Abstract
Objective
To determine the types of chronic disease management (CDM) programs offered for patients with diabetes in Alberta's primary care networks (PCNs).
Design
A survey was administered to PCNs to determine the types of CDM programs offered for patients with diabetes; CDM programs were organized into categories by their resource intensity and effectiveness. Results of the survey were reported using frequencies and percentages.
Setting
Alberta has recently created PCNs—groups of family physicians who receive additional funds to enable them to support activities that fall outside the typical physician-based fee-for-service model, but which address specified objectives including CDM. It is currently unknown what additional programs are being provided through the PCN supplemental funding.
Participants
A survey was administered to the individual responsible for CDM in each PCN. This included executive directors, chronic disease managers, and CDM nurses.
Main outcome measures
We determined the CDM strategies used in each PCN to care for patients with diabetes, whether they were available to all patients, and whether the services were provided exclusively by the PCN or in conjunction with other agencies.
Results
There was considerable variation across PCNs with respect to the CDM programs offered for people with diabetes. Nearly all PCNs used multidisciplinary teams (which could include nurses, dietitians, and pharmacists) and patient education. Fewer than half of the PCNs permitted personnel other than the primary physician to write or alter prescriptions for medications.
Conclusion
Alberta's PCNs have successfully established many different types of CDM programs. Multidisciplinary care teams, which are among the most effective CDM strategies, are currently being used by most of Alberta's PCNs.
Résumé
Objectif
Déterminer les types de programmes pour le traitement des maladies chroniques (TMC) qui sont offerts aux diabétiques fréquentant les réseaux de soins primaires (RSP) de l'Alberta.
Type d'étude
On a demandé aux RSP de répondre à une enquête afin de déterminer les types de programmes de TMC qu'ils offrent aux diabétiques; ces programmes ont été répartis en catégories en fonction de l'intensité et de l'efficacité de leur personnel. Les résultats de l'enquête ont été rapportés sous forme de fréquences et de pourcentages.
Contexte
L'Alberta a récemment créé des RSP–des groupes de médecins de famille qui reçoivent des sommes additionnelles pour certaines activités qui n'entrent pas dans le cadre habituel de la rémunération à l'acte, mais qui visent plutôt des objectifs déterminés, comme les TCM. On ignore pour l'instant quels autres programmes sont offerts grâce aux nouvelles subventions que reçoivent les RSP.
Participants
Ce sont les responsables du TMC dans chaque RSP qui ont répondu à l'enquête : directeurs exécutifs, responsables des maladies chroniques ou infirmiers fournissant ce genre de traitement.
Principaux paramètres à l'étude
Identification des stratégies de TMC appliquées aux diabétiques dans chaque RSP, qu'elles soient disponibles à tous les patients et que ces services soient dispensés uniquement par le RSP ou conjointement avec d'autres agences.
Résultats
Il y avait d'importantes variations entre les RSP pour ce qui est des programmes de TMC offerts aux diabétiques. Presque tous les réseaux utilisaient des équipes multidisciplinaires (pouvant inclure infirmiers, diététistes et pharmaciens) et faisaient de l'éducation des patients. Moins de la moitié des RSP permettaient à des membres du personnel autres que des médecins de famille de faire ou de modifier des prescriptions médicamenteuses.
Conclusion
Les RSP de l'Alberta ont réussi à instaurer plusieurs types de programmes de TDM. À l'heure actuelle, la plupart de des RSP utilisent des équipes de soins multidisciplinaires, une stratégie qui compte parmi les plus efficaces.
Diabetes affects 2.25 million Canadians, and managing diabetes and its complications costs more than $9 billion annually.1 Safe, effective, and cost-effective interventions for diabetes are available, including antihypertensive medications, cholesterol-lowering treatment, and glycemic control.2-9 To optimize the care of patients with diabetes, comprehensive care, including behaviour modification and pharmacologic therapy, has been shown to be highly effective.10 However, such care is difficult to deliver and usually requires the use of multidisciplinary chronic disease management (CDM) programs.11,12
Chronic disease management programs vary in design and effectiveness. In 2006, a systematic review of randomized trials evaluated the effectiveness of CDM care for diabetes, categorizing programs into 11 distinct strategies.13 The authors noted that most CDM programs improved glycosylated hemoglobin A1c (HbA1c) levels for participants, although to varying degrees.13 These different programs also vary in resource intensity, with some requiring the modification of electronic medical records (EMRs), and others necessitating the hiring of specific staff.
