Abstract
Objectives
Appropriate use of cranial computed tomography (CT) scanning in patients with mild blunt head trauma and pre-injury anticoagulant or antiplatelet use is unknown. The objectives of this study were: 1) to identify risk factors for immediate traumatic intracranial hemorrhage (tICH) in patients with mild head trauma and preinjury warfarin or clopidogrel use, and 2) to derive a clinical prediction rule to identify patients at low risk for immediate tICH.
Methods
This was a prospective, observational study at two trauma centers and four community hospitals that enrolled adult emergency department (ED) patients with mild blunt head trauma (initial ED Glasgow Coma Scale score 13 to 15) and pre-injury warfarin or clopidogrel use. The primary outcome measure was immediate tICH, defined as the presence of ICH or contusion on the initial cranial CT. Risk for immediate tICH was analyzed in eleven independent predictor variables. Clinical prediction rules were derived with both binary recursive partitioning and multivariable logistic regression.
Results
A total of 982 patients with a mean age of 75.4 years (SD ±12.6 years) were included in the analysis. Sixty patients (6.1%; 95% CI = 4.7% to 7.8%) had immediate tICH. History of vomiting (relative risk [RR] 3.53; 95% CI = 1.80 to 6.94), abnormal mental status (RR 2.85; 95% CI = 1.65 to 4.92), clopidogrel use (RR 2.52; 95% CI = 1.55 to 4.10), and headache (RR 1.81; 95% CI = 1.11 to 2.96) were associated with an increased risk for immediate tICH. Both binary recursive partitioning and multivariable logistic regression were unable to derive a clinical prediction model that identified a subset of patients at low risk for immediate tICH.
Conclusions
While several risk factors for immediate tICH were identified, the authors were unable to identify a subset of patients with mild head trauma and pre-injury warfarin or clopidogrel use who are at low risk for immediate tICH. Thus, the recommendation is for urgent and liberal cranial CT imaging in this patient population, even in the absence of clinical findings.
INTRODUCTION
Each year, traumatic brain injury (TBI) accounts for an estimated 1.4 million emergency department (ED) visits, 275,000 hospitalizations, and 52,000 deaths in the United States, at an estimated cost of 60 billion dollars.1 With an aging population, older adults with pre-injury anticoagulant or antiplatelet use represent an increasing proportion of TBI patients evaluated in the ED.2 These patients could be well-appearing and have low-impact mechanisms of injury, such as ground level falls,3,4 yet frequently have life-threatening traumatic intracranial hemorrhage (tICH) requiring neurosurgical interventions and specialized critical care.5,6
Thus, emergency physicians (EPs) are challenged with identifying which patients with head trauma and pre-injury anticoagulant or antiplatelet use are at high risk for acute tICH and require immediate cranial computed tomography (CT) imaging. Clinical prediction rules based on large, prospective studies accurately identify patients with mild TBI who are at very low risk for tICH (sensitivity range 83% to 100%) and neurosurgical lesions (sensitivity 100%).7-9 These studies, however, excluded or had very few patients with pre-injury anticoagulant or antiplatelet use.
Current mild TBI guidelines for patients with pre-injury anticoagulant or antiplatelet use are largely based on small, retrospective studies that suggest an increased risk for tICH following blunt head trauma.10-12 For patients with pre-injury anticoagulant use and head trauma, guidelines vary from liberal imaging (cranial CT regardless of loss of consciousness [LOC] or amnesia)13 to more limited imaging (cranial CT provided the patient sustain LOC or amnesia).14 For patients with pre-injury antiplatelet use and head trauma, current guidelines do not list antiplatelet medications as a risk factor for tICH.13,15 Thus, confusion exists regarding the appropriate utilization of cranial CT in patients with blunt head trauma and anticoagulant or antiplatelet use.
The objective of this study was to prospectively derive a clinical prediction rule to identify adult patients with mild head injury and pre-injury warfarin or clopidogrel use at low risk for tICH. This study represents a secondary aim of a larger prospective study evaluating the prevalence and incidence of immediate and delayed tICH in this patient population.16
METHODS
Study Design
This was a prospective, observational, multicenter study conducted at two trauma centers and four community hospitals in northern California. The study was approved by the institutional review boards at all sites with an alteration of informed consent. The sponsors of the study had no role in study design, data collection and analysis, or manuscript preparation. The corresponding author had full access to all the data and had final responsibility for the decision to submit for publication.
