Abstract
Overview
The proportion of preterm and low-birth-weight infants has been growing steadily for two decades. Most of the more than $10 billion spent on neonatal care in the United States in 2003 was spent on the 12.3% of infants who were born preterm. Research has shown higher initial hospital costs and a higher rate of acute care visits and rehospitalization for preterm and low-birth-weight infants, but only a limited number of studies of the cost of prematurity that follow infants through the first year of life have been conducted.
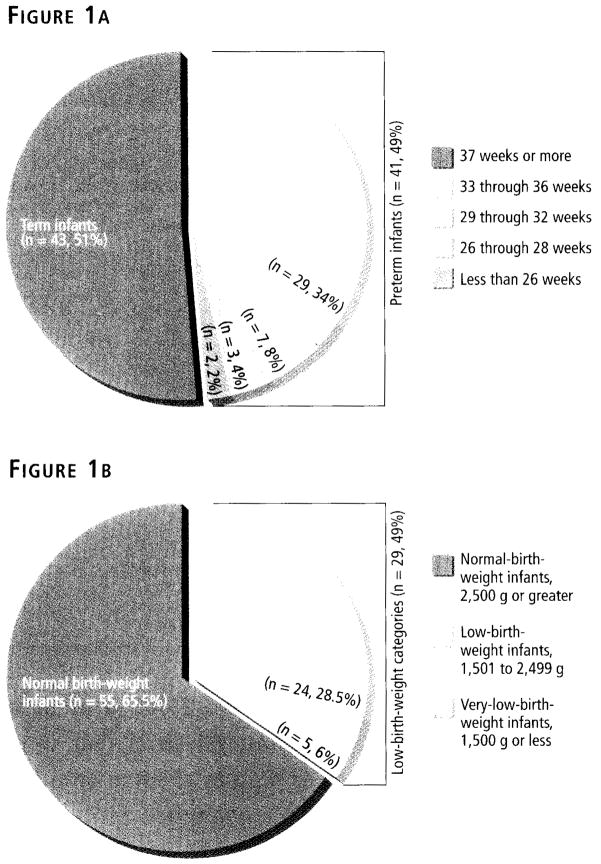
This study is a secondary analysis of data on a subset of infants drawn from a randomized clinical trial that examined health outcomes and health care costs in women with high-risk pregnancies and their infants. For the current study, a sample of 84 singleton infants was chosen. Forty-three infants (51 %) were full term (37 weeks’ gestation or more) and 41 (49%) were born preterm (less than 37 weeks’ gestation). Fifty-five infants (65.5%) were born at normal birth weights (2,500 g or greater), 24 (28.5%) were born at low birth weights (1,501 to 2,499 g), and five (6%) were born at very low birth weights (less than 1,500 g).
Data on the initial hospital charges and the rates of rehospitalization and acute care visits in the first year of life in relation to gestational age and birth weight were collected. The results clearly demonstrated that the charges for initial hospitalizations increased as birth weights and gestational ages decreased. Low-birth-weight infants were less likely to have unscheduled acute care visits than normal-birth-weight infants.
Interventions to improve prenatal care targeted to women at high risk for delivering preterm or low-birth-weight infants would reduce health care costs and improve health outcomes of infants as well.
More than 4 million infants were born in the United States in 2003; the cost of hospital care for these newborns was more than $10 billion. More than half of that sum was spent on the 12.3% of infants who were preterm (less than 37 weeks’ gestation).1–3
Also in 2003 low-birth-weight infants (less than 2,500 g) accounted for 7.9% of the total number of newborns.4 Since the mid-1980s the low-birth-weight rate has risen from 6.8%, while the very-low-birth-weight (less than 1,500 g) rate has risen from 1.16% in 1981 to 1.46% in 2002.5 The rise in the low-birth-weight rate, as a percentage of all births, has been linked in part to the increase in multiple births resulting from advances in artificial reproductive technologies.5
There are about as many preterm infants born today as there were 25 years ago; however, because of advances in prenatal and neonatal care, more of the low-birth-weight infants born in the United States survive, and they do so at increasingly shorter gestations, increasing health care costs further.6–9 The purpose of this study was to compare initial hospital charges for infants born preterm (less than 37 weeks’ gestation) and infants born at low birth weights (less than 2,500 g) with those of infants born full term (37 to 42 weeks’ gestation) and infants born at normal weight (2,500 g or greater). In addition, the rates of rehospitalizations and acute care visits over the first year of life in each infant group were compared.
