Abstract
Background:
Effective cancer pain management requires accurate knowledge, attitudes, and assessment skills. The purpose of this study was to obtain information about the knowledge and attitudes of nurses concerning cancer pain management with the use Health Belief Model (HBM) as conceptual framework.
Materials and Methods:
The study was a descriptive survey and included 98 randomly selected nurses from Alzahra hospital, Isfahan, Iran. A self-administered questionnaire which was designed on the basis of HBM was used to collect the data. Knowledge, attitudes, and HBM constructs regarding cancer pain were the main research variables. The obtained data were analyzed by SPSS (version11.5) using descriptive statistics, independent t–test, and Pearson correlation at the significant level of α=0.05.
Results:
Ninety-eight nurses aged 38.7 ± 7.04 years were studied in this survey. From the 10 pain knowledge questions assessed, the mean number of correctly answered question was 61.2 (SD=16.5), with a range of 30–100. There was a direct correlation between knowledge and attitude of nurses with HBM constructs except for perceived barriers and perceived threat. Among the HBM constructs, the highest score was related to self-efficacy with mean score of 87.2 (SD=16.4).
Conclusions:
The findings support the concern of inadequate knowledge and attitudes in relation to cancer pain management. We believe that basic and continuing education programs may improve the knowledge level of nursing about pain management.
Keywords: Attitude, cancer, Health Belief Model, knowledge, nurse, pain management
INTRODUCTION
Pain is one of the most feared consequences of cancer experienced by patients. It has a profound impact on every aspect of quality of life and is thus the dominant cause of total suffering for cancer patients[1] even though pain relief is achievable in more than 90% of the cases.[2] Inadequate pain relief in practice is well documented and can involve up to 40% of patients.[3] Nurses have a key role in effective pain management; therefore, nurses’ knowledge is of critical importance in the care of patients with cancer pain.[4–6] The nurse's accurate assessment, prompt intervention, and adequate evaluation of pain relief measures are necessary for better clinical outcomes.[7] However, nurses may not be prepared to assume a critical role because their lack of knowledge and individual attitudes on pain can interfere with their ability to effectively manage pain.[8,9] Several explanations have been offered for nurses’ inadequate knowledge and attitudes about pain management. The most common explanation is that nurses receive too little pain management education in their nursing curricula.[10] The majority of studies determined that nurses answered less than 70% of questions correctly, indicating that many nurses continue to lack sufficient knowledge regarding appropriate pain management.[11] One of the most important deficiencies of nurses about cancer pain assessment is that their assessment often focuses on patients’ behaviors rather than pain intensity and other descriptive characteristics of pain.[12] As a result, most nurses have overestimated the percentage of patients who over-report their pain.[13,14] It has been reported that opioid knowledge of nurses who cared for patients with cancer was generally weak.[15] Nurses also were unaware that a common side effect of opioid analgesics, constipation, does not decrease over time.[16] In addition, many nurses do not know that the incidence of psychologic dependence in patients with cancer is less than 1 in 1000 patients.[14,17] Many studies have also demonstrated that negative nursing attitudes create barriers to effective cancer pain management.[18,19] Howell et al., found that nurses believed that their patients should experience pain first before being given pain medication.[9] Visentin et al., in their study affirmed that nurses have poor knowledge and negative attitudes toward the approach and treatment of patients in pain.[20]
Health belief model
The Health Belief Model (HBM) is a psychological model that attempts to explain and predict health behaviors. This is done by focusing on the attitudes and beliefs of individuals. The HBM was spelled out in terms of four constructs representing the perceived threat and net benefits: Perceived susceptibility, perceived severity, perceived benefits, and perceived barriers. These concepts were proposed as accounting for people's “readiness to act.”[21]
The purpose of this study was to identify the level of knowledge, attitude, and HBM constructs among Aalzahra hospital nurses regarding the management of cancer pain.