Study Setting and Population
Consecutive adult (≥ 18 years old) ED patients with pre-injury warfarin or clopidogrel use (within the prior seven days) and mild blunt head trauma (initial ED Glasgow Coma Scale [GCS] score 13 to 15) were enrolled. We defined blunt head trauma as any blunt head injury regardless of LOC or amnesia. Patients who did not receive cranial CT scans during the index ED visit were excluded from the primary analysis. We also excluded patients with known injuries transferred from outside facilities.
Study Protocol
The treating ED faculty physicians completed standardized questionnaires prior to cranial CT imaging. All physicians participating in the study received an explanation of the questionnaire with definitions of each criterion. Items in the questionnaire were based on a review of the literature on minor head trauma, and included age, mechanism of injury (ground level fall versus non-ground level fall), warfarin use, clopidogrel use, concomitant aspirin use, headache, vomiting, LOC or amnesia, drug or alcohol intoxication, physical evidence of trauma above the clavicles, and abnormal mental status. A ground level fall was defined as a fall from standing height or less. Headache was defined as the presence of any head pain after injury. Vomiting was defined as any post-injury emesis. LOC or amnesia was defined as witnessed LOC or failure of the patient to recall the events of the injury. Drug or alcohol intoxication was defined as clinician impression of intoxication based on history, physical exam, or laboratory testing. Physical evidence of trauma above the clavicles was defined as any external injury to the face, neck, or scalp, and included abrasions, lacerations, contusions and hematomas, or fractures. An abnormal mental status was defined as an initial ED GCS score less than 15. Patients with a GCS score less than 15 but not differing from baseline (e.g., history of dementia) were not considered to have an abnormal mental status.
Cranial CT imaging and hospital admission were at the discretion of the patients’ treating physicians. Electronic medical records were reviewed in a standardized fashion by research coordinators and site investigators to assess CT scan results, ED disposition, and hospital course.
At each site, approximately 10% of patients (non-randomly selected) had a separate, independent faculty physician assessment that was masked to and completed within 60 minutes of the initial assessment to evaluate the reliability of pre-selected clinical variables. Data on patients eligible but not enrolled during ED evaluation were abstracted from their medical records to assess for enrollment bias.
Outcomes
The primary outcome measure was the presence of immediate tICH (defined as any ICH or contusion) as interpreted by the staff neuroradiologist on initial ED cranial CT. The patient was considered to have tICH if the radiology report was consistent with tICH. Patients with delayed tICH (initial normal CT but with a repeat CT consistent with tICH) were not considered to meet the primary outcome measure. The secondary outcome measure was the presence of neurosurgical intervention, which was defined as the use of intracranial pressure monitor or brain tissue oxygen probe, placement of burr hole, craniotomy/craniectomy, intraventricular catheter, subdural drain, or the use of mannitol or hypertonic saline.
Data Analysis
Data were compared using STATA for Windows, Rel. 11.0 (STATA Corp., College Station, TX). Normally distributed continuous data were reported as the mean with standard deviations (±SDs), and ordinal or non-normally distributed continuous data described as the median with interquartile (25% to 75%) ranges (IQR). Proportions and relative risks are presented with 95% confidence intervals (CI).
Eleven independent predictor variables (age 65 years or older, warfarin use, clopidogrel use, concomitant aspirin use, non-ground level fall mechanism of injury, headache, vomiting, LOC or amnesia, drug or alcohol intoxication, evidence of trauma above the clavicles, abnormal mental status), defined a priori, underwent bivariate testing with chi-square or Fisher’s exact test (in instances of small cell size). We used a standard model building approach as candidate variables predicting immediate tICH (threshold p < 0.20) were entered into a multivariable analysis using both binary recursive partitioning and logistic regression. Binary recursive partitioning was conducted with Classification and Regression Trees (CART) software (Salford systems, San Diego, CA). We used the Gini splitting function in CART and set the misclassification costs for missing a tICH at 100:1 (relative cost of 100 for misclassifying one patient with immediate tICH to that of misclassifying one patient without tICH). Logistic regression was conducted with a random-effects model to account for random variation. Model fit was tested using the Hosmer-Lemeshow goodness-of-fit test.17 Adjusted variables that were significant in the regression model (p < 0.05) were included in the clinical prediction rule. Derived prediction rules were validated using internal cross validation for the recursive partitioning model and bootstrap validation for the logistic regression model. We calculated the sensitivity, specificity, and positive and negative predictive values (PPV and NPV) with 95% CIs for both derived models. Inter-rater reliability of independent variables recorded by initial and second physicians are reported as the kappa coefficient and percent agreement.
