Abstract
After hospital discharge, correct understanding and use of medications are key components of patient safety. The current discharge process does not provide adequate fail-safes to ensure quality post-discharge care. This often leads to preventable medication errors as well as non-adherence. Several barriers to successful discharge counseling, including use of medical jargon, lack of educational and administrative resources, time constraints, and low health literacy, contribute to ineffective communication between hospital physicians and patients. Other obstacles include inaccurate or incomplete documentation of the medication history, lack of social support, financial constraints, and poor transfer of information to outpatient physicians. Solutions to improve medication use in the transition period after hospital discharge require effective communication with patients through the use of easily understood language, highlighting key information, and ensuring patient comprehension through the “teach back” technique. More timely communication with outpatient physicians in addition to a more comprehensive transfer of information further facilitate the transition home. Finally, a systematic process of medication reconciliation also aids in decreasing the incidence of medication errors. Hospital-based physicians who attend to key details in the process of discharging patients can have a profound impact on improving medication adherence, avoiding medication errors, and decreasing adverse outcomes in the post-discharge period.
Keywords: medication adherence, patient education, communication, hospital medicine, medication reconciliation
Introduction
Hospital discharge can be a complex and challenging time for physicians and patients alike. Patients are being discharged sooner, often in the process of convalescence rather than at baseline health status.1 This requires physicians to more effectively communicate instructions for post-discharge care to patients, family members, and outpatient providers. A comprehensive review on improving all aspects of this process is beyond the scope of this article; we will focus specifically on improving medication use. Patients are very susceptible to medical errors in the days immediately following hospital discharge. Forty-nine percent of hospitalized patients experience at least one medical error following discharge, most commonly involving medication use.2, 3 An estimated 19–23% of patients suffer an adverse drug event (ADE) after discharge.3–5 Most of these errors and ADEs could be prevented through better communication.2, 3 This commentary will discuss several common barriers to proper medication use after hospital discharge and review potential solutions based on the experience in the United States.
Barriers to Safe and Effective Medication Use
Inaccurate Documentation of Medications
Medication-related problems after hospital discharge sometimes begin with an inaccurate or incomplete medication history upon hospital admission. The quality of the medication list is influenced by interviewer skills, patient’s knowledge, availability of prior documentation, and time constraints.6, 7 Moreover, multiple hospital personnel may take a medication history and construct inconsistent lists that are never reconciled. Half of patients have at least one unintended medication discrepancy on admission, 39–45% of which are deemed potentially harmful.8, 9 The most common discrepancy is omission of a home medication.10
During hospitalization, documentation of medication changes, their rationale, and whether changes are temporary or permanent, is often lacking. Medications may change for a number of reasons. Acute illness may require that a medication be held, changed, or stopped altogether. Prophylactic temporary medications intended only for the inpatient stay may inadvertently remain on the medication list at discharge. Restricted hospital formularies often lead to substitution of medications on admission, which may not be switched back to the outpatient drug upon discharge.11 Transfers to different hospital wards, or changes to the regimen for surgical procedures, add further opportunities for discrepancies and errors that can persist through and beyond discharge.
Ineffective Physician-Patient Communication
Medication mismanagement after hospital discharge is often related to poor communication of discharge instructions. When physicians counsel patients at discharge, they typically present a large amount of information in a short period of time. This information may be laden with medical jargon, which patients and their family members struggle to understand.12, 13 Moreover, physicians tend to overestimate patients’ comprehension and may not provide enough opportunity for patients or family members to ask questions.14 Physicians expressly confirm patient understanding only 15% of the time.15 As a result, patients often return home from the hospital without complete and accurate understanding of their diagnoses, key test results, or discharge medication regimen.16, 17
This is particularly common when patients have limited educational attainment or health literacy, which refers to the ability to understand and act on health information.18, 19 Even in industrialized nations such as the United States, approximately one-third of adults lack sufficient levels of health literacy to understand common medication instructions.20 Language barriers and culturally diverse expectations may also limit patients’ comprehension and adherence. Finally, hospitalized patients may have transient or persistent cognitive impairment, which limits comprehension and memory.21
Poor Physician Handoffs
Poor communication may also occur among physicians at hospital discharge, when the responsibility for patient care is passed from the inpatient to outpatient provider. Transfer of information is most commonly done through discharge summaries. However, these documents may suffer from poor handwriting, delays in their preparation, and missing or erroneous information.22 For example, discharge medications are absent from 2–40% of summaries.22 Delays in receipt of discharge summaries also pose problems with medication management at follow-up appointments. About 75% of the time, patients contact or visit the primary care physician (PCP) before the discharge summary has arrived.22 The PCP has to then determine, with limited information, which medications were stopped and why, as well as reasons for any new prescriptions.
