Abstract
Objective:
Despite evidence that screening for breast cancer is effective, adherence with screening recommendations in Iranian women is low. The purposes of this study were to (1) identify the associations between individual characteristics, related health beliefs, and stages of mammography behavior and (2) examine the socio-demographic factors and the health beliefs that predicate stages of mammography behavior.
Design:
All health care centers were considered as clusters and 30 women were randomly selected from each of them. A sample of 689 Iranian women completed a questionnaire.
Materials and Methods:
The questionnaire used was based on Champion's revised Health Belief Model Scale (CHBMS). One-way analysis of covariance (ANCOVA) was used to assess differences in the outcome variables (perceived severity, susceptibility, benefits, and barriers) across the stages. Multinomial logistic regression was conducted to test multivariate relationships.
Results:
The percentage of participants in each stage was: 40.1% in pre-contemplation, 34.7 in contemplation, 7.5% in relapse, 12% in action, and 5.7% in maintenance stage of mammography adoption. Older women were most likely to be in the pre-contemplation stage and action stage, and the youngest women were most likely to be in the relapse stage. Differences across stages of change were found for related beliefs for all participants except those in the relapse stage.
Conclusion:
Iranian women are less likely to be in maintenance and action stages than ot er Asian women and this study identifies constructs that may be targeted in interventions.
Keywords: Breast cancer, Iranian women, stages of mammography behavior
INTRODUCTION
Breast cancer is the most common cancer in women worldwide.[1] Because of the lack of formal cancer registration in Iran, there are no valid and reliable statistics about the incidence and mortality from breast cancer. However, informal statistics show the incidence rate is about 24 and prevalence rate 120 per 100,000 women per year.[2] Considering the population of 35 million women in Iran, 8400 new cases of breast cancer are expected each year.
Incidence and mortality rate from breast cancer vary in different populations. It is realized that factors like age, race, ethnicity, and socioeconomic status can influence the incidence and mortality.[3–5] One of the most basic factors that can affect mortality from breast cancer is the stage of cancer disease that women are in when they present for medical care. Results of a study in Iran showed that among 1500 women, 78.3% were at stage 2 or more at the first visit, which means they had at least one involved lymph node. The most common reason that brought patients under medical attention was masses discovered in the breast.[6] Another study found that among 2946 females with breast cancer, 76.8% were T2 or higher and 65.3% had positive lymph nodes and were in the last phase.[7] These findings indicate the vast majority of breast cancer patients in Iran are diagnosed in advanced stages of the disease.
While the chance of developing breast cancer increases as a woman gets older in western countries,[8] Raafat's study revealed the mean age of Iranian patients was about 49 years and 15% were under 40 years.[6] Mean age at the time of disease emergence in Iran is lower than in western countries.[9,10] This low age presentation of breast cancer among Iranian women is likely related to race or low age at menarche[11] and having an overall younger population than in developed countries.
It is possible to reduce breast cancer mortality. Breast cancer survival varies by the stage at diagnosis; the later the stage of the disease at diagnosis, the lower the survival rate. Because of improvements in treatment, more women with breast cancer have been cured[12] and the number of women dying due to breast cancer is decreasing.[13] However, many Iranian women with breast cancer delay their first visit to a medical professional.[6,7,14] There is also lower compliance among Iranian women for regular breast cancer testing and a lack of specific national breast cancer screening programs. All of these factors result in often late breast cancer detection and subsequent increased mortality rate in this population. It is therefore necessary to create interventions aimed at increasing adherence to breast cancer screening among Iranian women.
When undertaking breast cancer screening behaviors, it is important that theoretically based factors are employed to maximize the impact of the intervention. The Health Belief Model (HBM)[15,16] has been used to explain factors influencing breast cancer screening behaviors and to plan and implement breast cancer screening programs in various populations.[4,17–19] The HBM is based on the theory that a person's willingness to change a health behavior is primarily due to the following factors: (1) perceived susceptibility (i.e., women's opinion of the chances of getting breast cancer), (2) perceived severity (i.e., a person's opinion of the seriousness of the condition), (3) perceived benefits (i.e., the opinion of the effectiveness of some advised action to reduce the risk, such as mammography), and (4) perceived barriers to having a mammography.