RESULTS
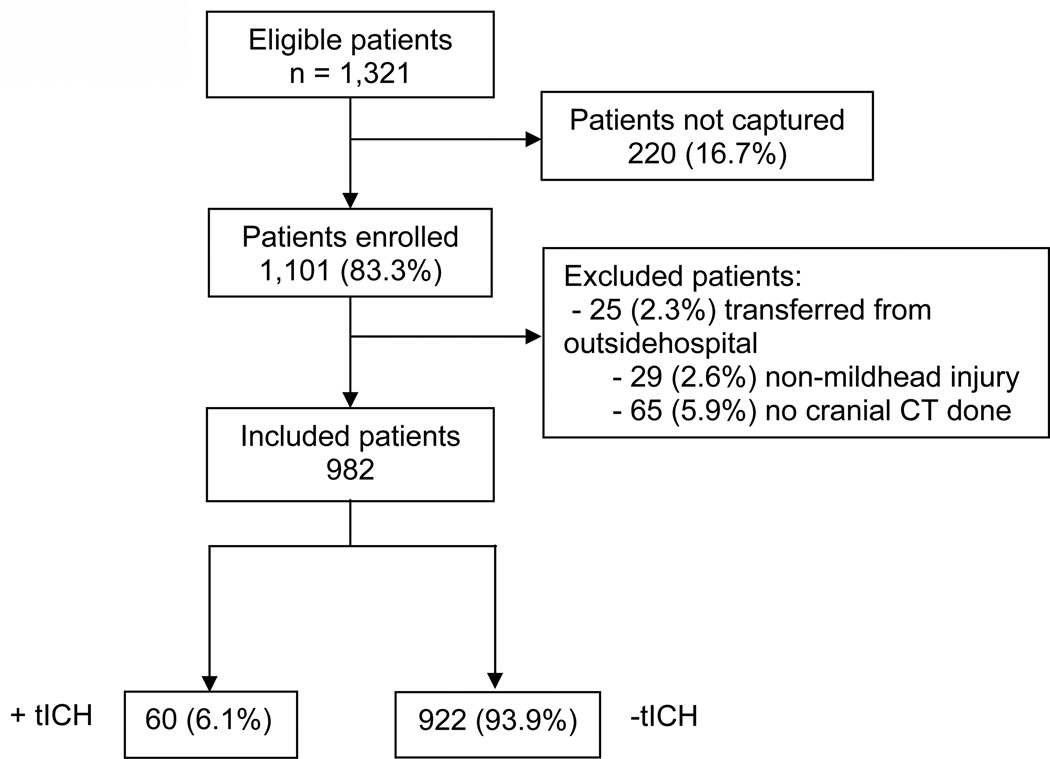
Between April 2009 and January 2011, 1101 patients were enrolled (83.3% of all eligible patients) (Figure 1). Comparison of patients enrolled and those eligible but not enrolled demonstrated similar characteristics (age, sex, medication use, ED cranial CT, and hospital admission) and outcomes (immediate tICH, neurosurgical intervention, and in-hospital mortality). Overall, 119 patients were excluded from analysis (25 transferred patients, 29 patients with non-mild head trauma, and 65 patients without cranial CT imaging at index ED visit), leaving 982 patients for data analysis.
Figure 1.
Flow of Patients in the Study
CT = computed tomography; tICH = traumatic intracranial hemorrhage
The mean age in the included cohort was 75.4 years (SD ± 12.6 years) and 464 patients (47.3%) were male. The majority of patients sustained ground level falls (83.6%), were taking warfarin (72.7%), did not sustain LOC or amnesia (81.0%), had evidence of trauma above the clavicles (70.9%), and had normal mental status (89.5%). See Table 1 for additional characteristics of the study population.
Table 1.
