Abstract
Frequency-specific microcurrent (FSM) is an emerging technique for treating many health conditions. Pairs of frequencies of microampere-level electrical stimulation are applied to particular places on the skin of a patient via combinations of conductive graphite gloves, moistened towels, or gel electrode patches. A consistent finding is a profound and palpable tissue softening and warming within seconds of applying frequencies appropriate for treating particular conditions. Similar phenomena are often observed with successful acupuncture, cranial-sacral, and other energy-based techniques. This article explores possible mechanisms involved in tissue softening. In the 1970s, neuroscientist and osteopathic researcher Irvin Korr developed a “γ-loop hypothesis” to explain the persistence of increased systemic muscle tone associated with various somatic dysfunctions. This article summarizes how physiologists, neuroscientists, osteopaths, chiropractors, and fascial researchers have expanded on Korr's ideas by exploring various mechanisms by which injury or disease increase local muscle tension or systemic muscle tone. Following on Korr's hypothesis, it is suggested that most patients actually present with elevated muscle tone or tense areas due to prior traumas or other disorders, and that tissue softening indicates that FSM or other methods are affecting the cause of their pathophysiology. The authors believe this concept and the research it has led to will be of interest to a wide range of energetic, bodywork, and movement therapists.
Introduction
Electricity has long been used to stimulate healing; the recorded history dates from 2750 bc when sick people were exposed to electric eels.1 In 1812, Dr. John Birch in London healed a nonunion of the tibia with electric currents passed through needles surgically implanted in the fracture region.2 By the mid 1800s, this had become the preferred method for treating slow-healing bone fractures. However, the Flexner Report and the Pure Food and Drug Act of 1906 led to the abolition of electricity for healing3 until the 1980s, when careful research confirmed the effectiveness of electrical currents for stimulating bone healing. It was then discovered that coils could be used to noninvasively induce current flows through fracture sites.4 This is known as pulsing electromagnetic field (PEMF) therapy. Following on this success, other investigators have successfully applied PEMF to a variety of other tissues, with each tissue responding to a particular frequency.5 For example, recent studies have documented frequency effects on tendon repair6 and collagen deposition in bone.7
To ensure patient compliance, many orthopedic surgeons have returned to electricity, supplied by small implantable stimulators for treating nonunions.8 Another approach to electrical stimulation is to use electrode patches on the skin to pass currents into the body (e.g., the transcutaneous electrical nerve stimulation device for treating pain).9
Electrotherapy and bioelectromagnetic therapies are different forms of energy medicine, which recognizes that the human body utilizes various forms of energy for the internal communications that maintain and organize vital living systems and for powering processes such as nerve conduction, digestion, circulation, and movement. Energy medicine also involves the use of energies of particular intensities and frequencies and other characteristics that stimulate the repair of one or more tissues, or that enable built-in healing mechanisms to operate more effectively. Such energies can come from the environment, from another human being, or from a medical device.
Physics and biophysics study how the various kinds of physical energy interact with each other and with living systems. For example, moving electrical charges create magnetic fields in the surrounding space (Ampère's Law, 1820),10 and moving magnetic fields induce currents to flow through conductors (Faraday's Law, 1831).11 Electromagnetic fields arise when charges accelerate.12 Hence, when oscillating or pulsing microcurrents are applied to the human body for therapeutic purposes, there is the possibility that beneficial effects may be due to the microcurrents themselves, to the magnetic fields induced in conductive tissues by charge movements, or to electromagnetic fields.
Energy medicine and bioelectromagnetics recognize the importance of resonance—the tendency of objects such as atomic nuclei, electrons, or molecules to vibrate strongly at certain frequencies and for these vibrations to be coupled through space to other objects with similar resonant frequencies. Magnetic resonance imaging, for example, is based on resonant interactions between magnetic and electromagnetic fields and protons in tissues. The high degree of frequency specificity of frequency-specific microcurrent (FSM) indicates that resonance is probably involved in the mechanism of action, in which the applied current is resonating with charged particles or dipoles in the tissues.
Frequency-Specific Microcurrent
FSM has emerged over the last decade as a reproducible treatment for various somatic and visceral conditions including fibromyalgia, chronic fatigue, and myofascial and neuropathic pain. Recent publications13,14,15 summarize the origins, possible mechanisms, applications, and practical details of FSM. The technique is based on pairs of frequencies, low-level micro-amperage currents, and the principles of biologic resonance. The publications describe protocols for treating various health complaints; multicenter clinical case reports documenting successful applications; and review condition pathophysiology, differential diagnosis, and current research. A study of delayed-onset muscle soreness summarizes the history of FSM, including the history of the discovery of effective frequencies and frequency combinations.16
FSM practitioners consistently observe a profound and easily palpable change in tissue texture within seconds of applying frequencies appropriate for a particular disorder. This “state change” can usually be detected anywhere on the body when one has found the correct frequencies and placements of the conductors (conductive graphite gloves, gloves wrapped in moist cloth, or gel electrode patches) (Fig. 1), provided the patient is hydrated. The softening is not superficial, as in the epidermal layer, but is in the deeper skeletal muscles.
