Abstract
Background
Sixty percent (60%) to 80% of patients who visit chiropractic, osteopathic, or Chinese medicine practitioners are seeking pain relief.
Objectives
This article aimed to identify the amount, quality, and type of complementary and alternative medicine (CAM) pain research in Australia by systematically and critically reviewing the literature.
Methods
PubMed, Scopus, Australasian Medical Index, and Cochrane library were searched from their inception to July 2009. Australian and New Zealand Clinical Trial Registration and National Health and Medical Research Council databases were searched for human studies yet to be completed. Predefined search terms and selection criteria were used for data identification.
Results
Of 204 studies selected, 54% were on chiropractic, 27% on Chinese medicine, 15% about multitherapy, and 4% on osteopathy. Chronic spinal pain was the most studied condition, with visceral pain being the least studied. Half of the articles in Chinese medicine or multitherapy were systematic reviews or randomized control trials. In comparison, only 5% of chiropractic and none of osteopathy studies were in these categories. Government funding was rare, and most studies were self-funded or internally funded. All chiropractic, osteopathic, and Chinese herbal medicine studies were conducted by the researchers of the professions. In contrast, half of the acupuncture studies and all t'ai chi studies were conducted by medical doctors or physiotherapists. Multidisciplinary collaboration was uncommon.
Conclusions
The quantity and the quality of CAM pain research in Australia are inconsistent with the high utilization of the relevant CAM therapies by Australians. A substantial increase in government funding is required. Collaborative research examining the multimodality or multidisciplinary approach is needed.
Introduction
One in 5 Australians suffers from persistent pain.1 Many of them seek pain relief and improvement in quality of life from complementary and alternative medicine (CAM) products and therapists. A computer-assisted telephone interview national population survey shows that pain is the leading reason that one quarter of Australians are using one of the three CAM therapies: acupuncture, chiropractic, and osteopathy.2 Furthermore, 40%–60% of Australians or Americans who visited acupuncture clinics come because of musculoskeletal pain or headache3,4; and 67%–72% who visited chiropractic or osteopath come for treatment of low-back pain, neck pain, thoracic pain, or headache.5,6
Given the wide use of CAM for pain relief, and the importance of clinical evidence in guiding the population in the use of CAM, in policy-making, and in identifying research direction, it is essential that the level of pain research activities in CAM in Australia be identified.
CAM is referred to as “medical and health care systems, practices, and products that are not generally considered part of conventional medicine,”7 and consists of a wide range of therapies. The definition of CAM is evolving and fluid. For instance, in Australia, acupuncture is considered a form of CAM, but many medical doctors provide acupuncture treatment and to them it is mainstream even though the National Health and Medical Research Council (NHMRC) considers acupuncture a form of CAM. Spinal manipulation is a key therapy provided by practitioners in physiotherapy, chiropractic, and osteopathy. The former is a form of allied health, whereas the latter two are CAMs.
This review focused on the commonly used CAM for pain relief and the professions that are and will be nationally registered by 2012, namely chiropractic, osteopathy, and Chinese medicine, including Chinese herbal medicine, acupuncture and t'ai chi. These professions have 4–5-year bachelor or master programs at public universities, including RMIT University (RMIT), Victoria University (VU; this program closed at the end of 2009), University of Western Sydney (UWS), University Technology of Sydney (UTS), Macquarie University (Macquarie), and Murdoch University (Murdoch).
Through systematically reviewing existing data, the aim was to identify the types of CAM research in pain in Australia, the background of the researchers, and the funding sources. This review intended neither to assess efficacy or effectiveness of various CAM therapies, nor to examine other areas of CAM research in this country, such as hay fever, cancer or women's health.
Methods
Search methods
PubMed, Scopus, Australasian Medical Index, and Cochrane library were searched from their inception to July 2009 to identify CAM research in pain carried out by Australian researchers. Search terms used were pain, acupuncture, electroacupuncture, dry needling, laser acupuncture, laser therapy, t'ai chi, chiropractic, osteopathy, spinal manipulation, joint mobilization, and herbal medicine. Medical Subject Headings (MeSH) terms were used when possible. Affiliation of the authors was limited to “Australia.” A sample search strategy is included in Appendix 1.
Databases of the Australian and New Zealand Clinical Trial Registration (ANZCTR) and NHMRC were searched for human studies yet to be completed.
Study selection
Included studies had to meet all of the following criteria: (1) one of the authors had to be affiliated with an Australian institution; (2) the study population had to be humans; (3) at least one of the interested professions or interventions was assessed as the main or a component of a combined therapy; (4) the study condition had to be pain or pain related, such as musculoskeletal conditions; and (5) the studies must have been published in a peer-reviewed journal.
Studies about spinal manipulation were only included if the intervention was delivered by a chiropractor or an osteopath practitioner, and were excluded if the therapy was delivered by physiotherapists.
Also excluded were studies examining public usage or opinion about the interested professions, comments, book reviews, letters to the editors, and animal research.
Data extraction and analysis
Data including the author, affiliation, type of research or publication, types of pain, number of participants, source of funding, and journal titles were extracted, and were summarized quantitatively and qualitatively as appropriate. Descriptive data are presented.
