Abstract
Necrotizing enterocolitis (NEC) primarily affects premature infants. It is less common in term and late preterm infants. The age of onset is inversely related to the postmenstrual age at birth. In term infants, NEC is commonly associated with congenital heart diseases. NEC has also been associated with other anomalies. More than 85% of all NEC cases occur in very low birth weight infants or in very premature infants. Despite incremental advances in our understanding of the clinical presentation and pathophysiology of NEC, universal prevention of this disease continues to elude us even in the twenty-first century.
Keywords: Necrotizing enterocolitis, Isolated intestinal perforation, Peritoneal drainage, Microecology, Inflammation
Key points
-
•
There is an inverse relationship between postmenstrual age (PMA) at birth and risk of NEC. It is less common in term or late preterm infants.
-
•
Intestinal immaturity, aggressive feedings, and inflammatory response to interactions between intestinal epithelial barrier and luminal microbes are key contributors to NEC.
-
•
At an early stage, NEC is difficult to differentiate from sepsis. Intramural gas or pneumatosis and portal venous gas are pathognomonic signs of NEC.
-
•
Pneumoperitoneum, a sign of intestinal perforation and signs of intestinal gangrene including severe metabolic acidosis, persistent and severe thrombocytopenia, adynamic dilated intestinal loops require surgical intervention.
-
•
Research focused at identifying infants at increased risk of NEC combined with techniques aimed at early diagnosis, should decrease incidence and mortality of NEC.
From the nineteenth to the twenty-first century
In 1823, Charles Billard described what could be argued to be the first case report of necrotizing enterocolitis (NEC) as gangrenous enterocolitis in a small weak infant with infection, inflammation, and necrosis of the gastrointestinal tract (GIT).1 This report was followed in 1850 by a publication of a series of 25 term and preterm infants who presented with nonspecific clinical signs that rapidly progressed and resulted in death and who demonstrated similar pathologic findings on postmortem examinations.1 With the advent of special care nurseries in Europe during the first part of the twentieth century, the clinical description of NEC began to emerge; by the latter half, this disease was widely recognized as the most serious gastrointestinal emergency in intensive care nurseries worldwide. In 1965, Mizrahi and colleagues2 first used the term necrotizing enterocolitis to describe a clinical syndrome consisting of vomiting, abdominal distension, shock, and intestinal hemorrhage and perforation. The initial surgical approach to this disease was formulated by Touloukian3 and Santulli and colleagues4 in the 1970s. In 1978, Bell and colleagues5 classified NEC into 3 stages based on the severity of the clinical presentation and recommended treatment strategies. Despite incremental advances in our understanding of the clinical presentation and pathophysiology of NEC, universal prevention of this serious and often fatal disease continues to elude us even in the twenty-first century.
Who is at risk? How prevalent it is?
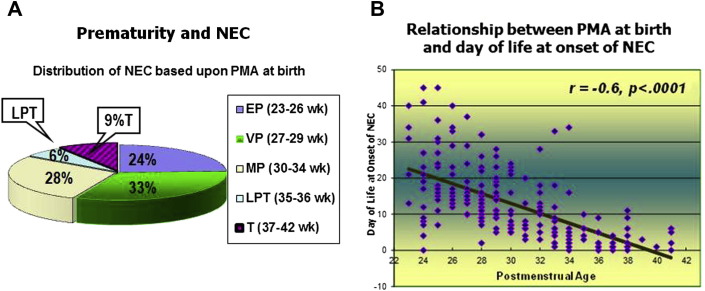
NEC primarily affects premature infants. It is less common in term and late preterm infants.6, 7 Only 7% to 15% of all NEC cases occur in term or late preterm infants (Fig. 1 A). The age of onset is inversely related to the postmenstrual age (PMA) at birth (see Fig. 1B).7 In term infants, NEC is commonly associated with congenital heart diseases, such as hypoplastic left heart syndrome and coarctation of the aorta, which result in intestinal hypoxia and/or hypoperfusion.8 NEC has also been associated with other anomalies, including aganglionosis9 and gastroschisis.10 More than 85% of all NEC cases occur in very low birth weight (VLBW) infants (<1500 g) or in very premature (VP) infants (<32 weeks of PMA).11
Fig. 1.
(A) Only 15% of term (T) and late preterm (LPT) infants developed NEC in this cohort of 202 infants with NEC. EP, extremely premature; MP, moderately premature; VP, very premature. (B) Age of onset of NEC is inversely related to PMA at birth.
(Data from Sharma R, Hudak ML, Tepas JJ 3rd, et al. Impact of gestational age on the clinical presentation and surgical outcome of necrotizing enterocolitis. J Perinatol 2006;26(6):342–7.)
The prevalence of NEC varies among centers. Multicenter and large population-based studies demonstrate that it is prevalent in 7% to 11% of VLBW infants.11, 12, 13 The National Institute of Child Health (NICHD) Neonatal Research Network (NRN) study reported a 7% prevalence rate of NEC in a population of 11,072 VLBW infants during 1999 to 2001.14 The Vermont Oxford Network also reported a similar prevalence rate (7.4%) in 71,808 VLBW infants during a study period from 2005 to 2006.15 A concurrent NICHD-NRN study from 2003 to 2007 found that the prevalence of NEC remained high (11%) among VP infants (born at 22–28 weeks of PMA, birth weight 401–1500 g).13 The prevalence of NEC seems to be less in Europe and Canada. A recent Swedish study found that 5.8% of infants born before 27 weeks of PMA developed NEC among a cohort of 638 infants.16 A Swiss neonatal network study reported that only 3% to 4% of infants born at less than 32 weeks of PMA during 2000 to 2004 developed NEC.17 The Canadian Neonatal Network documented that 5.1% of infants born earlier than 33 weeks of PMA developed NEC during 2003 to 2008 in a population of 16,669 infants.18 Despite the improvement in survival of VLBW infants, neonatal NEC remains quite prevalent in the United States (0.3–2.4 infants per 1000 live births).19
The overall mortality for NEC ranges from 20% to 40% but approaches 100% in infants with the most severe form of the disease.12, 15, 20 Boys have a higher risk of death than girls.12 Earlier studies have reported a slight increase in the prevalence of NEC among African American and male infants, but more recent studies have failed to verify these observations.12 Because NEC affects 2% to 5% of all NICU admissions and causes serious morbidity, NEC continues to impose a heavy burden on the neonatal population.19
What causes NEC? How does it happen?
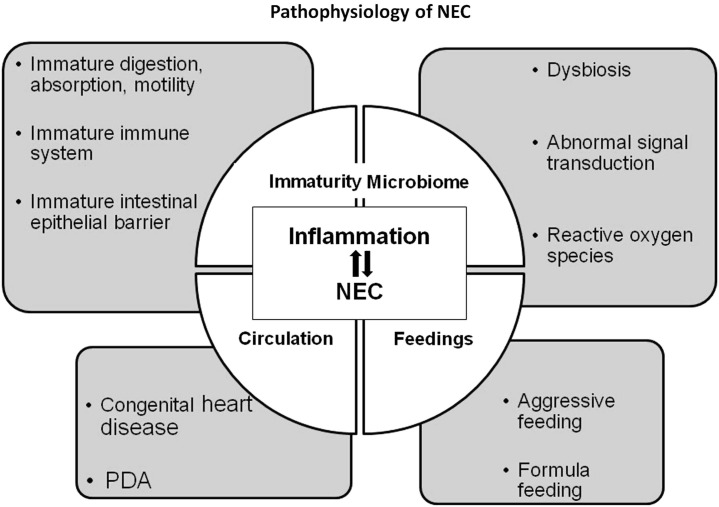
The pathophysiology of NEC in VP infants is not completely elucidated. Compared with NEC in term and late preterm infants in whom hypoxia-ischemia is a common precursor, recent advances in our understanding of NEC at the molecular level suggest that an inflammatory response in VP infants plays the inciting or dominant role in the pathogenesis of NEC.21, 22 Previously held beliefs that low Apgar scores,23 umbilical catheterizations, episodes of apnea and bradycardia, respiratory distress syndrome, anemia, hypothermia, hypoxic-ischemic events,24, 25, 26, 27 hypotension, and the use of vasoactive agents such as Indocin25 and pressors are important contributing causes of NEC in premature infants have not been supported by large epidemiologic and more recent clinical studies.6 Although hemorrhagic-ischemic necrosis is the terminal manifestation of NEC in premature infants, the interaction among milk substrate, microbes, and the immature host immunologic system is now thought to be key in initiating the pathogenesis of NEC (Fig. 2 ).22
Fig. 2.
Pathophysiology of NEC.
Aggressive Feeding
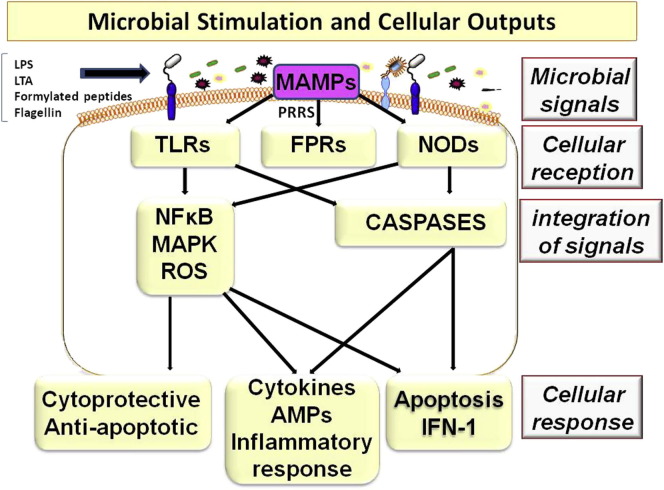
In premature infants, aggressive feeding may cause stasis of milk substrate in the lumen of the GIT because of dysmotility.28 Stasis can lead to intestinal dilatation with fluid and gas and possibly to impairment of the intestinal epithelial barrier (IEB).29, 30, 31 The development of endotoxemia in stable premature infants after feeding and evidence from other studies support that the IEB of premature infants is leakier compared with that of more mature infants.31, 32, 33, 34 Intestinal dilatation in the presence of abnormal microbial colonization (dysbiosis) can distort normal signal transduction (crosstalk) across the IEB and alter the normal message of growth and repair of enterocytes to one that instead produces excessive inflammation, apoptosis, and necrosis (Fig. 3 ).32, 34, 35
Fig. 3.
Microbial components, such as lipopolysaccharides (LPS), lipoteichoic acid (LTA), formylated peptides, and flagellin, serve as microbial-associated molecular patterns (MAMPs) and signal pattern recognition receptors (PRRs), including toll-like receptors (TLRs), formylated peptide receptors (FPRs), or nucleotide-binding oligomerization domain-like receptors (NODs). Integration of these signals evokes cellular outputs based on the initial perception of the triggering organism. Output can be a protective response to commensal microbiota, an inflammatory response to pathogenic organisms, or it can trigger apoptosis.
(Adapted from Sharma R, Young C, Neu J. Molecular modulation of intestinal epithelial barrier: contribution of microbiota. J Biomed Biotechnol 2010;2010:305879; with permission.)
