Abstract
Objective
Investigate factors that amplify or mitigate the effects of an indicated cognitive behavioral depression prevention program for adolescents with elevated depressive symptoms.
Method
Using data from a randomized trial (Registration No. NCT00183417; N = 173) in which adolescents (M age = 15.5, SD = 1.2) were assigned to a brief cognitive behavioral prevention program or an educational brochure control condition, we tested whether elevated motivation to reduce depression and initial depressive symptom severity amplified intervention effects and whether negative life events, social support deficits, and substance use attenuated intervention effects.
Results
Hierarchical linear modeling (HLM) indicated differential intervention effects for two of the five examined variables: negative life events and substance use. For adolescents at low and medium levels of substance use or negative life events, the CB intervention produced declines in depressive symptoms relative to controls. However, at high levels of substance use or negative life events, the CB intervention did not significantly reduce depressive symptoms in comparison to controls.
Conclusions
Results imply that high-risk adolescent with either high rates of major life stress or initial substance use may require specialized depression prevention efforts.
Prevention Intervention
Although cognitive behavioral (CB) depression prevention programs have reduced depressive symptoms and risk for future onset of major depression relative to assessment-only control conditions in randomized trials conducted with children, adolescents, and adults (Horowitz & Garber, 2006; Stice, Shaw, Bohon, Marti, & Rohde, 2009), few studies have investigated factors that moderate the effects of such prevention programs (Kazdin & Weisz, 1998; Lockman, 2001). Understanding the moderators of prevention programs is important because it may promote the development of more effective interventions that incorporate a focus on topics or skills that are implicated by these analyses. For example, if deficits in social support attenuate intervention effects, future iterations of the program might be improved by focusing on developing and maintaining support networks. Moderator analyses may also help identify subgroups that are particularly likely to benefit from the current CB intervention, which should make prevention programs more economical because they could focus on the individuals most likely to benefit from this intervention. Further, this information may help identify subgroups that are unresponsive to the intervention -- for which alternative prevention interventions with different targeted mechanisms might be indicated. In addition, knowledge of moderators informs the refinement of our prevention theories. Accordingly, the present report describes analyses focusing on identifying factors that moderate the effects of a brief cognitive behavioral depression prevention program for high-risk adolescents with initial elevations in depressive symptoms; previous reports have reported the main effects (Stice, Rohde, Gau, & Wade, 2010a; Stice, Rohde, Seeley, & Gau, 2008b) and mediators of intervention effects (Stice, Rohde, Seeley, & Gau, 2010b).
Moderators can be grouped into those that amplify and those that attenuate intervention effects. We hypothesized that two factors that putatively facilitate the acquisition and application of cognitive and behavioral skills will amplify program effects. First, we hypothesize that elevated motivation to reduce depressive symptoms might potentiate intervention effects. Readiness to change presumably increases motivation to engage in the program and participate in the exercises and homework assignments, thereby promoting skill acquisition. This prediction comes from evidence that elevated distress about psychiatric symptoms and motivation for symptom reduction predicts response to CB treatment for various psychiatric disorders in adults (Keijsers, Schaap, Hoogduin, Hoogsteyns, & Kemp, 1999; Moos & King, 1997). Second, we predict that intervention effects may be larger for adolescents with higher initial levels of depression because elevated initial symptoms have been found to amplify the effects of two eating disorder prevention programs for adolescents relative to changes observed in participants in an active intervention control condition (Stice et al., 2008a). It is possible that this is because elevated symptoms provide greater impetus for change, facilitate the acquisition and application of intervention skills to address current symptoms, or because there is more room to detect symptom improvement for such participants (i.e., absence of a “floor effect” that may impact analysis of universal prevention programs).
