Abstract
Postamputation pain (PAP) is highly prevalent after limb amputation but remains an extremely challenging pain condition to treat. A large part of its intractability stems from the myriad pathophysiological mechanisms. A state-of-art understanding of the pathophysiologic basis underlying postamputation phenomena can be broadly categorized in terms of supraspinal, spinal, and peripheral mechanisms. Supraspinal mechanisms involve somatosensory cortical reorganization of the area representing the deafferentated limb and are predominant in phantom limb pain and phantom sensations. Spinal reorganization in the dorsal horn occurs after deafferentataion from a peripheral nerve injury. Peripherally, axonal nerve damage initiates inflammation, regenerative sprouting, and increased “ectopic” afferent input which is thought by many to be the predominant mechanism involved in residual limb pain or neuroma pain, but may also contribute to phantom phenomena. To optimize treatment outcomes, therapy should be individually tailored and mechanism based. Treatment modalities include injection therapy, pharmacotherapy, complementary and alternative therapy, surgical therapy, and interventions aimed at prevention. Unfortunately, there is a lack of high quality clinical trials to support most of these treatments. Most of the randomized controlled trials in PAP have evaluated medications, with a trend for short-term Efficacy noted for ketamine and opioids. Evidence for peripheral injection therapy with botulinum toxin and pulsed radiofrequency for residual limb pain is limited to very small trials and case series. Mirror therapy is a safe and cost-effective alternative treatment modality for PAP. Neuromodulation using implanted motor cortex stimulation has shown a trend toward effectiveness for refractory phantom limb pain, though the evidence is largely anecdotal. Studies that aim to prevent PA P using epidural and perineural catheters have yielded inconsistent results, though there may be some benefit for epidural prevention when the infusions are started more than 24 hours preoperatively and compared with nonoptimized alternatives. Further investigation into the mechanisms responsible for and the factors associated with the development of PAP is needed to provide an evidence-based foundation to guide current and future treatment approaches.
Keywords: phantom pain, stump pain, residual limb pain
Historical aspects
The word amputation can trace its origin to the Latin term “amputatio,” meaning “to cut around.” Yet, amputations have been practiced since the dawn of mankind. Historical and archaeological records demonstrate that purposeful amputations have been performed since Neolithic times, dating back at least 45,000 years.1 This evidence consists of stone knives and saws found with the skeletal remains of amputated stumps.
It is likely that postamputation pain (PAP) has plagued humans for countless millennia. However, our understanding of PAP has significantly evolved over the centuries, with the full impact beginning to unravel only recently. Perhaps the major advances in amputation care and our understanding of their sequelae have occurred during war. For hundreds of years, horrific limb injuries have been the result of man’s fascination with armed conflict. Reporting on 86 civil war amputees, the renowned physician Weir Mitchell coined the term “phantom pain,” recording an incidence as high as 90%.2
But for the most part, the concept of PAP was largely ignored by the mainstream medical establishment, with post-World War II prevalence rates consistently estimated at less than 5%.3,4 Moreover, many of these patients were ostracized, and their symptoms attributed to either psychopathology or secondary gain.4
Today, the management of amputations engenders public attention and research dollars far in excess of its epidemiological burden. PAP is widely considered to be one of the most challenging among all pain conditions to treat, as is evidenced by the plethora of trials that continue to be conducted. A large part of its intractability stems from the myriad pathophysiological mechanisms that can result in PAP. Whereas mechanism-based pain treatment is generally considered to be superior to etiologic-based therapy,5,6 the obstacles involved in identifying the predominant mechanism(s) – which are prodigious under the best of circumstances – can become nearly insurmountable for a condition as phenotypically and pathogenetically disparate as PAP. The purpose of this review is therefore to provide an evidence-based framework from which to evaluate therapies and guide treatment for PAP.
Definitions and epidemiology
In the United States, the prevalence of limb loss was 1.6 million in 2005, which is projected to increase to 3.6 million by 2050.7 Approximately 185,000 upper- or lower-limb amputations are performed annually. According to a study by Dillingham and colleagues examining data from the Healthcare Cost and Utilization Project from 1988 to 1996, vascular pathology is the most common etiology, accounting for 82% of limb loss discharges followed, in descending order, by trauma (16.4%), cancer (0.9%), and congenital anomalies (0.8%).8 The loss of a body part can lead to painful and nonpainful neurologic sequelae that fall into three distinct descriptive categories: phantom limb pain (PLP), residual limb pain (RLP), and phantom sensations (PSs). Although these categories will be described independently, one cross-sectional study by Ephraim and colleagues performed in 914 individuals with limb loss found that up to 95% experienced at least one of these categories.9 Furthermore, patients surveyed about their postamputation sensations often have a difficult time distinguishing one category from another.10
PLP is a painful or unpleasant sensation in the distribution of the lost or deafferentated body part. PLP varies in character from neuropathic-type descriptors such as sharp, shooting, or electrical-like, to more nociceptive-specific adjectives such as dull, squeezing, and cramping. It can be localized to the entire limb or just one region of the missing limb. PLP typically occurs within the first 6 months after loss of a limb, but its prevalence several years after surgery has been reported to be as high as 85%, and it can persist for years after surgical amputation.11,12 In a prospective study evaluating 58 patients who underwent limb amputation, Jensen et al found that PLP changed over time from an exteroceptive-like pain (ie, knife-like or sticking) localized to the entire limb or a proximal region, to a more proprioceptive-like pain (burning or squeezing) localized to the distal areas of the amputated limb.13
PLP should be distinguished from RLP, also known as “stump” pain, which is localized to the remaining body part after amputation. Stump pain is typically described as a sharp, burning, electrical-like, or “skin-sensitive” pain which can be localized to a superficial incision, be perceived deep in the residual limb, or sometimes encompass the whole residual limb. The reported incidence of stump pain can be as high as 74%, and similar to phantom pain can persist for years.14 Stump pain can be further subdivided into postsurgical nociceptive, neurogenic, prosthogenic, arthrogenic, ischemic, sympathetically maintained, pain referred from the spine or joints, or pain secondary to abnormal stump tissue such as adhesive scar tissue or heterotopic ossification.12 Although PLP and RLP often coexist, RLP is usually more bothersome immediately after amputation, whereas PLP may predominate 1–12 months after the amputation event.15 Studies have found a significant correlation between the magnitude of RLP and PLP.16
PSs are defined as nonpainful perceptions emanating from the lost body part after deafferentation or amputation. PSs are common in the postoperative period, with one-third of patients experiencing PSs within 24 hours, three-quarters of patients within 4 days, and 90% of patients within 6 months after surgery.13 Unlike PLP and RLP, amputation of a body part is not essential prior to the development of PSs. PSs have been reported after avulsion of the brachial plexus without amputation of the limb,17 and following spinal cord injury.18 PSs can be subdivided into kinetic, kinesthetic, and exteroceptive perceptions. Kinetic sensations are perceived movements of the amputated body part that can be willed or spontaneous, such as the movement of toes in an amputated foot. Kinesthetic sensations refer to the size, shape or position of the amputated body part, such as feeling that a hand is twisted. Exteroceptive perceptions can include touch, pressure, tingling, temperature, itch, and vibratory sensations.18 PSs are typically experienced in regions with disproportionately large cortical representation, such as the hands and feet. PSs can result not just from amputation of an extremity but also excision of other body parts such as the breast after mastectomy, which is estimated to occur in approximately 25% of individuals.19 Telescoping refers to the perception of progressive shortening of the amputated limb, which results in the sensation that the distal part of the limb is becoming more proximal.13 For example, a patient with an above the elbow amputation may initially feel phantom pain or sensations in the entire forearm and hand. Over time, the same patient may perceive his or her hand to be close to the stump, but not feel the proximal forearm. This phenomenon occurs in one-quarter to two-thirds of major limb amputees.20
PAP is primarily a clinical diagnosis based on history and physical examination, though certain tests can help rule out alternative and often remediable diagnoses such as referred back pain, residual ischemia, prosthesis-related pain, neuromas, pressure-related wounds, and infection. A study by Smith and colleagues performed in 92 patients undergoing amputation found that back pain was more prevalent (71%) compared with that of the general population (45%).21 Patients with chronic mechanical lower-back pain may have referred pain to the leg from such sources as the lumbar zygapophysial and sacroiliac joints, which can be mistaken for PLP.22 Ischemic injury must be ruled out in patients presenting with PAP, especially since a large proportion of patients who undergo amputation have vascular insufficiency as the underlying etiology. Tests of distal perfusion such as transcutaneous oxygen tension (positive for ischemia if less than 20 mmHg) at the level of the residual limb can be useful in ruling out an ischemic etiology. Diagnosing a neuroma as a source of RLP may be useful when formulating a treatment plan. A positive Tinel’s sign (tapping on the injured nerve or neuroma elicits pain in the phantom limb or stump) represents a classic feature for neuroma. Prosthesis-related pain is often mistaken for classical RLP or PLP, and in some cases can be easily remedied. Occasionally, residual limbs may atrophy over time leading to stump shape changes relative to the original mold obtained during the casting process. This results in load-bearing and other forces inside the socket to shift from weight-tolerant to intolerant areas, which can cause erosion of the skin around contact points and overlying bony tissue. A careful skin and soft tissue examination of the stump can effectively rule out pressure wounds or frank infections that may be developing. Pressure points that develop over bone spurs or pathologic bone formation (ie, heterotopic ossification) can be a source of localized pain, which can be identified on plain radiographs. Infections such as osteomyelitis and residual graft infection can also be a source of chronic PAP.
Although primarily used in pain research, quantitative sensory testing (QST) may be a valuable tool for the diagnosis and management of PAP. QST entails the determination of pain thresholds or stimulus response curves for sensory processing under normal and pathophysiological conditions. For example, QST has been used to provide quantitative objective measures of neuropathic pain via the conductance of thermal testing in regions of heat allodynia, which can improve diagnosis and inform treatment.23–27 In short, QST may allow clinicians to better phenotype patients, which in turn may improve treatment outcomes.