LITERATURE REVIEW
Although many preterm and low-birth-weight infants survive, some have negative sequelae, including developmental disabilities, chronic respiratory problems, and vision and hearing impairments.10 Preterm and low-birth-weight infants are also significantly more likely to be rehospitalized and require more acute care visits over the first year of life than infants born full term and at normal birth weight.2 In 1988 the cost of providing health care to low-birth-weight infants through the first year of life was estimated to exceed $4 billion and to account for 35% of the total health care costs for all infants. This amount has since risen to $5 billion per year.1
Small increases in birth weight can result in health care cost savings in infants’ first year of life. In a study by St. John and colleagues of infants born between 1989 and 1992, those born at 24 weeks’ gestation who survived had an initial hospital cost of $145,892.3 Rogowski, reporting on first-year health care costs by birth-weight category, found that the treatment cost for infants born weighing 750 to 999 g who survived for at least the first year was a mean of $138,800 per baby; for those born weighing 1,000 to 1,249 g, the cost was $75,100 per baby; and for those born weighing 1,250 to 1,499 g, the cost was $58,000.2 The cost for infants born weighing less than 750 g who survived was $273,900. The study results demonstrated that, for all infants weighing more than 750 g, including those who didn’t survive, an increase of 250 g in birth weight generated a savings of $12,000 to $16,000 in the first year, and an increase of 500 g in birth weight saved $28,000. The largest of these costs in the first year of life were those incurred during initial hospitalization.
After initial hospitalization, many preterm and low-birth-weight infants in their first year undergo rehospitalization and acute care visits to a physician or ED that are not routinely scheduled. In a previous study, Brooten (a coauthor of this article) and colleagues found that among infants born weighing less than 1,500 g, 25% were rehospitalized and 82% had acute care visits in the first year of life.11 Stevenson and colleagues reported that infants weighing 1,501 to 2,000 g at birth had postdischarge hospital costs more than twice as high as children born full term, weighing 2,500 g or more.12 Tommiska and colleagues compared the cost of care for extremely-low-birth-weight infants (those weighing less than 1,000 g at birth) in the first two years of life and found that a normally developed extremely-low-birth-weight infant had costs 25 times greater than normal-birth-weight infants in that period.13 Petrou and colleagues examined the number and duration of hospital admissions for preterm infants born at less than 28 weeks’, 28 to 31 weeks’, 32 to 36 weeks’, and 37 weeks’ or longer gestation.14 The total number of days spent in the hospital in the first five years of life among infants born at less than 28 weeks’ gestation and those born at 28 to 31 weeks’ gestation was eight times that for full-term infants. The total number of days spent in the hospital for those born at 32 to 36 weeks’ gestation was 2.6 times that among full-term infants. When duration of life was taken into account, the total numbers of days spent in the hospital for infants born at less than 28 weeks’ gestation and those at 28 to 31 weeks’ gestation were 85 and 16 times that for full-term infants, respectively. In summary, research on the cost of health care for preterm and low-birth-weight infants during the first year of life and beyond indicates higher hospital costs and a higher rate of acute care visits and rehospitalization than for full-term and normal-weight infants. Unfortunately, in the past two decades, only a limited number of studies have been conducted on the cost of prematurity through the first year of life.
METHODS
Sample
This study is a secondary analysis of data on a subset of infants drawn from a randomized clinical trial that examined health outcomes and health care charges in women with high-risk pregnancies and their infants. In the original trial, one group of women with high-risk pregnancies received usual prenatal care delivered by physicians in a clinic or physician’s office. In a second group of women, half of the usual prenatal care that physicians would have provided was instead provided by master’s-prepared advanced practice nurses in the women’s homes.15 The original clinical trial consisted of 173 women and 194 infants. For the secondary analysis of data on infants, 50 infants in the intervention group and 50 infants in the control group were chosen by selecting every other infant from the appropriate group. Twins and infants for whom there were any missing charges were excluded from the sample, resulting in a final sample of 84 singleton infants.