MATERIALS AND METHODS
In this cross-sectional study, 98 randomly selected nurses, who were employed in Alzahra educational hospital in Isfahan, Iran, were enrolled in the study. All nurses agreed to participate in the study and therefore they did sign the consent form. Data were gathered with a self-administered questionnaire. Content and construct validity of the questionnaire was revised by a group of specialists in the field of health education, anesthesiology, and oncology. Reliability analysis was conducted for testing the reliability of knowledge and HBM constructs. Internal consistency of these sections of the questionnaire was calculated using Cronbach's alpha technique (0.82 for knowledge, 0.79 for attitude, 0.75 for perceive benefits, 0.68 for perceived barriers, 0.72 for perceived threat, 0.74 for self-efficacy, and 0.85 for cues to action). The questionnaire contained two sections: (a) socio-demographic characteristics of nurses (such as sex, education, marital status) and (b) knowledge and HBM constructs. To assess the knowledge of nurses regarding cancer pain management, there were 10 questions with yes/no response options. Each correct answer was given a score of 1 and each wrong answer a score of 0. HBM constructs section consisted of attitude (10 items), perceived benefits (5 items), perceived barriers (5 items), perceived threat (5 items), self-efficacy (5 items), and cues to action (5 items). For scoring this section of questionnaire, 5-point Likert scale (0=strongly disagree, 1=disagree, 2=no opinion, 3=agree, and 4=strongly agree) was used. For negative questions, reverse scoring was done. After completion of the questionnaire by the nurses, the obtained data were analyzed by SPSS (version 11.5, Chicago, IL, USA) using statistical tests (descriptive, Pearson correlation, independent t-test) at the significance level of α=0.05.
RESULTS
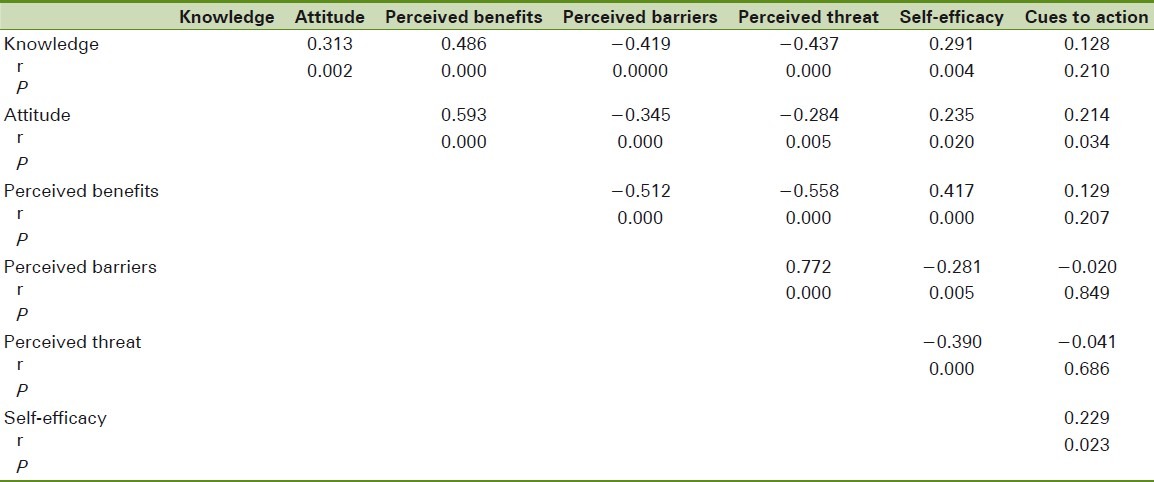
The demographic characteristics of the 98 nurses who responded to the questionnaire are presented in Table 1. As shown in the table, of the 98 nurses participating in the study, 81.6% were females, 67.3% were married, 80.6% had Bachelors degree, and 68.4% had moderate income. The majority of nurses had insufficient knowledge and attitude regarding cancer pain management. Among the HBM constructs, perceived barriers and perceived threat were in low range. The nurses also reported high self-efficacy in cancer pain management [Table 2]. Pearson correlation test showed that the knowledge of the nurses had a direct relationship with their attitude, perceived benefits, self-efficacy, and cues to action. But knowledge had reverse relationship with perceived barriers and perceived threat. The same test (Pearson correlation) also indicated that nurses’ attitude regarding cancer pain management had a direct relationship with perceived benefits, self-efficacy, and cues to action, but had reverse relationship with perceived barriers and perceived threat [Table 3]. Independent t-test showed that the mean scores of model variables in the two sexes had no significant difference (P>0.05). In other words, no relationship was observed between the two sexes and the mean score of HBM variables. Pearson correlation indicated that there was no significant relationship of age and work experience with the score of model variables (P>0.05).
Table 1.