Results
A summary of published studies
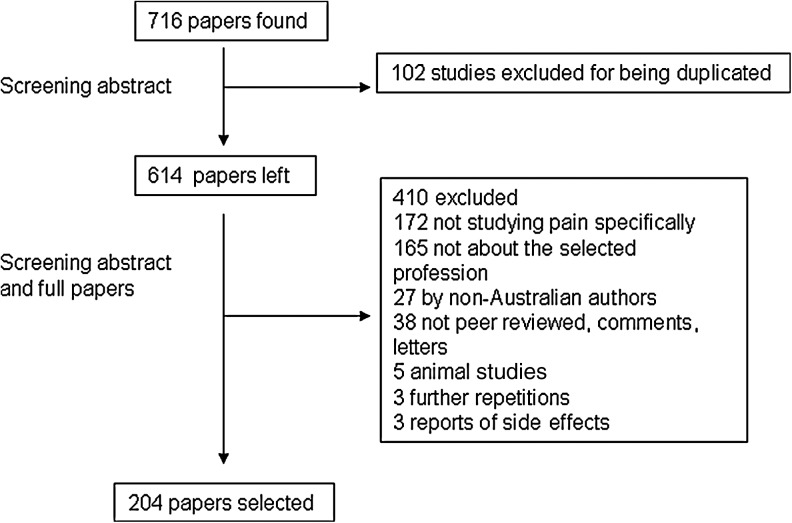
The search results are illustrated in Figure 1. Two hundred and four (204) out of 716 articles identified met the selection criteria. Nearly one third of studies were identified from PubMed search, one third from the Australasian Medical Index, and the remaining one third from Scopus search.
FIG. 1.
A flowchart of the study selection.
Table 1 summarizes the types of publications within each professional discipline. Data are organized according to whether monotherapy or multitherapy was studied. For instance, a trial comparing acupuncture with sham acupuncture was a monotherapy study. A trial comparing acupuncture with spinal manipulation or a review including all types of complementary therapies were multitherapy. All case reports were considered as monotherapy studies and were allocated to the professional category to which the author(s) belonged.
Table 1.
Types of Included Articles
| Types of intervention | No. of included studies (% of total articles) | SR | RCT | Protocol of RCT or SR | CT or cohort study | Uncontrolled | Follow up of RCT | Reliability and / or validity | Case control | Cross-sectional survey | Audit | Descriptive review | Case report | Discussion | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chinese medicine | Acupuncture | 50 (24.5) | 6 | 15 | 1 | 3 | 2 | 1 | 2 | 7 | 7 | 6 | |||
| T'ai chi | 3 (1.5) | 1 | 1 | 1 | |||||||||||
| Herbal medicine | 2 (1.0) | 1 | 1 | ||||||||||||
| Chiropractic | 111 (54) | 2 | 5 | 1 | 6 | 4 | 5 | 1 | 12 | 6 | 22 | 37 | 11 | ||
| Osteopath | 8 (4) | 1 | 2 | 1 | 2 | 2 | |||||||||
| Multi | 30 (15) | 11 | 4 | 1 | 1 | 1 | 6 | 1 | 5 | ||||||
| Total | 204 (100) | 21 | 24 | 4 | 11 | 8 | 1 | 9 | 36 | 45 | 17 |
SR, systematic review; RCT, randomized controlled trial; CT, controlled trial.
Fifty-four percent (54%) of the included studies were about chiropractic, followed by Chinese medicine (27%), and multitherapy (15%). Only eight studies were about osteopathy (4%).
Systematic review (SR) and randomized controlled trials (RCTs) provide a higher level of evidence when compared with case reports and descriptive reviews.8 Nearly half of the articles on Chinese medicine (47%) and multitherapy (53%) are in the former category. In contrast, only 7% of the studies on chiropractic are in this category, and none in osteopathy.
Within multitherapy studies, three RCTs in this category compared CAM therapies with standard medical treatment, and one compared spinal manipulation delivered by medical doctors or physiotherapists with that by chiropractors. SRs reviewed conservative therapies, noninvasive therapy, all forms of physical interventions and complementary therapies.
Types of pain studied
Table 2 summarizes the types of pain conditions studied. Over half of the studies were on spinal or trunk pain, including neck, thoracic, low back, and chest pain; 15% of location not specified, such as rheumatoid arthritis, widespread pain, fibromyalgia, or “musculoskeletal pain.” More than half of the studies (55%) reviewed did not specify the duration of pain; and nearly a third (31%) were on chronic pain. Visceral and acute pains were not commonly studied.
Table 2.
Types of Pain Conditions
| |
|
Types of clinical pain |
|
|
|
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
|
|
|
Musculoskeletal pain |
Duration of pain |
Others |
||||||
| Types of pain | Experimental pain | Visceral pain | Head or facial pain including TTH, migraine, facial pain) | Spinal pain and trunk | Shoulder or arm pain | Hip or knee pain (lower extremity) | Hand or foot pain | Location not specified | Acute pain and sub acute pain (<3 mo) | Chronic pain (>3 mo) | Not specified | About education or outcome measures of pain |
| Acupuncture | 4 | 1 | 2 | 17 | 4 | 4 | 1 | 17 | 6 | 23 | 21 | 0 |
| T'ai chi | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 1 | 0 | 3 | 0 | 0 |
| Herbal medicine | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 |
| Chiropractic | 0 | 2 | 9 | 66 | 11 | 6 | 4 | 9 | 12 | 27 | 68 | 4 |
| Osteopathy | 0 | 1 | 7 | 0 | 0 | 3 | 5 | 0 | ||||
| Multitherapy | 0 | 2 | 3 | 16 | 1 | 4 | 0 | 4 | 6 | 7 | 17 | 0 |
| Total (% of all articles) | 4 (2.0) | 6 (2.9) | 15 (7.3) | 108 (53) | 16 (7.8) | 15 (7.3) | 5 (2.5) | 31 (15) | 24 (12) | 64 (31) | 112 (55) | 4 (2.0) |
TTH, tension-type headache.