Mechanisms
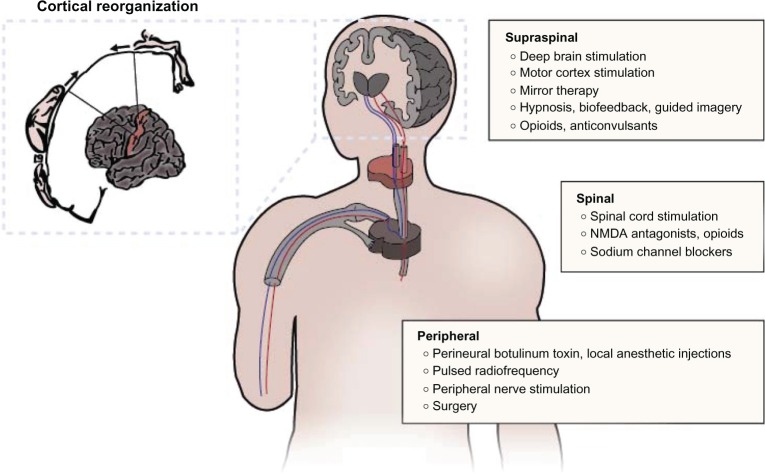
Treatment of PAP is very challenging because the underlying mechanisms are multifactorial in nature. Since mechanisticbased pain treatment is generally acknowledged to be superior to etiologic-based treatment, the difficulty in identifying a discrete mechanism(s) which can be directly addressed results in corresponding barriers to treatment.5 The pathophysiology underlying phantom phenomena can be broadly categorized in terms of supraspinal, spinal, and peripheral mechanisms (see Figure 1). Supraspinal mechanisms related to phantom limb phenomena primarily involve reorganization of the somatosensory cortex surrounding the area representing the deafferentated limb. Ramachandran and colleagues demonstrated that brushing the face of upper limb amputees could elicit PSs.28 They hypothesized that somatosensory cortical reorganization could explain why afferent nociceptive stimulation of a body part (eg, proximal stump or face for upperlimb amputees) whose cortical representation is adjacent to that of the phantom can produce sensations in the phantom. Specifically, tactile, proprioceptive, and nociceptive input from the face and tissues near the residual limb take over regions of the brain that no longer receive afferent input. Functional magnetic resonance imaging (MRI) studies after amputation of the hand have demonstrated that the cortical area corresponding to the hand is activated during proximal limb movements, and that cortical stimulation of this region evokes contraction of proximal upper-limb muscles.29–32 The greater the size of the deafferentated area and extent of cortical reorganization, the more intense the PSs.33,34
Figure 1.
Mechanism-based treatment modalities for postamputation pain.
Abbreviation: NMDA, N-methyl-D-aspartate.
The evidence for peripheral mechanisms playing a role in PAP include the demonstration of spontaneous neuronal activity in the proximal end of cut nerves, the presence of stump pathology in some patients with phantom pain and the strong correlation between RLP and PLP, and the relief of phantom pain after the injection of local anesthetic into the painful stump.13,35 Axonal nerve damage during an amputation initiates inflammation and regenerative sprouting which results in a neuroma. Afferent fibers in the neuroma develop ectopic activity, mechanical sensitivity, and chemosensitivity to catecholamines. Altered expression of transduction molecules, upregulation of voltage-sensitive sodium channels, downregulation of potassium channels, and the development of new nonfunctional connections between axons (ephapses) all serve to increase spontaneous afferent input to the spinal cord.36 These changes may lead to spontaneous pain, and help explain the amplification in pain caused by emotional distress and/or exposure to cold that leads to increased sympathetic discharge and circulating catecholamines.20
The spinal mechanisms for PAP are thought to center on functional changes in the dorsal horn of the spinal cord after deafferentation from a peripheral nerve injury. The loss of afferent input to the dorsal horn leads to decreased impulses from brainstem reticular areas, which normally exert inhibitory effects on sensory transmission.37 Therefore the absence of inhibitory effects for sensory input arising from the missing peripheral body part cause increased autonomous activity of dorsal horn neurons, in effect becoming “sensory epileptic discharges.”11,12 The contribution of spinal cord mechanisms is illustrated by the fact that anticonvulsants, and lesions placed in the substantia gelatinosa, are effective in treating phantom pain.38 Similar to cortical reorganization, a “spinal reorganization” process has also been described in which adjacent afferent fibers “invade” regions of the spinal cord that are functionally inactivated by injured afferent fibers.38 Clinically, the evidence supporting spinal mechanisms is bolstered by: the development of phantom pain in lower-extremity amputees following new lumbar disc herniations, and new-onset phantom pain in an amputated upper extremity associated with herpes zoster infection, both of which have been successfully treated with epidural steroid injections;39 the evocation of phantom pain with spinal analgesia;40 and an unusual case in which longstanding PLP disappeared with the development of cauda equina compression by a tumor and recurred following decompression.41
Multiple cellular, neurochemical and molecular changes underlie the peripheral and central reorganization phenomena that occur in the postamputation period. Studies of nonhuman primates have demonstrated that chronic deafferentation can cause distal axon sprouting and the formation of neuromas,42 chromatolysis (dissolution of Nissl bodies in the neuronal cell body) and loss and fibrosis of dorsal root ganglion cells,43–46 atrophy or degeneration of central terminations of sensory neurons in the brainstem46 and spinal dorsal horn,45,47 sprouting of sensory neuron terminations in the dorsal horn,48,49 decreased myelination, and changes in neuropeptide levels in dorsal root ganglia and the dorsal horn.50 In the first month after amputation, nerve injury can cause transsynaptic atrophy of central neurons. Neurochemically, lower-limb amputations lead to decreased lectin binding and substance P levels and upregulated neuropeptide Y.51,52 These peripheral neuronal changes have been observed from about 2 months to as many as 38 years after amputation, and appear to be concurrent with changes in the brainstem. Immunohistochemical studies evaluating changes in the dorsal column nuclei of chronic upper- and lower-limb amputees have revealed some atrophy of cuneate and gracile nuclei ipsilateral to the amputation, as well as proliferation of astrocytes, reactive gliosis, and inflamed axons (spheroids).53 These findings suggest that amputation triggers neurochemical/molecular changes that cause degenerative and regenerative changes in primary sensory axons in the dorsal column nuclei.
Ultimately, pain after amputation is likely caused by a combination of the above mechanisms as total spinal anesthesia, cordotomy, cordectomy, spinal cord stimulation, and regional anesthesia of the plexus or stump have at best yielded only modest relief of phantom pain. As noted above, in some cases spinal anesthesia can even rekindle phantom pain that previously subsided.54,55 Hence, the interactions between peripheral, spinal, and supraspinal phenomena are all thought to contribute to postamputation phenomena, and should all be considered when planning treatment.
Treatment
Injection therapy
There are few controlled trials available to guide pain practitioners in the optimal management of PAP, with most therapies extrapolated based on effectiveness in other neuropathic pain states. Presently, the state-of-the-art treatment of PAP involves a multimodal approach that includes injections, pharmacotherapy, complementary and alternative therapies, surgery, and prevention.
Based on available evidence, local injection therapy appears to be more efficacious in the treatment of RLP compared with PLP. This appears to be due to the greater contribution of peripheral mechanisms in RLP compared with PLP. Although regional nerve blocks using lidocaine and/or corticosteroid often results in immediate relief of RLP, the duration of pain relief is highly variable and temporary.56,57 An active area of research aims to prolong this effect. One small randomized controlled pilot study examined the Efficacy of focal chemo-denervation using perineural injection of botulinum toxin type A compared with combination lidocaine and depomedrol. The study found that while both therapies showed a trend toward Efficacy, botulinum toxin resulted in a statistically significant improvement in RLP at 1 month, which was sustained over the 6-month study period. Neither modality improved PLP.58 Another small series found a similar short-term benefit for RLP with the local injection of botulinum toxin B.59 A separate small case series found that for patients who experienced relief from a diagnostic lidocaine injection, pulsed radiofrequency was effective in relieving RLP, although the effects were mixed for PLP.60 Another small case series found perineural injection of the tumor necrosis factor inhibitor to be effective in patients with PLP and RLP of less than one year duration and tender points on physical examination.61 A small observational study demonstrated that sympathetic dysfunction may play a role in the pathogenesis of PAP, and that sympathetic nerve blocks may provide some short-term relief of PLP, and to a lesser extent RLP.62 It is important to note that local injection therapy may have effects beyond providing local peripheral blockade of pain input. One small observational study found that contralateral myofascial injection with local anesthetic in unilateral amputees attenuated PLP and PSs in the affected limb, though follow-up was limited to 1 hour.63 Whereas the precise mechanism for this effect is unclear, animal studies have demonstrated that blocking afferent inputs on the contralateral side can decrease spontaneous hyperactivity of wide dynamic response neurons on the injured side, suggesting that a spinal mechanism may be at work.64
Pharmacotherapy
When choosing pharmacotherapy for patients with established PAP, the practitioner must consider chronicity, route of administration, and adverse effects. There are six groups of medications for which there is evidence in the treatment of PAP: N-methyl-D-aspartate (NMDA) receptor antagonists, opioids, anticonvulsants, antidepressants, local anesthetics, and calcitonin (see Table 1).
Table 1.
Randomized controlled trials of pharmacologic interventions for the treatment of postamputation pain
| Study | N | Treatment/placebo | Chronicity | Adverse events | Follow-up | Effecta |
|---|---|---|---|---|---|---|
| NMDA antagonists | ||||||
| Memantine | ||||||
| Maier et al68 | 36 | 1. Oral memantine 30 mg/d × 3 weeks 2. Placebo |
> 12 months | Vertigo, fatigue, headache, nausea, restlessness, excitation, cramps | 3 weeks | − |
| Wiech et al69 | 8 | 1. Oral memantine titrated to 30 mg/d × 4 weeks 2. Placebo |
Chronic | Fatigue, agitation, dizziness, nausea, headache | 30 days | − |
| Schwenkreis et al70 | 16 | 1. Oral memantine titrated to 30 mg/d 2. Placebo |
> 12 months | Not described | 3 weeks | − |
| Dextromethorphan | ||||||
| Abraham et al67 | 10 | 1. Oral dextromethorphan 120 mg/d × 10 days 2. Oral dextromethorphan 180 mg/d × 10 days 3. Placebo |
Mean duration of pain 4.8 months |
None reported | 10 days | + |
| Ketamine | ||||||
| Nikolajsen et al65 | 11 | 1. IV ketamine 0.5 mg/kg infusion × 45 minutes 2. Placebo |
Mean duration of pain 4 years | Insobriety, mood elevation, discomfort | 45 minutes | + |
| Eichenberger et al66 | 20 | 1. IV ketamine 0.4 mg/kg infusion × 1 hour 2. IV calcitonin 200 IU infusion × 1 hour 3. Combination ketamine/calcitonin 4. Placebo |
Mean duration of pain 12 years | Loss of consciousness, light sedation, light visual hallucination, hearing impairment, position/feeling impairment | 48 hours | + |
| Anticonvulsants | ||||||
| Gabapentin | ||||||
| Bone et al76 | 19 | 1. Oral gabapentin titrated to 2400 mg or maximum tolerable 2. Placebo |
>6 months | Somnolence, dizziness, headache, nausea | 6 weeks | + |
| Smith et al77 | 24 | 1. Oral gabapentin titrated to 3600 mg or maximum tolerable 2. Placebo |
>6 months | Not described | 6 weeks | − |
| Antidepressants | ||||||
| Amitriptyline | ||||||
| Robinson80 | 39 | 1. Oral amitriptyline 10 mg/d titrated to maximum 125 mg/d 2. Oral benztropine 0.5 mg/d |
>3 months | Dry mouth, dizziness | 6 weeks | − |
| Calcitonins | ||||||
| Jaeger and Maier79 | 21 | 1. IV calcitonin 200 IU X 20-minute infusion 2. Saline |
0-7 days following amputation | Headache, vertigo, nausea, vomiting, augmented phantom sensations, drowsiness, hot flashes | 1 year | + |
| Opioids | ||||||
| Huse et al72 | 12 | 1. Oral morphine titrated to 300 mg/d or maximum tolerable 2. Placebo |
Chronic | Constipation | 4 weeks | + |
| Wu et al73 | 31 | 1. IV morphine 0.2 mg/kg infusion × 40 minutes 2. IV lidocaine 4 mg/k influsion × 40 minutes 3. Diphenhydramine placebo |
>6 months | Sedation (nonsignificant) | 30 minutes | + (morphine and lidocaine groups versus placebo) |
| Local anesthetics | ||||||
| Casale et al63 | 8 | 1. Contralateral myofascial inj with bupivacaine 2.5 mg/mL 2. Placebo |
>6 months | None | 60 minutes | + |
Notes:a“+” designates studies that show a statistically significant improvement of the study drug over placebo in the treatment of postamputation pain, and “−“ designates studies that do not
Abbreviations: IV, intravenous; NMDA, N-methyl-D-aspartate.
