SYNOPSIS
The management of patients after anterior cruciate ligament reconstruction should be evidence based. Since our original published guidelines in 1996, successful outcomes have been consistently achieved with the rehabilitation principles of early weight bearing, using a combination of weight-bearing and non–weight-bearing exercise focused on quadriceps and lower extremity strength, and meeting specific objective requirements for return to activity. As rehabilitative evidence and surgical technology and procedures have progressed, the original guidelines should be revisited to ensure that the most up-to-date evidence is guiding rehabilitative care. Emerging evidence on rehabilitative interventions and advancements in concomitant surgeries, including those addressing chondral and meniscal injuries, continues to grow and greatly affect the rehabilitative care of patients with anterior cruciate ligament reconstruction. The aim of this article is to update previously published rehabilitation guidelines, using the most recent research to reflect the most current evidence for management of patients after anterior cruciate ligament reconstruction. The focus will be on current concepts in rehabilitation interventions and modifications needed for concomitant surgery and pathology.
Keywords: ACL, graft, surgery
More than 200 000 anterior cruciate ligament (ACL) injuries occur each year in the United States, and approximately 65% of these injuries are treated with reconstructive surgery.8 A consistent approach to rehabilitation after ACL reconstruction can yield predictably good outcomes, such as a return to previous levels of activity and normal knee function. In 1996, the University of Delaware published criterion-based rehabilitation guidelines,58 in which a progression was established with specific clinical milestones following tissue-healing time frames. The goal of any criterion-based guideline is to maximize the patient’s response to exercise at the current level of function, while minimizing the risk of injury to the healing tissue. Based on sound principles and current evidence, the original guidelines have continued to guide rehabilitative care to successful outcomes.
Advancements in surgical procedures directly impact postoperative rehabilitation. Since the original guidelines were published in 1996, there have been considerable advancements in ACL reconstruction surgical procedures and common secondary surgical interventions to address injuries often associated with ACL tears. Rehabilitation after ACL reconstruction has continued to move away from surgery-modified rehabilitation, in which surgery constrains the rehabilitation progression, and toward rehabilitation-modified surgery, in which the reconstruction techniques are robust enough to withstand early mobilization and strengthening.33,37 Modifications of the surgery over the past 16 years (eg, soft tissue fixation) warrant a re-examination of the rehabilitative management of patients after ACL reconstruction. Further literature and understanding of secondary surgeries and their impact on ACL reconstruction call for further clarification of their impact on postsurgical treatment and outcomes. The purpose of this paper is to revisit the rehabilitation guidelines to reflect the most current evidence on management of patients following ACL reconstruction.
ISOLATED ACL RECONSTRUCTION
The original guidelines (TABLE 1) were developed around evidence-based medicine, with consideration given to biological healing time frames. As a result, the treatment of an isolated ACL reconstruction has required only minor adjustments to reflect recent advances in the rehabilitation literature and surgical techniques (APPENDIX). Though time frames have been included to guide the therapist, the patient is required to meet all of the clinical milestones prior to advancing to the next stage, no matter the time frame. Clarification and adjustments of clinical milestones and additions of interventions aim to improve functional outcomes and to provide a safe return to sport.
TABLE 1. Original Anterior Cruciate Ligament Reconstruction Rehabilitation Practice Guidelines*.
| Time Frame | Clinical Milestones | Activities |
|---|---|---|
| Days 1 to 3 |
|
|
| Week 2 |
|
|
| Week 4 |
|
|
| Weeks 6 to 8 |
|
|
| Week 12 |
|
|
Abbreviations: KOS, Knee Outcome Survey; KOS-ADL, Knee Outcome Survey activities of daily living subscale; ROM, range of motion.
Discontinue treatments when goals are met Recheck monthly until 6 months after surgery.
Compared with uninvolved.
Presurgical Rehabilitation
Knee function prior to surgery is important in expected and final outcomes after ACL reconstruction.17,22,23,47,49,50,81,83 The updated guidelines include preoperative milestones to reflect the importance of such factors on postoperative outcomes. Patients with full knee extension range of motion (ROM), absent or minimal effusion, and no knee extension lag during a straight leg raise preoperatively have better postsurgical outcomes, such as returning to previous levels of activity and demonstration of normal knee function.88
Quadriceps strength deficit is significant after ACL injury, ranging from 15% to 40%.14,17,23,35,40,45,65 Preoperative quadriceps strength is a significant predictor of knee function after ACL reconstruction.17,22,47,52,82 Because of the large impact that quadriceps strength may have on knee function, the identification and treatment of quadriceps weakness prior to ACL reconstruction are paramount in maximizing patient outcomes. Objective measures of quadriceps strength with isometric or isokinetic dynamometry allow the rehabilitation specialist to track the progress of this critical impairment throughout the recovery period. Preoperative rehabilitation that includes perturbation training and aggressive quadriceps strengthening should be used to reduce limb-to-limb differences, with the objective of improving the quadriceps index (the ratio of involved-side quadriceps strength to uninvolved-side quadriceps strength) to greater than 90% prior to surgery.21,54
Immediate Postoperative Phase
The milestones for the immediate postoperative phase (week 1) are active/passive ROM equal to 0° to 90° and the performance of an active quadriceps contraction with superior patellar glide. Knee extension ROM loss is unfortunately a common issue, with one study showing 25.3% of patients having more than a 5° side-to-side difference in passive knee extension ROM 4 weeks after ACL reconstruction.60 Even small losses (3°-5°) of knee extension adversely affect subjective and objective results following ACL reconstruction, with loss of normal extension and flexion being associated with weaker quadriceps.86 Early achievement of full knee extension also decreases the risk of postoperative complications such as arthrofibrosis.30,43 If full extension is not achieved by week 2, low-load long-duration stretching techniques, such as prone hangs (FIGURE 1) or bag hangs, are needed to effectively restore full knee extension.55,61
FIGURE 1.
Prone hang. Begin without weight for 10 minutes and progress to increased weight around the ankle and longer duration as needed for the desired result. A belt above the hips, wrapped around the table, may also be used to help avoid compensations at the hip during the activity.
Deficits in quadriceps strength after ACL reconstruction have been reported to be present months to years after surgery and at various isokinetic testing speeds.42 Quadriceps weakness occurs to the greatest extent in the first months after reconstruction.17,42,46 Neuromuscular electrical stimulation (NMES) (FIGURE 2) may be used to augment quadriceps strengthening activities and has been shown to improve outcomes.48,90,91 The quadriceps muscles are often affected by arthrogenic muscle inhibition after ACL reconstruction, which limits volitional contraction. A benefit of NMES is that it directly recruits the motor neurons to produce better quadriceps strength gains than voluntary exercise alone.74 Functional outcomes are improved with increased strength gains of the quadriceps.74
FIGURE 2.
Neuromuscular electrical stimulation (NMES). NMES is applied with the patient in a seated position and the knee in 60° of flexion (varying angles are used based on pain and comorbidities). The patient relaxes while electrical stimulation is applied to achieve 50% of the maximal volitional isometric contraction against a fixed resistance.
Early Postoperative Phase
The milestones of the early postoperative phase (week 2 postsurgery) are knee flexion greater than 110°, walking without crutches, the use of a cycle/stair climber without difficulty, walking with full knee extension, reciprocal stair climbing, straight leg raise without an extension lag, and a Knee Outcome Survey activities of daily living subscale score greater than 65%. When recently reviewed, the average Knee Outcome Survey activities of daily living subscale score for our patients at the end of week 2 was 60.2%, with a median of 64% (unpublished data, 2009). Because the median score more accurately reflected data that had large outliers, 65% was chosen as the suggested criterion. Crutches and an immobilizer may be used early after an ACL reconstruction. Crutches may be discontinued once a patient is able to ambulate without pain, and the immobilizer may be discontinued once the patient has demonstrated a straight leg raise without an extension lag. If a functional brace was ordered preoperatively, patients may use the brace once the immobilizer has been discontinued.
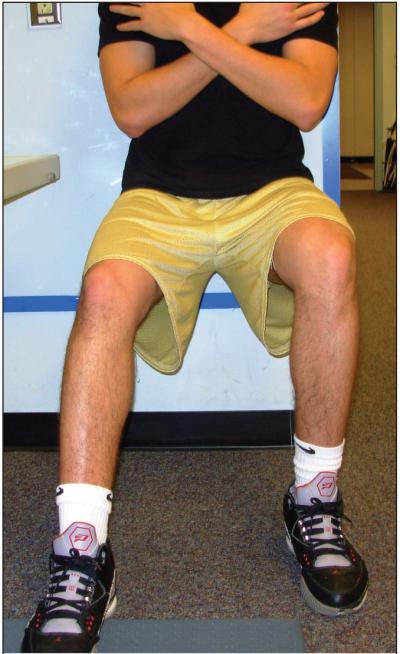
In this phase, treatments incorporate weight-bearing (closed-chain) activities (FIGURE 3), such as wall slides and stepups in pain-free ranges (typically 0°-60°), which have been shown to be safe and effective, to possibly place less stress on the healing graft, and to cause less patellofemoral pain.11 Mikkelsen et al63 found higher quadriceps strength and rates of return to sports but no difference in laxity when comparing the use of a combination of non–weight-bearing and weight-bearing exercises versus weight-bearing exercises alone. Based on this systematic review, it appears that non–weight-bearing exercises and weight-bearing exercises can be safely incorporated into the rehabilitation process without deleterious effects on the healing ACL graft, as long as undue strain on the healing graft is avoided (ie, limiting knee ROM from 90° to 45° for the non–weight-bearing exercises, progressing to knee ROM from 90° to 10° by week 12).