Lack of Social Support
Upon returning home, patients are often required to assume new self-care responsibilities. However, many lack adequate social support, which makes it difficult to perform necessary self-care tasks, including medication management, particularly if their functional status is limited. As a result, many patients are unable to comply with post-discharge medication regimens despite comprehending their instructions. Patients prescribed more than 5 medications may experience added difficulty, and they are also at greater risk of ADEs.23, 24
Medication Costs
Medication costs also pose a significant burden when patients are required to pay a large share of this expense. Many patients on a fixed monthly income simply cannot afford to purchase several new medications, and about 20% of discharge prescriptions may go unfilled.25 Other patients try to make medications last longer by taking them less frequently than prescribed. Unfortunately, physicians often are unaware of the cost of the medications they prescribe, and they may be unaccustomed to having open conversations with patients about medication costs.26–28
Many insurance companies in countries like the United States or government subsidized medication programs in other locations like Singapore, have restricted or tiered formularies which offer lower co-pays for certain medications and not others. Many physicians and patients are unaware of the formulary restrictions and tiered costs, and do not routinely use this information to guide prescribing. This can contribute to higher out-of-pocket costs for patients, which leads to lower adherence.
Solutions
Medication Reconciliation
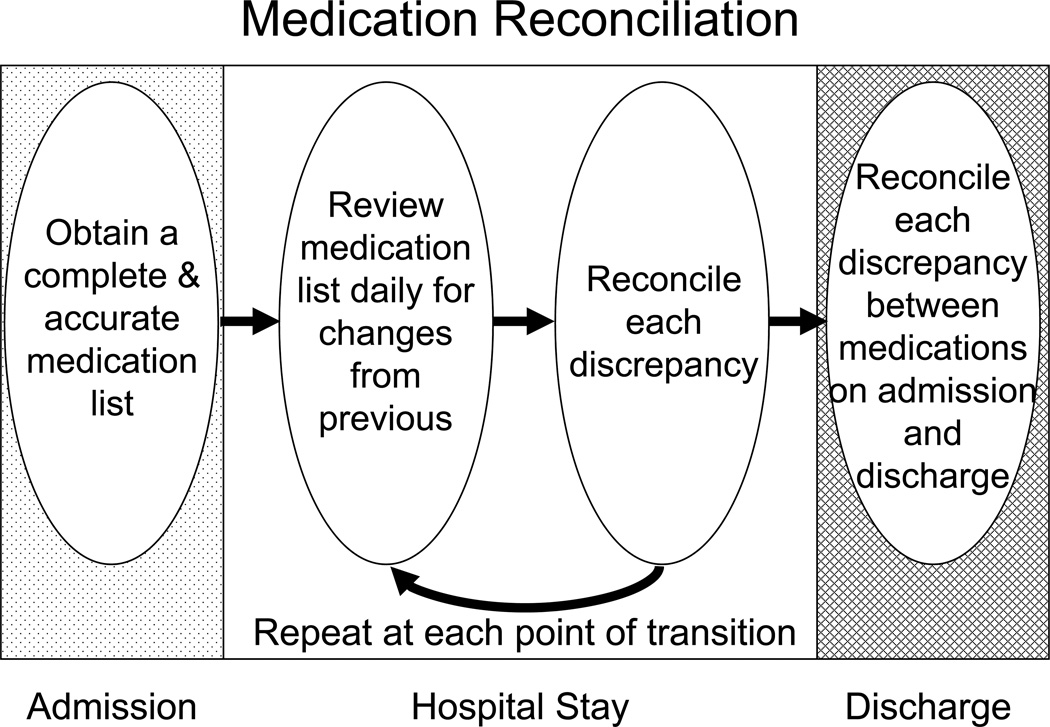
Better documentation of the patient’s medications reduces ADEs during and after hospitalization.29, 30 Medication reconciliation is the process of comparing the patient’s medication list to what he or she should be receiving, and resolving any discrepancies (Figure 1). This should occur daily throughout hospitalization, especially during transitions of care such as transfer to another ward or discharge, when errors most often occur.31 This process actually starts on admission, when it is important to obtain an accurate medication list by soliciting information from the patient, caregivers, pharmacies, pill bottles, and outpatient records or physicians. (See Table 1 for suggestions on improving the admission medication history.) Once the pre-admission list is confirmed, it should be written on a standardized form and placed in a consistent and prominent place in the chart. The intended plan for each medication should be explicitly stated (i.e., continue, discontinue, or change dosing). The purpose, planned duration, and dosing of each medication should also be listed. Resources to facilitate medication reconciliation, including sample forms, are available online.32–34
Figure 1.
