Abstract
Amblyopia, a developmental disorder of the visual cortex, is one of the leading causes of visual dysfunction in the working age population. Current estimates put the prevalence of amblyopia at approximately 1-3%1-3, the majority of cases being monocular2. Amblyopia is most frequently caused by ocular misalignment (strabismus), blur induced by unequal refractive error (anisometropia), and in some cases by form deprivation.
Although amblyopia is initially caused by abnormal visual input in infancy, once established, the visual deficit often remains when normal visual input has been restored using surgery and/or refractive correction. This is because amblyopia is the result of abnormal visual cortex development rather than a problem with the amblyopic eye itself4,5 . Amblyopia is characterized by both monocular and binocular deficits6,7 which include impaired visual acuity and poor or absent stereopsis respectively. The visual dysfunction in amblyopia is often associated with a strong suppression of the inputs from the amblyopic eye under binocular viewing conditions8. Recent work has indicated that suppression may play a central role in both the monocular and binocular deficits associated with amblyopia9,10 .
Current clinical tests for suppression tend to verify the presence or absence of suppression rather than giving a quantitative measurement of the degree of suppression. Here we describe a technique for measuring amblyopic suppression with a compact, portable device11,12 . The device consists of a laptop computer connected to a pair of virtual reality goggles. The novelty of the technique lies in the way we present visual stimuli to measure suppression. Stimuli are shown to the amblyopic eye at high contrast while the contrast of the stimuli shown to the non-amblyopic eye are varied. Patients perform a simple signal/noise task that allows for a precise measurement of the strength of excitatory binocular interactions. The contrast offset at which neither eye has a performance advantage is a measure of the "balance point" and is a direct measure of suppression. This technique has been validated psychophysically both in control13,14 and patient6,9,11 populations.
In addition to measuring suppression this technique also forms the basis of a novel form of treatment to decrease suppression over time and improve binocular and often monocular function in adult patients with amblyopia12,15,16 . This new treatment approach can be deployed either on the goggle system described above or on a specially modified iPod touch device15.
Keywords: Medicine, Issue 70, Ophthalmology, Neuroscience, Anatomy, Physiology, Amblyopia, suppression, visual cortex, binocular vision, plasticity, strabismus, anisometropia
Protocol
1. The Measurement of Suppression
Before beginning the measurement of suppression, give the patient detailed instructions (see 1.8) and show the visual stimuli relating to steps 1.2-1.8 below on the laptop screen. All patients should wear full refractive correction (glasses/contact lenses) throughout the procedure, suitably adjusted for the working distance.
The goggles (eMagin 8700) should be fitted to the patient (over the top of spectacles/contact lenses) and properly adjusted. Ensure that the screens sit parallel to the ocular surface. The screens can be adjusted to account for each patient's interpupillary distance. Instructions for connecting and calibrating the goggles can be found here: http://www.3dvisor.com/wpcontent/uploads/2010/08/UserGuide10.7.pdf.
The stimuli consist of two populations of moving dots, one population moving in a common direction (the 'signal' dots) and the other moving in random directions (the 'noise' dots). The observer's task is to report the signal direction. Task difficulty is manipulated by varying the relative proportion of signal to noise dots in the stimulus.
The custom Matlab programs which control these measurements utilize a 3-down 1-up staircase procedure. There are two separate measurement stages. The first provides a binocular threshold, that is, the threshold number of signal dots required when both signal and noise dots are presented to both eyes at high contrast. The second program measures the contrast imbalance required to achieve the same threshold when the dot populations are presented to separate eyes.
Different images are displayed on the goggles screens through the use of a Matrox DualHead2Go, (Montreal, Canada) device.
To begin the suppression assessment, first measure a binocular threshold. Here the same visual stimuli are shown to both eyes and the minimum number of signal dots required to accurately judge the direction of the dot movement is measured.
To align the eyes, the screens will display a black half cross in each eye against a white screen. Using the keyboard, the patient is asked to move the half of the cross seen by the amblyopic eye until it lines up with the half seen by the fellow eye. It is important that the patient is advised that the image seen by the amblyopic eye may be blurry, but it is the alignment that is important. If the moving image disappears from view ask the patient to blink more frequently as this may improve the visibility of the image. Exact ocular alignment (pixel values) can be extracted following each measurement to ascertain the repeatability of this task.