FIGURE 3.
Wall squats. The patient begins, back against the wall and legs shoulder-width apart, by lowering down into a squat position of up to 90° of knee flexion, as pain and strength allow. The exercise is progressed by adding a hold time in the squat position and progressing to 90° of knee flexion if not achieved initially.
Intermediate Postoperative Phase
The milestones for the intermediate postoperative phase are knee flexion within 10° of the uninvolved side and a quadriceps index greater than 60%. Balance and neuromuscular re-education exercises begin in this time frame (FIGURES 4 and 5). Neuromuscular alterations (ie, muscle inhibition, impaired sensorimotor function) around the ACL-reconstructed knee may contribute to clinical impairments, such as strength loss, atrophy, and altered function.42 The use of balance and neuromuscular re-education activities has shown no adverse effects of increased joint laxity or decreased strength when compared to standard rehabilitation methods.16 Self-reported knee function after ACL reconstruction improves with a neuromuscular rehabilitation program.80
FIGURE 4.
Single-leg balance. Single-leg balance should be performed with the stance knee slightly flexed and avoiding excessive genu valgum. Increasing time and adding distractions, such as a ball toss, will progress the difficulty.
FIGURE 5.
Single-leg cone pick-up. The single-leg cone pick-up is a single-leg squat, while touching cones in a semicircle using the same hand. Proper knee alignment should be maintained, especially as the trunk rotates to reach the cones. Decreasing the height of the cones and placing the stance leg on an unstable surface will progress the difficulty of the exercise.
Late Postoperative Phase
The frequency of treatment during the late-postoperative time frame is based on the remaining impairments. The milestones are a quadriceps index greater than 80%, a normal gait pattern, full knee ROM, and knee joint effusion equal to a grade of trace or less. The quadriceps index of 80% represents a minimal deficit in strength71,99 and has been previously used to distinguish between poor and good quadriceps strength.52,72,87 The quadriceps index of 80% has also been used as a cutoff for the use of NMES to augment quadriceps strengthening.91 Effusion can be assessed using the modified stroke test (TABLE 2) as a reliable method of rating knee effusion in the outpatient setting.95
TABLE 2. Effusion Grading Scale of the Knee Joint Based on the Stroke Test.
| Grade | Test Result |
|---|---|
| Zero | No wave produced on downstroke |
| Trace | Small wave on medial side with downstroke |
| 1+ | Larger bulge on medial side with downstroke |
| 2+ | Effusion spontaneously returns to medial side after upstroke (no downstroke necessary) |
| 3+ | So much fluid that it is not possible to move the effusion out of the medial aspect of the knee |
Reproduced from Sturgill et al.95
Transitional Phase
Once a patient is 8 weeks postsurgery and has met the criteria of 80% quadriceps index, effusion of trace or less, and demonstrated an understanding of the soreness rules (TABLE 3),24 a running progression may commence (TABLE 4, APPENDIX). All active patients after ACL reconstruction, including nonrunners, are encouraged to perform the running progression for the benefits of unilateral strengthening during the running gait and increased force generation from the dynamic nature of running. The running progression begins as a 2-mi (3.2-km) activity, with an alternation of jogging and walking. The ratio of jogging to walking distance is gradually increased and, beginning at level 6, the distance and pace are increased.
TABLE 3. Soreness Rules*.
| Criterion | Action |
|---|---|
| Soreness during warm-up that continues | 2 days off, drop down 1 level |
| Soreness during warm-up that goes away | Stay at level that led to soreness |
| Soreness during warm-up that goes away but redevelops during session |
2 days off, drop down 1 level |
| Soreness the day after lifting (not muscle soreness) | 1 day off, do not advance program to the next level |
| No soreness | Advance 1 level per week or as instructed by healthcare professional |
Reprinted with permission from SAGE Publications: Fees M, Decker T, Snyder-Mackler L, Axe MJ. Upper extremity weight-training modifications for the injured athlete. A clinical perspective. Am J Sports Med. 1998;26(5):735. Copyright ©1998 SAGE Publications.
TABLE 4. Running Progression*.
| Level | Treadmill | Track |
|---|---|---|
| Level 1 | 0.1-mi walk/0.1-mi jog, repeat 10 times | Jog straights/walk curves (2 mi) |
| Level 2 | Alternate 0.1-mi walk/0.2-mi jog (2 mi) | Jog straights/jog 1 curve every other lap (2 mi) |
| Level 3 | Alternate 0.1-mi walk/0.3-mi jog (2 mi) | Jog straights/jog 1 curve every lap (2 mi) |
| Level 4 | Alternate 0.1-mi walk/0.4-mi jog (2 mi) | Jog 1.75 laps/walk curve (2 mi) |
| Level 5 | Jog full 2 mi | Jog all laps (2 mi) |
| Level 6 | Increase workout to 2.5 mi | Increase workout to 2.5 mi |
| Level 7 | Increase workout to 3 mi | Increase workout to 3 mi |
| Level 8 | Alternate between running/jogging every 0.25 mi | Increase speed on straights/jog curves |
Progress to next level when patient is able to perform activity for 2 mi without increased effusion or pain. Perform no more than 4 times in 1 week and no more frequently than every other day. Do not progress more than 2 levels in a 7-day period. Conversion: 1 mi = 1.6 km. Reprinted with permission from Tara Manal, University of Delaware Physical Therapy Clinic.
During this transitional phase, patients who are no longer being treated in a clinical setting should progress their strengthening program at a fitness facility. Patients who have not met the quadriceps index milestone of 80% should continue quadriceps strengthening and NMES, and those patients who have a quadriceps index of at least 80% may continue with a gym strengthening program if no other impairments persist. Exercise prescription should continue to focus on unilateral lower extremity strengthening and neuromuscular control. Patients may have a desire to begin exercising the uninvolved side, and an individual plan should be designed to foster strength gains aiming for bilateral limb symmetry.
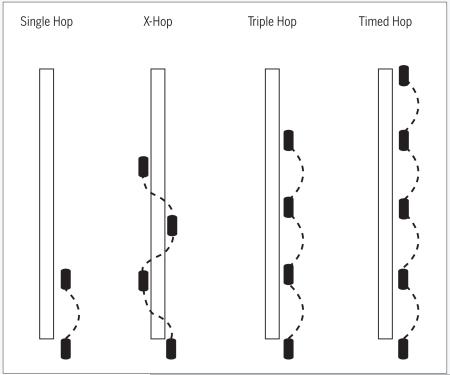
Hop tests are a functional assessment of dynamic stability of the knee,7,26,70,78 and patients can undergo hop testing as early as 12 weeks after ACL reconstruction, if all criteria are met. The quadriceps strength index (assessed with dynamometry) should be at least 80%. Additional criteria to meet for hop tests are trace or less effusion, full knee ROM, and no pain with single-leg hopping. Low to moderate correlations were found between hop test performance and lower extremity muscular strength, and between hop test performance and self-report outcome measures.26 Because a single test that captures all the essential components necessary for return to sport has not been established, several measurements of limb impairments may be used to capture different constructs of physical function that are necessary to gauge a patient’s function at a given time.26 Four single-limb hop tests commonly used in patients after ACL reconstruction are the single hop for distance, the crossover hop for distance, the triple hop for distance, and the 6-meter timed hop (instructions and milestones are detailed in the APPENDIX).
Quadriceps weakness can exceed 20% at 6 months after ACL reconstruction and 10% to 15% at 1 year.74 Recent research from our clinic indicates that, when following these clinical guidelines, limb-to-limb asymmetries are reduced and limb symmetry indexes are restored to greater than 90%, returning to preoperative levels by 6 months after ACL reconstruction.54 Previous research utilizing these clinical guidelines has found a quadriceps index of 90% or greater in patients at 3-, 6-, and 12-month follow-ups in 55%, 65%, and 73% of subjects, respectively.36 The mean quadriceps index values at the 3-, 6-, and 12-month follow-ups in groups that received either perturbation or strength training prior to surgery were 88.7% and 92.7%, 95.7% and 93.0%, and 98.7% and 98.1%, respectively.36 These quadriceps index values reflect good restoration of quadriceps and limb symmetries when following these clinical guidelines as an essential component of safe return to activity. We recommend that all patients should continue to strengthen the involved lower extremity until 90% quadriceps index is obtained.