Table 1.
Questions to help elicit a complete and accurate medication history from patients and family members
|
Adapted from Sullivan C, Gleason KM, Rooney D, et al. Medication reconciliation in the acute care setting: opportunity and challenge for nursing. J Nurs Care Qual 2005; 20:95–98; and from Kripalani S, Trobaugh AK, Coleman EA. Hospital Discharge. In: Williams MV, Hayward R, eds. Comprehensive Hospital Medicine, Elsevier (in press).
At discharge, medication reconciliation should identify and resolve differences between discharge medications and pre-admission medications. Attention should be given to several common discrepancies that can confuse the patient’s transition home if left uncorrected. For example, medications may be duplicated if the patient receives both a generic and branded version (e.g., if the patient already has the generic version at home and receives a new prescription at discharge for the same medication, but under a different branded name). A similar problem may occur if a brand is substituted due to hospital formulary restrictions, and a prescription for the new brand is written at discharge. Changes to the dose or frequency, as well as addition or deletion of medications, should be documented carefully. A new medication should be clearly marked as “New” and a specific comment made if it is replacing a previously taken medicine. Medications that were stopped should still be listed with a line through them and “Stop,” plus the reason for stopping them noted. The reason for each change, no matter how obvious, should be listed for the understanding of both the patient and outpatient provider. In addition, the purpose of each medicine should be documented in easily understood language. Grouping medications together by purpose rather than alphabetically or in a random fashion will also help the primary provider better comprehend the plan of care and serve as another “check” on the system to screen for omission or duplication errors.
The responsibility for medication reconciliation ultimately lies with the treating physician. However based on the hospital’s resources, specific tasks can be done by various members of the healthcare team, including pharmacists, nurses, and physician assistants. Responsibilities must be well-defined and should be complementary rather than duplicative. Pharmacists may be the ideal people to perform these activities, given their formal training in eliciting medication histories and counseling on their use.8 Using trained nursing staff and pharmacists to elicit admission medication histories, accuracy of admission medication orders increased from 40% to 95%.35 Another study showed that an intervention consisting of pharmacist medication review, patient counseling, and post-discharge telephone follow-up reduced preventable ADEs in the 30-day period after hospital discharge (1% in the intervention group vs. 11% in the control group, p=.01).30
Improving Physician-Patient Communication
When providing discharge instructions, physicians and other healthcare providers should make an effort to keep explanations simple and avoid medical jargon.19 Given the large amount of information that could potentially be conveyed, it is preferable to highlight key points, repeat them, and confirm understanding of these essential items. This is best done through an approach called “teach-back,” which involves asking the patient to repeat back their understanding of the instructions or to demonstrate a new technique (e.g. inhaler use).15 Teach-back is considered one of the most effective methods for improving patient safety.36, 37
Providing ample opportunity for questions is also important, as is the inclusion of all involved family members and caregivers, particularly because patients may leave the hospital with a physical or cognitive impairment and family may play an important role at home in managing the patient’s medications. Giving take-home instructions that are written in everyday language can enhance recall of discharge information.16, 17 Use of audiovisual materials or simple drawings made by the physician is also helpful.38, 39 An interpreter may be needed when a language barrier is present.
Patients are generally most concerned with what they need to do. Therefore, physicians should highlight important medication instructions and changes in the medication regimen, such as dose changes, deletions, and additions. It may be appropriate to arrange specialized counseling for patients who are prescribed high risk medications (e.g., coumadin, antiarrhythmics, immunosuppressants) or medications that require special administration skills (e.g., insulin, low molecular weight heparin, inhalers).3, 23
Informing patients about potential side effects and what to do if they occur can improve adherence and reduce unnecessary healthcare utilization after discharge. Such instructions should be very specific, including how to treat the symptoms, when to stop the medication, when to call the physician, and when to go to the emergency room.