Once the patient reports that the half crosses are aligned, the measurement procedure can begin. Each measurement takes about three minutes to complete. Five short staircase measurements are completed for each of the two parts of the measurement. The following instructions should be given before the measurement begins:
Instructions for the observer: "During this test you will be asked to make a judgment about the direction of moving images." "You will see a group of white/grey dots against a grey background. After each presentation I will ask you to decide if the dots are mostly moving to the left or right using the left and right arrow keys on the keyboard in front of you." "There are two groups of dots, some move smoothly to the left or right (the signal dots), the other group appear to move in random directions." "Please try to decide which direction the signal dots are moving in (right or left) amongst the confusion of the random dots." "As you continue to make decisions the number of random dots will increase, making it more difficult to see the signal dots, when it gets so difficult you cannot tell the direction, please just take your best guess".
The first measurement can now start. A good 'last minute' instruction is to remind the participant to blink regularly ("a good time to blink is when you press the button").
Five measurements using the binocular staircase paradigm are now made. Ocular alignment is repeated before each measurement is started.
The result obtained from each measurement is the threshold number of signal dots (out of 100 dots total) required to correctly judge the direction when both eyes see the same stimuli. The program also reports the range of responses as a standard error of the measurement.
For the next measurement, the contrast staircase, the five results from the binocular staircases are averaged and the resulting threshold defines the number of signal dots presented to the amblyopic eye. The remaining noise dots are presented to the non-amblyopic eye at varying contrasts to assess suppression.
For this measurement the amblyopic eye always sees high contrast dots whereas the contrast of the noise dots shown to the non-amblyopic eye is varied using a staircase procedure. At the start of the staircase a fixed number of signal dots (obtained from step 1.11) are shown to the amblyopic eye at 100% contrast and the remaining number of noise dots are shown to the fellow eye at 0% contrast (i.e. no noise dots are visible resulting in minimal suppression). Correct identification of the signal dot direction results in an increase in the contrast of the noise dots shown to the fellow eye according to the 3-down 1-up staircase algorithm. Throughout the measurement, the contrast of the noise dots shown to the fellow eye is varied by the staircase until task performance converges on 79% correct. This indicates that the signal and noise dots are being combined between the two eyes to produce the same level of task performance that was observed under binocular viewing conditions (step 1.11). The ratio of the contrast of the signal dots presented to the amblyopic eye (always 100%) relative to the contrast of the noise dots shown to the fellow eye at threshold is a measure of the balance point. Increasing the contrast of the noise dots shown to the fellow eye above this point would result in suppression of the signal dots shown to the amblyopic eye and impairment in task performance.
Five measurements are made of the contrast imbalance and an average result is calculated. The result informs the examiner about the level of contrast imbalance that is necessary to overcome suppression and allow the amblyopic eye and fellow eye to see the dots simultaneously.
2. Training Using this Method
The contrast imbalance found in step 1.14 above can be used as a starting point for a training regime. The training involves integrating the use of dichoptic images with the contrast imbalance into a video game format ("tetris"). The video game can be implemented on either the virtual reality goggles or on an ipod touch device.
The video game tetris involves a series of falling blocks which are fitted together to form complete lines. The amblyopic eye sees full contrast blocks, and the fellow eye sees reduced contrast images. Information presented to each eye must be perceived simultaneously for successful play.
Over time as the training regime continues the contrast imbalance is reduced by increasing the contrast to the fellow eye, making it more difficult for the visual system to overcome the suppression caused by more similar dichoptic images.
Training duration should be 1-2 hr a day and should be continued until no further improvement in contrast imbalance (increase in contrast presented to the fellow eye) is observed. During the training regime, checks of monocular and binocular function should be made regularly (determined by age of patient and underlying condition). Tests of monocular visual acuity, stereopsis and standard tests of suppression are particularly important for reporting progress.
Representative Results
The level of suppression found in the described method is dependent on the underlying cause of the amblyopia, previous treatment, use of refractive correction and visual acuity. Because each patient has a very unique history, it is difficult to define 'normal' values of suppression or make comparisons between people. Generally we expect those with worse visual acuity to have a deeper level of suppression9. During training, as we reduce the contrast imbalance between the eyes, the depth of suppression typically reduces and this improves a range of binocular and monocular functions. This change in suppression has been demonstrated in several patient populations (see Figures 3 and 4 in reference12, Table 3 and Figure 9 in reference 15 and Figure 2 in reference 16). It is important to note that detailed measurements of suppression using this technique have the potential to enhance our understanding of the amblyopia syndrome.