Patient Characteristics
| Characteristic | n (%) (N=982) |
|---|---|
| Demographics | |
| Age, mean (SD), y | 75.4 (12.6) |
| Male sex | 464 (47.3) |
| Mechanism of injury | |
| Ground level fall | 821 (83.6) |
| Fall from height | 36 (3.7) |
| MVC, < 35 miles per hour | 15 (1.5) |
| MVC, ≥ 35 miles per hour | 23 (2.3) |
| MVC, unknown speed | 8 (0.8) |
| Pedestrian struck by automobile | 4 (0.4) |
| Bicyclist struck by automobile | 4 (0.4) |
| Direct blow | 51 (5.2) |
| Unknown mechanism | 15 (1.5) |
| Other mechanism | 5 (0.5) |
| Medication use* | |
| Warfarin use | 714 (72.7) |
| Clopidogrel use | 279 (28.4) |
| Concomitant aspirin use | 45 (4.6) |
| Clinical history | |
| Vomiting | 41 (4.2) |
| Headache | 349 (35.5) |
| Loss of consciousness or amnesia | 187 (19.0) |
| Physical exam | |
| Alcohol intoxication | 34 (3.5) |
| Any evidence of trauma above the clavicles | 696 (70.9) |
| Trauma to face | 367 (37.4) |
| Trauma to neck | 33 (3.4) |
| Basilar skull fracture | 2 (0.2) |
| Scalp abrasion | 149 (15.2) |
| Scalp contusion | 292 (29.5) |
| Scalp laceration | 170 (17.3) |
| Normal mental status (GCS 15) | 879 (89.5) |
| ED course | |
| Admitted to hospital | 346 (33.1) |
SD = standard deviation; MVC = motor vehicle collision; GCS = Glasgow Coma Scale
11 patients with concomitant warfarin and clopidogrel use
There were 60 patients (6.1%; 95% CI = 4.7% to 7.8%) with the primary outcome of immediate tICH diagnosed on initial ED cranial CT. None of the 65 patients who did not receive initial ED cranial CT scans were later diagnosed with immediate tICH, although two patients were lost to follow-up.
Of the 60 patients diagnosed with immediate tICH, there were 12 patients (20.0%; 95% CI = 10.8% to 32.3%) who received neurosurgical interventions. These are listed in Table 2 and most frequently involved craniotomy/craniectomy (7 patients, 11.7%) and mannitol administration (5 patients, 8.3%). Ten of the 60 patients (16.7%; 95% CI = 8.3% to 28.5%) with immediate tICH died during hospitalization.
Table 2.
Neurosurgical interventions
| Intervention | No. (%) of patients (n=60) |
|---|---|
| Intracranial pressure monitor or oxygen probe | 0 |
| Burr hole | 3 (5.0) |
| Craniotomy/craniectomy | 7 (11.7) |
| Intraventricular catheter placement | 2 (3.3) |
| Subdural drain | 2 (3.3) |
| Mannitol use | 5 (8.3) |
| Hypertonic saline use | 0 |
| Total patients with neurosurgical interventions | 12 (20.0) |
Clopidogrel use, headache, vomiting, drug or alcohol intoxication, and abnormal mental status were associated with an increased risk for immediate tICH on bivariate analysis (p < 0.20) (Table 3). Binary recursive partitioning was unable to derive a prediction rule that reliably identified a subset of patients at low risk for tICH.
Table 3.
Relative risk ratios for the clinical variables for traumatic intracranial hemorrhage (tICH) (bivariate analysis)
| Clinical variable | tICH present n/N (%) |
tICH absent n/N (%) |
Relative risk (95% CI) |
|---|---|---|---|
| Age 65 years and older | 50/60 (83.3) | 750/922 (81.3) | 1.14 (0.59–2.20) |
| Warfarin use | 31/60 (51.7) | 683/922 (74.1) | 0.40 (0.25–0.65 |
| Clopidogrel use | 30/60 (50.0) | 249/922 (27.0) | 2.52 (1.55–4.10) |
| Concomitant aspirin use | 4/60 (6.7) | 41/922 (4.4) | 1.49 (0.56–3.92) |
| Non-ground level fall mechanism | 10/60 (16.7) | 151/922 (16.4) | 1.02 (0.53–1.97) |
| Headache | 30/60 (50.0) | 319/922 (34.6) | 1.81 (1.11–2.96) |
| Vomiting | 8/60 (13.3) | 33/922 (3.6) | 3.53 (1.80–6.94) |
| Loss of consciousness or amnesia | 15/60 (25.0) | 172/922 (18.7) | 1.42 (0.81–2.49) |
| Drug or alcohol intoxication | 4/60 (6.7) | 30/922 (3.3) | 1.99 (0.77–5.18) |
| Trauma above the clavicles | 41/60 (68.3) | 655/922 (71.0) | 0.89 (0.52–1.50) |
| Abnormal mental status | 15/60 (25.0) | 88/922 (9.5) | 2.85 (1.65–4.92) |
Multivariable logistic regression identified vomiting (adjusted odds ratio [aOR] 3.68; 95% CI = 1.55 to 8.76) and abnormal mental status (aOR 3.08; 95% CI = 1.60 to 5.94) as associated with immediate tICH (Table 4). The Hosmer-Lemeshow goodness of fit test had a p value of 0.004, suggesting poor calibration of the model. Test characteristics of the clinical prediction rule consisting solely of these two variables were poor (sensitivity 37%, specificity 87%, PPV 16%, NPV 95%). All clinical variables measured for inter-rater reliability had substantial agreement (range 91% to 97%) (Table 5).18
Table 4.
