Abstract
Mammography screening rates among Chinese American women have been reported to be low. This study examines whether and how culture views and language ability influence mammography adherence in this mostly immigrant population. Asymptomatic Chinese American women (n = 466) aged 50 and older, recruited from the Washington, D.C. area, completed a telephone interview. Regular mammography was defined as having two mammograms at age-appropriate recommended intervals. Cultural views were assessed by 30 items, and language ability measured women’s ability in reading, writing, speaking, and listening to English. After controlling for risk perception, worry, physician recommendation, family encouragement, and access barriers, women holding a more Chinese/Eastern cultural view were significantly less likely to have had regular mammograms than those having a Western cultural view. English ability was positively associated with mammography adherence. The authors’ results imply that culturally sensitive and language-appropriate educational interventions are likely to improve mammography adherence in this population.
Keywords: breast cancer screening, culture, minority health
INTRODUCTION
Asian Americans and Pacific Islanders (AAPIs) are one of the fastest growing and most culturally diverse minority groups in the United States. Chinese make up the largest AAPI ethnic group, comprising about 23.8% of AAPIs (U.S. Census Bureau, n.d.). However, AAPIs remain one of the most poorly understood minorities, mainly because of the lack of nationally representative data to specifically depict the more than 25 subgroups coming from different cultural backgrounds and speaking different languages or dialects (The American Community, 2007). For instance, not until recently was the SEER cancer registry able to report cancer incidence rates in 12 AAPI subgroups. However, because of the lack of detailed population estimates, mortality rates were calculated for only 9 of the 12 groups (Miller, Chu, Hankey, & Ries, 2008). The use of mammography in the general population has been increasing (Hiatt, Klabunde, Breen, Swan, & Ballard-Barbash, 2002) until recently, and has started to level off (Centers for Disease Control and Prevention, 2007). Mammography screening rates among AAPIs remain the lowest compared with non-Hispanic White women (Kagawa-Singer & Pourat, 2000). Similarly, Chinese American women have a lower mammography screening rate compared with Whites (45.8% vs. 57.4%; Tu, Taplin, Barlow, & Boyko, 1999). Although the use of mammography in Chinese American women has increased slightly, from 45.8% reporting ever having a mammogram in early 1990 to 74% in 1999, few women had recent screening, and even fewer received regular screening (Tu et al., 1999; Tu et al., 2003).
Currently, older Chinese American women consist of those who came as part of the large influx of Chinese Americans in the past four decades, including times such as 1965, after the National Origins Quota System was abolished; 1975, after the fall of Saigon; and 1989, after the violent events at Tiananmen Square (Mo, 1992). Some came to the United States to join their husbands or adult children, whereas others stayed in the United States after completing higher education. Regardless, because most Chinese Americans are foreign-born, and about 83% speak a language other than English at home (The American Community, 2007; U.S. Census Bureau, n.d.), Chinese American women may face unique cultural and language barriers to using health services like screening mammography (Ma, 1999), on top of other known screening barriers such as health insurance, physician communication, and attitudes toward screening (Tu et al., 2003; Yu, Kim, Chen, & Brintnall, 2001). For instance, our earlier research indicates that older Chinese American women emphasized self-care over preventive checkups by keeping moderate exercise and eating a hot–cold balanced diet (e.g., eating food that will make the body warm to counter the cold weather or cold body composition), and some held a fatalistic view of illness and cancer (Liang, Yuan, Mandelblatt, & Pasick, 2004). Chinese American women who held those traditional cultural views were less likely to receive cancer screening (Liang et al., 2008).
For immigrants from non-English-speaking countries, language use is a key component of acculturation (O’Malley, Kerner, Johnson, & Mandelblatt, 1999). Previous studies in Hispanic populations have found that acculturation, as measured by English ability, is associated with practice of breast self-examination (Peragallo, Fox, & Alba, 2000) and receipt of mammograms and Pap testing (O’Malley et al., 1999; Suarez & Pulley, 1995). A few studies indicate that the ability to speak English and the degree of English fluency are significantly related to recent mammography and Pap test use among Chinese American women (Tu et al., 2003; Yu, Seetoo, Tsai, & Sun, 1998).
The above literature has suggested that cultural views and language ability affect Chinese American women’s participation in cancer screening. However, scarce research has examined whether these dynamic cultural and language factors independently explain cancer screening outcomes when including other important covariates (i.e., use of medical care). A thorough understanding of the dynamics can potentially improve Chinese American women’s cancer screening by implementing culturally appropriate and language-specific programs or services. The goal of this study was to expand the knowledge of relationships between culture and language ability and Chinese American women’s receipt of mammography by using comprehensive cultural measures and evaluating their associations in the presence of important screening determinants such as the use of medical care and access and psychosocial barriers. We hypothesized that Chinese American women with a strong Chinese cultural view of health and medicine or limited English ability were less likely to have regularly received mammography than those with a less Chinese cultural view of health or better English ability.