FIG. 1.
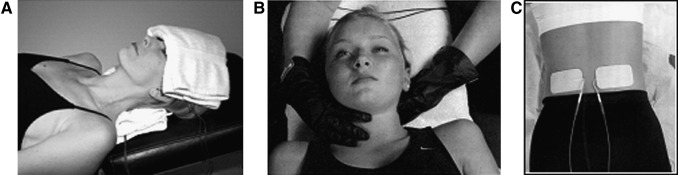
Examples of frequency-specific microcurrent methods for delivering microcurrents to the body. (A) Conductive gloves are placed in warm wet hand towels or face cloths placed on the neck and forehead for treatment of sinus conditions. Eight (8) possible frequency combinations previously identified for treating sinus conditions are tested in sequence until the therapist detects a profound softening of an arm muscle. (B) Treatment of the upper back, shoulder, and posterior part of the neck using conductive graphite gloves to restore biomechanics and relieve pain. The fingers sense change rather than force it. The frequencies and currents do the work. A latex or nitrile glove is worn under the graphite glove to prevent current conduction to the practitioner. (C) Gel electrode pads used to treat lumbar ligaments without nerve involvement. Another pair of electrode pads is placed on corresponding points on the abdomen (not shown). Electrode polarities are arranged to produce an interferential field so that the current and the frequencies pass diagonally through the area to be treated, as an “X” in three dimensions. For details and other treatment techniques, see reference 13.
Tissue softening provides rapid feedback when one is optimizing a protocol for a condition not previously treated with FSM. Since so many variables are involved—two separate frequencies, signal intensities and waveforms, positioning of the conductive materials, and the patient's condition—tissue softening facilitates the determination of the best combinations.
The purpose of this report is to explore the possible causes of changes in muscle tension and muscle tone* during the therapeutic encounter. The report is not about muscle testing and applied kinesiology, although the information presented may be relevant to those controversial subjects.**
Specific changes include the following:
The tissue rapidly and profoundly softens within seconds.
Usually tissue all over the body softens when a beneficial frequency combination is applied anywhere on the body for any condition—likely a change in systemwide muscle tone.
Sometimes there are unresponsive regions that stand out amid the softened tissue—apparently due to localized muscle tension. These areas can be addressed with additional frequency choices and locations of the conductors.
Muscle tissue that is hard, tough, scarred, firm, rigid, “gnarly,” or stiff begins to soften and within minutes feels “smooshy,” like pudding in a plastic sack.
The tissue becomes warm. This can be felt through the conductive gloves. Some sensitive practitioners can feel the warming with their hand several inches away from the skin.
The patient may become somewhat dreamy or “spaced out.”
For example, place a hand on an arm muscle while testing the eight possible frequency combinations previously identified for treating sinus conditions, with the microcurrent applied via conductive gloves inserted in warm moistened towels placed on the neck and forehead (Fig. 1A). One or more of the frequency combinations will result in profound softening of the arm muscle as the sinus condition begins to resolve. Figures 1B and 1C show the use of the conductive gloves and gel electrode patches, respectively.
Side-Effect or Causal Relationship
There are two contrasting perspectives on tissue softening with FSM. One is that it is a “side-effect” of the application of therapeutic frequencies, and has no physiologic significance. Another is that injuries, physical or emotional traumas, or other pathologic conditions can increase bodywide muscle tone or local muscle tension, and that tissue softening indicates that the pathophysiology is being addressed. On the basis of the work of Irvin Korr and others to be described below, it is suggested that patients often have some degree of elevated muscle tone or tension stemming from the trauma, disease, injury, or other condition that brought them to the physician's office, and that tissue softening indicates that treatment is progressing.
Many patients experiencing a traumatic event go on with their lives without lasting negative effects; others have reactions that lead to chronic physical and/or emotional issues. For example, psychologic factors have been associated with primary fibromyalgia syndrome,17 and Mines suggests that most people are “in shock” from old traumatic experiences.18 Musculoskeletal pain, for example, can have multiple causes, and some patients benefit from therapies that “unwind” old traumas.19
Physiologists, neuroscientists, osteopaths, chiropractors, and fascial researchers have explored various mechanisms by which injury or disease increases local or systemic muscle tension or tone. They have described a variety of connections between pain, injury, disease, and impaired movement, on the one hand, and palpable muscle tone or tension on the other. Their goal has been to find ways of resolving the causes of pathophysiologies of all kinds. Often distinctions have been made between visceral (organ) pathologies and somatic (body wall or musculoskeletal system, in contrast to the viscera) pathologies. As with reductionist “mind–body” distinctions, the holistic perspective teaches that we must be cautious about such separations, as they may have little relevance to how the human body actually responds in health and disease. For example, the distinction between electrical conduction “outside” and “inside” is blurred because the skin surface is anatomically continuous via the nose, nasal cavities, and bronchial tree, extending into the thin alveolar membranes separating the air space and the blood. A similar anatomically continuous outside–inside pathway connects to the body interior via the mouth and mucous membranes of the digestive tract.