Adjusted risk for traumatic intracranial hemorrhage (multivariable analysis)
| Variable | Adjusted Odds Ratio (95% CI) |
|---|---|
| Warfarin use | 0.62 (0.70–5.49) |
| Clopidogrel use | 1.68 (0.19–14.72) |
| Vomiting | 3.68 (1.55–8.76) |
| Headache | 1.60 (0.93–2.77) |
| Drug or alcohol intoxication | 1.61 (0.50–5.16) |
| Abnormal mental status | 3.08 (1.60–5.94) |
Table 5.
Inter-rater reliability of clinical variables
| Variable | Kappa (95% CI) | % agreement (95% CI) |
|---|---|---|
| Glasgow Coma Scale score | 0.65 (0.58–0.70) | 90.8 (84.9–96.2) |
| Evidence of trauma above clavicles | 0.93 (0.86–1.0) | 97.3 (92.2–99.4) |
| Vomiting | 0.65 (0.33–0.97) | 96.3 (90.9–99.0) |
| Headache | 0.80 (0.67–0.92) | 91.7 (84.9–96.2) |
| Loss of consciousness or amnesia | 0.84 (0.71–0.97) | 95.4 (89.6–98.5) |
| Drug or alcohol intoxication | 0.56 (0.00–0.71) | 97.3 (92.2–99.4) |
DISCUSSION
We were unable to derive a clinical prediction rule to accurately identify the presence of immediate tICH on cranial CT in patients with mild blunt head trauma and pre-injury warfarin or clopidogrel use. Two clinical variables, vomiting and abnormal mental status, were significantly associated with increased risk for immediate tICH on multivariable logistic regression. These two variables, however, were absent in a substantial number of our cohort of patients with tICH.
To our knowledge this is the first prospective study to evaluate risk factors for immediate tICH in patients with mild head injury and pre-injury anticoagulant or antiplatelet use. Prior retrospective studies were also unable to identify a number of clinical predictors for immediate tICH in this patient population. Li et al. were unable to identify any clinical predictors for abnormal cranial CT scans in patients with head injury and pre-injury warfarin use.10 Brewer et al found only LOC to be significantly associated with immediate tICH in trauma registry patients with pre-injury warfarin or clopidogrel use and a GCS of 15.3
The results of this study have a number of clinical implications. First, this study suggests that it is difficult to identify a low-risk group of patients with pre-injury warfarin or clopidogrel use and blunt head trauma who may be safely managed without cranial CT imaging. The inability to derive a clinical prediction rule is likely the result of the relative lack of differentiating clinical characteristics between patients with immediate tICH and those without. Patients in our study were relatively well-appearing and homogenous; they were 65 years and older with ground level falls, normal mental status, and few clinical symptoms. However, despite being well-appearing, these patients were still at risk for immediate tICH. Seven of the 60 patients (12%) with immediate tICH had low mechanisms of injury (ground level fall), no clinical symptoms (no history of LOC or amnesia, headache, vomiting), and normal clinical exams (no intoxication, normal mental status, and no evidence of trauma above the clavicles). Second, current National Institute for Health and Clinical Excellence head injury guidelines (updated 2007) recommend urgent (< 1 hour) CT imaging in patients with head injury and pre-injury warfarin use, provided they sustain loss of consciousness (LOC) or amnesia.14 However 45 of 60 (75%) of patients with immediate tICH in our study did not sustain LOC or amnesia. We thus recommend liberal cranial CT imaging for these patients, even those with minimal head trauma who do not sustain LOC or amnesia. Finally, patients with immediate tICH have high morbidity and mortality; 20% required neurosurgical intervention and 17% died during hospitalization. This emphasizes the importance of rapid diagnosis of tICH with cranial CT imaging to determine the need for reversal of anticoagulant or antiplatelet effects with medications and blood products. Patients with delayed reversal of anticoagulation have increased morbidity and mortality.19 Furthermore, in patients who require immediate neurosurgical intervention, rapid and efficacious reversal to an appropriate international normalized ratio (INR) level is essential; patients with INR levels >1.25 have increased postoperative mortality.20-22
LIMITATIONS
Our results should be interpreted in the context of several limitations. There were relatively few patients who met the primary outcome of immediate tICH (60 patients). However, there were enough outcomes for the accepted ratio of 10 outcomes of interest for every variable entered into the regression model.23 Furthermore, including more patients with tICH would not resolve the fact that many patients with immediate tICH appeared to have no risk factors for tICH beyond age and anticoagulant use. The relatively few outcomes also limited our ability to conduct subgroup analyses by type of medication use (warfarin or clopidogrel) or by INR level.