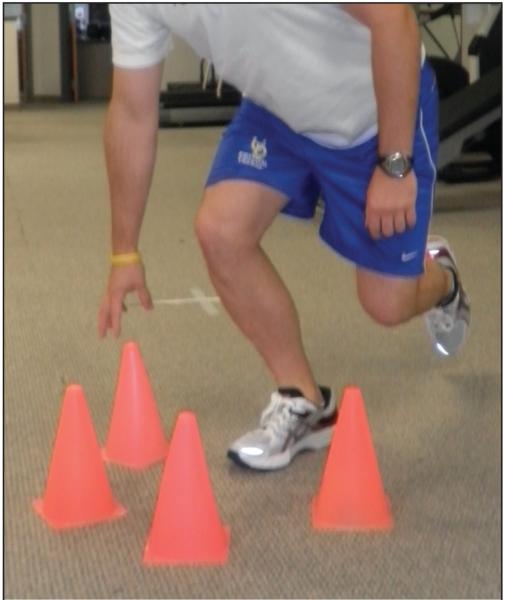
Agility, plyometric, and sport-specific activities can be added to the patient’s home exercise program,10 provided that the patient shows no adverse effects of the running progression (eg, increased effusion or pain) and demonstrates pain-free performance of loading activities. Patients should be instructed by the therapist and able to demonstrate proper technique under supervision, prior to adding these higher-level activities to a home program. Agility drills during a rehabilitation program can assist patients by allowing them to adjust to sport-specific activities, such as changing directions, accelerating, and decelerating.79 Plyometrics can improve neuromuscular control in athletes, which can become a learned skill that transfers to return to competitive play.67 Additionally, neuromuscular control of dynamic lower extremity valgus is enhanced with plyometric training,66 which may be critical for the prevention of ACL reinjury.39,66 Athletes participating in jumping activities may benefit from education on proper jumping and landing technique. High school female athletes in basketball, volleyball, and soccer, following a preseason jumping program with instruction on proper landing technique, showed significantly lower knee injury rates compared to untrained females.38 The effects of plyometrics, however, have not been investigated in the functional return of patients after ACL reconstruction.
Patients return for functional testing between 3 and 6 months, as needed, based on their ability to meet the milestones (TABLE 5) within healing time frames or their desire to return to sport. If any of the criteria are not met, the patient is not cleared to begin return-to-sport activity. Although return to preinjury levels or sport may be a short-term goal after reconstruction,19 the intention to return to sports is not predictive of actual return to play.4 Patients may reduce their activity levels for a variety of reasons, including social reasons, knee problems, or fear of reinjury.69,98 Additionally, not all athletes have or take the opportunity to return to previous activity levels or sports.
TABLE 5. Return-to-Sport Criteria*.
|
Abbreviation: KOS-ADL, Knee Outcome Survey-activities of daily living.
All criteria must be met prior to beginning a return-to-sport progression.
For those who do desire to return to their previous level of sport participation, strict return-to-sport criteria have been developed to ensure normal limb symmetry and knee function. Limb symmetry indexes of 90% have previously been suggested as the milestone for determining normal limb symmetry in quadriceps strength71,91,99 and functional testing.26,36,68,70,78 Additionally, the cutoff of 90% is used for 2 self-reported outcome measures in this population. Athletes must pass all the criteria to begin returning to sports. Following these rehabilitation guidelines and using the return-to-sport criteria (performance-based and self-report outcomes), 40% of athletes classified as noncopers preoperatively passed return-to-sport criteria at 6 months after ACL reconstruction and 73% passed at 12 months.37 When assessed at the 3-, 6-, and 12-month follow-ups for the self-report outcomes, the percentages of patients with 90% or greater were 70%, 92.5%, and 92.5% for the Knee Outcome Survey activities of daily living subscale, and 37.5%, 72.5%, and 87.5% for the global rating score of knee function.36 Using the age- and sex-matched norms on the International Knee Documentation Committee 2000 Subjective Knee Evaluation Form,1,31 75% of patients had knee function within normal ranges at 6 months after surgery and 87% by 1 year.54 Although we have not yet examined return to previous level of activity using these guidelines, current data suggest that it may improve self-report and performance-based knee function. Athletes not meeting the criteria continue rehabilitation focused on the areas in which they did not achieve the desired return-to-sport score.
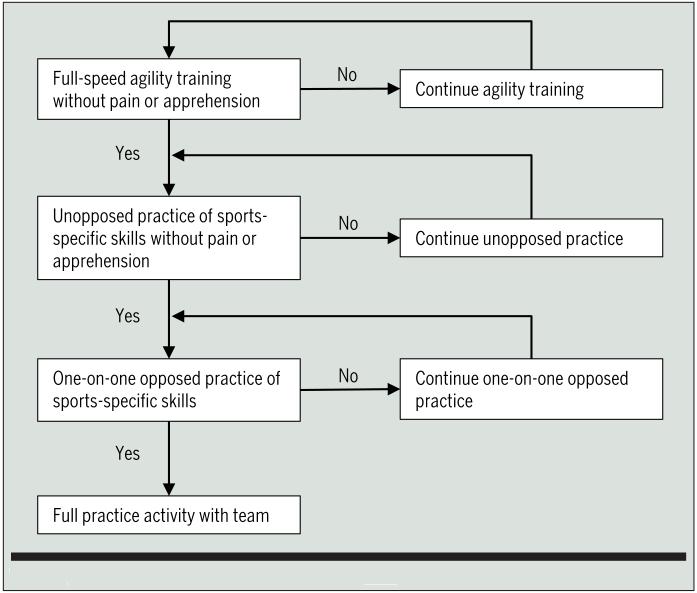
Once cleared, patients do not directly return to competition. Athletes begin with lower-level sports participation in practice and gradually build up to competition, while monitoring pain, effusion, and ROM.25 A systematic approach for return to sport participation that accounts for pain and apprehension is recommended (FIGURE 6).25 If postoperative bracing is used, our evidence shows that patients may discontinue use of the brace at 1 year.29 The patient’s activity level should be monitored utilizing the soreness guidelines to minimize the potential recurrence of impairments.
FIGURE 6.
Progression to sports-related activities (adapted from Fitzgerald et al25).
GRAFT TYPES
Graft selection is an important consideration for the rehabilitation specialist. Certain factors should be considered when rehabilitating patients with different graft types. With a bone-patellar tendon-bone autograft, donor-site morbidity can occur, and the rehabilitation specialist should be aware of patellar tendon pain during quadriceps strengthening.44 Although no difference in anterior knee pain has been consistently shown in patients who have had a bone-patellar tendon-bone compared to a hamstring autograft,84 an increased incidence of pain with kneeling has been found in those with the bone-patellar tendon-bone procedure.93 Patellar taping and pain modalities may be effective in decreasing patellar tendon pain that patients may experience.
If a hamstring autograft is used, resisted hamstring activities are not performed for 12 weeks after surgery. After hamstring graft harvest, the hamstring muscles retract, although most tendons eventually regenerate and muscle force improves by 6 to 12 months after ACL reconstruction.57,100,101 Resisted hamstring strengthening is delayed to allow for appropriate soft tissue healing and to limit irritation to the hamstring donor site. After 12 weeks, the patient can begin a resisted hamstring-strengthening progression and activities according to the soreness rules. The use of hamstring autografts does not appear to limit the recovery of hamstring strength.13,101 Additionally, bone-patellar tendon-bone and hamstring autograft procedures do not differ in clinical and functional outcomes in terms of laxity, clinical outcome, time to return to sports, patellofemoral crepitations, single-legged hop test, ROM, thigh muscle circumference, or anterior knee sensory deficit.85 Because the use of hamstring autografts does not influence clinical or functional outcomes and demonstrates good strength recovery,3,85 the 12-week restriction is used to allow for necessary hamstring recovery after harvesting.
Recent advances in surgical technique include use of a double-bundle graft to attempt to replicate the anatomical nature of the ACL. Double-bundle grafts have shown some advantage in decreasing anterior and rotational laxity after surgery,89 but no modifications to the rehabilitation guidelines are warranted when compared with single-bundle grafts.
Clinical and functional outcomes after ACL reconstruction using allograft tissue compared to autograft tissue appear to be similar.12,96 An allograft selection has the advantage of having no graft donor-site morbidity, and donor-site precautions are not necessary during the rehabilitation process.32 Even though nonirradiated allografts are equal in strength to autografts, allograft healing is delayed regarding graft incorporation and remodeling.32 An increased risk for graft failure has been proposed as a potential limitation to allograft utilization. Individuals with an allograft were 5 times more likely to have an ACL graft failure than those with an autograft.9,51 In patients participating at a high activity level after reconstruction, allograft failure was 14.1 times more likely than autograft failure.9 Patients following allograft ACL reconstruction have faster immediate postoperative recovery and less operative pain, suggesting that they may be more likely to attempt return to high-level sports prematurely.9,15 Combined with delayed healing of the allograft, premature return to sports may put these athletes at greater risk for graft failure. Recent evidence indicates that it may be more beneficial in younger patients to use an autograft,92 but there is no evidence that delaying return to sport decreases the likelihood of rerupture if an allograft is used. Therefore, all individuals, despite graft selection, should be required to meet the criteria at each phase before being able to progress to the next phase of the rehabilitation. Rehabilitation specialists should maintain the latest knowledge of the effect of graft selection, as evidence continues to emerge to determine the effect on return to sport.