NMDA receptor antagonists including ketamine, dextromethorphan, and memantine are thought to block a cascade of events leading to sensitization of dorsal horn wide dynamic range neurons. In patients with PLP or RLP, Nikolajsen and colleagues found a significant decrease in pain intensity, wind-up-like-pain, and pressure-pain thresholds following a 45-minute low-dose ketamine infusion compared with a normal saline control.65 Although most of the participants in this study had PAP following amputations for cancer, a more recent study by Eichenberger found 1 hour ketamine (0.4 mg/kg) and ketamine plus calcitonin infusions to be effective for up to 48 hours compared with placebo for participants with various etiologies of PLP. No benefit was noted for calcitonin either alone or combined with ketamine.66 Likewise, oral dextromethorphan has been shown to be effective in reducing pain intensity in a small placebo-controlled crossover study comprised of patients with PLP,67 but oral memantine has not been shown to have analgesic properties when treating patients with established PLP.68–70 Interestingly, memantine has been efficacious in combination with brachial plexus blockade to prevent PLP acutely, suggesting that the timing of administration may be important.71 Whereas the evidence for ketamine is strongest, the short follow-up periods and high incidence of adverse effects, including alterations in consciousness, visual hallucinations, hearing impairment and mood changes, limit its long-term usefulness.
Opioids may be beneficial in the treatment of PAP due to its mechanism of action at both the spinal level, where it inhibits pain signaling pathways, and supraspinal level, where it may diminish the degree of cortical reorganization associated with pain intensity.72 Both oral and intravenous opioids administered for up to 6 weeks have been shown to be effective for PAP.72–74 In fact, Huse and colleagues showed that cortical reorganization was reduced in two of three participants with PLP undergoing treatment with oral morphine at both 6 and 12 months follow-up for one patient, and during the treatment phase for the other.72 Similarly, tramadol has been shown to be effective in treatment of long-standing PAP compared with placebo over a 1-month treatment period.75 Among the two opioid class medications, morphine has the more severe adverse-event profile, which includes constipation, sedation, tiredness, dizziness, sweating, voiding difficulty, vertigo, itching, and respiratory problems.
Anticonvulsants have long been a mainstay in the treatment of neuropathic pain. However, studies examining gabapentin as a treatment for established PAP have been conflicting with both positive and negative trial results.76,77 Gabapentin was associated with significant side effects in both studies, including somnolence, dizziness, headache, and nausea.
Calcitonin has a direct central action which causes inhibition of neuronal firing in response to peripheral stimulation.78 This mechanism of action has encouraged interest in calcitonin as an adjunctive medication in the treatment of PAP. However, studies to date have been variable. One early controlled crossover study by Jaeger and Maier demonstrated a reduction in pain intensity compared with placebo that was sustained through 1-year follow-up in 8 of 13 patients with postoperative PLP who received a single calcitonin infusion.79 However, a more recent study by Eichenberger et al evaluating calcitonin as a treatment for established PLP found calcitonin to be ineffective compared with placebo, attributing its ineffectiveness to a possible lack of effect on central sensitization processes.66 Adverse effects of calcitonin included headache, vertigo, drowsiness, nausea, emesis, and hot/cold flashes.
Sodium channel blockers have been shown to be effective for both neuropathic and inflammatory pain. One study assessing amitriptyline in the treatment of PLP or RLP did not show a significant difference compared with placebo after 6 weeks of treatment, although patients in the treatment group did experience adverse effects such as dry mouth and dizziness severe enough to cause dropouts.80 Whereas tricyclic antidepressants act in part via the blockade of sodium channels, their main mechanisms of action involve enhancement of descending inhibitory pathways via the inhibition of serotonin and norepinephrine reuptake. Similarly, evidence for using primary sodium channel blocking medications has been mixed at best. One double-blind study by Wu et al found that whereas intravenous morphine provided significant immediate-term relief of both PLP and RLP compared with placebo, intravenous lidocaine alleviated only RLP.73 In a placebo-controlled follow-up study by the same group in 60 patients with PAP, morphine but not the oral lidocaine analogue mexiletine provided significant pain relief at 6-week follow-up.74
Complementary and alternative therapies
The refractory nature of PAP to traditional medical and interventional therapies underscores the importance of developing complementary and alternative therapies. Psychological interventions for PAP aim to facilitate adaptation to pain, body image, and negative emotions associated with amputation. In one randomized controlled trial of 20 patients with 6 months of RLP or PLP, hypnosis administered in three individual sessions reduced overall pain scores when compared with pre-intervention scores.81 Evidence for other psychological techniques such as guided imagery (creating mental images that help promote relaxation and healing) and biofeedback (learned control over autonomic physiologic processes) is mostly anecdotal.82,83 In one case series by Beaumont et al in which six amputees with chronic PLP underwent visual-kinesthetic feedback therapy over 8 weeks, four participants demonstrated greater than 30% reduction of pain after the intervention but only one maintained this over 6 months of follow-up. The authors pointed out that psychological health, social support, and the degree of control prior to the intervention may be significant factors in determining those who benefit compared with those who do not.82
Cognitive behavioral therapy (CBT) has been used successfully in patients with chronic neuropathic pain conditions.84–86 In particular, a case series by Tichelaar and colleagues involving three patients with complex regional pain syndrome type I suggested that CBT may address pain mediated by central cortical reorganization.86 Although there are no controlled trials showing Efficacy for CBT in PAP, there is an ongoing randomized controlled trial by McQuaid and colleagues designed to test whether CBT plus mirror therapy is superior to supportive care in amputees.87 Whereas psychological interventions such as hypnosis, biofeedback, guided imagery, and CBT are safe and minimally invasive, large-scale trials are lacking and there is little evidence for long-term benefit.
Mirror therapy exploits the brain’s predilection to prioritize visual information over somatosensory feedback and is believed to treat PAP by influencing cortical reorganization. Flor et al showed that the degree of phantom pain correlates with the degree of maladaptive reorganization of somatosensory pathways using functional MRI, and that reorganization can be reversed by mirror therapy with a corresponding reduction in pain.88,89 Also known as visual mirror feedback, mirror therapy involves placing a mirror adjacent to the intact limb to give the illusion that the amputated limb is present and can be purposefully moved. Since it was introduced in 1992 by Ramachandran and Altschuler,90 multiple studies have demonstrated short-term pain reduction using visual feedback using both mirrors and virtual reality or video modalities.91,92 Chan et al randomly assigned six patients each to one of three groups, mirror therapy, covered mirror therapy, and trained visual imagery, and showed that after 4 weeks, pain decreased in the mirror therapy group, stayed the same in the covered mirror therapy group, and increased in the visual imagery group. Nine of the patients in the covered mirror and visual imagery groups crossed over to the mirror therapy group, with a mean decrease in pain of 75% over the next 4 weeks compared with their baselines.93 Because sensory experiences can be evoked by visual stimuli, mirror therapy increases spinal motor and cortical excitability.94 The simplicity and noninvasiveness of this treatment modality has led to its application not only following limb loss, but also for the prevention of PAP.95
Surgical therapies
Although surgical interventions have not demonstrated significant benefit in well designed trials, patients with chronic intractable PAP who fail the aforementioned treatment modalities may sometimes be considered for surgical management.12 Surgical modalities fall into two general categories: neuromodulatory techniques and reconstructive. Neuromodulatory therapies are by definition mechanism driven, targeting maladaptive neuroplastic changes at the peripheral, spinal, and supraspinal levels. Although there are no randomized controlled trials to demonstrate Efficacy and safety for peripheral nerve stimulation (PNS), PNS has the potential to be especially effective in patients for whom the majority of pain is confined to the distribution of one or two peripheral nerves. Historically, peripherally placed electrodes required surgical dissection of the nerve in order to place the electrodes along the nerve trunk.96 Recently, Rauck and colleagues demonstrated that a PNS lead inserted percutaneously and remotely from the target nerve in a single patient with RLP could lead to both pain relief and improvement in quality of life outcomes at 2 weeks follow-up.97 The emergence of percutaneous techniques may change the risk/ benefit for patients with refractory RLP, and represents a promising area of future study. Whereas targeting peripheral mechanisms may be sufficient in patients with RLP, those with central sensitization or deafferentation, as occur with PLP, require neuromodulation at spinal or supraspinal levels. Spinal cord stimulation has been shown to be effective in a number of neuropathic pain states, but the evidence for its Efficacy in PAP is less robust, with several studies demonstrating inferior outcomes compared with peripheral neuropathic pain.98–102 The evidence that does exist is mainly limited to small case series that report “successful outcome,” with the criteria for a successful outcome varying drastically between studies98–104 (see Table 2). Nonetheless, spinal cord stimulation is reimbursed by Medicare specifically “to treat intractable pain caused by phantom limb syndrome that has not responded to medical management.”105 Although still considered investigational by the Food and Drug Administration, motor cortex stimulation in PAP is very promising. One meta-analysis of 155 patients from nine studies of motor cortex stimulation in various chronic pain states show that 53% of patients with PLP were treated successfully, with follow-up periods that ranged from 6 months to 10 years.106 Motor cortex stimulation directly targets the site of cortical reorganization and pain by using precise positioning techniques such as preoperative functional MRI and awake intraoperative stimulation. Deep brain stimulation has been shown to be more effective in nociceptive pain conditions such as failed back surgery syndrome rather than in deafferentation central pain states, and is associated with mixed results in patients with PA P.107
Table 2.
