Abstract
Objective
To investigate the way that family stress influences glycemic control among patients with diabetes who are younger than 18 years of age.
Data sources
PubMed and Scopus were searched for relevant studies published since 1990 using the following key words: diabetes type 1, glycemic control, family stress, family conflict, and family function.
Study selection
In total, 1478 papers were identified in the initial search. The final review included 6 cohort studies, 3 cross-sectional studies, and 1 qualitative review in which family stress was assessed using specific diabetes-related conflict measurement instruments, and glycemic control was evaluated by glycosylated hemoglobin measurement.
Synthesis
In most studies family stress was negatively correlated with patients' glycemic control. Family function was strongly related to patients' glycemic control, while family conflict was adversely associated with glycemic control. Families of low socioeconomic status, those of adolescents with diabetes, and those of single parents were more prone to diabetes-related stress and thus more susceptible to worse glycemic control.
Conclusion
Therapeutic psychological interventions and educational programs can help alleviate family diabetes-related stress and will likely improve glycemic control.
Type 1 diabetes mellitus (T1DM) is a metabolic disease in which insulin replacement therapy is required for life.1 The incidence of childhood-onset diabetes is increasing in many countries in the world.2 In 2002, it was 14.9/100 000 people yearly in those younger than 16 years of age in the United Kingdom. The estimated prevalence in those younger than 16 years of age is 1.62/1000 in England, 2.08/1000 in Northern Ireland, and 1.8/1000 in Wales; thus, in the United Kingdom, a general practice with 2500 child patients can expect 1 new diagnosis of T1DM every 2.5 to 3 years.3 There are clear indications of geographic differences in trends, but the overall annual increase is estimated to be about 3%.4,5 Type 1 diabetes can be a stressful condition owing to its unexpected and dramatic onset in childhood or early adulthood, the life-threatening nature of severe abnormalities in plasma glucose levels, and the potential long-term complications that can cause disability, employment difficulties, and career problems.6 Given the limited self-care abilities of young children, parents of children with diabetes bear nearly all of the responsibility for illness management. In cases of adolescent-onset T1DM, an additional set of stress factors comes into play.7-9
The families of young patients with diabetes experience high levels of stress (parental worries, for example, about long-term complications, or conflicts over T1DM management, such as diet issues, poor adherence to treatment, and patient resistance to the painful process of injection and measurement10) that influence not only the family itself but also the treatment process and thus the patients' glycemic control.11 The presence of a chronic pediatric condition is a recognized source of increased distress among family members,12 which can lead to disruptions in intrafamilial relationships, family structure, and family cohesion. It has also been consistently demonstrated that family functioning is a powerful determinant of overall quality of life and well-being in youth with chronic medical conditions.13 Family functioning can be affected differently based on specific characteristics of a child's chronic condition.14 Those patients with diabetes who experience high levels of family conflict, and hence family stress, show poor adherence to treatment and poorer glycemic control.15 There is, however, considerable variability in study design and in the family function measurement scales and questionnaires used in the studies examining this topic. In this systematic review, we chose to review articles that used glycosylated hemoglobin A1c (HbA1c) levels as a measure of glycemic control. The concentration of HbA1c, generally expressed as the proportion of hemoglobin that is HbA1c, is known to correlate with average blood glucose levels over the preceding 3 months.16 It is a valid tool for diabetes monitoring, for which robust outcome data are available. The recommended target HbA1c for all ages is below 7.5%.17
The main goal of this systematic review was to investigate the influence of family function, such as perceived family support (care and warmth), family stressors, the level of parental involvement in the care of diabetes (guidance and control, judgmental parental behaviour), and family organization (cohesion, conflict, expression), on the glycemic control of patients with T1DM. Additional goals were to explore predictors of conflict and the high diabetes-related stress within families, and to summarize the familial elements that might interfere with glycemic control for patients in the everyday practice of physicians.
Data Sources
The PubMed and Scopus databases were searched to identify relevant studies published since 1990. Search terms included MeSH terms relating to HbA1c for glycemic control and to diabetes-related family conflict or stress: diabetes type 1, glycemic control, family stress, family conflict, and family function.