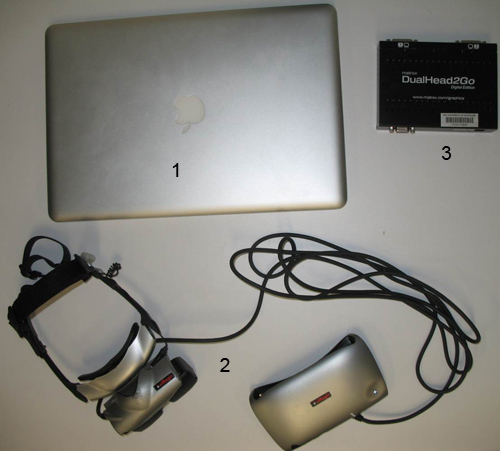 Figure 1. The equipment used for measuring suppression which includes 1) laptop 2) goggles 3) signal splitter.
Figure 1. The equipment used for measuring suppression which includes 1) laptop 2) goggles 3) signal splitter.
 Figure 2. The goggles fitted correctly on a study participant.
Figure 2. The goggles fitted correctly on a study participant.
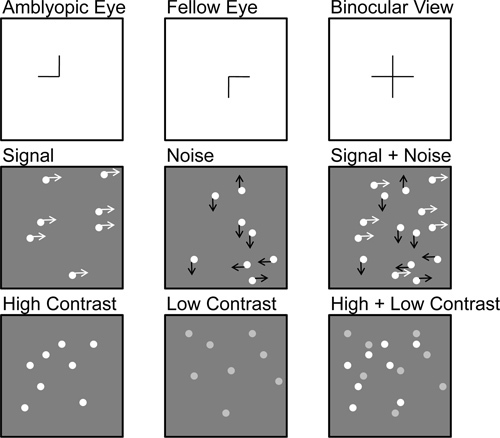 Figure 3. An overview of the random dot kinetogram stimuli (Step 1.2/1.3). The top panel demonstrates the alignment phase where a half cross is displayed to each eye monocularly as a cue for binocular alignment. The middle panel demonstrates the signal to noise paradigm where signal dots are presented to the amblyopic eye only and the noise dots are presented to the fellow eye, under binocular conditions the signal and noise are combined to give a motion coherence threshold which is then utilized in the contrast varying stage of the measurement. The bottom panel demonstrates the contrast threshold, this procedure uses the motion coherence threshold at a fixed level of signal to noise, and displays varying contrast levels between the two eyes. The point at which the two eyes see a balanced binocular input is the contrast threshold or "balance point".
Figure 3. An overview of the random dot kinetogram stimuli (Step 1.2/1.3). The top panel demonstrates the alignment phase where a half cross is displayed to each eye monocularly as a cue for binocular alignment. The middle panel demonstrates the signal to noise paradigm where signal dots are presented to the amblyopic eye only and the noise dots are presented to the fellow eye, under binocular conditions the signal and noise are combined to give a motion coherence threshold which is then utilized in the contrast varying stage of the measurement. The bottom panel demonstrates the contrast threshold, this procedure uses the motion coherence threshold at a fixed level of signal to noise, and displays varying contrast levels between the two eyes. The point at which the two eyes see a balanced binocular input is the contrast threshold or "balance point".
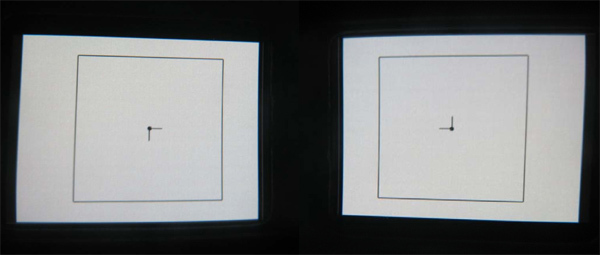 Figure 4. (Step 1.7) Alignment screens as seen through the goggles, horizontal and vertical arrow keys are used to align targets until an entire cross is seen.
Figure 4. (Step 1.7) Alignment screens as seen through the goggles, horizontal and vertical arrow keys are used to align targets until an entire cross is seen.