Studies evaluating neuromodulation for the treatment of postamputation pain
| Implant type | Implant location | Study | Number of implants | Criteria for successful outcome | Follow-up | Successful outcomes |
|---|---|---|---|---|---|---|
| MCS, DBS, SCS | Epidural | Katayama et al108 | 19 | >80% improvement in VAS | 2–18 years | 6/19 SCS, 6/10 DBS, 1/5 MCS |
| MCS | Epidural | Sol et al109 | 3 | >70% improvement in VAS | 24–29 months | 2/3 |
| DBS | Periventricular gray/thalamus | Bittar et al110 | 3 | >50% improvement in VAS | 8–20 months | 3/3 |
| SCS | Subdural | Nielson et al98 | 6 | Subjective pain relief | 7–25 months | 4 excellent, 1 good |
| SCS | Subdural, endodural | Hunt et al100 | 5 | Excellent: complete pain relief Partial: incomplete pain relief | Not noted | 1 excellent, 1 partial, 3 no benefit |
| SCS | Epidural | Miles and Lipton101 | 9 | Excellent: no narcotics Some: need for occasional narcotics | 1 year | 6 excellent, 1 some, 2 none |
| SCS | Subdural, endodural | Krainick et al99 | 61 | % subjective pain relief | Not noted | 0% – 28 |
| 1%–25% – 7 | ||||||
| 26%–50% – 12 | ||||||
| 51%–75% – 13 | ||||||
| >75% – 1 | ||||||
| SCS | Epidural | Sanchez-Ledesma et al102 | 3 trials 6 implants | >75% subjective pain relief | 5.5 years | 57% met success criteria |
| SCS | Epidural | Broggi et al104 | 23 trials 26 implants | Verbally classified pain intensity >50%, life standard | 2 years | 58% met success criteria |
| SCS | Epidural | Kumar et al103 | 3 | >50% improvement subjective pain relief | 6 months to 15 years | 0 |
| SCS | Epidural | McAuley et al111 | 12 | >50% improvement VAS | 5–20 years | 5/12 |
| PNS | Brachial plexus, sciatic, femoral | Long112 | 4 | Satisfactory pain relief | 3–18 months | 2/4 |
| PNS | Sciatic | Nashold et al113 | 1 | Satisfactory pain relief | 8 years | 1/1 |
| PNS | Brachial plexus, sciatic, femoral | Campbell and Long114 | 6 | >50% subjective pain relief | 6–54 months | 0/6 |
| PNS | Femoral | Rauck et al97 | 1 | Mean pain interference scores, pain disability index | 8 weeks | 1/1 70% and 52% improvement |
Abbreviations: DBS, deep brain stimulator; MCS, motor cortex stimulator; PNS, peripheral nerve stimulator; SCS, spinal cord stimulator; VAS, Visual Analog Scale.
The contribution of peripheral mechanisms is greater in RLP compared with PLP; therefore, surgical reconstruction can be successful in treating RLP associated with distinct pathologic lesions. For example, heterotopic ossification is highly prevalent in patients with traumatic amputation, with a prevalence rate of up to 63%.115 In the same study by Potter and colleagues, 20 of 25 patients with traumatic amputations whose heterotopic ossifications were excised were able to discontinue or reduce their opioid and/or neuropathic pain medication consumption at an average of 12 months follow-up.115 Neuromas are an inevitable sequelae of major nerve injury or transaction, and clinically significant neuromas may occur in up to 80% of cases, presenting as a discrete area of pain and abnormal sensation in the distribution of a single peripheral nerve.116 Frequently, a Tinel’s sign can be elicited. Whereas this typically manifests as pain in the residual limb, referred pain from the stump into the phantom limb can also occur. Unlike with heterotopic ossifications, the long-term outcomes of peripheral nerve surgery are mixed. Several older studies have reported only a short duration of pain relief, with recurrence of the neuromas and RLP redeveloping months after initial resection.117–119 Nonetheless, more recent retrospective and prospective studies have shown that peripheral nerve reconstructive techniques could lead to improvement in pain and quality of life for both RLP120 and PLP.121 Currently, peripheral nerve reconstruction remains a viable option for RLP refractory to interventional and pharmacologic treatment modalities.
Prevention
In view of the inherent challenges and limited success observed in treating PAP, many investigators have attempted to find ways to preemptively treat acute PAP, thereby preventing acute PAP from becoming chronic. For the purpose of this review, preemptive interventions shall refer to interventions which take place preoperatively, intraoperatively, or in the early postoperative period (<2 weeks) after an amputation, with the goal being to avert long-term spinal sensitization by blocking nociceptive input after peripheral nerve injury.122 In general, the evidence supporting preemptive interventions to reduce or prevent chronic pain have been limited to small trials of varying quality. A systematic review by Halbert et al identified eight controlled trials in which a preemptive intervention, including epidural treatments (three trials), regional nerve blocks (three trials), intravenous calcitonin infusion (one trial), and transcutaneous electrical nerve stimulation (TENS; one trial) was used to prevent or treat acute PLP.123 The results were mixed for epidural treatments, with one small trial showing decreased PLP at 1 week, 6 months, and 1 year follow-up, another small trial showing decreased PLP which only reached statistical significance at 6 months follow-up, and the largest, most methodologically sound trial showing no difference between the two groups.124–126 The trials for peripheral nerve blocks, calcitonin, and TENS all showed no difference in pain control between intervention and control groups in long-term follow-up (6 months or greater).127–130 The authors also used a quality assessment instrument to determine the likelihood of bias in three areas: randomization, double-blinding, and withdrawals or dropouts.131 In their discussion, they note that the reviewed trials were of poor overall quality due to the use of a variety of PLP outcome measures, which prevented examination of the treatment effect on pain. Overall, they concluded that the evidence does not support treatment of acute PLP in the acute postoperative period.123
Treatment strategies for preventing the development of chronic postsurgical PAP primarily focus on blocking nociception at the spinal and peripheral nerve levels. The area that has been best studied is the use of epidural anesthesia for prevention of PAP. As summarized in Table 3, the evidence overall has been conflicting, with several promising early studies suggesting that preoperative epidural anesthesia could decrease incidence of PLP.124,125,132 However, more recent studies have been mixed at best, with several showing no effect.126,133,134 One recent study by Karanikolas et al showed that optimized epidural or systemic analgesia started 48 hours preoperatively was similarly effective in reducing the incidence of PLP at 6 months.135 Overall, these studies suggest that timing may be critical; compared with studies that demonstrate no benefit for preemptive epidural analgesia, those that demonstrate effectiveness were more likely to implement treatment 24 hours or more preoperatively124,125,135 (see Table 3). Another important factor affecting study results seems to be the effectiveness of the “control” treatment, as those studies in which the nonepidural or control treatment group was carefully managed have been less likely to demonstrate a benefit than those in which postoperative pain care was suboptimal.134–136
Table 3.
Prospective studies evaluating epidural effect on preventing phantom limb pain
| Study | Number of patients | Treatments | Randomizationa | Blindinga | Preoperativeb | Hours preoperative | Intraoperativeb | Postoperativeb | Effectc |
|---|---|---|---|---|---|---|---|---|---|
| Bach et al124 | 25 | 1. Epidural bupivacaine, morphine 2. Opiods, paracetamol, dextropropoxiphen, acetylsalicylic acid |
− | − | + | 72 | + | − | + |
| Jahangiri etal125 | 24 | 1. Perioperative epidural bupivacaine, Clonidine, diamorphine 2. On-demand opioids |
− | − | + | >24 | + | + | + |
| Schug et al132 | 23 | 1. Perioperative epidural bupivacaine, fentanyl 2. Intraoperative epidural bupivacaine, fentanyl |
− | − | + | 2c | + | + | + |
| Katsuly-Liapis 1996148 | 45 | Not described | + | Not described | + | + | + | + | |
| Nikolajsen et al126 | 60 | 1. Epidural bupivacaine, morphine 2. Epidural saline and oral or IM morphine |
+ | + | + | 18 | + | + | − |
| Lambert et al133 | 30 | 1. Epidural bupivacaine and diamorphine 2. Perineural bupivacaine |
+ | + | 24 | + | + | No difference between epidural and perineural groups | |
| Wilson et al134 | 53 | 1. Epidural ketamine/bupivacaine 2. Epidural bupivacaine |
+ | + | 0 | + | + | No difference between epidural groups | |
| Karanikolas et al135 | 65 | 1. Epidural anesthesia and analgesia 2. Preoperative IV PCA, postoperative epidural analgesia and anesthesia 3. Perioperative IV PCA and epidural anesthesia 4. Perioperative IV PCA and general anesthesia 5. Conventional analgesia and anesthesia |
+ | + | + | 48 | + | + | + |
Notes:aRandomization and blinding of study participants and investigators was either employed “+” as a method in the study or not employed “–”;
“+” refers to when patients received epidural infusions (preoperatively, intraoperatively, postoperatively), and “–“ means that the epidural infusion was stopped or not started;
“+” designates studies that show a statistically significant improvement of the study drug over the placebo in the treatment of postamputation pain, and “–“ designates studies that do not
Abbreviations: IM, intramuscular; IV, intravenous; PCA, patient-controlled analgesia.
For perineural anesthesia, the available evidence is limited to several studies whose results are conflicting. An uncontrolled study by Borghi et al (n = 71)137 showed that continuous peripheral nerve blockade that starts immediately preoperatively or intraoperatively and continues postoperatively can be effective in reducing the incidence of severe PLP, with the benefit persisting for up to 12 months. A randomized, controlled study that compared continuous postoperative brachial plexus block with the oral NMDA receptor antagonist memantine to brachial plexus blockade alone found that that the addition of memantine reduces the incidence of PLP at 4 weeks and 6 months, but not at 12 months.71 However, a small (n = 21) randomized, controlled study by Pinzur et al found that sciatic nerve blockade begun immediately postoperatively fails to prevent phantom pain compared with a control group that received saline, though it did decrease postoperative opioid consumption.130 Collectively, these studies do not support the routine use of postoperative perineural anesthesia to prevent PLP, though the effect of preoperative nerve blockade warrants further investigation.
Systemic therapies have demonstrated mixed results in preventing PAP. A small placebo-controlled crossover study done in the early 1990s (n = 21) evaluating intravenous calcitonin early in the postoperative period found a reduction in lower extremity PLP for up to 24 hours that persisted in an open-label phase for most patients throughout their 1-year follow-up.79 Yet, a larger and more methodologically sound study comparing gabapentin – a first-line medication for neuropathic pain138 – with placebo starting on postoperative day 1 and continued over a 30-day period failed to show any benefit during the 6-month follow-up period.139
Several studies have examined the effects of complementary and alternative treatments in preventing PAP. A randomized, controlled study conducted in 51 patients with acute lower extremity amputations compared TENS with sham TENS plus chlorpromazine, and sham TENS alone, for the prevention of PLP, re-operation rates, and postoperative wound healing.140 Although a lower incidence of PLP occurred at 4 months in the active TENS group, no differences were observed at 4 weeks or 1-year post- amputation. Of note, the active TENS group experienced more rapid stump healing and a lower re-amputation rate than the control groups. Despite the recognition of the importance of supraspinal mechanisms in the treatment of existing chronic PAP, few studies have been performed evaluating the utilization of supraspinal modalities for the prevention of PAP. In a four-patient case series by Hanling and colleagues evaluating 2-weeks of preemptive mirror therapy prior to elective limb amputation, one patient did not experience PLP, two patients reported rare episodes of mild PLP, and one patient had moderate PLP, for up to 1-month post-surgery.95 This suggests that preventative strategies targeting supraspinal mechanisms such as mirror therapy, may be a promising area for future research.