Thirty-six of the infants were female and 48 were male. Figures 1a and 1b (at left) present gestational-age and birth-weight data on term and preterm infants. Gestational age ranged from 34 to 41 weeks among infants in the normal-birth-weight category and from 23 to 40 weeks among infants in the low-birth-weight categories (including very-low-birth-weight infants).
Figure 1.
Figure 1a. Gestational Ages of Term and Preterm Infants
Figure 1b. Birth Weights of Term and Preterm Infants
Measures
Birth weight was divided into the following categories: 1,000 g or less, 1,001 to 1,250 g, 1,251 to 1,500 g, 1,501 to 1,750 g, 1,751 to 2,000 g, 2,001 to 2,499 g, and 2,500 g or greater.
Gestational age at birth was divided into the following categories: less than 26 weeks’ gestation completed, 26 through 28 weeks’ gestation completed, 29 through 32 weeks’ gestation completed, 33 through 36 weeks’ gestation completed, and 37 weeks or more completed.
Costs of initial hospitalizations at birth were determined using data on hospital charges, which represent patients’ and insurers’ financial responsibilities.
Rehospitalizations were defined as any hospitalization that occurred following the initial hospitalization at birth through the first year of life.
Acute care visits were defined as visits to a physician, ED, or urgent care center that occurred during the first year of life and that were not routinely scheduled.
Procedures
A data form was used to collect data from the original chart logs used in the clinical trial and included information about initial hospital charges at the time of the infant’s birth, as well as the number of rehospitalizations and acute care visits in the first year of life.
RESULTS
The two general categories of data were the initial hospital charges in relation to gestational age and birth weight and the rates of rehospitalization and acute care visits in relation to gestational age and birth weight.
Initial hospital charges
Gestational age
Charges for hospitalization at birth decreased dramatically with increasing gestational age (see Table 1, above). Four of the five infants born at 28 weeks’ gestation or less had hospital charges greater than $200,000; one of those had charges exceeding $250,000. One infant who was born at less than 26 weeks’ gestation and died 18 days after birth had lower charges ($23,634).
Table 1.
Initial hospital charges by infants’ gestational age (N = 84)
| Infant Gestational Age at Birth (in weeks) | ||||||
|---|---|---|---|---|---|---|
| Initial Hospital Charge | Total No. of Infants | <26 (n = 2) | 26–28 (n = 3) | 29–32 (n = 7) | 33–36 (n = 29) | ≥ 37 (n = 43) |
| > $200,000 |
|
|
|
|||
| $150,001–$200,000 | — | |||||
| $100,001–$150,000 | — | |||||
| $50,001–$100,000 |
|
|
|
|||
| $25,001–$50,000 |
|
|
|
|||
| $15,001–$25,000 |
|
 * *
|
|
|
||
| $5,001–$15,000 |
|
|
|
|||
| $2,001–$5,000 |
|
|
|
|||
| $2,000 or Less |
|
|
|
|
||
| Mean Charge (SD) | $239,749 (SD = $37,941) | $55,792 (SD = $34,246) | $10,561 (SD = $10,194) | $4,788 (SD = $9,120) | ||
Infant died at 18 days; no mean charge was calculated for the remaining infant.
The highest initial-hospitalization charge for infants born after 28 weeks’ gestation was $100,000. One full-term infant experienced complications and incurred a hospital charge of $57,537.
We used one-way analysis of variance with Scheffé tests for post hoc comparisons. Three categories—the preterm category of less than 26 weeks’ gestation as well as the 26-through-28- and 29-through-32-weeks groups—had significantly higher mean hospital charges than the 33-through-36-weeks group and the 37-weeks-or-greater group. In the three shorter-gestation categories, increasing gestational age resulted in significantly lower mean initial hospital charges (F = 79.5, P < 0.001).
Birth weight
Charges for initial hospitalization after birth also decreased with increasing birth weights (see Table 2, page 62). Four of the five infants born weighing 1,250 g or less had hospital charges ranging from $200,576 to $283,137. One infant born weighing 676 g, who died in 18 days, had lower charges. The group of infants weighing 1,250 g or less at birth had significantly higher hospital charges than all other groups. Hospital charges for the 1,251-to-1,500-g group were significantly higher than hospital charges for the 2,001-to-2,499-g and 2,500-g-or-greater groups (F = 208.8, P < 0.01).