METHOD
This cross-sectional study was the first phase of a larger randomized controlled trial designed to improve cancer screening rates in Chinese American women. Results of this study were used to inform the design of the intervention trial of the larger study. The study protocol was approved by the institutional review board at Georgetown University.
Recruitment and Data Collection
A convenience sample of 558 Chinese American women aged 50 and older residing in the metropolitan Washington, D.C. area was recruited between 2003 and 2004 from Chinese churches (21%), other Chinese organizations (e.g., alumni associations; 29%), senior centers (17%), health fairs (14%), and Chinese print media or friend referrals (19%). Interested women were asked to provide a written consent and leave their contact information. All women providing the written consent received a bottle of a brand-name multivitamin supplement either on-site or by mail as a token of appreciation for participation.
Consenting women were then contacted by trained Chinese American interviewers for a 30-minute, computer-assisted telephone interview. A total of 507 (90% of 558) completed the interview; 39 interviews (7.7 %) were administered face-to-face in community or home settings because of difficulty in completing the interview over the phone or reaching the participants by telephone. In addition, three participants completed the mailed survey because they were too busy to set aside time for a telephone interview. A few interviews were conducted in languages other than Mandarin: 25 were conducted in Cantonese, 5 in Taiwanese, 4 in Fuzhou, and 3 in English.
Conceptual Framework
The conceptual framework used for this study was adapted from the PRECEDE/PROCEED framework (Green & Kreuter, 1991) that was designed for identifying community needs and planning educational interventions to change health-related behaviors. It suggests that community needs and problems, once identified, can be improved by modifying individuals’ predisposing, reinforcing, and enabling (PRE) factors that help shape the desired behavior as well as by changing the environment (e.g., local policies and regulations) that influences the PRE factors at the personal level. Predisposing factors are those that predispose a person to engage in the behavior, such as knowledge, attitudes, and other psychosocial factors. Reinforcing factors help reinforce a person’s behavior and usually come from people related to the person or the behavior (e.g., relatives and physicians) or incentives. Enabling factors include structural or environmental factors that facilitate the performance of the behavior. The PRECEDE framework was chosen because it provides a structure to explain known determinants of cancer screening and has been used in cancer screening research with other underserved populations (Bell & Alcalay, 1997). Previous research has demonstrated that certain predisposing factors, such as knowledge and attitudes (Taylor et al., 1999), worry (Consedine, Magai, Krivoshekova, Ryzewicz, & Neugut, 2004), and reinforcing (e.g., physician recommendation; Breen & Kessler, 1994) and enabling factors (e.g., access to care and health insurance; Potosky, Breen, Graubard, & Parsons, 1998) are strongly associated with cancer screening. The main focus of the study—cultural views and language use—can be considered as predisposing and enabling factors, respectively, because the former reflects internal cognitive values that may affect behavior, and the latter is a “skill” to get health information (Bell & Alcalay, 1997) and to use health care (Van der Stuyft, De Muynck, Schillemans, & Timmerman, 1989).
Measures
The selection of measures was guided by the conceptual framework, including outcome (mammography use), predictor (cultural views and language ability), and control variables and sociodemographics. Among control variables, perceived susceptibility and worry were considered predisposing factors; physician recommendation and family encouragement, reinforcing factors; and access barriers, enabling factors. We intended to examine whether and how cultural views and language ability influence mammography use in the presence of important PRE factors that have been shown to influence breast cancer screening.
Outcome Variable
Use of mammography, the primary outcome, was measured by questions about whether they ever had a mammogram, the date of the most recent mammogram, and the interval between the two most recent mammograms. Those questions were previously used to categorize women into stages of screening mammography by Rakowski, Fulton, and Feldman (1993). For this study, having regular mammography was defined as having had a mammogram in the past year and having had a previous mammogram within 2 years prior to the most recent test. Women who had mammograms beyond this time frame or who never had the tests were defined as not having regular mammography. Because only a small number (n = 85, 18%) of participants had never had a mammogram, and their characteristics were similar to those who did not have regular mammograms, we combined these two groups as the “nonregular” mammography users. Women who had undergone mammograms for diagnostic reasons were excluded from subsequent analyses.
Predictor Variables
Chinese cultural views were assessed by 30 items (Table 1) developed from qualitative data of older Chinese American women (Liang et al., 2004), theories of Chinese American elders’ view of health and illness (Chen, 1996), and existing measures, such as beliefs in the balance of yin and yang and fatalism (Lannin et al., 1998). Responses to each item were assessed on a 5-point Likert-type scale, ranging from strongly agree, agree, neutral, disagree, to strongly disagree. Principal component factor analysis of these 30 items yielded seven factors—namely, fatalism, self-care, hot–cold balance, use of herbs, Western medicine, medical checkup, and lifestyle (Liang et al., 2008). The Cronbach’s alpha reliability scores of the overall 30-item, fatalism, and self-care scales were .80, .82, and .73, respectively. The rest of the subscales had Cronbach’s alphas lower than .7 (ranging from .39 to .69). Each sum score of the cultural scale was standardized to a scale of 0 to 100, in which a higher value represented a more traditional Chinese cultural view. Because the overall 30-item, fatalism, and self-care scales had high reliability scores and were consistently and significantly associated with breast, cervical, and colorectal cancer screening, we decided to examine the relationships of the overall scale and subscales (i.e., fatalism and self-care) to mammography use in the presence of other important control variables in separate models. Subscales other than fatalism and self-care were not examined separately because they lacked high reliability; however, their collective contribution to mammography use was captured by the overall cultural scale.