In contrast, we predicted that three variables reflecting risk factors for depression that are not targeted in this intervention might attenuate program effects. Theoretically, these factors will promote depression, but the skills taught in the intervention will not directly defuse the effects of these risk factors. We hypothesize that the program will be less effective in reducing depressive symptoms for youth with elevated negative life events and deficits in social support because these factors increase the risk for future depression in adolescents and young adults (Garber, Keiley, & Martin, 2002; Lewinsohn et al., 1994; Tram & Cole, 2000; Turner & Lloyd, 2004). Although challenging negative cognitions about negative life events and support deficits, and encouraging increased engagement in pleasant events may attenuate the impact of these factors, we suspect cognitive restructuring will not completely counter the adverse effects of these variables. Indeed, negative life events predicted a poorer response to CB treatment for depression in adults (Jayson, Wood, Kroll, Fraser, & Harrington, 1998). We also hypothesized that concurrent substance use may mitigate program effects, as it may increase the risk for persistence or exacerbation of depressive symptoms (Brook, Brook, Zhang, Cohen, & Whitman, 2002; Rohde et al., 2001). In addition, substance use may reduce motivation for participants to engage in the intervention program or apply the skills taught or serve as a maladaptive coping mechanism for dealing with depressive symptoms. In support, substance use predicted a poorer response to CB treatment for depression in adolescent samples (Gilbert, Fine, & Haley, 1994; Rohde et al., 2001).
Methods
Participants were 173 high school students (58% female) who ranged from 14 to 19 years of age (M = 15.5; SD = 1.2) at pretest. The sample was composed of 2% Asians, 10% African Americans, 42% Caucasians, 35% Hispanics, and 11% who specified other or mixed heritage. Educational attainment of parents, a proxy for socioeconomic status, was 28% high school graduate or less; 19% some college; 36% college graduate; 17% graduate degree. The sample was more ethnically diverse than the populations from which we sampled (7% African American, 18% Hispanic, 65% Caucasian) but was representative in terms of parental education (34% high school graduate or less; 25% some college; 26% college graduate; 15% graduate degree).
Participants were recruited between 2004 – 2007 using mass mailings, handbills, and posters that invited students experiencing sadness to participate in a trial of interventions designed to improve current and future mood. Interested students (6-10% across the schools) who returned a consent form signed by both a parent and the student and who scored 20 or above on the Center for Epidemiologic Studies-Depression scale (Radloff, 1977) were invited to complete a pretest assessment. The assessment was conducted by research staff at the school in a setting that guaranteed the student privacy. Those who met criteria for current major depression upon interview were excluded and given treatment referrals (there were no other exclusion criteria). Parents were informed of current suicidal ideation. Participants were randomly assigned to cognitive behavioral (CB) group (n = 89), supportive expressive group (n = 88), CB bibliotherapy (n = 80), or an educational brochure control group (n = 84). The present study included only participants from the CB and educational brochure control groups because (a) the largest intervention effects relative to controls emerged for the CB prevention program, thereby maximizing our ability to detect moderators, (b) we suspected that there would be less interest in moderators of supportive expressive and CB bibliotherapy, as few prevention scientists are investigating these interventions, and (c) we were concerned about increasing the risk for chance findings by estimating three times as many models. The CB group intervention consisted of six weekly 1-hour sessions (44% of CB participants attended all 6 sessions; 86% attended at least 3 of the 6 sessions). Groups were facilitated by a clinical psychology graduate student and co-facilitated by an undergraduate psychology student. A detailed intervention manual for the intervention was used to insure standardized implementation. Control participants received a brochure describing depression symptoms and treatment options at the time of randomization. Participants completed a survey and diagnostic interview at pretest, posttest, and 6-month follow-up (they received $20 for completing each assessment). Assessors, who were blinded to condition, had at least a BA in psychology and received 40 hours of training in the use of the semi-structured interview. Assessors were required to show a minimum kappa agreement of .80 with expert raters before starting data collection. Assessment and groups were conducted at schools. The Oregon Research Institute Institutional Review Board approved this study. Group CB participants versus control participants showed greater reductions in depressive symptoms through 1-year follow-up and significantly reduced risk for onset of major depression through 2-year follow-up (Stice et al., 2008b; Stice et al., 2010a). See Stice et al. (2008b) for additional details regarding participant flow, facilitator training and supervision, and competence and fidelity ratings.
Depression severity
The 21-item Beck Depression Inventory (BDI; Beck, Steer, & Garbin, 1988) was used to assess depressive symptom severity at baseline. The BDI has shown internal consistency (α = .73 - .95), test-retest reliability (r = .60 - .90), and convergent validity with clinician ratings of depressive symptoms (M r = .75; Beck et al., 1988). The BDI showed internal consistency at baseline (α = .89) and 3-week test-retest in the control condition (r = .76).