Table 2.
Initial hospital charges by infants’ birth weight (N = 84)
| Infant Birth Weight (in grams) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Initial Hospital Charge | Total No. of Infants | ≤ 1,000 (n = 4) | 1,001–1,250 (n = 1 | 1,251–1,500 (n = 2) | 1,501–1,750 (n = 0) | 1,751–2,000 (n = 4) | 2,001–2,499 (n = 18) | ≥ 2,500 (n = 55) |
| > $200,000 |
|
|
|
|||||
| $150,001–$200,000 | — | |||||||
| $100,001–$150,000 | — | |||||||
| $50,001–$100,000 |
|
|
|
|
|
|||
| $25,001–$50,000 |
|
|
|
|
||||
| $15,001–$25,000 |
|
 * *
|
|
|
|
|||
| $5,001–$15,000 |
|
|
|
|||||
| $2,001–55,000 |
|
|
|
|||||
| $2,000 or Less |
|
|
|
|
||||
| Mean Charge (SD) | $250,596 (SD = $37,819) | $74,569 (SD = $1,458) | $32,169 (SD = $32,693)† | $16,944 (SD = $23,344)† | $5,816 (SD = $9,319)† | |||
Infant died at 18 days; charges for the infant not included in calculating mean charge for infants in very-low-birth-weight categories.
Charges for these three birth-weight groups were not significantly different from one another.
Rehospitalizations and acute care visits
Gestational age
The proportion of infants rehospitalized in the first year of life was slightly higher in the group of 41 preterm infants (27%) than in the group of 43 full-term infants (24%), but this wasn’t a statistically significant difference (χ2 = 0.1, P = 0.75). The rehospitalized group included 60% of those born at less than 28 weeks’ gestation, 14% of those born at 29 through 32 weeks, and 24% of those born at 33 through 36 weeks, all of whom had at least one rehospitalization. One infant in the 26-through-28-weeks group required four rehospitalizations. (See Figure 2, page 63.)
Figure 2.
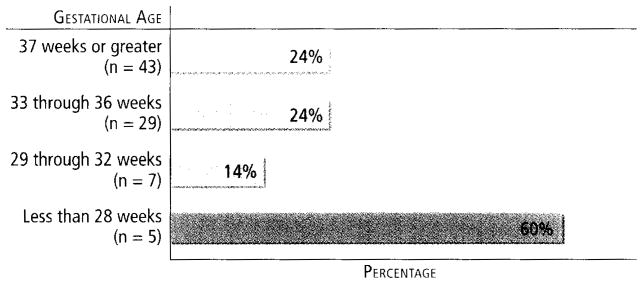
Percentages of Infants Rehospitalized at Least Once During the First Year of Life, by Gestational Age (N = 84)
However, the proportion of infants who required acute care visits (visits that weren’t routinely scheduled) to a health care provider in the first year of life increased with increasing gestational age: 67% of the 43 full-term infants, compared with only 54% of the 41 preterm infants, although the difference wasn’t statistically significant (χ2 = 1.67, P = 0.2). In the preterm group, 40% of those born at less than 28 weeks’ gestation, 50% of those born between 29 and 32 weeks’ gestation, and 55% of those born between 33 and 36 weeks’ gestation required at least one acute care visit. One infant born between 33 and 36 weeks’ gestation required six acute care visits in the first year of life. (See Figure 3, page 63.)
Figure 3.
