Abstract
Background
Fractures have been associated with subsequent increases in mortality, but it is unknown how long that increase persists.
Methods
5580 women from a large community-based multicenter US prospective cohort of 9704 (Study of Osteoporotic Fractures) were followed prospectively for almost 20 years. We age-matched 1116 hip fracture cases with four controls (n=4464). To examine the effect of health status, we examined a healthy older subset (n=960) aged 80+ who attended the 10-year follow-up examination, and reported good/excellent health. Incident hip fractures were adjudicated from radiology reports by study physicians. Death was confirmed by death certificates.
Results
Hip fracture cases had two-fold increased mortality in the year after fracture compared to controls [16.9% vs. 8.4%; Odds Ratio (OR)=2.4; 95% Confidence Interval (CI) 1.9, 3.1]. When examined by age and health status, short-term mortality was increased in those aged 65 to 70 (16.3% vs 3.7%; OR=5.0; 2.6, 9.5), aged 70 to 79 (16.5% vs 8.9%; OR=2.4; 1.8, 3.3), and only in aged 80+ with good/excellent health (15.1% vs. 7.2%; OR=2.8; 1.5, 5.2). After the first year, survival of hip fracture cases and controls was similar except in those aged 65 to 70 who continued to have increased mortality.
Conclusions
Short-term mortality is increased after hip fracture in women aged 65 to 79 and in exceptionally healthy women 80 or older. Women 70 and older return to previous risk levels after a year. Interventions are needed to decrease mortality in the year after hip fracture, when mortality risk is highest.
Keywords: Hip fracture, mortality, elderly, female
Introduction
Hip fractures are a major public health problem, with nearly 300,000 occurring annually in the United States.1 Hip fractures cause substantial short- and long-term disability1 as well as increased mortality.2-19
In a recent meta-analysis, women had nearly three-fold increased mortality risk in the year after hip fracture.16 Long-term (10 year) mortality data are mixed.2, 4, 7, 9, 12, 14, 20, 21 In the meta-analysis, excess mortality risk from hip fracture decreased during the first 2 years after fracture but did not return to the rate of aged matched controls during long-term (10 year) follow-up.16
Prior mortality risk estimates have some important limitations. Some studies used hospitalized patients or registries to identify samples while drawing controls from the general community.3, 6, 9, 10, 12, 14, 21 Such studies are likely biased by differences in health status of hip fracture cases compared to nonfracture controls. Using hospitalized patients or registries also does not allow for examination of health status or other important covariates, such as bone mineral density (BMD), prior to fracture occurrence. Other studies have combined nursing home residents and community-dwelling women, populations which would be expected to have very different health status.16
Such methodological limitations have made it difficult to determine whether the noted increase in mortality after hip fracture is due to underlying poor health or the hip fracture itself. Some studies have found that healthy participants without comorbidities have no increased mortality risk after hip fracture3, 4, 15 and have concluded that comorbidities explain much of the increased mortality risk after hip fracture;2, 6, 19, 22 others have noted higher mortality in those without comorbidities compared to those with comorbidities.14
Prior studies exploring the influence of age on mortality after hip fracture are conflicting, and limitations include insufficient information about health status13, 23 and use of registries to retrospectively identify cases.9, 13 Some studies have found mortality after hip fracture increases with age.6, 12, 24-26 However, in several studies from Europe, the relative risk of death after hip fracture compared to the risk of death in the general population was lower in older, compared to younger, hip fracture patients.9, 13, 23
Among 5580 community-dwelling ambulatory women age 65 and older enrolled in our prospective cohort (1116 incident hip cases and 4464 age-matched controls), our aim was to determine the short-(<1 year), intermediate-(≥1 to 5 years), and long-term (≥5 to 10 years) mortality associated with hip fracture. Because expected mortality rates increase significantly with advanced age combined with poor health, a secondary aim was to determine if healthy women aged 80 and older would have increased mortality associated with hip fracture, compared to healthy age-matched controls.
Methods
Study Sample
In 1986-88, the Study of Osteoporotic Fractures recruited 9704 community-dwelling women, age 65 or older (>99% Non-Hispanic White) in four US regions: Baltimore County, Maryland; Minneapolis, Minnesota; Portland, Oregon; and the Monongahela Valley near Pittsburgh.27 Women unable to walk without assistance and those with bilateral hip replacements were excluded. All women provided written consent, and SOF was approved by each site’s Institutional Review Board.