Table 1.
Description of the 30-Item Cultural View Scale
| Category | Statement |
|---|---|
| Fatalism (Cronbach’s α = .82) | If I am meant to get cancer, I will get it. |
| If we get cancer, the best way to deal with it is to accept it, just like the old saying: “Listen to heaven and follow fate.” | |
| Health or illness is a matter of fate. Some people are always healthy; others get sick very often. | |
| I cannot control my destiny. | |
| Avoiding cancer is a matter of personal luck. | |
| No matter what I do, if I am going to get cancer, I will get it. | |
| It is hard to prevent cancer. | |
| Getting cancer is like being sentenced to death. | |
| It is best not to think about cancer. If we think about it too much, we probably will get cancer. | |
| Self-care (Cronbach’s α = .73) | As long as I can take good care of myself and keep myself healthy, I don’t need to see a doctor. |
| I don’t visit doctors if I’m not feeling sick. | |
| Use of herbs (Cronbach’s α = .69) | Herbs are a better choice for preventing diseases than Western medicine. |
| Herbs are more effective in harmonizing a person’s yin–yang than Western medicine. | |
| Herbs are better remedy for illness than Western medicine. | |
| Lifestyle (Cronbach’s α = .59) | Regularity in meals and daily schedules can make us healthy. |
| Keeping my mind happy, doing my hobbies, and not competing with others can lead to better health. | |
| Regular outdoor walking is essential to achieve good health. | |
| Hot–cold balance (Cronbach’s α = .53) | Certain food is not good for me because it will disturb the hot–cold balance in my body. |
| Most diseases, excluding external wounds, are caused by the imbalance between hot and cold in a person’s body. | |
| Eating “cold” food in summer and “hot” food in winter will help strengthen my body. | |
| Medical examination (Cronbach’s α = .42) | I will be embarrassed if a doctor or a nurse checks my private parts. |
| A lot of medical tests are too intrusive and make me uncomfortable. | |
| Medical doctors usually do unnecessary tests. | |
| Western medicine (Cronbach’s α = .39) | We should not take “Western” medicine too often, because its chemical ingredients will hurt our bodies. |
| Western medicine is good for killing germs rather than preventing diseases. | |
| Miscellaneous | Eating food prepared by myself is a key to good health. |
| I know my body better than anyone else. | |
| Bodily constitution is different for every person; therefore, some kinds of people are more likely to get cancer than others do. | |
| Going to clinics or hospitals too often will cause me to catch diseases or get bad luck. | |
| Chi-Kung or Tai-Chi practice can help regulate the chi in the body, which can increase one’s stamina and prevent diseases. |
Women’s English ability was assessed by four items asking about their ability to read, write, listen to, and speak in English, with a 5-point Likert-type response ranging from not at all, not good, fair, good, to very good. To help interpret study results, we recategorize the sum score of these four items to a four-category interval variable based on distribution, with a higher value representing higher English ability.
Control Variables
Predisposing Factors
Worry about developing breast cancer was assessed by one question: “Overall, how worried are you that you might get breast cancer someday (1 = not worried; 2 = somewhat; 3 = worried; and 4 = very worried)?” Based on the distribution of responses, this variable was recategorized to “not worried at all” and “worried.” Perceived susceptibility was assessed by one question: “During last year, how often have you thought about your own chances of getting breast cancer (1 = not at all or rarely; 2 = sometimes; 3 = often; and 4 = a lot)?” Based on the distribution of responses, this variable was dichotomized into “not at all or rarely thinking about getting breast cancer” and “thinking about it (sometimes, often, or a lot).” Because 18.7% of the participants did not answer this question, we created a category for those missing responses to maximize the sample size for analysis.
Enabling Factors
In addition to the question on health insurance (yes vs. no), women were asked whether they had concerns about transportation, time constraints (e.g., unable to take time off from work or child care responsibilities), language, and health care coverage when making decisions on whether to seek health care. We constructed the access barrier variable categorized as “no” and “yes (having at least one of the concerns).”
Reinforcing Factors
Physician recommendation was assessed by one question: “In the past two years, did any doctor who you had visited recommend that you have breast cancer screening (yes vs. no)?” Women were also asked whether their family, relatives, or friends ever encouraged them to get mammography (yes vs. no).
Sociodemographics
We assessed age (50–64 vs. 65 and older), educational level (up to high school vs. college or higher), employment status (yes, part-time or full-time, vs. no), and annual income. Annual income was excluded from further analysis because the variable had greater than 30% missing values.