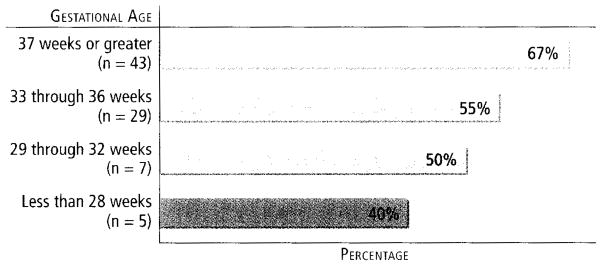
Percentages of Infants Who Required at Least One Acute Care Visit in the First Year of Life, by Gestational Age (N = 84)
Birth weight
In the analysis according to birth weight, the pattern of rehospitalizations and acute care visits was similar to that by gestational age. A greater proportion of infants born at low birth weights (31% of 29 infants) required at least one rehospitalization during the first year of life, compared with those born at normal weight (22% of 55 infants), although the difference was not statistically significant (χ2 = 0.78, P = 0.38). Two low-birth-weight infants required two rehospitalizations, one infant had three, and one required four. However, a significantly smaller proportion of low-birth-weight infants (45%) required acute care visits in the first year, compared with normal-birth-weight infants (69%) (X2 = 4.69, P = 0.03). One normal-weight infant required 12 visits.
DISCUSSION
Study data clearly demonstrate the effects of prematurity and low birth weight on health care charges, showing that the charges for initial hospitalizations increased as birth weights and gestational ages decreased.
Mean hospital charges ranged from $5,816 for infants born at normal weight (including one infant with complications who incurred a charge of $57,537) to $205,204 for the 1,250-g-or-less group (including an infant with lower charges who died at 18 days).
A similar picture is seen when comparing charges across gestational ages. Mean hospital charges ranged from $4,788 for those born after 37 or more completed weeks of gestation to $239,749 for infants born between 26 and 28 weeks’ gestation. These findings are consistent with those reported previously.1–4,6–8
Previous research on acute care visits and rehospitalization of low-birth-weight infants in the first year of life indicates that such infants have a higher rate of rehospitalization and acute care visits than normal-weight infants. In this study, 22% of normal-weight infants were rehospitalized in the first year of life, compared with 31 % of low-birth-weight infants, and 23% of full-term infants were hospitalized, compared with 27% of infants born preterm, although neither difference was statistically significant. These findings are similar to those of McCormick and colleagues.16
This analysis also indicated a higher rate of acute care visits in full-term infants (67%), compared with preterm infants (54%), and a higher rate of acute care visits in normal-weight infants (69%) than in low-birth-weight infants (45%). The latter difference, which was statistically significant, may be due to the fact that lower-birth-weight infants are seen more frequently for regularly scheduled visits because of their high-risk status. Also, parents of normal-birth-weight infants may be anxious to have their infants seen by health care providers. Normal-weight infants aren’t routinely seen as often as low-birth-weight or preterm infants. Another possibility is that a larger proportion of normal-birth-weight and full-term infants may be enrolled in family or organized day care, where they come into contact with other children, resulting in more upper respiratory and ear infections.
This study clearly demonstrates that even small increases in gestational age at birth and in birth weight result in cost savings for the initial hospital stay and fewer rehospitalizations in the first year of life. The rates of preterm births and low-birth-weight births as percentages of all births have increased over the past decade.4 Advances in prenatal and neonatal care have resulted in more infants surviving at increasingly shorter gestations, increasing health care costs. Interventions to improve prenatal care targeted to women at high risk for delivering preterm or low-birth-weight infants might not only reduce health care costs, but might improve health outcomes of infants as well.15
Maternal conditions, such as infection, hypertension, diabetes, and history of preterm birth, and behaviors associated with poor health, such as smoking, inadequate nutrition, and substance abuse, are strongly associated with low birth weight.4 With adequate prenatal care, high-risk physiologic conditions and behaviors can be monitored and treated. In 2000 data indicated that the proportion of pregnant women who received timely prenatal care was improving because of aggressive outreach programs and alternative methods of prenatal care delivery such as off-site clinics and mobile vans. However, despite these efforts, in 2003, 3.5% of all mothers received late or no prenatal care.4
Many women receive inadequate prenatal care because of a lack of child care or transportation, long waiting periods in a provider’s office or clinic, and other financial and personal hurdles. Waiting times in one study averaged 3.22 hours, while provider time often is as little as five minutes.17 Pregnant women at high risk for delivering low-birth-weight infants are often seen very frequently, increasing these difficulties. Reducing the number of preterm and low-birth-weight births will require more comprehensive education of infertile couples who seek technologic solutions to their infertility, and better application of that technology by providers. Local, regional, and national efforts to improve the education of childbearing couples and those considering becoming pregnant, as well as efforts to reduce barriers to care, could reduce initial health care costs associated with preterm and low-birth-weight infants. Such efforts should also pay dividends by reducing health care and educational costs in the longer term for these children and their families.
