004, p < .001. Those with higher scores on the BSI 18 Depression subscale at each assessment also had lower ADUSE total and Negative Affect scores at each assessment, such that an increase of one point on the BSI 18 Depression subscale was associated with a 0.02 decrease on the ADUSE total or Negative Affect scale.
Adding BSI 18 Depression scores to the two models did not change the effect of linear time on abstinence self-efficacy. This suggests that even after controlling for changes in BSI 18 Depression scores during and after treatment, there was still a significant increase in abstinence self-efficacy during treatment. Adding BSI 18 scores did not change the significance of any of the covariance parameter estimates from the previous model.
Post-Treatment Outcomes
At the three-month follow-up, which represented an average of 84.70 days (SD = 12.65), 58.4% of participants reported no substance use (n = 142). While the overall model predicting three-month abstinent status was non-significant (R2= .06), end of treatment ADUSE total did significantly predict abstinence status at three months, β = .44, SE = 0.20, p < .05, as previously demonstrated (Hoeppner, Kelly, Urbanoski, and Slaymaker, 2011). Neither end-of-treatment BSI 18 Depression scores, intake MDD nor the interaction between intake MDD and end-of-treatment ADUSE total were significant predictors of substance use outcome, indicating that depression status did not moderate the relationship of self-efficacy on treatment outcomes.
Discussion
The current study aimed to improve our understanding of how changes in abstinence self-efficacy (ASE) during treatment may be influenced by the common co-occurring problem of MDD among emerging adults. ASE did increase significantly during treatment, and the presence of MDD did not significantly attenuate this increase. Depression scores co-varied with ADUSE scores: those with more depressive symptoms reported lower abstinence self-efficacy throughout treatment in negative affect situations and overall.
The Relationship between Depression and Self-Efficacy
The characteristic low self-efficacy of depressed individuals was manifest in the significantly lower confidence that participants with MDD reported in their ability to resist substance use in negative affect situations. At intake, this relationship was situation-specific: in situations unrelated to negative affect, those with MDD did not have significantly different levels of self-efficacy from those without MDD. This corresponds with the finding that, following a depressed mood induction, college students reported lower self-efficacy specifically in negative affect-related situations (Ralston & Palfai, 2010), and suggests that major depression may selectively impact self-efficacy in negative affect situations, instead of being related to a more general sense of low self-efficacy. In their relapse prevention model, Marlatt and Gordon (1985) highlighted the importance of negative affect situations as high-risk situations for relapse. Such situations may be particularly salient for individuals with MDD because they experience them more frequently.
Considering the relationship between BSI 18 Depression scores and intake ADUSE scores adds complexity to this picture. Past-week depressive symptoms, as measured by the BSI 18 Depression subscale, were related not only to low self-efficacy in negative affect situations, but also to low self-efficacy in other high-risk situations except for those related to physical pain.
What might explain the broader relationship between a state-like measure of depressive symptoms and ASE, as compared to the more limited relationship between MDD and ASE? The added power of a continuous measure of depression, versus the dichotomous SCID major depression variable, may partially explain these findings. Alternatively, the two indices of depression may represent conceptually different types of relapse risk. Witkiewitz and Marlatt (2004) propose a model in which tonic (distal) factors and phasic (proximal) factors interact to predict relapse. MDD may be seen as a tonic factor that predisposes an individual to low self-efficacy in negative affect situations, while the more proximal BSI 18 recent depressive symptoms might represent a phasic state of depression that predisposes an individual to low self-efficacy in a number of different situations. This is a preliminary explanation of these findings and further study is warranted.
Additionally, although individuals with high BSI 18 depression scores did report lower ASE throughout treatment, the clinical significance of this difference is unknown. Future research should investigate whether this gap in ASE is clinically important, or accounts for the traditionally poorer outcomes of the depressed (Grant et al., 2004).
During-Treatment Changes in ASE
Similar to previous findings, abstinence self-efficacy increased during treatment (Goldbeck et al., 1997; Ilgen, McKellar, & Tiet, 2005; Wong et al., 2004). This mirrors findings of increased self-efficacy following brief interventions for college students (LaChance et al., 2009). Because abstinence self-efficacy is one of the most consistent predictors of outcomes (Ilgen et al., 2005; Moos & Moos, 2006), increases in abstinence self-efficacy during treatment bode well for treatment outcomes among more severe clinical populations. Bandura (2004) has suggested that self-efficacy may increase through social modeling or verbal persuasion. AA speakers, counselors and peers might convince an individual of his or her ability to maintain sobriety. Increases in abstinence self-efficacy may be a by-product of time spent in a controlled environment, among peers, learning about the 12 steps, and it remains for future research to uncover the specific mechanisms by which ASE increases during such treatment.