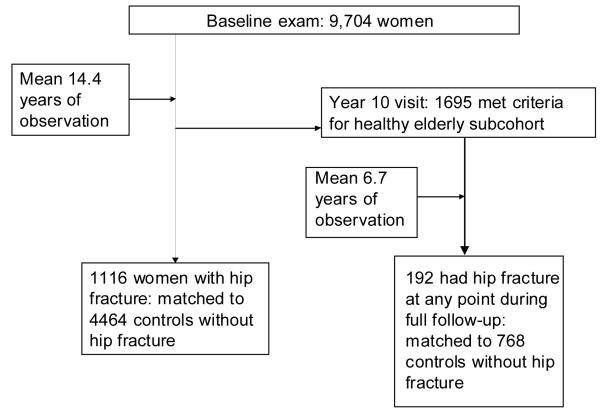
We prospectively followed 1116 women who had an adjudicated incident hip fracture (cases) during almost 20 years of follow-up until December, 2005 (mean 14.4 years; Figure 1).27 Each fracture case was matched by exact year of age at baseline with four controls (n=4464) without hip fracture; controls had to similarly survive at least to the time of the case hip fracture. To confirm that the selected controls were representative of the SOF population, we compared frequencies and means of selected baseline characteristics (age, body mass index, hip bone mineral density, pack years smoked, mini mental status exam, health status, standing from a chair, and medical conditions) between nonfracture participants who were selected and not selected for this analysis. The two groups were relatively similar except that those who were not selected for the study were younger (69 vs. 73 years [age was a matching criteria for the fracture cases]). We followed women for up to 19 years after hip fracture (mean 4.8 years).
Figure 1.
Flow of Study Participants
Healthy Subset Study Sample
To determine if healthy women age 80 and older have increased mortality associated with hip fracture compared to healthy age-matched controls, we also analyzed a healthy older subset of women, chosen based on their status at the year 10 SOF exam (Figure 1). Inclusion criteria for the healthy subset were: 1) survival to age 80 or more at Year 10; 2) healthy enough to return to the clinic for their year 10 examination (i.e., did not need to have the exam at their home); and 3) reported good or excellent health at year 10. Of this healthy subset, 192 had an adjudicated incident fracture during a mean of 6.7 years follow-up after the year 10 exam (defined as cases for this analysis). These cases were matched by age with four controls (n=768) from the healthy subset who had survived to the time of the case’s fracture.
Baseline characteristics
Weight was measured in light clothing without shoes by a balance-beam scale and height was measured by stadiometer. These measures were then used to compute body mass index (BMI).27 Cognitive function was assessed using a modified version of the Mini-Mental State Examination (MMSE).28 Neuromuscular function tests included a subject’s ability to stand from a chair, without using her arms.29 Age, smoking and alcohol consumption, medical history, and self-reported health were determined by questionnaire and interview at baseline and current medications were recorded.
Bone Mineral Density (BMD)
Dual-energy x-ray absorptiometry (DXA) was first available and measured by Hologic QDR 1000 in 1988-1990 at the two-year exam (Hologic, Bedford, Massachusetts). DXA BMD measurement standards and precision have been previously detailed30 and quality control procedures were rigorous.27 Complete data for DXA total hip BMD was available for 86.1% of the cohort at the year 2 exam.
Ascertainment of incident hip fractures and mortality
Participants were contacted every four months by postcard (with phone follow-up for non-responders) to ascertain incident hip fractures or death; more than 95% of these contacts were completed. Incident hip fractures were obtained from radiology reports. Cause of death was determined from death certificates and, if available, other supporting documentation (medical records, hospital discharge data) at each SOF clinic site. For consistency in coding across SOF sites, all final outcomes (hip fracture and cause of death) were centrally adjudicated by a physician at the SOF Coordinating Center. Final adjudicated cause of death was done using ICD-9 codes and cause of death was categorized at the coordinating center.31
Statistical Analyses
We identified death within the first year following the fracture for each woman within a matched case and control quintuplet (1 case plus 4 controls), based on the date of fracture for the case. When no death occurred for any woman within the quintuplet, we also evaluated mortality from one to five years; quintuplets without a death within 5 years post-case fracture were further evaluated for mortality from five to 10 years of the case fracture date. Thus, in the 5- to 10-year period, all five women in the quintuplet had to survive at least 5 years.
We used conditional logistic regression to evaluate the associations between hip fracture and mortality during several post-fracture time periods. Based on prior studies of the association between fracture and mortality,2, 32 models were adjusted for age, BMD, smoking status, self-reported health status, SOF clinical site, history of diabetes, hypertension, stroke or Parkinson’s disease, MMSE score, and ability to stand from a chair at the baseline exam. Total hip BMD was then added to the model to evaluate its effect. We tested for the presence of interaction by stratifying for age groups (<70, 70-79, 80+ years). We also examined the associations between intertrochanteric and femoral neck fractures on mortality. We repeated the analyses in the healthy subset of older women, as defined at the year 10 exam. We used SAS 8.2. We considered p<0.05 to be significant.