MENISCAL INJURY
The meniscus plays a large role in the integrity of the knee, with contributions to shock absorption, load transmission, joint nutrition, and stability.5 Typically, when a partial arthroscopic meniscectomy is performed concurrently with an ACL reconstruction, no modifications to rehabilitation are necessary unless specified by the surgeon.
Meniscal repairs have become increasingly more common with the introduction of arthroscopic fixation techniques.97 Meniscal repairs performed at the time of the ACL reconstruction have superior healing rates and better outcomes in comparison to isolated meniscal repairs.76 Toman et al97 showed a greater than 90% clinical success rate in patients who had meniscus repair in conjunction with ACL reconstruction. In that study,97 surgeons were allowed to select the postoperative rehabilitation program; however, other studies have included the more aggressive rehabilitation typically used following ACL reconstruction and have shown similar success rates.6,59 The clinical practice guidelines, “Knee Pain and Mobility Impairments: Meniscal and Articular Cartilage Lesions,”56 published by the Orthopaedic Section of the American Physical Therapy Association, suggest that clinicians consider early weight bearing and mobilization.56 If a meniscal repair is performed concurrently with ACL reconstruction, modifications include no weight-bearing activities at knee angles greater than 45° of flexion for 4 weeks, with no restrictions on weight bearing in full extension. After the initial 4 weeks, weight-bearing knee flexion, as in a deep squat, is limited to less than 90°. Because meniscal repairs are commonly performed on the posterior horn of the meniscus,94 increased knee flexion greater than 90° can irritate and potentially damage the healing meniscal repair site. After 8 weeks, the rehabilitation specialist should resume normal ACL guidelines. Therefore, there are no additional restrictions on running progressions for an ACL reconstruction with meniscal repair.
Meniscus transplantation is also now being performed more often. It is still considered a joint-preserving surgery without return to sports as a goal. Meniscus transplant is complex, and each procedure is different. Often, meniscus transplantation is performed with a concomitant tibial or femoral osteotomy. Meniscus transplantation and ACL reconstruction are often staged. The rehabilitation guidelines for meniscal transplantation are therefore beyond the scope of this paper, and these guidelines should not be used for patients with staged or concomitant ACL reconstruction and meniscus transplantation.
CHONDRAL DEFECTS
Addressing chondral defects of the knee has been an area of significant advancement in recent years. With the increased understanding of articular cartilage lesions and the development of chondral repair interventions (eg, autologous chondrocyte transplantation), these situations present unique tissue healing dilemmas. Similar to a meniscus transplant, articular cartilage repair is often performed with a concomitant tibial or femoral osteotomy, and articular cartilage repair and ACL reconstruction are often staged.53
A patient who undergoes a chondral debridement may be weight bearing as tolerated with crutches for 3 to 5 days after surgery, with no other modification of the post–ACL reconstruction rehabilitation guidelines.77 Microfracture procedures are performed arthroscopically, usually in conjunction with ACL reconstruction, with the cartilage surgical site requiring additional protection. Patients are non–weight bearing with crutches from 2 to 8 weeks, depending on knee pain, effusion, the surgeon’s preference, and the location and size of the lesion. Lesions that are larger in size and in weight-bearing zones will require additional precautions.77
Procedures aimed at repairing the damaged articular cartilage are becoming more popular. The influence of articular cartilage in the prevention of degenerative changes and generation of pain is more widely appreciated,2 and the preservation of the cartilage is encouraged when possible. Procedures such as osteochondral autograft transfer system (OATS) and autologous chondrocyte implantation (ACI) challenge the rehabilitation specialist to further enhance rehabilitation techniques. Recent literature has focused on identifying the most beneficial intervention and the individuals most likely to benefit from cartilage repair. Few of these studies have produced higher-level evidence and many lack control groups. ACI and OATS have been shown to lead to better outcomes than microfracture surgery. Microfracture, OATS, and ACI procedures have all demonstrated the ability to return athletes to sport with rates of 59% to 66%, 91% to 93%, and 67% to 78%, respectively.34,64 The patients who were younger, had shorter preoperative symptom duration, had no prior surgical intervention, and higher preinjury and postsurgical levels of sports participation, had better outcomes and higher rates of return to sport.34 Rehabilitation after isolated chondral repair surgery is highly individualized (depending on factors such as the size and location of the lesions), and rehabilitation guidelines can be found for the different isolated chondral repair surgeries.77 Due to the complexity of the surgeries and specific needs of postoperative management, the most conservative guidelines following chondral repair procedures should be followed with concomitant ACL reconstruction.77
Return to sports after chondral injuries is controversial, and studies to assess the effectiveness of chondral surgeries are increasingly available. The authors of a systematic review on articular cartilage repair in the athlete’s knee examined 20 studies on clinical outcomes and return to competition.64 With an average of 42-month follow-up, 79% of patients reported good to excellent results using self-report outcome measures. Seventy-three percent returned to sports participation 7 to 18 months postsurgery, depending on the surgical technique. A decline in continued sports participation at the same preinjury level was observed at 2 to 5 years after surgery.64 For microfracture and OATS procedures, we use the same criteria-based guidelines for progression of exercise and determination of readiness for return to sports. Our guidelines for ACI procedures are typically surgeon specific, due to the nature of the technique, larger lesion size, and length of healing time and rehabilitation.64 However, soreness and effusion guidelines are still used to direct the rehabilitation process and readiness for return-to-sport testing.
LIGAMENTOUS
When there is a tear of the medial collateral ligament (MCL) combined with an ACL rupture, the MCL is typically treated nonsurgically. The severity of the MCL injury may contribute to the outcome of a combined ACL-MCL injury when the MCL is treated nonoperatively.20,41 Much of the current histological and mechanical healing literature on nonoperative management of the MCL has been done on animals, and this should be considered when interpreting the literature. ACL reconstruction is usually delayed to allow for the MCL to heal and to correct any additional impairments that the patient may exhibit. Petersen and Laprell75 evaluated the effects of early (within 3 weeks of the original injury) versus delayed (minimum of 10 weeks after injury) ACL reconstruction in patients with combined ACL-MCL injuries. They found that patients who had late ACL reconstruction had significantly lower rates of ROM complications in both flexion and extension and lower rates of re-arthroscopies to address extension ROM losses, as well as significantly better outcomes in Lysholm scores.
When combined ACL-MCL injuries occur, during the preoperative stage, modifications to the rehabilitation process are warranted. Treatment should be restricted to the exercises/movements performed in the sagittal plane for 4 to 6 weeks to allow for MCL healing. Tibial internal rotation, to minimize valgus stresses on the healing MCL, should also be maintained during resisted strengthening exercises (TABLE 6).
TABLE 6. Range-of-Motion Restriction Guidelines for Nonoperative Management of Medial Collateral Ligament Injuries.
| Grade | Week 1 | Week 2 | Week 3 |
|---|---|---|---|
| I | No restrictions | No restrictions | No restrictions |
| II | 0°-90° | 0°-110° | No restrictions |
| III | 0°-30° | 0°-90° | 0°-110° |
For individuals with chronic MCL insufficiency and failed conservative management, an MCL repair with ACL reconstruction may be indicated. In this scenario, patients use crutches for 5 weeks, wear an immobilizer with the knee in full extension (0°) for 6 weeks, and are weight bearing as tolerated immediately postoperative day 1.73 Except for these modifications, these patients will continue with the ACL reconstruction guidelines for the isolated ACL reconstruction (APPENDIX).
Multiligament instability (ie, knee dislocation) occurs when the ACL, posterior cruciate ligament, and either the medial structures or the lateral and posterolateral structures of the knee are ruptured. This injury typically occurs in situations involving high-energy forces, such as motor vehicle accidents and catastrophic sports injuries. Typically, a 6- to 8-week period of non–weight bearing is recommended after multiligament stabilization surgery.20 Individuals who had a posterior cruciate ligament reconstruction concomitant with ACL reconstruction should follow the more conservative posterior cruciate ligament postsurgical rehabilitation guidelines. With posterolateral corner repair/reconstruction, the rehabilitation specialist should minimize tibial external rotation and varus stresses. These patients should also avoid hyperextension and resisted knee flexion for 12 weeks.62
There have been limited studies published on the effective management of an ACL revision. The current literature has shown worse outcomes after ACL revisions in comparison to primary ACL reconstruction.28 In a study by Fox et al,27 an identical rehabilitation program was used for revision and primary ACL reconstruction. Although the rehabilitation program itself could not be directly associated with a higher failure rate in those with revision surgeries, future studies should try to determine the best rehabilitation program for ACL revisions. Following a revision ACL reconstruction, the rehabilitation guidelines may need to be modified to account for possible fixation concerns and complications from previous procedures by slowing the progression.18 Patients should use crutches and an immobilizer for an additional 2 weeks after surgery. The initiation of a running progression and functional testing are delayed to 12 and 16 weeks, respectively, after surgery.