Depression as a Moderator of In-Treatment Changes in ASE
Contrary to our predictions, during treatment abstinence self-efficacy increased similarly for those who were depressed and those who were not. Even though individuals reporting past-week symptoms of depression had consistently lower levels of ASE, they still experienced similar increases in ASE during treatment. This is a hopeful finding for clinicians because it suggests that substance dependent emerging adults with MDD can experience growth in variables that are important to sustained recovery.
Limitations and Strengths
Our findings must be considered in light of several limitations. The sample was three-quarters male, consistent with admissions at the treatment facility, but depression occurs more frequently among women in the general U.S. population (Kessler et al., 2005). The sample was primarily Caucasian and findings may not generalize to ethnic minority samples. Emerging adulthood spans from age 18 to 25, but our sample was clustered primarily around the younger end of this range. Additionally, although raters were thoroughly trained in the administration of the SCID-I/P, no inter-rater reliability coefficients were computed for SUD or MDD diagnoses.
Despite these limitations, this study had several strengths. Large inpatient clinical samples are notoriously hard to access, and this study included multiple during treatment assessment points with such a population with impressive retention rates. It focused specifically on the high risk, but sorely understudied, population of emerging adults with severe SUD who seek residential treatment (Kelly, Magill, Slaymaker, & Kahler, 2010). Furthermore, emerging adults with MDD tend to exhibit a more chronic course of SUD into adulthood, which adds import to the study of comorbidity in emerging adults (Costanzo et al., 2007).
Conclusions and Future Directions
The goal of this study was to examine changes in abstinence self-efficacy over time and its relation to depression and psychological distress in a specific sample: emerging adults attending residential treatment. Participants with MDD reported significantly less ASE in negative affect situations, and depressive symptoms were related to lower ASE throughout treatment. Nevertheless, abstinence self-efficacy increased during treatment for the entire sample regardless of level of depression or psychological distress. The persistently lower ASE in regard to negative affect situations for those with MDD, however, may mean these individuals could benefit from a more focused clinical approach that attempts to increase negative affect-specific coping skills and distress tolerance.
Future analyses should investigate whether these observed increases in ASE are specific to 12-step based professional treatment, and how different facets of depression affect self-efficacy over the full course of treatment and recovery. In this way, we will better understand the specific role that ASE plays in the recovery experiences of treatment-seeking emerging adults.
Acknowledgments
Preparation of this paper was supported by the third author’s NIAAA grant 1R21AA018185-01A. The research was also supported by an anonymous grant given to the Butler Center for Research at Hazelden.
We wish to thank the study participants for the time they dedicated to this study, the staff at the Hazelden Center for Youth and Family in Plymouth, Minnesota for their willingness to collaborate in research procedures, and Dr. Barbara McCrady for her careful editing of an early version of the manuscript.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/adb.
Contributor Information
Brenna L. Greenfield, Department of Psychology and Center on Alcoholism, Substance Abuse, and Addictions, University of New Mexico
Kamilla L. Venner, Department of Psychology and Center on Alcoholism, Substance Abuse, and Addictions, University of New Mexico
John F. Kelly, Center for Addiction Medicine, Department of Psychiatry, Massachusetts General Hospital and Harvard Medical School
Valerie Slaymaker, Hazelden Graduate School for Addiction Studies, Hazelden Foundation.
Angela D. Bryan, Psychology Department and Center on Alcoholism, Substance Abuse, and Addictions, University of New Mexico
References
- Adamson SJ, Sellman JD, Frampton CMA. Patient predictors of alcohol treatment outcome: a systematic review. Journal of Substance Abuse Treatment. 2009;36(1):75–86. doi: 10.1016/j.jsat.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. The American Psychologist. 2000;55(5):469–480. [PubMed] [Google Scholar]
- Arnett JJ. The developmental context of substance use in emerging adulthood. Journal of Drug Issues. 2005;35(2):235–254. [Google Scholar]
- Bandura A. Swimming against the mainstream: The early years from chilly tributary to transformative mainstream. Behaviour Research and Therapy. 2004;42(6):613–630. doi: 10.1016/j.brat.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Blanchard KA, Morgenstern J, Morgan TJ, Lobouvie EW, Bux DA. Assessing consequences of substance use: psychometric properties of the inventory of drug use consequences. Psychology of Addictive Behaviors. 2003;17(4):328–331. doi: 10.1037/0893-164X.17.4.328. [DOI] [PubMed] [Google Scholar]