Perceived social support
Items were drawn from the Network of Relationships Inventory (Furman, 1996) that assessed companionship, guidance, intimacy, affection, admiration, and reliable alliance from parents and peers (6 items each). These scales have shown internal consistency (M r = .88), test–retest reliability (M r = .69), and predictive validity (Furman, 1996; Burton, Stice, & Seeley, 2004). Combined parental and peer social support items showed good internal consistency (α = .83) and 6-week test-retest reliability in the control condition (r = .76).
Substance use
Substance use was measured with 10 items from Stice, Barrera, and Chassin (1998). Adolescents reported the frequency and quantity of intake of beer/wine/wine coolers and hard liquor, frequency of heavy drinking (5 or more drinks in a row), and frequency and quantity of cigarettes (number of smoking days, number of cigarettes per smoking day), and frequency of marijuana, stimulants, downers, inhalants, and hallucinogen use during the past month. Items used 6-point response scales ranging from never to 3-7 times a week for frequency of use, zero to 6 or more for drinks for quantity of alcohol use, and zero to 21 or more cigarettes a day for frequency of cigarette use. Items were averaged to form an overall substance use measure, which was then normalized with a square-root transformation. This scale has shown internal consistency, 1-year test-retest reliability, and predictive validity for substance use symptoms (Stice et al., 1998). It showed adequate internal consistency (α = .79) and 6-week test-retest reliability in the control condition (r = .71).
Motivation to reduce depression
Given the absence of an available measure for this purpose, a 4-item scale assessing motivation to reduce feelings of depression was developed for this trial. Items were: I have been struggling with the feeling of depression for a long time and am really ready to tackle this problem now; I am so tired of feeling depressed that I am willing to try anything that might help me; I am very motivated to participate in an intervention that will help me reduce my feelings of depression; I am prepared to give this intervention my best shot because I really want to overcome my problems with depression; and were rated on a 5-point Likert scale and averaged to form a scale score. Pilot testing (N = 44) indicated the scale showed internal consistency (α = .93) and 1-week test-retest r = .83. This scale showed a moderate correlation with BDI scores (r = .37), suggesting that it is not merely tapping depressive pathology. This scale showed good internal consistency at baseline (α = .88).
Negative life events
A modified version of The Major Life Events scale (Lewinsohn et al., 1994) was used to assess the occurrence of 14 negative life events during the past year with response options of 0 = no, 1 = once, and 2 = at least twice. Three events from the original measure that were potentially symptoms of psychopathology were dropped (“got in a lot of arguments and fights,” “had problems with drugs or alcohol,” “tried to commit suicide”) and replaced with three additional major stressors (“experienced academic failure,” “your home was damaged by fire, flood, or other disaster,” “lost a close friend”). A sum score was computed across the 14 items. The original version of the scale has shown 1-week test-retest reliability (r = .90) and predictive validity for future onset of major depression (Burton et al., 2004; Lewinsohn et al., 1994; Monroe, Rohde, Seeley, & Lewinsohn, 1999). Negative life events endorsed with these items showed convergence with interview-confirmed negative life events (M % agreement = 68; Lewinsohn, Rohde, & Gau, 2003). The adapted scale showed predictive validity for future onset of major depression (Burton, Stice, & Seeley, 2004) and showed significant, albeit moderate, concurrent validity (r =.31) with baseline measures of the Beck Depression Inventory (Beck et al., 1988) in the current study.
Depressive symptoms
The outcome measure was derived from sixteen items assessing major depression symptoms based on the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM–IV; American Psychiatric Association, 1994) adapted from the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS; Kaufman, Birmaher, Brent, Rao, & Ryan, 1996), a semi-structured diagnostic interview. Adolescents reported the peak severity of each symptom over their lifetime or since the last interview on a month-by-month basis with an expanded response format (response options: 1 = not at all to 4 = severe symptoms [with ratings of 3 and 4 reflecting diagnostic levels]). We averaged across the 16 severity items to form a continuous depressive symptom composite, which captured severity of symptoms over the past month for the baseline assessment, past 6-weeks for the posttest assessment, and past 6 months for follow-up. This adapted version of the K-SADS has shown 1-week test-retest reliability (k = .63 to 1.00) and inter-rater reliability for depression diagnosis (k = .73 to 1.00) and internal consistency (α = .68 to .84), 1-week test-retest reliability (r = .93) and inter-rater agreement (r = .85) for the symptom composite (Stice et al., 2008b).