Study selection
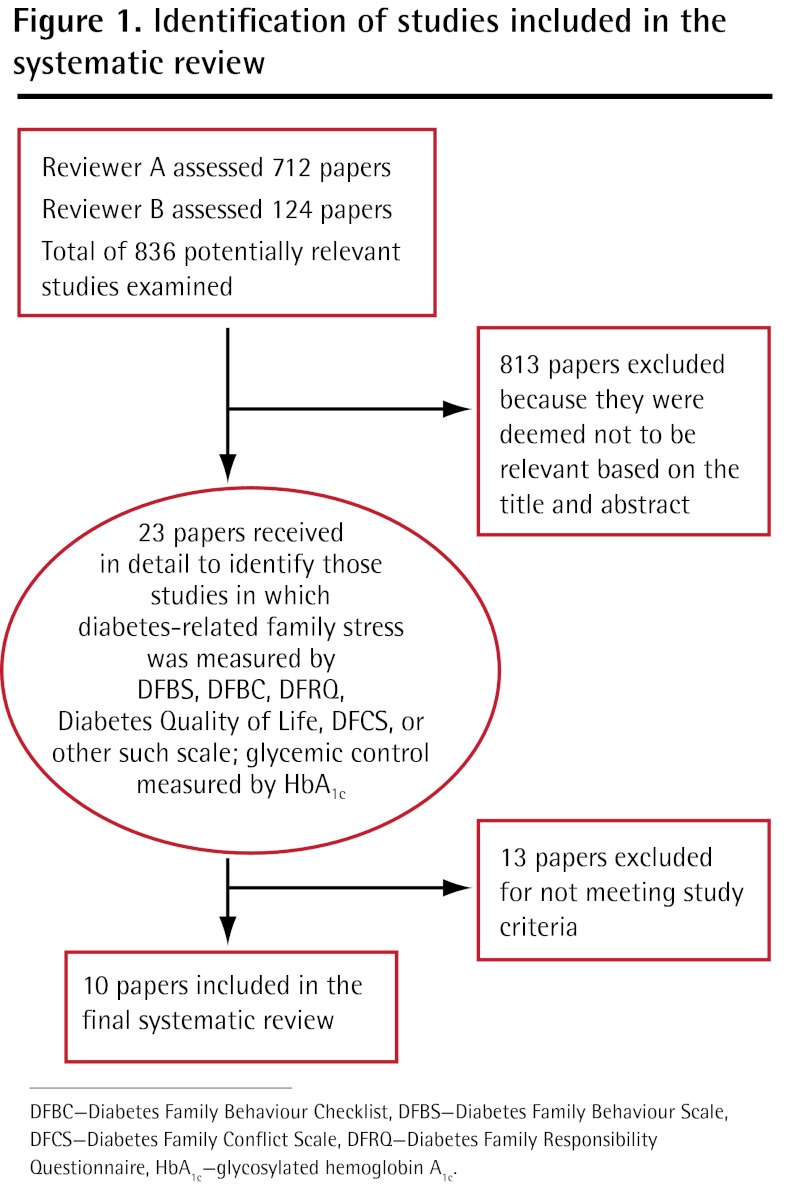
Studies of young patients with diabetes (younger than 18 years of age) and their families were included. Family stress–assessment instruments had to be used to evaluate diabetes-related family stress and conflict. Measurement of HbA1c had to be used to assess glycemic control. Studies that subsumed family stress assessment and HbA1c measurement through scaled questionnaires were included. Papers not reporting on the relationships between the specific variables under study (and examining instead topics such as type 2 pediatric diabetes, management strategies or glycemic control factors, or stressful life events around T1DM onset) or that examined stress resulting from family dysfunction and not T1DM-related stress were also excluded. No other exclusion criteria were used. Any relevant study indexed in the PubMed or Scopus databases was initially selected. The initial search retrieved 1478 papers. All titles and abstracts were independently assessed by 2 reviewers (E.T. and C.S.) to determine which articles should be included in the systematic review. All discrepancies with respect to relevance and disagreements about quality assessment were resolved through consensus. Ten of the 1478 papers met the eligibility criteria and were included in the systematic review: 9 longitudinal studies and 1 qualitative review (Figure 1). Data were extracted from each study and summarized in text and table format, and were then used to create a descriptive synthesis of the findings.
Figure 1.