Another model that can be applied to this research area is the Stage of Change Model (SCM) which includes the stages of change that a person moves through when adopting a behavior. The SCM framework proposes that individuals move through a temporal sequence of five stages: Pre-contemplation (never having a mammogram and not planning to get one within the next 1–2 years), contemplation (never having a mammogram but intends to get one within the next 1–2 years), action (having one mammogram on schedule and intends to get another on schedule), maintenance (having at least two mammograms and intends to get another on schedule), and relapse (having one or more mammograms but is now off schedule and does not plan to have a mammogram in the next 1–2 years).[20] Many researchers have applied the SCM to identify and promote breast cancer screening.[21–25]
Although both these models offer unique theoretical strengths for studying breast cancer screening behaviors, few researchers have conducted theoretically based studies of Iranian women's participation in breast cancer screening behaviors such as mammography. Therefore, the aims of the current study were to use HBM and SCM constructs to examine: 1) associations between individual characteristics and stages of mammography behavior; 2) relationships between the related beliefs (perceived susceptibility, severity, benefits and barriers) while controlling for socio-demographic factors and stages of mammography behavior associations; and 3) socio-demographic factors and the health beliefs that predict stages of mammography behavior among a cluster random sample of Iranian women.
We hypothesized that 1) there will be significant socio-demographic and belief differences in the women in each of the SCM stages related to mammography and 2) the socio-demographic factors will predict stages of mammography behavior.
MATERIALS AND METHODS
Participants
Participants were from Sanandaj, Iran, which is a city with diverse socioeconomic status with 28 primary health care centers. All health care centers were considered as clusters and 30 women were randomly selected from each. Information letters were sent to women up to 40 years or older than 40. If they were interested in participating, they were asked to sign an enclosed consent form and return it to the study investigators. A total of 810 women had agreed to participate and a questionnaire was sent to them. Inclusion criteria were: Not having breast cancer and not breastfeeding or pregnant. Seventy-five women were excluded because they did not meet these criteria. Of these 712 participants, 23 cases with incomplete or missing data were deleted, yielding a final sample size of 689. The Ethical Committee of Kurdistan Medical University approved the study.
Measures
The socio-demographic items included in the survey were age, marital status, employment status, educational status, family history of breast cancer, and health insurance.
The questionnaire used in the current study was based on Champion's revised Health Belief Model Scale (CHBMS). The CHBMS was tested in a previous study to assess perceived severity and susceptibility to mammography, with the Cronbach's alpha reliability coefficients 0.82 and 0.84, respectively, in Iranian women. Further, the Cronbach's alpha coefficients were 0.72 and 0.73 for the perceived benefits and barriers, respectively.[19]
Belief statements were rated on a 5-point scale (1=not at all sure to 5=very true) and scored by calculating the means of all item scores. Perceived benefits of mammography are defined as positive or reinforcing aspects of getting mammography and were measured on 6-items scale. Perceived barriers refer to real or imagined impediments that prevent, or make participation in mammography difficult and were measured by a 10-item instrument. Perceived severity is beliefs about the seriousness of a condition and its consequences. The participants were asked to respond to a 7-item scale to measure this concept. Perceived susceptibility reflects individuals’ feeling of personal vulnerability to chances of a specific health problem. This was assessed using a 4-item scale.
Stage of mammography (SOM) adoption was assessed by an adapted measure recommended by Rakowski et al.[20,26] The test–retest reliability of the staging algorithm in the current study within a 2-week interval was 0.94 (n=48).
The women were classified based on frequency and regularity of current screening behavior and future intention to get mammography as follows:
Pre-contemplation: Never had a mammogram and not planning to get one within the next 1–2 years.
Contemplation: Never had a mammogram but intends to get one within the next 1–2 years.
Action: Had one mammogram on schedule and intends to get another on a time frame that will keep the women on schedule.
Maintenance: Had at least two mammograms on schedule and intends to get another on a time frame that will keep the women on schedule.
Relapse: Had one or more mammograms in the past but is now off schedule and does not plan to have a mammogram within 1–2 years.
Data analysis
The Statistical Package for the Social Sciences (SPSS) Version 16 was used for all statistical analyses. In order to test hypothesis 1, Chi-square tests were used to examine associations between stage of mammography adoption and socio-demographic factors. One-way analysis of covariance (ANCOVA) which considered socio-demographic variables as covariates was used to assess differences in the outcome variables (perceived severity, susceptibility, benefits, and barriers) across the stages with Tukey–Kramer tests to identify the stage differences of the outcome variables. To test multivariate relationships, multinomial logistic regression was conducted. We used the pre-contemplation stage as the reference group to compare separately with contemplation, relapse, action, and maintenance stages. Outcome variables and socio-demographic factors were entered independently into the multinomial logistic regression.
RESULTS
Participants had a mean age of 55.72 (SD=7.42) years (range=40–72 years); 46.9% were single and 53.1% were married (divorced or common-law is not an option in Iran); 53.6% did not work outside of the home; 48.2% had less than a high school education, 32.7% had a high school education, and 19.2% had attended university. In terms of income, 10.45% perceived their income as bad or very bad, 23.8% as middle, and 65.75% as good or very good. 94.8% of the participants reported no history of family breast cancer and 18.4% were uninsured.