Implementing CDM programs is challenging, as additional resources and changes to practice style are often required to ensure that all patients have adequate access. Primary care reform (a potential means of improving access) has become topical across Canada, although it is being proposed and accomplished in varying ways.14 In most provinces, primary care reform is aimed at increasing interdisciplinary care, providing extended hours for care delivery, and placing increased emphasis on prevention and patient education.15
In Alberta, primary care reform has taken the form of primary care networks (PCNs), which aim to improve access to and coordination of care for patients.16 A PCN consists of primary care physicians working with other health care providers, including nurses, dietitians, and pharmacists, to provide care to patients in a specific catchment area. While each network provides care to patients with and without chronic diseases (and has the flexibility to focus on any aspect of care that will benefit patients according to local need), CDM for patients with diabetes has been identified as a priority by most PCNs.16 Additional funding ($50 per enrolled patient per year) is provided to the PCNs to support activities that are not funded by the typical physician-based fee-for-service model but that address specified objectives such as CDM.17 These funds may be used to hire nurses, to enable allied health care professionals to work to their full scope of practice, or for supporting other initiatives, including CDM programs.
Given differences in local priorities, personnel available, and historical patterns of care, it has been anecdotally noted that PCNs have established different types of CDM programs. Given the differences in effectiveness and costs between the various CDM programs, we sought to determine which types of CDM programs have been adopted to manage diabetes by Alberta's PCNs and whether these choices are consistent with current evidence.
METHODS
In August 2010, we conducted a telephone survey of all Alberta PCNs to determine details of the CDM strategies for diabetes used in each PCN. The study was approved by the University of Calgary's Conjoint Health Research Ethics Board.
The PCNs studied
In 2003, the Alberta Primary Care Initiative was formed with the goal of creating PCNs to achieve primary care reform. The first PCNs opened in 2005. As of October 2010, there were 38 PCNs operating in Alberta, with another 2 recently approved and 3 pending approval.17 We assumed that 18 months would be required for a PCN to implement its CDM programs and we therefore limited our sample to the 30 PCNs that were established as of January 2009.
Method of survey
Our telephone survey was aimed at PCN employees who were familiar with all the CDM programs offered at the PCN. We identified these individuals through PCN websites or by calling PCN administrative staff. The position of the PCN contact person varied greatly and included executive directors, medical directors, CDM nurses, and coordinators. Responses to the survey were collected via telephone following distribution of the survey to contacts by e-mail.
Categorization of CDM programs for diabetes
Several different CDM program strategies have been shown to improve intermediate health indicators (eg, HbA1c levels, use of cardioprotective medications) in patients with diabetes.18,19 Because CDM programs for diabetes are heterogeneous and do not conform to uniform guidelines, we classified them into categories as proposed by Shojania et al.13 This scheme divides CDM strategies into 11 categories: clinician reminders; patient reminders; facilitated relay of clinical data to providers; audit and feedback; electronic patient registries; clinician education; patient education; promotion of self-management; team changes; case management; and continuous quality improvement (Table 1).13
Table 1. Types of CDM strategies for diabetes.
| STRATEGY* | DEFINITION | EXAMPLES |
|---|---|---|
| Electronic medical record | Electronic system for tracking patient appointments or for tracking specific patients with diabetes | NA |
| Patient reminders | Telephone calls or postcards to patients to remind them of upcoming appointments or other aspects of diabetes management | Reminders of annual ophthalmology appointments |
| Clinician reminders | Prompts to health care providers to remind them of patient-specific diabetes management | Flag for patients who have not had recent HbA1c measurements recorded |
| Audit and feedback | A summary of a physician's clinical performance is sent to him or her for self-evaluation | Each month the physician receives the average of the most recent HbA1c values of each patient with diabetes |
| Facilitated relay of patient data | Clinical information from patients that is transmitted to the physician via some other route than traditional medical interactions | Patient home glucometer readings are uploaded and e-mailed to the case manager on a weekly basis |
| Clinician education | Increasing physicians awareness of current clinical practice guidelines and evidence-based recommendations | Conferences, workshops, educational outreach visits from PCN staff |
| Patient education | Increasing patient understanding of disease pathophysiology and effective methods of secondary prevention | One-on-one counseling with nursing staff, group diabetes classes |
| Promotion of self-management | Providing resources for patients to succeed in self-management | Glucometers, meal-tracking charts |
| Team changes | Addition of 1 or more members to the health care team | Adding CDM nurses, dietitians, or pharmacists to the patient care team |
| Case management | A team member other than the primary care physician assumes primary responsibility for coordinating care of patients with diabetes | Registered nurses track home glucose readings, send patients for bloodwork, and ensure that patients are seeing specialists appropriately |
CDM–chronic disease management, HbA1c–glycosylated hemoglobin A1c, NA–not applicable, PCN–primary care network.