Transfusion and NEC
In recent years, several reports have attempted to establish a causal relationship between blood transfusion (BT) and NEC.36, 37, 38, 39, 40, 41, 42 These studies propose that BT for anemia of prematurity in relatively stable growing premature infants increases the risk of late-onset NEC. The authors think that additional prospective reports that use a more robust design and analysis are needed before a causative relationship can be accepted because of the weaknesses in study designs of these investigations (eg, failure to include all BT, retrospective nature of data collection, lack of appropriate case-control matching, and failure to control for confounding variables). A recently completed prospective, matched, case-control investigation that used robust methodology does not substantiate an association between BT and NEC.
Microbial Mucosal Interactions and NEC
At the mucosal surface, signals from microbial ligands like endotoxin (synonymous with lipopolysaccharide [LPS]), flagellin, lipoteichoic acid, peptidoglycans, and formylated peptides are communicated through a sophisticated process (crosstalk) to appropriate epithelial receptors specific for that ligand referred to as pattern recognition receptors (PRRs), including Toll-like receptors (TLRs), formylated peptide receptors, and nucleotide-binding oligomerization domains.35 Activation of these PRRs initiates regulatory pathways, including mitogen-activated protein kinase, nuclear factor κB (NFκB), and caspase-dependent pathways (see Fig. 3).22, 29, 35, 43, 44, 45 These interrelated complex pathways determine mucosal and submucosal responses. Based on the perception of interrelated signals, the response can be cytoprotective (ie, promoting growth and repair) or it can be destructive if apoptosis or inflammatory responses is triggered (see Fig. 3).22, 35, 44 The terminal event in NEC is hemorrhagic-ischemic necrosis, which is the consequence of a dysregulated inflammatory response mediated by endogenous factors that include platelet-activating factor (PAF), proinflammatory cytokines (such as tumor necrosis factor-α, interleukins 1 & 6 [IL-1, IL-6]), chemokines (MIP-2/CXCL2), NF-κB, and the complement system.29
Because of the relative immaturity of key gastrointestinal functions, such as digestion, absorption, motility, and abnormalities in immune responses, a premature newborn is exquisitely vulnerable to gastrointestinal injury.46 The cellular response to signal transduction as described earlier is orchestrated by the innate immune system in mucosa and submucosa.45, 47 Microbial interaction with intestinal epithelium (PRRS) signals tissue-specific functions, such as T-cell expansion and elaboration of cytokines and chemokines. Normally after birth, exposure to LPS downregulates IL-1 receptor associated kinase 1 (IRAK), an intermediary for epithelial TLR4 signaling, and promotes tolerance to LPS.19, 22, 43 This postnatal adaptation helps to achieve host-microbe homeostasis with microbial tolerance.22, 44 Premature infants are exposed shortly after birth to a massive microbial antigenic challenge that may be distorted by frequent and prolonged use of antibiotics. As a result, the GIT of premature infants gravitates toward mounting an inflammatory response rather than establishing tolerance (T-helper-1 response).30, 35, 47 The premature infant seems to mimic a response that is similar to the immune-naïve response demonstrated by the fetus, which is characterized by hyper-responsiveness to LPS.22, 48
Intestinal colonization with commensal Bifidobacterium and Lactobacillus species reduces the risk of NEC.49, 50 The frequent and prolonged use of antibiotics results in an overgrowth of potentially pathogenic species.51 Distortion of intestinal microecology by exposure to broad-spectrum antibiotics may result in colonization with inflammogenic microbial consortia that are more likely to direct the immune repertoire in the direction of an inflammatory response, thereby increasing the risk for NEC.51, 52 Metagenomic studies indicate that intestinal microecology during the early postnatal period greatly influences the evolution of immune health.53, 54 Infants who later develop NEC show evidence for a dysbiotic microecology before the diagnosis of NEC.55 A recent clinical study found that exposure to broad-spectrum antibiotics for more than 10 days increased the risk of NEC by nearly threefold.51
Recent advances in the proteomics and microecology pertinent to NEC strongly suggest that a distorted innate-immune response of premature infants increases the vulnerability to NEC.22, 55 Glucocorticoid-mediated maturation of the IEB has been shown to protect against NEC and to blunt the inflammatory response seen in NEC.46, 48, 56, 57 Furthermore, the vulnerability to NEC is not unique to premature neonates, it is also seen in the older immune-compromised population.58, 59, 60 A NEC-like illness has been described in the geriatric population and in patients with human immunodeficiency virus.56, 58
Hypoxic-Ischemic Mechanisms
Under normal conditions, a state of high intestinal blood flow and low resting vascular resistance is maintained by nitric oxide.26 Impaired endothelial function or elaboration of proinflammatory mediators may alter the balance between vasoconstriction (as mediated by endothelin-1) and vasodilatation (as mediated by nitric oxide) and lead to a relatively ischemic state. In animal models of hypoxia-ischemia, derangements of intestinal microcirculation develop at the premucosal arteriolar inflow location with a distinct stop-and-go pattern consistent with severe vascular dysfunction.61 Levels of inflammatory mediators increase markedly in real-time animal models of NEC.61, 62, 63 The elaboration of inflammatory mediators (eg, PAF) early in the pathogenesis of NEC may have important secondary effects on local circulation that contribute to the development of the intestinal necrosis.19, 27, 43, 63, 64, 65
Infectious Agents
Despite 4 decades of exhaustive search, no consistent single microbial species has been isolated from infants with NEC.66 Enterobacteriaceae sp are the most common, followed by Staphylococcus sp and Clostridium sp.19, 67, 68, 69, 70 Outbreaks of NEC linked to consumption of formula contaminated by Enterobacter sakazakii and breast milk contaminated by Staphylococci have occurred.69, 70, 71 Although bacteria are most commonly associated with NEC, several enteric viruses (rotavirus, echovirus, coronavirus, torovirus, norovirus [NoV]) and Candida sp have also been described.72, 73, 74, 75, 76, 77, 78, 79, 80
Generally, NEC occurs sporadically but may also occur in clusters or outbreaks.81 Temporal clustering of such outbreaks and their cessation with the implementation of infection control measures supports an association of these outbreaks with a single transmissible agent during a given outbreak.82, 83 As cited earlier, varieties of organisms, including bacteria and viruses, have been linked to outbreaks of NEC. Among viruses, NoV, astrovirus, torovirus, coronavirus, and rotavirus have been linked with outbreaks of hemorrhagic gastroenteritis and necrotizing enterocolitis.75, 79, 84, 85, 86 In a recent study, compared with infants with rotavirus or norovirus enteritis, infants with astrovirus were more likely to develop NEC and the systemic inflammatory response syndrome.87
Viral enterotoxin, such as the nonstructural protein (NSP4) of rotavirus, stimulates a secretory response that is Ca++dependent that results in watery diarrhea in mature infants but hemorrhagic enteritis or NEC in premature infants.75, 88 This viral enterotoxin induces an age- and dose-dependent response.88 NSP4 increases paracellular permeability and alters the integrity of the IEB. It binds with caveolin-1 (scaffolding protein) and alters tight junction assembly.89, 90, 91 Consequently, a weakened IEB permits the translocation of microbes and the initiation of endotoxemia and the inflammatory response characteristic of NEC.90
Regardless of whether a pathogen can be identified during a local epidemic of NEC, implementation of infection control measures are effective in stopping the outbreak.81, 83, 92, 93
How does it present? How do we diagnose?
Clinical Signs
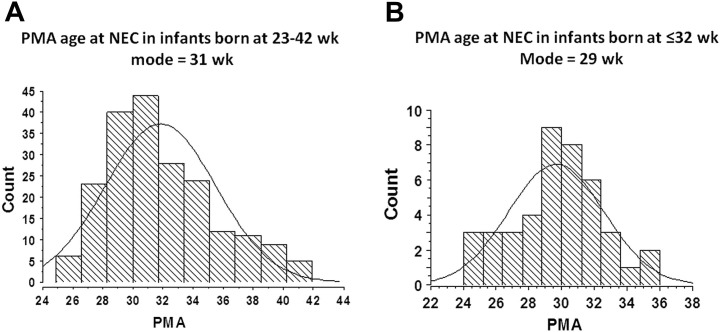
During the 1980s, investigators found that NEC occurred more commonly in preterm infants between 33 to 35 weeks of PMA.94, 95 More recent studies have found that a peak distribution of NEC occurs at 29 to 31 weeks of PMA (Fig. 4 ).7 This shift to an earlier PMA may be a reflection of the current practice to introduce enteral feedings earlier compared with the delayed feeding practices of the 1980s.94, 95
Fig. 4.
PMA at onset of NEC in 2 different study cohorts. (A) Single-center study cohort of 202 infants with NEC during 1991 to 2003 born at 23 to 42 weeks; NEC was most common at 31 weeks of PMA. (B) Multicenter study cohort of 42 infants with NEC during 2008 to 2012 born at 23 to 32 weeks; NEC occurred most commonly at 29 weeks of PMA.
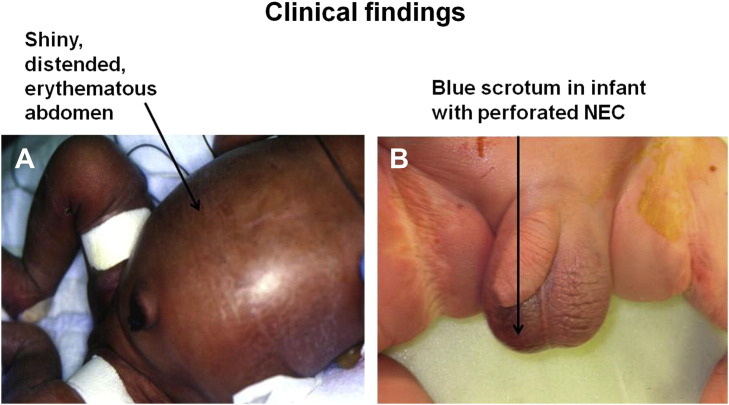
The clinical presentation of NEC can range from nonspecific signs that progress insidiously over several days to a fulminant onset of gastrointestinal signs, multiorgan system dysfunction, and shock over a few hours.6 Early signs of NEC are nonspecific and may be indistinguishable from those of sepsis.5, 6, 11, 29, 94, 95 Clinical signs include both intestinal and systemic perturbations. Intestinal signs in early NEC can present as feeding intolerance that may manifest as increased prefeeding gastric residuals, emesis, abdominal distension, and bloody stools (hematochezia). Less commonly, when the stomach is involved, NEC can present as bloody emesis or a bloody gastric residual.95, 96 During the advanced stage of NEC, the abdomen may appear shiny, distended, and erythematous. Infants generally prefer to assume a frog-leg position (position of comfort, Fig. 5 A) and are hyporesponsive.6, 94, 95, 96 On gentle palpation, the abdomen may feel firm, tense, and tender, and a tender mass may be palpable. Bowel perforation may cause the abdomen to appear blue or discolored.6, 94, 95, 96 An infant with a blue discolored abdomen secondary to isolated intestinal perforation may be indistinguishable from an infant with NEC. In a male infant, erythema or bluish discoloration of the scrotum may appear if peritoneal fluid from perforated bowel herniates into the scrotum (see Fig. 5B).
Fig. 5.
(A) Shiny, distended, erythematous abdomen (arrow) of an infant with advanced NEC in frog-leg position. (B) Discolored scrotum (arrow) in an infant with perforated advanced NEC; no pneumoperitoneum was seen in abdominal radiographs.