Among the 689 participants, 40.1% were in pre-contemplation stage, 34.7% in contemplation, 7.5% in relapse, 12% in action, and 5.7% in maintenance stage of mammography adoption. The distribution of the participants’ characteristics across the stages is outlined in Table 1. Age groups, marital status, and health insurance were significantly associated with the stage of adoption (P<0.001). There were more number of older women in the pre-contemplation stage (44.5%) and action stage (16.7%) compared with those in the other age groups. The middle-aged (50–59) women were more than the other two age groups in the maintenance stage (9.4%). The youngest women were most likely to be in the relapse stage (19%).
Table 1.
Bivariate relationships between participants’ socio-demographic factors and stage of mammography
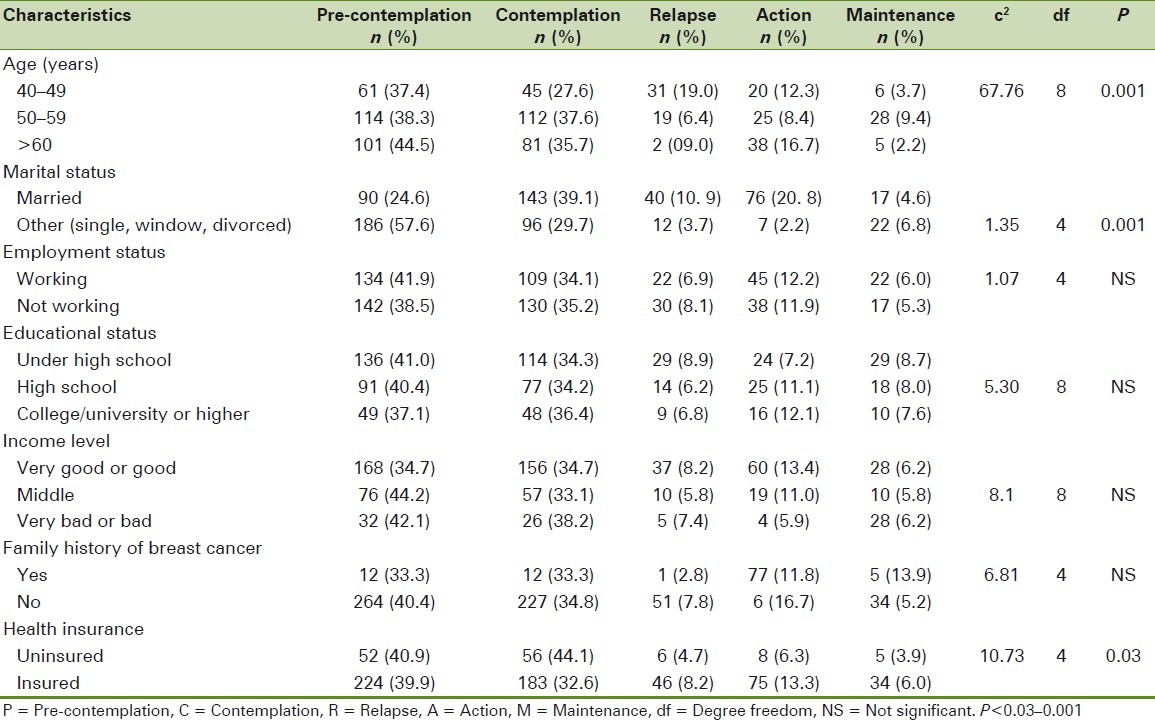
Married women were more likely to be in the action stage compared to single women. Fewer health uninsured women were found to be in action and maintenance stages. Results did not show significant associations between the stages for other demographic factors.
Because age, marital status, and health insurance were significantly associated with the stage of mammography adoption, these variables were included as covariates in the ANCOVA. Differences between stages of adoption were found for all psychosocial factors (all P<0.001). The results of the ANCOVA are presented in Table 2. As hypothesized, among the health beliefs variables, perceived susceptibility, severity, and benefits were positively associated with the stage of adoption while perceived barriers were negatively associated with the stage of adoption. Perceived susceptibility scores were higher in maintenance and relapse stages. Those in action and relapse stages had higher adjusted means for perceived benefits. It was found that the women in the relapse group had the lowest scores for perceived barriers, followed by the women in the maintenance group.
Table 2.