Analysis
Descriptive analyses were performed first using t tests or chi-square tests to compare differences in sociodemographics, cultural views, language ability, and other control variables between women getting or not getting regular mammograms. Next, a series of logistic regression analyses were conducted to examine associations between cultural views, language ability, and mammography use. First, the base model consisted of sociodemographic variables (Model I). In Model II, control variables were included. Next, cultural views and language ability variables were added to the second model. As mentioned before, we used both the overall 30-item cultural scale (Model III) and the fatalism and self-care subscales (Model IV) to test the effect of overall and specific cultural views on mammography use.
RESULTS
After excluding women who had diagnostic mammography, 466 (91.9%) women constituted the final sample. About 64% were born in China, 3% in Hong Kong, 29% in Taiwan, and 4% in other Asian countries. Participants’ mean age was 64.5 years (standard deviation = 9 years; range = 50–89 years). The majority of participating women had a college degree or higher (68%), had health insurance (77%), were married (73%), and were not employed (37%). About 53% regularly obtained mammograms (Table 2).
Table 2.
Characteristics of Participating Chinese American Women Aged 50 and Older by Mammography Status (N = 466)
| Characteristics | Total N = 466 |
Not Having Regular Mammography n = 221 (47.4%) |
Having Regular Mammography n = 245 (52.6%) |
p Values |
|---|---|---|---|---|
| Demographics | ||||
| Age (mean: 64.5 years, standard deviation: 9 years; range: 50 to 89 years) | ||||
| 50–64 | 256 (55.1%) | 111 (45.5%) | 145 (65.6%) | <.0001 |
| ≥65 | 209 (44.9%) | 133 (54.5%) | 76 (34.4%) | |
| Education | ||||
| High school or less | 147 (31.6%) | 110 (44.9%) | 37 (16.7%) | <.0001 |
| College or above | 319 (68.4%) | 135 (55.1%) | 184 (83.3%) | |
| Employed (percentage yes) | 171 (36.7%) | 55 (22.5%) | 116 (52.5%) | <.0001 |
| Control variables | ||||
| Cancer worry (percentage ever) | 172 (36.9%) | 69 (28.2%) | 103 (46.6%) | <.0001 |
| Perceived susceptibility | ||||
| Low | 225 (48.2%) | 133 (54.3%) | 92 (41.6%) | .0009 |
| High | 154 (33.1%) | 62 (25.3%) | 92 (41.6%) | |
| Missing | 87 (18.7%) | 50 (20.4%) | 37 (16.7%) | |
| Health insurance (percentage yes) | 357 (76.6%) | 154 (62.9%) | 203 (91.9%) | <.0001 |
| Perceived access barriers (percentage yes) | 260 (55.8%) | 158 (64.5%) | 102 (46.2%) | <.0001 |
| MD recommendation (percentage yes) | 244 (52.4%) | 85 (34.7%) | 159 (72.0%) | <.0001 |
| Family/friend encouragement (percentage yes) | 123 (26.4%) | 76 (31.0%) | 47 (21.3%) | .0171 |
| Predictor variables | ||||
| Language ability | ||||
| Meana | 2.43 | 1.98 | 2.94 | <.0001 |
| 1 (score ≤8) | 120 (25.8%) | 98 (40.0%) | 22 (10.0%) | |
| 2 (8 < score ≤12) | 132 (28.3%) | 82 (33.5%) | 50 (22.6%) | |
| 3 (12 < score ≤16) | 105 (22.5%) | 36 (14.7%) | 69 (31.2%) | |
| 4 (16 < score) | 109 (23.4%) | 29 (11.8%) | 80 (36.2%) | |
| Cultural viewsb | ||||
| Overall sum score (mean) | 54.1 | 57.0 | 50.9 | <.0001 |
| Fatalism (mean) | 41.9 | 46.6 | 36.7 | <.0001 |
| Self-care (mean) | 45.2 | 54.0 | 35.5 | <.0001 |
The mean score of the interval scale created by dividing the original sum score of four 5-point Likert-type scales asking about participants’ ability to read, write, listen to, and speak English, each with responses ranging from 1 = not at all to 5 = very good. A lower mean score represents a lower English ability.
High scores on cultural views indicate a more Chinese/Eastern view of care; low scores reflect a more Western view of care.
Women who reported having had regular mammography were significantly more likely to be younger, highly educated, and employed than those not having regular mammograms (Table 2). Compared with those not having regular mammograms, women who had regular mammograms were also more likely to worry about getting breast cancer, perceive a higher risk of getting breast cancer, have health insurance, receive physician recommendation, and have higher English ability. They were less likely to perceive access barriers, receive encouragements from family and friends for mammography, and hold Chinese cultural views of health and illness.
