Abstract
Purpose
Levodopa is the most effective anti-Parkinsonian agent. It has also been known to exhibit analgesic properties in laboratory and clinical settings. However, studies evaluating its effects on neuropathic pain are limited. The aim of the present study was to examine the anti-allodynic effects of levodopa in neuropathic rats.
Materials and Methods
Sprague-Dawley male rats underwent the surgical procedure for L5 and L6 spinal nerves ligation. Sixty neuropathic rats were randomly divided into 6 groups for the oral administration of distilled water and levodopa at 10, 30, 50, 70, and 100 mg/kg, respectively. We co-administered carbidopa with levodopa to prevent peripheral synthesis of dopamine from levodopa, and observed tactile, cold, and heat allodynia pre-administration, and at 15, 30, 60, 90, 120, 150, 180, and 240 min after drug administration. We also measured locomotor function of neuropathic rats using rotarod test to examine whether levodopa caused side effects or not.
Results
Distilled water group didn't show any difference in all allodynia. For the levodopa groups (10-100 mg/kg), tactile and heat withdrawal thresholds were increased, and cold withdrawal frequency was decreased dose-dependently (p<0.01). In addition, levodopa induced biphasic analgesia. Different dosage of levodopa did not impact on the rotarod time (p>0.05).
Conclusion
Levodopa reversed tactile, cold and heat allodynia in neuropathic rat without any side effects.
Keywords: Allodynia, levodopa, neuropathy, pain
INTRODUCTION
In the clinical setting, treatment of neuropathic pain remains difficult. Many mechanisms for causing and maintaining neuropathic pain have been postulated. However, no single mechanism has been clearly defined. Non-steroidal analgesics, anti-depressants, calcium channel blockers, alpha(2)-delta ligands, lidocaine, opioids, and anti-epileptic medications have been used for the management of neuropathic pain with limited success.1
Levodopa is the precursor to the neurotransmitter dopamine. Exogenously administered levodopa increases dopaminergic concentrations. Levodopa has traditionally been used to treat dopamine-deficiency conditions, such as Parkinson's disease2 and restless legs syndrome.3 Although levodopa is not a conventional analgesic, studies using levodopa have been performed for the treatment of chronic pain conditions secondary to bone metastasis,4 painful diabetic polyneuropathy5 and herpes zoster pain.6 However, the use of levodopa for painful neuropathy simply hasn't been widely considered on the clinical side. Levodopa has been shown to have anti-nociceptive properties in animal studies,7,8 acting at the level of the spinal cord or the brain via the dopaminergic receptors. Animal studies on the analgesic activity of levodopa, in the setting of chronic pain, have been limited and inconclusive.9,10 Therefore, the aim of this study was to investigate, in a rat model, the anti-allodynic effects of levodopa to determine if levodopa should be further investigated as a novel treatment modality in humans.
MATERIALS AND METHODS
Animals
The study was approved by our Institutional Animal Care and Use Committee at the Catholic University of Korea. The protocol used in this study was modified from our groups' previous studies for testing the analgesic properties of oxycarbazepine and pregabalin in a rat model of neuropathic pain.11,12 Sprague-Dawley rats (male 100-150 g) were housed up to 3-4 animals in plastic cages and maintained on a 12 hours light/dark cycle. Food and water were available freely.
Spinal nerve ligation
Left L5 and L6 spinal nerves ligation procedure was used, as described by Kim and Chung.13 After 7-day recovery of surgery, rats that exhibited tactile allodynia to von Frey hairs (Stoelting Co., Wood Dale, IL, USA) with an applied bending force (<4 g), were employed for the experiments. Rats that showed any complication or those which didn't show tactile allodynia were discarded.
Drug administration
Levodopa+carbidopa (SINEMET®, MSD-Korea Inc., Seoul, Korea) was dissolved in distilled water. Neuropathic rats were randomly assigned to 6 groups of increasing oral administration of levodopa+carbidopa. Each group received either distilled water or levodopa and carbidopa at 10/2.5, 30/7.5, 50/12.5, 70/17.5 and 100/25 mg/kg (n=10 per group).