Improving Physician Handoffs
Effective transfer of information from the hospitalist to the outpatient provider at discharge should include timely, accurate, and complete documentation of discharge medications.22 This was rated one of the most important components of the discharge summary in a survey of outpatient providers.40 Such information should include the dosage, frequency, route of administration, planned duration of use, and purpose of all medications. Reasons for discontinuing or changing any medications and indications for new drugs should be highlighted.22
To help ensure timely and consistent communication of discharge information, hospitals are advised to take several steps.22 First, confirm the name, address, phone number, fax, and/or email address for the primary care provider upon admission and include it in the discharge summary. Second, have a standard system in place for prompt delivery of patient information upon discharge. Third, on the day of discharge, alert the outpatient provider of the discharge and provide a reconciled list of medications with indications via email, fax, telephone, or linked electronic medical records. Providing the patient with the same list of medications can also help ensure this information will be delivered to the outpatient provider. Finally, send a detailed discharge summary to the outpatient provider within 7 days. Ensure that it includes the reconciled medication regimen with reasons for any changes and indications for medicines. Of course, other elements of the hospitalization must be communicated as well, and these issues are summarized in a recent systematic review.22 All of these steps tend to be performed as a one-way “information transfer,” but ideally, they would involve a two-way “information exchange.” Greater collaboration between inpatient and outpatient providers is thought to improve the effectiveness and continuity of care, as well as physician satisfaction.41
Providing Medical and Social Support
Often questions and problems aren’t obvious until the patient returns home. Calling the patient by telephone a few days after discharge offers patients the opportunity to clarify medication regimens, report unforeseen problems in filling their prescriptions, or question new symptoms which may be medication-related.42–44 Home visits or home health nurses for the elderly or disabled afford the opportunity to see firsthand how medications are being stored and taken at home, and to discard old medications.45, 46
Empowering patients and their families to participate in their post-discharge care is also important. In the Care Transitions Intervention, a “transition coach” helped patients and families take a more active role in their care and facilitate communication during the transition period after discharge. The intervention was effective in reducing rehospitalization rates at 30 days (8.3% vs. 11.9%, p<.05) and 90 days (16.7% vs. 22.5%, p<.05), and it also saved money ($2058 USD vs. $2546 USD, p<.05).47
Addressing Medication Costs
Getting familiar with the climate of medication costs within your patient population will help with the problem of rising healthcare costs. Moreover, by prescribing medications from the least expensive tier of your patient’s medication formulary when possible will reduce out-of-pocket costs. Using combination medications, when available, may not only cut the number of copays, but more importantly by decreasing the pill burden, may further enhance patient adherence.
Conclusion
Hospital discharges are high-risk periods for potential medication confusion and errors. A standardized team approach to discharge planning in tandem with effective and timely communication are the cornerstones of successful execution of this process. Ensuring patient comprehension of medication instructions should be an endpoint of discharge counseling, not just the act of delivering the information. Hospitalists partnering with outpatient physicians play a vital role in opening and maintaining 2-way communication to improve the exchange of information at points of transition and guarantee continuity of care.
Acknowledgements
The authors thank Ms. Hanah Geiser for her editorial assistance on an earlier version of this paper. Dr. Kripalani is supported by a K23 Career Development Award (HL 0770597).