Identification of studies included in the systematic review
Synthesis
In this study, we focused on diabetes-related family stress defined as stress induced in the family by the disease and its management (degree of responsibility regarding T1DM and the child's care, degree of family support, diabetes family conflict, degree of parental involvement, and degree of family consistency or cohesion). The papers retrieved were evaluated in terms of the way family diabetes-related stress (exposure) was measured and how that stress related to glycemic control (outcome). The studies included in this paper are outlined in Table 1.18-27
Table 1.
Summary of reviewed studies: All studies measured outcomes using measurement of glycosylated hemoglobin levels.
| STUDY | TYPE | PARTICIPANTS | MEASUREMENT TOOLS | MAIN RESULTS |
|---|---|---|---|---|
| Anderson,18 2004 | Qualitative review | NA | NA |
|
| Duke et al,19 2008 | Cross-sectional | 120 young people and their caregivers (low income) | DFBS* DFBC,† DSMP‡ (adherence to treatment measurement) |
|
| Laffel et al,20 2003 | Cohort | 104 children or adolescents and their families | Child quality of life,§ DFCS‖ |
|
| Lewin et al,21 2006 | Cohort | 109 children (aged 8-18 y) and 1 parent each | DFBS* DFBC,† DFRQ¶ |
|
| Viner et al,22 1996 | Cross-sectional | 43 children and adolescents and their mothers | FILE# |
|
| Jacobson et al,23 1994 | Cohort | 61 children and adolescents (aged 9-16 y) and their mothers | FES** |
|
| Grey et al,24 2011 | Cohort | 181 parents and their children | Issues in Coping With IDDM–Parent Scale,†† CES-D,‡‡ Diabetes Responsibility and Conflict Scale, Parents DQoL§§ |
|
| Williams et al,25 2009 | Cohort | 187 children and adolescents | DFCS,‖ CES-D,‡‡ STAI,‖‖ CDI¶¶ |
|
| Pereira et al,26 2008 | Cross-sectional | 157 children and adolescents (age 10-18 y) and their parents | DFBS,* FES,** DQoL§§ |
|
| Stallwood,27 2005 | Cohort | 73 caregivers and children | PAID,## ADS,*** CHIP,††† DSMP‡ |
|
ADS—Appraisal of Diabetes Scale, CDI—Children's Depression Inventory, CES-D—Center for Epidemiologic Studies Depression Scale, CHIP—Coping Health Inventory for Parents, DFBC—Diabetes Family Behaviour Checklist, DFBS—Diabetes Family Behaviour Scale, DFCS—Diabetes Family Conflict Scale, DFRQ—Diabetes Family Responsibility Questionnaire, DQoL—Diabetes Quality of Life scale, DSMP—Diabetes Self-Management Profile, FES—Family Environment Scale, FILE—Family Inventory of Life Events, HbA1c—glycosylated hemoglobin A1c, IDDM—insulin-dependent diabetes mellitus, NA—not applicable, PAID—Problem Areas in Diabetes scale, STAI—State-Trait Anxiety Inventory, T1DM—type 1 diabetes mellitus.
Subscales of warmth-care and guidance-control, and perceived family support.
Supportive behaviour related to the diabetic diet.
Use of structured interview that included 5 areas of diabetes management.
Measuring children's and parents' perceptions about the quality of life of children; 2 subscales of natural and psychosocial function used.
Section on the management of diabetes.
Family sharing of responsibilities in diabetes treatment.
Evaluating stressful family factors; was filled out by the main parental figure.
Subscales of cohesion, conflict, and expression, and scale of family organization.
Evaluating mothers' perceptions of coping with the stress of their children's diabetes.
Assessment of mothers' current depressive symptoms.
Assessment of parents' perceptions of the effects of diabetes.
Measurement of the transient state of arousal subjectively experienced as anxiety; the Trait scale was developed to assess the more enduring characteristic presence of this emotion.
Assessment of depression in children between the ages of 7 and 17 y.
Measurement of changes in psychosocial and emotional states associated with diabetes.
Assessment of the effects of family environment on glycemic control and psychosocial adaptation in adults with diabetes.
Assessment of parental coping patterns.