As this was an observational study, CT scans were not obtained on all patients, and ethical considerations prevented CT scanning solely for study purposes. Some patients not undergoing CT scans during their initial ED visits potentially had undiagnosed tICH. However, none were identified in clinical follow-up, which is a reasonable method to evaluate for clinically important outcomes when the definitive test is not ethical or feasible.24
CONCLUSIONS
While we identified several risk factors for immediate traumatic intracranial hemorrhage, we were unable to identify a subset of patients with mild head trauma and pre-injury warfarin or clopidogrel use who are at low risk for immediate traumatic intracranial hemorrhage. We thus recommend urgent and liberal cranial computed tomography imaging in this patient population, even in the absence of clinical findings.
Acknowledgments
This work was supported by The Garfield Memorial Fund (Kaiser Permanente). DN was supported through a Mentored Clinical Research Training Program Award (K30 and KL2), Grant Number UL1 RR024146 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. The Garfield Memorial Fund, NCRR, and NIH had no role in the design and conduct of the study, in the analysis or interpretation of the data, or in the preparation of the data. The views expressed in this article are solely the responsibility of the authors and do not necessarily represent the official view of Kaiser Permanente, NCRR, or the NIH. Information on NCRR (now National Center for Advancing Translational Sciences [NCATS]), is available at http://www.ncats.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Footnotes
Conflict of interest: None
Presentations: None
REFERENCES
- 1.Faul MXL, Wal MM, Coronado VG. US Department of Health and Human Services. Atlanta, GA: CDC; 2010. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths 2002–2006. [Google Scholar]
- 2.McMillian WD, Rogers FB. Management of prehospital antiplatelet and anticoagulant therapy in traumatic head injury: a review. J Trauma. 2009;66:942–950. doi: 10.1097/TA.0b013e3181978e7b. [DOI] [PubMed] [Google Scholar]
- 3.Brewer ES, Reznikov B, Liberman RF, et al. Incidence and predictors of intracranial hemorrhage after minor head trauma in patients taking anticoagulant and antiplatelet medication. J Trauma. 2011;70:E1–E5. doi: 10.1097/TA.0b013e3181e5e286. [DOI] [PubMed] [Google Scholar]
- 4.Sasser SM, Hunt RC, Faul M, et al. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012;61:1–20. [PubMed] [Google Scholar]
- 5.Reynolds FD, Dietz PA, Higgins D, Whitaker TS. Time to deterioration of the elderly, anticoagulated, minor head injury patient who presents without evidence of neurologic abnormality. J Trauma. 2003;54:492–496. doi: 10.1097/01.TA.0000051601.60556.FC. [DOI] [PubMed] [Google Scholar]
- 6.Rockswold GL, Leonard PR, Nagib MG. Analysis of management in thirty-three closed head injury patients who "talked and deteriorated". Neurosurgery. 1987;21:51–55. doi: 10.1227/00006123-198707000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357:1391–1396. doi: 10.1016/s0140-6736(00)04561-x. [DOI] [PubMed] [Google Scholar]
- 8.Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux PM. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000;343:100–105. doi: 10.1056/NEJM200007133430204. [DOI] [PubMed] [Google Scholar]
- 9.Smits M, Dippel DW, de Haan GG, et al. External validation of the Canadian CT Head Rule and the New Orleans Criteria for CT scanning in patients with minor head injury. JAMA. 2005;294:1519–1525. doi: 10.1001/jama.294.12.1519. [DOI] [PubMed] [Google Scholar]