Strategy categories are taken from Shojania et al.13
The CDM strategies for diabetes were also grouped based on their resource intensity (Table 2). The strategies requiring the fewest resources are those that can be facilitated through existing EMR systems (provided the practice is already using an EMR). The next most resource-intensive strategies are those related to educational interventions, which might require part-time staff members to run educational sessions. The most resource-intensive strategies are those that require dedicated full-time staff members such as case managers or members of multidisciplinary teams (Table 2).
Table 2. Resource intensities of various CDM strategies.
| Resource intensity⇓ | EMR-RELATED INTERVENTIONS | EDUCATION-RELATED INTERVENTIONS | PERSONNEL-BASED INTERVENTIONS |
|
| |||
| EMR | Clinician education | Team changes | |
| Patient reminders | Patient education | Case management | |
| Clinician reminders | Promotion of self-management | ||
| Audit and feedback | |||
| Facilitated relay of patient data | |||
| Resource intensity | ⇒ | ||
CDM–chronic disease management, EMR–electronic medical record.
Analysis
Results of the survey were presented using frequencies, as the goal of this study was to gain an understanding of the programs offered by PCNs. Microsoft Access was used to manage the data and produce descriptive charts and tables.
RESULTS
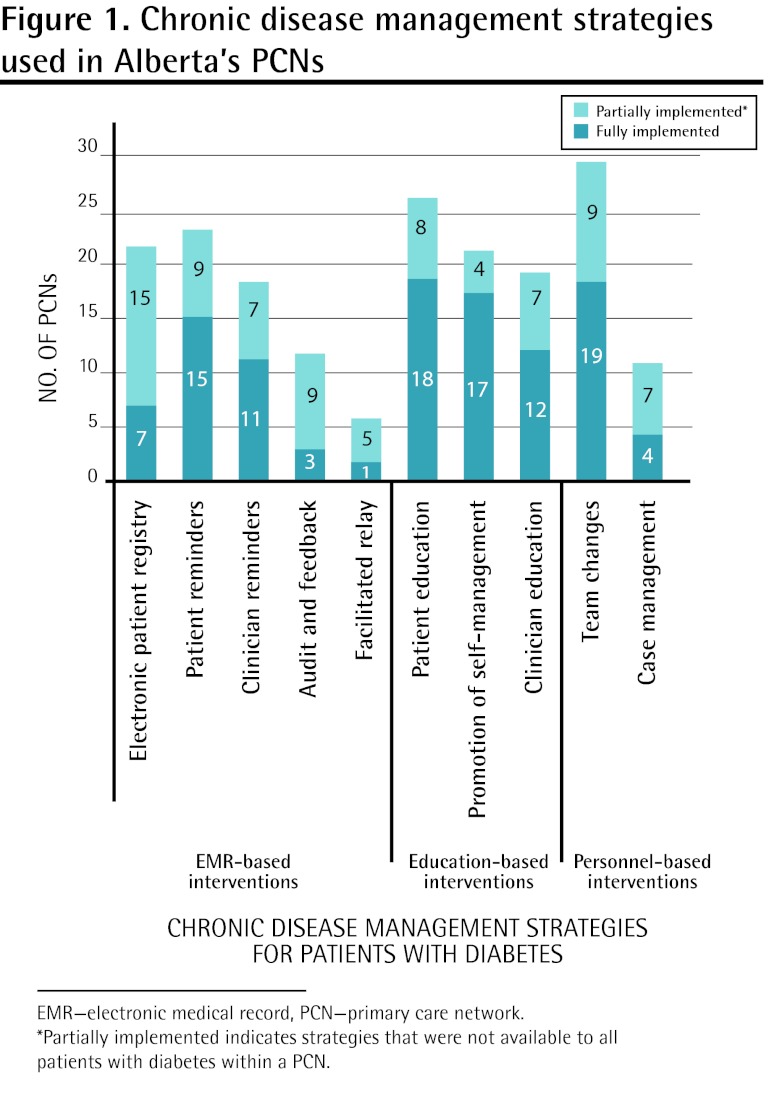
The response rate to the survey was 97% (29 of 30), with only 1 PCN abstaining from participation. Of these 29 PCNs, 28 offered a variety of CDM programs for diabetes. In many PCNs, CDM programs were offered by some clinics in the PCN, rather than by all clinics, or programs were geographically based and therefore not necessarily accessible to all patients in the PCN (Figure 1).