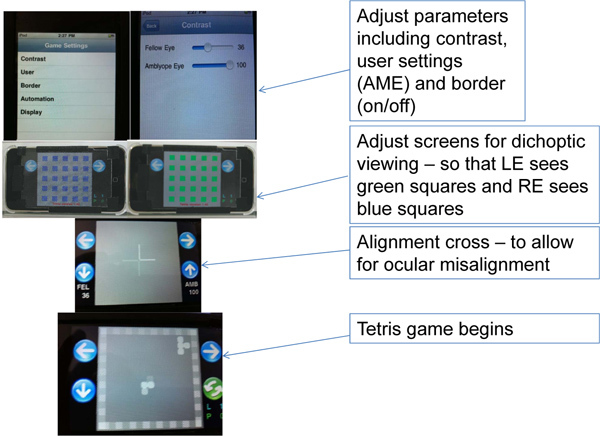 Figure 5. An overview of the training protocol.
Figure 5. An overview of the training protocol.
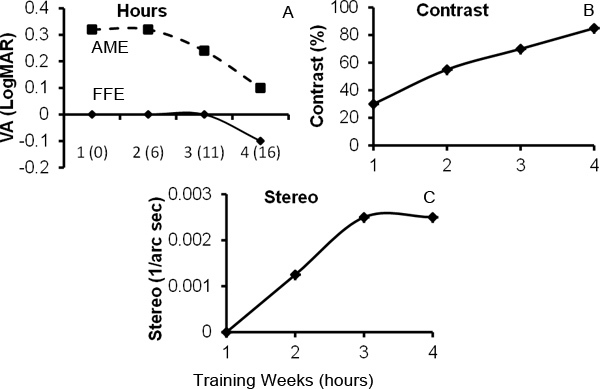 Figure 6. Example of clinical and psychophysical data obtained from one adult participant with strabismic amblyopia who completed the training procedure (steps 2.1 to 2.4). Figure 6A demonstrates the change in visual acuity (measured with a logarithmic style chart in logMAR units over four weeks of training for both the amblyopic eye (AME) and fellow eye (FFE)). Smaller LogMAR values indicate better visual acuity. The cumulative number of hours of game play is shown in brackets on the x-axis. Figure 6B demonstrates the change in contrast imbalance over four weeks of training. The y-axis shows the contrast that could be tolerated in the fellow eye, therefore larger values indicate less suppression. At the start of training only 30% contrast could be tolerated in the fellow eye before the amblyopic eye was suppressed. However as training progressed, more contrast could be tolerated indicating a reduction in suppression. Figure 6C shows the improvement in stereoacuity over the training period (measured with the Randot stereo test). Zero on the y-axis indicates no stereo vision and increasing values indicate improving stereo sensitivity (units are the reciprocal of the stereo threshold in seconds of arc).
Figure 6. Example of clinical and psychophysical data obtained from one adult participant with strabismic amblyopia who completed the training procedure (steps 2.1 to 2.4). Figure 6A demonstrates the change in visual acuity (measured with a logarithmic style chart in logMAR units over four weeks of training for both the amblyopic eye (AME) and fellow eye (FFE)). Smaller LogMAR values indicate better visual acuity. The cumulative number of hours of game play is shown in brackets on the x-axis. Figure 6B demonstrates the change in contrast imbalance over four weeks of training. The y-axis shows the contrast that could be tolerated in the fellow eye, therefore larger values indicate less suppression. At the start of training only 30% contrast could be tolerated in the fellow eye before the amblyopic eye was suppressed. However as training progressed, more contrast could be tolerated indicating a reduction in suppression. Figure 6C shows the improvement in stereoacuity over the training period (measured with the Randot stereo test). Zero on the y-axis indicates no stereo vision and increasing values indicate improving stereo sensitivity (units are the reciprocal of the stereo threshold in seconds of arc).
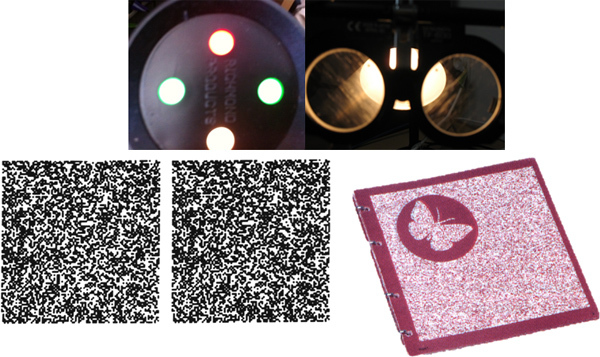 Figure 7. Standard clinical tests used to assess binocular vision status before and after training including the Worth 4 dot test (top left), Bagollini lenses (top right), Randot Stereopsis test (bottom left) and TNO stereopsis test (bottom right).