Results and discussion
A qualitative review by Anderson18 concluded that high levels of diabetes-related family conflict and authoritarian parental style were related to lower levels of treatment adherence and poorer glycemic control. Family warmth and authoritative parenting style with reasonable parental demands were found to be related to better glycemic control in adolescent patients with T1DM. The main conclusion was that the family conflict related to diabetes predicted glycemic control, as family conflict was negatively correlated with such control. No age-related differences in youth report of diabetes-related family stress were found. In this study,18 emotional expressiveness within the family appeared to be more important for the patient's glycemic control. Steady parental involvement was related to better glycemic control in children and adolescents. Moreover, family reactions were more disturbing and vexatious to the patients than to their parents. Parental involvement in treatment or care issues was not correlated with the level of diabetes-related stress. Parental involvement emanating from propagative parenting style was experienced as a supportive and not a stressful intervention.18
Duke et al19 studied family prognostic factors for glycemic control. A combination of special measurements of family behaviour explained 11.8% of the variability in glycemic control, after controlling for demographic variables. Patients who reported more judgmental parental behaviour around the management of their diabetes had higher HbA1c levels. In a 2003 study, Laffel et al20 examined diabetes-related family behaviour and family conflict. The main finding was that patient report of family conflict around diabetes was the only significant (P < .01) prognostic factor for quality of life. To summarize the 2 previous studies,19,20 glycemic control in children, adolescents, and young adults with T1DM seems to be correlated with the emotional expressiveness of the family, family support, family function, family stress factors related to the management of the disease, parental involvement in the treatment, family adjustment, and cohesion and conflict resolution.
Lewin et al21 investigated the prognostic value of family factors in the glycemic control of children with T1DM. They showed that children of single parents had significantly higher HbA1c levels than children of 2-parent families did (P < .05). These results confirmed some findings of another study on family cohesion conducted in 2001.28 Viner et al22 also studied the relationship between family stress and glycemic control. Data on demographic characteristics, the routine around diabetes, and family stress were recorded by the mothers of the patients, as mothers generally seemed to be the dominant parental figure in diabetes treatment. Family stress was significantly (P < .01) related to worse metabolic control not only for children but also for adolescents with T1DM.22 Unlike previous findings, in the study by Lewin et al,21 a weak relationship was demonstrated between a child's age and the duration of his or her diabetes, and no important effects of socioeconomic status were observed. Family function variables explained 34% of HbA1c variance.21 During early adolescence, poor glycemic control was strongly related to parents' judgmental and negative behaviour; but this relationship was not found in preadolescent patients.21
In a study by Jacobson et al,23 no correlation between family organization and glycemic control was found. Another study by Grey et al24 confirmed that decreased parental involvement in diabetes management led to improvement in metabolic control in the short term. The same study also showed that early withdrawal of parental involvement in diabetes management could cause aggravation of glycemic control. Conversely, extended parental authoritarian involvement could lead to increased parent-child conflict and thus to worse glycemic control. Williams et al25 suggested that families of children with diabetes felt constant apprehension about their children's glycemic control, which is positively correlated with diabetes-related family stress.
Pereira et al26 showed that glycemic control was related to family conflict in patients of higher socioeconomic class. Absence of family conflict was related to better quality of life. Also, boys had greater compliance with treatment than girls did. Treatment adherence and glycemic control were negatively correlated with disease duration. Similar results were found when socioeconomic class and glycemic control were tested. Higher socioeconomic class was the only predictive factor for glycemic control. Family conflict was correlated with poorer quality of life and vice versa. Both problematic youth behaviour and judgmental parental behaviour contributed to reduced compliance with treatment, which, in return, limited glycemic control. Jacobson et al23 studied the family environment in relation to glycemic control by conducting a 4-year study that comprised 61 children (age 9 to 16) and their mothers. Glycemic control deteriorated during the 4-year study. No significant relationship with family status or socioeconomic level and glycemic control was found. Family cohesion, conflict, and expression showed the strongest correlation to glycemic control.
The relationship between the family environment and glycemic control was also examined according to the sex of the child.23 Neither the child's sex nor the family expression interactions were significant predictors of the initial level or the monthly levels of difference in glycemic control.23 Grey et al24 reported that for preadolescents and adolescents, parental involvement in diabetes treatment declined in intensity, without any obvious worsening of glycemic control. In 2005, Stallwood27 corroborated the results of previous studies that had claimed that families of younger children suffered from higher diabetes-related stress, but the important finding in this particular study27 was that higher levels of caregiver stress were associated with lower HbA1c levels.