Results
Baseline characteristics
Hip fracture cases had lower BMI, lower total hip BMD, and more cigarette exposure than age matched non-fracture controls (Table 1). A slightly greater proportion of cases had Parkinson’s disease and needed their arms to stand from a chair compared with controls, but mean MMSE score was similar in the two groups. In those under the age of 70 (but not in the older age groups), more cases than controls had diabetes (p=.002). Self-reported health status was worse in those over the age of 80 who fractured compared to non-fracture controls (p=.04), but health status was not different between younger cases and controls (data not shown).
Table 1.
Characteristics of Study Participants
| Overall | Healthy Elderly Subset | |||||
|---|---|---|---|---|---|---|
|
|
||||||
|
Hip
Fractures (N=1116) |
Non- Fractures (N=4464) |
p-Value |
Hip
Fractures (N=192) |
Non- Fractures (N=768) |
p-Value | |
| Age, years (mean, SD) | 73.0 (5.1) | 73.0 (5.1) | * | 83.7 (3.2) | 83.7 (3.2) | * |
| Body mass index, kg/m2 (mean, SD) |
25.4 (4.1) | 26.7 (4.6) | .0001 | 24.3 (4.0) | 26.1 (4.2) | .0001 |
| Total hip BMD, grams/cm2 (mean, SD) |
0.69 (0.1) | 0.76 (0.1) | .0001 | 0.63 (0.1) | 0.72 (0.1) | .0001 |
| Current smoker (n, %) | 120 (10.8) | 334 (7.5) | .001 | 10 (5.2) | 19 (2.5) | .05 |
| Self-rated health, good/excellent (n,%) |
925 (82.9) | 3761 (84.3) | .27 | 192 (100.0) | 768 (100.0) | - |
| Diabetes (n, %) | 85 (7.6) | 280 (6.3) | .10 | 6 (3.1) | 21 (2.7) | .77 |
| Hypertension (n, %) | 446 (40.0) | 1761 (39.5) | .76 | 65 (33.9) | 249 (32.4) | .71 |
| Stroke (n, %) | 37 (3.3) | 129 (2.9) | .45 | 9 (4.7) | 29 (3.8) | .56 |
| Parkinson’s disease (n, %) |
13 (1.2) | 21 (0.5) | .01 | †† | †† | - |
| MMSE score (mean, SD) † |
24.6 (1.7) | 24.6 (1.7) | .99 | 27.7 (2.0) | 27.8 (2.2) | .46 |
| Uses arms to stand from chair (n, %) |
58 (5.2) | 171 (3.8) | .04 | 24 (12.5) | 121 (15.8) | .26 |
Hip fracture cases and non-fracture controls were matched on exact year of age at baseline
Modified Mental Status Exam
Data not available
Association between hip fracture and subsequent mortality
Overall, 48.2% (n=2690) of the sample died during a mean 14.4 (± 4.1 SD) years of follow-up. Mortality risk was highest in the first year after hip fracture (Table 2). During the first year after an index hip fracture, 16.9% (n=189) of the cases died compared with 8.4% (n=374) of the non-fracture controls [OR 2.2 (1.8, 2.7)]. This increase in mortality persisted when the analysis was adjusted for other risk factors for hip fracture, including total hip BMD [OR 2.4 (1.9, 3.1)]. While deaths in the control group were evenly spread over the first year of observation (~25% every 3 months), 72% of year 1 deaths in the cases occurred within 6 months of a hip fracture. Moreover, over half (52%) of deaths in the first year following hip fracture occurred within the first 3 months for the cases.
Table 2.
Effects of Hip Fracture on Subsequent Mortality
| Hip fracture participants No. Deaths /Total No.* (%) |
Non-fracture participants No. Death/ Total No.* (%) |
Unadjusted OR† |
Multivariable Adjusted OR†† |
|
|---|---|---|---|---|
| OVERALL | 655 / 1116 (58.7) |
2035 / 4464 (45.6) |
2.0 (1.7, 2.3) |
2.0 (1.6, 2.4) |
| 0 to <1 YEAR | 189 / 1116 (16.9) |
374 / 4464 (8.4) |
2.2 (1.8, 2.7) |
2.4 (1.9, 3.1) |
| ≥1 to 5 YEARS | 164 / 668 (24.6) |
585 / 2672 (21.9) |
1.2 (1.0, 1.5) |
1.2 (0.9, 1.5) |
| ≥5 to10 YEARS | 36 / 253 (14.2) |
101 / 1012 (10.0)‡‡ |
1.6 (1.0, 2.6) |
1.4 (0.8, 2.6) |
Decrease in total number of deaths with each time strata reflects removal of entire quintuplets (case and 4 matching controls) from analysis upon death of any member of quintuplet.