Data Analysis
Random effects growth models within the hierarchical linear modeling (HLM) framework were used to test hypothesis of moderation (see Table 1 for descriptive statistics and intercorrelations of moderators). Individual variability in level-1 change in depressive symptoms from baseline through the 6-month follow-up assessment was modeled as a function of two level-2 predictor variables; treatment condition and the hypothesized moderator. The multiplicative interaction between the level-2 main-effect predictors constitutes a three-way cross-level interaction with time (Curran, Bauer, & Willoughby, 2006) and addresses whether the level of the baseline moderator impacted the magnitude of the effects of intervention condition on change in the outcome. We probed all significant three-way cross-level interactions by computing sample-estimated intercepts and slopes of the trajectories of depressive symptoms on time at conditional levels of the moderator, separately, within the CB group and the control group (i.e., simple trajectories) using methods described in Curran, et al. (2006). We followed recommendations in standard regression (Aiken & West, 1991) and selected values at one standard deviation below the mean-centered moderator, at the mean, and one standard deviation above the mean to represent low, medium, and high levels of the moderator, respectively. HLM models were estimated with SAS PROC MIXED using an unstructured covariance structure and individual varying time scores measured in months. Effect size is summarized by the r equivalent (Rosenthal & Rubin, 2003).
Table 1.
Descriptive Statistics and Intercorrelations for Hypothesized Study Moderators
| Hypothesized Moderator | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1 Depression severity | 1.00 | |||||
| 2 Perceived social support | −.38 | 1.00 | ||||
| 3 Substance use | .12 | −.05 | 1.00 | |||
| 4 Motivation to reduce depression | .37 | −.06 | −.08 | 1.00 | ||
| 5 Negative life events | .30 | −.30 | .27 | .10 | 1.00 | |
| 6 Initial depressive symptoms | .55 | −.26 | .10 | .33 | .29 | 1.00 |
|
| ||||||
| Mean | 19.82 | 3.56 | 0.43 | 3.36 | 5.17 | 1.84 |
| Standard deviation | 9.80 | 0.75 | 0.56 | 0.93 | 3.08 | 0.33 |
Notes. Bolded correlations are significant at p<.05, bolded and underlined correlations at p<.001. Mean and standard deviation for substance use is reported in its original metric, not the log transformed scale. Depression severity is the Beck Depression Inventory score and initial depressive symptoms are derived from the Schedule for Affective Disorders and Schizophrenia for School-Age Children.
Results
The two groups did not significantly differ (at p < .05) on demographic characteristics or any of the study variables, which suggested that randomization produced initially equivalent groups. Two percent of participants did not provide data at posttest, and 10% at the 6-month follow-up. Incomplete data for baseline predictors (i.e., study hypothesized moderators) ranged from 0%-4%. Attrition was not significantly associated (at p>.05) with any baseline outcomes or demographic characteristics. Since the missing at random assumption remained tenable we used full information maximum likelihood estimation, which uses all available data from each participant to accommodate the missing data. Intent to treat analyses were computed.
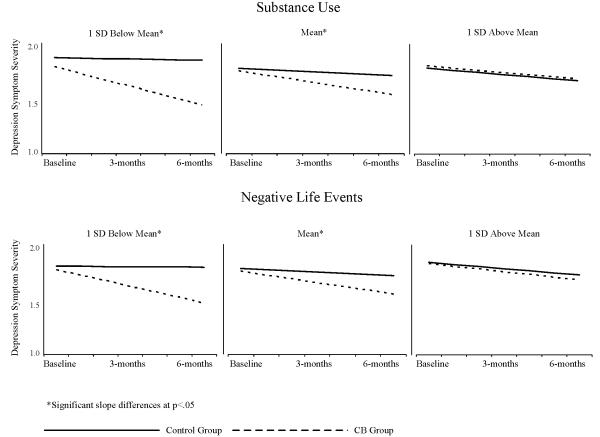
All first and second order terms and the three-way interaction term were entered into the HLM and estimated. Three of the five hypothesized moderators did not show significant three-way cross-level interactions with treatment condition and time: motivation to reduce depression (t[154]=−0.81, p=.422); social support (t[154]=0.93, p=.353); and depressive symptoms (t[154]=0.02, p=.982). However, the two remaining hypothesized moderators showed a significant three-way cross-level interaction with treatment condition and time: substance use (t[154]=−2.87, p=.005) and negative life events (t[154]=−2.33, p=.021).Table 2 shows the estimated slopes and corresponding tests statistics at low, medium, and high levels of substance use and negative life events for the CB and control conditions (to interpret the substance use measure, a participant who drank three beers 5-7 times a week and smoked marijuana a few times in the past month would be classified at the “high level” of substance use (score = 1.0, approximately 1 SD above the mean). Estimates indicate that trajectories of depressive symptoms vary over time as a function of the moderator and the magnitude of that relation depends on study condition (see also Figure 1). At low and medium levels of the moderators, CB participants showed greater reductions in depressive symptoms from baseline to 6-month follow-up than control participants, according to non-overlapping 95% confidence intervals. However, at the high level of both moderators, CB participants did not show significantly different change in depressive symptoms relative to control participants.