A Web of Interactions
Extensive literature describes how pathophysiology and emotional issues can be expressed as pain and increased muscle tone and tension.20,21,22,23 The report by Kokebie et al.23 is particularly relevant to FSM because the report shows that muscle tension is measurably increased in fibromyalgia. FSM is an effective treatment for fibromyalgia.14
The terms “visceral and somatic disorder, dysfunction, lesion, reflex pathway, trigger point, and pathophysiology” are widely used. Lesions are described as subluxations (chiropractic), energy blocks (acupuncture), osteopathic lesions (osteopathy), and myofascial constrictions (in other forms of structural bodywork). There is a widely held belief that somatic issues are associated with visceral illness and vice versa, sometimes related to the vertebral level associated with a particular organ. These effects have been termed somatovisceral and visceralsomatic reflexes. These concepts were developed in an effort to explain the frequent observation that the symptoms of organic disease seem to be relieved through manipulative or bodywork techniques. For example, a patient with deep radiating pain involving their upper back, chest, and arm (symptoms most often associated with cardiac angina) may experience significant relief immediately following an upper thoracic or lower cervical spinal adjustment. The frequency of such observations led to a number of theories that attempt to explain how patients appearing to be suffering from any of a variety of internal organ diseases often respond quickly and dramatically to therapies delivered to purely somatic structures (e.g., spinal manipulation, massage, Structural Integration, or other bodywork techniques). A possible interpretation of this kind of clinical observation is that disorders involving various somatic paraspinal structures are capable of inducing secondary disorders or diseases involving segmentally related visceral organs. For a detailed introduction, see Morris24 and Simons and Travell,25 who devoted a chapter to the abdominal muscles and their associated somatovisceral and visceralsomatic reflexes. For example, they associated trigger points in the oblique abdominals with diarrhea, belching, dysmenorrhea, or nausea. Simons and Travell also reported that a specific trigger point in the pectoralis major is associated with a type of ectopic cardiac arrhythmia and that elimination of this trigger point immediately restored normal cardiac rhythms.25
While these ideas are widely taught, there is much doubt and controversy. In a thoughtful review, Nansel and Szlazk explore the concept that somatic therapies can treat the causes of visceral (organ) disorders by removing blockages at particular segments of the spinal cord. After review of some 350 articles published over a period of about 75 years, Nansel and Szlazk concluded that misalignment in the vertebral column can cause symptoms that can be mistaken for, or mimic, visceral diseases, but that there is no substantial scientific evidence that segmental misalignment can actually cause true visceral disease. Nansel and Szlazak continued to be open to a segmental theory of visceral disease, but were simply unable to find objective evidence for it. They emphasized that “afferent convergence” can create somatic signs and symptoms that are virtually indistinguishable from those produced by organ malfunctions.26 This brought into question the widely taught concepts of somatovisceral and visceralsomatic pathways. The resulting arguments were summarized by Seaman.27
Convergence of visceral and somatic afferents continues to be a topic of neurophysiologic research. For example, noxious stimuli in the esophagus can cause pain that is referred to the anterior chest wall because of convergence of visceral and somatic afferents within the spinal cord.28
These discussions are relevant to this report both because FSM provides clinically verifiable relief from both somatic and visceral issues, and because there is still widespread acceptance that visceral dysfunctions can elevate somatic muscle tension. For example, flank muscle hypertonicity can arise secondary to renal dysfunction, and trigger points can be activated in acute appendicitis, peptic ulcer, ulcerative colitis, and diverticulitis.29 FSM, acupuncture, and other energy medicine techniques document interactions between the epidermis and internal organs. Whether these interactions are best referred to as somatovisceral reflexes is an open question. Certainly relationships between somatic and visceral systems can be described in terms of chemistry (metabolic imbalances in the periphery might impact organ functions and vice versa); in terms of neurology, such as the convergence of visceral and somatic afferent nerves; in terms of structural or fascial relationships between peripheral structures and organs; in terms related to the endocrine system and lymphatic drainage (Chapman's Points)30,31; and in terms of energetic pathways between the skin and internal organs, as theorized, for example, in acupuncture. The questions arising from these ideas are profound and are of major medical significance.
Several inter-related hypotheses have therefore been explored in order to provide a perspective on tissue softening with FSM. The concepts are presented in historical sequence, without favoring any one of them. The goal is to provide a background for further theoretical, clinical and applied research, recognizing that aspects of several of these mechanisms may be involved simultaneously.
The Vicious Cycle Relating Muscle Spasm and Pain (1940s)
A “vicious cycle” hypothesis of pain and increased muscle tension was proposed in 1942:
Limitation of motion is primarily a reaction to pain rather than the result of structural lesion. If muscle spasm causes pain, and pain reflexively produces muscle spasm, a self-perpetuating cycle might be established.32
While this concept is still widely held, controlled studies have shown no significant difference in resting electromyographic activity when painful and nonpainful muscles are compared.33,34,35 A painful inflamed muscle can actually have lower-than-normal tension.36
The Vascular Autonomic Signal (1950s)
The vascular autonomic signal (VAS) is an instantaneous change in the tone of the walls of all arteries, mediated by the autonomic nervous system.37 Changes are palpable at the radial or carotid arteries. The VAS is thought to be a sensitive indicator of autonomic changes from a variety of external or internal factors, and was first used to study the effects of auricular (ear) acupuncture. It is unlikely that the momentary shift in arterial pressure observed in the VAS explains tissue softening with FSM, which has a slower onset and persists for the duration of a treatment.
