Abstract
Objective
To measure adherence and to identify factors associated with adherence to antihypertensive medications in family practice patients with diabetes mellitus (DM) and hypertension.
Design
A cross-sectional study using a mailed patient self-report survey and clinical data.
Setting
Twenty-seven family physician and nurse practitioner clinics from Nova Scotia, New Brunswick, and Prince Edward Island (the Maritime Family Practice Research Network).
Participants
A total of 527 patients with type 2 DM and hypertension who had had their blood pressure measured with the BpTRU (an automated oscillometric instrument) at family practice clinic visits within the previous 6 months.
Main outcome measures
Level of adherence to antihypertension medications as measured by patients' self-report on the Morisky scale; association between high adherence on the Morisky scale and 22 patient factors related to demographic characteristics, clinical variables, knowledge, beliefs, behaviour, health care provider relationships, and health system influences.
Results
The survey response rate was 89.6%. The average age of patients was 66 years, and 51.6% of participants were men. Forty-three percent of patients had had a diagnosis of DM for more than 10 years, and 49.7% had had a diagnosis of hypertension for more than 10 years. Eighty-nine percent of patients had some form of medical insurance. All patients had seen their family physician providers at least once within the past year. Seventy-seven percent of patients reported high adherence as measured by the Morisky scale. On multiple logistic regression, being older than 55, taking more than 7 prescribed medications, and having a lifestyle that included regular exercise or a healthy diet with low salt intake or both were significant independent predictors of high adherence scores on the Morisky scale (P ≤ .05).
Conclusion
More than three-quarters of patients with type 2 DM and hypertension from community family practice clinics in Maritime Canada reported high adherence to their antihypertensive medications. Family physicians and nurse practitioners can apply strategies to improve antihypertensive medication adherence among type 2 DM patients who are younger, taking fewer medications, or not maintaining a lifestyle that includes regular exercise or a healthy diet or both. Future studies will need to determine whether focusing adherence strategies on these patients will improve their cardiovascular outcomes.
Résumé
Objectif
Évaluer l'observance du traitement antihypertenseur et identifier les facteurs associés chez des patients de cliniques de médecine familiale souffrant de diabète et d'hypertension.
Type d'étude
Étude transversale à l'aide d'une enquête postale par auto-déclaration et de données cliniques.
Contexte
Vingt-sept médecins de famille et infirmières praticiennes de cliniques de la Nouvelle-Écosse, du Nouveau-Brunswick et de l'Ile-du-Prince-Edouard (le Maritime Family Practice Research Network).
Participants
Un total de 527 patients souffrant de diabète de type 2 et d'hypertension, dont la tension artérielle avait été mesurée à l'aide du BpTRU (un sphingomanomètre automatique) lors de visites aux cliniques de médecine familiale au cours des 6 mois précédents.
Principaux paramètres à l'étude
Niveau d'observance du traitement antihypertenseur tel que coté par les patients eux-mêmes sur l'échelle de Morisky; association entre un niveau élevé d'observance à l'échelle de Morisky et 22 facteurs en rapport avec les caractéristiques démographiques des patients, leurs particularités cliniques, leurs connaissances et croyances, leurs relations avec les soignants et les influences du système de santé.
Résultats
Le taux de réponse à l'enquête était de 89,6 %. Les patients avaient en moyenne 66 ans et 51,6 % d'entre eux étaient des hommes. Pour 43 % des diabétiques et 49,7 % des hypertendus, le diagnostic avait été posé depuis plus de 10 ans. Quatre-vingt-neuf pour cent des patients détenaient une certaine forme d'assurance médicale. Tous avaient vu leur médecin de famille au moins une fois dans l'année précédente. Soixante-dix-sept pour cent des patients rapportaient un niveau élevé de respect tel que mesuré à l'échelle de Morisky. L'analyse de régression logistique multiple a révélé qu'un âge supérieur à 55 ans, la prise de plus de 7 médicaments prescrits et un mode de vie incluant de l'exercice régulier ou une alimentation saine avec une faible consommation de sel, ou les deux, étaient des facteurs permettant de prédire de façon indépendante et significative un score d'observance élevé à l'échelle de Morisky (P ≤ ,05).
Conclusion
Plus des trois quarts des diabétiques de type 2 hypertendus de ces cliniques communautaires de médecine familiale des provinces maritimes ont déclaré un niveau élevé d'observance à la prise d'antihypertenseurs. Les médecins de famille et les infirmières praticiennes peuvent utiliser des stratégies pour améliorer l'observance de la prise de médicaments antihypertenseurs chez les diabétiques de type 2 qui sont plus jeunes, qui prennent moins de médicaments ou qui n'ont pas un style de vie qui comporte des habitudes d'exercice régulier ou une alimentation saine, ou les deux. D'autres études devront déterminer si on peut améliorer les issues cardiovasculaires de ces patients en leur appliquant ces stratégies d'observance.