- Bradizza CM, Stasiewicz PR, Paas ND. Relapse to alcohol and drug use among individuals diagnosed with co-occurring mental health and substance use disorders: a review. Clinical Psychology Review. 2006;26(2):162–178. doi: 10.1016/j.cpr.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Brown TG, Seraganian P, Tremblay J, Annis H. Process and outcome changes with relapse prevention versus 12-Step aftercare programs for substance abusers. Addiction. 2002;97(6):677–689. doi: 10.1046/j.1360-0443.2002.00101.x. [DOI] [PubMed] [Google Scholar]
- Chung T, Maisto SA. Relapse to alcohol and other drug use in treated adolescents: review and reconsideration of relapse as a change point in clinical course. Clinical Psychology Review. 2006;26(2):149–161. doi: 10.1016/j.cpr.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences, third edition. Routledge Academic; 2002. [Google Scholar]
- Costanzo PR, Malone PS, Belsky D, Kertesz S, Pletcher M, Sloan FA. Longitudinal differences in alcohol use in early adulthood. Journal of Studies on Alcohol and Drugs. 2007;68(5):727–737. doi: 10.15288/jsad.2007.68.727. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. BSI-18: Administration, Scoring, and Procedures Manual. Minneapolis, MN: National Computer Systems; 2000. [Google Scholar]
- DiClemente CC, Carbonari JP, Montgomery RPG, Hughes SO. The Alcohol Abstinence Self-Efficacy scale. Journal of Studies on Alcohol. 1994;55(2):141–148. doi: 10.15288/jsa.1994.55.141. [DOI] [PubMed] [Google Scholar]
- Dodge R, Sindelar J, Sinha R. The role of depression symptoms in predicting drug abstinence in outpatient substance abuse treatment. Journal of Substance Abuse Treatment. 2005;28(2):189–196. doi: 10.1016/j.jsat.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Dolan SL, Martin RA, Rohsenow DJ. Self-efficacy for cocaine abstinence: pretreatment correlates and relationship to outcomes. Addictive Behaviors. 2008;33(5):675–688. doi: 10.1016/j.addbeh.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. The Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II): II. Multi-site test-retest reliability study. Journal of Personality Disorders. 1995;9(2):92–104. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Gillaspy JA, Jr, Campbell TC. Reliability and Validity of Scores from the Inventory of Drug Use Consequences. Journal of Addictions & Offender Counseling. 2006;27(1):17–27. [Google Scholar]
- Goldbeck R, Myatt P, Aitchison T. End-of-treatment self-efficacy: a predictor of abstinence. Addiction. 1997;92(3):313–324. [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, Michael J. The effect of depression on return to drinking: A prospective study. Archives of General Psychiatry. 1998;55(3):259–265. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- Gwaltney CJ, Metrik J, Kahler CW, Shiffman S. Self-efficacy and smoking cessation: A meta-analysis. Psychology of Addictive Behaviors. 2009;23(1):56–66. doi: 10.1037/a0013529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeppner B, Kelly JF, Urbanoski K, Slaymaker V. Comparative utility of a single-item measure of self-efficacy vs. multiple-item scale scores in predicting substance use relapse among treatment-seeking young adults. Journal of Substance Abuse Treatment. 2011;41(3):305–312. doi: 10.1016/j.jsat.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilgen M, McKellar J, Tiet Q. Abstinence self-efficacy and abstinence 1 year after substance use disorder treatment. Journal of Consulting and Clinical Psychology. 2005;73:1175–1180. doi: 10.1037/0022-006X.73.6.1175. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Magill M, Slaymaker V, Kahler C. Psychometric validation of the Leeds Dependence Questionnaire (LDQ) in a young adult clinical sample. Addictive Behaviors. 2010;35(4):331–336. doi: 10.1016/j.addbeh.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Magill M, Stout RL. How do people recover from alcohol dependence? A systematic review of the research on mechanisms of behavior change in Alcoholics Anonymous. Addiction Research & Theory. 2009;17(3):236–259. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kranzler HR, Kadden RM, Babor TF, Tennen H. Validity of the SCID in substance abuse patients. Addiction. 1996;91(6):859–868. [PubMed] [Google Scholar]
- LaChance H, Feldstein Ewing SW, Bryan AD, Hutchison KE. What makes group MET work? A randomized controlled trial of college student drinkers in mandated alcohol diversion. Psychology of Addictive Behaviors. 2009;23(4):598–612. doi: 10.1037/a0016633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Kilmer JR, Lee CM. College student drug prevention: A review of individually-oriented prevention strategies. Journal of Drug Issues. 2005;35(2):431–456. [Google Scholar]
- Maddux JE, Meier LJ. Self-efficacy and depression. In: Maddux JE, editor. Self-efficacy, adaptation, and adjustment: Theory, research, and application. New York, NY: Springer; 1995. pp. 143–169. [Google Scholar]