The γ-Loop Hypothesis (1970s)
In 1975 and 1978 Irvin Korr introduced a “γ-loop hypothesis” to explain the persistence of increased local or systemic muscle contractions associated with various somatic and/or visceral dysfunctions.38,39 The hypothesis states that such dysfunctions lead to increased resting muscle contractions mediated by the autonomic nervous system and by the γ efferent loops regulating local muscle tension or global muscle tone.* Appropriate FSM treatments targeting specific conditions may therefore restore normal autonomic function and/or shift the “γ gain” regulating muscle tone or tension. Autonomic effects could also account for circulatory changes (tissue warming) and effects on consciousness (the dreamy or “spaced out” condition often observed in FSM). Perhaps resetting the γ gain and lowering resting tonus of the musculature causes a transient drop in blood pressure (indicated by the VAS) from reduced muscular compression on the vasculature. The carotid sinus and aortic baroreceptor feedback loops40 would quickly restore blood volume and pressure, explaining why the VAS is a transient change arterial pressure.
Korr pointed out that there is a large though scattered body of clinical and experimental literature describing chronic hyperactivity of sympathetic pathways in many clinical conditions, involving a variety of organs and tissues. He suggested that this widely shared feature of local, regional, or segmental sympathetic hyperactivity is overlooked because of barriers created by specialization: The ophthalmologist is not ordinarily exposed to the gastroenterologic literature, the gastroenterologist to the cardiologic, and so on. Each discoverer of a sympathetic component seems to regard it as peculiar to this or that disease, rather than as part of a general theme. Korr referred to this hypothesis and its consequences as sustained sympatheticotonia.39
Sympathetic activation can have both local and systemic effects on cardiac output, distribution of blood flow, heat dissipation through the skin, release of stored metabolites, local muscle tension or systemic skeletal muscle tone, range of motion, and emotional affect.41 In other words, any injury or inflammation or any somatic or visceral dysfunction anywhere in the body can elevate muscle tone throughout the musculoskeletal system, or increase skeletal muscle tension in selected areas, depending on the myotome, dermatome, or sclerotome involved.*
Korr's hypothesis of sustained sympatheticotonia may apply to FSM, since a consistent observation is that application of the correct treatment frequencies leads to a palpable local or bodywide tissue softening and warming, which is often associated with vasodilation. Frequency effects on the autonomic nervous system have been noted before (e.g., McKay et al., 2006).42 FSM may actually reset γ gain and sympathetic tone, with beneficial local and/or systemic consequences on resting muscle tone and visceral functioning.** How specific frequencies may cause such changes remains an open question.
The Johansson/Sojka Hypothesis (1990s)
In 1991, Swedish physiologists H. Johansson and P. Sojka developed a model to help explain why chronic musculoskeletal pain syndromes such as those encountered with industrial injuries have a tendency to perpetuate themselves and spread from one muscle to another.43 The hypothesis is that metabolites produced by static or chronic muscle contractions stimulate muscle afferents, activating the γ-motor neurons, increasing muscle stiffness, leading to further production of metabolites, thereby creating a “built-in” positive feedback loop or “vicious cycle” that perpetuates and spreads the hypertonicity from muscle to muscle. While the model is popular, it is not clinically proven to operate in humans.33 More recently, studies on humans demonstrated that acute activation of muscle or skin nociceptors*** does not cause a reflexive increase in γ gain.44
The Facilitated Segment Theory (2003)
Chiropractic researchers extended Korr's work and developed a facilitated segment theory: chronic, repetitive, and abnormal segmental input creates referred segmental pain and tenderness, hypertonicity of key muscles, and even secondary soft-tissue changes within the girdles and limbs. A facilitated segment can maintain a disturbed state from impulses of endogenous origin entering the corresponding dorsal root ganglion. All somatic and visceral structures receiving efferent nerve fibers from that segment are potentially exposed to excessive excitation or inhibition.45 Impulses of endogenous origin include autonomic and γ efferent fibers to muscle.