Behavioral tests
Testing was performed at pre-defined periods (10:00 am-5:00 pm) to avoid circadian rhythm errors. The tactile allodynia was evaluated with von Frey hairs (0.6-26.0 g) using up-down method.14 After rats were placed on a metal mesh covered with a plastic dome (8×8×18 cm), the third metatarsal bone area of the injured hind paw was stimulated with von Frey hairs at 3-4 s intervals. We recorded the minimum gram of von Frey hair that initiated nocifencive responses. The cut-off threshold was 26.0 g. Cold allodynia was examined as the % response frequency of paw withdrawals divided by total 5 trials.15 It was measured as the number of paw withdrawal responses after the application of cold stimuli (100% acetone) to the plantar surface of the injured hind paw. The heat allodynia was expressed as noxious heat threshold using a hot plate (IITC Life Science, Woodland Hills, CA, USA).16 After habituation, the rats were placed onto the plate, which was then heated up at a rate of 12℃/min from a starting temperature of 30℃ until the animal showed nocifensive behavior. The corresponding plate temperature was considered as the noxious heat threshold. Rotarod (Ugo Basile, Comerio-Varese, Italy) testing was executed for locomotor function evaluation. All behavioral tests were performed prior to oral administration, and also at 15, 30, 60, 90, 120, 150, 180, and 240 min following administration. Positive pain responses for all tests included paw withdrawal responses such as lifting, shaking and licking behaviors.
Statistical analysis
Results are expressed as mean±standard error (SE). Two ways analysis of variance (ANOVA) was used to determine general difference, depending on the treatment group and time. This was followed by post hoc Bonferroni multiple comparisons' test. A percent of the maximal possible effect (%MPE) was used for dose-response curves. It was analyzed by 1-way ANOVA followed by post hoc Tukey's multiple comparisons' test. A %MPE was calculated as follows: 1) for mechanical allodynia=(treatment threshold-baseline threshold)/(26.0 g-baseline threshold)×100, and 2) for cold and heat allodynia=(baseline frequency-treatment frequency)/(baseline frequency)×100. A p value of <0.05 was considered significant. All analysis was executed by GraphPad Prism 5.0 (GraphPad Software Inc., San Diego, CA, USA).
RESULTS
Tactile allodynia
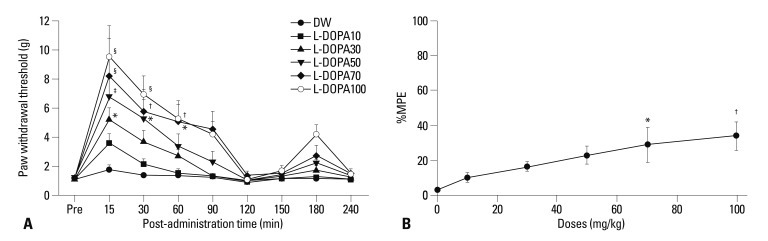
All rats showed mechanical allodynia after spinal nerve ligation surgery. In the vehicle group, the tactile thresholds were 1.1±0.3, 1.8±0.9, 1.4±0.4, 1.3±0.3, 1.2±0.2, 1.2±0.3, 1.1±0.3, 1.1±0.3, and 1.1±0.3 g prior to distilled water administration and at 15, 30, 60, 90, 120, 150, 180, and 240 min after distilled water administration, respectively. The tactile thresholds increased at 15 min for 30 mg/kg, from 15 to 30 min for 50 mg/kg, from 15 to 60 min for 70 mg/kg and 100 mg/kg, as compared to the vehicle group (p<0.001) (Fig. 1A). Oral administration of levodopa reduced tactile allodynia in a dose-dependent fashion (p=0.006) (Fig. 1B). In general, the figures showed a biphasic analgesia pattern. Therefore, we devided Phase I and Phase II by 120 min. The Phase I ED50 was calculated to be 130.3 mg/kg [95% confidence interval (CI): 90.92 to 169.6], whereas the Phase II ED50 was not acquired.
Fig. 1.