VP infants do not manifest tenderness and guarding unless NEC is advanced. Therefore, a high index of suspicion is required to establish a diagnosis of NEC if multiple subtle signs appear that produce a deviation from baseline clinical status.6, 7 NEC can also present with bloody stools (hematochezia) without any other initial signs, especially when NEC involves the distal colon. If the jejunum and terminal ileum are the predominant sites of NEC, then emesis, increased gastric residuals, and/or abdominal distension are the more likely initial clinical signs.97, 98 Occult hematochezia diagnosed by a hemoccult test correlates poorly with NEC.99
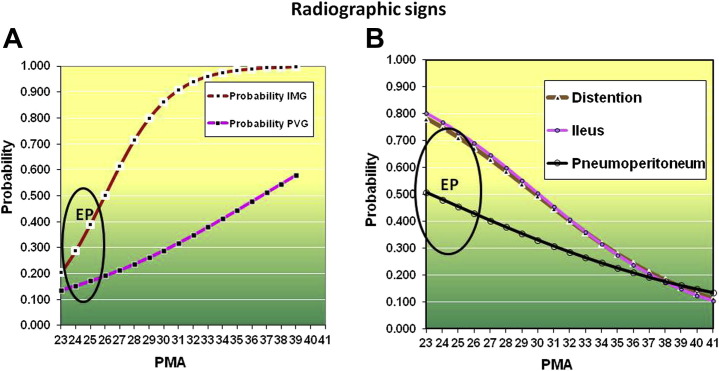
Extremely premature infants with NEC are more likely to present with abdominal distension, ileus, and emesis. They are less likely to present with pneumatosis but are more likely to develop pneumoperitoneum compared with late-term or term infants (Fig. 6 A, B). Observation of a lightly bile-stained gastric residual in VP infants, especially before any feeding, is common and normally resolves as gradual advancement of feeding volumes elicits improvement in intestinal motility. Consistent dark-green bilious gastric residual may indicate gastrointestinal obstruction and requires further investigation.98
Fig. 6.
(A) Probability by PMA at birth that an infant with NEC will present with intramural gas (IMG) or portal venous gas (PVG). There is less than 50% probability for an extremely premature (EP) infant to manifest IMG. (B) Radiographic signs that are more probable in infants with decreasing PMA. There is more than 50% probability that an EP infant will present with these signs.
(Adapted and Modified from Sharma R, Hudak ML, Tepas JJ 3rd, et al. Impact of gestational age on the clinical presentation and surgical outcome of necrotizing enterocolitis. J Perinatol 2006;26(6):342–7; with permission.)
Systemic signs include lethargy, hypotension, poor perfusion and pallor, increased episodes of apnea and bradycardia, worsening of respiratory function, temperature instability, tachycardia, hyperglycemia, or hypoglycemia.95, 96, 97, 98
Abnormal laboratory tests include anemia, left shift of neutrophils, neutropenia, thrombocytopenia, metabolic acidosis, and hyponatremia.98, 100 In some instances, NEC may present as unexplained hyponatremia. Concurrent bacteremia and sepsis occurs in 40% to 60% of NEC cases.97, 98, 100, 101, 102 Sepsis caused by gram-negative bacteria is more common.97, 102 Conversely, if an infant presents with sepsis caused by gram-negative bacteria and nonspecific intestinal and radiographic signs, there is a greater likelihood that NEC is the underlying cause of this illness.102
In 5% to 6% of cases, NEC may recur.97, 103 Recurrence is more likely if the initial episode of NEC was associated with congenital heart disease or with rotavirus. Recurrence can also occur with cow milk protein allergy.104, 105 However, NEC can recur after either medical or surgical NEC without specific risk factors.97, 103
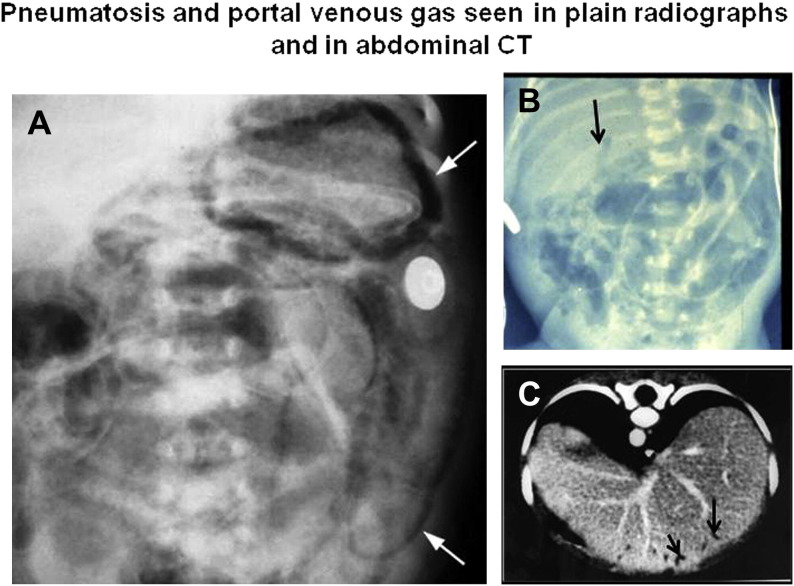
Radiographic Signs
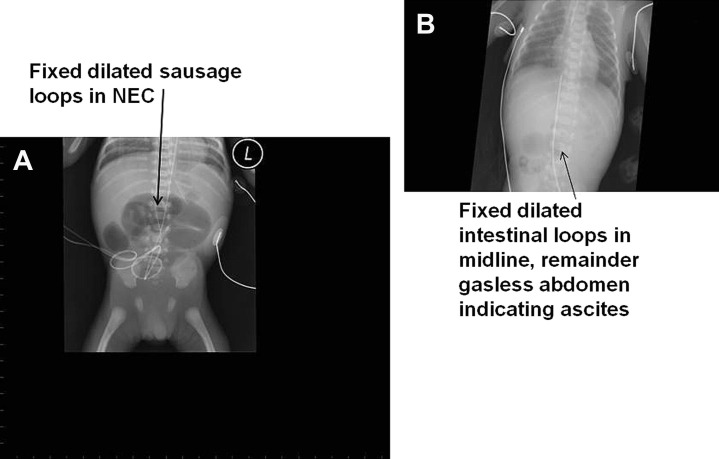
Intramural gas or pneumatosis and portal venous gas are pathognomonic signs of NEC. They may appear even before clinical signs. The absence of these radiographic signs by no means confirms the absence of NEC. Pneumatosis is caused by gas within the bowel wall and may appear linear (like railroad tracks) or circular if gas is subserosal or bubbly if gas is submucosal (Fig. 7 ).106, 107 Bubbly gas lucencies could also indicate air within intraluminal fecal material. Pneumatosis is more commonly seen in the right lower quadrant but it can be seen anywhere because necrosis may involve any section of bowel extending from the stomach to the rectum.97, 106, 107 The amount of pneumatosis does not always relate to the severity of disease, and its disappearance does not necessarily imply pathologic or clinical improvement.7, 97, 106, 107 Other nonspecific but common abdominal radiographic findings include thickened bowel walls, dilated bowel loops, a paucity of bowel gas, and a fixed dilated loop (Fig. 8 ).106, 107 Inflamed, edematous, and hemorrhagic bowel wall may be separated from each other because of thickening of bowel wall and the normal sausage-like mosaic configuration may be lost. A persistent, fixed, dilated loop may indicate a necrotic bowel loop. Dilated, gas-filled loops in the central abdomen may indicate the presence of ascites or free peritoneal fluid because dilated bowel loops float (and migrate to the least dependent region of the abdomen) when peritoneal fluid is present.106, 107 A paucity of bowel gas may be associated with ileus and abdominal decompression. These nonspecific signs may not be diagnostic of NEC but nonetheless are non-reassuring and suspicious for NEC, thereby warranting immediate intervention and treatment implementation.106, 107
Fig. 7.
(A) There is extensive pneumatosis (arrows); left upper arrow pointing at gastric pneumatosis. Pneumatosis is seen as multiple curvilinear radiolucencies in this plain radiograph. (B) Arrow pointing toward portal venous gas seen as curvilinear radiolucency over liver; distended bowel loops and diffuse pneumatosis is seen throughout. (C) Portal venous gas (arrows) is seen as lucencies in on computed tomography (CT) scan.
([A] Adapted from Epelman M, Daneman A, Navarro OM, et al. Necrotizing enterocolitis: review of state-of-the-art imaging findings with pathologic correlation. Radiographics 2007;27:285–305; with permission.)
Fig. 8.
(A) A dynamic loop in serial radiographs indicates intestinal necrosis. (B) Gasless abdomen with a few loops in midline indicates ascites (peritonitis) and intestinal necrosis.
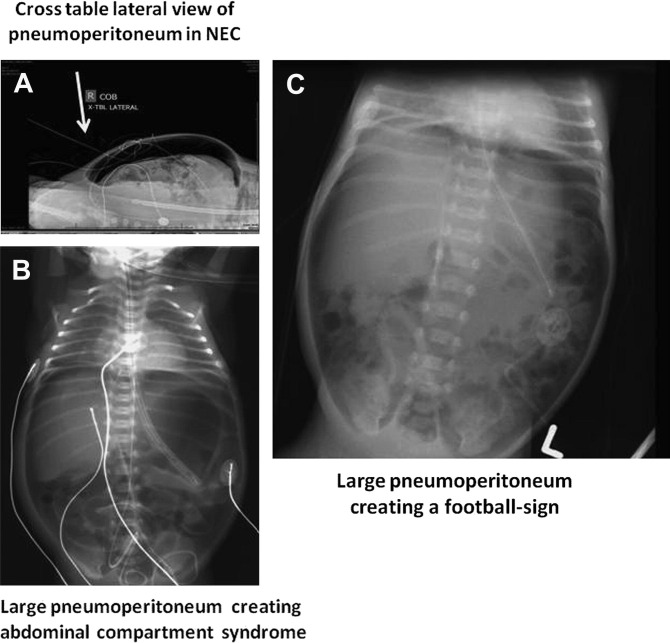
Pneumatosis intestinalis can extend to the portal venous circulation and typically appear as curvilinear lucencies over the hepatic silhouette in a plain radiograph (see Fig. 7).97 A pneumoperitoneum is diagnostic of a perforated viscus. In a supine position, it may appear as a rounded or oval extraluminal lucency beneath the upper anterior abdominal wall (Fig. 9 ). When there is a large pneumoperitoneum, it may outline the falciform ligament giving it the appearance of a longitudinal strip of sutures in a football (American football and rugby but not soccer ball), leading to its designation as the football sign (see Fig. 9).106, 107 A cross-table lateral film may demonstrate small air collection just beneath the abdomen (see Fig. 9). A small pneumoperitoneum may be difficult to visualize on a single plain film. A left lateral decubitus film will allow free air to rise to the top over a nondependent surface, facilitating visualization of an abnormal lucency. A small amount of free air may present as a small triangular or a rectangular lucency and make a definitive diagnosis of free air difficult. Sometimes free air may present as a double-wall sign when the bowel loop is outlined and gas is present along serosal and mucosal surfaces.106, 107
Fig. 9.
(A) Cross-table lateral and (B) plain abdominal radiographs illustrating radiolucent pneumoperitoneum (indicated by arrows). (C) Another large pneumoperitoneum creating a football sign.
