Introduction
Ovarian cysts frequently occur in women of reproductive age. Fertility sparing surgery should be reserved for women desirous of future pregnancy. We present a case report of a young woman who resumed fertility following unilateral salpingo oophorectomy and contralateral ovarian cystectomy with an over all small ovarian reserve left for ovulation.
Case Report
A 20 year old unmarried girl was admitted to our hospital with chief complaints of pain in lower abdomen associated with vomiting for 1 day.
Past History
Two months prior to admission she had heaviness in the lower abdomen for which she took treatment from a local doctor and got an ultrasound done. It showed a mass 6.6 × 6.5 × 6.1 cm anterior to the uterus with hyper and hypo echogenic areas with an area of dense echogenicity. Both the ovaries could not be visualized separately. No free fluid in the peritoneal cavity could be appreciated.
Patient was advised surgery but the patient refused.
Menstrual History
She had attained menarche at the age of 13 years and had regular cycles, with moderate amount of flow. There had been no associated dysmenorrhea.
Family History
Family history was of no significance.
On examination
Patient was conscious, well oriented in time, space and person. Mild pallor was present. There was no edema, cyanosis, jaundice, clubbing or lymphadenopathy.
JVP was normal, trachea central and thyroid not enlarged. Her pulse rate was 88/min blood pressure 110/70 mmHg, temperature 99 ºF and respiratory rate was 20/min. On systemic examination her CVS and RS were normal.
On abdominal examination, it was soft and no distension was felt. Tenderness was present in the right lumbar and iliac regions but there was no guarding or rigidity. No mass was palpable. Bowel sounds were present.
A provisional diagnosis of twisted ovarian cyst was made.
A diagnostic laparoscopy was planned, following investigation.
Laparoscopic Findings
On laparoscopy, there were bilateral ovarian masses, gangrenous on the right side hence, decision for laparotomy was taken.
Operative Findings
Uterus was nulliparous size. Right ovary was gangrenous and measured approximately 8 × 6 × 5 cm. Left ovary was cystic and enlarged to about 7 × 7 × 6 cm. Right salpingo-ovariotomy and left sided ovarian cystectomy was done leaving behind a very small ovarian tissue (approximately 0.8 × 0.5 cm). Post operative period was uneventful.
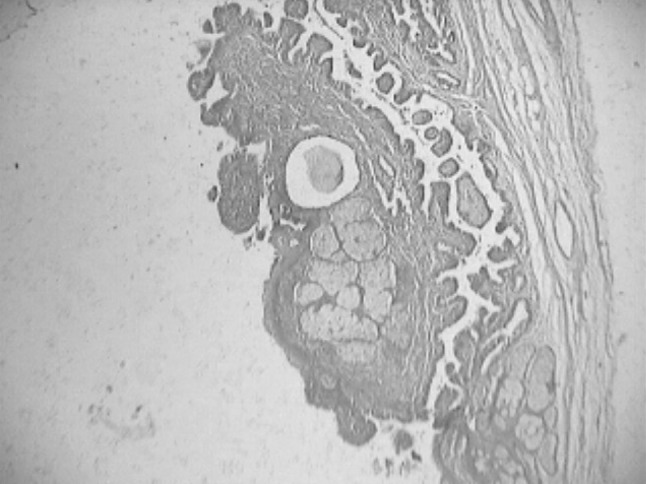
Histopathology revealed right ovary with follicular and corpus luteal cyst as shown in Fig. 1. Left ovarian cyst was benign cystic teratoma as shown in Fig. 2.
Fig. 1.

Right ovary—follicular cyst & corpus luteal cyst
Fig. 2.
Left ovary—benign cystic teratoma
Follow Up
On follow up, patient got married after 10 months. She reported again after 4 months with 6 weeks amenorrhea. Her first and second trimesters were uneventful. At 36 weeks she reported with premature rupture of membranes. She developed fetal distress. Hence a lower segment cesarean section was done. A live male baby weighing 2.75 kg was extracted. Apgar score was 8/10 and 9/10 at 1 and 5 min respectively.
Post operative period was uneventful.
Discussion
Ovarian cysts in reproductive age group may be functional or non functional. Functional cysts usually resolve spontaneously. Common non functional cysts are cystadenomas, endometriomas, and dermoid cysts of germ cell origin. Dermoid cysts make up to 10–15 % of all ovarian tumors and are bilateral in 12 % of cases. They are prone to undergo torsion.
In early diagnosis of torsion, the ovary can be managed by detorsion whereas a gangrenous adnexa needs removal.
Ding and Chen [1] reported conservative laparoscopic management of torsion of ovarian teratoma in a young woman, by performing detorsion followed by cystectomy.
For young women with ovarian cysts, conservative treatment to shell out the cyst and preserve functional ovarian tissue should be performed. Pelvic laparoscopy is the surgical approach of choice for the treatment of non functional benign ovarian cysts [2].
Post cystectomy restoration of the normal appearing anatomy is the most logical approach for creating maximal ovarian surface to facilitate ovarian pick up.
Van der Watt [3] reported concern over ovarian surgery of 36 young women operated for an ovarian cyst. 45 % were noted to be infertile.
Principles of surgery must be re emphasized to reduce the rate of post operative adhesion formation and subsequent subfertility.
Kentaro et al. [4] studied the post operative function of residual ovaries in women who underwent ovarian cystectomy. They found that number of developing follicles naturally and after induction of ovulation was significantly less in diseased ovary. Hence the need for preventing posts operative adhesion formation in the diseased ovary is necessary.
Conclusion
Retaining a small amount of normal tissue in a diseased ovary can save the obstetrical career of a patient.
References
- 1.Ding DC, Chen SS. Conservative laparoscopic management of ovarian teratoma torsion in young woman. J Chin Med Assoc. 2005;68:37–39. doi: 10.1016/S1726-4901(09)70130-3. [DOI] [PubMed] [Google Scholar]
- 2.Raiga J, Djafer R, Benort B, et al. Management of ovarian cysts. J Chir (Paris) 2006;143:278–284. doi: 10.1016/S0021-7697(06)73692-4. [DOI] [PubMed] [Google Scholar]
- 3.Van der Watt J. The mutilated ovary syndrome. S Afr Med J. 1970;44:687. [PubMed] [Google Scholar]
- 4.Kentaro T, Tomoya O, Haruchi KK, et al. Influence of ovarian cystectomy on the ovulatory function of the residual ovary. Eur J Obstet Gynecol Reprod Biol. 2005;121:191–194. doi: 10.1016/j.ejogrb.2005.01.011. [DOI] [PubMed] [Google Scholar]