Demographic characteristics of the nurses participating in the study
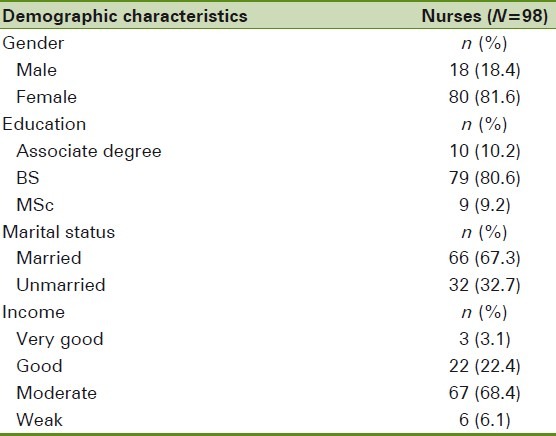
Table 2.
Mean (SD) of the knowledge, attitude, and HBM constructs of nurses regarding cancer pain management
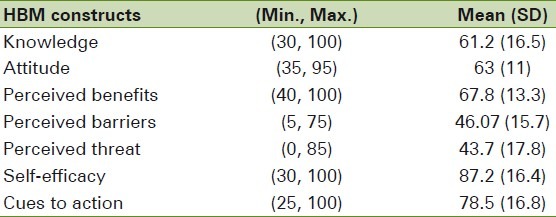
Table 3.
Pearson correlation coefficient between knowledge, attitude and HBM constructs
DISCUSSION
This study provides important information about the level of nurses’ pain knowledge and attitude in Isfahan, Iran. The findings showed that on average, the nurses included in this study showed low scores on knowledge and attitudes regarding cancer pain management. In other words, these results demonstrated that the nurses’ knowledge and attitude about cancer pain management is far from optimal. Regarding knowledge section, the mean score for correctly answered items was 61.2. Some other studies like those of Bernardi et al. and Yildirim et al. also reported insufficient nurses’ knowledge toward cancer pain management.[12,22] Inadequacy of health care professionals’ knowledge and education has been proposed as one of the major factors contributing to inadequate pain relief in cancer patients worldwide.[23] It is also well documented that there is a lack of professional health care education about pain management, which has resulted in less than optimal pain management for cancer patients.[24] One of the important knowledge questions was related to addiction to opioid. An earlier survey has shown that an addiction to opioid is observed in less than 1% of cancer patients.[25] In this study, only 12.4% of nurses correctly identified that less than 1% of patients who receive opioids for pain relief will develop addiction and 87.6% erroneously believed that addiction will occur in patients. Compared with the nurses in Western countries,[12,14,26] more nurses in this study were concerned about addiction. Our study's results revealed that among the HBM constructs, the highest mean score was related to self-efficacy. In other words, the participating nurses believed that they had enough ability to manage cancer pain issues such as emotional relationship with patients, to use the needed dose of opioid, and to give relevant information to the patient and his/her caregivers. This finding contradicts the results of Wells-Federman et al.'s study which had reported low self-efficacy among nurses regarding cancer pain management.[27] We considered that, this difference may arise from work experience of our study subjects who have long-term clinical experiences. Regarding cues to action , results of this study indicate that 78.5% of nurses agreed with the important role of seminars and workshops to increase their knowledge toward cancer pain management. In Mamishi et al.'s study, the most important source of information from nurses’ viewpoint was university curriculum.[28] In our study, there was direct correlation between knowledge and other HBM constructs except for perceived barriers and perceived threat. It means with increasing knowledge of nurses, their perceived barriers and perceived threat regarding cancer pain management have been decreased. There was also a reverse correlation between nurse's self-efficacy and their perceived barriers and perceived threat. This finding is in accordance with earlier findings in this regard.[29–31] The present study provides important information about nurse's knowledge and attitude deficits in pain management of cancer patients. Pain is a neglected topic in nursing educational programs. When major medical and nursing textbooks published worldwide are examined, it is seen that pain makes up a small part of the content. In a study by Ferrell et al. in 2000, it was observed that pain-related issues and pain management were addressed in only 284 of 45,683 pages in nurses’ textbooks.[32] Additionally, it is reported that baccalaureate nursing programs allocate little time to pain management.[33,34]
Limitations
There are some limitations of the present study. First, the sample size was relatively small and may not represent all nurses in Isfahan. Additionally, the study sample was taken from a university hospital, so it cannot necessarily be generalized to other staff populations.