Model I shows that after controlling for other sociodemographics, the effect of age on mammography use became insignificant (Table 3). After adding PRE factors in Model II, education and employment status were still significantly associated with mammography use. All the PRE factors, except for perceived risk for breast cancer and perceived access barriers, remained significantly associated with mammography use. After cultural views and language ability were included in Model III, higher education and being employed no longer predicted regular mammography use. On the other hand, cultural views and English ability significantly predicted Chinese American women’s regular use of mammography (odds ratio [OR] = 0.96, 95% confidence interval [CI] = 0.94–0.99 and OR = 1.43, 95% CI = 1.10–1.86, respectively). Similar patterns emerged after the overall 30-item cultural view scale was replaced by fatalism and self-care subscales in Model IV: Both scales were significantly associated with regular mammography use (OR = 0.98, 95% CI = 0.97–0.99 and OR = 0.99, 95% CI = 0.98–0.99, respectively). With a 10-point increase in the fatalism and the self-care subscales, there is a 20% and 40% decreased likelihood, respectively, for a Chinese woman to have regular mammography. Similarly, with each increase in the English ability scale, there is a 44% increase in regular use of mammography. Including variables of cultural views and language ability significantly improve the model fit, as indicated by the significant increments of chi-square values (p < .01).
Table 3.
Logistic Regression Models Describing Associations of Cultural Views With Mammography Adherence in Chinese American Women (N = 466)
| Variable | Model I (Demographics) |
Model II (Model I + Control Variables) |
Model III (Model II + Predictor Variables) |
Model IV (Model II + Predictor Variables) |
|---|---|---|---|---|
| Demographics | ||||
| Age (≥65 vs. 50–64) | 0.91 (0.57–1.43) | 0.96 (0.57–1.63) | 1.05 (0.61–1.79) | 1.06 (0.61–1.82) |
| Education (college or above vs. high school or less) | 2.92 (1.85–4.63) | 2.12 (1.27–3.54) | 1.14 (0.63–2.07) | 1.05 (0.57–1.94) |
| Employed (yes vs. no) | 2.74 (1.71–4.39) | 2.02 (1.17–3.48) | 1.67 (0.95–2.95) | 1.52 (0.85–2.70) |
| Control variables | ||||
| Cancer worry (ever vs. never) | 1.91 (1.18–3.08) | 1.98 (1.21–3.22) | 1.94 (1.19–3.18) | |
| Perceived susceptibility | ||||
| Missing vs. high | 0.80 (0.41–1.54) | 0.83 (0.42–1.64) | 0.83 (0.41–1.67) | |
| Low vs. high | 0.72 (0.43–1.20) | 0.72 (0.43–1.20) | 0.70 (0.42–1.18) | |
| Health insurance (yes vs. no) | 3.82 (2.07–7.08) | 3.28 (1.74–6.20) | 3.12 (1.65–5.92) | |
| Perceived access barriers (yes vs. no) | 0.75 (0.48–1.18) | 0.82 (0.52–1.30) | 0.84 (0.53–1.34) | |
| MD recommendation (yes vs. no) | 3.20 (2.05–5.01) | 2.92 (1.85–4.61) | 2.80 (1.76–4.46) | |
| Family/friend encouragement (yes vs. no) | 0.46 (0.28–0.76) | 0.50 (0.30–0.84) | 0.51 (0.30–0.86) | |
| Predictor variables | ||||
| Language abilitya | 1.43 (1.10–1.86) | 1.44 (1.11–1.89) | ||
| Cultural viewsb | ||||
| Overall sum score | 0.96 (0.94–0.99) | |||
| Fatalism | 0.98 (0.97–0.99) | |||
| Self-care | 0.99 (0.98–0.99) | |||
| Model chi-square test (χ2) | 68.7 (df = 3) | 154.3 (df = 10) | 163.2 (df = 11) | 172.5 (df = 12) |
| (Δχ2)c | 85.6 | 8.9 | 9.3 | |
| (vs. Model I)*** | (vs. Model II)** | (vs. Model III)** |
Language was recoded as an interval variable (scores ranging from 1 to 4). High language scores mean higher English ability.
High scores on cultural views indicate a more Chinese/Eastern view of care; low scores reflect a more Western view of care.
The symbol Δχ2 denotes the differences in likelihood ratio chi-square (χ2) tests between the tested model and the compared model.
p < .01.
p < .001.