Details of the SRs and RCTs
SRs or RCTs were conducted by whom, about what, and when?
As illustrated in Table 3, nearly half of 22 SRs and RCTs of acupuncture were conducted by qualified researchers from RMIT, UTS, and VU, and the other half were by medical or physiotherapy researchers from the University of Melbourne (Melbourne), Monash University (Monash), and Queensland University (QU). All RCTs were sham procedure controlled. Two (2) pain studies with Chinese herbal medicine were by researchers from the professions, whereas two t'ai chi studies were by physiotherapists.
Table 3.
Details of Systematic Reviews and Randomized Controlled Trials
| Total number | Is 1st author in the profession? (Y) | If N, what is the profession?Med | Physcio | Psycho | Other CAM | Is there more than one author? (Y / N) | Is one of the CAM teaching institute involved (any coauthors?) | Is there collaboration with other profession? (Y/N) | Sta/epid | Med | Physio | CAM | Others | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Acupuncture | 22 | 9 | 6 | 5 | 0 | 2 | 20 | RMIT (5), UTS (2) and VU (1) | 14 | 9 | 11 | 5 | 2 (chiropractor) | 2 (pharmacologist) |
| T'ai chi | 2 | 0 | 0 | 2 | 0 | 0 | 2 | 0 | 1 | 1 | 0 | 1 (medical T'ai chi) | ||
| Herbal medicine | 2 | 2 | 0 | 0 | 0 | 0 | 2 | UWS (1) and overseas (1) | 1 | 1 | 0 | 1 (psychologist) | ||
| Chiropractic | 8 | 8 | 0 | 0 | 0 | 0 | 7 | Macquarie (6), Murdoch (1); private (1) | 0 | 0 | 0 | 0 | 0 | 2 (psychologist) |
| Osteopathy | 2 | 2 | 0 | 0 | 0 | 0 | 2 | UWS (1); | 0 | 0 | 0 | 0 | 0 | 0 |
| Multitherapy | 16 | 6 | 1 | 8 | 0 | 1 | 15 | Macquarie (1), Murdoch (1); Private (2) | 11 | 6 | 4 | 2 | 0 | 1 (medical T'ai chi practitioner), 1 (public health) and 1 (pharmacologist) |
| Total | 52 | 28 | 6 | 15 | 0 | 3 | 48 | 26 | 15 | 16 | 6 | 2 | 7 |
See Appendix 2 for references.
CAM, complementary and alternative medicine; RMIT, RMIT University; UTS, University Technology of Sydney; VU, Victoria University; UWS, University of Western Sydney.
Collaborative research was common in Chinese medicine, with 24 out of 26 being co-authored and 16 involved medical doctors, statisticians, physiotherapists, or other CAM professions.
In contrast, all eight SRs and RCTs of chiropractic were conducted by researchers in the field, and only two involved collaboration with other professions. It is interesting to note that the RCTs were not limited to therapies traditionally delivered by chiropractors; electro neuro adaptive regulator, trigger-point therapy, and neuro-emotional technique (NET) were also studied. Four out of six RCTs were sham procedure controlled.
There was no SR or RCT in osteopathy, but two n=1 trials for pain by Australian authors with no collaboration with other professions.
Half of 16 multitherapy studies were first authored by physiotherapists comparing different types of physical therapies. Six (6) were by CAM researchers, including three by chiropractors, two by acupuncturists, and one by osteopath researchers. Eleven (11) out of 16 studies were collaborative research. However, only two of the CAM training universities were involved in any of those studies.
Table 4 shows a surge in SRs and RCTs of CAM in the 2000s. Most of the Chinese medicine or multitherapy studies were published in medical or related journals, whereas studies of chiropractic or osteopathy were often published in their professional journals.
Table 4.
Year of Publication and Types of Journals (Systematic Reviews and Randomized Controlled Trials only)
| |
Year of publication |
Types of journals |
||||||
|---|---|---|---|---|---|---|---|---|
| 1970–1979 | 1980–1989 | 1990–1999 | 2000–2009 | Mainstream med journal | CAM journal | Own professional journal | Other (sports med, musculoskeletal, laser) | |
| Acupuncture | 0 | 2 | 2 | 18 | 9 | 2 | 5 | 6 |
| T'ai chi | 2 | 1 | 1 | |||||
| Herbal medicine | 2 | 1 | 1 | |||||
| Chiropractic | 0 | 0 | 2 | 6 | 0 | 0 | 5 | 3 |
| Osteopathy | 2 | 2 | ||||||
| Multitherapy | 1 | 0 | 1 | 14 | 6 | 0 | 1 | 9 |
| Total | 1 | 2 | 5 | 44 | 17 | 3 | 13 | 19 |
CAM, complementary and alternative medicine.
Overall, all completed RCTs were of relative small sample sizes, varying from 14 to 109 participants per trial, with none of the studies having over 50 participants per intervention group. Two RCT protocols estimated to recruit over 160 participants.
How were SRs or RCTs funded?