CONCLUSION
The deficits in knowledge and attitude identified in this survey are a significant barrier to the effective management of pain in cancer patients. We believe that pain management issues in master nursing programs in Iran are insufficient as well. National and local course programs about pain management are also insufficient, although remedial interventions such as rearing palliative care nurses to improve the standard of clinical practice are currently being implemented and the impact on knowledge and outcomes of these interventions will be the subject of future studies in a countrywide continual quality improvement project.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Kuppelomaki M, Lauri S. Cancer patients’ reported experiences of suffering. Clin J Oncol Nurs. 2000;4:45–6. [PubMed] [Google Scholar]
- 2.Geneva: World Health Organization; 1996. WHO. Cancer pain relief: With a guide to opioid availability. [Google Scholar]
- 3.Cohen MZ, Easley MK, Ellis C, Hughes B, Ownby K, Rashad BG, et al. Cancer pain management and the JCAHO's pain standards: An institutional challenge. J Pain Symptom Manage. 2003;25:519–27. doi: 10.1016/s0885-3924(03)00068-x. [DOI] [PubMed] [Google Scholar]
- 4.de Rond ME, de Wit R, van Dam FS, van Campen BT, den Hartog YM, Klievink RM. A pain monitoring program for nurses: Effects on nurses’ pain knowledge and attitude. J Pain Symptom Manage. 2000;19:457–67. doi: 10.1016/s0885-3924(00)00128-7. [DOI] [PubMed] [Google Scholar]
- 5.Spross JA, McGuire DB, Schmitt RM. Oncology Nursing Society position paper on cancer pain. Oncol Nurs Forum. 1990;17:825. [PubMed] [Google Scholar]
- 6.Ferrell BR, McCaffery M. Nurses’ knowledge about equianalgesia and opioid dosing. Cancer Nurs. 1997;20:201–12. doi: 10.1097/00002820-199706000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Plaisance L, Logan C. Nursing students’ knowledge and attitudes regarding pain. Pain Manag Nurs. 2006;7:167–75. doi: 10.1016/j.pmn.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Max MB. Improving outcomes of analgesic treatment: Is education enough? Ann Intern Med. 1990;113:885–9. doi: 10.7326/0003-4819-113-11-885. [DOI] [PubMed] [Google Scholar]
- 9.Howell D, Butler L, Vincent L, Watt-Watson J, Stearns N. Influencing nurses’ knowledge, attitudes, and practice in cancer pain management. Cancer Nurs. 2000;23:55–63. doi: 10.1097/00002820-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 10.McMillan SC, Tittle M, Hagan S, Laughlin J, Tabler RE. Knowledge and attitudes of nurses in veterans hospitals about pain management in patients with cancer. Oncol Nurs Forum. 2000;27:1415–23. [PubMed] [Google Scholar]
- 11.Tafas CA, Patiraki E, McDonald DD, Lemonidou C. Testing an instrument measuring Greek nurses’ knowledge and attitudes regarding pain. Cancer Nurs. 2002;25:8–14. doi: 10.1097/00002820-200202000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Bernardi M, Catania G, Tridello G. Knowledge and attitudes about cancer pain management: A national survey of Italian hospice nurses. Cancer Nurs. 2007;30:E20–6. doi: 10.1097/01.NCC.0000265299.25017.24. [DOI] [PubMed] [Google Scholar]
- 13.Bernardi M, Catania G, Lambert A, Tridello G, Luzzani M. Knowledge and attitudes about cancer pain management: A national survey of Italian oncology nurses. Eur J Oncol Nurs. 2007;11:272–9. doi: 10.1016/j.ejon.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Brown ST, Bowman JM, Eason FR. Assessment of nurses’ attitudes and knowledge regarding pain management. J Contin Educ Nurs. 1999;30:132–9. doi: 10.3928/0022-0124-19990501-10. [DOI] [PubMed] [Google Scholar]
- 15.Pederson C, Parran L. Bone marrow transplant nurses’ knowledge, beliefs, and attitudes regarding pain management. Oncol Nurs Forum. 1997;24:1563–71. [PubMed] [Google Scholar]
- 16.Ryan P, Vortherms R, Ward S. Cancer pain: Knowledge, attitudes of pharmacologic management. J Gerontol Nurs. 1994;20:7–16. doi: 10.3928/0098-9134-19940101-02. [DOI] [PubMed] [Google Scholar]
- 17.Hollen CJ, Hollen CW, Stolte K. Hospice and hospital oncology unit nurses: A comparative survey of knowledge and attitudes about cancer pain. Oncol Nurs Forum. 2000;27:1593–9. [PubMed] [Google Scholar]