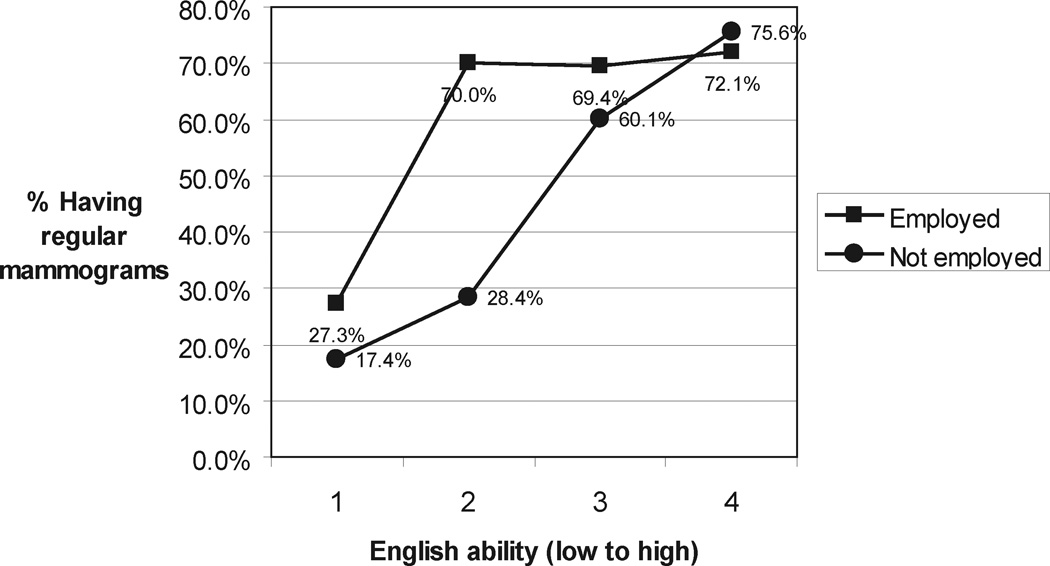
The interactions between demographics and language ability and cultural view were examined in the multivariate logistic regression (Model III). Only the interaction between language ability and employment status was significant (p < .006). The positive association between English ability and having regular mammograms was more prominent among those reporting not being employed (Figure 1). Women who were employed were more likely to have had regular mammograms even with a somewhat lower English ability.
Figure 1.
Interactions between employment status and English ability in their relationships with regular use of mammograms.
DISCUSSION
This is one of the first studies that examines the associations between cultural views, language ability, and regular mammography use in Chinese American women using comprehensive measures and controlling for other important PRE factors related to mammography use. As hypothesized, women who held a more Chinese/Eastern cultural view were less likely to adhere to mammography screening guidelines. Our findings are consistent with previous studies showing that cultural views, such as believing in karma and modesty, are associated with cancer screening practice among Asian minorities (Taylor et al., 1999). The linear association between cultural views and mammography adherence cannot be overlooked. The predictive power of cultural views on mammography use is robust, as evidenced by narrow confidence intervals for either the overall scale or the fatalism and self-care subscales. These suggest that the degree of inclination to Chinese cultural views influences a Chinese woman’s mammography screening behavior, and a change in certain aspects of the cultural views, especially about fatalism and self-care, is likely to modify Chinese American women’s mammography behavior.
Our finding of the positive association between English ability and regular mammography use is consistent with prior research showing that language ability is associated with initiation of health services or screening (Tu et al., 2003; Yu et al., 1998). The association persists after controlling for physician recommendation and other known PRE factors related to mammography use. One possible explanation is that women who had no or limited English ability were not able to fully communicate with their physicians and understand the need for regular screening, even if mammography was recommended by their physicians. Another possible reason is that women with low English ability were not as equally exposed to cancer-related information as their White counterparts, which is evidenced by our previous study showing that Chinese American women seldom identified brochures/pamphlets displayed in hospitals or clinics, newspapers, or television channels as sources of health-related information (Liang et al., 2004).
The associations between education and employment and mammography use were cancelled out after cultural views and language ability were included in the model. In other words, the influence of education and employment on mammography use is mediated by cultural views and language ability. Chinese American women who had a higher educational level or who were employed were more likely to adhere to mammography screening, compared with those with a lower educational level or who were not employed, probably because they were more likely to better communicate with health care professionals in English or understand health-related information written in English. Similarly, they were less likely to hold certain cultural views that kept them from seeking regular mammography. These findings suggest that addressing cultural and language barriers to mammography screening experienced by Chinese American women, especially those with a lower socioeconomic status, is a promising strategy to reduce screening disparities between women of lower and higher socioeconomic status.
Consistent with prior research in general and Asian populations, our data indicate that physician recommendation, health insurance, and worry about breast cancer are significant reinforcing, enabling, and predisposing factors associated with women’s mammography use (Breen & Kessler, 1994; Consedine et al., 2004; Potosky et al., 1998). This suggests that language and culturally appropriate cancer screening education programs, which are important for immigrants such as older Chinese American women, will need to be combined with efforts to improve physician recommendation and reduce financial and psychological barriers in order to reach optimal impacts on women’s cancer screening behavior. Those efforts are likely to reduce the sociodemographic difference in screening adherence observed in our sample because the effect of age, education, and employment status on mammography use can be explained by cultural views and language ability as well as other important predisposing, reinforcing, and enabling factors. Finally, the interaction between employment status and language ability shown in our data implies that work-site mammography education or services may have been effective in increasing mammography use among working Chinese Americans with a somewhat low English ability. On the other hand, efforts should be made to design language-appropriate educational programs or interventions that target nonworking Chinese American women with a low English proficiency.