Why Every Nurse Should Be Concerned About Prematurity: If you treat women, you can help prevent preterm births.
Prematurity is an intractable public health concern in the United States. Significant health care resources are expended on it, and the financial and emotional costs to families and communities are staggering. It’s an area in which the nation is clearly backsliding (the incidence of prematurity has been rising for two decades), and it’s an example of gross racial and ethnic disparities in health care outcomes.1
Recently the March of Dimes initiated a five-year campaign to educate consumers, health care providers, and policymakers on the seriousness of the problem (see ). Each year, approximately 470,000 premature infants are born in the United States; estimates of the annual cost exceed $10 billion.2
In the United States, 12.3% of all births are premature,3 while the national goal articulated in Healthy People 2010 is 7.6%.4 Each year, the United States—the richest country on earth—lags behind 18 to 20 countries in infant mortality, and prematurity contributes to this (for more on prematurity worldwide, see ). Racial and ethnic disparities are glaring: 17.6% of African American, 12.9% of Native American, 11.4% of Hispanic, 10.7% of white, and 10.7% of Asian American newborns are premature. The incidence has increased 13% from 1992 to 2002 despite intensive efforts by the government and private foundations to stem the tide. We know that prematurity risk decreases with early and frequent prenatal care, but often those most at risk don’t have access to adequate care.
An additional risk factor is the age of the mother, particularly if she is older than 35 or younger than 20. Older women already have a higher risk of giving birth prematurely because there’s a greater prevalence of preexisting diseases, such as diabetes and hypertension, among them. They also tend to use reproductive technologies to manage infertility more often younger women do, leading to more multiple pregnancies and premature births. Young mothers often have the added independent risk factors of unplanned pregnancy, infection (including but not limited to urinary tract infections and sexually transmitted diseases), and poor nutrition. Both underweight and obesity, the latter a national epidemic, also increase the incidence of prematurity.
Few nurses in practice are completely removed from issues related to prematurity, which include the following: the increased incidence of severe disabilities and the reduced likelihood of completing high school and attending college associated with the earlier births of smaller babies5,6; the association of prematurity with maternal drug abuse and smoking; the fact that women are choosing to have babies in their late 30s, 40s, and beyond; and the growing recognition that women who have experienced racism and violence may be more likely to give birth prematurely.7
Prematurity is more than a health issue; it’s a matter of social justice. A solution to this problem will require the efforts of all health care personnel who work with pregnant women and women who may bear children. For nurses in administrative and health policy positions, the choices of where to direct scarce health care dollars will only become more difficult in the face of such trends as the aging of the baby boom generation and the expected increased incidence of diabetes and heart disease associated with our national obesity epidemic. While technologic innovations have done much to improve the prognosis of infants born prematurely, in the future real progress toward solving both the financial and health problems associated with prematurity will be made only with increased emphasis on prevention. Nurses can play an important role in preventing premature births by becoming well informed about the multifaceted nature of prematurity, educating women on it, identifying risk factors in their patients as early as possible and recommending timely interventions, and being strong advocates for universal access to health care. —Nancy C. Sharts-Hopko, PhD, RN, FAAN, professor and director of the doctoral program at the Villanova University College of Nursing, Villanova, PA.
REFERENCES
- 1.Mattison DR, et al. Preterm delivery: a public health perspective. Paediatr Perinat Epidemiol. 2001;15 (Suppl 2):7–16. doi: 10.1046/j.1365-3016.2001.00004.x. [DOI] [PubMed] [Google Scholar]
- 2.March of Dimes. Prematurity: the answers can’t come soon enough. 2005 http://vvww.marchofdimes.com/prematurity/15341_10734.asp.
- 3.Hamilton BE, et al. Births: preliminary data for 2003. Natl Vital Stat Rep. 2004;53(9):1–17. [PubMed] [Google Scholar]
- 4.The U.S. Department of Health and Human Services. Healthy People 2010: 16-11. Reduce preterm births. 2005 http://www.heaIthypeople.gov/document/html/objectives/16-11.htm.