(A) Time course of paw withdrawal threshold to tactile stimuli in the neuropathic pain model. The withdrawal threshold was measured before (Pre) and after oral administration of distilled water (DW), levodopa 10 mg/kg (L-DOPA10), levodopa 30 mg/kg (L-DOPA30), levodopa 50 mg/kg (L-DOPA50), levodopa 70 mg/kg (L-DOPA70), and levodopa 100 mg/kg (L-DOPA100). The results are expressed as mean±SE (n=10 in each group). *p<0.05, †p<0.01, ‡p<0.001, §p<0.0001 significantly different from the DW group. (B) Dose-response curve from the peak effects of percentage maximal possible effect (%MPE) for tactile anti-allodynia in the levodopa groups. This shows a dose-dependent tactile anti-allodynic effect. Each line represents mean±SE for 10 rats. Doses (mg/kg) are represented logarithmically on the x-axis and peak %MPE is represented on the y-axis. *p<0.05 vs. DW, †p<0.01 vs. DW.
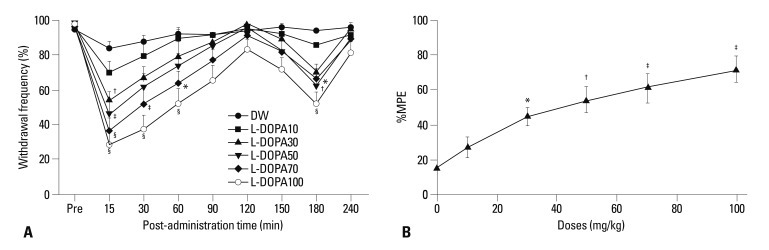
Cold allodynia
After ligation surgery, all rats showed cold withdrawal frequencies of 94% or more. Oral administration of levodopa decreased the cold withdrawal frequency at 15 min for 30 mg/kg, at 15 min and at 180 min for 50 mg/kg, from 15 to 60 min and at 180 min for 70 mg/kg, from 15 to 60 min and at 180 min for 100 mg/kg, as compared to the vehicle group (p<0.001) (Fig. 2A). The linear regression curve shows that levodopa reduced cold allodynia in a dose-dependent manner (p<0.001) (Fig. 2B). The ED50 was calculated to be 49.2 mg/kg (95% CI: 38.5 to 59.8).
Fig. 2.
(A) Time course of paw withdrawal frequency to cold stimuli. The response frequencies were measured before (Pre) and after oral administration of distilled water (DW), levodopa 10 mg/kg (L-DOPA10), levodopa 30 mg/kg (L-DOPA30), levodopa 50 mg/kg (L-DOPA50), levodopa 70 mg/kg (L-DOPA70), and levodopa 100 mg/kg (L-DOPA100). The results are expressed as mean±SE (n=10 in each group). *p<0.05, †p<0.01, ‡p<0.001, §p<0.0001 significantly different from the DW group. (B) Dose-response curve from the peak effects of percentage maximal possible effect (%MPE) for cold anti-allodynia in the levodopa groups. This shows a dose-dependent cold anti-allodynic effect. Each line represents mean±SE for 10 rats. Doses (mg/kg) are represented logarithmically on the x-axis and peak %MPE is represented on the y-axis. *p<0.05 vs. DW, †p<0.01 vs. DW, ‡p<0.001 vs. DW.
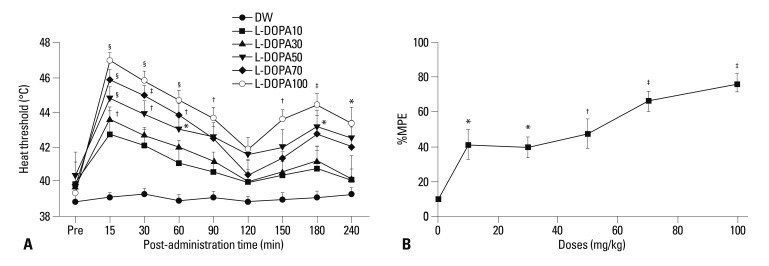
Heat allodynia
All rats showed a baseline heat threshold of 39.5±2.3℃. Oral administration of levodopa increased the heat thresholds at 15 min for 30 mg/kg, from 15 to 60 min and at 180 min for 50 mg/kg, from 15 to 60 min for 70 mg/kg, from 15 to 90 min and from 150 to 240 min for 100 mg/kg (p<0.001) (Fig. 3A). The linear regression curve shows that levodopa decreased heat allodynia dose-dependently (p<0.001) (Fig. 3B). The ED50 was calculated to be 49.3 mg/kg (95% CI: 38.5 to 60.2).
Fig. 3.