Table 2.
Simple Slopes for Change in Depression at Low, Medium, and High Levels of Moderators
| CB Group |
Control Group |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est. | SE | t | p | 95% CI | r | Est. | SE | t | p | 95% CI | r | |
| Substance use | ||||||||||||
| Low | −.051 | .009 | −5.95 | <.001 | −.067,−.034 | .41 | −.003 | .008 | −0.36 | .719 | −.019,.013 | .07 |
| Medium | −.035 | .006 | −6.19 | <.001 | −.046,−.024 | .45 | −.011 | .006 | −1.75 | .087 | −.022,.001 | .14 |
| High | −.019 | .008 | −2.55 | .012 | −.034,−.004 | .20 | −.019 | .009 | −2.12 | .036 | −.036,−.001 | .17 |
| Negative life events | ||||||||||||
| Low | −.044 | .008 | −5.44 | <.001 | −.060,−.028 | .40 | −.001 | .009 | 0.15 | .883 | −.019,.087 | .01 |
| Medium | −.034 | .006 | −5.98 | <.001 | −.045,−.023 | .43 | −.001 | .006 | −1.58 | .115 | −.022,.001 | .13 |
| High | −.024 | .008 | −3.12 | .002 | −.039,−.009 | .24 | −.019 | .009 | −2.14 | .034 | −.036,−.002 | .17 |
CB = cognitive behavioral, Est. = estimate, SE = standard error, CI = confidence interval.
Notes. CB group t-tests are based on 87 degrees of freedom, control group 82 degrees of freedom.
Figure 1.
Simple Slopes at Low, Medium, and High Levels of Substance Use and Negative Life Events
Discussion
The purpose of this report was to investigate factors that potentiate or attenuate the effects of an indicated CB depression prevention program for adolescents in producing reductions in depressive symptoms during and closely following the end of intervention. Results indicated that whereas the CB depression prevention program resulted in significant decreases in depressive symptoms through 6-month follow-up for those with low and medium levels of substance use or negative life events, the intervention effects did not emerge for participants with elevated baseline levels of either substance use or negative life events. To our knowledge, this is the first randomized prevention trial to find that these two factors mitigate the intervention effects of CB prevention programs. The former effect dovetails with findings from studies that have investigated moderators of CB treatment for depression (Gilbert et al., 1994; Rohde et al., 2001). Theoretically, elevated levels of substance use and negative life events weaken the intervention effects because they increase risk for persistence of depressive symptoms and are not directly addressed by components in the present CB prevention program.
Contrary to expectations, baseline social support deficits did not mitigate intervention effects and motivation to reduce depression and baseline depressive symptom severity did not potentiate intervention effects. The fact that we assessed perceived social support, rather than enacted support reported by peers and family members, may have made it difficult to detect moderating effects for this factor. Further, the use of a short measure of motivation to reduce depression that we created for this trial might have limited our ability to detect moderating effects for this factor. Perhaps the limited range in depressive symptom severity, as it was an inclusion criterion, rendered it difficult to detect the effect of this potential moderator. In this context, it should be noted that power exceeded .80 to detect even small effect sizes (d = .22), suggesting that the null findings are not due to limited power.