Odds ratios based on conditional logistic regression.
Multivariable model (n=4716) includes age, BMI, pack years of smoking, clinic, history of diabetes, hypertension, stroke, MMSE score, ability to stand from chair at baseline exam, self-reported health, Parkinson’s disease, and total hip BMD.
The participants remaining in the analysis by ≥5 to10 years after their hip fracture were younger, had a higher hip BMD, had higher self rated health, had less diabetes and hypertension, had higher MMSE scores, and were less likely to use their arms to stand from a chair compared to those not remaining the analysis. These differences likely account for the lower absolute death rate in years 5 to 10 compared to years zero to five. This decrease in mortality rate at the ≥5 to10 year time point also occurred when all 5,580 women in the cohort were considered, confirming that cases and controls remained comparable over time.
Mortality risks for fracture and non-fracture participants were generally similar after the first year (Table 2). In the 3340 participants who remained in the analysis after the first year (because no one in their quintuplet had died), 24.6% (n=164) of hip fracture cases and 21.9% (n=585) of controls died by year 5 [OR 1.2 (1.0, 1.5)]; the association was no longer significant after adjusting for potential confounders [1.2 (0.9, 1.5)]. Among the 1265 remaining in the analysis between five and 10 years, 14.2% (n=36) of hip fracture cases compared with 10.0% (n=101) of non-fracture controls had died by the end of follow-up [OR 1.6 (1.0, 2.6)]; however, this increased risk was no longer present in multivariable models [OR 1.4 (0.8, 2.6]. The associations were similar when stratified by type of fracture (femoral neck and intertrochanteric fracture data available in online tables).
We noted a significant interaction between age and risk of death after hip fracture (p=0.002). When stratified into 3 age categories (<70, 70 to 79, and 80+ years at baseline exam), the risk of death from hip fracture decreased as age increased (Table 3). Those aged 65 to 69 who suffered a hip fracture had a 5-fold increased risk of death in the first year [OR 5.0 (2.6, 9.5)]. In contrast, there was no increased risk of death in the first year after a hip fracture in those over the age of 80 years [OR 1.1 (0.6, 2.1)]. Those aged 70 to 79 had a risk of death in the first year that was intermediate between the youngest and oldest SOF participants [OR 2.4 (1.8, 3.3)]. Examining longer term follow-up, those aged 65 to 70 had an increased risk of mortality after hip fracture during the 1 to 5 [OR 1.9 (1.1, 3.2)] and 5 to 10 year follow-up [OR 3.2 (1.0, 10.2)] periods, although risks were attenuated compared to the first year. The older age groups did not have an increased risk of death in longer term follow-up.
Table 3.
Odds of death after hip fracture according to age strata
| Age <70 N=1630 |
Age 70-79 N=3235 |
Age 80+ N=715 |
|
|---|---|---|---|
| OVERALL | 2.9 (2.0, 4.1) | 1.8 (1.4, 2.2) | 0.9 (0.5, 1.7) |
| 0 to < 1 YEAR | 5.0 (2.6, 9.5) | 2.4 (1.8, 3.3) | 1.1 (0.6, 2.1) |
| ≥ 1 to 5 YEARS | 1.9 (1.1, 3.2) | 1.1 (0.8, 1.5) | 0.7 (0.3, 1.7) |
| ≥ 5 to10 YEARS | 3.2 (1.0, 10.2) | 0.9 (0.4, 2.0) | 0.5 (0.1, 3.7) |
Odds ratios are based on conditional logistic regression and adjusted for age, BMI, pack years of smoking, clinic, history of diabetes, hypertension, stroke, MMSE score, ability to stand from chair at baseline exam, self-reported health, Parkinson’s disease, and total hip BMD. If model variables were non-estimable because of small cell size, we removed them.
Association between hip fracture and subsequent mortality in the healthy subset
Healthy women over the age of 80 years did not have overall increased mortality after fracture (Table 4). However, short-term mortality was increased among these women: hip fracture cases had a nearly three-fold increased risk of death in the first year after a fracture, even after adjustment for other risk factors including BMD [OR 2.8 (1.5, 5.2)]. In the 600 women who remained in the analysis after the first year (because no one in quintuplet had died), the risk of death was not increased. Indeed, there may even have been a decreased risk of death in hip fracture cases from 1 to 5 years after hip fracture, although the results were statistically significant only in the multivariable models adjusted for total hip BMD [OR 0.4 (0.2, 0.8)].