SUMMARY
The goal of the original guidelines was to create a criterion-based progression to protect healing structures and ensure appropriate progression of activities for maximizing patient outcomes. Upon revisiting the original guidelines with a look at the current evidence, we have shown continued support for the foundation of the guidelines. The principles of early weight bearing, incorporation of weight-bearing and non–weight-bearing exercises at the appropriate time frames, and the use of objective measures for determining progression and return to activities continue to have growing support. The role of concomitant injury and subsequent intervention necessitates rehabilitation modification to protect the integrity of the knee. Chondral surgical techniques and continued understanding of the role of the menisci are areas of expanding knowledge with which rehabilitation specialists should become familiar to provide the most up-to-date evidence-based practice. With ACL reconstruction rehabilitation guidelines reaffirmed by the latest evidence and continued understanding of concomitant injuries, the rehabilitation specialist can ensure the best postsurgical outcomes.
APPENDIX
REHABILITATION PRACTICE GUIDELINES FOR ANTERIOR CRUCIATE LIGAMENT (ACL) RECONSTRUCTION
Primary surgery
ACL reconstruction
Assumptions
Isolated ACL injury
Autograft: see specific graft types for precautions
Expected number of visits
25 to 38
Secondary surgery (possible)
See precautions section for modifications
Neuromuscular electrical stimulation (NMES) guidelines
Electrodes placed over proximal lateral quadriceps and distal medial quadriceps (modify distal electrode placement as needed to avoid covering superior medial arthroscopy portal until the stitches have been removed and skin is healed).
Stimulation parameters: 2500 Hz; 75 bursts; 2-second ramp; 12 seconds on, 50 seconds rest; intensity to maximum tolerable (at least 50% maximal volitional isometric contraction [MVIC]); 10 contractions per session. Three sessions per week until quadriceps strength MVIC is 80% of uninvolved side.
Stimulation performed isometrically at 60° (dependent on graft site).
Preoperative goals
Full knee extension range of motion (ROM)
Absent or minimal effusion
No knee extension lag with straight leg raise
Immediate Postoperative Phase (Week 1)
Total visits
1 to 3
Milestones
Knee active/passive ROM, 0° to 90°
Active quadriceps contraction with superior patellar glide
Treatment
Wall slides, patellar mobilization, gait training, NMES (see guidelines), bike for ROM
Home exercise program: supine wall slides, self-patellar mobilizations 30 to 50 times per day, quadriceps set, long-arc quadriceps (90°-45°), and straight leg raise 3 × 10 repetitions (3 times per day)
Early Postoperative Phase (Week 2)
Total visits
4 to 6
Milestones
Knee flexion greater than 110°
Walking without crutches
Use of cycle/stair climber without difficulty
Walking with full knee extension
Reciprocal stair climbing
Straight leg raise without a knee extension lag
Knee Outcome Survey activities of daily living (KOS-ADL) greater than 65%
Treatment
Step-ups in pain-free range
Portal/incision mobilization as needed (if skin is healed)
StairMaster, wall squats/sits
Progress to functional brace as swelling permits
Prone hangs if lacking full extension
Patellar mobilization in flexion (if flexion is limited)
Intermediate Postoperative Phase (Weeks 3-5)
Total visits
7 to 15
Milestones
Knee flexion ROM to within 10° of uninvolved side
Quadriceps strength greater than 60% of uninvolved side
Treatment
Tibiofemoral mobilizations with rotation for ROM if joint mobility is limited
Progress bike and StairMaster duration (10-minute minimum)
Begin balance and proprioceptive activities
Late Postoperative Phase (Weeks 6-8)
Total visits
16 to 25
Milestones
Quadriceps strength greater than 80% of uninvolved side
Normal gait pattern
Full knee ROM (compared to uninvolved side)
Knee effusion of trace or less
Treatment
Progress exercises in intensity and duration
Begin running progression (see running progression below); on treadmill or track with functional brace (if all milestones are met; may vary with physician)
Transfer to fitness facility (if all milestones are met)
Transitional Phase (Weeks 9-12)
Total visits
25 to 38
Milestones
Maintaining or gaining quadriceps strength (greater than 80% of uninvolved side)
Hop tests greater than 85% of uninvolved side (see below) at 12 weeks
KOS-sports questionnaire greater than 70%
Treatment
Sports-specific activities
Agility exercises
Functional testing (see description below)
Follow-up Functional Testing (4 Months, 5 Months, 6 Months, 1 Year Postoperative)
Milestones
Maintaining gains in strength (greater than or equal to 90% to 100%)
Hop test 90% or greater
KOS-sports 90% or greater
Return-to-sport criteria (see below)
Recommend changes in rehabilitation as needed. Progression may emphasize single-leg activities in gym, explosive types of activities (cutting, jumping, plyometrics, landing training)
MVIC
Patient is asked to volitionally extend the involved leg as hard as possible, while knee is maintained isometrically at 60° of knee flexion
Side-to-side comparison (involved/uninvolved × 100 = % MVIC)
Precautions
- Patellar tendon autograft technique
-
-Be aware of patellofemoral forces and possible irritation during progressive resistive exercises
-
-Treat patellofemoral pain if it arises: modalities, possible patellar taping
-
-Consider alteration of knee flexion angle to most comfortable between 45° and 60° for MVIC assessment and NMES treatments
-
-
- Hamstring tendon autograft technique
-
-No resisted hamstring strengthening until week 12
-
-
- Partial meniscectomy
-
-No modifications required; progress per patient tolerance and protocol
-
-
- Meniscal repair
-
-No weight-bearing flexion beyond 45° for 4 weeks
-
-Weight bearing in full extension is allowed
-
-Seated Kinetron and multi-angle quadriceps isometric can substitute for weight-bearing exercises
-
-
- Concomitant abrasion chondroplasty
-
-Weight bearing as tolerated with axillary crutches 3 to 5 days
-
-No modifications required; progress per patient tolerance and protocol
-
-
- Concomitant microfracture (consider location and size of lesion for exercise-specific alterations)
-
-Non–weight bearing 2 to 4 weeks with axillary crutches
-
-No weight-bearing activities in treatment for 4 weeks
-
-
- Chondral repair (osteochondral autograft transfer system, autologous chondrocyte implantation, matrix-induced autologous chondrocyte implantation)
-
-Follow procedure-specific protocol if done concomitantly
-
-
- Meniscal transplantation
-
-Follow procedure-specific protocol if done concomitantly
-
-
- Medial collateral ligament injury
-
-Restrict motion to sagittal plane until weeks 4 to 6 to allow healing of medial collateral ligament
-
-Perform progressive resistive exercises with tibia in internal rotation during early postoperative period to decrease medial collateral ligament stress
-
-Consider brace for exercise and periods of activity if severe sprain and/or patient has pain
-
-Nonrepaired ROM restrictions: grade I, no ROM restrictions; grade II, 0° to 90° in week 1, 0° to 110° in week 2; grade III, 0° to 30° in week 1, 0° to 90° in week 2, 0° to 110° in week 3
-
-
- Posterior cruciate ligament injury
-
-Follow posterior cruciate ligament rehabilitation guidelines (not ACL protocol)
-
-
- Posterolateral corner repair
-
-Minimize external rotation torques and varus stress (6-8 weeks)
-
-Avoid hyperextension
-
-No resisted knee flexion (12 weeks)
-
-
- ACL revision
-
-Delay progression of running, hop testing, agility drills, and return to sport by 4 weeks
-
-Crutches and immobilizer are used for 2 weeks following surgery. Otherwise, follow same milestones
-
-
Running Progression (requires trace or less effusion, 80% or greater strength, understand soreness rules)*
| Level | Treadmill | Track |
|---|---|---|
| Level 1 | 0.1-mi† walk/0.1-mi jog, repeat 10 times | Jog straights/walk curves (2 mi) |
| Level 2 | Alternate 0.1-mi walk/0.2-mi jog (2 mi) | Jog straights/jog 1 curve every other lap (2 mi) |
| Level 3 | Alternate 0.1-mi walk/0.3-mi jog (2 mi) | Jog straights/jog 1 curve every lap (2 mi) |
| Level 4 | Alternate 0.1-mi walk/0.4-mi jog (2 mi) | Jog 1.75 laps/walk curve (2 mi) |
| Level 5 | Jog full 2 mi | Jog all laps (2 mi) |
| Level 6 | Increase workout to 2.5 mi | Increase workout to 2.5 mi |
| Level 7 | Increase workout to 3 mi | Increase workout to 3 mi |
| Level 8 | Alternate between running/jogging every 0.25 mi | Increase speed on straights/jog curves |
*Conversion: 1 mi = 1.6 km.
Progress to next level when patient is able to perform activity for 2 mi without increased effusion or pain. Perform no more than 4 times in 1 week and no more frequently than every other day. Do not progress more than 2 levels in a 7-day period.
Functional Testing (Week 12)
Testing
Patient performs 2 practice trials on each leg for each hop sequence
Patient performs 2 timed or measured trials on each leg for each hop sequence
Measured trials are averaged and compared (involved to uninvolved) for single, triple, and crossover hop
Measured trials are averaged and compared (uninvolved to involved) for timed hop
Passing criteria for return to sport
Greater than or equal to 90% on quadriceps MVIC, hop testing, KOS-ADL score, and global rating of knee function score
Reprinted with permission from Tara Manal, University of Delaware Physical Therapy Clinic.