A nonionic water-soluble contrast study (typically, an upper gastrointestinal series followed by an enema) can be obtained in circumstances when anatomic gastrointestinal obstruction is suspected.107 Hypertonic water-soluble agents are not routinely recommended because hypovolemia can result from a shift of fluid from the intravascular space to the intestinal lumen.107
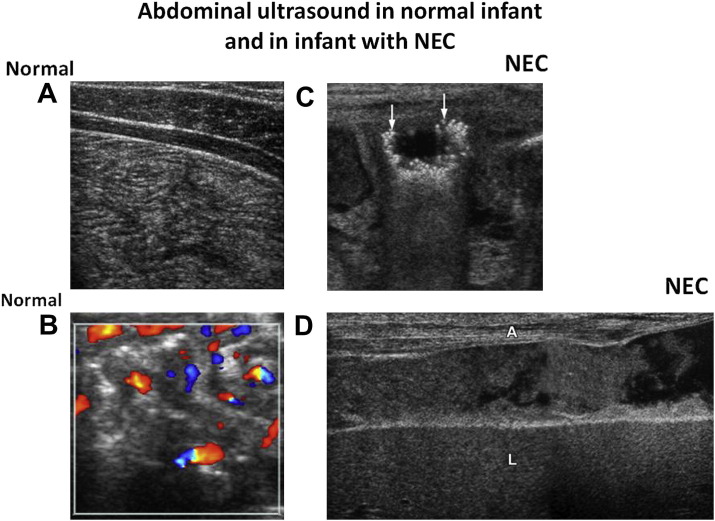
Ultrasound
In situations when radiographic signs are nonspecific, the abdominal ultrasound (US) is another modality that can identify even small volumes of free gas. US is also the preferred modality for visualization of abdominal fluid and ascites. Thickness and echogenicity of the bowel wall and qualitative assessment of peristalsis can be visualized best by US color Doppler. It can also be used to assess arterial perfusion of the bowel wall (Fig. 10 ). Portal venous gas can be more readily seen using abdominal sonography than plain film.107 Faingold and colleagues108 used color Doppler sonography and demonstrated 100% sensitivity for free air and absent blood flow (necrotic gut) compared with 40% sensitivity by radiography. The use of computed tomography is not advocated for the diagnosis of NEC.107
Fig. 10.
Sonogram of normal bowel (A, B). (A) Normal non-distended bowel; echogenic markings represent mucosal interface with lumen, and hypoechoic linear bands represent the muscularis of the bowel wall. (B) Color Doppler image of non-distended normal bowel with color dots of blood flow in normal bowel. (C) Sonogram shows a distended loop with many pneumatoses seen as hyper-echoic bubbles (arrows). (D) Free intraperitoneal fluid in perforated NEC. Echogenic fluid between abdominal wall (A) and liver (L) is seen containing much debris, which is more indicative of bowel perforation than free fluid.
(Adapted from Epelman M, Daneman A, Navarro OM, et al. Necrotizing enterocolitis: review of state-of-the-art imaging findings with pathologic correlation. Radiographics 2007;27:285–305; with permission.)
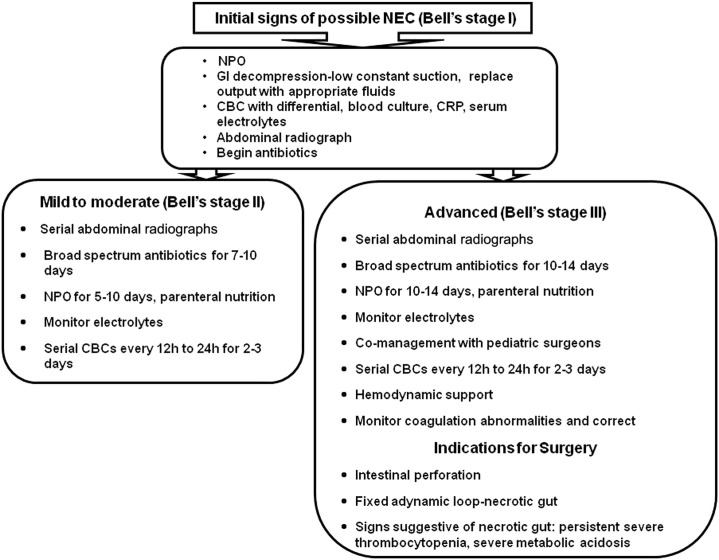
Management
Medical
When an infant is suspected to have NEC, all enteral feedings and medications should be discontinued (Fig. 11 ). Prompt decompression of the GIT should be accomplished by the placement of a double-lumen gastric tube (large lumen for aspiration and small lumen for irrigation and venting) with the institution of low, constant suction. Aspirated volume should be replaced with intravenous Ringer lactate solution with extra potassium chloride that is lost in gastric output. It is crucial to ensure the patency of the tube. If the abdomen continues to distend despite ongoing continuous suction, the tube should be checked for proper placement and for blockage and nasal continuous positive airway pressure should be discontinued. Endotracheal intubation is preferred in infants who are deteriorating and have frequent episodes of apnea. Intravascular volume must be monitored rigorously to ensure adequate tissue perfusion and may be gauged by frequent assessment of serum electrolytes, hematocrit, and urinary output. As a rule of thumb, anticipation of third spacing in infants with NEC will require 1.5-fold maintenance fluid plus replacement of gastric output. Failure to maintain euvolemia and proper electrolyte repletion can result in shock with hypochloremia, hyponatremia, and hypokalemia. Parenteral nutrition should be started early with adequate protein (3.5–4.0 g/kg/d) to maintain positive nitrogen balance and to allow the repair of injured tissue.6, 46, 109, 110, 111
Fig. 11.
Clinical decision algorithms. NPO, nil per os (nothing by mouth); CBC, complete blood cell count; CRP, C-reactive protein.
Strict implementation of infection control measures is critical. Following the culture of blood and urine, prompt initiation of treatment with appropriate broad-spectrum antibiotics based on known sensitivities of prevalent pathogens in the individual neonatal intensive care unit is vital. If surgical intervention is performed, peritoneal fluid and intestinal tissue should be sent for gram stain, culture, and sensitivity. The utility of a stool culture for bacteria in neonates has been questioned because fecal matter has many bacterial species. However, during outbreaks of NEC, attempts should be made to identify the infectious agent whenever possible. Usual regimens include ampicillin (or a cephalosporin) and gentamicin (or other aminoglycoside). The addition of a third antibiotic that provides anaerobic coverage (eg, clindamycin or metronidazole) is indicated when there is evidence of peritonitis or bowel perforation (see Fig. 11). Inflammation of the intestine and peritoneum is excruciatingly painful; therefore, attention to pain control and minimal handling during cares are integral parts of management.6, 46, 109, 110, 111
Hematocrit should be monitored and packed red cells should be provided to replace occult intestinal hemorrhage. Adjunctive treatment includes judicious correction of significant thrombocytopenia, coagulopathy, and metabolic acidosis. Abdominal girth should be measured frequently. A sudden increase in abdominal girth warrants an immediate abdominal radiograph to assess for a pneumoperitoneum. Co-management with pediatric surgeons is recommended when a diagnosis of NEC is strongly suspected or confirmed. In sick infants who are not improving despite supportive medical management and in whom NEC is suspected, consultation with a pediatric surgeon and radiologist may help to arrive at a specific diagnosis.6, 46, 107, 109, 110, 111, 112, 113
In the most premature infants, a high index of suspicion is required to make a timely diagnosis of NEC because these infants are less likely to manifest tenderness and the pathognomonic radiographic findings of NEC.7 By the time VP infants manifest tenderness or abdominal mass, NEC has usually progressed to an advanced stage.7
Surgical
Identification of a pneumoperitoneum caused by bowel perforation and the presence of necrotic bowel (either may be difficult to diagnose) are 2 absolute indications for surgical intervention. Severe and persistent metabolic acidosis and/or thrombocytopenia in conjunction with a lack of improvement with medical management strongly suggest the presence of necrotic bowel and warrants surgery (see Fig. 11).7, 97, 100, 102, 110, 112, 113
The timely diagnosis of bowel perforation or dead gut can be difficult in extremely premature infants with NEC.7 A negative laparotomy is just as detrimental as failure to recognize perforation early in this group of patients.107 Pneumoperitoneum can be missed in about 20% of cases of bowel perforation.107 In such cases, the use of a 7-point scoring system using 7 components that quantitate the presence of metabolic derangement, in conjunction with an infant’s ongoing evaluation by a pediatric surgeon, has been found to optimize the timing of the surgical intervention.114 These metabolic derangements include severe metabolic acidosis, severe thrombocytopenia, hypotension, hyponatremia, neutropenia, left shift of neutrophils, and positive blood culture. It is recommended that this scoring system be used only as an adjunct to careful serial clinical and radiologic evaluation of infants.108, 110, 114
With respect to the type of surgery, primary peritoneal drainage (PPD) has emerged as an alternative to laparotomy in VP infants with bowel perforation.100, 115 Peritoneal drainage serves as a definitive treatment of some patients and as a temporizing measure for unstable sick infants until laparotomy can be performed after their stabilization.115, 116, 117, 118, 119
The choice of PPD or laparotomy as a primary surgical intervention has been argued for a decade.116, 117, 118 In their review of only 2 randomized controlled trials, Rao and colleagues116 report that there were no differences with respect to mortality and duration for total parenteral nutrition between the drainage and laparotomy. However, these studies did not distinguish between isolated perforation and NEC.120 Neither of these two trials reached the recruitment target nor showed improved survival from PPD or laparotomy. One of these two trials [Necrotizing Enterocolitis Trial (NET) from the United Kingdom] found that 74% of infants initially treated with PPD required a rescue laparotomy. The second NICHD NRN trial did not encourage rescue laparotomy (which nonetheless was allowed) and did not distinguish NEC from isolated intestinal perforation (IIP).117, 118, 119 This latter trial, conducted in extremely low birth weight infants (≤1000 g), found that laparotomy had an advantage over PPD with respect to the likelihood of survival and better neurodevelopmental outcome at 18 to 22 months of age.120 Death or impairment occurred in 78% of the drainage group and in 66% of the laparotomy group.
The ability to accurately distinguish NEC from IIP is important when making a comparison between PPD and laparotomy because mortality associated with NEC is greater than with IIP.120, 121 A large, single-center, prospective study showed that bowel perforation in infants with severe NEC who were treated with primary laparotomy fared better than infants treated with a PPD.100, 121, 122 Conversely, infants with IIP fared better with PPD. These investigators devised the 7-point metabolic derangement score and used it in conjunction with ultrasonography or contrast imaging to distinguish NEC from IIP.