Table 4.
Effects of Hip Fracture on Subsequent Mortality in Healthy Subset of Elderly Women
| Hip fracture participants No. Death /Total No.* (%) |
Non-fracture participants No. Death /Total No.* (%) |
Unadjusted OR† |
Multivariable Adjusted OR†† |
|
|---|---|---|---|---|
| OVERALL | 66 / 192 (34.4) |
214 / 768 (27.9) |
1.4 (1.0, 2.0) |
1.3 (0.9, 2.0) |
| 0 to <1 YEAR | 29 / 192 (15.1) |
55 / 768 (7.2) |
2.3 (1.4, 3.7) |
2.8 (1.5, 5.2) |
| ≥1 to 5 YEARS | 18 / 120 (15.0) |
94 / 480 (19.6) |
0.7 (0.4, 1.2) |
0.4 (0.2, 0.8) |
| ≥5 to10 YEARS | 3 / 53 (5.7%) |
7 / 212 (3.3)‡‡ |
2.2 (0.4, 11.7) |
2.3 (0.3, 19.0) |
Decrease in total number of deaths with each time strata reflects removal of entire quintuplets (case and 4 matching controls) from analysis upon death of any member of quintuplet.
Odds ratios based on conditional logistic regression.
Multivariable model (n=891) includes age, BMI, current smoke status, clinic, history of diabetes, hypertension, stroke, MMSE score, ability to stand from chair at baseline exam, and total hip BMD. If model variables were non-estimable because of small cell size, we removed them.
The participants remaining in the analysis by ≥5 to10 years after their hip fracture were younger, had a higher hip BMD, had higher self rated health, had less diabetes and hypertension, had higher MMSE scores, and were less likely to use their arms to stand from a chair compared to those not remaining the analysis. These differences likely account for the lower absolute death rate in years 5 to 10 compared to years zero to five. This decrease in mortality rate at the ≥5 to10 year time point also occurred when all 5,580 women in the cohort were considered, confirming that cases and controls remained comparable over time.
Causes of death
In the overall sample, the leading causes of death were coronary heart disease, cancer, and stroke in both the hip fracture cases and controls. There were no differences in death rate from coronary heart disease between fracture cases and controls (24.9% vs 26.0%), stroke (9.8% vs 11.7%), or sepsis (1.8 % vs 2.1%). However, a greater proportion of hip fracture cases than controls died from pneumonia (10.5% vs 5.6%; p<.0001), cognitive disorders (9.2% vs 6.7%; p=0.03), and osteoporotic fracture (2% vs 0%; p<.0001); in contrast, more controls died of cancer (11.0% cases vs 18.2% controls; p<.0001).
Discussion
We found women over the age of 65 who suffer a hip fracture have a two-fold increased risk of death in the first year after the fracture compared with similarly aged women who do not suffer a hip fracture. After the first year, mortality rates are similar when we examined the entire cohort of SOF women. Our overall findings of increased short-term mortality are consistent with a recent meta-analysis16 that found an almost three-fold increased risk of death in the first year after a hip fracture. Previous data on long-term mortality are mixed2, 4, 7, 9, 12, 14, 16, 21, 33 with some,16 but not all,7, 12 showing increased mortality risk for up to 10 years after hip fracture, although excess mortality risk was lower during later years of follow-up compared to the first year or two after hip fracture.16
Limitations in previous study designs have made it difficult to determine whether excess mortality was driven by the hip fracture itself or differences in pre-fracture health status and/or age. Because of the large size and prospective, extended follow-up of the SOF cohort, we were able to examine the effects of both health status and age on the association between hip fracture and mortality and found they may influence mortality risk after fracture. Those aged 65 to 70 years had the greatest risk of short-term death (5-fold) after a hip fracture. In contrast, the oldest participants (80+ years) overall had no increased short-term mortality risk after a hip fracture. However, when we separately examined women over the age of 80 who reported good to excellent health status, we did find a two-fold increased risk of death in the first year after a fracture. Similarly, when we examined long-term mortality by age and health status, we found that those age 65 to 70 had a persistent increase in intermediate and long-term (5 to 10 year) mortality, although the risks were attenuated compared to short-term risk. In contrast, the oldest participants (80+ years) had no increased intermediate or long-term mortality risk after a hip fracture, regardless of their health status. Our data suggest that previous mixed results with regard to mortality, especially long-term mortality, after hip fracture may have been due to differences in the underlying age and health status of the population being studied.