The prevalence of hypertension among Canadian primary care patients with diabetes mellitus (DM) has been reported to be 63%,1 76%,2 and 79%.3 Cardiovascular (CV) disease accounts for up to 80% of deaths in those with type 2 DM, and up to 75% of CV disease might be attributable to hypertension.4 Appropriate management of hypertension in patients with DM is considered key to reducing the risk of CV events and premature death.5
A systematic review of 24 observational studies including 47 964 patients with both DM and hypertension reported that only 12% (range 6% to 30%) of participants had controlled blood pressure (BP).6 Studies of patients with DM and hypertension have reported a relationship between low adherence to antihypertensive medication and uncontrolled BP.7,8 Poor adherence to antihypertensive medication has also been directly linked to increased risk of CV disease, CV events, and mortality.8-11
Adherence is a complex process and patients' decisions about how to manage their medications are likely based on economic, physical, psychological, and social considerations.12-14 Identifying factors associated with adherence would be of value for family physicians in focusing strategies to enhance patient adherence to antihypertensive medications. The objective of this study was to measure adherence and to identify factors associated with adherence to antihypertensive medications in family practice patients with DM and hypertension.
METHODS
Design and setting
This is a cross-sectional substudy of a larger practice-based, observational study that gathered patient information from rural and urban family practices in Nova Scotia, New Brunswick, and Prince Edward Island (the Maritime Family Practice Research Network).3 The larger observational study included all consenting patients with type 2 DM who could understand English and who were available for follow-up for more than 1 year. All patients who were part of the larger observational study who had been diagnosed with type 2 DM and hypertension and who had had their BP measured with the BpTRU (an automated oscillometric instrument) by their family physicians or nurse practitioners within the past 6 months were eligible to participate in the substudy. Twenty-seven community-based health care providers (family physicians and nurse practitioners) contributed patient data to this substudy. As part of the study, each practice had a BpTRU device installed in the office for measurement of BP. Ethics approval for the project was granted from each of the 7 research ethics boards with jurisdiction over the participating practices.
Clinical data
Clinical data relevant to the diagnosis and management of type 2 DM and hypertension were extracted from patients' medical records by their health care providers. The clinical data were BP, glycosylated hemoglobin results, medications prescribed, smoking status, alcohol consumption, height, and weight.
Survey data
A patient self-report survey was designed by the research team. The survey incorporated questions from commonly used instruments: the Canadian Community Health Survey,15 the National Population Health Survey,16 the International Physical Activity Questionnaire,17 and the Bayliss Comorbidity Index,18 in conjunction with questions adapted from other instruments.19,20 Items from these instruments were included in the survey to gather demographic, health, and lifestyle information that would not generally be found in a patient chart. The survey also included the Morisky scale (Table 1),21 a 4-item adherence measure designed to evaluate medication adherence in patients with hypertension, which has been validated and found to be reliable in a variety of medication-adherence studies.22-29 Before administration, the survey was first reviewed and modified by the research team and by health care professionals with expertise in diabetes and hypertension; it was then pilot-tested in a convenience sample of 10 patients with diagnosed diabetes and hypertension.
Table 1.
Morisky scale: No—0 points, Yes—1 point; total score of 0—high adherence, 1 to 2—medium adherence, 3 to 4— low adherence.
| QUESTION | ANSWER |
|---|---|
| 1. Do you ever forget to take your medicine? | Yes or No |
| 2. Are you careless at times about taking your medicine? | Yes or No |
| 3. When you feel better, do you sometimes stop taking your medicine? | Yes or No |
| 4. Sometimes if you feel worse when you take the medicine, do you stop taking it? | Yes or No |
Adapted from Morisky et al.21
The survey was mailed to patients using a modified Dillman method.30,31 Participants were included in the study if they identified on the survey that they were currently taking any antihypertensive medication.
Analysis
Patients' adherence to antihypertensive medication was measured using the Morisky scale (Table 1).21 Patients who answered no to all 4 questions were classified as highly adherent. Patients who answered yes to at least 1 question were classified as having medium or low adherence. This scoring is consistent with the scoring used in developing the original scale and has been used in other studies to categorize adherence.22-29 Few patients reported low adherence on the Morisky scale, so the patient adherence outcome variable was dichotomized into 2 groups: high adherence versus medium or low adherence. Twenty-two patient factors were examined using data extracted from patient answers on the survey and clinical data. Other authors have considered similar factors when investigating patients' adherence with prescribed therapy.12,14,32 Univariate analysis was used to examine the association between patients' high adherence as rated on the Morisky scale and each of the 22 factors. Those factors found to be statistically significant at the level of P ≤ .10 in univariate analysis formed an initial multivariate model. Multivariate logistic regression was then performed using manual backward elimination to determine the most parsimonious model of factors associated with high adherence on the Morisky scale. Factors were sequentially eliminated from the initial multivariate model until only factors significant at the level of P ≤ .05 remained in the final model. All statistical analyses were completed using SAS, version 9.1.