Table 5 outlines the types of financial support. A majority of trials did not report the funding sources. Within those reported, a combined internal and external funding was common. External funding sources included governments, commercial or non-commercial industrial, and philanthropic grants. Only three projects were supported by NHMRC grants.
Table 5.
Sources of Funding
| |
|
External funding |
|
|
|
|
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Internal funding | Noncommercial industrial | Commercial or industrial | State government | Federal government | NHMRC | Overseas | Author self-funded | Not mentioned | No funding | Philanthropic | |
| Acupuncture | 5 | 2 | 2 | 1 | 2 | 1 | 2 | 1 | 12 | 0 | 0 |
| T'ai chi | 2 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 0 |
| Herbal medicine | 1 | 1 | |||||||||
| Chiropractic | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 6 | 1 | 0 |
| Osteopath | 2 | ||||||||||
| Multitherapy | 7 | 2 | 0 | 1 | 1 | 2 | 3 | 0 | 4 | 0 | 1 |
| Total | 15 | 4 | 3 | 2 | 5 | 5 | 5 | 1 | 25 | 1 | 1 |
NHMRC, National Health and Medical Research Council.
Registered trials
ANZCTR search resulted in 10 studies (Table 6). The protocols of two trials were published and included in the above-mentioned section. They were excluded from the statistics. Seven (7) out of eight remaining studies were monotherapy, and one was multitherapy examining combined acupuncture and cognitive behavioral therapy for tension headache. Seven (7) trials were registered by institutions offering CAM training. Similar to the published studies, most of the trials were internally or self-funded. No trial was supported by any government funding.
Table 6.
A Summary of Australian and New Zealand Clinical Trial Registration Complementary and Alternative Medicine Trials on Pain
| Category | Registered sponsor | Year | Type of interventions | Phase | Status | Types of pain | Participation | Affiliation | Funding source | Note |
|---|---|---|---|---|---|---|---|---|---|---|
| Acupuncture | Glazov | 2006 | Laser acupuncture | N/R | Recruiting | Chronic LBP | RCT- Placebo n=100 | Monash | Monash/ Aust Medical Acu College | |
| Pirotta | 2005 | Laser acupuncture | N/R | Open to recruitment | Acute and subacute LBP | RCT - Placebo/ sham n=250 | Melbourne | Melbourne | ||
| RMIT | 2005 | Acupuncture | 2 | Completed | Migraine | RMIT | ||||
| Chinese herbal medicine | Compmed | 2004 | Chinese herbal medicine | 2 | Completed | Primary dysmenorrhea | RCT - Placebo/ formular vs. individualized n=120 | UWS | UWS and commercial | |
| Compmed | 2004 | Chinese herbal medicine | 2 or 3 | Completed | Endometriosis | RCT - Placebo n=150 | UWS | UWS | ||
| T'ai chi | Chris Maher | 2008 | T'ai chi | N/R | Recruiting | Long-term LBP | RCT – no treatment/ usual care n=160 | Sydney | Self-funded - unfunded | Protocol published |
| Chiropractic | Walker | 2008 | Spinal manipulation | N/R | Yet to recruit | Nonspecific thoracic pain | RCT - Graston therapy/ Placebo n=100 | Murdoch | Murdoch | Protocol published |
| Pollard | 2008 | Neuro Emotional Technique | N/R | Yet to recruit | Chronic LBP | RCT - Placebo/ Sham n=120 | Macquarie | Self-funded | ||
| Pollard | 2005 | Neuro Emotional Technique | 2 | Completed | LBP | RCT - sham NET n=17 | Macquarie | Self-funded | ||
| Multitherapy | Greenwood | 2008 | Acupuncture and cognitive behavioral therapy | 2 | Yet to recruit | TTH | RCT - pragmatic trial (pilot) n=30 | RMIT | RMIT |
N/R, not rated; LBP, low-back pain; RCT, randomized controlled trial; RMIT, RMIT University; UWS, University of Western Sydney; NET, Neuro-emotional technique; TTH, tension-type headache.
NHMRC and Australian Research Council (ARC)
Available NHMRC data between 2000 and 2008 under “Pain” and “rehabilitation” were summarized. During the period, funding to CAM was below $170,000 until a major increase in 2008 to over $1.5 million. The percentage of funding on CAM of the total annual NHMRC budget improved from 0.003% to 0.27% in 2008. Funding to pain research varied from 1.35% to 2.3% of the total NHMRC annual budget. Within pain research, funding to CAM varied between 0 and 2.07% at best in 2008.
Table 7 lists NHMRC-funded CAM projects on pain starting from 2009. Four (4) out of six projects were on chronic pain, one on acute pain, and the remaining one on experimental pain in rats. In all of them, acupuncture was the study intervention. All projects were collaborative research.
Table 7.
National Health and Medical Research Council–Funded Complementary and Alternative Medicine (CAM) Trials on Pain Starting from 2009
| CAM area | Administering university | Title | Types of pain | Background of CIA | Collaboration with other profession |
|---|---|---|---|---|---|
| Acupuncture | Sydney | Investigation of neural mechanisms of 670 & 830 nm laser acupuncture in pain relief, using rat | Experimental pain | Western medicine | Medical acupuncture |
| Acupuncture | RMIT | Acupuncture on opioid consumption by chronic noncancer pain patients | Chronic pain | Chinese medicine | Western medicine, psychology |
| Acupuncture | RMIT | Acupuncture and psychological treatment for tension headache | Chronic pain | Psychology | Chinese medicine |
| Acupuncture | RMIT | Multiple Emergency Department Acupuncture Trials | Acute pain | Integrative medicine | Western medicine, Chinese medicine |
| Acupuncture | Melbourne | Laser acupuncture in patients with chronic knee pain | Chronic pain | Physiotherapy | Physiotherapy |
| Acupuncture | Queensland | Dry-needling, advice, and graded exercise for chronic whiplash | Chronic pain | Physiotherapy | Physiotherapy |
CIA, chief investigator A; RMIT, RMIT University.