(A) Time course of paw withdrawal heat threshold. The heat threshold was measured before (Pre) and after oral administration of distilled water (DW), levodopa 10 mg/kg (L-DOPA10), levodopa 30 mg/kg (L-DOPA30), levodopa 50 mg/kg (L-DOPA50), levodopa 70 mg/kg (L-DOPA70), and levodopa 100 mg/kg (L-DOPA100). The results are expressed as mean±SE (n=6 in each group). *p<0.05, †p<0.01, ‡p<0.001, §p<0.0001 significantly different from the DW group. (B) Dose-response curves from the peak effects of percentage maximal possible effect (%MPE) for heat anti-allodynia in the levodopa groups. These curves show a dose-dependent heat anti-allodynic effect. Each line represents mean±SE for 6 rats. Doses (mg/kg) are represented logarithmically on the x-axis and peak %MPE is represented on the y-axis. *p<0.05 vs. DW, †p<0.01 vs. DW, ‡p<0.001 vs. DW.
Rotarod performance
Treatment with 10-100 mg/kg of levodopa did not significantly decrease the rotarod testing time. Rotarod performance was 147.7±0.9, 132.1±12.1, 136.1±8.8, 137.7±9.8, 141.0±5.6, 144.1±3.3, 148.3±1.2 and 150.0±0.0 at pre-levodopa administration and at 15, 30, 60, 90, 120, 150, and 180 min after 100 mg/kg levodopa administration, respectively. The rotarod time appeared to be slightly decreased 15 min after administration of 100 mg/kg levodopa. However, this time was not significantly different from the cut off time (150.0 sec, p>0.05).
DISCUSSION
The present study showed that oral administration of levodopa dose-dependently decreased tactile, cold, and heat allodynia in neuropathic rats. In addition, levodopa induced a biphasic analgesia pattern.
Three previous studies have shown the analgesia of levodopa in animal models.7,8,10 However, only one study investigated neuropathic pain. Cobacho, et al.10 reported that intraperitoneal and intrathecal injection of levodopa reduced mechanical and cold allodynia in mono-neuropathic rat models. However, they executed a sciatic nerve ligation according to the method originally developed by Bennett and Xie,17 and assessed the tactile and cold allodynia pre-administration, and at 20, 90, 180 min and 24 hours after intraperitoneal injection of a single dose of levodopa (200 mg/kg). In contrast to the methods used in the Cobacho, et al.10 study, we performed the spinal nerve ligation developed by Kim and Chung,13 and observed the tactile, cold, and heat allodynia pre-administration, and at 15, 30, 60, 90, 120, 150, 180, and 240 min after oral administration of 10, 30, 50, 70, and 100 mg/kg of levodopa. Shimizu, et al.8 reported that intrathecal injection of levodopa reduced substance P-evoked nocifensive behaviors, however, they utilized substance P mice models and observed licking and scratching behaviors. Compared with Shimizu, et al.8 study, we administered levodopa orally, not intrathecally, in spinal nerve-ligated rat models and observed tactile, cold, and heat allodynia. Paalzow7 reported that intraperitoneal injection of levodopa induced analgesic effects when they applied electrical stimulation to the tail of rats. However, normal rats were used in the study and allodynia was not assessed. They evaluated vocalization only. Therefore, their results may not be applicable for the treatment of neuropathic pain.
Levodopa crosses the blood-brain barrier, whereas dopamine itself cannot. Outside the central nervous system, levodopa is also converted into dopamine within the peripheral nervous system. The resulting hyperdopaminergia may cause adverse side effects secondary to sole levodopa administration. In order to prevent the peripheral synthesis of dopamine from levodopa, we co-administered a peripheral DOPA decarboxylase inhibitor, carbidopa, along with levodopa.
It remains unclear how levodopa has an analgesic effect on neuropathic pain. However, levodopa's analgesic effects may be produced by dopamine, a metabolite of levodopa, since dopamine antagonist completely abolished the anti-nociceptive action of levodopa.8
Spinal cord dopaminergic termination originates in the A11 periventricular hypothalamic group neuron.18,19 Despite small number, A11 neuron projects broadly into all spinal lamina except substantia gelatinosa.20 There is a dopaminergic descending system from the A10 and A11 to the spinal dorsal horn in mice.21 As such, stimulation of A10 and A11 neurons inhibits nocifensive response of the spinal cord.22
Dopaminergic terminations of the spinal cord have also been shown to be involved in nociceptive transmission.22-25 Especially, the D2 receptor is distributed in the spinal dorsal horn, whose primary sensory afferent fibers terminate in.26 Anti-allodynic effects of levodopa were suppressed by concurrent intrathecal administration of D2 receptor antagonist sulpiride.10 As such, dopamine may affect the primary sensory afferent system via the D2 receptor.