Conclusion and future directions
PAP remains a highly prevalent but difficult-to-treat condition for patients undergoing amputations. Treatment must be multimodal and mechanism-based in nature, taking into consideration supraspinal, spinal, and peripheral mechanisms. Further investigation into the mechanisms responsible for and the factors associated with the development of PAP is needed to provide an evidence-based foundation to guide current and future treatment approaches. The authors believe that the following developments have the potential to provide additional tools to the pain practitioner.
Because there are different mechanisms involved in PAP, a systematic method for classifying patients is needed. Based on current understanding of the disorder, a phenotypic model may be helpful. For example, classifying patients by diagnostic category (ie, RLP versus PLP), referral patterns, descriptors, associated signs and symptoms, as well as chronicity may help determine which mechanisms predominate and guide therapy. These phenotype therapies would not necessarily be multimodal since they would be individualized to each patient’s predominant pain mechanism. Future studies could be designed to elucidate how phenotypic groups respond to different mechanism-specific therapies.
Controlled studies exploring multimodal treatments and preventative measures may also be on the horizon. Gilron and colleagues have described similar studies for the use of preemptive multimodal analgesics in the perioperative period for patients undergoing abdominal hysterectomy.141
Monoclonal antibody-based therapeutics have revolutionized the treatment of oncologic and inflammatory disorders, and hold promise in the treatment of chronic pain.142 For patients with PAP, antibody-based treatments could offer safer and more effective alternatives to currently available treatments. In addition to tumor necrosis factor alpha inhibitors, antibodies against several other pain-specific targets are currently under development. For example, anti–nerve growth factor antibodies have demonstrated Efficacy in the treatment of pain in patients with osteoarthritis and chronic low back pain.143,144 This may herald the advent of a new class of medications for the treatment of PAP.
Finally, though phenotypic classification of patients may be more applicable in the near term, preclinical studies have shown that a portion of individual variability in pain thresholds and susceptibility can be explained by differences (or mutations) in genotypes and gene expression.145,146 Costigan et al identified one single nucleotide polymorphism within KCNS1, the gene encoding a voltage-gated potassium channel, which is constitutively expressed in sensory neurons downregulated following nerve injury.147 In this study, six different cohorts of chronic pain patients to include two separate groups of lumbosacral radiculopathy subjects, women with post-mastectomy pain, PAP, and PLP, along with a control group of healthy adults, were tested for experimental pain. Collectively, these patients showed a significant increase in self-reported pain that was associated with a specific single nucleotide polymorphism of KCNS1. Further genotypic studies of this nature may help to identify individuals at higher risk for developing neuropathic pain after amputation who need aggressive early pain management to prevent the development of PAP.
Footnotes
Disclosure
The authors did not receive any grants, consulting fees, honorariums, support for travel, or costs associated with writing or editing this manuscript.
References
- 1.Padul PA, Friedmann LW. Acquired amputation and prostheses before the sixteenth century. Angiology. 1987;38(2):133–141. doi: 10.1177/000331978703800207. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell SW, Morehouse GR, Keen WW. Gunshot Wounds and other Injuries of Nerves. Philadelphia: JB Lippincott and Co; 1864. [DOI] [PubMed] [Google Scholar]
- 3.Henderson WR, Smythe GE. Phantom limbs. J Neurol Neurosurg Psychiatry. 1948;11:88–112. doi: 10.1136/jnnp.11.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ewalt JR, Randall GC, Morris H. The phantom limb. Pyschosom Med. 1947;9:118–123. doi: 10.1097/00006842-194703000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Woolf CJ. Pain: moving from symptom control toward mechanism-specific pharmacologic management. Ann Intern Med. 2004;140:441–451. doi: 10.7326/0003-4819-140-8-200404200-00010. [DOI] [PubMed] [Google Scholar]
- 6.Woolf CJ, Max MB. Mechanism-based pain diagnosis: issues for analgesic drug development. Anesthesiology. 2001;95:241–249. doi: 10.1097/00000542-200107000-00034. [DOI] [PubMed] [Google Scholar]
- 7.Owings MF, Kozak LJ. Ambulatory and inpatient procedures in the United States, 1996. Vital Health Stat. 1998;13(139):1–119. [PubMed] [Google Scholar]
- 8.Dillingham T, Pezzin L, MacKenzie E. Limb amputation and limb deficiencies: epidemiology and recent trends in the United States. South Med J. 2002;95:875–883. doi: 10.1097/00007611-200208000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Ephraim P, Wegener S, MacKenzie E, Dillingham T, Pezzin L. Phantom pain, residual limb pain, and back pain in amputees: results of a national survey. Arch Phys Med Rehabil. 2005;86:1910–1919. doi: 10.1016/j.apmr.2005.03.031. [DOI] [PubMed] [Google Scholar]
- 10.Sherman RA, Sherman CJ. Prevalence and characteristics of chronic phantom limb pain among American veterans: results of a trial survey. Am J Phys Med. 1983;62(5):227–238. [PubMed] [Google Scholar]
- 11.Jensen TS, Krebs B, Nielsen J, Rasmussen P. Immediate and long-term phantom limb pain in amputees. incidence, clinical characteristics and relationship to pre-amputation limb pain. Pain. 1985;21(3):267–278. doi: 10.1016/0304-3959(85)90090-9. [DOI] [PubMed] [Google Scholar]
- 12.Davis RW. Phantom sensation, phantom pain, and stump pain. Arch Phys Med Rehabil. 1993;74:79–91. [PubMed] [Google Scholar]
- 13.Jensen TS, Krebs B, Nielsen J, Rasmussen P. Phantom limb, phantom pain and stump pain in amputees during the first 6 months following limb amputation. Pain. 1983;17(3):243–256. doi: 10.1016/0304-3959(83)90097-0. [DOI] [PubMed] [Google Scholar]
- 14.Ehde DM, Czerniecki JM, Smith DG, et al. Chronic phantom sensations, phantom pain, residual limb pain, and other regional pain after lower limb amputation. Arch Phys Med Rehabil. 2000;81(8):1039–1044. doi: 10.1053/apmr.2000.7583. [DOI] [PubMed] [Google Scholar]
- 15.Schley MT, Wilms P, Toepfner S, et al. Painful and nonpainful phantom and stump sensations in acute traumatic amputees. J Trauma. 2008;65(4):858–864. doi: 10.1097/TA.0b013e31812eed9e. [DOI] [PubMed] [Google Scholar]
- 16.Montoya P, Larbig W, Grulke N, Flor H, Taub E, Birbaumer N. The relationship of phantom limb pain to other phantom limb phenomena in upper extremity amputees. Pain. 1997;72(1–2):87–93. doi: 10.1016/s0304-3959(97)00004-3. [DOI] [PubMed] [Google Scholar]
- 17.Berman JS, Birch R, Anand P. Pain following human brachial plexus injury with spinal cord root avulsion and the effect of surgery. Pain. 1998;75(2–3):199–207. doi: 10.1016/s0304-3959(97)00220-0. [DOI] [PubMed] [Google Scholar]
- 18.Hains BC, Waxman SG. Activated microglia contribute to the maintenance of chronic pain after spinal cord injury. J Neuroscience. 2006;26(16):4308–4317. doi: 10.1523/JNEUROSCI.0003-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hansen DM, Kehlet H, Gartner R. Phantom breast sensations are frequent after mastectomy. Dan Med Bull. 2011;58(4):A4259. [PubMed] [Google Scholar]
- 20.Bartels K, Cohen SP, Raja SN. Postamputation pain. In: Benzon H, Raja SN, Fishman SM, Liu SS, Cohen SP, editors. Essentials of Pain Medicine. 3rd ed. Philadelphia, PA: Elsevier Health; 2011. pp. 365–369. [Google Scholar]
- 21.Smith DG, Ehde DM, Legro M W, et al. Phantom limb, residual limb, and back pain after lower extremity amputations. Clin Orthop Relat Res. 1999;361:29–38. doi: 10.1097/00003086-199904000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007;106:591–614. doi: 10.1097/00000542-200703000-00024. [DOI] [PubMed] [Google Scholar]
- 23.Dyck PJ, Davies JL, Litchy WJ, et al. Longitudinal assessment of diabetic polyneuropathy using a composite score in the Rochester Diabetic Neuropathy Study cohort. Neurology. 1997;49:229–239. doi: 10.1212/wnl.49.1.229. [DOI] [PubMed] [Google Scholar]
- 24.Cheng WY, Jiang YD, Chuang LM, et al. Quantitative sensory testing and risk factors of diabetic sensory neuropathy. J Neurol. 1999;246:394–398. doi: 10.1007/s004150050370. [DOI] [PubMed] [Google Scholar]
- 25.Attal N, Brasseur L, Parker F, et al. Effects of gabapentin on the different components of peripheral and central neuropathic pain syndromes: a pilot study. Eur Neurol. 1998;40:191–200. doi: 10.1159/000007979. [DOI] [PubMed] [Google Scholar]
- 26.Eisenberg E, Alon N, Ishay A, et al. Lamotrigine in the treatment of painful diabetic neuropathy. Eur J Neurol. 1998;5:167–173. doi: 10.1046/j.1468-1331.1998.520167.x. [DOI] [PubMed] [Google Scholar]
- 27.Zaslansky R, Yarnitsky D. Clinical applications of quantitative sensory testing (QST) J Neurol Sci. 1998;153:215–238. doi: 10.1016/s0022-510x(97)00293-1. [DOI] [PubMed] [Google Scholar]
- 28.Ramachandran VS, Rogers-Ramachandran D, Stewart M. Perceptual correlates of massive cortical reorganization. Science. 1992;258(5085):1159–1160. doi: 10.1126/science.1439826. [DOI] [PubMed] [Google Scholar]