No ARC data were available online. The authors contacted the ARC for further data and did not receive any reply.
Discussion
Summary of findings
This article identified inconsistency between Australians' use of CAM for pain relief, the amount of research conducted, and the level of funding. While a high proportion of patients visit Chinese medicine, chiropractic, or osteopathic practitioners for pain relief, high-quality Australian CAM research in pain was not developed until the last decade. Multidisciplinary, collaborative research among CAM and conventional medical professions or allied health practitioners is not common. Furthermore, government funding to pain research in CAM is very small.
In the recently released National Pain Strategy,9 the high-priority areas are enhancing research and education in all health professions and encouraging interdisciplinary knowledge exchange and multidisciplinary pain management. The findings of this article conform to the proposed priorities.
Possible reasons for a lack of quality CAM pain research in Australia
Internationally, the use of the three CAM in the United States, Germany, and United Kingdom is similar to or more than that in Australia.10 Those countries produced a large amount of high-quality clinical research, and 185 acupuncture and 22 chiropractic trials on pain were identified through a PubMed search. Similarly, many Chinese herbal medicine studies have been published in China, Korea, and Japan. Results of trials conducted in Asian countries or other Western countries could be useful and relevant to the Australian setting, but need to be validated in this country because of the differences in climate, diet, population, and health care system.
The low number of high-quality CAM research studies in pain could be due to a relatively short history of CAM professions in Australia, research culture, and available funding. Degree courses in these CAM courses offered by Australian public universities only started in the 1980s and 1990s, although formal education had been taught in private colleges,11 which had less incentive to invest in scientific research.
Within CAM professions, the concept of evidence-based medicine is yet to be embraced. In a qualitative study, none of 42 Australian acupuncturists interviewed used evidence from quality research to inform their decision-making. Some of them felt that efficacy trials did not inform clinical practice.12 The many case reports, surveys, and reliability studies in chiropractic and osteopathy also indirectly reflect slow adoption of evidence-based medicine by the professions. In addition, not publishing the results of CAM research in mainstream medical journals further reduces the visibility and awareness of CAM studies.
Finally, a lack of funding is evident. In 1980, the Medical Advisory Committee of the NHMRC conducted a review into chiropractic. The report stated a “lack of an adequate body of scientific research” and recommended that “special attention should be given to supporting (chiropractic, osteopathy, homeopathy and naturopathy) research projects in the field of low back pain and other musculoskeletal disorders.” Musculoskeletal conditions incur the highest out-of-pocket expense and are the third most expensive health problem in Australia.13 Between 1974 and 1991, a few NHMRC inquiries were also made into acupuncture in the area of education, training, practice, and efficacy. In 1975, the council recommended that “controlled clinical trials may be conducted to evaluate the use of acupuncture in…alleviation of pain…treatment of narcotic and alcohol withdrawal states.”14 Little federal funding was given to pain and CAM research until 2008, 30 years after the initial inquiry.
In comparison, the funding to CAM therapies in the United States is correlated with the cost of illness. From 2000 to 2003 alone, the funding by the National Institute of Health (NIH) to CAM on arthritis and low-back pain, the second and sixth most expensive conditions in the United States, has increased from $3.6 million US dollars to nearly $10 million.15
Emerging themes and future directions of CAM research in pain
Two (2) emerging themes were identified from this review. First, the boundaries between professions are less clear and new techniques are developed based on theories from other disciplines. Examples of the former are that researchers of some acupuncture and t'ai chi studies are medical doctors and physiotherapists. An example for the latter is NET, a new therapy combining some theory of Chinese medicine and knowledge of neuroanatomy. Such knowledge and practice transmigration will reshape health professions, and its impact on regulation and registration needs to be studied.
Second, multiple modalities are often used by one practitioner, reflecting the reality of pain management, in which multiple therapies and multidisciplinary collaboration are needed and encouraged.16 Pain patients use a number of therapies.17 The current study found very few Australian trials comparing therapies head to head and none examining the effect of the combined effect of CAM and other therapy on pain except for two yet-to-be-completed trials.
Multidisciplinary and multimodality pain research require collaboration. Participation of CAM researchers in multitherapy studies was low at 30%. This could lead to questions about content validity of the study intervention. Development of acupuncture research in NIH is a good example of the importance of collaboration. Before the 1990s, less than 10% of investigators of acupuncture projects were acupuncturists. This number has increased to over 90% in 2006,18 which might lead to high-quality research.
Finally, to maximize the effective translation of clinical evidence of commonly used CAM therapies such as acupuncture, chiropractic, and osteopathy into clinical practice, international multicenter phase III trials with consistent research protocols are needed to ensure the comparability of findings from such studies.