Therefore, oral levodopa in the present study may have analgesic effect via the spinal and supraspinal dopaminergic systems. As demonstrated in the present study, the dopaminergic enhancement in the spinal cord was sufficient to suppress ascending pain, including non-nociceptive, neuropathic pain.10,22-25 It is also known that increased dopaminergic activity in the encephalic regions modulates pain sensitivity.27-32
In this study, we observed the absence of analgesia around 2 hours after oral levodopa administration in each allodynic response. This observation is likely to be secondary to levodopa-induced hyperalgesia, since high dose of intraperitoneal levodopa has been shown to induce initial anti-nociception and then hyperalgesia after 2 hours.7 In addition, Shimizu, et al.33 reported that levodopa-evoked hyperalgesia occurred after conversion of levodopa to dopamine. Dopamine contents in the spinal cord increased 1 min after levodopa administration, expressing about 100 times more than control, and then decreased to beaseline after 1 hour.33 This suggested that overload of dopamine which was converted from levodopa temporarily disabled the dopaminergic inhibitory system for pain and was involved in hyperalgesia.33
The side effects of levodopa include dyskinesia,34 sudden onset of sleep,35 and psychosis.36 In our rat pilot study, 200 mg/kg of levodopa caused rupture of a capillary in the eye of a rat. Some rats crouched without moving, and some rats showed hair loss, increased locomotion, and exhibited abnormal licking behaviors. However, no altered behavior was observed when 10-100 mg/kg of levodopa were administered. Moreover, systemic levodopa, at all dose levels administered did not affect rat's rotarod performance. Consequently, the anti-allodynic effect of levodopa at 10-100 mg/kg is not thought to be due to the effect of sedation, ataxia or altered locomotion.
In conclusion, orally administered levodopa attenuated tactile, cold and heat allodynia exhibited by spinal nerve ligated rats. Sedation and motor disturbance were not observed at any of the dose levels used in this study. In addition, levodopa may induce a biphasic pattern of analgesia in rats suffering from neuropathic pain. Therefore, further studies may be required to determine optimal dose and time interval to avoid hyperalgesia. Human studies will also be required to determine if the results in rats are applicable to humans.
ACKNOWLEDGEMENTS
This research was supported by Seoul St. Mary's Clinical Medicine Research Program year of 2009 through the Catholic University of Korea. We thank Young Eun Choi for her technical assistance.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Park HJ, Moon DE. Pharmacologic management of chronic pain. Korean J Pain. 2010;23:99–108. doi: 10.3344/kjp.2010.23.2.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mercuri NB, Bernardi G. The 'magic' of L-dopa: why is it the gold standard Parkinson's disease therapy? Trends Pharmacol Sci. 2005;26:341–344. doi: 10.1016/j.tips.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 3.Conti CF, de Oliveira MM, Andriolo RB, Saconato H, Atallah AN, Valbuza JS, et al. Levodopa for idiopathic restless legs syndrome: evidence-based review. Mov Disord. 2007;22:1943–1951. doi: 10.1002/mds.21662. [DOI] [PubMed] [Google Scholar]
- 4.Nixon DW. Letter: use of L-dopa to relieve pain from bone metastases. N Engl J Med. 1975;292:647. [PubMed] [Google Scholar]
- 5.Ertas M, Sagduyu A, Arac N, Uludag B, Ertekin C. Use of levodopa to relieve pain from painful symmetrical diabetic polyneuropathy. Pain. 1998;75:257–259. doi: 10.1016/s0304-3959(98)00003-7. [DOI] [PubMed] [Google Scholar]