RESULTS
Descriptive statistics
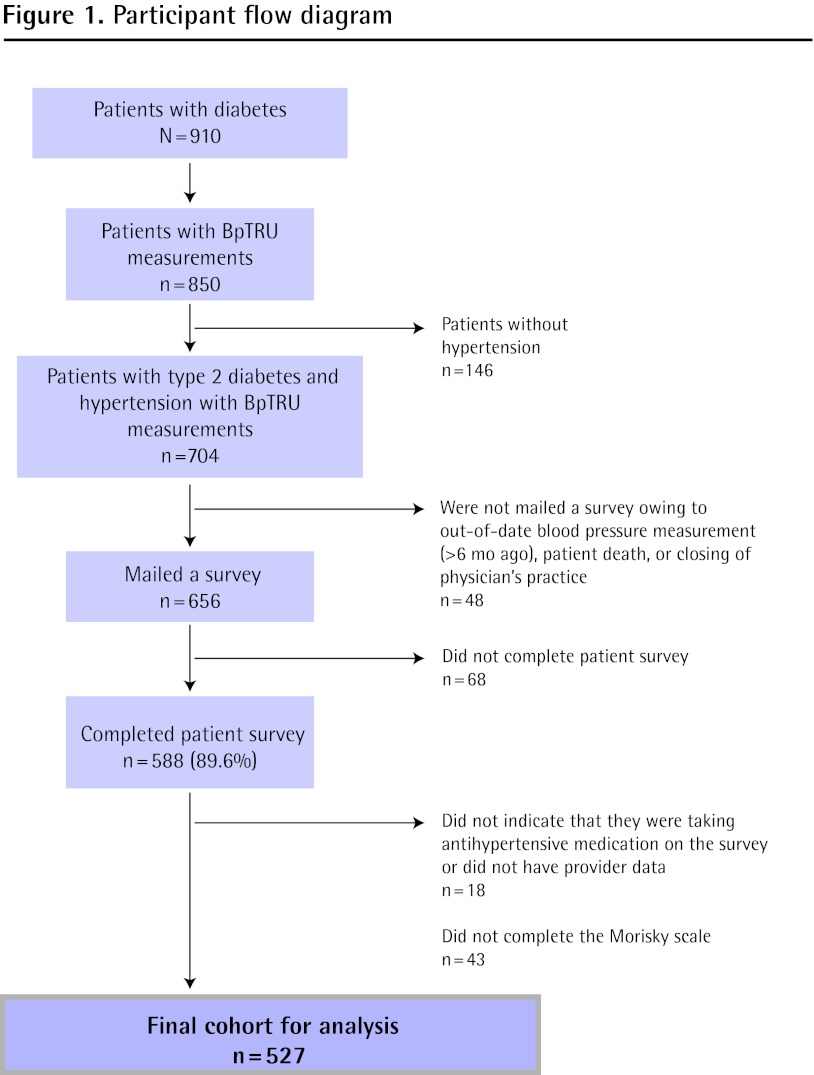
The survey response rate was 89.6%; 656 patients were mailed the survey and 588 completed it. Forty-three patients did not fully complete the Morisky scale. There was no difference between the patients who completed the survey and the 43 patients who did not complete the Morisky scale in terms of age (P = .07), sex (P = .84), or BP (P = .09). Eighteen patients did not indicate that they were taking antihypertensive medication or did not have provider data. The effective sample size was 527 patients (Figure 1). The mean (SD) patient age was 66 (10) years. Fifty-three percent of patients had BP levels at or below target (≤ 130/80 mm Hg).33 The frequency distribution of all 22 factors explored in the study can be found in Table 2.
Figure 1. Participant flow diagram.
Table 2.
Factors explored in the study: Participants had a mean (SD) of 8.04 (4.57) comorbid diseases.