Adjusted marginal means (SD) on perceived benefits, barriers, susceptibility, and severity for the five stages of mammography
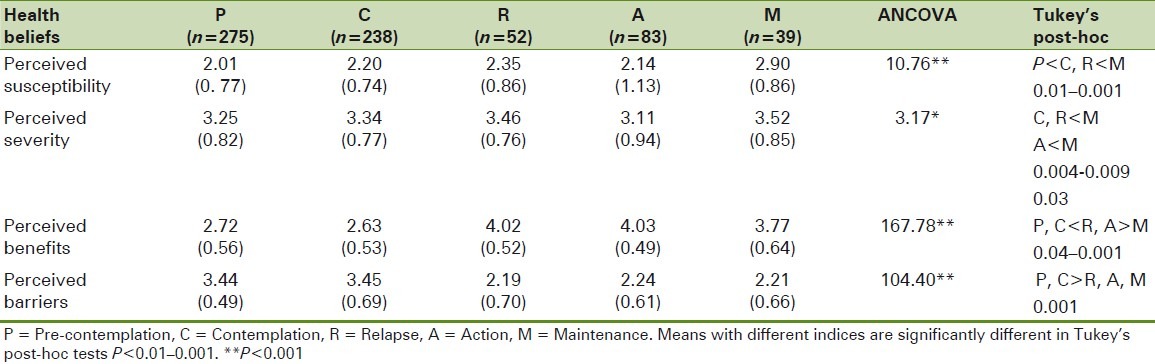
In addition, the relationships between demographic factors as covariates and health beliefs were examined. Health insurance was associated with higher perceived susceptibility, greater benefits, and lower barriers (P<0.03–0.001). Age and marital status were associated with higher perceived benefits, greater susceptibility, and fewer perceived barriers (P<0.01–0.001). Significant relationships were not seen between the health beliefs and the covariate factors.
Multiple regression analysis
Results of the multinomial logistic regression and pair-wise comparison across stages of mammography adoption on socio-demographic variables and the health beliefs are reported in Tables 3 and 4, respectively. Women were more likely to be in the maintenance stage than in the pre-adoption stage if they were in the middle age group (50–59 years) [OR=4.96, 95% confidence interval (CI)=1.85–13.33], than in the youngest age group (OR=1.98, 95% CI=0.56–6.80). The younger women (<50 years) compared to older women were about 26 times more likely to be in the relapse stage and the odds for middle age were about 9 times compared to women more than 60 years old. Married women had higher odds of being in the action group than in the pre-contemplation stage compared with single women (96% vs. 0.4%), although the odds of being in the maintenance stage were lower for married women (37% vs. 63%). No significant differences were found across the stages of mammography adoption on employment status, education level, income level, family history of breast cancer, and health insurance except for those women with a family history of breast cancer, who were more likely in the maintenance than in the pre-contemplation stage (99%) compared with those not having this family history.
Table 3.
Odds of being in stage of mammography screening by socio-demographic factors
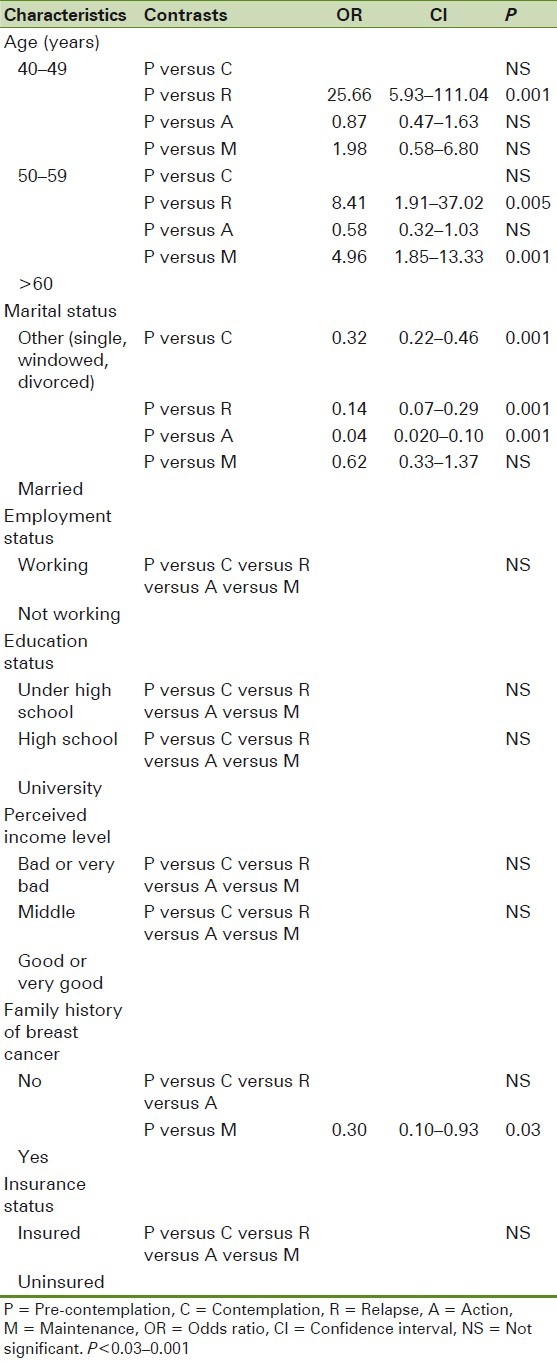
Table 4.