- 29.Kew JJ, Ridding MC, Rothwell JC, et al. Reorganization of cortical blood flow and transcranial magnetic stimulation maps in human subjects after upper limb amputation. J Neurophysiol. 1994;72(5):2517–2524. doi: 10.1152/jn.1994.72.5.2517. [DOI] [PubMed] [Google Scholar]
- 30.Giraux P, Sirigu A, Schneider F, Dubernard JM. Cortical reorganization in motor cortex after graft of both hands. Nat Neurosci. 2001;4(7):691–692. doi: 10.1038/89472. [DOI] [PubMed] [Google Scholar]
- 31.Roricht S, Meyer BU, Niehaus L, Brandt SA. Long-term reorganization of motor cortex outputs after arm amputation. Neurology. 1999;53(1):106–111. doi: 10.1212/wnl.53.1.106. [DOI] [PubMed] [Google Scholar]
- 32.Mercier C, Reilly KT, Vargas CD, Aballea A, Sirigu A. Mapping phantom movement representations in the motor cortex of amputees. Brain. 2006;129(8):2202–2210. doi: 10.1093/brain/awl180. [DOI] [PubMed] [Google Scholar]
- 33.Karl A, Birbaumer N, Lutzenberger W, Cohen LG, Flor H. Reorganization of motor and somatosensory cortex in upper extremity amputees with phantom limb pain. J Neurosci. 2001;21(10):3609–3618. doi: 10.1523/JNEUROSCI.21-10-03609.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lotze M, Flor H, Grodd W, Larbig W, Birbaumer N. Phantom movements and pain. An fMRI study in upper limb amputees. Brain. 2001;124(11):2268–2277. doi: 10.1093/brain/124.11.2268. [DOI] [PubMed] [Google Scholar]
- 35.Carlen PL, Wall PD, Nadvorna H, Steinbach T. Phantom limbs and related phenomena in recent traumatic amputations. Neurology. 1978;28(3):211–217. doi: 10.1212/wnl.28.3.211. [DOI] [PubMed] [Google Scholar]
- 36.Flor H, Nikolajsen L, Staehelin Jensen T. Phantom limb pain. A case of maladaptive CNS plasticity. Nat Rev Neurosci. 2006;7(11):873–881. doi: 10.1038/nrn1991. [DOI] [PubMed] [Google Scholar]
- 37.Iacono R P, Linford J, Sandyk R. Pain management after lower extremity amputation. Neurosurgery. 1987;20(3):496–500. doi: 10.1227/00006123-198703000-00027. [DOI] [PubMed] [Google Scholar]
- 38.Kroner K, Krebs B, Skov J, Jorgensen HS. Immediate and long-term phantom breast syndrome after mastectomy, incidence, clinical characteristics and relationship to pre-mastectomy breast pain. Pain. 1989;36(3):327–334. doi: 10.1016/0304-3959(89)90092-4. [DOI] [PubMed] [Google Scholar]
- 39.Cohen SP, Villena F, Mao J. Two unusual cases of postamputation pain from Operation Iraqi Freedom. J Trauma. 2007;62(3):759–761. doi: 10.1097/01.ta.0000235268.32690.8b. [DOI] [PubMed] [Google Scholar]
- 40.Schmidt A P, Takahashi ME, de Paula Posso ID. Phantom limb pain induced by spinal anesthesia. Clinics (Sao Paulo) 2005;60(3):263–264. doi: 10.1590/s1807-59322005000300014. [DOI] [PubMed] [Google Scholar]
- 41.Aydin MD, Cesur M, Aydin N, Alici H. Disappearance of phantom limb pain during caudaequina compression by spinal meningioma and gradual reactivation after decompression. Anesth Analg. 2005;101(4):1123–1126. doi: 10.1213/01.ANE.0000175768.11507.BC. [DOI] [PubMed] [Google Scholar]
- 42.Dellon AL, Mackinnon SE, Pestronk A. Implantation of sensory nerve into muscle: preliminary clinical and experimental observations on neuroma formation. Ann Plast Surg. 1984;12:30–40. doi: 10.1097/00000637-198401000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Carmel PW, Stein BM. Cell changes in sensory ganglia following cortex following proximal and distal nerve section in the monkey. J Comp Neurol. 1969;135:145–166. doi: 10.1002/cne.901350203. [DOI] [PubMed] [Google Scholar]
- 44.Liss AG, af Ekenstam FW, Wiberg M. Loss of neurons in the dorsal root ganglia after transection of a peripheral sensory nerve. Scand J Plast Reconstr Surg Hand Surg. 1996;30:1–6. doi: 10.3109/02844319609072397. [DOI] [PubMed] [Google Scholar]
- 45.Liss AG, Wiberg M. Loss of nerve endings in the spinal dorsal horn after a peripheral nerve injury. An anatomical study in Macacafascicularis monkeys. Eur J Neurosci. 1997;9:2187–2192. doi: 10.1111/j.1460-9568.1997.tb01385.x. [DOI] [PubMed] [Google Scholar]
- 46.Liss AG, Wiberg M. Loss of primary afferent nerve terminals in the brainstem after peripheral nerve transection: an anatomical study in monkeys. Anat Embryol. 1997;196:279–289. doi: 10.1007/s004290050097. [DOI] [PubMed] [Google Scholar]
- 47.Csillik B, Knyihar E, Rakic P. Transganglionic degenerative atrophy and regenerative proliferation in the rolando substance of the sensorimotor cortex of the primate spinal cord: discoupling and restoration of synaptic connectivity in the central nervous system after peripheral nerve lesions. Folia Morphol. 1982;30:189–193. [PubMed] [Google Scholar]
- 48.Calford MB, Tweedale R. Immediate expansion of receptive fields of neurons in area 3b of macaque monkeys after digit denervation. Somatosens Motor Res. 1991;8:249–260. doi: 10.3109/08990229109144748. [DOI] [PubMed] [Google Scholar]
- 49.Florence SL, Garraghty PE, Carlson M, Kaas JH. Sprouting of peripheral nerve axons in the spinal cord of monkeys. Brain Res. 1993;601:343–348. doi: 10.1016/0006-8993(93)91734-a. [DOI] [PubMed] [Google Scholar]
- 50.Zhang X, Ju G, Elde R, Hokfelt T. Effect of peripheral nerve cut on neuropeptides in dorsal root ganglia and the spinal cord of monkey with special reference to galanin. J Neurocytol. 1993;22:342–381. doi: 10.1007/BF01195558. [DOI] [PubMed] [Google Scholar]
- 51.Fischer J, Csillik B. Lectin binding: a genuine marker for transganglionic regulation of human primary sensory neurons. Neurosci Lett. 1985;54:263–267. doi: 10.1016/s0304-3940(85)80089-6. [DOI] [PubMed] [Google Scholar]
- 52.Hunt SP, Rossor MN, Emson PC, Clement-Jones V. Substance P and enkephalins in spinal cord after limb amputation. Lancet. 1982;1(8279):1023. doi: 10.1016/s0140-6736(82)92025-6. [DOI] [PubMed] [Google Scholar]
- 53.Ohara S, Takahashi H, Kato M, Nakamura T, Tsukada M. Transganglionic gracile response following limb amputation in man. Acta Neuropathol. 2000;100:469–474. doi: 10.1007/s004010000210. [DOI] [PubMed] [Google Scholar]
- 54.Devor M, Wall PD. Reorganisation of spinal cord sensory map after peripheral nerve injury. Nature. 1978;276(5683):75–76. doi: 10.1038/276075a0. [DOI] [PubMed] [Google Scholar]
- 55.Murphy JP, Anandaciva S. Phantom limb pain and spinal anaesthesia. Anaesthesia. 1984;39:188. doi: 10.1111/j.1365-2044.1984.tb09516.x. [DOI] [PubMed] [Google Scholar]
- 56.Rasmussen MR, Kitaoka HB, Patzer GL. Nonoperative treatment of plantar interdigital neuroma with a single corticosteroid injection. Clin Orthop. 1996;326:188–193. doi: 10.1097/00003086-199605000-00022. [DOI] [PubMed] [Google Scholar]
- 57.Nicholson B. Evaluation and treatment of central pain syndromes. Neurology. 2004;62(2):S30–S36. doi: 10.1212/wnl.62.5_suppl_2.s30. [DOI] [PubMed] [Google Scholar]
- 58.Wu H, Sultana R, Taylor KB, Szabo A. A prospective randomized double-blinded pilot study to examine the effect of botulinum toxin type A injection versus lidocaine/depomedrol injection on residual and phantom limb pain. Clin J Pain. 2012;28:108–112. doi: 10.1097/AJP.0b013e3182264fe9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kern U, Martin C, Scheicher S, Muller H. Effects of botulinum toxin type B on stump pain and involuntary movements of the stump. Am J Phys Med Rehabil. 2004;83(5):396–399. doi: 10.1097/01.phm.0000124444.32257.04. [DOI] [PubMed] [Google Scholar]
- 60.West M, Wu H. Pulsed radiofrequency ablation for the management of residual limb pain and phantom limb pain. Pain Practice. 2010;10(5):485–491. doi: 10.1111/j.1533-2500.2009.00353.x. [DOI] [PubMed] [Google Scholar]
- 61.Dahl E, Cohen SP. Perineural injection of etanercept as a treatment for postamputation pain. Clin J Pain. 2008;24(2):172–175. doi: 10.1097/AJP.0b013e31815b32c8. [DOI] [PubMed] [Google Scholar]
- 62.Cohen SP, Gambel JM, Raja SN, Galvagno S. The contribution of sympathetic mechanisms to postamputation phantom and residual limb pain: a pilot study. J Pain. 2011;12(8):859–867. doi: 10.1016/j.jpain.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 63.Casale R, Ceccherelli F, Labeeb AA, Biella GE. Phantom limb pain relief by contralateral myofascial injection with local anaesthetic in a placebo-controlled study: preliminary results. J Rehab Med. 2009;41(6):418–422. doi: 10.2340/16501977-0353. [DOI] [PubMed] [Google Scholar]
- 64.Bilevicuite-Ljungara I, Biellab G, Bellomib P, Sotgiub M. Contralateral treatment with lidocaine reduces spinal neuronal activity in mononeu-ropathic rat. Neurosci Lett. 2001;311(3):157–160. doi: 10.1016/s0304-3940(01)02154-1. [DOI] [PubMed] [Google Scholar]
- 65.Nikolajsen L, Hansen C, Nielsen J, Keller J, Arendt-Nielsen L, Jensen T. The effect of ketamine on phantom pain: a central neuropathic disorder maintained by peripheral input. Pain. 1996;67(1):69–77. doi: 10.1016/0304-3959(96)03080-1. [DOI] [PubMed] [Google Scholar]
- 66.Eichenberger U, Neff F, Sveticic G, et al. Chronic phantom limb pain: the effects of calcitonin, ketamine, and their combination on pain and sensory thresholds. Anesth Analg. 2008;106(4):1265–1273. doi: 10.1213/ane.0b013e3181685014. [DOI] [PubMed] [Google Scholar]
- 67.Abraham R, Marouani N, Weinbroum A. Dextromethorphan mitigates phantom pain in cancer amputees. Ann Surg Oncol. 2003;10(3):268–274. doi: 10.1245/aso.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 68.Maier C, Dertwinkel R, Mansourian N, et al. Efficacy of the NMDA receptor antagonist memantine in patients with chronic phantom limb pain-results of a randomized double-blinded, placebo-controlled trial. Pain. 2003;103(3):277–283. doi: 10.1016/S0304-3959(02)00456-6. [DOI] [PubMed] [Google Scholar]