| VARIABLES | N (%),* N = 527 |
|---|---|
| Demographic characteristics | |
| Age, y | |
| • < 55 | 77 (14.6) |
| • 55-64 | 166 (31.5) |
| • 65-74 | 173 (32.8) |
| • ≥ 75 | 111 (21.1) |
| Sex | |
| • Male | 272 (51.6) |
| • Female | 255 (48.4) |
| Marital status | |
| • Married or common law | 360 (68.3) |
| • Single, separated, widowed, or divorced | 167 (31.7) |
| Ethnicity | |
| • White | 453 (86.0) |
| • Other | 14 (2.7) |
| • Unknown | 60 (11.4) |
| Education | |
| • Grade 8-11 | 238 (45.2) |
| • Completed high school | 93 (17.6) |
| • More than high school | 176 (33.4) |
| • Unknown | 20 (3.8) |
| Clinical variables | |
| Duration of diabetes, y | |
| • < 5 | 149 (28.3) |
| • 5-10 | 146 (27.7) |
| • > 10 | 225 (42.7) |
| • Unknown | 7 (1.3) |
| Duration of hypertension, y | |
| • < 5 | 113 (21.4) |
| • 5-10 | 148 (28.1) |
| • > 10 | 262 (49.7) |
| • Unknown | 4 (0.8) |
| Glycemic control† | |
| • Controlled (HbA1c ≤ 7%) | 294 (56.4) |
| • Uncontrolled (HbA1c > 7%) | 227 (43.6) |
| No. of prescription medications | |
| • 1-6 | 275 (52.2) |
| • ≥ 7 | 252 (47.8) |
| No. of cardiovascular diseases | |
| • 0 | 258 (49.0) |
| • 1 | 151 (28.7) |
| • 2 | 52 (9.9) |
| • 3 | 31 (5.9) |
| • 4 | 35 (6.6) |
| Depression or anxiety | |
| • Yes | 432 (82.0) |
| • No | 95 (18.0) |
| Lifestyle factors | |
| • Exercise and healthy diet | 228 (43.3) |
| • Either exercise or healthy diet | 231 (43.8) |
| • Neither exercise nor healthy diet | 68 (12.9) |
| Alcohol intake | |
| • Non or occasional drinker | 361 (68.5) |
| • Mild drinker | 153 (29.0) |
| • Heavy drinker | 13 (2.5) |
| Smoking status | |
| • Current | 55 (10.4) |
| • Past | 237 (45.0) |
| • Never | 208 (39.5) |
| • Unknown | 27 (5.1) |
| Knowledge, beliefs, behaviour | |
| Told BP target by provider | |
| • No | 33 (6.3) |
| • Yes | 458 (86.9) |
| • I do not remember | 36 (6.8) |
| Risk awareness of high BP | |
| • Not aware | 7 (1.3) |
| • Aware | 492 (93.4) |
| • Unsure | 28 (5.3) |
| Beliefs that BP medications are helpful in controlling BP | |
| • Not helpful at all | 5 (0.9) |
| • Somewhat helpful | 14 (2.7) |
| • Very helpful | 494 (93.7) |
| • Not sure | 14 (2.7) |
| BP self-monitoring | |
| • No | 204 (38.7) |
| • Sometimes | 228 (43.3) |
| • Often | 95 (18.0) |
| Health care provider relationships | |
| Visits to diabetes education program in past year | |
| • None | 356 (67.6) |
| • 1 visit | 88 (16.7) |
| • ≥ 2 visits | 83 (15.7) |
| Seen a family doctor in past year | |
| • No | 0 (0.0) |
| • Yes | 527 (100.0) |
| Health system influences | |
| Drug insurance coverage† | |
| • No | 56 (10.8) |
| • Yes | 464 (89.2) |
BP—blood pressure, HbA1c—glycosylated hemoglobin A1c.
Not all categories add to 100% owing to rounding.
An HbA1c measurement was not available for 6 participants.
Information on insurance coverage was not available for 7 participants.
Measurement of adherence
On the Morisky scale, 77.4% of patients reported high adherence, 20.9% reported medium adherence, and 1.7% reported low adherence.
Univariate analyses
After univariate analyses was performed on each of the 22 factors, only 7 factors remained significant (P ≤ .10) predictors of high adherence on the Morisky scale (Table 3).
Table 3. Results of univariate and multivariate analyses examining the relationship between high adherence to antihypertensive medication, as measured by the Morisky scale, and factors explored in the study.
| FACTOR | N (%), N = 527 | ODDS RATIO (95% CI) | |
|---|---|---|---|
|
| |||
| UNIVARIATE MODEL* | FINAL MULTIVARIATE MODEL† | ||
| Age, y | |||
| • <55 | 77 (14.6) | 1.00 | 1.00 |
| • 55-64 | 166 (31.5) | 1.93 (1.09 to 3.42) | 1.92 (1.07 to 3.43) |
| • 65-74 | 173 (32.8) | 2.97 (1.64 to 5.39) | 2.71 (1.48 to 4.95) |
| • ≥ 75 | 111 (21.1) | 5.08 (2.43 to 10.61) | 4.56 (2.16 to 9.61) |
| Sex | |||
| • Male | 272 (51.6) | 1.00 | NS |
| • Female | 255 (48.4) | 1.46 (0.96 to 2.20) | |
| Education | |||
| • Grade 8-11 | 238 (45.2) | 1.04 (0.59 to 1.85) | NS |
| • Completed high school | 93 (17.6) | 1.00 | |
| • More than high school | 176 (33.4) | 0.85 (0.47 to 1.53) | |
| • Unknown | 20 (3.8) | 5.54 (0.70 to 43.86) | |
| Duration of hypertension, y | |||
| • < 5 | 113 (21.4) | 1.00 | NS |
| • 5-10 | 148 (28.1) | 1.44 (0.82 to 2.52) | |
| • > 10 | 262 (49.7) | 1.63 (0.98 to 2.70) | |
| • Unknown | 4 (0.8) | > 999.99 (< 0.001 to > 999.99) | |
| Prescription medications | |||
| • 1-6 | 275 (52.2) | 1.00 | 1.00 |
| • ≥ 7 | 252 (47.8) | 1.69 (1.12 to 2.57) | 1.54 (1.00 to 2.38) |
| BP self-monitoring | |||
| • No | 204 (38.7) | 1.00 | NS |
| • Sometimes | 228 (43.3) | 1.05 (0.68 to 1.63) | |
| • Often | 95 (18.0) | 2.10 (1.08 to 4.09) | |
| Healthy lifestyle | |||
| • Exercise and healthy diet | 228 (43.3) | 1.00 | 1.00 |
| • Either exercise or healthy diet | 231 (43.8) | 1.23 (0.78 to 1.97) | 1.10 (0.69 to 1.76) |
| • Neither exercise nor healthy diet | 68 (12.9) | 0.53 (0.29 to 0.95) | 0.53 (0.29 to 0.98) |
BP—blood pressure, NS—not significant.