References
- 1.Clarke A, Rosen R. Length of stay. How short should hospital care be? European Journal of Public Health. 2001;11(2):166–170. doi: 10.1093/eurpub/11.2.166. [DOI] [PubMed] [Google Scholar]
- 2.Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18:646–651. doi: 10.1046/j.1525-1497.2003.20722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 4.Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ Canadian Medical Association Journal. 2004;170(3):345–349. [PMC free article] [PubMed] [Google Scholar]
- 5.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. Adverse drug events occurring following hospital discharge. J Gen Intern Med. 2005;20:317–323. doi: 10.1111/j.1525-1497.2005.30390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andersen SE, Pedersen AB, Bach KF. Medication history on internal medicine wards: assessment of extra information collected from second drug interviews and GP lists. Pharmacoepidemiology & Drug Safety. 2003;12(6):491–498. doi: 10.1002/pds.835. [DOI] [PubMed] [Google Scholar]
- 7.Jacobson J. Ensuring continuity of care and accuracy of patients' medication history on hospital admission. Am J Health Syst Pharm. 2002;59(11):1054–1055. doi: 10.1093/ajhp/59.11.1054. [DOI] [PubMed] [Google Scholar]
- 8.Gleason KM, Groszek JM, Sullivan C, Rooney D, Barnard C, Noskin GA. Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients. Am J Health Syst Pharm. 2004;61(16):1689–1695. doi: 10.1093/ajhp/61.16.1689. [DOI] [PubMed] [Google Scholar]
- 9.Cornish PL, Knowles SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165(4):424–429. doi: 10.1001/archinte.165.4.424. [DOI] [PubMed] [Google Scholar]
- 10.Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ Canadian Medical Association Journal. 2005;173(5):510–515. doi: 10.1503/cmaj.045311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schachtner JM, Guharoy R, Medicis JJ, Newman N, Speizer R. Prevalence and cost savings of therapeutic interchange among U.S. hospitals. Am J Health Syst Pharm. 2002;59(6):529–533. doi: 10.1093/ajhp/59.6.529. [DOI] [PubMed] [Google Scholar]
- 12.Spees CM. Knowledge of medical terminology among clients and families. Image J Nurs Sch. 1991;23(4):225–229. doi: 10.1111/j.1547-5069.1991.tb00676.x. [DOI] [PubMed] [Google Scholar]
- 13.Spiro D, Heidrich F. Lay understanding of medical terminology. J Fam Pract. 1983;17(2):277–279. [PubMed] [Google Scholar]
- 14.Katz MG, Jacobson TA, Veledar E, Kripalani S. Patient literacy and question-asking behavior in the medical encounter: a mixed-methods analysis. J Gen Intern Med. 2007;22(6):782–786. doi: 10.1007/s11606-007-0184-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schillinger D, Piette J, Grumbach K, et al. Closing the loop. Physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163:83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 16.Calkins DR, Davis RB, Reiley P, et al. Patient-physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan. Arch Intern Med. 1997;157(9):1026–1030. [PubMed] [Google Scholar]
- 17.Makaryus AN, Friedman EA. Patients' understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80(8):991–994. doi: 10.4065/80.8.991. [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine. Health Literacy. A Prescription to End Confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 19.Williams MV, Davis TC, Parker RM, Weiss BD. The role of health literacy in patient-physician communication. Fam Med. 2002;34(5):383–389. [PubMed] [Google Scholar]
- 20.Kutner M, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy (NCES 2006-483) Washington, DC: U.S: Department of Education, National Center for Education Statistics; 2006. [Google Scholar]
- 21.Kiely DK, Bergmann MA, Murphy KM, Jones RN, Orav EJ, Marcantonio ER. Delirium among newly admitted postacute facility patients: prevalence, symptoms, and severity. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2003;58(5):M441–M445. doi: 10.1093/gerona/58.5.m441. [DOI] [PubMed] [Google Scholar]
- 22.Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 23.Gandhi TK, Weingart SN, Borus J, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348(16):1556–1564. doi: 10.1056/NEJMsa020703. [DOI] [PubMed] [Google Scholar]
- 24.Kripalani S, Price M, Vigil V, Epstein KR. Frequency and predictors of prescription-related issues after hospital discharge. Journal of Hospital Medicine. doi: 10.1002/jhm.248. (in press). [DOI] [PubMed] [Google Scholar]
- 25.The Boston Consulting Group. The hidden epidemic: finding a cure for unfilled prescriptions and missed doses. 2003 Available at http://www.bcg.com/publications/publications_splash.jsp.