Following up on Korr's concepts and the Johansson and Sojka hypothesis, in 2003 chiropractic researchers Knutson and Owens reviewed the complexities of skeletal muscle in regard to anatomy, active and passive tone, detection of muscle tone, neurophysiology, and how muscle function fits into a variety of subluxation/joint dysfunction models.46,47 (The Association of Chiropractic Colleges defines subluxation as a complex of functional and/or structural and/or pathologic articular changes that compromise neural integrity and that may influence organ system function and general health.)45 Part II of the Knutson and Owens report discusses the extensive literature on how the various degrees of elevated muscle tone and their causes can help clinicians find underlying sources of neuromusculoskeletal problems and select appropriate interventions.47 All of these concepts are controversial.48
Tension and Softening of Connective Tissue/Fascia (Beginning in 2004)
Fascia is the bodywide structural and tensional component of the musculoskeletal system and has extensions to all of the viscera. In the past there has been uncertainty as to which kinds of connective tissue should be included under the term “fascia”—superficial fascia, endomysium, perineurium, visceral membranes, aponeuroses, retinaculae, tendons, ligaments, or joint/organ capsules. At the 1st International Fascia Research Congress, held at Harvard Medical School in 2007, it was proposed that all collagenous connective tissues whose morphology is shaped primarily by tensional loading and that is part of the interconnected tensional network that extends throughout the body could be considered “fascial tissues.”49
Fascia has usually been viewed as a passive material that simply transmits forces exerted by muscles and gravity. However, a series of reports by Robert Schleip and colleagues, beginning in 2004, confirmed earlier suggestions that fascia may have both sensory and contractile properties. They showed that lumbar fascia, plantar fascia, and the fascia lata contain myofibroblast cells that stain for α-smooth-muscle actin.50 Further in vitro research showed that smooth muscle-like contractions can be both induced and inhibited pharmacologically.51 Schleip and colleagues recognized that contractility of intramuscular connective tissue could be a significant component of passive muscle stiffness, which is also referred to as passive elasticity, passive muscular compliance, passive extensibility, resting tension, or passive muscle tone.52
These important findings have implications for visceral and somatic disorders or dysfunctions, and could also be a component of the elevated tissue stiffness discussed here. The observed time-course of fascial lengthening is probably too slow to account for the tissue softening taking place during FSM, but could be a component of the longer-term healing responses triggered by FSM.
Discussion
The main hypothesis of this report is that tissue softening noted when a therapeutic frequency is applied to the body is accounted for by the fact that most patients actually present with elevated muscle tone or tense areas related to previous traumatic or disease experiences, as originally proposed by Irvin Korr. Several possible mechanisms have been discussed by which trauma and disease lead to elevated muscle tone or tense areas. The most recent research has shown that fascia has both sensory and contractile properties that can influence passive muscle stiffness, elasticity, compliance, extensibility, resting tension, and muscle tone. This new work was unknown to the earlier investigators cited here.
The fascial network is pervasive, extending to the capsules and interiors of organs, and could therefore be involved in both the origin and resolution of both somatic and visceral disorders. A recent report by Finando and Finando suggests that fascia is the medium involved in the effects of acupuncture, including effects on organ pathology.53 When the body is injured, stressed, or traumatized, fascia responds by laying down new fibers to provide support for the injured area (Wolff's Law for bone,54 and Davis's Law for soft tissues) and by “gluing” adjacent muscles to each other. Thickening and gluing of fascial layers can persist long after an injury has healed and leave behind dense pockets or nonresilient bands that can be felt deep in the tissues.55 These palpable densities may correspond to the trigger points and taut bands described by Simons and Travell56 and/or to the inflammatory pockets described by Selye.57 Residual local tensions and gluing in the fascial network can give rise to compensating tensions extending throughout the musculoskeletal system. Such compensations can disturb more distant structures, leading to compromised movement patterns that leave the body vulnerable to further injury.
Conclusions
Because of its anatomical pervasiveness, the fascia is involved in every aspect of physiology. Hence, the fascia constitutes a medium by which superficial injuries or contractions or constrictions might influence internal organs, and by which organ pathologies might be expressed in the periphery. Recent research has indicated that fibrosis created by a superficial injury can extend into the viscera to create so-called fibrocontractive diseases.58,59,60,61 These concepts provide a possible fascial basis for the so-called somatovisceral and visceralsomatic reflexes. The review of Nansel and Szlazak26 cast doubt on the existence of such reflex pathways as they were described in the earlier literature. However, such reflexes could have an anatomical and energetic basis in the form of specific pathways through the fascial network. The tissue softening taking place with FSM renews interest in the possible relations between somatic and visceral pathologies.
Footnotes
The terms “muscle tone” or “residual muscle tension” or “muscle tonus” refer to the continuous and passive partial contraction of the resting skeletal muscles, or the muscle's resistance to passive stretch while in the resting state, as opposed to active contraction. Physical disorders, injuries, and stress can result in abnormally low (hypotonia) or high (hypertonia) muscle tone throughout the body. In contrast, muscle tension refers to a condition in which particular muscles remain chronically semicontracted. Muscle tension is typically a response to stress, overuse, or injury to a particular part of the body. Stress can also lead to sympathetically mediated constriction of blood vessels, reducing the flow of oxygen and nutrients to muscles, tendons, and nerves, often referred to as ischemia. This can lead to the local or systemic buildup of metabolic waste products, resulting in muscle tension, spasm, and pain. FSM is effective at normalizing both bodywide muscle tone and localized muscle tension, and at ameliorating their consequences.
Muscle testing or applied kinesiology uses muscle relaxation as an indicator of a biologic response. The method has been used at various stages in the development of methods that involve “listening” to obtain feedback on the functional status of the body and appropriateness of various interventions. Examples of therapists who use muscle testing include chiropractors, naturopaths, medical doctors, dentists, nutritionists, physical therapists, massage therapists, nurse practitioners, practitioners of BodyTalk, Holographic or Resonance Repatterning, and many others.