Odds of being in stage of mammography screening by health beliefs
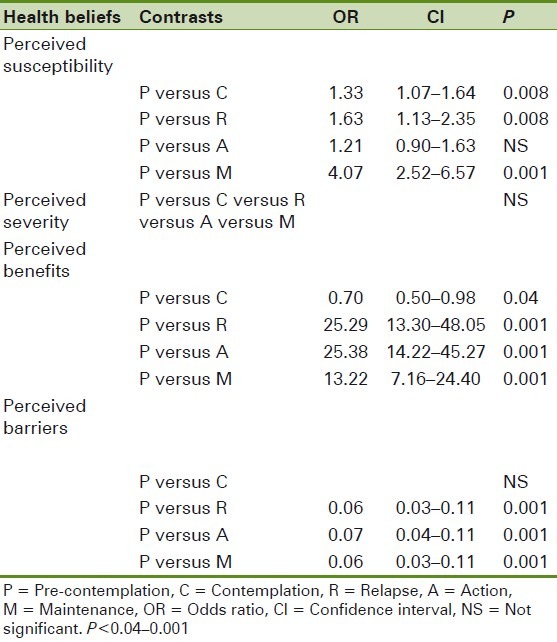
Among the health beliefs examined, all were significantly different between stages (P<0.04–0.001). Those who were in relapse, action, and maintenance stages had higher perceived benefits and susceptibility scores than those in pre-adoption stages. Women in pre-adoption stages were 4 times in maintenance stage if they had lower perceived susceptibility (P<0.001).
Women in maintenance, action, and relapse stages had lower barriers to mammography and were less likely to be in pre-contemplation stage. Interestingly, the odds of being in adoption stages (action and maintenance) were no different than of women being in the relapse stage (OR=0.06). It means the odds of being in adoption or relapse stages compared to being in pre-adoption stages (pre-contemplation, contemplation) were higher for women with fewer barriers compared with those who had higher barriers to mammogram.
DISCUSSION
Among the 689 participants, 75% were in pre-contemplation and contemplation stages of mammography adoption compared with only 17.5% in action and maintenance stages, leaving 7.5% in the relapse stage. The low rate of mammography adoption behavior is consistent with previous research with Iranian women. Aalvi found that even among female Iranian gynecologists, only 27% had regularly mammogram testing. Another study showed 12% of women had gotten a mammogram within the previous 3 years.[19] Low adherence to recommended screening behaviors has similarly been demonstrated in Iranian women.[27] When compared to other studies, Iranian women were found to be less likely to be in maintenance and action stages than Asian American, Indian and Filipino,[25] Cambodian,[22] Chinese,[23] or Chinese and Filipino[28] women. This likely reflects greater acculturation to regular -mammography -testing than is found among Iranian women.
We found that the stage distribution varied by age, marital status, and health insurance coverage. The largest group in the pre-contemplation stage was the oldest women, which is likely to be due to cultural beliefs like not needing a routine mammogram done if one is old and related health beliefs to getting a mammogram done. Although older women were the most likely to be in the action stage, they also formed the lowest numbers in the maintenance stage. The odds of being in the maintenance stage were more likely in the middle age, followed by the youngest women (OR=4.96 and 1.96, respectively). These findings could help with the creation of interventions tailored to encourage older women to progress toward maintenance stage. The normative belief among Iranians is that older women should spend more time on family issues rather than on themselves. So, it would be helpful if other family members, such as husbands, were informed about the risk of developing breast cancer and the importance of regular mammogram screening to detect early diagnosis.
Our results are similar to those reported for Cambodian, Korean, Chinese, Filipino American,[22,28] and Swiss women,[29] but inconsistent with studies on Chinese[23] and Korean immigrants[21] who were not found to differ across stages by marital status. Considering the high percent of married women in the action stage, our results again suggest that spouses may be a useful source of social support. The number of married women in the action stage dropped from 21 to 5% in the maintenance stage. There is a need to motivate married women and their family members to adhere to regular mammography.
Women with a history of breast cancer in their families compared to those without such history were more likely to be in the maintenance stage than in the pre-contemplation stage. However, sometimes family history can create fear and apprehension to impede getting a mammogram done and it can become a barrier rather than a facilitator, although our findings do not support this idea. There is a need to further explore the cultural beliefs to find out why despite the positive perceived outcomes when breast cancer is diagnosed in an early stage, having a history becomes a barrier in some women.