Significant results (P ≤ .10) of the univariate analyses examining the unadjusted relationships between high adherence on the Morisky scale and patient factors.
Significant results (P ≤ .05) of the multivariate analyses examining the adjusted relationships between high adherence on the Morisky scale and patient factors.
Multivariate analyses
The 7 factors found to be significant (P ≤ .10) in univariate analyses formed the initial multivariate model. In the final model, age older than 55 years, taking more than 7 medications of any type, and having a lifestyle of regular exercise or a healthy diet or both remained significantly (P ≤ .05) independently associated with high adherence on the Morisky scale (Table 3).
DISCUSSION
A recent publication of results from the same group of patients with type 2 DM and hypertension as our current study found that high adherence to antihypertensive medication was associated with better BP control.34 In the current study of family practice patients with DM and hypertension, 77% of patients reported high adherence to their antihypertensive medication. Other studies report similar results, but comparison to our study is difficult because previous studies were based on differing patient populations and used a variety of definitions, data sources, and methods to measure adherence. An Ontario prescription database study of 207 473 elderly hypertensive patients (20% with DM) that followed prescriptions filled, found that more than 90% of participants had high adherence in the first 2 years after their initial antihypertensive prescription.35 A US prescription database study of 161 697 adult patients with DM that defined adherence using prescription medication gaps, found that 80% of patients were adherent with their antihypertensive medication.36 Finally, a retrospective cohort study of 11 532 adult patients with DM (with or without hypertension) in the United States that calculated adherence as the proportion of days covered for all filled prescriptions of antihypertensive medications found that 79% of patients were adherent.8
Several reasons might exist for the high level of adherence reported by patients in our study. First, 88% of the patients had some form of health insurance, and so the cost of medications was not likely an important barrier. Other studies report that medication cost and lack of insurance coverage can affect medication adherence.32,37,38 A second reason for the high rate of adherence in our study might be that all participants had seen their family doctors at least once in the year before the study, with the potential for monitoring treatment, discussing adverse affects, changing the regimen when appropriate, and improving patient understanding of treatment. A 2005 US study of 1432 patients taking antihypertensive medication reported that not having a health care provider was a barrier to medication adherence, and patients with more primary care visits had less difficulty taking their medication.38
Three factors in our study of family practice patients with DM and hypertension were found to be associated with high adherence to antihypertensive medications. Compared with patients younger than 55 years of age, those aged 55 to 64 were almost 2 times more likely, those 65 to 74 were almost 3 times more likely, and those 75 and older were almost 5 times more likely to report high adherence to their antihypertensive medication. Our findings are in keeping with prescription database studies of patients with hypertension with or without diabetes that have found a similar relationship between older age and better patient adherence to antihypertensive medications.8,39-42
Patients in our study who were taking more than 7 medications of any type were more likely to report high adherence compared with those taking 1 to 6 medications. This could be the result of better organization of medications with prolonged duration of disease, organization systems such as pill organizers or blister packing as more medications are added, or more frequent visits to the family physician for medication refills that might reinforce adherence. Two patient self-report studies and a database study reported similar findings to our study, with patients reporting better adherence to their antihypertensive medications when they were taking more medications of any type.38,43,44
Regular exercise, a healthy diet with low salt intake, and medication adherence are recommended by the Canadian Hypertension Education Program as patient-modifiable factors in improving BP control.5 Patients in our study who reported that they maintained a lifestyle of regular exercise or a healthy diet including low salt intake or both were twice as likely to report high adherence. This result suggests that interventions to support healthy lifestyle changes might be beneficial in improving medication adherence.
This study had many strengths, including participants from community family medicine practices and a high survey response rate.
Limitations
All participants in this study had seen their health care providers within the past 6 months and had had BpTRU measurements. This might have led to selection bias: those patients who had not seen their providers recently might have had lower adherence than those patients who participated in the study. The study population was older and largely white and English-speaking. This might limit the generalizability of our results and did not allow us to analyze ethnic and language diversity as factors; these have been found to be associated with adherence in other studies.42,4445 The survey was designed by our research team and incorporated questions from other surveys, so we cannot be certain of its validity and reliability. Patients were asked to return the survey anonymously and were guaranteed that no feedback would be given to their health care providers, but reporting bias might still have occurred. The study was a secondary analysis of data from a larger community-based study, and there might be other factors that are associated with adherence that we were unable to investigate. We also did not ask patients to specify which antihypertensive medications they were taking. Other studies have found variable rates of adherence between drug classes.35 Finally, adjusted CIs associated with the number of prescribed medications were relatively wide. This is an indication of a level of imprecision in these results and the potential need for additional participants to increase power.