Basic demographic factors are also important potential factors that may identify subgroups that do or do not benefit from prevention interventions; they are easily measured and inform the generalizability of findings. The present results extend null findings of demographic characteristics as potential moderators; program effects for depressive symptoms were not moderated by participant gender or age (Stice, Rohde, Gau, & Wade, 2010) or participant race/ethnicity (Marchand, Ng, Rohde, & Stice, 2010). Previous findings regarding the moderating effects of gender on depression prevention efforts have been varied, with some trials suggesting intervention effects are stronger for females (Jaycox, Reivich, Gillham, & Seligman, 1994; Petersen, Leffert, Graham, Alwin, & Ding, 1997; Gillham, Hamilton, Freres, Patton, & Gallop, 2006), others suggesting they are stronger for males (Clarke, Hawkins, Murphy, & Sheeber, 1993; Ialongo, et al., 1999; Seligman, Schulman, DeRubies, & Hollon, 1999) and still others finding no gender differences (Horowitz, Garber, Ciesla, Young, & Mufson, 2007). Although few trials have tested whether race/ethnicity moderated the effects of depression prevention programs, one meta-analytic review found that programs were significantly more effective for samples with a greater proportion of ethnic minority individuals (Stice et al., 2009). The evidence that this indicated CB depression prevention program was similarly efficacious for both genders, adolescents of different ages, and adolescents from different ethnic/racial groups is encouraging because it suggests this intervention is effective for a broad range of adolescences at risk for onset of major depression and that it may not be necessary to adapt this prevention program for different populations, which should facilitate dissemination.
Limitations to the current study should be noted. First, we focused on change in depressive symptoms rather than onset of depressive diagnoses. It is possible that moderators of the brief CB depression program for risk of future depressive episodes exist; however, with the study sample size it was not feasible to test moderating hypothesis for depression onset due to the low number of incidence cases. Second, we only examined a limited number of potential moderators; it is possible that other variables moderate the effects of the brief CB depression program (e.g., personality traits) on reductions in depressive symptoms. Finally, moderators were all assessed with brief self-report scales, some of which were created for this study. The self-report scales may have been biased in ways due to subthreshold depressive symptoms (e.g., resulting from a negative attributional style). Further, adolescents can over-report negative life events (e.g., reporting a negative life event from a relatively trivial reason, such as a minor injury or illness versus a serious injury or illness) and, in addition, our self-report stress measure recorded higher scores for multiple instances of the same event. Thus, mean values on the life events measure do not refer to unique, verified major life events, as would have been possible had we used an interview methodology. Given the finding that stress may moderate the effectiveness of CB prevention but that self-report of major life events may result in over-reporting (e.g., Lewinsohn, Rohde, & Gau, 2003), future research should include an interview-based measurement of major life events.
The present findings have important research and clinical implications. The evidence that negative life events attenuated the effects of this CB depression prevention program suggests that future iterations of this intervention could be improved by expressly encouraging participants to identify negative life events that they have experienced relatively recently or are likely to experience in the future and apply the CB skills to negative cognitions about these events. For example, participants could be encouraged to apply cognitive reframing skills to personally relevant negative life events. The finding that elevated baseline substance use attenuated the effects of this prevention program implies that it might be advantageous to screen adolescents who enroll in indicated depression prevention programs for substance use, and triage those who report elevated use to a concurrent substance use intervention program. Given our previous finding that participation in the CB group was associated with reduced substance use (Stice et al., 2008b), the two studies suggest that the CB group may delay initial onset of substance use in this high-risk sample but that those participants who are already using substances above average may not receive appreciable benefit from this intervention, as opposed to a brochure control.
Acknowledgments
This study was supported by a research grants MH067183 and MH080760 from the National Institute of Health.