Conclusions
In Australia, the use of CAM therapies for pain relief is high. Research quality in the CAM area needs to be improved considerably, and a substantial increase in government funding is required to assess the safety and efficacy of the CAM therapies. Future research needs to involve CAM researchers and practitioners as well as researchers from other health research backgrounds, and should examine the combined effect of multiple therapies. International multicenter phase III studies will facilitate the translation of research evidence into practice.
Appendix 1. Example of Search Strategy: PubMed
#1 Acupuncture Field: Title/Abstract (9980)
#2 Australia Field: Affiliation (188938)
#3 #1 AND #2 (93)
#4 #3 AND pain Field: Title/Abstract [27]
#6 Acupuncture Field: MeSH Terms (12088)
#7 Pain Field: MeSH Terms (236584)
#8 #2 AND #6 AND #7 [19]
#9 Electroacupuncture Field: Title/Abstract (1588)
#10 electroacupuncture AND #2 Field [5]
#11 Search Chiropractic Field: Title/Abstract ( 2759)
#12 #11 AND #2 AND Pain Field: Title/abstract [33]
#13 Osteopathy Field: Title/Abstract (1163)
#14 #13 AND #2 [13]
#15 #14 and Pain Field: Title / Abstract [6]
#16 Herbal medicine Field: Title/Abstract (4355)
#17 #16 AND #2 (99)
#18 #17 AND Pain Field: Title/Abstract [4]
Appendix 2. Additional References
Acupuncture Randomized Controlled Trials (15)
1. Xu H, Ryan JD, Li K. Clinical investigation into the effectiveness of needleless acupuncture in the management of the symptoms of osteoarthritis of the knee: A preliminary single-blind and sham-controlled study. Austral J Acupunct Chin Med 2007;2:9–15.
2. Grimmer K. A controlled double blind study comparing the effects of strong Burst Mode TENS and High Rate TENS on painful osteoarthritic knees. Austral J Physiother 1992;38:49–56.
3. Li W, Cobbin D, Zaslawski C. A comparison of effects on regional pressure pain threshold produced by deep needling of LI4 and LI11, individually and in combination. Complement Ther Med 2008;16:278–287.
4. Zaslawski CJ, Cobbin D, Lidums E, Petocz P. The impact of site specificity and needle manipulation on changes to pain pressure threshold following manual acupuncture: A controlled study. Complement Ther Med 2003;11:11–21.
5. Zhu XM, Polus B. A controlled trial on acupuncture for chronic neck pain. Am J Chin Med 2002;30:13–28.
6. Zheng Z, Guo RJ, Helme RD, et al. The effect of electroacupuncture on opioid-like medication consumption by chronic pain patients: A pilot randomized controlled clinical trial. Eur J Pain 2008;12:671–676.
7. Huguenin L, Brukner PD, McCrory P, et al. Effect of dry needling of gluteal muscles on straight leg raise: A randomised, placebo controlled, double blind trial. Br J Sports Med 2005;39:84–90.
8. Xue CCL, Dong L, Polus B, et al. Electroacupuncture for tension-type headache on distal acupoints only: A randomized, controlled, crossover trial. Headache 2004;44:333–341.
9. Mendelson G, Selwood TS, Kranz H, et al. Acupuncture treatment of chronic back pain: A double-blind placebo-controlled trial. Am J Med 1983;74:49–55.
10. Chow RT, Heller GZ, Barnsley L. The effect of 300 mW, 830 nm laser on chronic neck pain: A double-blind, randomized, placebo-controlled study. Pain 2006;124:201–210.
11. O'Reilly BA, Dwyer PL, Hawthorne G, et al. Transdermal posterior tibial nerve laser therapy is not effective in women with interstitial cystitis. J Urol 2004;172:1880–1883.
12. Zoghi M, Jaberzadeh S. Effects of high voltage electro-auriculotherapy on experimental pain threshold. Physiotherapy 2002;88:658–666.
13. Harkin C, Parker R. A prospective, randomised control trial of acupuncture for select common conditions within the Emergency Department. J Chin Med 2007;85:45–52.
14. Chow RT, Barnsley L, Heller GZ, Siddall PJ. A pilot study of low-power laser therapy in the management of chronic neck pain. J Musculoskel Pain 2004;12:71–81.
15. Heussler JK, Hinchey G, Margiotta E, et al. A double blind randomised trial of low power laser treatment in rheumatoid arthritis. Ann Rheum Dis 1993;52:703–706.
Acupuncture Systematic Review (6)
1. Wang Y, Zheng Z, Xue CC. Acupuncture for migraine: A systematic review of Chinese literature. Austral J Acupunct Chin Med 2008;3:3–16.
2. Ee CC, Manheimer E, Pirotta MV, White AR. Acupuncture for pelvic and back pain in pregnancy: A systematic review. Am J Obstet Gynecol 2008;198:254–259.
3. Green S, Buchbinder R, Hetrick S. Acupuncture for shoulder pain. Cochrane Database Syst Rev 2005;2:CD005319.
4. Green S, Buchbinder R, Barnsley L, et al. Acupuncture for lateral elbow pain. Cochrane Database Syst Rev 2002;1:CD003527.
5. Chow RT, Barnsley L. Systematic review of the literature of low-level laser therapy (LLLT) in the management of neck pain. Lasers Surg Med 2005;37:46–52.