Other traditional surgical procedures at laparotomy include debridement and the resection of clearly necrotic bowel and creation of an enterostomy.113, 120, 121 Sometimes multiple excisions are needed to preserve bowel length. Viable ends of bowel are exteriorized as stomas with the distal end as a mucous fistula. Sometimes single stoma with a Hartmann pouch is created. In this procedure, a colostomy or ileostomy is created and the distal limb is closed by suturing it and placing it back in the peritoneal cavity as a temporary measure until the patient is ready for re-anastomosis.110, 113, 123
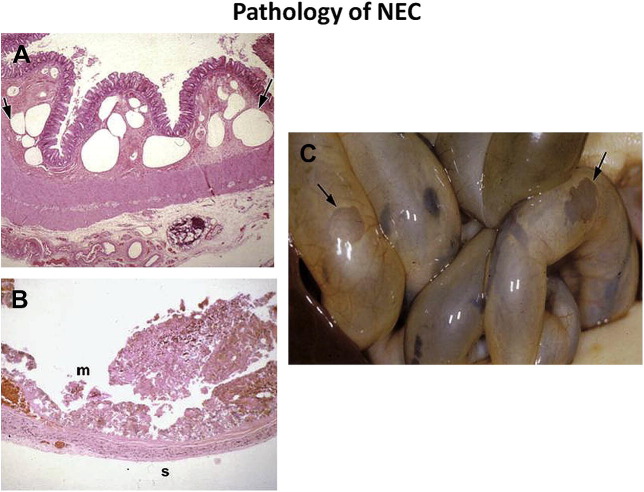
Pathology
Coagulation (hemorrhagic-ischemic) necrosis, inflammation, and bacterial overgrowth are salient features of the histopathology of NEC. Reparative tissue changes, such as epithelial regeneration, formation of granulation tissue, and fibrosis, are found in two-thirds of cases and provide evidence for a duration of tissue injury/reparation processes of at least several days.124, 125 Damage to the intestinal tract may range from mucosal injury to full-thickness necrosis with focal perforation. Gas bubbles (pneumatosis intestinalis) can be seen in mucosa, submucosa, and serosal surfaces (Fig. 12 ).125 Although NEC can involve the gut from the stomach to the distal colon (NEC totalis), disease is most commonly found in the terminal ileum and ascending colon. Rotavirus-associated NEC most often involves the distal colon.75 NEC can cause focal disease or manifest as multiple large diffuse necrotic areas alternating with patches of unaffected bowel. Serosal exudation without obvious perforation can also occur. In mild stages of NEC, intense congestion of superficial mucosa can result in focal necrosis of villous tips and epithelial sloughing into bowel lumen.124, 125
Fig. 12.
(A) Histology of small bowel (original magnification × 100; hematoxylin-eosin stain) illustrating rounded large bubbles (arrows) of pneumatosis (intramural gas) in the submucosa. (B) At a more advanced stage, there is necrosis of mucosa, submucosa, and muscularis with intraluminal necrotic debris on the mucosal side (m), (original magnification × 100; hematoxylin-eosin stain). Only the serosa (s) appears intact. (C) Gross pathology at postmortem examination shows severe NEC. Arrows indicate severe sloughing of mucosa, submucosa, and muscularis mucosa. Only a thin layer of serosa is intact allowing the intestinal lumen to be seen.
(Adapted from Epelman M, Daneman A, Navarro OM, et al. Necrotizing enterocolitis: review of state-of-the-art imaging findings with pathologic correlation. Radiographics 2007;27:285–305; with permission.)
Differential diagnosis
IIP
It is more common for extremely premature infants with NEC to develop pneumoperitoneum than pneumatosis.7 This population is also more vulnerable to IIP. Infants with IIP are generally more stable but they can develop peritonitis and sepsis syndrome mimicking NEC.25, 100, 102 Generally, IIP presents during the first week of life and has been commonly associated with early indocin prophylaxis against intraventricular hemorrhage or patent ductus arteriosus (Table 1 ).25 Pathologically IIP is a focal perforation without an inflammatory component. It is not associated with feeding and does not present as hemorrhagic ischemic necrosis.25
Table 1.
Comparison between IIP and NEC
| Characteristics | IIP (n = 26) | NEC (n = 113) |
|---|---|---|
| Birth weight, mean ± SD (g) | 828 ± 203 | 923 ± 202 |
| Gestational age at birth, mean ± SD (wk) | 25.9 ± 2.1 | 26.7 ± 2.0 |
| Age at diagnosis (d) | 6.7 ± 15.5 | 15.6 ± 9.1 |
| Association with indomethacin (early, first dose on day 1) | Yes | No |
| Association with PDA | No | Yes |
| Predominant feature of pathophysiology | Circulatory | Inflammation |
| Mortality | 42% | 26% |
Adapted from Sharma R, Hudak ML, Tepas JJ 3rd, et al. Prenatal or postnatal indomethacin exposure and neonatal gut injury associated with isolated intestinal perforation and necrotizing enterocolitis. J Perinatol 2010;30(12):786–93; with permission.
In contrast with the multifactorial pathogenesis of NEC, IIP usually develops suddenly without clinical evidence of intestinal inflammation.25 The propensity for these focal lesions to occur in the watershed areas of terminal ileum or jejunum supports the theory of arterial occlusion with embolism.25, 126, 127, 128 Arterial rectae are end arteries that supply intestinal villi.126, 127, 128 Persistence of right to left shunt through a patent foramen ovale or PDA during the early critical postnatal period presents a scenario for arterial embolism that potentially can create lesions similar to IIP, especially when these lesions occur near the antimesenteric border.25
Sepsis
Sepsis can masquerade in a manner similar to NEC.6 Many intestinal and systemic signs of sepsis also are characteristic of NEC. Specifically, ileus, hypotension, respiratory deterioration, thrombocytopenia, metabolic acidosis, left shift of neutrophils and neutropenia, and systemic inflammatory response syndrome (SIRS) also occur with septic shock unaccompanied by intestinal inflammation.114 Although sepsis and SIRS are complications of NEC, it is important to exclude NEC as the underlying cause of sepsis. The following two findings, if present, favor the diagnosis of NEC:
-
•
New-onset hyponatremia (<130 mEq/L) that cannot be explained by dilution or by treatment with diuretics (Generally, this finding appears early before significant clinical illness develops.)
-
•
Hematochezia (blood in the stool, not occult blood) that may appear early in the disease process or later after resolution of ileus
The differential diagnosis also includes other causes of anatomic and functional intestinal obstruction (eg, malrotation, intestinal atresia, intussusceptions, aganglionosis); conditions that can result in intestinal ischemia (eg, volvulus, critical coarctation of the aorta, hypoplastic left heart syndrome); omphalitis; and milk protein intolerance.8, 9, 105
Outcomes and complications
The overall mortality rate in NEC is between 20% and 40% but varies with the severity and extent of gut necrosis.129, 130, 131 Mortality is inversely related to PMA at birth.6, 15 Other complications of NEC include intestinal strictures, enterocutaneous fistula, intra-abdominal abscess, cholestasis, and short-bowel syndrome.7, 130, 131 Intestinal and liver failure can also occur that requires transplantation. Strictures typically occur 3 to 8 weeks after the acute episode but can also present several months later.97 Contrast enema is indicated if signs of subacute intestinal obstruction appear several weeks after the acute episode of NEC. The colon is the most common site for stricture development, but strictures can also occur in the ileum or jejunum.97, 98 Diffuse pneumatosis increases the risk for strictures.97, 98 Risks of all comorbidities of prematurity increase with NEC, including neurodevelopmental, motor, sensory, and cognitive problems.129, 130, 131, 132, 133, 134
Future directions
Prediction
The prediction of infants at an increased risk of NEC may be possible in the future through the use of methods that are currently available at a few research facilities. These methods use noninvasive indicators, such as profiling of the fecal microbiome,55 and the identification of the expression of inflammatory proteins from buccal epithelium using buccal swab collection.135 The determination of oxidative stress by measuring concentrations of non–protein-bound iron, advanced oxidation protein products, and total hydroxides in cord blood has been reported to be useful in predicting which VP infants are at risk for NEC but requires additional validation.136
Predisposing Factors and Management Planning
Earlier noninvasive diagnosis of NEC through the use of abdominal sonography in infants with nonspecific clinical and radiographic signs and through the assessment of metabolic derangement may result in more timely and appropriate medical treatment and surgical intervention.107, 112 However, no studies have demonstrated improved clinical outcomes caused by facilitated diagnosis and management. Future trials comparing outcomes of peritoneal drainage with laparotomy should include distinguishing NEC from IIP.100
Perforation Versus NEC
Clinical studies suggest that the isolated perforation occurs when the intestinal mucosa has been weakened by processes, such as local ischemia-reperfusion or thromboembolism. Conversely, NEC involves both infectious and inflammatory mechanisms.137 Designing strategies to prevent the occurrence of NEC and to improve outcomes of infants who develop NEC should consider these diagnoses as fundamentally different disease processes.
The focus of NEC research is shifting from concentrating on the distinct nature of this disease to understanding the unique characteristics of immune-naïve premature patients. Hence, investigative and interventional techniques aimed at ensuring a more appropriate and mature intestinal immune response should be tested as preventative strategies.
Footnotes
This work was supported by the National Institute of Child Health and Human Development grant number RO1 HD 059143.
The authors have no conflict of interest to declare.