The γ loops consist of efferent neurons (neurons from the central nervous system to the periphery, such as motor neurons) and afferent neurons (neurons from the periphery to the central nervous system, such as sensory nerves). Gamma (γ) motor neurons are the efferent component of the fusimotor system that controls and modifies the sensitivity of muscle spindles. The muscle spindles provide proprioceptive feedback for the movement, position and extension of muscles. Gamma (γ) motor neurons are located in the brainstem and spinal cord and are smaller than their α-motoneuron counterparts, which stimulate contractions of the skeletal muscles.
The terms, myotomes, dermatomes and sclerotomes refer to tissues that develop from particular masses of embryonic mesoderm. Dermatomes develop into dermis, myotomes develop into skeletal muscle, and sclerotomes develop into vertebrae and most of the skull bones. The terms “myotome” and “dermatome” also respectively describe the muscles and skin areas served by a single nerve root.
There is histological evidence that muscle spindles are innervated by sympathetic nerves, but little is known about their function.
Nociceptors or pain receptors are lightly myelinated or unmyelinated afferent sensory neurons that are found in any area of the body that can sense pain caused by mechanical, thermal, or chemical stimuli that are strong enough to damage tissues.
Disclosure
The second author (JLO) has received lecture honoraria and consulting fees from Frequency Specific Seminars Inc. in Vancouver, Washington for the research and writing of this article.
References
- 1.Kellaway P. The part played by electric fish in the early history of bioelectricity and electrotherapy. Bull History Med. 1946;20:112–132. [PubMed] [Google Scholar]
- 2.Becker RO. Seldon G. The Body Electric: Electromagnetism and the Foundation of Life. New York: William and Morrow Company, Inc.; 1985. p. 172. [Google Scholar]
- 3.Oschman JL. Energy Medicine: The Scientific Basis. Vol. 15. Churchill Livingstone/Harcourt Brace; Edinburgh, Scotland: 2000. [Google Scholar]
- 4.Bassett CAL. Bioelectromagnetics in the service of medicine. In: Blank M, editor. Electromagnetic Fields: Biological Interactions and Mechanisms. Washington, DC: American Chemical Society; 1995. pp. 265–275. Advances in Chemistry Series 250. [Google Scholar]
- 5.Siskin BF. Walker J. Therapeutic aspects of electromagnetic for soft-tissue healing. In: Blank M, editor. Electromagnetic Fields: Biological Interactions and Mechanisms. Washington, DC: American Chemical Society; 1995. pp. 277–285. Advances in Chemistry Series 250. [Google Scholar]
- 6.Strauch B. Patel MK. Rosen DJ, et al. Pulsed magnetic field therapy increases tensile strength in a rat Achilles' tendon repair model. J Hand Surg Am. 2006;31:1131–1135. doi: 10.1016/j.jhsa.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 7.Soda A. Ikehara T. Kinouchi Y. Yoshizaki K. Effect of exposure to an extremely low frequency-electromagnetic field on the cellular collagen with respect to signaling pathways in osteoblast-like cells. J Med Invest. 2008;55:267–278. doi: 10.2152/jmi.55.267. [DOI] [PubMed] [Google Scholar]
- 8.Cundy PJ. Paterson DC. A ten-year review of treatment of delayed union and nonunion with an implanted bone growth stimulator. Clin Orthop Relat Res. 1990;259:216–222. [PubMed] [Google Scholar]
- 9.Melzack R. Prolonged relief of pain by brief, intense transcutaneous somatic stimulation. Pain. 1975;1:357–373. doi: 10.1016/0304-3959(75)90073-1. [DOI] [PubMed] [Google Scholar]
- 10.Ampère A-M. Annales de Chimie et de Physique XV; Paris, France: V. Masson: 1820. Mémoire présenté à l'Académie royale des sciences. Submission presented to the Royal Academy of Sciences [in French] [Google Scholar]
- 11.Faraday M. First report on magneto-electric induction, read before the Royal Society on the 24th of November. London, UK: 1831. [Google Scholar]
- 12.Boulware DG. Radiation from a uniformly accelerated charge. Ann Phys. 1980;124:169–188. [Google Scholar]
- 13.McMakin C. Frequency Specific Microcurrent in Pain Management. Edinburgh: Churchill Livingstone/Elsevier; 2011. [Google Scholar]
- 14.McMakin C. Qi in chronic fatigue and fibromyalgia. In: Mayor D, editor; Micozzi M, editor. Energy Medicine East and West. Edinburgh: Churchill Livingstone/Elsevier; 2011. pp. 289–296. [Google Scholar]
- 15.McMakin C. Microcurrent therapy in the treatment of fibromyalgia. In: Chaitow L, editor. Fibromyalgia Syndrome: A Practitioner's Guide to Treatment. Edinburgh: Churchill Livingstone; 2003. pp. 179–206. [Google Scholar]