- 69.Wiech K, Kiefer RT, Topfner S, et al. A placebo-controlled randomized crossover trial of the N-methyl-D-aspartic acid receptor antagonist, memantine, in patients with chronic phantom limb pain. Anesth Analg. 2004;98(2):408–413. doi: 10.1213/01.ANE.0000096002.53818.BD. [DOI] [PubMed] [Google Scholar]
- 70.Schwenkreis P, Maier C, Pleger B, et al. NMDA-mediated mechanisms in cortical excitability changes after limb amputation. Acta Neurol Scand. 2003;108(3):179–184. doi: 10.1034/j.1600-0404.2003.00114.x. [DOI] [PubMed] [Google Scholar]
- 71.Schley M, Topfner S, Wiech K, et al. Continuous brachial plexus blockade in combination with the NMDA receptor antagonist memantine prevents phantom pain in acute traumatic upper limb amputees. Eur J Pain. 2007;11(3):299–308. doi: 10.1016/j.ejpain.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 72.Huse E, Larbig W, Flor H, Birbaumer N. The effect of opioids on phantom limb pain and cortical reorganization. Pain. 2001;90(1–2):47–55. doi: 10.1016/s0304-3959(00)00385-7. [DOI] [PubMed] [Google Scholar]
- 73.Wu C, Tella P, Staats P, et al. Analgesic effects of intravenous lidocaine and morphine on postamputation pain. Anesthesiology. 2002;96(2):841–848. doi: 10.1097/00000542-200204000-00010. [DOI] [PubMed] [Google Scholar]
- 74.Wu CL, Agarwal S, Tella PK, et al. Morphine versus mexiletine for treatment of postamputation pain: a randomized, placebo controlled, crossover trial. Anesthesiology. 2008;109(2):289–296. doi: 10.1097/ALN.0b013e31817f4523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wilder-Smith CH, Hill LT, Laurent S. Postamputation pain and sensory changes in treatment-naive patients: characteristics and responses to treatment with tramadol, amitriptyline, and placebo. Anesthesiology. 2005;103(3):619–628. doi: 10.1097/00000542-200509000-00027. [DOI] [PubMed] [Google Scholar]
- 76.Bone M, Critchley P, Buggy D. Gabapentin in postamputation phantom limb pain: a randomized, double-blind, placebo-controlled, cross-over study. Reg Anesth Pain Med. 2002;27(5):481–486. doi: 10.1053/rapm.2002.35169. [DOI] [PubMed] [Google Scholar]
- 77.Smith D, Ehde D, Hanley M, et al. Efficacy of gabapentin in treating chronic phantom limb and residual limb pain. J Rehabil Res Dev. 2005;42(5):645–654. doi: 10.1682/jrrd.2005.05.0082. [DOI] [PubMed] [Google Scholar]
- 78.Azria M. Possible mechanisms of the analgesic action of calcitonin. Bone. 2002;30(5):80S–83S. doi: 10.1016/s8756-3282(02)00701-9. [DOI] [PubMed] [Google Scholar]
- 79.Jaeger H, Maier C. Calcitonin in phantom limb pain: a doubleblind study. Pain. 1992;48:21–27. doi: 10.1016/0304-3959(92)90127-W. [DOI] [PubMed] [Google Scholar]
- 80.Robinson L, Czerniecki J, Ehde D, et al. Trial of amitriptyline for relief of pain in amputees: results of a randomized controlled study. Arch Phys Med Rehabil. 2004;85(1):1–6. doi: 10.1016/s0003-9993(03)00476-3. [DOI] [PubMed] [Google Scholar]
- 81.Rickard JA. Effects of Hypnosis in the Treatment of Residual Stump and Phantom Limb Pain [dissertation] Pullman, WA: Washington State University; 2004. [Google Scholar]
- 82.Beaumont G, Mercier C, Michon PE, Malouin F, Jackson PL. Decreasing phantom limb pain through observation of action and imagery: a case series. Pain Med. 2011;12(2):289–299. doi: 10.1111/j.1526-4637.2010.01048.x. [DOI] [PubMed] [Google Scholar]
- 83.Harden RN, Houle TT, Green S, et al. Biofeedback in the treatment of phantom limb pain: a time-series analysis. Appl Psychophysiol Biofeedback. 2005;30:83–93. doi: 10.1007/s10484-005-2177-8. [DOI] [PubMed] [Google Scholar]
- 84.Wetering EJ, Lemmens KM, Nieboer AP, Huijsman R. Cognitive and behavioral interventions for the management of chronic neuropathic pain in adults – a systematic review. Eur J Pain. 2010;14(7):670–681. doi: 10.1016/j.ejpain.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 85.Prakash SP, Golwala P. Phantom headache: pain-memory-emotion hypothesis for chronic daily headache? J Headache Pain. 2011;12(3):281–286. doi: 10.1007/s10194-011-0307-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tichelaar Y V, Geertzen JH, Keizer D, Van Wilgen C P. Mirror box therapy added to cognitive behavioural therapy in three chronic complex regional pain syndrome type I patients: a pilot study. Int J Rehabil Res. 2007;30(2):181–188. doi: 10.1097/MRR.0b013e32813a2e4b. [DOI] [PubMed] [Google Scholar]
- 87.Department of Veterans Affairs Cognitive behavior therapy (CBT) and mirror training for phantom limb pain ClinicalTrialsgov [website on the Internet] Bethesda, MD: US National Library of Medicine; Available from: http://www.clinicaltrials.gov/ct2/show/study/NCT00731614NLM identifier: NCT00731614. Accessed December 7, 2012 [Google Scholar]
- 88.Flor H, Diers M, Christmann C, Koeppe C. Mirror illusions of phantom hand movements brain activity mapped by fMRI. Neuro Image. 2006;31:S159. [Google Scholar]
- 89.Flor H, Elbert T, Knecht S, et al. Phantom-limb pain as a perceptual correlate of cortical reorganization following arm amputation. Nature. 1995;375(6531):482–484. doi: 10.1038/375482a0. [DOI] [PubMed] [Google Scholar]
- 90.Ramachandran VS, Altschuler EL. The use of visual feedback, in particular mirror visual feedback, in restoring brain function. Brain. 2009;132:1693–1710. doi: 10.1093/brain/awp135. [DOI] [PubMed] [Google Scholar]
- 91.Mercier C, Sirigu A. Training with virtual visual feedback to alleviate phantom limb pain. Neurorehabil Neural Repair. 2009;23:587–594. doi: 10.1177/1545968308328717. [DOI] [PubMed] [Google Scholar]
- 92.Cole J, Crowle S, Austwick G, et al. Exploratory findings with virtual reality for phantom limb pain; from stump motion to agency and analgesia. Disabil Rehabil. 2009;31(10):846–854. doi: 10.1080/09638280802355197. [DOI] [PubMed] [Google Scholar]
- 93.Chan BL, Witt R, Charrow AP, et al. Mirror therapy for phantom limb pain. N Engl J Med. 2007;357:2206–2207. doi: 10.1056/NEJMc071927. [DOI] [PubMed] [Google Scholar]
- 94.Garry MI, Loftus A, Summers JJ. Mirror, mirror on the wall: viewing a mirror reflection of unilateral hand movements facilitates ipsilateral M1 excitability. Exp Brain Res. 2005;163:118–122. doi: 10.1007/s00221-005-2226-9. [DOI] [PubMed] [Google Scholar]
- 95.Hanling SR, Wallace SC, Hollenbeck KJ, et al. Preamputation mirror therapy may prevent development of phantom limb pain: a case series. Anesth Analg. 2010;110:611–614. doi: 10.1213/ANE.0b013e3181b845b0. [DOI] [PubMed] [Google Scholar]
- 96.Mobbs RJ, Nair S, Blum P. Peripheral nerve stimulation for the treatment of chronic pain. J Clin Neurosci. 2007;14:216–223. doi: 10.1016/j.jocn.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 97.Rauck RL, Kapural L, Cohen SP, et al. Peripheral nerve stimulation for the treatment of postamputation pain – a case report. Pain Pract. 2012;12(8):649–655. doi: 10.1111/j.1533-2500.2012.00552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nielson KD, Adams JE, Hosobuchi Y. Phantom limb pain: treatment with dorsal column stimulation. J Neurosurg. 1975;42:301–307. doi: 10.3171/jns.1975.42.3.0301. [DOI] [PubMed] [Google Scholar]
- 99.Krainick JU, Thoden U, Riechert T. Pain reduction in amputees by long-term spinal cord stimulation: long term follow-up study over 5 years. J Neurosurg. 1980;52:346–350. doi: 10.3171/jns.1980.52.3.0346. [DOI] [PubMed] [Google Scholar]
- 100.Hunt WE, Goodman JH, Bingham WG. Stimulation of the dorsal spinal cord for treatment of intractable pain: a preliminary report. Surg Neurol. 1975;4:153–156. [PubMed] [Google Scholar]
- 101.Miles J, Lipton S. Phantom limb pain treated by electrical stimulation. Pain. 1978;5:373–382. doi: 10.1016/0304-3959(78)90006-4. [DOI] [PubMed] [Google Scholar]
- 102.Sanchez-Ledesma MJ, Garcia-March G, Diaz-Cascajo P, Gomez-Moreta J, Broseta J. Spinal cord stimulation in deafferentation pain. Stereotact Funct Neurosurg. 1989;53:40–45. doi: 10.1159/000099520. [DOI] [PubMed] [Google Scholar]
- 103.Kumar K, Toth C, Nath R, Laing P. Epidural spinal cord stimulation for treatment of chronic pain – some predictors of success. A 15-year experience. Surg Neurol. 1998;50:110–121. doi: 10.1016/s0090-3019(98)00012-3. [DOI] [PubMed] [Google Scholar]
- 104.Broggi G, Servello D, Dones I, Carbone G. Italian multicenter study on pain treatment with epidural spinal cord stimulation. Stereotact Funct Neurosurg. 1994;62:273–278. doi: 10.1159/000098632. [DOI] [PubMed] [Google Scholar]
- 105.Indication and limitations of coverage and/or medical necessity. Centers for Medicare and Medicaid Website http://www.findacode.com/medicare/policies-guidelines/display-medicare-info.php?type=LCD&type_id=26741Accessed October 30, 2012
- 106.Nguyen JP, Lefaucheur JP, Raoul S, et al. Motor cortex stimulation for the treatment of neuropathic pain. In: Krames ES, Peckham PH, Rezai AR, editors. Neuromodulation. 1st ed. Amsterdam: Elsevier Science; 2009. pp. 515–526. [Google Scholar]
- 107.Rasche D, Rinaldi PC, Young RF, Tronnier VM. Deep brain stimulation for the treatment of various chronic pain syndromes. Neurosurg Focus. 2006;21(6):E8. doi: 10.3171/foc.2006.21.6.10. [DOI] [PubMed] [Google Scholar]