- 18.Clarke EB, French B, Bilodeau ML, Capasso VC, Edwards A, Empoliti J. Pain management knowledge, attitudes and clinical practice: The impact of nurses’ characteristics and education. J Pain Symptom Manage. 1996;11:18–31. doi: 10.1016/0885-3924(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 19.Ferrell BR, Grant M, Ritchey KJ, Ropchan R, Rivera LM. The pain resource nurse training program: A unique approach to pain management. J Pain Symptom Manage. 1993;8:549–56. doi: 10.1016/0885-3924(93)90084-9. [DOI] [PubMed] [Google Scholar]
- 20.Visentin M, Trentin L, de Marco R, Zanolin E. Knowledge and attitudes of Italian medical staff towards the approach and treatment of patients in pain. J Pain Symptom Manage. 2001;22:925–30. doi: 10.1016/s0885-3924(01)00355-4. [DOI] [PubMed] [Google Scholar]
- 21.Glanz K, Rimer BK, Lewis FM. Theory, Research and Practice. San Fransisco: Wiley and Sons; 2002. Health Behavior and Health Education. [Google Scholar]
- 22.Yildirim YK, Cicek F, Uyar M. Knowledge and attitudes of Turkish oncology nurses about cancer pain management. Pain Manag Nurs. 2008;9:17–25. doi: 10.1016/j.pmn.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 23.Ger LP, Ho ST, Wang JJ. Physicians’ knowledge and attitudes toward the use of analgesics for cancer pain management: A survey of two medical centers in Taiwan. J Pain Symptom Manage. 2000;20:335–44. doi: 10.1016/s0885-3924(00)00207-4. [DOI] [PubMed] [Google Scholar]
- 24.McCaffery M, Ferrell BR. Nurses’ knowledge of pain assessment and management: How much progress have we made? J Pain Symptom Manage. 1997;14:175–88. doi: 10.1016/s0885-3924(97)00170-x. [DOI] [PubMed] [Google Scholar]
- 25.McCaffery M, Ferrell B, O’Neil-Page E, Lester M, Ferrell B. Nurses’ knowledge of opioid analgesic drugs and psychological dependence. Cancer Nurs. 1990;13:21–7. [PubMed] [Google Scholar]
- 26.Furstenberg CT, Ahles TA, Whedon MB, Pierce KL, Dolan M, Roberts L, et al. Knowledge and attitudes of health-care providers toward cancer pain management: A comparison of physicians, nurses, and pharmacists in the state of New Hampshire. J Pain Symptom Manage. 1998;15:335–49. doi: 10.1016/s0885-3924(98)00023-2. [DOI] [PubMed] [Google Scholar]
- 27.Wells-Federman C, Arnstein P, Caudill M. Nurse-led pain management program: Effect on self-efficacy, pain intensity, pain-related disability, and depressive symptoms in chronic pain patients. Pain Manag Nurs. 2002;3:131–40. doi: 10.1053/jpmn.2002.127178. [DOI] [PubMed] [Google Scholar]
- 28.Mamishi N, Behroozishad F, Mohagheghi MA, Eftekhar Z, Shahabi Z. The study of nurses’ knowledge and attitudes regarding cancer pain management. HAYAT. 2006;12:23–32. [Google Scholar]
- 29.Randall-David E, Wright J, Porterfield DS, Lesser G. Barriers to cancer pain management: Home-health and hospice nurses and patients. Support Care Cancer. 2003;11:660–5. doi: 10.1007/s00520-003-0497-x. [DOI] [PubMed] [Google Scholar]
- 30.Yates P, Baker D, Barrett L, Christie L, Dewar AM, Middleton R, et al. Cancer nursing research in Queensland, Australia: Barriers, priorities, and strategies for progress. Cancer Nurs. 2002;25:167–80. doi: 10.1097/00002820-200206000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Joranson DE, Gilson AM. Regulatory barriers to pain management. Semin Oncol Nurs. 1998;14:158–63. doi: 10.1016/s0749-2081(98)80022-3. [DOI] [PubMed] [Google Scholar]
- 32.Ferrell B, Virani R, Grant M, Vallerand A, McCaffery M. Analysis of pain content in nursing textbooks. J Pain Symptom Manage. 2000;19:216–28. doi: 10.1016/s0885-3924(00)00107-x. [DOI] [PubMed] [Google Scholar]
- 33.O’Brien S, Dalton JA, Konsler G, Carlson J. The knowledge and attitudes of experience oncology nurses regarding the management of cancer-related pain. Oncol Nurs Forum. 1996;23:515–21. [PubMed] [Google Scholar]
- 34.Ferrell BR, McGuire DB, Donovan MI. Knowledge and beliefs regarding pain in a sample of nursing faculty. J Prof Nurs. 1993;9:79–88. doi: 10.1016/8755-7223(93)90023-6. [DOI] [PubMed] [Google Scholar]