Our finding that short-term mortality risk was only elevated in the exceptionally healthy over the age of 80 and not the whole population of over 80 suggests that hip fracture itself may contribute to increased mortality in these older women. Most, but not all,9, 14 prior studies have concluded that increased mortality risk after hip fracture was due to underlying comorbidities such as cardiovascular disease, stroke, respiratory disease, diabetes, or cancer.2-4, 6, 14, 15, 19, 22 An earlier study conducted in the SOF cohort concluded that a two-fold increased mortality risk in hip or pelvic fracture cases compared to non-fracture controls during 5.9 years of study (n=64 deaths)2 was a consequence of increased comorbid conditions in hip fracture cases.
Because the background mortality rate is very high in women age 80 and older, especially with poor health, it would be more difficult to distinguish an additional independent risk of hip fracture on mortality. Our purpose in evaluating the exceptionally healthy subset was to better isolate the independent effects of hip fracture on mortality from that of comorbidities, and indeed we found an increased risk in the first year after hip fracture compared to their similarly healthy age-matched controls.
Consistent with hip fracture being a contributor to death, among the whole cohort we also found the highest increase in mortality risk was in the first 3 months after hip fracture. Although in our study less than 15% of the deaths were due to infection or osteoporosis, the most likely causes of death to be directly attributed to the fracture itself, hip fracture could have been a contributing cause in many of the remaining deaths, including those attributed to coronary heart disease and stroke.
Our finding that younger women have the highest mortality risk is consistent with some9, 13, 23 but not all previous studies.6, 12, 24-26 However, prior studies were unable to disentangle the effects of age from health status. Our identification of women prior to their fracture, prospective study design, and extensive data on co-morbidities allowed us to better examine how age and health status each influence mortality after hip fracture. We hypothesize that age influences risk of death after hip fracture by affecting the baseline death rate in the population. Those who are younger and/or healthier have a low risk of dying from other causes. Therefore, suffering a hip fracture may increase their mortality risk compared to nonfracture controls. In contrast, octogenarians generally have a relatively high risk of dying from other causes and so suffering a hip fracture does not actually result in an increased risk of death over the next year compared to other women their age, unless they are exceptionally healthy. This hypothesis is supported by the recent meta-analysis on the association between hip fracture and mortality;16 in that analysis, mortality from other causes increased rapidly with age, reducing the absolute excess mortality after hip fracture in the oldest group of patients.
Our study has important strengths. It was set within a large community-based prospective study of older women, with rigorous quality control of BMD measurements and study physician-adjudicated hip fracture data. Retention of survivors was excellent, with well over 95% completion of follow-up information—including women who became too frail to attend subsequent visits. We were able to adjust for several important covariates.
Our study also has several limitations. It was conducted in postmenopausal white women age 65 years or older and may not be generalizable to men, other ethnic groups, and younger women. However, it provides important information on the group most likely to suffer from hip fracture—older white women. One of our study’s strengths—its long observation period--is also a limitation in that standard care for treatment of hip fractures has changed over time.34 However, as mortality rates after hip fracture have not decreased much, if at all, over the past 10 to 40 years,7, 35, 36 our results are likely still relevant to considerations for prevention of hip fracture and its associated mortality.
Despite our selection of a healthy subset and adjustment for multiple risk factors, we cannot exclude residual confounding by other diseases or frailty. We often measured covariates months to years prior to the time of fracture and during that period, women’s health status may have changed. In the healthy subcohort, women may have developed new co-morbidities that might have changed their health status between the year 10 visit (when the healthy subcohort was defined) and fracture occurrence. It is also important to note that in age-stratified analyses, because of decreased overall survival, the number of cases and events in the oldest population was lower than in the younger age groups, and so we had decreased power to detect a significant association if it were present.
Conclusions
Because hip fracture risk increases with age, hip fractures are expected to become an even larger public health issue as the population ages; some experts predict there will be 6.3 to 8.2 million hip fractures annually worldwide in 2050.1, 37 Overall, older women who suffer a fracture have a two-fold increased mortality in the first year after hip fracture. Women who are either less than 80 or 80+ and healthy have the highest risk of dying in the first year compared to women of similar age and health status. If our findings are replicated, they would suggest that research should focus on hip fracture prevention and interventions in these groups that could decrease mortality during that high-risk period. Women who are between the age of 65 and 70 continue to have an increased risk of mortality for up to 5 to 10 years and so prevention of hip fractures in these women should be of high priority.