REFERENCES
- 1.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34:128–135. doi: 10.1177/0363546505280214. http://dx.doi.org/10.1177/0363546505280214. [DOI] [PubMed] [Google Scholar]
- 2.Anderson DD, Chubinskaya S, Guilak F, et al. Post-traumatic osteoarthritis: improved understanding and opportunities for early intervention. J Orthop Res. 2011;29:802–809. doi: 10.1002/jor.21359. http://dx.doi.org/10.1002/jor.21359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ardern CL, Webster KE, Taylor NF, Feller JA. Hamstring strength recovery after hamstring tendon harvest for anterior cruciate ligament reconstruction: a comparison between graft types. Arthroscopy. 2010;26:462–469. doi: 10.1016/j.arthro.2009.08.018. http://dx.doi.org/10.1016/j.arthro.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 4.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39:538–543. doi: 10.1177/0363546510384798. http://dx.doi.org/10.1177/0363546510384798. [DOI] [PubMed] [Google Scholar]
- 5.Barber FA. Accelerated rehabilitation for meniscus repairs. Arthroscopy. 1994;10:206–210. doi: 10.1016/s0749-8063(05)80095-7. [DOI] [PubMed] [Google Scholar]
- 6.Barber FA, Click SD. Meniscus repair rehabilitation with concurrent anterior cruciate reconstruction. Arthroscopy. 1997;13:433–437. doi: 10.1016/s0749-8063(97)90120-1. [DOI] [PubMed] [Google Scholar]
- 7.Barber SD, Noyes FR, Mangine R, DeMaio M. Rehabilitation after ACL reconstruction: function testing. Orthopedics. 1992;15:969–974. doi: 10.3928/0147-7447-19920801-17. [DOI] [PubMed] [Google Scholar]
- 8.Benjaminse A, Gokeler A, van der Schans CP. Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther. 2006;36:267–288. doi: 10.2519/jospt.2006.2011. http://dx.doi.org/10.2519/jospt.2006.2011. [DOI] [PubMed] [Google Scholar]
- 9.Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009;37:2362–2367. doi: 10.1177/0363546509340633. http://dx.doi.org/10.1177/0363546509340633. [DOI] [PubMed] [Google Scholar]
- 10.Brotzman SB, Wilk KE. Clinical Orthopaedic Rehabilitation. 2nd ed. Mosby; St Louis, MO: 2003. [Google Scholar]
- 11.Bynum EB, Barrack RL, Alexander AH. Open versus closed chain kinetic exercises after anterior cruciate ligament reconstruction. A prospective randomized study. Am J Sports Med. 1995;23:401–406. doi: 10.1177/036354659502300405. [DOI] [PubMed] [Google Scholar]
- 12.Carey JL, Dunn WR, Dahm DL, Zeger SL, Spindler KP. A systematic review of anterior cruciate ligament reconstruction with autograft compared with allograft. J Bone Joint Surg Am. 2009;91:2242–2250. doi: 10.2106/JBJS.I.00610. http://dx.doi.org/10.2106/JBJS.I.00610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carter TR, Edinger S. Isokinetic evaluation of anterior cruciate ligament reconstruction: hamstring versus patellar tendon. Arthroscopy. 1999;15:169–172. doi: 10.1053/ar.1999.v15.0150161. http://dx.doi.org/10.1053/ar.1999.v15.0150161. [DOI] [PubMed] [Google Scholar]
- 14.Chmielewski TL, Stackhouse S, Axe MJ, Snyder-Mackler L. A prospective analysis of incidence and severity of quadriceps inhibition in a consecutive sample of 100 patients with complete acute anterior cruciate ligament rupture. J Orthop Res. 2004;22:925–930. doi: 10.1016/j.orthres.2004.01.007. http://dx.doi.org/10.1016/j.orthres.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 15.Clark JC, Rueff DE, Indelicato PA, Moser M. Primary ACL reconstruction using allograft tis-sue. Clin Sports Med. 2009;28:223–244. doi: 10.1016/j.csm.2008.10.005. http://dx.doi.org/10.1016/j.csm.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Cooper RL, Taylor NF, Feller JA. A systematic review of the effect of proprioceptive and balance exercises on people with an injured or reconstructed anterior cruciate ligament. Res Sports Med. 2005;13:163–178. doi: 10.1080/15438620590956197. http://dx.doi.org/10.1080/15438620590956197. [DOI] [PubMed] [Google Scholar]
- 17.de Jong SN, van Caspel DR, van Haeff MJ, Saris DB. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23:21.e1–21.e11. doi: 10.1016/j.arthro.2006.08.024. http://dx.doi.org/10.1016/j.arthro.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 18.Denti M, Lo Vetere D, Bait C, Schonhuber H, Melegati G, Volpi P. Revision anterior cruciate ligament reconstruction: causes of failure, surgical technique, and clinical results. Am J Sports Med. 2008;36:1896–1902. doi: 10.1177/0363546508318189. http://dx.doi.org/10.1177/0363546508318189. [DOI] [PubMed] [Google Scholar]
- 19.Dunn WR, Spindler KP. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38:2040–2050. doi: 10.1177/0363546510370280. http://dx.doi.org/10.1177/0363546510370280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edson CJ. Conservative and postoperative rehabilitation of isolated and combined injuries of the medial collateral ligament. Sports Med Arthrosc. 2006;14:105–110. doi: 10.1097/01.jsa.0000212308.32076.f2. http://dx.doi.org/10.1097/01.jsa.0000212308.32076.f2. [DOI] [PubMed] [Google Scholar]
- 21.Eitzen I, Eitzen TJ, Holm I, Snyder-Mackler L, Risberg MA. Anterior cruciate ligament-deficient potential copers and noncopers reveal different isokinetic quadriceps strength profiles in the early stage after injury. Am J Sports Med. 2010;38:586–593. doi: 10.1177/0363546509349492. http://dx.doi.org/10.1177/0363546509349492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43:371–376. doi: 10.1136/bjsm.2008.057059. http://dx.doi.org/10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 23.Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A progressive 5-week exercise therapy program leads to significant improvement in knee function early after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2010;40:705–721. doi: 10.2519/jospt.2010.3345. http://dx.doi.org/10.2519/jospt.2010.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fees M, Decker T, Snyder-Mackler L, Axe MJ. Upper extremity weight-training modifications for the injured athlete. A clinical perspective. Am J Sports Med. 1998;26:732–742. doi: 10.1177/03635465980260052301. [DOI] [PubMed] [Google Scholar]
- 25.Fitzgerald GK, Axe MJ, Snyder-Mackler L. Proposed practice guidelines for nonoperative anterior cruciate ligament rehabilitation of physically active individuals. J Orthop Sports Phys Ther. 2000;30:194–203. doi: 10.2519/jospt.2000.30.4.194. [DOI] [PubMed] [Google Scholar]
- 26.Fitzgerald GK, Lephart SM, Hwang JH, Wainner RS. Hop tests as predictors of dynamic knee stability. J Orthop Sports Phys Ther. 2001;31:588–597. doi: 10.2519/jospt.2001.31.10.588. [DOI] [PubMed] [Google Scholar]
- 27.Fox JA, Pierce M, Bojchuk J, Hayden J, Bush-Joseph CA, Bach BR., Jr. Revision anterior cruciate ligament reconstruction with nonirradiated fresh-frozen patellar tendon allograft. Arthroscopy. 2004;20:787–794. doi: 10.1016/j.arthro.2004.07.019. http://dx.doi.org/10.1016/j.arthro.2004.07.019. [DOI] [PubMed] [Google Scholar]
- 28.George MS, Dunn WR, Spindler KP. Current concepts review: revision anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34:2026–2037. doi: 10.1177/0363546506295026. http://dx.doi.org/10.1177/0363546506295026. [DOI] [PubMed] [Google Scholar]
- 29.Goodstadt N, Snyder-Mackler L, Axe M. Functional testing to discontinue brace use for sport after ACL reconstruction. Med Sci Sports Exerc. 2010;42:96. http://dx.doi.org/10.1249/01.MSS.0000385652.64740.7b. [PMC free article] [PubMed] [Google Scholar]
- 30.Graf BK, Ott JW, Lange RH, Keene JS. Risk factors for restricted motion after anterior cruciate reconstruction. Orthopedics. 1994;17:909–912. doi: 10.3928/0147-7447-19941001-07. [DOI] [PubMed] [Google Scholar]
- 31.Grindem H, Logerstedt D, Eitzen I, et al. Single-legged hop tests as predictors of self-reported knee function in nonoperatively treated individuals with anterior cruciate ligament injury. Am J Sports Med. 2011;39:2347–2354. doi: 10.1177/0363546511417085. http://dx.doi.org/10.1177/0363546511417085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gulotta LV, Rodeo SA. Biology of autograft and allograft healing in anterior cruciate ligament reconstruction. Clin Sports Med. 2007;26:509–524. doi: 10.1016/j.csm.2007.06.007. http://dx.doi.org/10.1016/j.csm.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 33.Hapa O, Barber FA. ACL fixation devices. Sports Med Arthrosc. 2009;17:217–223. doi: 10.1097/JSA.0b013e3181bf668c. http://dx.doi.org/10.1097/JSA.0b013e3181bf668c. [DOI] [PubMed] [Google Scholar]