- Marlatt GA, Gordon JR. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York: Guilford Press; 1985. [Google Scholar]
- McKellar J, Ilgen M, Moos BS, Moos R. Predictors of changes in alcohol-related self-efficacy over 16 years. Journal of Substance Abuse Treatment. 2008;35(2):148–155. doi: 10.1016/j.jsat.2007.09.003. [DOI] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol. 1994;S12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Moos RH. Active ingredients of substance use-focused self-help groups. Addiction. 2008;103(3):387–396. doi: 10.1111/j.1360-0443.2007.02111.x. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction. 2006;101(2):212–222. doi: 10.1111/j.1360-0443.2006.01310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, Labouvie E, McCrady BS, Kahler CW, Frey RM. Affiliation with Alcoholics Anonymous after treatment: A study of its therapeutic effects and mechanisms of action. Journal of Consulting and Clinical Psychology. 1997;65(5):768–777. doi: 10.1037//0022-006x.65.5.768. [DOI] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Martens MP, McDevitt-Murphy ME. Computerized versus motivational interviewing alcohol interventions: Impact on discrepancy, motivation, and drinking. Psychology of Addictive Behaviors. 2010;24(4):628–639. doi: 10.1037/a0021347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Lewis MA, Atkins DC, Jensen MM, Walter T, Fossos N, Larimer ME. Efficacy of web-based personalized normative feedback: A two-year randomized controlled trial. Journal of Consulting and Clinical Psychology. 2010;78(6):898–911. doi: 10.1037/a0020766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ralston TE, Palfai TP. Effects of depressed mood on drinking refusal self-efficacy: Examining the specificity of drinking contexts. Cognitive Behaviour Therapy. 2010;39(4):262–269. doi: 10.1080/16506073.2010.501809. [DOI] [PubMed] [Google Scholar]
- Ramo DE, Brown SA. Classes of substance abuse relapse situations: a comparison of adolescents and adults. Psychology of Addictive Behaviors. 2008;22(3):372–379. doi: 10.1037/0893-164X.22.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice C. Retest reliability of self-reported daily drinking: Form 90. Journal of Studies on Alcohol and Drugs. 2007;68(4):615–618. doi: 10.15288/jsad.2007.68.615. [DOI] [PubMed] [Google Scholar]
- Rohde P. Comorbidities with adolescent depression. In: Nolen-Hoeksema S, Hilt LM, editors. Handbook of depression in adolescents. New York, NY: Routledge; 2009. pp. 139–177. [Google Scholar]
- Slesnick N, Tonigan JS. Assessment of alcohol and other drug use by runaway youths: A test-retest study of the Form 90. Alcoholism Treatment Quarterly. 2004;22(2):21–34. doi: 10.1300/J020v22n02_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The NSDUH Report: Co-Occurring Major Depressive Episode (MDE) and Alcohol Use Disorder Among Adults (Office of Applied Studies) Rockville, MD: 2007. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings (Office of Applied Studies, NSDUH Series H-38A, DHHS Publication No. SMA 10-4586Findings) Rockville, MD: 2010. [Google Scholar]
- Tonigan JS, Miller WR, Brown JM. The reliability of Form 90: An instrument for assessing alcohol treatment outcome. Journal of Studies on Alcohol. 1997;58(4):358–364. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Miller WR. The inventory of drug use consequences (InDUC): test-retest stability and sensitivity to detect change. Psychology of Addictive Behaviors. 2002;16(2):165–168. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, National Institutes of Health, Office of the Surgeon General. The Surgeon General’s call to action to prevent and reduce underage drinking. 2007 Retrieved from http://www.niaaa.nih.gov/AboutNIAAA/NIAAASponsoredPrograms/Documents/calltoaction.pdf. [PubMed]
- Warren JI, Stein JA, Grella CE. Role of social support and self-efficacy in treatment outcomes among clients with co-occurring disorders. Drug and Alcohol Dependence. 2007;89(2–3):267–274. doi: 10.1016/j.drugalcdep.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westerberg VS, Tonigan JS, Miller WR. Reliability of Form 90D: An instrument for quantifying drug use. Substance Abuse. 1998;19(4):179–189. doi: 10.1080/08897079809511386. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was Zen, this is Tao. American Psychologist. 2004;59(4):224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Wong CJ, Anthony S, Sigmon SC, Mongeon JA, Badger GJ, Higgins ST. Examining interrelationships between abstinence and coping self-efficacy in cocaine-dependent outpatients. Experimental and Clinical Psychopharmacology. 2004;12(3):190–198. doi: 10.1037/1064-1297.12.3.190. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR. Attainment and maintenance of reliability of axis I and II disorders over the course of a longitudinal study. Comprehensive Psychiatry. 2001;42(5):369–374. doi: 10.1053/comp.2001.24556. [DOI] [PubMed] [Google Scholar]
- Zarate CA., Jr . Psychiatric disorders in young adults: Depression assessment and treatment. In: Grant JE, Potenza MN, editors. Young adult mental health. Oxford, England: Oxford University Press; 2009. pp. 206–230. [Google Scholar]