- 16.Curtis D. Fallows S. Morris M. McMakin C. The efficacy of frequency specific microcurrent therapy on delayed onset muscle soreness. J Bodywork Move Ther. 2010;14:272–279. doi: 10.1016/j.jbmt.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 17.Antes TA. Yunus MB. Ritey SD, et al. Psychological factors associated with primary fibromyalgia syndrome. Arthritis Rheum. 1984;2:1101–1106. doi: 10.1002/art.1780271004. [DOI] [PubMed] [Google Scholar]
- 18.Mines S. We Are All in Shock. How Overwhelming Experiences Shatter You…and What You Can Do About It. Franklin Lakes, NJ: New Page Books; 2003. [Google Scholar]
- 19.Barnes JF. Healing Ancient Wounds: The Renegade's Wisdom. Sedona, AZ: MFR Treatment Centers and Seminars; Jun 1, 2000. [Google Scholar]
- 20.Willis WD. The somatosensory system, with emphasis on structures important for pain. Brain Res Rev. 2007;55:297–313. doi: 10.1016/j.brainresrev.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 21.Gamsa A. The role of psychological factors in chronic pain: I. A half century of study. Pain. 1994;57:5–15. doi: 10.1016/0304-3959(94)90103-1. [DOI] [PubMed] [Google Scholar]
- 22.Apkarian AV. Bushnell MC. Treede RD. Zubieta JK. Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain. 2005;9:463–484. doi: 10.1016/j.ejpain.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 23.Kokebie R. Aggarwal R. Kahn S. Kartz RS. Muscle tension is increased in fibromyalgia: Use of a pressure gauge. Abstract 1935, American College of Rheumatology 2008 Annual Scientific Meeting; Oct 24–29;2008 ; San Francisco, California. [Google Scholar]
- 24.Morris C. Low Back Syndromes: Integrated Clinical Management; New York: McGraw-Hill Medical; 2005. [Google Scholar]
- 25.Simons DG. Travell JG. Travell & Simons' Myofascial Pain and Dysfunction: The Trigger Point Manual. Baltimore: Williams & Wilkins; 1999. p. 660. [Google Scholar]
- 26.Nansel D. Szlazak M. Somatic dysfunction and the phenomenon of visceral disease simulation: A probable explanation for the apparent effectiveness of somatic therapy in patients presumed to be suffering from true visceral disease. J Manip Physiol Ther. 1995;18:379–397. [PubMed] [Google Scholar]
- 27.Seaman D. Chiropractic care and visceral disorders: What is the neurological link? www.dynamicchiropractic.com/mpacms/dc/article.php?id=39453. [Dec 29;2011 ];Dynamic Chiropractic. 1996 14(24) [Google Scholar]
- 28.Hobson AR. Chizh B. Hicks K, et al. Neurophysiological evaluation of convergent afferents innervating the human esophagus and area of referred pain on the anterior chest wall. Am J Physiol Gastrointest Liver Physiol. 2010;298:G31–G36. doi: 10.1152/ajpgi.00288.2009. [DOI] [PubMed] [Google Scholar]
- 29.Morris CE. Low Back Syndromes: Integrated Clinical Management. New York: McGraw-Hill; 2005. p. 267. [Google Scholar]
- 30.Owens C. An Endocrine Explanation for Chapman's Reflexes. 2nd. Indianapolis, IN: Academy for Applied Osteopathy; 1963. [Google Scholar]
- 31.Washington K. Mosiello R. Venditto M, et al. Presence of Chapman reflex points in hospitalized patients with pneumonia. J Osteopath Assoc. 2003;103:479–483. [PubMed] [Google Scholar]
- 32.Travell J. Rinzter S. Herman M. Pain and disability of the shoulder and arm. JAMA. 1942;120:417–422. [Google Scholar]
- 33.Knutson G. The role of the γ-motor system in increasing muscle tone and muscle pain syndromes: A review of the Johansson/Sojka hypothesis. J Manip Physiol Ther. 2000;23:564–572. doi: 10.1067/mmt.2000.109674. [DOI] [PubMed] [Google Scholar]
- 34.Matre DA. Sinkjaer T. Svensson P. Arendt-Nielsen L. Experimental muscle pain increases the human stretch reflex. Pain. 1998;75:331–339. doi: 10.1016/s0304-3959(98)00012-8. [DOI] [PubMed] [Google Scholar]
- 35.Mense S. Pathophysiologic basis of muscle pain syndromes. Phys Med Rehab Clin N Am. 1997;8:23–53. [Google Scholar]
- 36.Mense S. Skeppar P. Discharge behavior of feline gamma motorneurons following induction of an artificial myositis. Pain. 1991;46:201–210. doi: 10.1016/0304-3959(91)90077-B. [DOI] [PubMed] [Google Scholar]
- 37.Ackerman JM. The Biophysics of the Vascular Autonomic Signal and Healing: Frontier Perspectives. Vol. 10. Philadelphia: Temple University; 2001. pp. 9–15. [Google Scholar]
- 38.Korr IM. Proprioceptors and somatic dysfunction. J Am Osteopath Assoc. 1975;74:638–650. [PubMed] [Google Scholar]
- 39.Korr IM. Sustained sympathicotonia as a factor in disease. In: Korr IM, editor. The Neurobiologic Mechanisms in Manipulative Therapy. New York: Plenum Press; 1978. [Google Scholar]