- 34.Harris JD, Brophy RH, Siston RA, Flanigan DC. Treatment of chondral defects in the athlete’s knee. Arthroscopy. 2010;26:841–852. doi: 10.1016/j.arthro.2009.12.030. http://dx.doi.org/10.1016/j.arthro.2009.12.030. [DOI] [PubMed] [Google Scholar]
- 35.Hartigan E, Axe MJ, Snyder-Mackler L. Perturbation training prior to ACL reconstruction improves gait asymmetries in non-copers. J Orthop Res. 2009;27:724–729. doi: 10.1002/jor.20754. http://dx.doi.org/10.1002/jor.20754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40:141–154. doi: 10.2519/jospt.2010.3168. http://dx.doi.org/10.2519/jospt.2010.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harvey A, Thomas NP, Amis AA. Fixation of the graft in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2005;87:593–603. doi: 10.1302/0301-620X.87B5.15803. http://dx.doi.org/10.1302/0301-620X.87B5.15803. [DOI] [PubMed] [Google Scholar]
- 38.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27:699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 39.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33:492–501. doi: 10.1177/0363546504269591. http://dx.doi.org/10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 40.Hurd WJ, Axe MJ, Snyder-Mackler L. Influence of age, gender, and injury mechanism on the development of dynamic knee stability after acute ACL rupture. J Orthop Sports Phys Ther. 2008;38:36–41. doi: 10.2519/jospt.2008.2609. http://dx.doi.org/10.2519/jospt.2008.2609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ichiba A, Nakajima M, Fujita A, Abe M. The effect of medial collateral ligament insufficiency on the reconstructed anterior cruciate ligament: a study in the rabbit. Acta Orthop Scand. 2003;74:196–200. doi: 10.1080/00016470310013950. http://dx.doi.org/10.1080/00016470310013950. [DOI] [PubMed] [Google Scholar]
- 42.Ingersoll CD, Grindstaff TL, Pietrosimone BG, Hart JM. Neuromuscular consequences of anterior cruciate ligament injury. Clin Sports Med. 2008;27:383–404. doi: 10.1016/j.csm.2008.03.004. http://dx.doi.org/10.1016/j.csm.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 43.Irrgang JJ, Harner CD, Fu FH, Silbey MB, DiGiacomo R. Loss of motion following ACL reconstruction: a second look. J Sport Rehabil. 1997;6:213–225. [Google Scholar]
- 44.Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 2001;17:971–980. doi: 10.1053/jars.2001.28979. http://dx.doi.org/10.1053/jars.2001.28979. [DOI] [PubMed] [Google Scholar]
- 45.Keays SL, Bullock-Saxton J, Keays AC, Newcombe P. Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendonosus and gracilis. Knee. 2001;8:229–234. doi: 10.1016/s0968-0160(01)00099-0. [DOI] [PubMed] [Google Scholar]
- 46.Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI. A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and gracilis tendon graft. Am J Sports Med. 2007;35:729–739. doi: 10.1177/0363546506298277. http://dx.doi.org/10.1177/0363546506298277. [DOI] [PubMed] [Google Scholar]
- 47.Keays SL, Bullock-Saxton JE, Newcombe P, Keays AC. The relationship between knee strength and functional stability before and after anterior cruciate ligament reconstruction. J Orthop Res. 2003;21:231–237. doi: 10.1016/S0736-0266(02)00160-2. http://dx.doi.org/10.1016/S0736-0266(02)00160-2. [DOI] [PubMed] [Google Scholar]
- 48.Kim KM, Croy T, Hertel J, Saliba S. Effects of neuromuscular electrical stimulation after anterior cruciate ligament reconstruction on quadriceps strength, function, and patient-oriented outcomes: a systematic review. J Orthop Sports Phys Ther. 2010;40:383–391. doi: 10.2519/jospt.2010.3184. http://dx.doi.org/10.2519/jospt.2010.3184. [DOI] [PubMed] [Google Scholar]
- 49.Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins RJ. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2002;84-A:1560–1572. doi: 10.2106/00004623-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 50.Kowalchuk DA, Harner CD, Fu FH, Irrgang JJ. Prediction of patient-reported outcome after single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009;25:457–463. doi: 10.1016/j.arthro.2009.02.014. http://dx.doi.org/10.1016/j.arthro.2009.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Krych AJ, Jackson JD, Hoskin TL, Dahm DL. A meta-analysis of patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction. Arthroscopy. 2008;24:292–298. doi: 10.1016/j.arthro.2007.08.029. http://dx.doi.org/10.1016/j.arthro.2007.08.029. [DOI] [PubMed] [Google Scholar]
- 52.Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon) 2002;17:56–63. doi: 10.1016/s0268-0033(01)00097-3. [DOI] [PubMed] [Google Scholar]
- 53.Lewis PB, McCarty LP, 3rd, Kang RW, Cole BJ. Basic science and treatment options for articular cartilage injuries. J Orthop Sports Phys Ther. 2006;36:717–727. doi: 10.2519/jospt.2006.2175. http://dx.doi.org/10.2519/jospt.2006.2175. [DOI] [PubMed] [Google Scholar]
- 54.Logerstedt D. Restoring knee function: physical impairment measures, activity limitations, and patient-reported outcomes after anterior cruciate ligament injury, surgery, and rehabilitation [thesis] University of Delaware; Newark, DE: 2011. [Google Scholar]
- 55.Logerstedt D, Sennett BJ. Case series utilizing drop-out casting for the treatment of knee joint extension motion loss following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2007;37:404–411. doi: 10.2519/jospt.2007.2466. http://dx.doi.org/10.2519/jospt.2007.2466. [DOI] [PubMed] [Google Scholar]
- 56.Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ. Knee pain and mobility impairments: meniscal and articular cartilage lesions. J Orthop Sports Phys Ther. 2010;40:A1–A35. doi: 10.2519/jospt.2010.0304. http://dx.doi.org/10.2519/jospt.2010.0304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Maeda A, Shino K, Horibe S, Nakata K, Buccafusca G. Anterior cruciate ligament reconstruction with multistranded autogenous semitendinosus tendon. Am J Sports Med. 1996;24:504–509. doi: 10.1177/036354659602400416. [DOI] [PubMed] [Google Scholar]
- 58.Manal TJ, Snyder-Mackler L. Practice guidelines for anterior cruciate ligament rehabilitation: a criterion-based rehabilitation progression. Oper Tech Orthop. 1996;6:190–196. http://dx.doi.org/10.1016/S1048-6666(96)80019-X. [Google Scholar]
- 59.Mariani PP, Santori N, Adriani E, Mastantuono M. Accelerated rehabilitation after arthroscopic meniscal repair: a clinical and magnetic resonance imaging evaluation. Arthroscopy. 1996;12:680–686. doi: 10.1016/s0749-8063(96)90170-x. [DOI] [PubMed] [Google Scholar]
- 60.Mauro CS, Irrgang JJ, Williams BA, Harner CD. Loss of extension following anterior cruciate ligament reconstruction: analysis of incidence and etiology using IKDC criteria. Arthroscopy. 2008;24:146–153. doi: 10.1016/j.arthro.2007.08.026. http://dx.doi.org/10.1016/j.arthro.2007.08.026. [DOI] [PubMed] [Google Scholar]
- 61.McGrath MS, Mont MA, Siddiqui JA, Baker E, Bhave A. Evaluation of a custom device for the treatment of flexion contractures after total knee arthroplasty. Clin Orthop Relat Res. 2009:1485–1492. doi: 10.1007/s11999-009-0804-z. http://dx.doi.org/10.1007/s11999-009-0804-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Medvecky MJ, Zazulak BT, Hewett TE. A multidisciplinary approach to the evaluation, reconstruction and rehabilitation of the multi-ligament injured athlete. Sports Med. 2007;37:169–187. doi: 10.2165/00007256-200737020-00005. [DOI] [PubMed] [Google Scholar]
- 63.Mikkelsen C, Werner S, Eriksson E. Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg Sports Traumatol Arthrosc. 2000;8:337–342. doi: 10.1007/s001670000143. [DOI] [PubMed] [Google Scholar]
- 64.Mithoefer K, Hambly K, Della Villa S, Silvers H, Mandelbaum BR. Return to sports participation after articular cartilage repair in the knee: scientific evidence. Am J Sports Med. 2009;37(suppl 1):167S–176S. doi: 10.1177/0363546509351650. http://dx.doi.org/10.1177/0363546509351650. [DOI] [PubMed] [Google Scholar]
- 65.Moksnes H, Engebretsen L, Risberg MA. Performance-based functional outcome for children 12 years or younger following anterior cruciate ligament injury: a two to nine-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2008;16:214–223. doi: 10.1007/s00167-007-0469-7. http://dx.doi.org/10.1007/s00167-007-0469-7. [DOI] [PubMed] [Google Scholar]