Figure 7. Standard clinical tests used to assess binocular vision status before and after training including the Worth 4 dot test (top left), Bagollini lenses (top right), Randot Stereopsis test (bottom left) and TNO stereopsis test (bottom right).
Discussion
The suppression measurement and treatment techniques described in this paper critically depend on manipulation of the contrast of the images seen by each eye. Specifically, the relative interocular contrast imbalance at which binocular combination occurs, i.e. the "balance point contrast", provides a measure of suppression6,11,17 . In addition, by repeatedly exposing patients with amblyopia and suppression to "balanced" visual stimuli, it is possible to reduce suppression and potentially improve both monocular and binocular visual function12,15,16 . These techniques represent an advance in suppression measurement and a new approach to amblyopia treatment respectively. Currently available clinical tests for assessing suppression such as the Worth 4 lights test and the Bagolini striated lenses assess whether suppression is present or absent, and other tests such as the sbisa bar quantify the level of suppression by the use of neutral density filters. Our technique provides additional clinical information by allowing for the strength of suppression to be precisely quantified. Amblyopia, which is often associated with suppression, is generally treated by occluding the non-amblyopic eye or degrading the image in the non-amblyopic eye in order to encourage use of the amblyopic eye18. While this technique is effective in improving amblyopic eye function18, it does not directly address the binocular deficits associated with amblyopia. Our technique directly targets binocular visual function and we have found that this approach can improve both monocular and binocular function in adult patients with amblyopia12,15,16. The measurement and treatment approaches described are suitable for use in adults and children, although the games may need to be adapted for use in younger pediatric populations. We are currently developing additional games for this purpose.
Our techniques do have limitations. Some patients with a strabismus and strong suppression find it challenging to align the images shown to each eye at the start of the suppression measurement protocol. While it is possible for such patients to align the images17, this can be time consuming. With regards to treatment it is important to work alongside a suitably qualified clinician throughout the training regime, and to consider the risk of diplopia (double vision) if suppression is reduced. Our prior work on this treatment approach has focused on patients with anisometropia or small-angle strabismus and no patients have developed diplopia, however the risk of diplopia should be carefully considered by a suitably qualified clinician on a patient by patient basis before the treatment is administered.
When setting up the techniques for the first time it is important to ensure that all hardware connections are secure and that all relevant drivers are installed and updated on the host computer. It is also important to use a computer equipped with a graphics card that is compatible with the Matrox graphics board described in the protocol and that supports a screen resolution of 1600x600 (once the Matrox drivers are installed) to ensure that each goggle screen has a distinct image. We have found that most problems encountered when setting up the system occur due to incorrect screen resolution settings and the absence of up to date drivers for the necessary hardware. It is also important to ensure that both goggle screens have equal luminance prior to measuring suppression to ensure accurate and stable measurements.
The techniques described provide a foundation for further development of suppression measurement and treatment approaches. In particular, the development of more engaging video games based on the core principle of varying contrast between the eyes could make this approach more efficient and more appealing to younger patients. Aside from their clinical use, these techniques can also be used in a research setting to explore the neural mechanisms underlying suppression and the role that inhibitory interactions between the eyes play in the normal visual system13.
Disclosures
The techniques described in this manuscript form the basis of two patents held by BT and RFH, one of which is also held by JC and LT.