Conclusion
More than three-quarters of patients with type 2 DM and hypertension from community family practices in Maritime Canada reported high adherence to their antihypertensive medications. Patients who were younger, taking fewer medications of any type, or did not maintain a lifestyle of regular exercise or a healthy diet including low salt intake reported poor adherence to their medication. The findings from our study can help family physicians and nurse practitioners identify patients in their practices who might be less likely to be adherent to their antihypertensive medications. Future studies will need to determine whether focusing adherence strategies on these patients will improve their CV outcomes.
Acknowledgment
We thank all of the participating community family physicians who recruited patients for this study, and the patients themselves for their willingness to be involved and to complete our mailed survey We also thank Dr Carl Abbott of the Department of Medicine at Dalhousie University in Halifax, NS; Dr Ingrid Sketris of the College of Pharmacy at Dalhousie University; Dr Elizabeth Mann of the Department of Medicine at Dalhousie University; Celeste Latter of the Department of Family Medicine at Dalhousie University; Peggy Dunbar of the Diabetes Care Program of Nova Scotia; and Dr Marshall Godwin of the Department of Family Medicine at Memorial University in St John's, Nfld, for their assistance with the concept and design of this study The operating funding for this phase of our project was provided by the Canadian Institutes of Health Research (ROP-82512), the Nova Scotia Health Research Foundation, and the Heart and Stroke Foundation of Nova Scotia. The BpTRU equipment used in this study was funded by the Office of Research Services of the Faculty of Medicine at Dalhousie University and the Capital District Health Authority of Halifax. The earlier phase of our study, which was essential to the report, was also supported by the Dalhousie Medical Research Foundation and the Prince Edward Island Health Research Institute.
EDITOR'S KEY POINTS
Appropriate management of hypertension in patients with diabetes mellitus is considered key to reducing the risk of cardiovascular events and premature death. This study aimed to measure adherence and to identify factors associated with adherence to antihypertensive medications among patients with diabetes mellitus and hypertension.
Results of this study suggest that family physicians might do well to focus their efforts to improve adherence on younger patients, those taking fewer medications, and those not maintaining a healthy lifestyle. Patients who reported that they maintained a lifestyle of regular exercise or a healthy diet or both were twice as likely to report high adherence; interventions to support healthy lifestyle changes might be beneficial in improving medication adherence.
POINTS DE REPÈRE DU RÉDACTEUR
On admet généralement qu'un traitement adéquat de l'hypertension chez le diabétique joue un rôle clé pour réduire le risque d'accident cardiovasculaire et de mort prématurée. Cette étude cherchait à évaluer le degré d'observance de la médication antihypertensive et à identifier les facteurs qui favorisent cette observance chez des patients souffrant de diabète et d'hypertension.
Les résultats de cette étude donnent à croire que les médecins de famille feraient bien de concentrer leurs efforts sur les patients plus jeunes, ceux qui prennent moins de médicaments et ceux qui n'ont pas un mode de vie sain s'ils veulent améliorer l'observance de la médication. Les patients qui déclaraient maintenir un style de vie comportant une pratique régulière d'exercice et une alimentation saine étaient deux fois plus susceptibles de rapporter un fort degré d'observance; des interventions pour promouvoir un mode de vie sain pourraient être utiles pour augmenter la fidélité à la prise de médicaments.
Footnotes
Contributors: Dr Natarajan participated in conception and design of the study, acquisition of data, analysis and interpretation of data, and drafting and revising the manuscript. Dr Putnam participated in conception and design of the study, interpretation of the results, and drafting and revising the manuscript. Ms Van Aarsen participated in analysis and interpretation of the data and drafting and revising the manuscript. Ms Lawson participated in conception and design of the study and drafting and revising the manuscript. Dr Burge participated in conception and design of the study and drafting and revising the manuscript. All authors approved the final version to be submitted.