- 66.Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34:445–455. doi: 10.1177/0363546505281241. http://dx.doi.org/10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 67.Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36:385–402. doi: 10.2519/jospt.2006.2222. http://dx.doi.org/10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
- 68.Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41:377–387. doi: 10.2519/jospt.2011.3547. http://dx.doi.org/10.2519/jospt.2011.3547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Myklebust G, Bahr R. Return to play guidelines after anterior cruciate ligament surgery. Br J Sports Med. 2005;39:127–131. doi: 10.1136/bjsm.2004.010900. http://dx.doi.org/10.1136/bjsm.2004.010900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 71.Noyes FR, Mooar PA, Matthews DS, Butler DL. The symptomatic anterior cruciate-deficient knee. Part I: the long-term functional disability in athletically active individuals. J Bone Joint Surg Am. 1983;65:154–162. doi: 10.2106/00004623-198365020-00003. [DOI] [PubMed] [Google Scholar]
- 72.Nyland J, Cook C, Keen J, Caborn DN. Lower extremity neuromuscular recovery following anterior cruciate ligament reconstruction; a 2-week case study. Electromyogr Clin Neurophysiol. 2003;43:41–49. [PubMed] [Google Scholar]
- 73.Osti L, Papalia R, Del Buono A, Merlo F, Denaro V, Maffulli N. Simultaneous surgical management of chronic grade-2 valgus instability of the knee and anterior cruciate ligament deficiency in athletes. Knee Surg Sports Traumatol Arthrosc. 2010;18:312–316. doi: 10.1007/s00167-009-0966-y. http://dx.doi.org/10.1007/s00167-009-0966-y. [DOI] [PubMed] [Google Scholar]
- 74.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med. 2008;27:405–424. doi: 10.1016/j.csm.2008.02.001. http://dx.doi.org/10.1016/j.csm.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 75.Petersen W, Laprell H. Combined injuries of the medial collateral ligament and the anterior cruciate ligament. Early ACL reconstruction versus late ACL reconstruction. Arch Orthop Trauma Surg. 1999;119:258–262. doi: 10.1007/s004020050405. [DOI] [PubMed] [Google Scholar]
- 76.Pyne SW. Current progress in meniscal repair and postoperative rehabilitation. Curr Sports Med Rep. 2002;1:265–271. doi: 10.1249/00149619-200210000-00003. [DOI] [PubMed] [Google Scholar]
- 77.Reinold MM, Wilk KE, Macrina LC, Dugas JR, Cain EL. Current concepts in the rehabilitation following articular cartilage repair procedures in the knee. J Orthop Sports Phys Ther. 2006;36:774–794. doi: 10.2519/jospt.2006.2228. http://dx.doi.org/10.2519/jospt.2006.2228. [DOI] [PubMed] [Google Scholar]
- 78.Risberg MA, Ekeland A. Assessment of functional tests after anterior cruciate ligament surgery. J Orthop Sports Phys Ther. 1994;19:212–217. doi: 10.2519/jospt.1994.19.4.212. [DOI] [PubMed] [Google Scholar]
- 79.Risberg MA, Holm I. The long-term effect of 2 postoperative rehabilitation programs after anterior cruciate ligament reconstruction: a randomized controlled clinical trial with 2 years of follow-up. Am J Sports Med. 2009;37:1958–1966. doi: 10.1177/0363546509335196. http://dx.doi.org/10.1177/0363546509335196. [DOI] [PubMed] [Google Scholar]
- 80.Risberg MA, Holm I, Myklebust G, Engebretsen L. Neuromuscular training versus strength training during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys Ther. 2007;87:737–750. doi: 10.2522/ptj.20060041. http://dx.doi.org/10.2522/ptj.20060041. [DOI] [PubMed] [Google Scholar]
- 81.Risberg MA, Holm I, Tjomsland O, Ljunggren E, Ekeland A. Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29:400–412. doi: 10.2519/jospt.1999.29.7.400. [DOI] [PubMed] [Google Scholar]
- 82.Risberg MA, Moksnes H, Storevold A, Holm I, Snyder-Mackler L. Rehabilitation after anterior cruciate ligament injury influences joint loading during walking but not hopping. Br J Sports Med. 2009;43:423–428. doi: 10.1136/bjsm.2008.056846. http://dx.doi.org/10.1136/bjsm.2008.056846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ross MD, Irrgang JJ, Denegar CR, McCloy CM, Unangst ET. The relationship between participation restrictions and selected clinical measures following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2002;10:10–19. doi: 10.1007/s001670100238. http://dx.doi.org/10.1007/s001670100238. [DOI] [PubMed] [Google Scholar]
- 84.Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med. 2006;34:1933–1940. doi: 10.1177/0363546506290726. http://dx.doi.org/10.1177/0363546506290726. [DOI] [PubMed] [Google Scholar]
- 85.Samuelsson K, Andersson D, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy. 2009;25:1139–1174. doi: 10.1016/j.arthro.2009.07.021. http://dx.doi.org/10.1016/j.arthro.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 86.Shelbourne KD, Gray T. Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med. 2009;37:471–480. doi: 10.1177/0363546508326709. http://dx.doi.org/10.1177/0363546508326709. [DOI] [PubMed] [Google Scholar]
- 87.Shelbourne KD, Vanadurongwan B, Gray T. Primary anterior cruciate ligament reconstruction using contralateral patellar tendon autograft. Clin Sports Med. 2007;26:549–565. doi: 10.1016/j.csm.2007.06.008. http://dx.doi.org/10.1016/j.csm.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 88.Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19:332–336. doi: 10.1177/036354659101900402. [DOI] [PubMed] [Google Scholar]
- 89.Siebold R, Dehler C, Ellert T. Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2008;24:137–145. doi: 10.1016/j.arthro.2007.11.013. http://dx.doi.org/10.1016/j.arthro.2007.11.013. [DOI] [PubMed] [Google Scholar]
- 90.Snyder-Mackler L, Delitto A, Bailey SL, Stralka SW. Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. A prospective, randomized clinical trial of electrical stimulation. J Bone Joint Surg Am. 1995;77:1166–1173. doi: 10.2106/00004623-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 91.Snyder-Mackler L, Delitto A, Stralka SW, Bailey SL. Use of electrical stimulation to enhance recovery of quadriceps femoris muscle force production in patients following anterior cruciate ligament reconstruction. Phys Ther. 1994;74:901–907. doi: 10.1093/ptj/74.10.901. [DOI] [PubMed] [Google Scholar]
- 92.Spindler KP, Huston LJ, Wright RW, et al. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med. 2011;39:348–359. doi: 10.1177/0363546510383481. http://dx.doi.org/10.1177/0363546510383481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE., Jr. Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32:1986–1995. doi: 10.1177/0363546504271211. [DOI] [PubMed] [Google Scholar]
- 94.Starke C, Kopf S, Petersen W, Becker R. Meniscal repair. Arthroscopy. 2009;25:1033–1044. doi: 10.1016/j.arthro.2008.12.010. http://dx.doi.org/10.1016/j.arthro.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 95.Sturgill LP, Snyder-Mackler L, Manal TJ, Axe MJ. Interrater reliability of a clinical scale to assess knee joint effusion. J Orthop Sports Phys Ther. 2009;39:845–849. doi: 10.2519/jospt.2009.3143. http://dx.doi.org/10.2519/jospt.2009.3143. [DOI] [PubMed] [Google Scholar]
- 96.Tibor LM, Long JL, Schilling PL, Lilly RJ, Carpenter JE, Miller BS. Clinical outcomes after anterior cruciate ligament reconstruction: a meta-analysis of autograft versus allograft tissue. Sports Health. 2010;2:56–72. doi: 10.1177/1941738109347984. http://dx.doi.org/10.1177/1941738109347984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Toman CV, Dunn WR, Spindler KP, et al. Success of meniscal repair at anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37:1111–1115. doi: 10.1177/0363546509337010. http://dx.doi.org/10.1177/0363546509337010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9:9–15. doi: 10.1016/j.ptsp.2007.09.003. http://dx.doi.org/10.1016/j.ptsp.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 99.Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;20:60–73. doi: 10.2519/jospt.1994.20.2.60. [DOI] [PubMed] [Google Scholar]
- 100.Williams GN, Snyder-Mackler L, Barrance PJ, Axe MJ, Buchanan TS. Muscle and tendon morphology after reconstruction of the anterior cruciate ligament with autologous semitendinosus-gracilis graft. J Bone Joint Surg Am. 2004;86-A:1936–1946. doi: 10.2106/00004623-200409000-00012. [DOI] [PubMed] [Google Scholar]
- 101.Yasuda K, Tsujino J, Ohkoshi Y, Tanabe Y, Kaneda K. Graft site morbidity with autogenous semitendinosus and gracilis tendons. Am J Sports Med. 1995;23:706–714. doi: 10.1177/036354659502300613. [DOI] [PubMed] [Google Scholar]