Several caveats should be considered when interpreting the results. First, the cultural view scales were developed primarily from responses of Chinese American women aged 50 and older to questions regarding their perceptions about health and illness/cancer and their experiences with U.S. health care (Liang et al., 2004; Liang et al., 2008). It is possible that other aspects of cultural views held by Chinese Americans were not captured. In addition, subscales that had limited predictive power, compared with fatalism and self-care subscales, could have been so partly because of the few items included in each subscale. Adding more items and improving reliability may help strengthen their predictive power. Second, the generalizability of this study is limited by the use of a convenience sample drawn mainly from Chinese community organizations, churches, and senior centers. Although mass media were used to encourage participation, relatively small numbers of women participated through this channel. Therefore, women who did not attend any activities or programs held by Chinese organizations, such as restaurant workers or those speaking in other Chinese dialects, are likely to be underrepresented in our sample. Cultural patterns as well as their associations with cancer screening behaviors may be different if these people are included. However, because these people are likely to be less Westernized than women in our sample, it is possible that our results underestimate the true effects of cultural views on cancer screening. In addition, measures of cancer screening behaviors are subject to self-report bias, which has been identified in the general and minority populations (Hiatt et al., 1995; Norman et al., 2003).
Despite these limitations, this study demonstrates that different aspects of cultural views and English ability are important factors influencing older Chinese American women’s mammography screening behavior. These two aspects are relatively modifiable, compared with other known factors such as health insurance coverage and other access barriers. Future research is needed to examine whether addressing cultural barriers through language-appropriate education and/or counseling will improve Chinese American women’s cancer screening adherence in a large representative sample.
Implications for Practice
Cancer screening educational programs targeting Chinese American women are likely to be successful if we acknowledge women’s cultural views related to nonadherence to cancer screening and include messages that counter those cultural barriers. For instance, women with a sense of fatalism need to be empowered to take charge of their breast health. Likewise, health care providers should be sensitive to possible cultural barriers of their Chinese American patients, especially those who are older immigrants, and address their specific concerns that keep them from getting mammograms. In addition, Chinese language educational materials, such as brochures, videos, booklets, and displays need to be readily available in clinics, hospitals, libraries, and mass media to provide accessible information to older Chinese American women with limited English ability.
Acknowledgments
This study was supported by funding from the National Cancer Institute Career Development Award (K07 CA90352, W. Liang), the Susan G. Komen Breast Cancer Foundation Population Specific Research Grant (POP0100855, W. Liang), U.S. Department of Defense (BC010208, J. H. Wang and W. Liang), and the National Cancer Institute (K05 CA96940, J. M. Mandelblatt).
Footnotes
Part of the study results were orally presented in the 132nd APHA annual meeting, November 6–10, 2004, Washington, DC.
REFERENCES
- The American Community—Asians: 2004. Washington, DC: U.S. Census Bureau; 2007. [Google Scholar]
- Bell RA, Alcalay R. The impact of the Wellness Guide/Guia on Hispanic women’s well-being-related knowledge, efficacy beliefs, and behaviors: The mediating role of acculturation. Health Education and Behavior. 1997;24:326–343. doi: 10.1177/109019819702400306. [DOI] [PubMed] [Google Scholar]
- Breen N, Kessler L. Changes in the use of screening mammography: Evidence from the 1987 and 1990 National Health Interview Surveys. American Journal of Public Health. 1994;84:62–67. doi: 10.2105/ajph.84.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Use of mammograms among women aged > or = 40 years—United States, 2000–2005. MMWR Morbidity and Mortality Weekly Report. 2007;56(3):49–51. [PubMed] [Google Scholar]
- Chen YL. Conformity with nature: A theory of Chinese American elders’ health promotion and illness prevention processes. Advances in Nursing Science. 1996;19(2):17–26. doi: 10.1097/00012272-199612000-00004. [DOI] [PubMed] [Google Scholar]
- Consedine NS, Magai C, Krivoshekova YS, Ryzewicz L, Neugut AI. Fear, anxiety, worry, and breast cancer screening behavior: A critical review. Cancer Epidemiology, Biomarkers and Prevention. 2004;13:501–510. [PubMed] [Google Scholar]
- Green LW, Kreuter MW. Health promotion planning: An educational and environmental approach. Mountain View, CA: Mayfield; 1991. [Google Scholar]