References
- 1.Obladen M. Necrotizing enterocolitis –150 years of fruitless search of the cause. Neonatology. 2009;96:203–210. doi: 10.1159/000215590. [DOI] [PubMed] [Google Scholar]
- 2.Mizrahi A., Barlow O., Berdon W. Necrotizing enterocolitis in premature infants. J Pediatr. 1965;66:697–705. doi: 10.1016/s0022-3476(65)80003-8. [DOI] [PubMed] [Google Scholar]
- 3.Touloukian R.J. Neonatal enterocolitis: an update on etiology, diagnosis, and treatment. Surg Clin North Am. 1976;55:376–387. doi: 10.1016/s0039-6109(16)40877-7. [DOI] [PubMed] [Google Scholar]
- 4.Santulli T.V., Schullinger J.N., Heird W.C. Acute necrotizing enterocolitis in infancy: a review of 64 cases. Pediatrics. 1975;55:376–387. [PubMed] [Google Scholar]
- 5.Bell M.J., Ternberg J.L., Feigin R.D. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187(1):1–7. doi: 10.1097/00000658-197801000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neu J., Walker W.A. Necrotizing enterocolitis. N Engl J Med. 2011;364(3):255–264. doi: 10.1056/NEJMra1005408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma R., Hudak M.L., Tepas J.J., 3rd Impact of gestational age on the clinical presentation and surgical outcome of necrotizing enterocolitis. J Perinatol. 2006;26(6):342–347. doi: 10.1038/sj.jp.7211510. [DOI] [PubMed] [Google Scholar]
- 8.De La Torre C.A., Miguel M., Martínez L. The risk of necrotizing enterocolitis in newborns with congenital heart disease, a single institution-cohort studyCir Pediatr. 2010;23(2):103–106. [in Spanish] [PubMed] [Google Scholar]
- 9.Raboei E.H. Necrotizing enterocolitis in full-term neonates: is it aganglionosis? Eur J Pediatr Surg. 2009;19(2):101–104. doi: 10.1055/s-0029-1202771. [DOI] [PubMed] [Google Scholar]
- 10.Snyder C.L. Outcome analysis for gastroschisis. J Pediatr Surg. 1999;34(8):1253–1256. doi: 10.1016/s0022-3468(99)90162-8. [DOI] [PubMed] [Google Scholar]
- 11.Thompson A.M., Bizzarro M.J. Necrotizing enterocolitis in newborns: pathogenesis, prevention and management. Drugs. 2008;68(9):1227–1238. doi: 10.2165/00003495-200868090-00004. [DOI] [PubMed] [Google Scholar]
- 12.Fanaroff A.A., Stoll B.J., Wright L.L., NICHD Neonatal Research Network Trends in neonatal morbidity and mortality for very low birth weight infants. Am J Obstet Gynecol. 2007;196(2):147.e1–147.e8. doi: 10.1016/j.ajog.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 13.Stoll B.J., Hansen N.I., Bell E.F. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126(3):443–456. doi: 10.1542/peds.2009-2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guillet R., Stoll B.J., Cotten C.M. Association of H2-blocker therapy and higher incidence of necrotizing enterocolitis in very low birth weight infants. Pediatrics. 2006;117(2):e137–e142. doi: 10.1542/peds.2005-1543. [DOI] [PubMed] [Google Scholar]
- 15.Fitzgibbons S.C., Ching Y., Yu D. Mortality of necrotizing enterocolitis expressed by birth weight categories. J Pediatr Surg. 2009;44(6):1072–1075. doi: 10.1016/j.jpedsurg.2009.02.013. [discussion: 1075–6] [DOI] [PubMed] [Google Scholar]
- 16.EXPRESS group Incidence of and risk factors for neonatal morbidity after active perinatal care: extremely preterm infants study in Sweden (EXPRESS) Acta Paediatr. 2010;99(7):978–992. doi: 10.1111/j.1651-2227.2010.01846.x. [DOI] [PubMed] [Google Scholar]
- 17.Bajwa N.M., Berner M., Worley S., Swiss Neonatal Network Population based age stratified morbidities of premature infants in Switzerland. Swiss Med Wkly. 2011;141:w13212. doi: 10.4414/smw.2011.13212. [DOI] [PubMed] [Google Scholar]
- 18.Yee W.H., Soraisham A.S., Shah V.S. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics. 2012;129(2):e298–e304. doi: 10.1542/peds.2011-2022. [DOI] [PubMed] [Google Scholar]
- 19.Hunter C.J., Upperman J.S., Ford H.R. Understanding the susceptibility of the premature infant to necrotizing enterocolitis (NEC) Pediatr Res. 2008;63(2):117–123. doi: 10.1203/PDR.0b013e31815ed64c. [DOI] [PubMed] [Google Scholar]
- 20.Berrington J.E., Hearn R.I., Bythell M. Deaths in preterm infants: changing pathology over 2 decades. J Pediatr. 2012;160(1):49–53.e1. doi: 10.1016/j.jpeds.2011.06.046. [DOI] [PubMed] [Google Scholar]
- 21.Neu J., Mihatsch W. Recent developments in necrotizing enterocolitis. JPEN J Parenter Enteral Nutr. 2012;36(Suppl 1):30S–35S. doi: 10.1177/0148607111422068. [DOI] [PubMed] [Google Scholar]
- 22.Sharma R., Tepas J.J. Microecology, intestinal epithelial barrier and necrotizing enterocolitis. Pediatr Surg Int. 2010;26:11–21. doi: 10.1007/s00383-009-2536-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Young C.M., Kingma S.D., Neu J. Ischemia-reperfusion and neonatal intestinal injury. J Pediatr. 2011;158:e25–e28. doi: 10.1016/j.jpeds.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 24.Neu J. The myth of asphyxia and hypoxia-ischemia as primary causes of necrotizing enterocolitis. Biol Neonate. 2005;87:97–98. doi: 10.1159/000081898. [DOI] [PubMed] [Google Scholar]
- 25.Sharma R., Hudak M.L., Tepas J.J., 3rd Prenatal or postnatal indomethacin exposure and neonatal gut injury associated with isolated intestinal perforation and necrotizing enterocolitis. J Perinatol. 2010;30(12):786–793. doi: 10.1038/jp.2010.59. [DOI] [PubMed] [Google Scholar]
- 26.Nowicki P.T., Caniano D.A., Hammond S. Endothelial nitric oxide synthase in human intestine resected for necrotizing enterocolitis. J Pediatr. 2007;150(1):40–45. doi: 10.1016/j.jpeds.2006.09.029. [DOI] [PubMed] [Google Scholar]
- 27.Nankervis C.A., Giannone P.J., Reber K.M. The neonatal intestinal vasculature: contributing factors to necrotizing enterocolitis. Semin Perinatol. 2008;32:83–91. doi: 10.1053/j.semperi.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 28.Berseth C.L. Gut motility and the pathogenesis of necrotizing enterocolitis. Clin Perinatol. 1994;21(2):263–270. [PubMed] [Google Scholar]
- 29.Wu S.F., Caplan M., Lin H.C. Necrotizing enterocolitis: old problem with new hope. Pediatr Neonatol. 2012;53(3):158–163. doi: 10.1016/j.pedneo.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 30.Morowitz M.J., Poroyko V., Caplan M. Redefining the role of intestinal microbes in the pathogenesis of necrotizing enterocolitis. Pediatrics. 2010;125(4):777–785. doi: 10.1542/peds.2009-3149. [DOI] [PubMed] [Google Scholar]
- 31.Sharma R., Tepas J.J., 3rd, Hudak M.L. Neonatal gut barrier and multiple organ failure: role of endotoxin and proinflammatory cytokines in sepsis and necrotizing enterocolitis. J Pediatr Surg. 2007;42(3):454–461. doi: 10.1016/j.jpedsurg.2006.10.038. [DOI] [PubMed] [Google Scholar]
- 32.Ravindranath T., Yoshioka T., Goto M. Endotoxemia following enteral refeeding in children. Clin Pediatr (Phila) 1997;36(9):523–528. doi: 10.1177/000992289703600905. [DOI] [PubMed] [Google Scholar]
- 33.Kau A., Ahren P.P., Griffin N.W. Human nutrition, the gut microbiome, and immune system: envisioning the future. Nature. 2012;474(7351):327–336. doi: 10.1038/nature10213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu Z., Li N., Neu J. Tight junctions, leaky intestines, and pediatric diseases. Acta Paediatr. 2005;94(4):386–393. doi: 10.1111/j.1651-2227.2005.tb01904.x. [DOI] [PubMed] [Google Scholar]
- 35.Sharma R., Young C., Neu J. Molecular modulation of intestinal epithelial barrier: contribution of microbiota. J Biomed Biotechnol. 2010;2010:305879. doi: 10.1155/2010/305879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Josephson C.D., Wesolowski A., Bao G. Do red cell transfusions increase the risk of necrotizing enterocolitis in premature infants? J Pediatr. 2010;157(6):972–978.e1–3. doi: 10.1016/j.jpeds.2010.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Christensen R.D., Lambert D.K., Henry E. Is “transfusion-associated necrotizing enterocolitis” an authentic pathogenic entity? Transfusion. 2010;50(5):1106–1112. doi: 10.1111/j.1537-2995.2009.02542.x. [DOI] [PubMed] [Google Scholar]
- 38.Singh R., Visintainer P.F., Frantz I.D., 3rd Association of necrotizing enterocolitis with anemia and packed red blood cell transfusions in preterm infants. J Perinatol. 2011;31(3):176–182. doi: 10.1038/jp.2010.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Paul D.A., Mackley A., Novitsky A. Increased odds of necrotizing enterocolitis after transfusion of red blood cells in premature infants. Pediatrics. 2011;127(4):635–641. doi: 10.1542/peds.2010-3178. [DOI] [PubMed] [Google Scholar]
- 40.Blau J., Calo J.M., Dozor D. Transfusion-related acute gut injury: necrotizing enterocolitis in very low birth weight neonates after packed red blood cell transfusion. J Pediatr. 2011;158(3):403–409. doi: 10.1016/j.jpeds.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 41.dos Santos A.M., Guinsburg R., de Almeida M.F., Brazilian Network on Neonatal Research Red blood cell transfusions are independently associated with intra-hospital mortality in very low birth weight preterm infants. J Pediatr. 2011;159(3):371–376.e1–3. doi: 10.1016/j.jpeds.2011.02.040. [DOI] [PubMed] [Google Scholar]
- 42.El-Dib M., Narang S., Lee E. Red blood cell transfusion, feeding and necrotizing enterocolitis in preterm infants. J Perinatol. 2011;31(3):183–187. doi: 10.1038/jp.2010.157. [DOI] [PubMed] [Google Scholar]
- 43.Afrazi A., Sodhi C.P., Richardson W. New insights into the pathogenesis and treatment of necrotizing enterocolitis: toll-like receptors and beyond. Pediatr Res. 2011;69(3):183–188. doi: 10.1203/PDR.0b013e3182093280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Neish A.S. Microbes in gastrointestinal health and disease. Gastroenterology. 2009;136(1):65–80. doi: 10.1053/j.gastro.2008.10.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kawai T., Akira S. Toll-like receptors and their crosstalk with other innate receptors in infection and immunity. Immunity. 2011;34(5):637–650. doi: 10.1016/j.immuni.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 46.Lin P.W., Nasr T.R., Stoll B.J. Necrotizing enterocolitis: recent scientific advances in pathophysiology and prevention. Semin Perinatol. 2008;32(2):70–82. doi: 10.1053/j.semperi.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 47.Neu J., Chen M., Beierle E. Intestinal innate immunity: how does it relate to the pathogenesis of necrotizing enterocolitis. Semin Pediatr Surg. 2005;14(3):137–144. doi: 10.1053/j.sempedsurg.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 48.Nanthakumar N., Meng D., Goldstein A.M. The mechanism of excessive intestinal inflammation in necrotizing enterocolitis: an immature innate response. PLoS One. 2011;6(3):e17776. doi: 10.1371/journal.pone.0017776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ganguli K., Walker W.A. Probiotics in the prevention of necrotizing enterocolitis. J Clin Gastroenterol. 2011;45(Suppl):S133–S138. doi: 10.1097/MCG.0b013e318228b799. [DOI] [PubMed] [Google Scholar]