6. Trinh K, Graham N, Gross A, et al. Acupuncture for neck disorders. Spine 2007;32:236–243.
Acupuncture Sytematic Review Protocol (1)
1. Deare J, Zheng Z, Xue CL, et al. Acupuncture for treating fibromyalgia (protocol). Cochrane Database Syst Rev 2008;2. Art. No.: CD007070. DOI: 10.1002/14651858.CD007070.
Chinese herbal medicine randomized controlled trials (1)
1. Cao Y, Shi Y, Zheng Y, et al. Blood-nourishing and hard-softening capsule costs less in the management of osteoarthritic knee pain: A randomized controlled trial. Evidence-Based Complement Altern Med 2005;2:363–368.
Chinese herbal medicine systematic review (1)
1. Zhu X, Proctor M, Bensoussan A, et al. Chinese herbal medicine for primary dysmenorrhoea. Cochrane Database Syst Rev 2007;4:CD005288.
T'ai Chi RCT (1) protocol
1. Hall AM, Maher CG, Latimer J, et al. A randomized controlled trial of tai chi for long-term low back pain (TAI CHI): Study rationale, design, and methods. BMC Musculoskel Disord 2009;10:55.
T'ai chi systematic review (1)
1. Hall A, Maher C, Latimer J, Ferreira M. The effectiveness of Tai Chi for chronic musculoskeletal pain conditions: A systematic review and meta-analysis. Arthritis Rheum 2009;61:717–724.
Chiropractic randomized controlled trials (5)
1. Vitiello AL, Bonello R, Pollard H. The effectiveness of ENAR for the treatment of chronic neck pain in Australian adults: A preliminary single-blind, randomised controlled trial. Chiropractic Osteopathy 2007;15:91KB.
2. Tuchin PJ. Spinal care education as a preventative strategy for occupational health and safety: A new role for chiropractors. Australasian Chiropract Osteopathy. 1998;7:8–14.
3. O'Reilly A, Pollard H. TMJ pain and chiropractic adjustment: A pilot study. Chiropract J Australia 1996;26:125–129.
4. Tuchin PJ, Pollard H, Bonello R. A randomized controlled trial of chiropractic spinal manipulative therapy for migraine. J Manipul Physiol Ther 2000;23:91–95.
5. Bablis P, Pollard H, Bonello R. Neuro emotional technique for the treatment of trigger point sensitivity in chronic neck pain sufferers: A controlled clinical trial. Chiropract Osteopathy 2008;16:4; DOI: 10.1186/1746-1340-16-4
Chiropractic randomized controlled trial protocol (1)
1. Crothers A, Walker B, French SD. Spinal manipulative therapy versus Graston technique in the treatment of non-specific thoracic spine pain: Design of a randomised controlled trial. Chiropract Osteopathy 2008;16:2; DOI: 10.1186/1746-1340-16-12
Chiropractic systematic review (2)
1. Hoskins W, McHardy A, Pollard H, et al. Chiropractic treatment of lower extremity conditions: A literature review. J Manipul Physiol Ther 2006;29:658–671.
2. McHardy A, Hoskins W, Pollard H, et al. Chiropractic treatment of upper extremity conditions: A systematic review. J Manipul Physiol Ther 2008;31:146–159.
Osteopathy n=1 (2)
1. Eldridge L, Russell J. Effectiveness of cervical spine manipulation and prescribed exercise in reduction of cervicogenic headache pain and frequency: A single case study experimental design. Int J Osteopath Med 2005;8:106–113.
2. McCarthy S, Rickards LD, Lucas N. Using the concept of ideomotor therapy in the treatment of a patient with chronic neck pain: A single system research design. Int J Osteopath Med 2007;10:104–112.
Multitherapy RCT (5)
1. Giles LG, Muller R. Chronic spinal pain: A randomized clinical trial comparing medication, acupuncture, and spinal manipulation. Spine 2003;28:1490–502; discussion 502–503.
2. Giles LG, Muller R. Chronic spinal pain syndromes: A clinical pilot trial comparing acupuncture, a nonsteroidal anti-inflammatory drug, and spinal manipulation. J Manipul Physiol Ther 1999;22:376–381.
3. Fransen M, Nairn L, Winstanley J, et al. Physical activity for osteoarthritis management: A randomized, controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Rheum 2007;57:407–414.
4. Parker GB, Tupling H, Pryor DS. A controlled trial of cervical manipulation for migraine. Austral NZ J Med 1978;8:589–593.
Multitherapy RCT protocol (1)
1. Leaver AM, Refshauge KM, Maher CG, et al. Efficacy of manipulation for non-specific neck pain of recent onset: Design of a randomised controlled trial. BMC Musculoskel Disord 2007;8:18.
Multitherapy SR (11)
1. Smith CA, Collins CT, Cyna AM, Crowther CA. Complementary and alternative therapies for pain management in labour. Cochrane Database Syst Rev 2006;4:CD003521.
2. Smith CA, Collins CT, Cyna AM, Crowther CA. Complementary and alternative therapies for pain management in labour. Cochrane Database Syst Rev 2003;2:CD003521.
3. Crossley K, Bennell K, Green S, McConnell J. A systematic review of physical interventions for patellofemoral pain syndrome. Clin J Sport Med 2001;11:103–110.
4. Bisset L, Paungmali A, Vicenzino B, Beller E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med 2005;39:411–22; discussion 22.