Unlike other findings, health insurance did not predict the stage of adoption for mammography.[22–23,28] These results may be related to the difference in insurance coverage in Iran compared to other countries. There are several different types of insurance in Iran that provide rather similar services, so we integrated them into one category. Further, even with insurance coverage, one must pay a high cost to visit a physician, so this issue may influence regular physician visits which will subsequently result in not receiving a physician's recommendation for regular mammography. In addition, insurance pays only a small part of mammography costs, so there is not a salient difference between insured and uninsured women in this regard.
The results proved our hypothesis that health beliefs will be related to the stage of adoption of mammography. The HBM suggests that greater perceived threat results in more -preventive behaviors. Women in more advanced stages of change reported higher perceived susceptibility. For women in the relapse stage, it seems that they retained their beliefs regarding mammography but did not act accordingly. SCM theory posits a cycle between pre-contemplation and maintenance stages. It is not clear if when one recycles to pre-adoption stages, beliefs undergo salient changes such as decreasing perceived threats and increasing barriers or if there are other factors influencing the health behaviors.
Contrary to results from previous studies conducted in rural Korea[30] and on Korean immigrants to the USA[21] which reported that perceived susceptibility predicted the stage of mammography or recent mammogram, our findings were more similar to those of Kathleen that there is not greater likelihood of being in action than in relapse stage due to perceived susceptibility.[3]
It must be noted that perceived threat about developing breast cancer is an overall concept while risk appraisal goes beyond the perceived threat.[31] This may be a reason for there not being different perceived severity for women in the different stages. There is a need to further explore the risk appraisal according to normative beliefs, characteristic culture, socio-demographic status, and access to effective screening and treatment services related to breast cancer among Iranian women.
HBM and SCM postulate that people will take action for healthy behavior if they believe in the efficacy of action and if the barriers are outweighed by perceived positive outcomes.[15,32] Contrary to these hypotheses, our results did not show any significant differences between those who were in relapse and action stages given perceived benefits, but differed between pre-adoption and adoption stages as reported by other researchers.[17,28,33–35] The women in the maintenance stage even had lower benefits than those in the relapse and action stages. According to SCM, all beliefs will not differ by stage,[36] as supported by our results; women in the relapse stage reported the highest perceived benefits to getting a mammogram done than the women in all other stages. There is the possibility that despite someone not acting on a recommended health behavior, they still may acknowledge and express the benefits of that behavior. The odds were greater in the adoption than in the pre-adoption stages when adding the perceived benefits, as reported in other studies.[23,28,33]
Women in the relapse stage had the lowest barriers compared to those who were in action and maintenance stages. The prior experiences with getting a mammogram done may have influenced the current and future intentions and attitudes related to breast cancer screening.[21] It may be that women in the relapse stage experienced some barriers like pain, embarrassment, or fear. These feelings may have been normalized explaining why women in the relapse stage had lower perceived barriers than those in the adoption stages. Except those who were in the relapse stage, there were important differences between pre-contemplators and those in the adoption stages related to perceived barriers to getting a mammogram done. Similar to other findings,[3,23,24,28,33] our results revealed that when stages progress from early to advanced, perceived barriers decreased.
The findings of the current study indicate that women in the relapse stage reported the highest perceived benefits, rather higher perceived susceptibility, severity, and the lowest barriers. It is a unique finding that needs further research to detect the other factors that may impact having a regular mammogram. For example, interpersonal influences including social support, exposure to models, and interpersonal norms are likely to be important correlates, particularly within the Iranian cultural context. It must be realized which specific changes at an item level regarding perceived beliefs predict progress across stages.[24] For example, if a woman in the pre-adoption stages declares that getting a mammogram done is painful, it means this belief is influenced by vicarious learning rather than her own prior experience. Exploring item-level beliefs would help to plan and conduct effective interventions tailored to the stage of mammography adoption.
CONCLUSION
This study provides the first test of the associations between stages of mammography adoption based on SCM combined with selected aspects of the HPM among Iranian women. Results indicate differences across stages of change were found for related beliefs, and also for current and future intentions for all participants, except for those in the relapse stage. Thus, Iranian women in the relapse stage of mammography do not significantly differ in beliefs, but in their intention to getting a mammogram done compared to women in the action and maintenance stages. This finding requires further exploration.
Given the lack of population-based mammography and clinical breast exam screening programs, the rate of relapse as well as the low adherence to regular screening behavior for breast cancer among the women in this sample and other Iranian women, there is a need to conduct further research in theoretically based interventions designed to decrease relapse, especially in younger Iranian women. If the intervention programs achieve success to keep the same number in the adoption stages and prevent relapse, it is worth it. Further, it is important to understand why older women are less likely to maintain the behavior. It is important that the distinction between perceived related beliefs to mammography according to age is better understood. Therefore, intervention programs aimed at increasing mammogram behavior must be tailored to the stage of change, age, and other socioeconomic factors.