Thanks go to project research assistants, Courtney Byrd, Kathryn Fischer, Amy Folmer, Cassie Goodin, Jacob Mase, and Emily Wade, a multitude of undergraduate volunteers, the Austin Independent School District, and the participants who made this study possible.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park, CA: 1991. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed Author; Washington, DC: 1994. [Google Scholar]
- Beck AT, Steer RM, Garbin M. Psychometric properties of the Beck Depression Inventory: 25 years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Brook D, Brook J, Zhang C, Cohen P, Whiteman M. Drug use and the risk for major depressive disorder, alcohol dependence, and substance use disorders. Archives of General Psychiatry. 2002;59:1039–1044. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- Burton EM, Stice E, Seeley JR. A prospective test of the stress-buffering model of depression in adolescent girls: No support once again. Journal of Consulting and Clinical Psychology. 2004;72:689–697. doi: 10.1037/0022-006X.72.4.689. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Hawkins W, Murphy M, Sheeber L. Schoolbased primary prevention of depressive symptomatology in adolescents: Findings from two studies. Journal of Adolescent Research. 1993;8:183–204. [Google Scholar]
- Cleary PJ. Problems of internal consistency and scaling in life events schedules. Journal of Psychometric Research. 1981;25:309–320. doi: 10.1016/0022-3999(81)90008-8. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Bauer DJ, Willoughby MT. Testing and probing interactions in hierarchical linear growth models. In: Bergeman CS, Boker SM, editors. The Notre Dame Series on Quantitative Methodology, Volume 1: Methodological Issues in Aging Research. Lawrence Erlbaum Associates; Mahwah, NJ: 2006. pp. 99–129. [Google Scholar]
- Furman W. Measurement of friendship perceptions: Conceptual and methodological issues. In: Bukowski WM, Newcomb AF, Hartup WW, editors. The company we keep. Cambridge Univ; NY: 1996. pp. 41–65. [Google Scholar]
- Garber J, Keiley MK, Martin NC. Developmental trajectories of adolescents’ depressive symptoms: Predictors of change. Journal of Consulting and Clinical Psychology. 2002;70:79–95. doi: 10.1037//0022-006x.70.1.79. [DOI] [PubMed] [Google Scholar]
- Gilbert M, Fine S, Haley G. Factors associated with dropout from group psychotherapy with depressed adolescents. Canadian Journal of Psychiatry. 1994;39:358–359. doi: 10.1177/070674379403900608. [DOI] [PubMed] [Google Scholar]
- Gillham JE, Hamilton J, Freres DR, Patton K, Gallop R. Preventing depression among early adolescents in the primary care setting: A randomized controlled study of the Penn Resiliency Program. Journal of Abnormal Child Psychology. 2006;34:203–219. doi: 10.1007/s10802-005-9014-7. [DOI] [PubMed] [Google Scholar]
- Horowitz JL, Garber J, Ciesla JA, Young JF, Mufson L. Prevention of depressive symptoms in adolescents: A randomized trial of cognitive-behavioral and interpersonal prevention programs. Journal of Consulting and Clinical Psychology. 2007;75:693–706. doi: 10.1037/0022-006X.75.5.693. [DOI] [PubMed] [Google Scholar]
- Hurst MW, Jenkins CD, Rose RM. The assessment of life change stress: A comparative and methodological inquiry. Psychometric Medicine. 1978;40:126–141. doi: 10.1097/00006842-197803000-00005. [DOI] [PubMed] [Google Scholar]
- Ialongo NS, Werthamer L, Kellam SG, Brown CH, Wang S, Lin Y. Proximal impact of two first-grade preventive interventions on the early risk behaviors for later substance abuse, depression, and antisocial behavior. American Journal of Community Psychology. 1999;27:599–641. doi: 10.1023/A:1022137920532. [DOI] [PubMed] [Google Scholar]
- Jaycox LH, Reivich KJ, Gillham J, Seligman MEP. Prevention of depressive symptoms in school children. Behavioral Research and Therapy. 1994;32:801–816. doi: 10.1016/0005-7967(94)90160-0. [DOI] [PubMed] [Google Scholar]
- Jayson D, Wood A, Kroll L, Fraser J, Harrington R. Which depressed patients respond to cognitive-behavioral treatment? Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:35–39. doi: 10.1097/00004583-199801000-00014. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Ryan N. Schedule for Affective Disorder and Schizophrenia for School Age Children (6-18 Years) - Present and Lifetime Version (K-SADS-PL. Version 1.0 The Department of Psychiatry of the University of Pittsburgh School of Medicine; 1996. [Google Scholar]
- Kazdin AE, Weisz J. Identifying and developing empirically supported child and adolescent treatments. Journal of Consulting and Clinical Psychology. 1998;66:19–36. doi: 10.1037//0022-006x.66.1.19. [DOI] [PubMed] [Google Scholar]