References
- Webber AL, Wood J. Amblyopia: prevalence, natural history, functional effects and treatment. Clin. Exp. Optom. 2005;88:365–375. doi: 10.1111/j.1444-0938.2005.tb05102.x. [DOI] [PubMed] [Google Scholar]
- Dirani M, et al. Prevalence of refractive error in Singaporean Chinese children: the strabismus, amblyopia, and refractive error in young Singaporean Children (STARS) study. Invest. Ophthalmol. Vis. Sci. 2010;51:1348–1355. doi: 10.1167/iovs.09-3587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group, M.-e. P.E.D.S. Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months the multi-ethnic pediatric eye disease study. Ophthalmology. 2008;115:1229–1236. doi: 10.1016/j.ophtha.2007.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess RF, Li X, Lu G, Thompson B, Hansen BC. The contrast dependence of the cortical fMRI deficit in amblyopia; a selective loss at higher contrasts. Hum. Brain Mapp. 2010;31:1233–1248. doi: 10.1002/hbm.20931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Dumoulin SO, Mansouri B, Hess RF. Cortical deficits in human amblyopia: their regional distribution and their relationship to the contrast detection deficit. Invest. Ophthalmol. Vis. Sci. 2007;48:1575–1591. doi: 10.1167/iovs.06-1021. [DOI] [PubMed] [Google Scholar]
- Mansouri B, Thompson B, Hess RF. Measurement of suprathreshold binocular interactions in amblyopia. Vision Res. 2008;48:2775–2784. doi: 10.1016/j.visres.2008.09.002. [DOI] [PubMed] [Google Scholar]
- Agrawal R, Conner IP, Odom JV, Schwartz TL, Mendola JD. Relating binocular and monocular vision in strabismic and anisometropic amblyopia. Arch. Ophthalmol. 2006;124:844–850. doi: 10.1001/archopht.124.6.844. [DOI] [PubMed] [Google Scholar]
- Baker DH, Meese TS, Hess RF. Contrast masking in strabismic amblyopia: attenuation, noise, interocular suppression and binocular summation. Vision research. 2008;48:1625–1640. doi: 10.1016/j.visres.2008.04.017. [DOI] [PubMed] [Google Scholar]
- Li J, et al. The role of suppression in amblyopia. Invest. Ophthalmol. Vis. Sci. 2011;52:4169–4176. doi: 10.1167/iovs.11-7233. [DOI] [PubMed] [Google Scholar]
- Rahi J, Logan S, Timms C, Russell-Eggitt I, Taylor D. Risk, causes, and outcomes of visual impairment after loss of vision in the non-amblyopic eye: a population-based study. Lancet. 2002;360:597–602. doi: 10.1016/s0140-6736(02)09782-9. [DOI] [PubMed] [Google Scholar]
- Black JM, Thompson B, Maehara G, Hess RF. A compact clinical instrument for quantifying suppression. Optom. Vis. Sci. 2011;88:334–343. doi: 10.1097/OPX.0b013e318205a162. [DOI] [PubMed] [Google Scholar]
- Hess RF, Mansouri B, Thompson B. A binocular approach to treating amblyopia: antisuppression therapy. Optom. Vis. Sci. 2010;87:697–704. doi: 10.1097/OPX.0b013e3181ea18e9. [DOI] [PubMed] [Google Scholar]
- Li J, et al. Quantifying sensory eye dominance in the normal visual system: a new technique and insights into variation across traditional tests. Invest. Ophthalmol. Vis. Sci. 2010;51:6875–6881. doi: 10.1167/iovs.10-5549. [DOI] [PubMed] [Google Scholar]
- Zhang P, Bobier W, Thompson B, Hess RF. Binocular Balance in Normal Vision and Its Modulation by Mean Luminance. Optom. Vis. Sci. 2011. [DOI] [PubMed]
- To L, et al. A game platform for treatment of amblyopia. IEEE Trans. Neural Syst. Rehabil. Eng. 2011;19:280–289. doi: 10.1109/TNSRE.2011.2115255. [DOI] [PubMed] [Google Scholar]
- Hess RF, Mansouri B, Thompson B. A new binocular approach to the treatment of amblyopia in adults well beyond the critical period of visual development. Restor. Neurol. Neurosci. 2010;28:793–802. doi: 10.3233/RNN-2010-0550. [DOI] [PubMed] [Google Scholar]
- Goodman LK, Black JM, Phillips G, Hess RF, Thompson B. Excitatory binocular interactions in two cases of alternating strabismus. J. Aapos. 2011;15:345–349. doi: 10.1016/j.jaapos.2011.03.017. [DOI] [PubMed] [Google Scholar]
- Holmes JM, Clarke MP. Amblyopia. Lancet. 2006;367:1343–1351. doi: 10.1016/S0140-6736(06)68581-4. [DOI] [PubMed] [Google Scholar]
- Brainard DH. The Psychophysics Toolbox. Spat. Vis. 1997;10:433–436. [PubMed] [Google Scholar]
- Pelli DG. The VideoToolbox software for visual psychophysics: transforming numbers into movies. Spat. Vis. 1997;10:437–442. [PubMed] [Google Scholar]