ACKNOWLEDGMENT
We would like to thank Deputy of Research and Technology of Kurdistan University of Medical Sciences for providing financial support for this study.
Footnotes
Source of Support: Deputy of Research and Technology of Kurdistan University of Medical Sciences.
Conflict of Interest: None declared
REFERENCES
- 1.Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, et al. Major depression after breast cancer: A review of epidemiology and treatment. Gen Hosp Psychiatry. 2008;30:112–26. doi: 10.1016/j.genhosppsych.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 2.Mousavi SM, Montazeri A, Mohagheghi MA, Jarrahi AM, Harirchi I, Najafi M, et al. Breast cancer in Iran: An epidemiological review. Breast J. 2007;13:383–91. doi: 10.1111/j.1524-4741.2007.00446.x. [DOI] [PubMed] [Google Scholar]
- 3.Russell KM, Monahan P, Wagle A, Champion V. Differences in health and cultural beliefs by stage of mammography screening adoption in African American women. Cancer. 2007;109(2 Suppl):386–95. doi: 10.1002/cncr.22359. [DOI] [PubMed] [Google Scholar]
- 4.Allahverdipour H, Asghari-Jafarabadi M, Emami A. Breast cancer risk perception, benefits of and barriers to mammography adherence among a group of Iranian women. Women Health. 2011;51:204–19. doi: 10.1080/03630242.2011.564273. [DOI] [PubMed] [Google Scholar]
- 5.Coleman MP, Gatta G, Verdecchia A, Estève J, Sant M, Storm H, et al. EUROCARE-3 summary: Cancer survival in Europe at the end of the 20th century. Ann Oncol. 2003;14(Suppl 5):v128–49. doi: 10.1093/annonc/mdg756. [DOI] [PubMed] [Google Scholar]
- 6.Raafat J, Atri M. Demographic characteristics and clinical tableau of 1500 cases of breast cancer in Iranian Women. Iran J Surg. 2010;18:85–90. [Google Scholar]
- 7.Harichi I, Kolahdoozan S, Karbakhsh M, Chegini N, Mohseni SM, Montazeri A, et al. Twenty years of breast cancer in Iran: Downstaging without a formal screening porgram. Ann Oncol. 2011;22:93–7. doi: 10.1093/annonc/mdq303. [DOI] [PubMed] [Google Scholar]
- 8.Yip CH. Breast cancer in Asia. Methods Mol Biol. 2009;471:51–64. doi: 10.1007/978-1-59745-416-2_3. [DOI] [PubMed] [Google Scholar]
- 9.Kolahdoozan S, Sadjadi A, Radmard AR, Khademi H. Five common cancers in Iran. Arch Iran Med. 2010;13:143–6. [PubMed] [Google Scholar]
- 10.Heydari ST, Mehrabani D, Tabei SZ, Azarpira N, Vakili MA. Survival of Breast Cancer in Southern Iran. Iran J Cancer Prev. 2009;2:51–4. [Google Scholar]
- 11.Tehranian N, Shobeiri F, Pour FH, Hagizadeh E. Risk Factors for Breast Cancer in Iranian Women Aged Less than 40 Years. Asian Pac J Cancer Prev. 2010;11:1723–5. [PubMed] [Google Scholar]
- 12.Kirshbaum M. Promoting physical exercise in breast cancer care. Nurs Stand. 2005;19:41–8. doi: 10.7748/ns2005.06.19.41.41.c3895. [DOI] [PubMed] [Google Scholar]
- 13.Wonghongkul T, Dechaprom N, Phumivichuvate L, Losawatkul S. Uncertainty appraisal coping and quality of life in breast cancer survivors. Cancer Nurs. 2006;29:250–7. doi: 10.1097/00002820-200605000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Harirchi I, Ghaemmaghami F, Karbakhsh M, Moghimi R, Mazaherie H. Patient delay in women presenting with advanced breast cancer: An Iranian study. Public Health. 2005;119:885–91. doi: 10.1016/j.puhe.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988;15:175–83. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 16.Rosenstock M. Why people use health services. Milbank Mem Fund Q. 1996;44(3):94–127. [PubMed] [Google Scholar]
- 17.Shirazi M, Champeau D, Talebi A. Predictors of breast cancer screening among immigrant Iranian women in California. Journal of Women's Health (Larchmt) 2006;15:485–506. doi: 10.1089/jwh.2006.15.485. [DOI] [PubMed] [Google Scholar]
- 18.Noroozi A, Jomand T, Tahmasebi R. Determinants of breast self-examination performance among Iranian Women: An application of the health belief model. J Cancer Educ. 2011;26:365–74. doi: 10.1007/s13187-010-0158-y. [DOI] [PubMed] [Google Scholar]