- 26.Alexander GC, Casalino LP, Meltzer DO. Patient-physician communication about out-of-pocket costs. JAMA. 2003;290(7):953–958. doi: 10.1001/jama.290.7.953. [DOI] [PubMed] [Google Scholar]
- 27.Reichert S, Simon T, Halm EA. Physicians' attitudes about prescribing and knowledge of the costs of common medications. Arch Intern Med. 2000;160(18):2799–2803. doi: 10.1001/archinte.160.18.2799. [DOI] [PubMed] [Google Scholar]
- 28.Tarn DM, Paterniti DA, Heritage J, Hays RD, Kravitz RL, Wenger NS. Physician communication about the cost and acquisition of newly prescribed medications. Am J Manag Care. 2006;12(11):657–664. [PubMed] [Google Scholar]
- 29.Kaboli PJ, Hoth AB, McClimon BJ, Schnipper JL. Clinical pharmacists and inpatient medical care: a systematic review. Arch Intern Med. 2006;166(9):955–964. doi: 10.1001/archinte.166.9.955. [DOI] [PubMed] [Google Scholar]
- 30.Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166(5):565–571. doi: 10.1001/archinte.166.5.565. [DOI] [PubMed] [Google Scholar]
- 31.Pronovost P, Weast B, Schwarz M, et al. Medication reconciliation: a practical tool to reduce the risk of medication errors. J Crit Care. 2003;18(4):201–205. doi: 10.1016/j.jcrc.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 32.Arizona Acute Care Quality Initiative. [Accessed Dec 11, 2007];Medication reconciliation. Available at http://acute.hsag.com/medication_reconciliation.asp.
- 33.Institute for Healthcare Improvement. [Accessed Dec 11, 2007];Medication reconciliation form. Available at http://www.ihi.org/IHI/Topics/PatientSafety/MedicationSystems/Tools/BMHMemphisMedicationReconciliationForm.htm.
- 34.Society of Hospital Medicine. [Accessed Dec 11, 2007];Quality improvement tools. Available at http://www.hospitalmedicine.org/Content/NavigationMenu/QualityImprovement/QIClinicalTools/Quality_Improvement.htm.
- 35.Whittington J, Cohen H. OSF healthcare's journey in patient safety. Qual Manag Health Care. 2004;13(1):53–59. doi: 10.1097/00019514-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 36.Washington, DC: 2005. National Quality Forum. Improving patient safety through informed consent for patients with limited health literacy. [Google Scholar]
- 37.Shojania KG, Duncan BW, McDonald KM, Wachter RM, editors. Making Healthcare Safer: A Critical Analysis of Patient Safety Practices. Evidence Report No.43 from the Agency for Healthcare Research and Quality. AHRQ Publication No. 01-E058. 2001
- 38.Houts P, Bachrach R, Witmer J, Tringali C, Bucher J, Localio F. Using pictographs to enhance recall of spoken medical instructions. Patient Educ Couns. 1998;35:83–88. doi: 10.1016/s0738-3991(98)00065-2. [DOI] [PubMed] [Google Scholar]
- 39.Katz MG, Kripalani S, Weiss BD. Use of pictorial aids in medication instructions: a review of the literature. Am J Health Syst Pharm. 2006;63:2391–2397. doi: 10.2146/ajhp060162. [DOI] [PubMed] [Google Scholar]
- 40.Pantilat SZ, Lindenauer PK, Katz PP, Wachter RM. Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9B):15S–20S. doi: 10.1016/s0002-9343(01)00964-0. [DOI] [PubMed] [Google Scholar]
- 41.Lee RG, Garvin T. Moving from information transfer to information exchange in health and health care. Soc Sci Med. 2003;56(3):449–464. doi: 10.1016/s0277-9536(02)00045-x. [DOI] [PubMed] [Google Scholar]
- 42.Nelson JR. The importance of postdischarge telephone follow-up for hospitalists: a view from the trenches. Am J Med. 2001;111(9B):43S–44S. doi: 10.1016/s0002-9343(01)00970-6. [DOI] [PubMed] [Google Scholar]
- 43.Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Am J Med. 2001;111(9B):26S–30S. doi: 10.1016/s0002-9343(01)00966-4. [DOI] [PubMed] [Google Scholar]
- 44.Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database of Systematic Reviews. 2007:1. doi: 10.1002/14651858.CD004510.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stewart S, Pearson S. Uncovering a multitude of sins: medication management in the home post acute hospitalisation among the chronically ill. Aust N Z J Med. 1999;29(2):220–227. doi: 10.1111/j.1445-5994.1999.tb00687.x. [DOI] [PubMed] [Google Scholar]
- 46.Holland R, Lenaghan E, Harvey I, et al. Does home based medication review keep older people out of hospital? The HOMER randomised controlled trial. BMJ. 2005;330(7486):293. doi: 10.1136/bmj.38338.674583.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Coleman EA, Parry C, Chalmers S, Min S. The Care Transitions Intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]