Figure 1. Chronic disease management strategies used in Alberta's PCNs.
The 2 most commonly used strategies were team changes (28 of 29 offered programs to at least some patients in the PCN) and patient education (26 of 29 offered programs to at least some patients in the PCN). Multiple strategies were available to some patients in at least half of the PCNs surveyed. Fewer than half of the PCNs (12 of 28) had programs in which team members other than the primary physician had the authority to write or alter prescriptions for medications.
The PCNs were as likely to offer CDM programs that required high resource intensity as those that required low resource intensity (Figure 1). For instance, team changes are among the most resource-intensive strategies but are also among the most widely used. Alternatively, the strategies that can be facilitated by an effective electronic patient registry (eg, audit and feedback) might be among the less resource-intensive strategies (for clinics with a functioning electronic patient registry), but these were among the least widely used strategies in Alberta's PCNs.
DISCUSSION
Given that most PCNs care for more than 60 000 patients, they receive a substantial budget to provide enhanced services. The PCNs face difficult decisions regarding how to best use these additional resources. Despite the many competing priorities in primary care, we found that most of Alberta's PCNs have identified CDM for diabetes as a priority and offer at least some form of CDM program for diabetes. Many PCNs employ several CDM strategies concurrently in the management of patients with diabetes. This makes sense given that some strategies, such as patient education, might be more useful for newly diagnosed patients, while others might have a larger role for patients with severe disease and diabetic complications (eg, case management).
Not all CDM strategies are equally effective for improving care. Two recent systematic reviews have compared the effectiveness of the various CDM strategies,13,20 highlighting that team changes are among the most effective strategies. An additional review by Shojania et al13 included 66 studies (50 of which were randomized trials), and concluded that the 2 interventions associated with the largest changes in HbA1c levels were team changes and case management. They also noted 4 other strategies that resulted in statistically significant differences in HbA1c levels: patient education, patient reminders, electronic patient registries, and clinician education. A separate systematic review that focused on the efficacy of case management in diabetes concluded that there was strong evidence supporting the use of this strategy to reduce HbA1c levels and decrease complications of diabetes.21 Finally, a systematic review done by Zwar et al compared CDM strategies based on the classification of strategies defined by the chronic care model.20 Similar to Shojania et al, this study found that changes in delivery system design had the largest effect on HbA1c levels. This category includes team changes, case management, electronic patient registries, and patient reminders.
The results of our study demonstrate that Alberta PCNs are employing several of the strategies that have been proven to be most effective. Nearly all PCNs use team changes (including adding nurses, dietitians, or pharmacists) to supplement standard physician care. Furthermore, the strategies shown to be most effective by Zwar et al20 were the most commonly used strategies in the PCNs surveyed in our study.
Although team changes had been widely used across Alberta PCNs, fewer than half (12 of 28) had adopted one of the potentially most important components of the multidisciplinary team—namely, allowing team members other than the primary physician to alter medications autonomously. This strategy was shown to be the most effective in case management programs,13 yielding an absolute reduction in HbA1c levels of 0.96%, compared with 0.41% for case management programs without this feature. It is possible that the resources required to hire allied health professionals with prescribing authority are prohibitive for some PCNs. In Alberta, only certain pharmacists have the authority to initiate and modify prescriptions.22 Nurse practitioners and advance practice nurses have similar prescribing authority, but standard registered nurses currently do not have this capability.23,24 It is also possible that the reluctance relates to physician views on allied health prescribing. According to a Canadian Medical Association survey reported in 2007, physicians recognize the value of collaborative care, with 93% of respondents supporting collaborative models throughout the system.25 However, they also identified a number of barriers to the successful implementation of collaborative care:
Where non-physicians have been provided with an opportunity to undertake activities related to patient care typically unique to the practice of medicine (e.g. ordering tests), they must not do so independently but undertake these activities within the context of the team and in a manner acceptable to the clinical leader.25
To enhance the uptake of proven CDM methods in Alberta primary care networks, further study of existing barriers is warranted. Research should help to inform the ongoing discussion on extending the effectiveness of care teams in a context acceptable to participating physicians. It will also be important to track the effects of PCNs on intermediate markers of high-quality diabetes care, including HbA1c levels and the use of medications associated with high-quality care.