- 6.Kernbaum S, Hauchecorne J. Administration of levodopa for relief of herpes zoster pain. JAMA. 1981;246:132–134. [PubMed] [Google Scholar]
- 7.Paalzow GH. L-dopa induces opposing effects on pain in intact rats: (-)-sulpiride, SCH 23390 or alpha-methyl-DL-p-tyrosine methylester hydrochloride reveals profound hyperalgesia in large antinociceptive doses. J Pharmacol Exp Ther. 1992;263:470–479. [PubMed] [Google Scholar]
- 8.Shimizu T, Iwata S, Morioka H, Masuyama T, Fukuda T, Nomoto M. Antinociceptive mechanism of L-DOPA. Pain. 2004;110:246–249. doi: 10.1016/j.pain.2004.03.038. [DOI] [PubMed] [Google Scholar]
- 9.Sindrup SH, Jensen TS. Efficacy of pharmacological treatments of neuropathic pain: an update and effect related to mechanism of drug action. Pain. 1999;83:389–400. doi: 10.1016/S0304-3959(99)00154-2. [DOI] [PubMed] [Google Scholar]
- 10.Cobacho N, De la Calle JL, González-Escalada JR, Paíno CL. Levodopa analgesia in experimental neuropathic pain. Brain Res Bull. 2010;83:304–309. doi: 10.1016/j.brainresbull.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 11.Thompson EB, Galysh FT. Quantitative assessment of anesthetic-induced cardiac sensitization to epinephrine. Anesth Analg. 1973;52:800–806. [PubMed] [Google Scholar]
- 12.Park HJ, Joo HS, Chang HW, Lee JY, Hong SH, Lee Y, et al. Attenuation of neuropathy-induced allodynia following intraplantar injection of pregabalin. Can J Anaesth. 2010;57:664–671. doi: 10.1007/s12630-010-9318-0. [DOI] [PubMed] [Google Scholar]
- 13.Kim SH, Chung JM. An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain. 1992;50:355–363. doi: 10.1016/0304-3959(92)90041-9. [DOI] [PubMed] [Google Scholar]
- 14.Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods. 1994;53:55–63. doi: 10.1016/0165-0270(94)90144-9. [DOI] [PubMed] [Google Scholar]
- 15.Choi Y, Yoon YW, Na HS, Kim SH, Chung JM. Behavioral signs of ongoing pain and cold allodynia in a rat model of neuropathic pain. Pain. 1994;59:369–376. doi: 10.1016/0304-3959(94)90023-X. [DOI] [PubMed] [Google Scholar]
- 16.Almási R, Pethö G, Bölcskei K, Szolcsányi J. Effect of resiniferatoxin on the noxious heat threshold temperature in the rat: a novel heat allodynia model sensitive to analgesics. Br J Pharmacol. 2003;139:49–58. doi: 10.1038/sj.bjp.0705234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bennett GJ, Xie YK. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain. 1988;33:87–107. doi: 10.1016/0304-3959(88)90209-6. [DOI] [PubMed] [Google Scholar]
- 18.Björklund A, Skagerberg G. Evidence for a major spinal cord projection from the diencephalic A11 dopamine cell group in the rat using transmitter-specific fluorescent retrograde tracing. Brain Res. 1979;177:170–175. doi: 10.1016/0006-8993(79)90927-2. [DOI] [PubMed] [Google Scholar]
- 19.Skagerberg G, Lindvall O. Organization of diencephalic dopamine neurones projecting to the spinal cord in the rat. Brain Res. 1985;342:340–351. doi: 10.1016/0006-8993(85)91134-5. [DOI] [PubMed] [Google Scholar]
- 20.Holstege JC, Van Dijken H, Buijs RM, Goedknegt H, Gosens T, Bongers CM. Distribution of dopamine immunoreactivity in the rat, cat and monkey spinal cord. J Comp Neurol. 1996;376:631–652. doi: 10.1002/(SICI)1096-9861(19961223)376:4<631::AID-CNE10>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 21.Qu S, Ondo WG, Zhang X, Xie WJ, Pan TH, Le WD. Projections of diencephalic dopamine neurons into the spinal cord in mice. Exp Brain Res. 2006;168:152–156. doi: 10.1007/s00221-005-0075-1. [DOI] [PubMed] [Google Scholar]