- 108.Katayama Y, Yamamoto T, Kobayashi K, Kasai M, Oshima H, Fukaya C. Motor cortex stimulation for phantom limb pain: comprehensive therapy with spinal cord and thalamic stimulation. Stereotact Funct Neurosurg. 2001;77(1–4):159–162. doi: 10.1159/000064593. [DOI] [PubMed] [Google Scholar]
- 109.Sol JCH, Casaux J, Roux FE, et al. Chronic motor cortex stimulation for phantom limb pain: correlations between pain relief and functional imaging studies. Stereotact Funct Neurosurg. 2001;77:172–176. doi: 10.1159/000064616. [DOI] [PubMed] [Google Scholar]
- 110.Bittar RG, Otero S, Carter H, Aziz TZ. Deep brain stimulation for phantom limb pain. J Clin Neurosci. 2005;12(4):399–404. doi: 10.1016/j.jocn.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 111.McAuley J, Groningen RV, Green C.Spinal cord stimulation for intractable pain following limb amputation NeuromodulationEpub September252012 [DOI] [PubMed]
- 112.Long DM. Electrical stimulation for relief of pain from chronic nerve injury. J Neurosurg. 1973;39:718–722. doi: 10.3171/jns.1973.39.6.0718. [DOI] [PubMed] [Google Scholar]
- 113.Nashold BS, Jr, Goldner JL, Mullen JB, Bright DS. Long-term pain control by direct peripheral-nerve stimulation. J Bone Joint Surg Am. 1982;64:1–10. [PubMed] [Google Scholar]
- 114.Campbell JN, Long DM. Peripheral nerve stimulation in the treatment of intractable pain. J Neurosurg. 1976;45:692–699. doi: 10.3171/jns.1976.45.6.0692. [DOI] [PubMed] [Google Scholar]
- 115.Potter BK, Burns TC, Lacap A P, Granville RR, Grajewski DA. Heterotopic ossification following traumatic and combat-related amputations: prevalence, risk factors, and preliminary results of excision. J Bone Joint Surg. 2007;89:476–485. doi: 10.2106/JBJS.F.00412. [DOI] [PubMed] [Google Scholar]
- 116.Herta F. Phantom-limb pain: characteristics, causes, and treatment. Lancet Neurol. 2002;1:182–189. doi: 10.1016/s1474-4422(02)00074-1. [DOI] [PubMed] [Google Scholar]
- 117.Sturm V, Kroger M, Penzholz H. Problems of peripheral nerve surgery in amputation stump pain and phantom limbs. Chirurg. 1975;46:389–391. [PubMed] [Google Scholar]
- 118.Dellon AL, Mackinnon SE. Treatment of the painful neuroma by neuroma resection and muscle implantation. Plast Reconstr Surg. 1986;77:427–438. doi: 10.1097/00006534-198603000-00016. [DOI] [PubMed] [Google Scholar]
- 119.Burchiel KJ, Johans TJ, Ochoa J. The surgical treatment of painful traumatic neuromas. J Neurosurg. 1993;78:714–719. doi: 10.3171/jns.1993.78.5.0714. [DOI] [PubMed] [Google Scholar]
- 120.Ducic I, Mesbahi AN, Attinger CE, Graw K. The role of peripheral nerve surgery in the treatment of chronic pain associated with amputation stumps. Plast Reconstr Surg. 2008;121:908–914. doi: 10.1097/01.prs.0000299281.57480.77. [DOI] [PubMed] [Google Scholar]
- 121.Prantl L, Schreml S, Heine N, Eisenmann-Klein M, Angele P. Surgical treatment of chronic phantom limb sensation and limb pain after lower limb amputation. Plast Reconstr Surg. 2006;118:1562–1572. doi: 10.1097/01.prs.0000233048.15879.0e. [DOI] [PubMed] [Google Scholar]
- 122.Woolf CJ, Chong MS. Preemptive analgesia: treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg. 1993;77:362–379. doi: 10.1213/00000539-199377020-00026. [DOI] [PubMed] [Google Scholar]
- 123.Halbert J, Crotty M, Cameron ID. Evidence for the optimal management of acute and chronic phantom limb pain. A systematic review. Clin J Pain. 2002;18:84–92. doi: 10.1097/00002508-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 124.Bach S, Noreng MF, Tjellden NU. Phantom limb pain in amputees during the first 12 months following limb amputation, after preoperative lumbar epidural blockade. Pain. 1988;33:297–301. doi: 10.1016/0304-3959(88)90288-6. [DOI] [PubMed] [Google Scholar]
- 125.Jahangiri M, Jayatunga A P, Bradley JW, Dark CH. Prevention of phantom pain after major lower limb amputation by epidural infusion of diamorphine, clonidine and bupivacaine. Ann R Coll Surg Engl. 1994;76(5):324–326. [PMC free article] [PubMed] [Google Scholar]
- 126.Nikolajsen L, Ilkjaer S, Christensen JH, Kroner K, Jensen TS. Randomised trial of epidural bupivacaine and morphine in prevention of stump and phantom pain in lower-limb amputation. Lancet. 1997;350(9088):1353–1357. doi: 10.1016/S0140-6736(97)06315-0. [DOI] [PubMed] [Google Scholar]
- 127.Elizaga AM, Smith DG, Sharar SR, et al. Continuous regional analgesia by intraneural block: effect on postoperative opioid requirements and phantom limb pain following amputation. J Rehabil Res Dev. 1994;31:179–187. [PubMed] [Google Scholar]
- 128.Finsen V, Persen L, Lovlien M, et al. Transcutaneous electrical nerve stimulation after major amputation. J Bone Joint Surg Br. 1988;70:109–112. doi: 10.1302/0301-620X.70B1.3257494. [DOI] [PubMed] [Google Scholar]
- 129.Fisher A, Meller Y. Continuous postoperative regional analgesia by nerve sheath block for amputation surgery: a pilot study. Anesth Analg. 1991;72:300–303. doi: 10.1213/00000539-199103000-00004. [DOI] [PubMed] [Google Scholar]
- 130.Pinzur MS, Garla PG, Pluth T, Vrbos L. Continuous postoperative infusion of a regional anesthetic after an amputation of the lower extremity. A randomized clinical trial. J Bone Joint Surg Am. 1996;78:1501–1505. doi: 10.2106/00004623-199610000-00007. [DOI] [PubMed] [Google Scholar]
- 131.Jadad AR, Moore A, Carroll D, et al. Assessing the quality of reports of randomised clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 132.Schug SA, Burrell R, Payne J, Tester P. Pre-emptive epidural analgesia may prevent phantom limb pain. Reg Anesth. 1995;20:256. [PubMed] [Google Scholar]
- 133.Lambert AW, Dashfeld AK, Cosgrove C, Wilkins DC, Walker AJ, Ashley S. Randomized prospective study comparing preoperative epidural and intraoperative perineural analgesia for the prevention of postoperative stump and phantom limb pain following major amputation. Reg Anesth Pain Med. 2001;26(4):316–321. doi: 10.1053/rapm.2001.23934. [DOI] [PubMed] [Google Scholar]
- 134.Wilson JA, Nimmo AF, Fleetwood-Walker SM, Colvin LA. A randomised double blind trial of the effect of pre-emptive epidural ketamine on persistent pain after lower limb amputation. Pain. 2008;135:108–118. doi: 10.1016/j.pain.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 135.Karanikolas M, Aretha D, Tsolakis I, et al. Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency: a prospective, randomized, clinical trial. Anesthesiology. 2011;114(5):1144–1154. doi: 10.1097/ALN.0b013e31820fc7d2. [DOI] [PubMed] [Google Scholar]
- 136.Nikolajsen L, Ilkjaer S, Kroner K, Christensen JH, Jensen TS. The influence of preamputation pain on postamputation stump and phantom pain. Pain. 1997;72:393–405. doi: 10.1016/s0304-3959(97)00061-4. [DOI] [PubMed] [Google Scholar]
- 137.Borghi B, D’Addabbo M, White P F, et al. The use of prolonged peripheral neural blockade after lower extremity amputation: the effect on symptoms associated with phantom limb syndrome. Anesth Analg. 2010;111(5):1308–1315. doi: 10.1213/ANE.0b013e3181f4e848. [DOI] [PubMed] [Google Scholar]
- 138.Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010;85(3):S3–S14. doi: 10.4065/mcp.2009.0649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Nikolajsen L, Finnerup NB, Kramp S, Vimtrup AS, Keller J, Jensen TS. A randomized study of the effects of gabapentin on postamputation pain. Anesthesiology. 2006;105(5):1008–1015. doi: 10.1097/00000542-200611000-00023. [DOI] [PubMed] [Google Scholar]
- 140.Finsen V, Persen L, Løvlien M, Veslegaard EK, Simensen M, Gåsvann AK, Benum P. Transcutaneous electrical nerve stimulation after major amputation. J Bone Joint Surg Br. 1988;70(1):109–112. doi: 10.1302/0301-620X.70B1.3257494. [DOI] [PubMed] [Google Scholar]
- 141.Gilron I, Orr E, Tu D, O’Neill J P, Zamora JE, Bell AC. A placebo-controlled randomized clinical trial of perioperative administration of gabapentin, rofecoxib and their combination for spontaneous and movement-evoked pain after abdominal hysterectomy. Pain. 2005;113(1–2):191–200. doi: 10.1016/j.pain.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 142.Chessell IP, Dudley A, Billinton A. Biologics: the next generation of analgesic drugs? Drug Discov Today. 2012;17(15):875–879. doi: 10.1016/j.drudis.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 143.Lane NE, Schnitzer TJ, Birbara CA, et al. Tanezumab for the treatment of pain from osteoarthritis of the knee. N Engl J Med. 2010;363:1521–1531. doi: 10.1056/NEJMoa0901510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Katz N, Borenstein DG, Birbara C, et al. Efficacy and safety of tanezumab in the treatment of chronic low back pain. Pain. 2011;152(10):2248–2258. doi: 10.1016/j.pain.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 145.Nielsen CS, Price DD, Vassend O, Stubhaug A, Harris JR. Characterizing individual differences in heat-pain sensitivity. Pain. 2005;119:65–74. doi: 10.1016/j.pain.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 146.Foulkes T, Wood JN. Pain genes. PLoS Genet. 2008;4(7):e1000086. doi: 10.1371/journal.pgen.1000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Costigan M, Belfer I, Griffin RS, et al. Multiple chronic pain states are associated with a common amino acid-changing allele in KCNS1. Brain. 2010;133:2519–2527. doi: 10.1093/brain/awq195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Katsuly-Liapis I, Georgakis P, Tierry C. Preemptive extradural analgesia reduces the incidence of phantom pain in lower limb amputees [abstract] Br J Anaesth. 1996;76:125. [Google Scholar]