Limitations
As in all studies that depend on the classification of quality improvement strategies, not all CDM strategies fit exactly within a prespecified category. We used the definitions provided by Shojania et al,13 and categorized CDM activities into existing categories as well as possible. Furthermore, PCNs are organized differently across Alberta—some use a centralized model in which all patient services are provided in a central location, whereas others prefer to sponsor allied health care professionals to work in various clinics throughout their jurisdiction. For centralized PCNs, data collection was straightforward; however, for PCNs where each clinic was more autonomous, the collection of data on a PCN-wide scale was difficult. In these situations, we noted that CDM services were often only available for a portion of PCN members.
Conclusion
We found that PCNs in Alberta varied in the types of CDM programs that they offered for patients with diabetes. While team changes have been shown to be effective, and the most commonly used strategy in Alberta, the effectiveness of such changes might be increased by having someone other than the primary care physician able to prescribe and alter medications. Given limited resources within PCNs, future expansion of CDM programs in existing and new PCNs should consider differential effectiveness and resource intensity in addition to ease of implementation.
Acknowledgment
This research was funded by Alberta Innovates-Health Solutions (formerly Alberta Heritage Foundation for Medical Research).
EDITOR'S KEY POINTS
In Alberta, primary care reform has taken the form of primary care networks (PCNs), which aim to improve access to and coordination of care for patients. A PCN consists of primary care physicians working with other health care providers, including nurses, dietitians, and pharmacists, to provide care to patients in a specific catchment area.
Given differences in local priorities, personnel available, and historical patterns of care, it has been anecdotally noted that PCNs have established different types of chronic disease management (CDM) programs. This research sought to determine which types of CDM programs have been adopted to manage diabetes by Alberta's PCNs and whether these choices were consistent with current evidence.
The results show that most of Alberta's PCNs have identified CDM for diabetes as a priority and offer at least some form of a CDM program for diabetes.
POINTS DE REPÈRE DU RÉDACTEUR
En Alberta, la réforme des soins primaires a pris la forme de réseaux de soins primaires (RSP), lesquels cherchent à améliorer l'accès et la coordination des soins aux patients. Un RSP est formé d'un médecin de soins primaires qui collabore avec d'autres membres du personnel soignant, incluant des infirmiers, des diététistes et des pharmaciens, dans le but de fournir aux patients des soins dans un domaine médical spécifique.
En raison de différences dans les priorités locales , et selon le personnel disponible et le modèle traditionnel des soins, il a été occasionnellement noté que les RSP ont instauré différents types de programmes pour le traitement des maladies chroniques (TMC). Cette étude voulait déterminer quels types de programmes de TMC ont été adoptés pour les diabétiques dans les RSP albertains et vérifier si ces choix étaient conformes aux données probantes disponibles.
Les résultats montrent que la plupart des RSP albertains ont déclaré que le TMC du diabète était une priorité et ont offert au moins une forme de programme de TMC pour les diabétiques.
Footnotes
Contributors: Drs Campbell and Manns made substantial contributions to study conception and design, and to drafting the article and critical revision. Dr Campbell administered the surveys and collected the data. Drs Campbell, Manns, and Hemmelgarn were involved in study design, data analysis, and interpretation of data. Drs Hemmelgarn, Tonelli, McBrien, Sargious, and Lewanczuk had input into study design and provided critical revisions to the manuscript. Dr Manns accepts full responsibility for the work and the conduct of the study. He had access to the data and controlled the decision to publish.