Acknowledgments
Thank you to Martie Sucec for her editorial assistance and Desirée Pheister for her assistance with manuscript preparation.
Funding Acknowledgment: This research was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Institute on Aging (Public Health Service grants 2 R01 AG027574-22A1, R01 AG005407, R01 AG027576-22, 2 R01 AG005394-22A1, AG05407, AG05394, AR35583, AR35582 and AR35584). In addition, ESL is supported by K23-RR020049. The SOF investigators were completely independent of the funding source to design and conduct the study including data.
Footnotes
Conflict of Interest: The authors have no conflict of interests to disclose.
Reference List
- (1).Marks R, Allegrante JP, Ronald MC, Lane JM. Hip fractures among the elderly: causes, consequences and control. Ageing Res Rev. 2003 Jan;2(1):57–93. doi: 10.1016/s1568-1637(02)00045-4. [DOI] [PubMed] [Google Scholar]
- (2).Browner WS, Pressman AR, Nevitt MC, Cummings SR. Mortality following fractures in older women. The study of osteoporotic fractures. Arch Intern Med. 1996 Jul 22;156(14):1521–5. [PubMed] [Google Scholar]
- (3).Meyer HE, Tverdal A, Falch JA, Pedersen JI. Factors associated with mortality after hip fracture. Osteoporos Int. 2000;11(3):228–32. doi: 10.1007/s001980050285. [DOI] [PubMed] [Google Scholar]
- (4).Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003 Jan;17(1):53–6. doi: 10.1097/00005131-200301000-00008. [DOI] [PubMed] [Google Scholar]
- (5).Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ. Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc. 2002 Oct;50(10):1644–50. doi: 10.1046/j.1532-5415.2002.50455.x. [DOI] [PubMed] [Google Scholar]
- (6).Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK. The components of excess mortality after hip fracture. Bone. 2003 May;32(5):468–73. doi: 10.1016/s8756-3282(03)00061-9. [DOI] [PubMed] [Google Scholar]
- (7).Giversen IM. Time trends of mortality after first hip fractures. Osteoporos Int. 2007 Jun;18(6):721–32. doi: 10.1007/s00198-006-0300-1. [DOI] [PubMed] [Google Scholar]
- (8).Empana JP, rgent-Molina P, Breart G. Effect of hip fracture on mortality in elderly women: the EPIDOS prospective study. J Am Geriatr Soc. 2004 May;52(5):685–90. doi: 10.1111/j.1532-5415.2004.52203.x. [DOI] [PubMed] [Google Scholar]
- (9).Farahmand BY, Michaelsson K, Ahlbom A, Ljunghall S, Baron JA. Survival after hip fracture. Osteoporos Int. 2005 Dec;16(12):1583–90. doi: 10.1007/s00198-005-2024-z. [DOI] [PubMed] [Google Scholar]
- (10).Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA. Race and sex differences in mortality following fracture of the hip. Am J Public Health. 1992 Aug;82(8):1147–50. doi: 10.2105/ajph.82.8.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Wolinsky FD, Fitzgerald JF, Stump TE. The effect of hip fracture on mortality, hospitalization, and functional status: a prospective study. Am J Public Health. 1997 Mar;87(3):398–403. doi: 10.2105/ajph.87.3.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Schroder HM, Erlandsen M. Age and sex as determinants of mortality after hip fracture: 3,895 patients followed for 2.5-18.5 years. J Orthop Trauma. 1993;7(6):525–31. doi: 10.1097/00005131-199312000-00007. [DOI] [PubMed] [Google Scholar]
- (13).Forsen L, Sogaard AJ, Meyer HE, Edna T, Kopjar B. Survival after hip fracture: short- and long-term excess mortality according to age and gender. Osteoporos Int. 1999;10(1):73–8. doi: 10.1007/s001980050197. [DOI] [PubMed] [Google Scholar]
- (14).Magaziner J, Lydick E, Hawkes W, et al. Excess mortality attributable to hip fracture in white women aged 70 years and older. Am J Public Health. 1997 Oct;87(10):1630–6. doi: 10.2105/ajph.87.10.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (15).Poor G, Atkinson EJ, O’Fallon WM, Melton LJ., III Determinants of reduced survival following hip fractures in men. Clin Orthop Relat Res. 1995 Oct;(319):260–5. [PubMed] [Google Scholar]