5. Trinh K, Graham N, Gross A, et al. Acupuncture for neck disorders. Spine 2007;32:236–243.
6. Bjordal JM, Johnson MI, Lopes-Martins RA, et al. Short-term efficacy of physical interventions in osteoarthritic knee pain: A systematic review and meta-analysis of randomised placebo-controlled trials. BMC Musculoskel Disord 2007;8:51.
7. Rickards LD. The effectiveness of non-invasive treatments for active myofascial trigger point pain: A systematic review of the literature. Int J Osteopath Med 2006;9:120–136.
8. Gross AR, Hoving JL, Haines TA, et al. A Cochrane review of manipulation and mobilization for mechanical neck disorders. Spine 2004;29:1541–1548.
9. Machado LAC, Kamper SJ, Herbert RD, et al. Analgesic effects of treatments for non-specific low back pain: A meta-analysis of placebo-controlled randomized trials. Rheumatology 2009;48:520–527.
10. Pengel HM, Maher CG, Refshauge KM. Systematic review of conservative interventions for subacute low back pain. Clin Rehabil 2002;16:811–820.
11. Gross AR, Goldsmith C, Hoving JL, et al. Conservative management of mechanical neck disorders: A systematic review. J Rheumatol 2007;34:1083–1102.
Acknowledgments
The preparation of this article is partially supported by a National Health and Medical Research Council project grant (No. 555411).
Disclosure Statement
No competing financial interests exist.
References
- 1.Blyth FM. Chronic pain in Australia: A prevalence study. Pain. 2001;89:127–134. doi: 10.1016/s0304-3959(00)00355-9. [DOI] [PubMed] [Google Scholar]
- 2.Xue CCL. Zhang TL. Lin V, et al. Acupuncture, chiropractic and osteopathy use in Australia: A national population survey. BMC Public Health. 2008;8:105. doi: 10.1186/1471-2458-8-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meier P. Rogers C. Reporting traditional Chinese medicine morbidity: A University of Technology, Sydney, project with an emphasis on developing standards for testing and reporting data. J Altern Complement Med. 2006;12:529–534. doi: 10.1089/acm.2006.12.529. [DOI] [PubMed] [Google Scholar]
- 4.Xing M. Long AF. A retrospective survey of patients at the University of Salford Acupuncture Clinic. Complement Ther Clin Pract. 2006;12:64–71. doi: 10.1016/j.ctcp.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 5.Mootz RD. Cherkin DC. Odegard CE, et al. Characteristics of chiropractic practitioners, patients, and encounters in Massachusetts and Arizona. J Manipul Physiol Ther. 2005;28:645–654. doi: 10.1016/j.jmpt.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 6.Orrock. Australian Osteopathic Association; Chastwood West, NSW: 2004. 2005. Osteopathic Census. [Google Scholar]
- 7.NCCAM. What is complementary and alternative medicine? Apr, 2010. [May 20;2010 ]. http://nccam.nih.gov/health/whatiscam/ p. D347.http://nccam.nih.gov/health/whatiscam/
- 8.NHMRC. Canberra: National Health and Medical Research Council; 2000. How to use the evidence: Assessment and application of scientific evidence. [Google Scholar]
- 9.National Pain Summit Initiative. Draft National Pain Strategy. 2010. [Aug 30;2010 ]. www.painsummit.org.au/strategy/Strategy-NPS.pdf/view p. 95.www.painsummit.org.au/strategy/Strategy-NPS.pdf/view
- 10.Ernst E. Prevalence of use of complementary/alternative medicine: A systematic review. Bull World Health Organization. 2000;78:252–257. [PMC free article] [PubMed] [Google Scholar]
- 11.Bolton SP. Chiropractic education in Australia: A short history of its emergence and development. Chiropr J Aust. 2010;40:88–90. [Google Scholar]
- 12.Ryan D. The Use of Evidence in Acupuncture Clinical Practice. Aust J Acup Chin Med. 2006;1:21–25. [Google Scholar]
- 13.ABS. 4823.0.55.001—Musculoskeletal Conditions in Australia: A Snapshot, 2004–05. Australian Bureau of Statistics. 2006. [May 20;2010 ]. www.abs.gov.au/ausstats/abs@nsf/mf/4823.0.55.001 www.abs.gov.au/ausstats/abs@nsf/mf/4823.0.55.001
- 14.NHMRC. Acupuncture. Canberra: National Health and Medical Research Council; 1974. [Google Scholar]
- 15.Nahin RL. Identifying and pursuing research priorities at the National Center for Complementary and Alternative Medicine. FASEB J. 2005;19:1209–1215. doi: 10.1096/fj.05-3727LFE. [DOI] [PubMed] [Google Scholar]
- 16.APS. Pain Management Programmes for Chronic, Persistent, or Long Lasting Pain. Australian Pain Society. 2002. [Aug 30;2011 ]. www.apsoc.org.au/pdfs/APSpainProgs.pdf www.apsoc.org.au/pdfs/APSpainProgs.pdf
- 17.Blyth FM. March LM. Cousins MJ. Chronic pain-related disability and use of analgesia and health services in a Sydney community. Med J Aust. 2003;179:84–87. doi: 10.5694/j.1326-5377.2003.tb05441.x. [DOI] [PubMed] [Google Scholar]
- 18.Nahin RL. The Status and Future of Acupuncture Research: 10 Years Post-NIH Consensus Conference. 2007 Annual Conference of Society for Acupuncture Research; Baltimore, MD. Nov 8–11;2007 ; [DOI] [PMC free article] [PubMed] [Google Scholar]