- 5.Hack M, et al. Outcomes in young adulthood for very-low-birth-weight infants. N Engl J Med. 2002;346(3):149–57. doi: 10.1056/NEJMoa010856. [DOI] [PubMed] [Google Scholar]
- 6.Marlow N, et al. Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med. 2005;352(1):9–19. doi: 10.1056/NEJMoa041367. [DOI] [PubMed] [Google Scholar]
- 7.Rich-Edwards J, et al. Maternal experiences of racism and violence as predictors of preterm birth: rationale and study design. Paediatr Perinat Epidemiol. 2001;15 (Suppl 2):124–35. doi: 10.1046/j.1365-3016.2001.00013.x. [DOI] [PubMed] [Google Scholar]
Nurses who work in areas other than obstetrics lor gynecology might assume that the problem of preterm birth isn’t their concern. If this statement applies to you, think again. Whenever you take care of a woman who is of childbearing age, you have an opportunity to help prevent preterm birth.
The article by Cuevas and colleagues joins the numerous other scholarly articles that have, over the past 25 years, documented the distressing history of a common but serious problem that’s only gotten worse over the years. The rate of preterm birth has increased by 28% since 1983, and was 12.3% in 2003.1 Even if you’ve never taken care of a woman in preterm labor, you probably know someone—a family member, a friend—who’s delivered a preterm infant. The March of Dimes has committed itself to a campaign to stop the scourge of preterm birth and unhealthy birth outcomes in the United States. This campaign has two main goals: between 2003 and 2010, the March of Dimes wants to increase awareness of the problem of preterm birth and decrease the rate of preterm birth, from “12.1% in 2002 to 7.6% in 2010.”
Why increase public awareness? Because many people simply don’t understand that having a baby prematurely is dangerous. Part of the reason for that may be that our colleagues in neonatal intensive care do such a great job that the message about how important it is to stay pregnant for the full 40 weeks of gestation has become lost. But we need to help the general public understand the devastating sequelae of preterm birth. The March of Dimes is also committed to urging corporate and civic leaders to take action on the issue, rather than merely discuss it—helping them to understand why preterm birth has such astronomical costs for society. The March of Dimes will invest in media advertising and be an advocate of state and federal funding of research. The March of Dimes will lead the way by investing in research on the causes of preterm labor (only half of preterm births have a known cause) and will work toward educating women and health care providers on the seriousness and prevalence of prematurity.
HOW CAN YOU HELP?
You can teach women of childbearing age—your patients, sisters, friends, and neighbors—about the dangers of preterm birth and help them to reduce some of their risk factors. The following are some specific risk-reduction messages you can deliver to women.
Strive for optimal health.
Take a multivitamin daily (folic acid is known to prevent birth defects if taken before conception).
Avoid alcohol, tobacco, and illegal drugs.
Achieve your ideal weight before getting pregnant.
If you know pregnant women (patients or others), you can help them to understand the signs and symptoms of preterm labor and explain what to do if the symptoms appear. You can also tell women about the March of Dimes Web site ( ), where they can get all the information they need about preterm labor. Patient education materials are available in print and on videotape and DVD.
Even if you don’t work in perinatal health, you can help to prevent preterm birth by becoming knowledgeable about the March of Dimes prematurity campaign. We look forward to your participation. — Margaret Comerford Freda, EdD, RN, CHES, FAAN, chairperson of the March of Dimes National Nurse Advisory Council and a professor of obstetrics and gynecology and women’s health at Albert Einstein College of Medicine, Montefiore Medical Center, Bronx, NY.
REFERENCE
- 1.Hamilton BE, et al. Births: preliminary data for 2003. Natl Vital Stat Rep. 2004;53(9):1–17. [PubMed] [Google Scholar]
Acknowledgments
This study is a secondary analysis of data on a subset of infants drawn from a randomized clinical trial funded by the National Institute for Nursing Research. National Institutes of Health (grant no. ROl NR02897).
Footnotes
The authors of this article have no significant ties, financial or otherwise, to any company that might have an interest in the publication of this educational activity.
Contributor Information
Katherine D. Cuevas, VITAS Innovative Hospice Care in Miami, FL.
Debra R Silver, Institute for Mental Health, St. Mary’s Medical Center, West Palm Beach, FL.