Competing interests: None declared
This article has been peer reviewed. Can Fam Physician 2013;59:e86-92
References
- 1.Simpson SH, Corabian P, Jacobs P, Johnson J. The cost of major comorbidity in people with diabetes mellitus. CMAJ 2003;168(13):1661-7 [PMC free article] [PubMed] [Google Scholar]
- 2.United Kingdom Prospective Diabetes Study (UKPDS) 13: relative efficacy of randomly allocated diet, sulphonylurea, insulin, or metformin in patients with newly diagnosed non-insulin dependent diabetes followed for three years. BMJ 1995;310(6972):83-8 [PMC free article] [PubMed] [Google Scholar]
- 3.Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ 1998;317(7160):703-13 Erratum in: BMJ 1999;318(7175):29. [PMC free article] [PubMed] [Google Scholar]
- 4.Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001;345(12):861-9 [DOI] [PubMed] [Google Scholar]
- 5.Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet 2004;364(9435):685-96 [DOI] [PubMed] [Google Scholar]
- 6.De Zeeuw D, Lewis EJ, Remuzzi G, Brenner BM, Cooper ME. Renoprotective effects of renin-angiotensin-system inhibitors. Lancet 2006;367(9514):899-900 [DOI] [PubMed] [Google Scholar]
- 7.Eijkelkamp WB, Zhang Z, Brenner BM, Cooper ME, Devereux RB, Dahlof B, et al. Renal function and risk for cardiovascular events in type 2 diabetic patients with hypertension: the RENAAL and LIFE studies. J Hypertens 2007;25(4):871-6 [DOI] [PubMed] [Google Scholar]
- 8.Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet 2005;366(9500):1849-61 Erratum in: Lancet 2006;368(9545):1415. [DOI] [PubMed] [Google Scholar]
- 9.Psaty BM, Lumley T, Furberg CD, Schellenbaum G, Pahor M, Alderman MH, et al. Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA 2003;289(19):2534-44 [DOI] [PubMed] [Google Scholar]
- 10.Gaede P, Vedel P, Larsen N, Jensen GV, Parving H, Pedersen O. Multifactorial interventions and cardiovascular disease in patients with type 2 diabetes. N Engl J Med 2003;348(5):383-93 [DOI] [PubMed] [Google Scholar]
- 11.Gruman J, VonKorff M, Reynolds J, Wagner EH. Organizing health care for people with seizures and epilepsy. J Ambul Care Manage 1998;21(2):1-13 [DOI] [PubMed] [Google Scholar]
- 12.Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med 1997;127(12):1097-102 [DOI] [PubMed] [Google Scholar]
- 13.Shojania KG, Ranji SR, McDonald KM, Grimshaw JM, Sundaram V, Rushakoff RJ, et al. Effects of quality improvement strategies for type 2 diabetes on glycemic control. JAMA 2006;296(4):427-40 [DOI] [PubMed] [Google Scholar]
- 14.Primary care reform—a national overview. In: Canadian Medical Association. Primary care reform Ottawa, ON: Canadian Medical Association; 2005. p. 22-31 [Google Scholar]
- 15.Shortt S. Primary care reform: change in search of evidence? In: Canadian Medical Association. Primary care reform Ottawa, ON: Canadian Medical Association; 2005. p. 15-17 [Google Scholar]
- 16.Primary Care Initiative [website] Supporting primary care networks. Edmonton, AB: Primary Care Initiative; 2012. Available from: www.albertapci.ca/Pages/default.aspx Accessed 2009 Dec 30 [Google Scholar]
- 17.Primary Care Initiative [website] About PCI. Edmonton, AB: Primary Care Initiative; 2010. Available from: www.albertapci.ca/AboutPCI/Pages/default.aspx Accessed 2010 Sep 8 [Google Scholar]
- 18.Knight K, Badamgarav E, Henning JM, Hasselblad V, Gano AD, Jr, Ofman JJ, et al. A systematic review of diabetes disease management programs. Am J Manag Care 2005;11(4):242-50 [PubMed] [Google Scholar]
- 19.Rubin RJ, Dietrich KA, Hawk AD. Clinical and economic impact of implementing a comprehensive diabetes management program in managed care. J Clin Endocrinol Metab 1998;83(8):2635-42 [DOI] [PubMed] [Google Scholar]
- 20.Zwar N, Harris M, Griffiths R, Roland M, Dennis S, Davies G, et al. A systematic review of chronic disease management. Canberra, Australia: Australian Primary Health Care Research Initiative; 2006 [Google Scholar]
- 21.Norris SL, Nichols PJ, Caspersen CJ, Glasgow RE, Engelgau MM, Jack L, et al. The effectiveness of disease and case management for people with diabetes. Am J Prev Med 2002;22(4 Suppl):15-38 [DOI] [PubMed] [Google Scholar]
- 22.CTV News [website] Not many pharmacists prescribing medication. Calgary, AB: CTV News; 2010. Available from: http://calgary.ctvnews.ca/not-many-pharmacists-prescribing-medication-1.575402 Accessed 2013 Jan 20 [Google Scholar]
- 23.Forchuk C, Kohr R. Prescriptive authority for nurses: the Canadian perspective. Perspect Psychiatr Care 2009;45(1):3-8 [DOI] [PubMed] [Google Scholar]
- 24.College and Association of Registered Nurses of Alberta Prescribing and distributing guidelines for nurse practitioners. Edmonton, AB: College and Association of Registered Nurses of Alberta; 2004 [Google Scholar]
- 25.Canadian Medical Association Putting patients first: patient-centered collaborative care. Ottawa, ON: Canadian Medical Association; 2007 [Google Scholar]