Competing interests: None declared
This article has been peer reviewed. Can Fam Physician 2013;59:e93-100
References
- 1.Harris SB, Ekoé J, Zdanowicz Y, Webster-Bogaert S. Glycemic control and morbidity in the Canadian primary care setting (results of the Diabetes in Canada Evaluation Study). Diabetes Res Clin Pract 2005;70(1):90-7 [DOI] [PubMed] [Google Scholar]
- 2.Supina AL, Guirguis LM, Majumdar SR, Lewanczuk RZ, Lee TK, Toth EL, et al. Treatment gaps for hypertension management in rural Canadian patients with type 2 diabetes mellitus. Clin Ther 2004;26(4):598-606 [DOI] [PubMed] [Google Scholar]
- 3.Putnam W, Buhariwalla F, Lacey K, Foodfellow M, Goodine RA, Hall J, et al. Drug management for hypertension in type 2 diabetes in family practice. Can Fam Physician 2009;55:728-34 [PMC free article] [PubMed] [Google Scholar]
- 4.Sowers JR, Epstein M, Frohlich ED. Diabetes, hypertension, and cardiovascular disease: an update. Hypertension 2001;37(4):1053-9 [DOI] [PubMed] [Google Scholar]
- 5.Canadian Hypertension Education Program Management of hypertension for people with diabetes. Clinical paper. Markham, ON: Hypertension Canad; 2011. Available from: www.hypertension.ca//images/stories/dls/HTN_Diabetes/2011_ManagementOfHypertensionForPeopleWithDiabetesClinicalPaperEN.pdf Accessed 2013 Jan 14 [Google Scholar]
- 6.McLean DL, Simpson SH, McAlister FA, Tsuyuki RT. Treatment and blood pressure control in 47,964 people with diabetes and hypertension: a systematic review of observational studies. Can J Cardiol 2006;22(10):855-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grant RW, Devita NG, Singer DE, Meigs JB. Polypharmacy and medication adherence in patients with type 2 diabetes. Diabetes Care 2003;26(5):1408-12 [DOI] [PubMed] [Google Scholar]
- 8.Ho PM, Rumsfeld JS, Masoudi FA, McClure DL, Plomondon ME, Steiner JF, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med 2006;166(17):1836-41 [DOI] [PubMed] [Google Scholar]
- 9.Kettani FZ, Draomir A, Côté R, Roy L, Bérard A, Blais L, et al. Impact of better adherence to antihypertensive agents on cerebrovascular disease for primary prevention. Stroke 2009;40(1):213-20 Epub 2008 Nov 28. [DOI] [PubMed] [Google Scholar]
- 10.Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa E, Immordino V, et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation 2009;120(16):1598-605 Epub 2009 Oct 5. [DOI] [PubMed] [Google Scholar]
- 11.Esposti LD, Saragoni S, Benemei S, Batacchi P, Geppetti P, Di Bar M, et al. Adherence to antihypertensive medications and health outcomes among newly treated hypertensive patients. Clinicoecon Outcomes Res 2011;3:47-54 Epub 2011 Mar 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol 2004;19(4):357-62 [DOI] [PubMed] [Google Scholar]
- 13.Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther 2001;26(5):331-42 [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization Hypertension in adherence to long-term therapies: evidence for action. Geneva, Switz: World Health Organization; 2003 [Google Scholar]
- 15.Statistics Canada Canadian Community Health Survey. Detailed information, 2005. Ottawa, ON: Statistics Canada; 2006. Available from: www5.statcan.gc.ca/bsolc/olc-cel/olc-cel?catno=82-576-X&CHROPG=1&lang=eng Accessed 2013 Jan 14 [Google Scholar]
- 16.Statistics Canada National Population Health Survey (NPHS). Ottawa, ON: Statistics Canada; 2004. Available from: www.statcan.gc.ca/concepts/nphs-ensp/index-eng.htm Accessed 2013 Jan 14 [Google Scholar]
- 17.International physical activity questionnaires. IPAQ: short. Last 7 days self-administered format. Geneva, Switz: The IPAQ Group; 2002. Available from: www.ipaq.ki.se Accessed 2013 Jan 14 [Google Scholar]
- 18.Bayliss EA, Ellis JL, Steiner JF. Subjective assessments of comorbidity correlate with quality of life health outcomes: initial validation of a comorbidity assessment instrument. Health Qual Life Outcomes 2005;3:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oliveria SA, Chen RA, McCarthy BD, Davis CC, Hill MN. Hypertension knowledge, awareness, and attitudes in a hypertensive population. J Gen Intern Med 2005;20(3):219-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stewart J, Brown K, Kendrick D, Dyas J, Nottingham Diabetes and Blood Pressure Study Group Understanding of blood pressure by people with type 2 diabetes: a primary care focus group study. Br J Gen Pract 2005;55(513):298-304 [PMC free article] [PubMed] [Google Scholar]
- 21.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986;24(1):67-74 [DOI] [PubMed] [Google Scholar]
- 22.Sung JC, Nichol MB, Venturini F, Bailey KL, McCombs JS, Cody M. Factors affecting patient compliance with antihyperlipidemic medications in an HMO population. Am J Manag Care 1998;4(10):1421-30 [PubMed] [Google Scholar]