For critical appraisal reasons, the present study briefly presents data from older studies20,22,23 in order to highlight the differences and to point out the recent research data on the influence of family stress on the glycemic control of patients with T1DM.
Review evaluation
In summarizing the evidence, one has to keep in mind that we have reviewed studies published since 1990 that were indexed in the PubMed and Scopus databases. Consequently, there is the possibility that we have missed studies. The different designs of included studies, the heterogeneity in measuring of family function, the sampling methods (different demographic characteristics of subjects), and the heterogeneity in statistical elaboration methods, limit this study's generalizability and should also be taken into account.
In the study by Pereira et al,26 in which treatment compliance was evaluated through self-reporting questionnaires, family involvement in diabetes treatment seemed to have a favourable effect on glycemic control, resulting in improvement in family conflict. The differences between the findings in this study and those of the study by Laffel et al20 could be attributed to the sample's heterogeneity as well as the different study designs. There were also differences in the family stress evaluation tools.
In most studies, family conflict has been examined in relation to diabetes. Nevertheless, there were studies that included a more general evaluation of family adjustment and cohesion. The study by Viner et al22 had opposite findings relative to many previous studies that argued that paternal support did not influence stressful family relations in adolescents. This can be partly explained by the fact that measurement tools of family support were completed by adolescents' mothers only, in addition to the adolescents' perceptions of paternal support. In the Jacobson et al study,23 the differences that were observed—such as the fact that there was no correlation between family organization and glycemic control and that the sentimental family climate appeared to be the most important factor to the child's metabolic control level—might be caused by how HbA1c levels were evaluated, the study design, and the fact that only the mothers were involved in diabetes treatment.
In the Laffel et al study,20 family conflict demonstrated a strong relationship with quality of life and a less strong relationship with family cohesion and disease adjustment. The main limitation was the absence of investigation of both general and specific quality of life of the patients with diabetes, in a wider age range, with longer duration of the disease and from all socioeconomic levels. Finally, the Duke et al study19 was cross-sectional and had limitations in terms of causal inference. In spite of their inherent differences and heterogeneity, these studies showed that diabetes-related family stress affected patients' glycemic control.
Despite the limitations, most studies included agreed on depicting diabetes-related family conflict and authoritarian parenting style as leading causal components in deteriorating adherence to treatment, which aggravated glycemic control.
Conclusion
All the reviewed studies support the fact that dysfunctional family interactions, authoritarian parenting, and diabetes-related family stress are related to worse glycemic control. Stress leads to problematic child behaviour and deterioration of glycemic control23; therefore, diabetes-related family conflict is negatively correlated with glycemic control, showing a reciprocal relationship between family stress and diabetes control. Interventions in dysfunctional family interactions might lead to improvements in family conflict and therefore to better glycemic control, even though a few studies suggest otherwise.29 This review confirms the dominant principle that specific factors of family function influence glycemic control in young patients with T1DM.
Family involvement is an important predictive factor for glycemic control. Participation of the entire family in educational programs on disease management and psychotherapeutic programs for stress management would likely help young patients deal with the stress of treatment and achieve desired glycemic control, as parents' behaviour is a factor for creating independent and responsible patients who can take care of their diabetes. Consequently, physicians and medical educators must be alert for any sign or symptom of stress or depression, not only in patients but also in their family members, throughout medical visits. Physicians could also integrate a self-efficacy evaluation test after each teaching module for those families participating in educational programs to determine if further teaching is needed before moving on, which would highlight areas in which parents and their children need supplementary support.30 The goal of the interdisciplinary team that provides care to the child or adolescent and the family should be the empowerment of the patient and his or her family for acceptance of the condition and education on the skills for successful diabetes management.
Finally, in order to better plan supportive interventions in this area, future systematic reviewers should include studies that examine the operation of particular stressors in families of young patients with diabetes and the interaction effects between the family diabetes variables, adherence behaviour, and metabolic control.
KEY POINTS
The presence of a chronic pediatric condition is a recognized source of increased distress among family members. This systematic review investigated the influence of family function, such as perceived family support (care and warmth), family stressors, the level of parental involvement in the care of diabetes (guidance and control, judgmental parental behaviour), and family organization (cohesion, conflict, expression) on the glycemic control of young patients with type 1 diabetes. The reviewed studies suggest that dysfunctional family interactions, authoritarian parenting, and diabetesrelated family stress are related to worse glycemic control. Interventions in dysfunctional family interactions might lead to improvements in family conflict and, therefore, better glycemic control, although a few studies did suggest otherwise.