- 50.Lin P.W., Myers L.E., Ray L. Lactobacillus rhamnosus blocks inflammatory signaling in vivo via reactive oxygen species generation. Free Radic Biol Med. 2009;47(8):1205–1211. doi: 10.1016/j.freeradbiomed.2009.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Alexander V.N., Northrup V., Bizzarro M.J. Antibiotic exposure in the newborn intensive care unit and the risk of necrotizing enterocolitis. J Pediatr. 2011;159(3):392–397. doi: 10.1016/j.jpeds.2011.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cotten C.M., Taylor S., Stoll B. Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics. 2009;123:58–66. doi: 10.1542/peds.2007-3423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bengmark S. Gut microbiota, immune development and function. Pharmacol Res. 2012 doi: 10.1016/j.phrs.2012.09.002. pii: S1043–6618(12)00166-1. [DOI] [PubMed] [Google Scholar]
- 54.Cilieborg M.S., Boye M., Sangild P.T. Bacterial colonization and gut development in preterm neonates. Early Hum Dev. 2012;88(Suppl 1):S41–S49. doi: 10.1016/j.earlhumdev.2011.12.027. [Epub 2012 Jan 28] [DOI] [PubMed] [Google Scholar]
- 55.Mai V., Young C.M., Ukhanova M. Fecal microbiota in premature infants prior to necrotizing enterocolitis. PLoS. 2011;6(6):e20647. doi: 10.1371/journal.pone.0020647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mohankumar K., Kaza N., Jagadeeswaran R. Gut mucosal injury in neonates is marked by macrophage infiltration in contrast to pleomorphic infiltrates in adult: evidence from an animal model. Am J Physiol Gastrointest Liver Physiol. 2012;303(1):G93–G102. doi: 10.1152/ajpgi.00016.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nanthakumar N.N., Young C., Ko J.S. Glucocorticoid responsiveness in developing human intestine: possible role in prevention of necrotizing enterocolitis. Am J Physiol Gastrointest Liver Physiol. 2005;288(1):G85–G92. doi: 10.1152/ajpgi.00169.2004. [DOI] [PubMed] [Google Scholar]
- 58.Desfrere L., de Oliveira I., Goffinet F. Increased incidence of necrotizing enterocolitis in premature infants born to HIV-positive mothers. AIDS. 2005;19(14):1487–1493. doi: 10.1097/01.aids.0000183123.09206.07. [DOI] [PubMed] [Google Scholar]
- 59.Cunningham S.C., Fakhry K., Bass B.L. Neutropenic enterocolitis in adults: case series and review of the literature. Dig Dis Sci. 2005;50(2):215–220. doi: 10.1007/s10620-005-1585-1. [DOI] [PubMed] [Google Scholar]
- 60.Choi J.H., Lee J.M., Shin W.S. Necrotizing enterocolitis: experience of 27 cases from a single Korean institution. Int J Hematol. 2000;72(3):358–361. [PubMed] [Google Scholar]
- 61.Downard C.D., Grant S.N., Matheson P.J. Altered intestinal microcirculation is the critical event in the development of necrotizing enterocolitis. J Pediatr Surg. 2011;46(6):1023–1028. doi: 10.1016/j.jpedsurg.2011.03.023. [DOI] [PubMed] [Google Scholar]
- 62.Kim M., Christley S., Alverdy J.C. Immature oxidative stress management as a unifying principle in the pathogenesis of necrotizing enterocolitis: insights from an agent-based model. Surg Infect (Larchmt) 2012;13(1):18–32. doi: 10.1089/sur.2011.057. [Epub 2012 Jan 4] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chokshi N.K., Guner Y.S., Hunter C.J. The role of nitric oxide in intestinal epithelial injury and restitution in neonatal necrotizing enterocolitis. Semin Perinatol. 2008;32(2):92–99. doi: 10.1053/j.semperi.2008.01.002. [review] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li N., Quidgley M.C., Kobeissy F.H. Microbial cell components induced tolerance to flagellin-stimulated inflammation through Toll-like receptor pathways in intestinal epithelial cells. Cytokine. 2012;60(3):806–811. doi: 10.1016/j.cyto.2012.08.003. [PMID: 22944462] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Smith B., Bodé S., Skov T.H. Investigation of the early intestinal microflora in premature infants with/without necrotizing enterocolitis using two different methods. Pediatr Res. 2012;71(1):115–120. doi: 10.1038/pr.2011.1. [DOI] [PubMed] [Google Scholar]
- 66.Peter C.S., Feuerhahn M., Bohnhorst B. Necrotising enterocolitis: is there a relationship to specific pathogens? Eur J Pediatr. 1999;158:67–70. doi: 10.1007/s004310051012. [DOI] [PubMed] [Google Scholar]
- 67.Powell J., Bureau M.A., Pare C. Necrotizing enterocolitis. Epidemic following an outbreak of Enterobacter cloacae type 3305573 in a neonatal intensive care unit. Am J Dis Child. 1980;134:1152–1154. [PubMed] [Google Scholar]
- 68.Mollitt D.L., Tepas J.J., 3rd, Talbert J.L. The microbiology of neonatal peritonitis. Arch Surg. 1988;123:176–179. doi: 10.1001/archsurg.1988.01400260056006. [DOI] [PubMed] [Google Scholar]
- 69.Howard F.M., Flynn D.M., Bradley J.M. Outbreak of necrotising enterocolitis caused by Clostridium butyricum. Lancet. 1977;2:1099–1102. doi: 10.1016/s0140-6736(77)90546-3. [DOI] [PubMed] [Google Scholar]
- 70.Van Acker J., de Smet F., Muyldermans G. Outbreak of necrotizing enterocolitis associated with Enterobacter sakazakii in powdered milk formula. J Clin Microbiol. 2001;39:293–297. doi: 10.1128/JCM.39.1.293-297.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Smith B., Bodé S., Petersen B.L. Community analysis of bacteria colonizing intestinal tissue of neonates with necrotizing enterocolitis. BMC Microbiol. 2011;11:73. doi: 10.1186/1471-2180-11-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tzialla C., Civardi E., Borghesi A. Emerging viral infections in neonatal intensive care unit. J Matern Fetal Neonatal Med. 2011;24(Suppl 1):156–158. doi: 10.3109/14767058.2011.607588. [Epub 2011 Aug 31] [DOI] [PubMed] [Google Scholar]
- 73.Sharma R., Hudak M.L., Premachandra B.R. Clinical manifestations of rotavirus infection in the neonatal intensive care unit. Pediatr Infect Dis J. 2002;21(12):1099–1105. doi: 10.1097/00006454-200212000-00003. [DOI] [PubMed] [Google Scholar]
- 74.Stuart R.L., Tan K., Mahar J.E. An outbreak of necrotizing enterocolitis associated with norovirus genotype GII.3. Pediatr Infect Dis J. 2010;29(7):644–647. doi: 10.1097/inf.0b013e3181d824e1. [DOI] [PubMed] [Google Scholar]
- 75.Sharma R., Garrison R.D., Tepas J.J., 3rd Rotavirus-associated necrotizing enterocolitis: an insight into a potentially preventable disease? J Pediatr Surg. 2004;39(3):453–457. doi: 10.1016/j.jpedsurg.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 76.Birenbaum E., Handsher R., Kuint J. Echovirus type 22 outbreak associated with gastro-intestinal disease in a neonatal intensive care unit. Am J Perinatol. 1997;14:469–473. doi: 10.1055/s-2007-994182. [DOI] [PubMed] [Google Scholar]
- 77.Chany C., Moscovici O., Lebon P. Association of coronavirus infection with neonatal necrotizing enterocolitis. Pediatrics. 1982;69:209–214. [PubMed] [Google Scholar]
- 78.Bagci S., Eis-Hübinger A.M., Franz A.R. Detection of astrovirus in premature infants with necrotizing enterocolitis. Pediatr Infect Dis J. 2008;27(4):347–350. doi: 10.1097/INF.0b013e318162a17a. [DOI] [PubMed] [Google Scholar]
- 79.Lodha A., de Silva N., Petric M. Human torovirus: a new virus associated with neonatal necrotizing enterocolitis. Acta Paediatr. 2005;94:1085–1088. doi: 10.1111/j.1651-2227.2005.tb02049.x. [DOI] [PubMed] [Google Scholar]
- 80.Karlowicz M.G. Risk factors associated with fungal peritonitis in very low birth weight neonates with severe necrotizing enterocolitis: a case-control study. Pediatr Infect Dis J. 1993;12:574–577. doi: 10.1097/00006454-199307000-00005. [DOI] [PubMed] [Google Scholar]
- 81.Boccia D., Stolfi I., Lana S. Nosocomial necrotizing outbreaks: epidemiology and control measures. Eur J Pediatr. 2001;160:385–391. doi: 10.1007/s004310100749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lemyre B., Xiu W., Bouali N.R. A decrease in the number of cases of necrotizing enterocolitis associated with the enhancement of infection prevention and control measures during a Staphylococcus aureus outbreak in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2012;33(1):29–33. doi: 10.1086/663343. [DOI] [PubMed] [Google Scholar]
- 83.Faustini A., Forastiere F., Giorgi-Rossi P. An epidemic of gastroenteritis and mild necrotizing enterocolitis in two neonatal units of a university hospital in Rome, Italy. Epidemiol Infect. 2004;132(3):455–465. doi: 10.1017/s0950268804002006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Turcios-Ruiz R.M., Axelrod P., St John K. Outbreak of necrotizing enterocolitis caused by norovirus in a neonatal intensive care unit. J Pediatr. 2008;153(3):339–344. doi: 10.1016/j.jpeds.2008.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chappé C., Minjolle S., Dabadie A. Astrovirus and digestive disorders in neonatal units. Acta Paediatr. 2012;101(5):e208–e212. doi: 10.1111/j.1651-2227.2011.02569.x. [DOI] [PubMed] [Google Scholar]
- 86.Moscovici O., Chany C., Lebon P. Association of coronavirus infection with hemorrhagic enterocolitis in newborn infantsC R Seances Acad Sci D. 1980;290(13):869–872. [in French] [PubMed] [Google Scholar]
- 87.Bagci S., Eis-Hübinger A.M., Yassin A.F. Clinical characteristics of viral intestinal infection in preterm and term neonates. Eur J Clin Microbiol Infect Dis. 2010;29(9):1079–1084. doi: 10.1007/s10096-010-0965-4. [DOI] [PubMed] [Google Scholar]
- 88.Ball J.M., Tian P., Zeng C.Q. Age-dependent diarrhea induced by rotavirus nonstructural glycoprotein. Science. 1996;272:101–104. doi: 10.1126/science.272.5258.101. [DOI] [PubMed] [Google Scholar]
- 89.Guttman J.A., Finlay B.B. Tight junctions as targets of infectious agents. Biochim Biophys Acta. 2009;1788(4):832–841. doi: 10.1016/j.bbamem.2008.10.028. [DOI] [PubMed] [Google Scholar]
- 90.Morris A.P., Estes M.K. Microbes and microbial toxins: paradigms for microbial-mucosal interactions. VIII. Pathological consequences of rotavirus infection and its enterotoxin. Am J Physiol Gastrointest Liver Physiol. 2001;281(2):G303–G310. doi: 10.1152/ajpgi.2001.281.2.G303. [DOI] [PubMed] [Google Scholar]
- 91.Schroeder M.E., Hosteller H.A., Schroeder F. Elucidation of the rotavirus NSP4-caveolin-1 and-cholesterol interactions using synthetic peptides. J Amino acids. 2012;2012:575180. doi: 10.1155/2012/575180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Neish A.S. The gut microflora and intestinal epithelial cells: a continuing dialogue. Microbes infect. 2002;4:309–317. doi: 10.1016/s1286-4579(02)01543-5. [DOI] [PubMed] [Google Scholar]