- 23.Krapek K, King K, Warren S, George K, Caputo D, Mihelich K, et al. Medication adherence and associated hemoglobin A1c in type 2 diabetes. Ann Pharmacother 2004;38(9):1357-62 Epub 2004 Jul 6. [DOI] [PubMed] [Google Scholar]
- 24.Venturini F, Nichol MB, Sung JC, Bailey KL, Cody M, McCombs JS. Compliance with sulfonylureas in a health maintenance organization: a pharmacy record-based study. Ann Pharmacother 1999;33(3):281-8 [DOI] [PubMed] [Google Scholar]
- 25.George CF, Peveler RC, Heiliger S, Thompson C. Compliance with tricyclic antidepressants: the value of four different methods of assessment. Br J Clin Pharmacol 2000;50(2):166-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Turbí C, Herrero-Beaumont G, Acebes JC, Torrijos A, Graña J, Miguelez R, et al. Compliance and satisfaction with raloxifene versus alendronate for the treatment of postmenopausal osteoporosis in clinical practice: an open-label, prospective, nonrandomized, observational study. Clin Ther 2004;26(2):245-56 [DOI] [PubMed] [Google Scholar]
- 27.Patel RP, Taylor SD. Factors affecting medication adherence in hypertensive patients. Ann Pharmacother 2002;36(1):40-5 [DOI] [PubMed] [Google Scholar]
- 28.Gascón JJ, Sánchez-Ortuño M, Llor B, Skidmore D, Saturno PJ, Treatment Compliance in Hypertension Study Group Why hypertensive patients do not comply with the treatment: results from a qualitative study. Fam Pract 2004;21(2):125-30 [DOI] [PubMed] [Google Scholar]
- 29.Horne R, Weinman J. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res 1999;47(6):555-67 [DOI] [PubMed] [Google Scholar]
- 30.Dillman DA. Mail and telephone surveys: the total design method. New York, NY: John Wiley & Sons; 1978 [Google Scholar]
- 31.Salant P, Dillman DA. How to conduct your own survey.New York, NY: John Wiley & Sons; 1994 [Google Scholar]
- 32.Grégoire JP, Moisan J, Guibert R, Ciampi A, Milot A, Gaudet M, et al. Determinants of discontinuation of new courses of antihypertensive medications. J Clin Epidemiol 2002;55(7):728-35 [DOI] [PubMed] [Google Scholar]
- 33.Canadian Diabetes Association 2008 clinical practice guidelines for the prevention and management of diabetes in Canada Can J Diabetes 2008;32(Suppl 1):S1-201 [DOI] [PubMed] [Google Scholar]
- 34.Putnam W, Lawson B, Buhariwalla F, Goodfellow M, Goodine RA, Hall J, et al. Hypertension and type 2 diabetes: what family physicians can do to improve control of blood pressure—an obersational study. BMC Fam Pract 2011;12:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Friedman O, McAlister FA, Yun L, Campbell NR, Tu K, Canadian Hypertension Education Program Outcomes Research Taskforce Antihypertensive drug persistence and compliance among newly treated elderly hypertensives in Ontario. Am J Med 2010;123(2):173-81 [DOI] [PubMed] [Google Scholar]
- 36.Schmittdiel JA, Uratsu CS, Karter AJ, Heisler M, Subramanian U, Mangione C, et al. Why don't diabetes patients achieve recommended risk factor targets? Poor adherence versus lack of treatment intensification. J Gen Intern Med 2008;23(5):588-94 Epub 2008 Mar 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rubin RR. Adherence to pharmacologic therapy in patients with type 2 diabetes mellitus. Am J Med 2005;118(Suppl 5A):27S-34S [DOI] [PubMed] [Google Scholar]
- 38.Vawter L, Tong X, Gemilyan M, Yoon PW. Barriers to antihypertensive medication adherence among adults—United States, 2005. J Clin Hypertens (Greenwhich) 2008;10(12):922-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shaya FT, Du D, Gbarayor CM, Frech-Tamas F, Lau H, Weir MR. Predictors of compliance with antihypertensive therapy in a high-risk Medicaid population. J Natl Med Assoc 2009;101(1):34-9 [DOI] [PubMed] [Google Scholar]
- 40.Morris AB, Li J, Kroenke K, Bruner-England TE, Young JM, Murray MD. Factors associated with drug adherence and blood pressure control in patients with hypertension. Pharmacotherapy 2006;26(4):483-92 [DOI] [PubMed] [Google Scholar]
- 41.Ren XS, Kazis LE, Lee A, Zhang H, Miller DR. Identifying patient and physician characteristics that affect compliance with antihypertensive medications. J Clin Pharm Ther 2002;27(1):47-56 [DOI] [PubMed] [Google Scholar]
- 42.Yang Y, Thumula V, Pace P, Banahan F, Wilkin N, Lobb W. Predictors of medication nonadherence among patients with diabetes in Medicare Part D programs: a retrospective cohort study. Clin Ther 2009;31(10):2178-88 [DOI] [PubMed] [Google Scholar]
- 43.Grégoire J, Moisan J, Guibert R, Ciampi A, Milot A. Predictors of self-reported noncompliance with antihypertensive drug treatment: a prospective cohort study. Can J Cardiol 2006;22(4):323-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Siegel D, Lopez J, Meier J. Antihypertensive medication adherence in the Department of Veterans Affairs. Am J Med 2007;120(1):26-32 [DOI] [PubMed] [Google Scholar]
- 45.Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J Gen Intern Med 2010;25(11):1172-7 [DOI] [PMC free article] [PubMed] [Google Scholar]