- 22.Fleetwood-Walker SM, Hope PJ, Mitchell R. Antinociceptive actions of descending dopaminergic tracts on cat and rat dorsal horn somatosensory neurones. J Physiol. 1988;399:335–348. doi: 10.1113/jphysiol.1988.sp017084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao X, Zhang Y, Wu G. Effects of dopaminergic agents on carrageenan hyperalgesia after intrathecal administration to rats. Eur J Pharmacol. 2001;418:73–77. doi: 10.1016/s0014-2999(01)00930-x. [DOI] [PubMed] [Google Scholar]
- 24.Jensen TS, Yaksh TL. Effects of an intrathecal dopamine agonist, apomorphine, on thermal and chemical evoked noxious responses in rats. Brain Res. 1984;296:285–293. doi: 10.1016/0006-8993(84)90064-7. [DOI] [PubMed] [Google Scholar]
- 25.Tamae A, Nakatsuka T, Koga K, Kato G, Furue H, Katafuchi T, et al. Direct inhibition of substantia gelatinosa neurones in the rat spinal cord by activation of dopamine D2-like receptors. J Physiol. 2005;568(Pt 1):243–253. doi: 10.1113/jphysiol.2005.091843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yokoyama C, Okamura H, Nakajima T, Taguchi J, Ibata Y. Autoradiographic distribution of [3H]YM-09151-2, a high-affinity and selective antagonist ligand for the dopamine D2 receptor group, in the rat brain and spinal cord. J Comp Neurol. 1994;344:121–136. doi: 10.1002/cne.903440109. [DOI] [PubMed] [Google Scholar]
- 27.Ansah OB, Leite-Almeida H, Wei H, Pertovaara A. Striatal dopamine D2 receptors attenuate neuropathic hypersensitivity in the rat. Exp Neurol. 2007;205:536–546. doi: 10.1016/j.expneurol.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 28.Magnusson JE, Fisher K. The involvement of dopamine in nociception: the role of D(1) and D(2) receptors in the dorsolateral striatum. Brain Res. 2000;855:260–266. doi: 10.1016/s0006-8993(99)02396-3. [DOI] [PubMed] [Google Scholar]
- 29.Michael-Titus A, Bousselmame R, Costentin J. Stimulation of dopamine D2 receptors induces an analgesia involving an opioidergic but non enkephalinergic link. Eur J Pharmacol. 1990;187:201–207. doi: 10.1016/0014-2999(90)90007-s. [DOI] [PubMed] [Google Scholar]
- 30.Pertovaara A, Wei H. Dual influence of the striatum on neuropathic hypersensitivity. Pain. 2008;137:50–59. doi: 10.1016/j.pain.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 31.Sheng HY, Qu CL, Huo FQ, Du JQ, Tang JS. D2-like but not D1-like dopamine receptors are involved in the ventrolateral orbital cortex-induced antinociception: a GABAergic modulation mechanism. Exp Neurol. 2009;215:128–134. doi: 10.1016/j.expneurol.2008.09.018. [DOI] [PubMed] [Google Scholar]
- 32.Taylor BK, Joshi C, Uppal H. Stimulation of dopamine D2 receptors in the nucleus accumbens inhibits inflammatory pain. Brain Res. 2003;987:135–143. doi: 10.1016/s0006-8993(03)03318-3. [DOI] [PubMed] [Google Scholar]
- 33.Shimizu T, Iwata S, Miyata A, Fukuda T, Nomoto M. Delayed L-DOPA-induced hyperalgesia. Pharmacol Biochem Behav. 2006;85:643–647. doi: 10.1016/j.pbb.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 34.Calabresi P, Di Filippo M, Ghiglieri V, Tambasco N, Picconi B. Levodopa-induced dyskinesias in patients with Parkinson's disease: filling the bench-to-bedside gap. Lancet Neurol. 2010;9:1106–1117. doi: 10.1016/S1474-4422(10)70218-0. [DOI] [PubMed] [Google Scholar]
- 35.Körner Y, Meindorfner C, Möller JC, Stiasny-Kolster K, Haja D, Cassel W, et al. Predictors of sudden onset of sleep in Parkinson's disease. Mov Disord. 2004;19:1298–1305. doi: 10.1002/mds.20163. [DOI] [PubMed] [Google Scholar]
- 36.Moskovitz C, Moses H, 3rd, Klawans HL. Levodopa-induced psychosis: a kindling phenomenon. Am J Psychiatry. 1978;135:669–675. doi: 10.1176/ajp.135.6.669. [DOI] [PubMed] [Google Scholar]