Footnotes
This article is eligible for Mainpro-M1 credits. To earn credits, go to www.cfp.ca and click on the Mainpro link
Contributors: Ms Tsiouli wrote part of the manuscript, found the references, and reviewed the papers included in the review. Dr Alexopoulos designed the study, corrected the manuscript, and prepared the manuscript for submission. Dr Stefanaki wrote part of the manuscript, translated in French, found the references, reviewed the papers included in the review, and prepared the manuscript for submission. Prof Darviri corrected the manuscript and contributed to the editing. Prof Chrousos corrected the manuscript and contributed to the editing. All authors approved the final manuscript for submission.
Competing interests: None declared
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de février 2013 à la page e75.
This article has been peer reviewed. Can Fam Physician 2013;59:143-9
References
- 1.Schmid J, Ludwig B, Schally AV, Steffen A, Ziegler CG, Block NL, et al. Modulation of pancreatic islets-stress axis by hypothalamic releasing hormones and 11beta-hydroxysteroid dehydrogenase. Proc Natl Acad Sci U S A 2011;108(33):13722-7 Epub 2001 Aug 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature 2001;414(6865):782-7 [DOI] [PubMed] [Google Scholar]
- 3.Rewers A, Chase HP, Mackenzie T, Walravens P, Roback M, Rewers M, et al. Predictors of acute complications in children with type 1 diabetes. JAMA 2002;287(19):2511-8 [DOI] [PubMed] [Google Scholar]
- 4.EURODIAB ACE Study Group Variation and trends in incidence of childhood diabetes in Europe. Lancet 2000;355(9207):873-6 Erratum in: Lancet 2000;356(9242):1690. [PubMed] [Google Scholar]
- 5.Green A, Patterson CC, EURODIAB TIGER Study Group Europe and Diabetes. Trends in the incidence of childhood-onset diabetes in Europe 1989-1998. Diabetologia 2001;44(Suppl 3):B3-8 [DOI] [PubMed] [Google Scholar]
- 6.Delamater AM. Psychological care of children and adolescents with diabetes. Pediatr Diabetes 2009;10(Suppl 12):175-84 [DOI] [PubMed] [Google Scholar]
- 7.Wasserman LI, Trifonova EA. Diabetes mellitus as a model of psychosomatic and somatopsychic interrelationships. Span J Psychol 2006;9(1):75-85 [DOI] [PubMed] [Google Scholar]
- 8.Onkamo P, Väänänen S, Karvonen M, Tuomilehto J. Worldwide increase in incidence of type I diabetes—the analysis of the data on published incidence trends. Diabetologia 1999;42(12):1395-403 Erratum in: Diabetologia 2000;43(5):685. [DOI] [PubMed] [Google Scholar]
- 9.Hall V, Thomsen RW, Henriksen O, Lohse N. Diabetes in Sub Saharan Africa 1999-2011: epidemiology and public health implications. A systematic review. BMC Public Health 2011;11(1):564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mellin AE, Neumark-Sztainer D, Patterson JM. Parenting adolescent girls with type 1 diabetes: parents' perspectives. J Pediatr Psychol 2004;29(3):221-30 [DOI] [PubMed] [Google Scholar]
- 11.Hauser ST, Jacobson AM, Lavori P, Wolfsdorf JI, Herskowitz RD, Milley JE, et al. Adherence among children and adolescents with insulin-dependent diabetes mellitus over a four-year longitudinal follow-up. II. Immediate and long-term linkages with the family milieu. J Pediatr Psychol 1990;15(4):527-42 [DOI] [PubMed] [Google Scholar]
- 12.Anderson BJ, Holmbeck G, Iannotti RJ, McKay SV, Lochrie A, Volkening LK, et al. Dyadic measures of the parent-child relationship during the transition to adolescence and glycemic control in children with type 1 diabetes. Fam Syst Health 2009;27(2):141-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen LL, La Greca AM, Blount RL, Kazak AE, Holmbeck GN, Lemanek KL. Introduction to special issue: evidence-based assessment in pediatric psychology. J Pediatr Psychol 2008;33(9):911-5 Epub 2006 May 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herzer M, Godiwala N, Hommel KA, Driscoll K, Mitchell M, Crosby LE, et al. Family functioning in the context of pediatric chronic conditions. J Dev Behav Pediatr 2010;31(1):26-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller-Johnson S, Emery RE, Marvin RS, Clarke W, Lovinger R, Martin M. Parent-child relationships and the management of insulin-dependent diabetes mellitus. J Consult Clin Psychol 1994;62(3):603-10 [DOI] [PubMed] [Google Scholar]