Dorothy Brooten, Florida International University School of Nursing, Miami.
JoAnne M. Youngblut, Florida International University School of Nursing, Miami.
Charles M. Bobo, Florida International University School of Nursing, Miami.
References
- 1.Morrison J, et al. Telemedicine: cost-effective management of high-risk pregnancy. Manag Care. 2001;10(11):42–6. 48–9. [PubMed] [Google Scholar]
- 2.Rogowski J. Cost-effectiveness of care for very low birth weight infants. Pediatrics. 1998;102(1 Pt 1):35–43. doi: 10.1542/peds.102.1.35. [DOI] [PubMed] [Google Scholar]
- 3.St John EB, et al. Cost of neonatal care according to gestational age at birth and survival status. Am J Obstet Gynecol. 2000;182(1 Pt 1):170–5. doi: 10.1016/s0002-9378(00)70509-6. [DOI] [PubMed] [Google Scholar]
- 4.Hamilton BE, et al. Births: preliminary data for 2003. Natl Vital Stat Rep. 2004;53(9):1–17. [PubMed] [Google Scholar]
- 5.Martin JA, et al. Births: final data for 2002. 2003 http://www.cdc.gov/nchs/data/nvsr/nvsr52/nvsr52_10.pdf. [PubMed]
- 6.Mozurkewich EL, et al. Predicting preterm birth: a cost-effectiveness analvsis. Am J Obstet Gynecol. 2000;182(6):1589–98. doi: 10.1067/mob.2000.106855. [DOI] [PubMed] [Google Scholar]
- 7.Petrou S, et al. The long-term costs of preterm birth and low birth weight: results of a systematic review. Child Care Health Dev. 200l;27(2):97–115. doi: 10.1046/j.1365-2214.2001.00203.x. [DOI] [PubMed] [Google Scholar]
- 8.Zupancic JA, et al. Economics of prematurity in the era of managed care. Clin Perinatal. 2000;27(2):483–97. doi: 10.1016/s0095-5108(05)70032-4. [DOI] [PubMed] [Google Scholar]
- 9.Shinwell ES. Neonatal and long-term outcomes of very low birth weight infants from single and multiple pregnancies. Semin Neonatal. 2002;7(3):203–9. doi: 10.1053/siny.2002.0107. [DOI] [PubMed] [Google Scholar]
- 10.March of Dimes. Prematurity: a national health crisis. 2005 http://www.marchofdimes.com/premaruritv/5413_11560.asp.
- 11.Brooten D, et al. A randomized clinical trial of early hospital discharge and home follow-up of verv-low-birth-weight infants. N Engl J Med. 1986;315(15):934–9. doi: 10.1056/NEJM198610093151505. [DOI] [PubMed] [Google Scholar]
- 12.Stevenson RC, et al. Cost of care for a geographically determined population of low birthweight infants to age 8–9 years. I: children without disability. Arch Dis Child Fetal Neonatal Ed. 1996;74(2):F114–7. doi: 10.1136/fn.74.2.f114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tommiska V, et al. Economic costs of care in extremely low birthweight infants during the first 2 years of life. Pediatr Crit Care Med. 2003;4(2):157–63. doi: 10.1097/01.PCC.0000059731.74435.02. [DOI] [PubMed] [Google Scholar]
- 14.Petrou S, et al. The impact of preterm birth on hospital inpatient admissions and costs during the first 5 years of life. Pediatrics. 2003;112(6 Pt 1):1290–7. doi: 10.1542/peds.112.6.1290. [DOI] [PubMed] [Google Scholar]
- 15.Brooten D, et al. A randomized trial of nurse specialist home care for women with high-risk pregnancies: outcomes and costs. Am J Manag Care. 2001;7(8):793–803. [PMC free article] [PubMed] [Google Scholar]
- 16.McCormick MC, et al. Costs incurred by parents of very low birth weight infants after the initial neonatal hospitalization. Pediatrics. 1991;88(3):533–41. [PubMed] [Google Scholar]
- 17.Stringer M. Personal costs associated with high-risk prenatal care attendance. J Health Care Poor underserved. 1998;9(3):222–35. doi: 10.1353/hpu.2010.0248. [DOI] [PubMed] [Google Scholar]