- 19.Taymoori P, Berry T. The validity and reliability of Champion's Health Belief Model Scale for breast cancer screening behaviors among Iranian women. Cancer Nurs. 2009;32:465–72. doi: 10.1097/NCC.0b013e3181aaf124. [DOI] [PubMed] [Google Scholar]
- 20.Rakowski W, Fulton JP, Feldman JP. Women's decision making about mammography: A replication of the relationship between stages of adoption and decisional balance. Health Psychol. 1993;12:209–14. doi: 10.1037//0278-6133.12.3.209. [DOI] [PubMed] [Google Scholar]
- 21.Lee H, Kim J, Han HR. Do cultural factors predict mammography behaviour among Korean immigrants in the USA? J Adv Nurs. 2009;65:2574–84. doi: 10.1111/j.1365-2648.2009.05155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tu SP, Yasui Y, Kuniyuki A, Schwartz SM, Jackson JC, Taylor VM. Breast cancer screening: Stages of adoption among Cambodian American women. Cancer Detect Prev. 2002;26:33–41. doi: 10.1016/S0361-090X(02)00013-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strong C, Liang W. Relationships between decisional balance and stage of adopting mammography and Pap testing among Chinese American women. Cancer Epidemiol. 2009;33:374–80. doi: 10.1016/j.canep.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu TY, Hsieh HF, West BT. Stages of mammography adoption in Asian American women. Health Educ Res. 2009;24:748–59. doi: 10.1093/her/cyp009. [DOI] [PubMed] [Google Scholar]
- 25.Wu TY, West BT. Mammography stage of adoption and decision balance among Asian Indian and Filipino American women. Cancer Nurs. 2007;30:390–8. doi: 10.1097/01.NCC.0000290812.14571.2c. [DOI] [PubMed] [Google Scholar]
- 26.Rakowski W, Clark MA, Pearlman DN, Ehrich B, Rimer BK, Goldstein MG, et al. Integrating pros and cons for mammography and Pap testing: Extending the construct of decisional balance to two behaviors. Prev Med. 1997;26:664–73. doi: 10.1006/pmed.1997.0188. [DOI] [PubMed] [Google Scholar]
- 27.Montazeri A, Vahdaninia M, Harirchi I, Harirchi AM, Sajadian A, Khaleghi F, et al. Breast cancer in Iran: Need for greater women awareness of warning signs and effective screening methods. Asia Pac Fam Med. 2008;7:6. doi: 10.1186/1447-056X-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Otero-Sabogal R, Stewart S, Shema SJ, Pasick RJ. Ethnic differences in decisional balance and stages of mammography adoption. Health Educ Behav. 2007;34:278–96. doi: 10.1177/1090198105277854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chamot E, Charvet AI, Perneger TV. Predicting stages of adoption of mammography screening in a general population. Eur J Cancer. 2001;37:1869–77. doi: 10.1016/s0959-8049(01)00234-9. [DOI] [PubMed] [Google Scholar]
- 30.Hur HK KG, Park SM. Predictors of mammography participation among rural Korean women age 40 and over. Taehan Kanho Hakhoe Chi. 2005;35:1443–50. doi: 10.4040/jkan.2005.35.8.1443. [DOI] [PubMed] [Google Scholar]
- 31.Wood RY, Della-Monica NR. Psychosocial factors influencing breast cancer risk appraisal among older women. Qual Health Res. 2011;21:783–95. doi: 10.1177/1049732311401036. [DOI] [PubMed] [Google Scholar]
- 32.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 33.Menon U, Champion V, Monahan PO, Daggy J, Hui S, Skinner CS. Health belief model variables as predictors of progression in stage of mammography adoption. Am J Health Promot. 2007;21:255–61. doi: 10.4278/0890-1171-21.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stewart SL, Rakowski W, Pasick RJ. Behavioral constructs and mammography in five ethnic groups. Health Educ Behav. 2009;36(5 Suppl):36S–54S. doi: 10.1177/1090198109338918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Champion VL. Revised susceptibility, benefits, and barriers scale for mammography screening. Res Nurs Health. 1999;22:341–8. doi: 10.1002/(sici)1098-240x(199908)22:4<341::aid-nur8>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 36.Glanz K, Rimer BK, Viswanath K. Health behavior and health education: Theory, Research, and Practice. In: Prochaska JO, Redding CA, Evers KE, editors. The trastheoretical model and stages of change. 4th ed. San Francisco: Jossey-Bass; 2008. pp. 97–117. [Google Scholar]