- 16.Hare MJ, Shaw JE, Zimmet PZ. Current controversies in the use of haemoglobin A1c. J Intern Med 2012;271(3):227-36 [DOI] [PubMed] [Google Scholar]
- 17.Rewers M, Pihoker C, Donaghue K, Hanas R, Swift P, Klingensmith GJ. Assessment and monitoring of glycemic control in children and adolescents with diabetes. Pediatr Diabetes 2009;10(Suppl 12):71-81 [DOI] [PubMed] [Google Scholar]
- 18.Anderson BJ. Family conflict and diabetes management in youth: clinical lessons from child development and diabetes research. Diabetes Spectrum 2004;17(1):22-6 [Google Scholar]
- 19.Duke DC, Geffken GR, Lewin AB, Williams LB, Storch EA, Silverstein J. Glycemic control in youth with type I diabetes: family predictors and mediators. J Pediatr Psychol 2008;33(7):719-27 [DOI] [PubMed] [Google Scholar]
- 20.Laffel LM, Connell A, Vangsness L, Goebel-Fabbri A, Mansfeld A, Anderson B. General quality of life in youth with type I diabetes: relationship to patient management and diabetes specific family conflict. Diabetes Care 2003;26(11):3067-73 [DOI] [PubMed] [Google Scholar]
- 21.Lewin AB, Heidgerken AD, Geffken GR, Williams LB, Storch EA, Gelfand KM, et al. The relation between family factors and metabolic control: the role of diabetes adherence. J Pediatr Psychol 2006;31(2):174-83 Epub 2005 Mar 3. [DOI] [PubMed] [Google Scholar]
- 22.Viner R, McGrath M, Trudinger P. Family stress and metabolic control in diabetes. Arch Dis Child 1996;74(5):418-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jacobson AM, Hauser ST, Lavori P, Willett JB, Cole ChF, Wolfsdorf JI, et al. Family environment and glycemic control: a four-year prospective study of children and adolescents with insulin-dependent diabetes mellitus. Psychosom Med 1994;56(5):401-9 [DOI] [PubMed] [Google Scholar]
- 24.Grey M, Jaser SS, Whittemore R, Jeon S, Lindemann E. Coping skills training for parents of children with type I diabetes: 12-month outcomes. Nurs Res 2011;60(3):173-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams LB, Laffel LM, Hood KK. Education and psychological aspects diabetes-specific family conflict and psychological distress in paediatric type 1 diabetes. Diabet Med 2009;26(9):908-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pereira MG, Berg-Cross L, Almeida P, Machado C. Impact of family environment and support on adherence, metabolic control and quality of life in adolescents with diabetes. Int J Behav Med 2008;15(3):187-93 [DOI] [PubMed] [Google Scholar]
- 27.Stallwood L. Influence of caregiver stress and coping on glycemic control of young children with diabetes. J Pediatr Health Care 2005;19(5):293-300 [DOI] [PubMed] [Google Scholar]
- 28.Thompson SJ, Auslander WF, White NH. Comparison of single-mother and two-parent families on metabolic control of children with diabetes. Diabetes Care 2001;24(2):234-8 [DOI] [PubMed] [Google Scholar]
- 29.Jaser SS, Grey M. A pilot study of observed parenting and adjustment in adolescents with type 1 diabetes and their mothers. J Pediatr Psychol 2010;35(7):738-47 Epub 2009 Nov 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nicholson TR, Taylor JP, Gosden C, Trigwell P, Ismail K. National guidelines for psychological care in diabetes: how mindful have we been? Diabet Med 2009;26(4):447-50 [DOI] [PubMed] [Google Scholar]