- Hiatt RA, Klabunde C, Breen N, Swan J, Ballard-Barbash R. Cancer screening practices from National Health Interview Surveys: Past, present, and future. Journal of the National Cancer Institute. 2002;94:1837–1846. doi: 10.1093/jnci/94.24.1837. [DOI] [PubMed] [Google Scholar]
- Hiatt RA, Perez-Stable EJ, Quesenberry C, Jr, Sabogal F, Otero-Sabogal R, McPhee SJ. Agreement between self-reported early cancer detection practices and medical audits among Hispanic and non-Hispanic White health plan members in northern California. Preventive Medicine. 1995;24:278–285. doi: 10.1006/pmed.1995.1045. [DOI] [PubMed] [Google Scholar]
- Kagawa-Singer M, Pourat N. Asian American and Pacific Islander breast and cervical carcinoma screening rates and Healthy People 2000 objectives. Cancer. 2000;89:696–705. doi: 10.1002/1097-0142(20000801)89:3<696::aid-cncr27>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Lannin DR, Matthews HF, Mitchell J, Swanson MS, Swanson FH, Edwards MS. Influence of socioeconomic and cultural factors on racial differences in late-stage presentation of breast cancer. Journal of the American Medical Association. 1998;279:1801–1807. doi: 10.1001/jama.279.22.1801. [DOI] [PubMed] [Google Scholar]
- Liang W, Wang JH, Chen MY, Feng S, Yi B, Lee MM, et al. Developing and validating a measure of Chinese cultural views of health and cancer. Health Education and Behavior. 2008;35:361–375. doi: 10.1177/1090198106294893. [DOI] [PubMed] [Google Scholar]
- Liang W, Yuan E, Mandelblatt JS, Pasick RJ. How do older Chinese women view health and cancer screening? Results from focus groups and implications for interventions. Ethnicity and Health. 2004;9:283–304. doi: 10.1080/1355785042000250111. [DOI] [PubMed] [Google Scholar]
- Ma GX. Between two worlds: The use of traditional and Western health services by Chinese immigrants. Journal of Community Health. 1999;24:421–437. doi: 10.1023/a:1018742505785. [DOI] [PubMed] [Google Scholar]
- Miller BA, Chu KC, Hankey BF, Ries LA. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes & Control. 2008;19:227–256. doi: 10.1007/s10552-007-9088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo B. Modesty, sexuality, and breast health in Chinese-American women. Western Journal of Medicine. 1992;157:260–264. [PMC free article] [PubMed] [Google Scholar]
- Norman SA, Localio AR, Zhou L, Bernstein L, Coates RJ, Flagg EW, et al. Validation of self-reported screening mammography histories among women with and without breast cancer. American Journal of Epidemiology. 2003;158:264–271. doi: 10.1093/aje/kwg136. [DOI] [PubMed] [Google Scholar]
- O’Malley AS, Kerner J, Johnson AE, Mandelblatt J. Acculturation and breast cancer screening among Hispanic women in New York City. American Journal of Public Health. 1999;89:219–227. doi: 10.2105/ajph.89.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peragallo NP, Fox PG, Alba ML. Acculturation and breast self-examination among immigrant Latina women in the USA. International Nursing Review. 2000;47:38–45. doi: 10.1046/j.1466-7657.2000.00005.x. [DOI] [PubMed] [Google Scholar]
- Potosky AL, Breen N, Graubard BI, Parsons PE. The association between health care coverage and the use of cancer screening tests: Results from the 1992 National Health Interview Survey. Medical Care. 1998;36:257–270. doi: 10.1097/00005650-199803000-00004. [DOI] [PubMed] [Google Scholar]
- Rakowski W, Fulton JP, Feldman JP. Women’s decision making about mammography: A replication of the relationship between stages of adoption and decisional balance. Health Psychology. 1993;12:209–214. doi: 10.1037//0278-6133.12.3.209. [DOI] [PubMed] [Google Scholar]
- Suarez L, Pulley L. Comparing acculturation scales and their relationship to cancer screening among older Mexican-American women. Journal of the National Cancer Institute Monographs. 1995;18:41–47. [PubMed] [Google Scholar]
- Taylor VM, Schwartz SM, Jackson JC, Kuniyuki A, Fischer M, Yasui Y, et al. Cervical cancer screening among Cambodian-American women. Cancer Epidemiology, Biomarkers and Prevention. 1999;8:541–546. [PubMed] [Google Scholar]
- Tu SP, Taplin SH, Barlow WE, Boyko EJ. Breast cancer screening by Asian-American women in a managed care environment. American Journal of Preventive Medicine. 1999;17(1):55–61. doi: 10.1016/s0749-3797(99)00043-4. [DOI] [PubMed] [Google Scholar]
- Tu SP, Yasui Y, Kuniyuki AA, Schwartz SM, Jackson JC, Hislop TG, et al. Mammography screening among Chinese-American women. Cancer. 2003;97:1293–1302. doi: 10.1002/cncr.11169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. [Retrieved January 20, 2009];U.S. census 2000. (n.d.). from www.census.gov/main/www/cen2000.html.
- Van der Stuyft P, De Muynck A, Schillemans L, Timmerman C. Migration, acculturation and utilization of primary health care. Social Science and Medicine. 1989;29:53–60. doi: 10.1016/0277-9536(89)90127-5. [DOI] [PubMed] [Google Scholar]
- Yu ES, Kim KK, Chen EH, Brintnall RA. Breast and cervical cancer screening among Chinese American women. Cancer Practice. 2001;9:81–91. doi: 10.1046/j.1523-5394.2001.009002081.x. [DOI] [PubMed] [Google Scholar]
- Yu MY, Seetoo AD, Tsai CK, Sun C. Sociodemographic predictors of Papanicolaou smear test and mammography use among women of Chinese descent in south-eastern Michigan. Women’s Health Issues. 1998;8:372–381. doi: 10.1016/s1049-3867(98)00020-6. [DOI] [PubMed] [Google Scholar]