- (16).Haentjens P, Magaziner J, Colon-Emeric CS, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010 Mar 16;152(6):380–90. doi: 10.1059/0003-4819-152-6-201003160-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (17).Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009 Feb 4;301(5):513–21. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- (18).Petersen MB, Jorgensen HL, Hansen K, Duus BR. Factors affecting postoperative mortality of patients with displaced femoral neck fracture. Injury. 2006 Aug;37(8):705–11. doi: 10.1016/j.injury.2006.02.046. [DOI] [PubMed] [Google Scholar]
- (19).Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005 Dec 10;331(7529):1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).LeBlanc ES, Carlson NE, Carello PE, Samuels MH. Relationship between estradiol fluctuations over 24 hours and menopausal symptoms; Endo Society poster presentation (#P2-509); 2008. Ref Type: Generic. [Google Scholar]
- (21).Pitto RP. The mortality and social prognosis of hip fractures. A prospective multifactorial study. Int Orthop. 1994 Apr;18(2):109–13. doi: 10.1007/BF02484420. [DOI] [PubMed] [Google Scholar]
- (22).Hamlet WP, Lieberman JR, Freedman EL, Dorey FJ, Fletcher A, Johnson EE. Influence of health status and the timing of surgery on mortality in hip fracture patients. Am J Orthop (Belle Mead NJ) 1997 Sep;26(9):621–7. [PubMed] [Google Scholar]
- (23).Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004 Nov;15(11):897–902. doi: 10.1007/s00198-004-1627-0. [DOI] [PubMed] [Google Scholar]
- (24).Mortimore E, Haselow D, Dolan M, et al. Amount of social contact and hip fracture mortality. J Am Geriatr Soc. 2008 Jun;56(6):1069–74. doi: 10.1111/j.1532-5415.2008.01706.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (25).Bass E, French DD, Bradham DD, Rubenstein LZ. Risk-adjusted mortality rates of elderly veterans with hip fractures. Ann Epidemiol. 2007 Jul;17(7):514–9. doi: 10.1016/j.annepidem.2006.12.004. [DOI] [PubMed] [Google Scholar]
- (26).Holt G, Smith R, Duncan K, Finlayson DF, Gregori A. Early mortality after surgical fixation of hip fractures in the elderly: an analysis of data from the scottish hip fracture audit. J Bone Joint Surg Br. 2008 Oct;90(10):1357–63. doi: 10.1302/0301-620X.90B10.21328. [DOI] [PubMed] [Google Scholar]
- (27).Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995 Mar 23;332(12):767–73. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- (28).Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987 Aug;48(8):314–8. [PubMed] [Google Scholar]
- (29).Nelson HD, Nevitt MC, Scott JC, Stone KL, Cummings SR. Smoking, alcohol, and neuromuscular and physical function of older women. Study of Osteoporotic Fractures Research Group. JAMA. 1994 Dec 21;272(23):1825–31. doi: 10.1001/jama.1994.03520230035035. [DOI] [PubMed] [Google Scholar]
- (30).Steiger P, Cummings SR, Black DM, Spencer NE, Genant HK. Age-related decrements in bone mineral density in women over 65. J Bone Miner Res. 1992 Jun;7(6):625–32. doi: 10.1002/jbmr.5650070606. [DOI] [PubMed] [Google Scholar]
- (31).Cauley JA, Seeley DG, Browner WS, et al. Estrogen replacement therapy and mortality among older women. The study of osteoporotic fractures. Arch Intern Med. 1997 Oct 27;157(19):2181–7. [PubMed] [Google Scholar]
- (32).Ensrud KE, Ewing SK, Taylor BC, et al. Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci. 2007 Jul;62(7):744–51. doi: 10.1093/gerona/62.7.744. [DOI] [PubMed] [Google Scholar]
- (33).Robbins JA, Biggs ML, Cauley J. Adjusted mortality after hip fracture: From the cardiovascular health study. J Am Geriatr Soc. 2006 Dec;54(12):1885–91. doi: 10.1111/j.1532-5415.2006.00985.x. [DOI] [PubMed] [Google Scholar]
- (34).Gehlbach SH, Avrunin JS, Puleo E. Trends in hospital care for hip fractures. Osteoporos Int. 2007 May;18(5):585–91. doi: 10.1007/s00198-006-0281-0. [DOI] [PubMed] [Google Scholar]
- (35).Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ. Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury. 2008 Oct;39(10):1157–63. doi: 10.1016/j.injury.2008.03.022. [DOI] [PubMed] [Google Scholar]
- (36).Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009 Oct 14;302(14):1573–9. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (37).Sambrook P, Cooper C. Osteoporosis. Lancet. 2006 Jun 17;367(9527):2010–8. doi: 10.1016/S0140-6736(06)68891-0. [DOI] [PubMed] [Google Scholar]