- 40.Stanfield CL. Germann WJ. Principles of Human Physiology. 3rd. New York: Pearson Benjamin Cummings; 2008. p. 427. [Google Scholar]
- 41.Robertson D, et al. Primer on the Autonomic Nervous System. 3rd. New York: Academic Press; 2011. [Google Scholar]
- 42.McKay KC. Prato FS. Thomas AW. A literature review: The effects of magnetic field exposure on blood flow and blood vessels in the microvasculature. Bioelectromagnetics. 2007;28:81–98. doi: 10.1002/bem.20284. [DOI] [PubMed] [Google Scholar]
- 43.Johansson H. Sojka P. Pathophysiological mechanisms involved in genesis and spread of muscular tension in occupational muscle pain and in chronic musculoskeletal pain syndromes: A hypothesis. Med Hypoth. 1991;35:196–203. doi: 10.1016/0306-9877(91)90233-o. [DOI] [PubMed] [Google Scholar]
- 44.Birznieks I. Burton AR. Macefield VG. The effects of experimental muscle and skin pain on the static stretch sensitivity of human muscle spindles in relaxed leg muscles. J Physiol. 2008;586:2713–2723. doi: 10.1113/jphysiol.2008.151746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pettman E. The facilitated segment. www.naiomt.com/www.naiomt.com/articles/05Oct.pdf. [Jul 4;2011 ];The North American Institute of Orthopædic Manual Therapy. 2005 IX(5) [Google Scholar]
- 46.Knutson GA. Owens EF. Active and passive characteristics of muscle tone and their relationship models of subluxation/joint dysfunction: Part I. J Can Chiopr Assoc. 2003;47:168–179. [Google Scholar]
- 47.Knutson GA. Owens EF. Active and passive characteristics of muscle tone and their relationship models of subluxation/joint dysfunction. Part II. J Can Chiopr Assoc. 2003;47:269–283. [Google Scholar]
- 48.Seaman D. Chiropractic Care and Visceral Disorders: What Is the Neurological Link? www.cpdo.net/res/page15.html. [Jan 19;2012 ]. www.cpdo.net/res/page15.html
- 49.Findley TW. Schleip R. Fascia Research: Basic Science and Implications for Conventional and Complementary Health Care. Munich: Elsevier GmbH; 2007. [Google Scholar]
- 50.Schleip R. Klingler W. Lehmann-Horn F. Active contraction of the thoracolumbar fascia: Indications of a new factor in low back pain research with implications for manual therapy. Presented at: 5th Interdisciplinary World Congress on Low Back & Pelvic Pain; Melbourne. Nov;2004 . [Google Scholar]
- 51.Schleip R. Klingler W. Lehmann-Horn F. Fascia is able to contract in a smooth muscle-like manner and thereby influence musculoskeletal mechanics. Presented at: 5th World Congress of Biomechanics; Munich, Germany. Jul 29;; 2006. August 4. [Google Scholar]
- 52.Schleip R. Naylor IL. Ursu D, et al. Passive muscle stiffness may be influenced by active contractility of intramuscular connective tissue. Med Hypotheses. 2006;66:66–71. doi: 10.1016/j.mehy.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 53.Finando S. Finando D. Fascia and the mechanism of acupuncture. J Bodywork Movement Ther. 2011;15:168–176. doi: 10.1016/j.jbmt.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 54.Wolff J. The Law of Bone Remodeling. Translation of the 1892 German edition. Berlin: Springer; 1986. [Google Scholar]
- 55.Rolf IP. Rochester, VT: Healing Arts Press; 1989. Rolfing. Reestablishing the Natural Alignment and Structural Integration of Human Body for Vitality and Well-Being; p. 129. [Google Scholar]
- 56.Simons DG. Travell JG. Travell & Simons' Myofascial Pain and Dysfunction: The Trigger Point Manual. 2nd. Baltimore: Williams & Wilkins; 1999. pp. 8–9. [Google Scholar]
- 57.Selye H. The Stress of Life. New York: McGraw-Hill Book Company; 1956. 1984. p. 219. Plate 3, or revised edition. [Google Scholar]
- 58.Hinz B. Masters and servants of the force: The role of matrix adhesions in myofibroblast force perception and transmission. Eur J Cell Biol. 2006;85:175–181. doi: 10.1016/j.ejcb.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 59.Tomasek J, et al. Myofibroblasts and mechano-regulation of connective tissue remodeling. Nat Rev Mol Cell Biol. 2002;3:349–363. doi: 10.1038/nrm809. [DOI] [PubMed] [Google Scholar]
- 60.Gabbiani G. The myofibroblast in wound healing and fibrocontractive diseases. J Pathol. 2003;200:500–503. doi: 10.1002/path.1427. [DOI] [PubMed] [Google Scholar]
- 61.Desmoulière A. Badid C. Bochaton-Piallat ML. Gabbiani G. Apoptosis during wound healing, fibrocontractive diseases and vascular wall injury. Int J Biochem Cell Biol. 1997;29:19–30. doi: 10.1016/s1357-2725(96)00117-3. [DOI] [PubMed] [Google Scholar]