- 10.Li J, Brown J, Levine M. Mild head injury, anticoagulants, and risk of intracranial injury. Lancet. 2001;357:771–772. doi: 10.1016/S0140-6736(00)04163-5. [DOI] [PubMed] [Google Scholar]
- 11.Mina AA, Knipfer JF, Park DY, Bair HA, Howells GA, Bendick PJ. Intracranial complications of preinjury anticoagulation in trauma patients with head injury. J Trauma. 2002;53:668–672. doi: 10.1097/00005373-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Jones K, Sharp C, Mangram AJ, Dunn EL. The effects of preinjury clopidogrel use on older trauma patients with head injuries. Am J Surg. 2006;192:743–745. doi: 10.1016/j.amjsurg.2006.08.037. [DOI] [PubMed] [Google Scholar]
- 13.Jagoda AS, Bazarian JJ, Bruns JJ, Jr, et al. Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. Ann Emerg Med. 2008;52:714–748. doi: 10.1016/j.annemergmed.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 14.National Collaborative Centre for Acute Care and National Institute for Health and Clinical Excellence. [Accessed July 12, 2012];Head injury: triage, assessment, investigation and early management of head injury in infants, children, and adults. Available at: http://www.nice.org.uk/nicemedia/pdf/CG56NICEGuideline.pdf. [PubMed]
- 15.Servadei F, Teasdale G, Merry G. Defining acute mild head injury in adults: a proposal based on prognostic factors, diagnosis, and management. J Neurotrauma. 2001;18:657–664. doi: 10.1089/089771501750357609. [DOI] [PubMed] [Google Scholar]
- 16.Nishijima DK, Offerman SR, Ballard DW, et al. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59:460–468. doi: 10.1016/j.annemergmed.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Concato J, Feinstein AR, Holford TR. The risk of determining risk with multivariable models. Ann Intern Med. 1993;118:201–210. doi: 10.7326/0003-4819-118-3-199302010-00009. [DOI] [PubMed] [Google Scholar]
- 18.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 19.Ivascu FA, Howells GA, Junn FS, Bair HA, Bendick PJ, Janczyk RJ. Rapid warfarin reversal in anticoagulated patients with traumatic intracranial hemorrhage reduces hemorrhage progression and mortality. J Trauma. 2005;59:1131–1137. doi: 10.1097/01.ta.0000189067.16368.83. [DOI] [PubMed] [Google Scholar]
- 20.Boulis NM, Bobek MP, Schmaier A, Hoff JT. Use of factor IX complex in warfarin-related intracranial hemorrhage. Neurosurgery. 1999;45:1113–1118. doi: 10.1097/00006123-199911000-00020. [DOI] [PubMed] [Google Scholar]
- 21.Kawamata T, Takeshita M, Kubo O, Izawa M, Kagawa M, Takakura K. Management of intracranial hemorrhage associated with anticoagulant therapy. Surg Neurol. 1995;44:438–442. doi: 10.1016/0090-3019(95)00249-9. [DOI] [PubMed] [Google Scholar]
- 22.Yasuda CL, Morita ME, Nishimori FY, Yasuda AM, Alves HL. [Chronic subdural hematoma: study of 161 patients and the relationship with coagulation abnormalities] (in Portuguese) Arq Neuropsiquiatr. 2003;61:1011–1014. doi: 10.1590/s0004-282x2003000600023. [DOI] [PubMed] [Google Scholar]
- 23.Wasson JH, Sox HC, Neff RK, Goldman L. Clinical prediction rules. Applications and methodological standards. N Engl J Med. 1985;313:793–799. doi: 10.1056/NEJM198509263131306. [DOI] [PubMed] [Google Scholar]
- 24.Jaeschke R, Guyatt G, Sackett DL. Users' guides to the medical literature. III. How to use an article about a diagnostic test. A. Are the results of the study valid? Evidence-Based Medicine Working Group. JAMA. 1994;271:389–391. doi: 10.1001/jama.271.5.389. [DOI] [PubMed] [Google Scholar]