- 93.Cilieborg M.S., Boye M., Mølbak L. Preterm birth and necrotizing enterocolitis alter gut colonization in pigs. Pediatr Res. 2011;69(1):10–16. doi: 10.1203/PDR.0b013e3181ff2a89. [DOI] [PubMed] [Google Scholar]
- 94.Kliegman R.M., Hack M., Jones P. Epidemiological study of necrotizing enterocolitis among low birth weight infants. J Pediatr. 1982;100:440–444. doi: 10.1016/s0022-3476(82)80456-3. [DOI] [PubMed] [Google Scholar]
- 95.Kanto W.P., Jr., Hunter J.E., Stoll B.J. Recognition and medical management of necrotizing enterocolitis. Clin Perinatol. 1994;21(2):335–346. [PubMed] [Google Scholar]
- 96.Gephart S.M., McGrath J.M., Effken J.A. Necrotizing enterocolitis risk: state of the science. Adv Neonatal Care. 2012;12(2):77–87. doi: 10.1097/ANC.0b013e31824cee94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sharma R., Tepas J.J., 3rd, Hudak M.L. Portal venous gas and surgical outcome of neonatal necrotizing enterocolitis. J Pediatr Surg. 2005;40(2):371–376. doi: 10.1016/j.jpedsurg.2004.10.022. [DOI] [PubMed] [Google Scholar]
- 98.Faix R.G., Nelson M. Neonatal enterocolitis: progress, problems, and prospects. In: David T.J., editor. vol. 16. Churchill Livingstone; Edinburgh: 1998. pp. 359–407. (Recent advances in Paediatrics). [Google Scholar]
- 99.Abramo T.J., Evans J.S., Kokomoor F.W. Occult blood in stools and necrotizing enterocolitis. Am J Dis Child. 1988;142:451–452. doi: 10.1001/archpedi.1988.02150040105030. [DOI] [PubMed] [Google Scholar]
- 100.Sharma R., Tepas J.J., 3rd, Mollitt D.L. Surgical management of bowel perforations and outcome in very low-birth-weight infants (≤1,200 g) J Pediatr Surg. 2004;39(2):190–194. doi: 10.1016/j.jpedsurg.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 101.Cole C.R., Hansen N.I., Higgins R.D., Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Neonatal Research Network Bloodstream infections in very low birth weight infants with intestinal failure. J Pediatr. 2012;160(1):54–59.e2. doi: 10.1016/j.jpeds.2011.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sharma R., Tepas J.J., 3rd, Hudak M.L. Neonatal gut injury and infection rate: impact of surgical debridement on outcome. Pediatr Surg Int. 2005;21(12):977–982. doi: 10.1007/s00383-005-1539-x. [DOI] [PubMed] [Google Scholar]
- 103.Stringer M.D., Brereton R.J., Drake D.P. Recurrent necrotizing enterocolitis. J Pediatr Surg. 1993;28(8):979–981. doi: 10.1016/0022-3468(93)90496-8. [DOI] [PubMed] [Google Scholar]
- 104.Srinivasan P., Brandler M., D'Souza A. Allergic enterocolitis presenting as recurrent necrotizing enterocolitis in preterm neonates. J Perinatol. 2010;30(6):431–433. doi: 10.1038/jp.2009.153. [DOI] [PubMed] [Google Scholar]
- 105.Coviello C., Rodriquez D.C., Cecchi S. Different clinical manifestation of cow's milk allergy in two preterm twins newborns. J Matern Fetal Neonatal Med. 2012;25(Suppl 1):132–133. doi: 10.3109/14767058.2012.663171. [DOI] [PubMed] [Google Scholar]
- 106.Morrison S.C., Jacobson J.M. The radiology of necrotizing enterocolitis. Clin Perinatol. 1994;21(2):347–363. [PubMed] [Google Scholar]
- 107.Epelman M., Daneman A., Navarro O.M. Necrotizing enterocolitis: review of state-of-the-art imaging findings with pathologic correlation. Radiographics. 2007;27:285–305. doi: 10.1148/rg.272055098. [DOI] [PubMed] [Google Scholar]
- 108.Faingold R., Daneman A., Tomlinson G. Necrotizing enterocolitis: assessment of bowel viability with color Doppler US. Radiology. 2005;235(2):587–594. doi: 10.1148/radiol.2352031718. [DOI] [PubMed] [Google Scholar]
- 109.Kanto W.P., Jr., Wilson R., Ricketts R.R. Management and outcome of necrotizing enterocolitis. Clin Pediatr (Phila) 1985;24(2):79–82. doi: 10.1177/000992288502400203. [DOI] [PubMed] [Google Scholar]
- 110.Walsh M.C., Kliegman R.M. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986;33(1):179–201. doi: 10.1016/S0031-3955(16)34975-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Neu J. Neonatal necrotizing enterocolitis: an update. Acta Paediatr Suppl. 2005;94(449):100–105. doi: 10.1111/j.1651-2227.2005.tb02163.x. [DOI] [PubMed] [Google Scholar]
- 112.Tepas J.J., 3rd, Leaphart C.L., Plumley D. Trajectory of metabolic derangement in infants with necrotizing enterocolitis should drive timing and technique of surgical intervention. J Am Coll Surg. 2010;210:847–852. doi: 10.1016/j.jamcollsurg.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 113.Musemeche C.A., Kosloske A.M., Ricketts R.R. Enterostomy in necrotizing enterocolitis: an analysis of techniques and timing of closure. J Pediatr Surg. 1987;22(6):479–483. doi: 10.1016/s0022-3468(87)80200-2. [DOI] [PubMed] [Google Scholar]
- 114.Tepas J.J., 3rd, Sharma R., Leaphart C.L. Timing of surgical intervention in necrotizing enterocolitis can be determined by trajectory of metabolic derangement. J Pediatr Surg. 2010;45(2):310–313. doi: 10.1016/j.jpedsurg.2009.10.069. [discussion: 313–4] [DOI] [PubMed] [Google Scholar]
- 115.Ein S.H., Shandling B., Wesson D. A 13-year experience with peritoneal drainage under local anesthesia for necrotizing enterocolitis perforation. J Pediatr Surg. 1990;25:1034–1036. doi: 10.1016/0022-3468(90)90213-s. [DOI] [PubMed] [Google Scholar]
- 116.Rao S.C., Basani L., Simmer K. Peritoneal drainage versus laparotomy as initial surgical treatment for perforated necrotizing enterocolitis or spontaneous intestinal perforation in preterm low birth weight infants. Cochrane Database Syst Rev. 2011;(6) doi: 10.1002/14651858.CD006182.pub2. CD006182. [DOI] [PubMed] [Google Scholar]
- 117.Rees C.M., Eaton S., Kiely E.M. Peritoneal drainage or laparotomy for neonatal bowel perforation? A randomized controlled trial. Ann Surg. 2008;248:44–51. doi: 10.1097/SLA.0b013e318176bf81. [DOI] [PubMed] [Google Scholar]
- 118.Moss R.L., Dimmit R.A., Barnhart D.C. Laparotomy versus peritoneal drainage for necrotizing enterocolitis. N Engl J Med. 2006;354:2225–2234. doi: 10.1056/NEJMoa054605. [DOI] [PubMed] [Google Scholar]
- 119.Pierro A., Eaton S., Rees C.M. Is there a benefit of peritoneal drainage for necrotizing enterocolitis in newborn infants? J Pediatr Surg. 2010;45:2117–2118. doi: 10.1016/j.jpedsurg.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 120.Blakely M.L., Tyson J.E., Lally K.P. Laparotomy versus peritoneal drainage for necrotizing enterocolitis or isolated intestinal perforation in extremely low birth weight infants: outcomes through 18 months adjusted age. Pediatrics. 2006;117(4):e680–e687. doi: 10.1542/peds.2005-1273. [DOI] [PubMed] [Google Scholar]
- 121.Sola J.E., Tepas J.J., 3rd, Koniaris L.G. Peritoneal drainage versus laparotomy for necrotizing enterocolitis and intestinal perforation: a meta-analysis. J Surg Res. 2010;161(1):95–100. doi: 10.1016/j.jss.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 122.Tepas J.J., 3rd, Sharma R., Hudak M.L. Coming full circle: an evidence-based definition of the timing and type of surgical management of very low-birth-weight (<1000 g) infants with signs of acute intestinal perforation. J Pediatr Surg. 2006;41(2):418–422. doi: 10.1016/j.jpedsurg.2005.11.041. [DOI] [PubMed] [Google Scholar]
- 123.Kosloske A.M. Indications for operation in necrotizing enterocolitis revisited. J Pediatr Surg. 1994;29(5):663–666. doi: 10.1016/0022-3468(94)90736-6. [DOI] [PubMed] [Google Scholar]
- 124.Ballance W.A., Dahms B.B., Shenker N. Pathology of necrotizing enterocolitis: a ten year experience. J Pediatr. 1990;117:S6–S13. doi: 10.1016/s0022-3476(05)81124-2. [DOI] [PubMed] [Google Scholar]
- 125.Gould S.J. The pathology of necrotizing enterocolitis. Semin Neonatol. 1997;4:239–244. [Google Scholar]
- 126.Jacobs J.E., Birnbaum B.A., Maglinte D.D. Vascular disorders of the small intestine. In: Herlinger H., Maglinte D.D., Birnbaum B.A., editors. Clinical imaging of the small intestine. 2nd edition. Springer-Verlag; New York: 1999. pp. 439–465. [Google Scholar]
- 127.Nankervis C.A., Reber K.M., Nowicki P.T. Age-dependent changes in the postnatal intestinal microcirculation. Microcirculation. 2001;8(6):377–387. doi: 10.1038/sj/mn/7800110. [DOI] [PubMed] [Google Scholar]
- 128.Nowicki P.T., Miller C.E., Edwards R.C. Effects of hypoxia and ischemia on autoregulation in postnatal intestine. Am J Physiol. 1991;261:G152–G157. doi: 10.1152/ajpgi.1991.261.1.G152. [DOI] [PubMed] [Google Scholar]
- 129.Sankaran K., Puckett B., Lee D.S., Canadian Neonatal Network Variations in incidence of necrotizing enterocolitis in Canadian neonatal intensive care units. J Pediatr Gastroenterol Nutr. 2004;39(4):366–372. doi: 10.1097/00005176-200410000-00012. [DOI] [PubMed] [Google Scholar]
- 130.Abdullah F., Zhang Y., Camp M. Necrotizing enterocolitis in 20,822 infants: analysis of medical and surgical treatments. Clin Pediatr (Phila) 2010;49(2):166–171. doi: 10.1177/0009922809349161. [DOI] [PubMed] [Google Scholar]
- 131.Guner Y.S., Friedlich P., Wee C.P. State-based analysis of necrotizing enterocolitis outcomes. J Surg Res. 2009;157(1):21–29. doi: 10.1016/j.jss.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 132.Martin C.R., Dammann O., Allred E.N. Neurodevelopment of extremely preterm infants who had necrotizing enterocolitis with or without late bacteremia. J Pediatr. 2010;157(5):751–756.e1. doi: 10.1016/j.jpeds.2010.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Shah D.K., Doyle L.W., Anderson P.J. Adverse neurodevelopment in preterm infants with postnatal sepsis or necrotizing enterocolitis is mediated by white matter abnormalities on magnetic resonance imaging at term. J Pediatr. 2008;153(2):170–175. doi: 10.1016/j.jpeds.2008.02.033. 175.e1 [Epub 2008 Apr 3] [DOI] [PubMed] [Google Scholar]
- 134.Pike K., Brocklehurst P., Jones D. Outcomes at 7 years for babies who developed neonatal necrotising enterocolitis: the ORACLE Children Study. Arch Dis Child Fetal Neonatal Ed. 2012;97(5):F318–F322. doi: 10.1136/fetalneonatal-2011-300244. [DOI] [PubMed] [Google Scholar]
- 135.Warner B.B., Ryan A.L., Seeger K. Ontogeny of salivary epidermal growth factor and necrotizing enterocolitis. J Pediatr. 2007;150(4):358–363. doi: 10.1016/j.jpeds.2006.11.059. [DOI] [PubMed] [Google Scholar]
- 136.Perrone S., Tataranno M.L., Negro S. May oxidative stress biomarkers in cord blood predict the occurrence of necrotizing enterocolitis in preterm infants? J Matern Fetal Neonatal Med. 2012;25(Suppl 1):128–131. doi: 10.3109/14767058.2012.663197. [DOI] [PubMed] [Google Scholar]
- 137.Chan K.Y., Leung F.W., Lam H.S. Immunoregulatory protein profiles of necrotizing enterocolitis versus spontaneous intestinal perforation in preterm infants. PLoS One. 2012;7(5):e36977. doi: 10.1371/journal.pone.0036977. [DOI] [PMC free article] [PubMed] [Google Scholar]