- Keijsers G, Schaap C, Hoogduin C, Hoogsteyns B, de-Kemp E. Preliminary results of a new instrument to assess patient motivation for treatment in cognitive-behaviour therapy. Behavioural and Cognitive Psychotherapy. 1999;27:165–179. [Google Scholar]
- Lewinsohn PM, Roberts RE, Seeley JR, Rohde P, Gotlib IH, Hops H. Adolescent psychopathology: II. Psychosocial risk factors for depression. Journal of Abnormal Psychology. 1994;103:302–315. doi: 10.1037//0021-843x.103.2.302. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Gau J. Comparability of self-report checklist and interview data in the assessment of stressful life events in young adults. Psychological Reports. 2003;93:459–471. doi: 10.2466/pr0.2003.93.2.459. [DOI] [PubMed] [Google Scholar]
- Lockman JE. Issues in prevention with school-aged children: Ongoing intervention refinement, developmental theory, prediction and moderation, and implementation and dissemination. Prevention and Treatment. 2001;4 np. [Google Scholar]
- Marchand E, Ng J, Rohde P, Stice E. Effects of an indicated cognitive-behavioral depression prevention program are similar for Asian American, Latino, & European American adolescents. Journal of Consulting and Clinical Psychology. 2010;48:821–825. doi: 10.1016/j.brat.2010.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM, Rohde P, Seeley JR, Lewinsohn P. Life events and depression in adolescence: Relationship loss as a prospective risk factor for first onset of major depressive disorder. Journal of Abnormal Psychology. 1999;108:606–614. doi: 10.1037//0021-843x.108.4.606. [DOI] [PubMed] [Google Scholar]
- Moos RH, King MJ. Participation in community residential treatment and substance abuse patients’ outcomes at discharge. Journal of Substance Abuse Treatment. 1997;14:71–80. doi: 10.1016/s0740-5472(96)00189-4. [DOI] [PubMed] [Google Scholar]
- Petersen AC, Leffert N, Graham B, Alwin J, Ding S. Promoting mental health during the transition into adolescence. In: Schulenberg J, Muggs JL, Hierrelmann AK, editors. Health risks and developmental transitions during adolescence. Cambridge University Press; New York: 1997. pp. 471–497. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general populaion. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rohde P, Clarke GN, Lewinsohn PM, Seeley JR, Kaufman NK. Impact of comorbidity on a cognitive-behavioral group treatment for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:795–802. doi: 10.1097/00004583-200107000-00014. [DOI] [PubMed] [Google Scholar]
- Rothenthal R, Rubin DB. requivalent: A simple effect size indicator. Psychological Methods. 2003;8:492–96. doi: 10.1037/1082-989X.8.4.492. [DOI] [PubMed] [Google Scholar]
- Seligman ME, Schulman P, DeRubeis RJ, Hollon SD. The prevention of depression and anxiety. Prevention and Treatment. 1999;2 np. [Google Scholar]
- Stice E, Barrera M, Jr., Chassin L. Prospective differential prediction of adolescent alcohol use and problem use: Examining mechanisms of effect. Journal of Abnormal Psychology. 1998;107:616–628. doi: 10.1037//0021-843x.107.4.616. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti N, Shaw H, O’Neil K. General and program-specific moderators of two eating disorder prevention programs. International Journal of Eating Disorders. 2008a;41:611–617. doi: 10.1002/eat.20524. [DOI] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau JM, Wade E. Efficacy trial of a brief cognitive-behavioral depression prevention program for high-risk adolescents: Effects at 1- and 2-year follow-up. Journal of Consulting and Clinical Psychology. 2010a doi: 10.1037/a0020544. doi: 10.1037/a0020544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Seeley J, Gau J. Brief cognitive-behavioral depression prevention program for high-risk adolescents outperforms two alternative interventions: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008b;76:595–606. doi: 10.1037/a0012645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Seeley J, Gau J. Testing mediators of intervention effects in randomized controlled trials: An evaluation of three depression prevention programs. Journal of Consulting and Clinical Psychology. 2010b;78:273–280. doi: 10.1037/a0018396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology. 2009;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tram JM, Cole DA. Self-perceived competence and the relation between life events and depressive symptoms in adolescence: Mediator or moderator? Journal of Abnormal Psychology. 2000;109:753–760. doi: 10.1037//0021-843x.109.4.753. [DOI] [PubMed] [Google Scholar]
- Turner JR, Lloyd DA. Stress burden and the lifetime incidence of psychiatric disorder in young adults. Archives of General Psychiatry. 2004;61:481–488. doi: 10.1001/archpsyc.61.5.481. [DOI] [PubMed] [Google Scholar]