Abstract
Salivary gland trauma is uncommon. Parotid gland and duct injuries are far more common than injuries to submandibular and sublingual glands due to anatomic position. Several methods of treating salivary duct injuries and their complications have been advocated. Optimal treatment outcomes can be achieved with early diagnosis, adequate evaluation, and proper management. This article presents current diagnostic and treatment protocols of salivary gland trauma. The anatomy of the salivary glands is briefly described and clinical cases are also presented to illustrate the treatment options described.
Keywords: parotid injury, parotid gland injury, submandibular gland trauma
Salivary gland injuries have been described in the literature for more than 100 years.1 They usually occur following a penetrating trauma of the parotid or submandibular region and occasionally they are associated with injuries to the adjacent facial structures such as the facial and lingual nerves, the ear, and bony structures of the face.2,3 Other causes of salivary gland trauma involve blunt injuries and trauma following radiotherapy of the head and neck. Blunt injuries often remain unnoticed and they are recognized by their complications which involve chronic obstruction of the excretory system of the glands and subsequent infection and sialadenitis.4 Radiotherapy can also cause irreversible damage to the salivary glands. Fortunately, some portions of the glands usually remain protected. These portions gradually grow and compensate for the lost portions of the gland, maintaining an adequate function.4
Parotid gland and duct injuries, although rare, are far more common than injuries to submandibular and sublingual glands. This can readily be explained by the anatomic position of submandibular and sublingual glands which are protected by the mandible, whereas parotid gland is more exposed to penetrating trauma. Lewis and Knottenbelt reported that the incidence of parotid gland injuries is ∼0.21% of trauma cases.5 Only half of these injuries are recognized as acute parotid trauma whereas the rest appear later as sialoceles or fistulas.6 Nevertheless, in every case optimal outcome can be expected when an early diagnosis is made and when an adequate management is provided.
Parotid Gland and Duct Injuries
Anatomy
Parotid gland is the largest of all the major salivary glands and it is entirely serous in secretion. About 75% or more of the parotid gland overlies masseter muscle, while the rest of it is located behind the ramus.7 Posterior to the parotid gland the external acoustic meatus is found as well as sternocleidomastoid muscle, while posteromedially the parotid gland is defined by the posterior belly of digastric muscle and stylohyoid muscle. Anteriorly, parotid gland overlies masseter muscle and more medially it is bordered by the ramus of the mandible and the medial pterygoid muscle. Inferiorly, the gland covers the superior and anterior portion of sternocleidomastoid muscle and the zygomatic arch defines the superior border of the parotid gland. The parotid gland is covered by the investing layer of deep cervical fascia, which contributes to the formation of the capsule of the gland, subcutaneous fat, and the skin.
Parotid or Stensen duct exits from the anterior and superior portion of the gland. It passes superficial to the masseter muscle and 1 cm beyond the anterior border of the masseter muscle, penetrates the buccal fat pad and buccinator muscle, to exit into the oral cavity opposite the second maxillary molar. Its course is parallel to the zygomatic arch and often parallel to the buccal branch of the facial nerve.8,9 Van Sickels10 divided the duct into three distinct sites to establish a treatment protocol. Site A corresponds to the most proximal part of the duct where it exits from the substance of the gland to the posterior border of the masseter muscle. Site B represents the part of the duct which is located superficial to the masseter muscle. This part of the duct is unprotected from any overlying structure and that is the reason why injury to the duct occurs nearly always in site B. Site C corresponds to the portion of the duct which is located distal to the anterior border of the masseter muscle to the exit of the duct in the oral cavity (Fig. 1).
Figure 1.
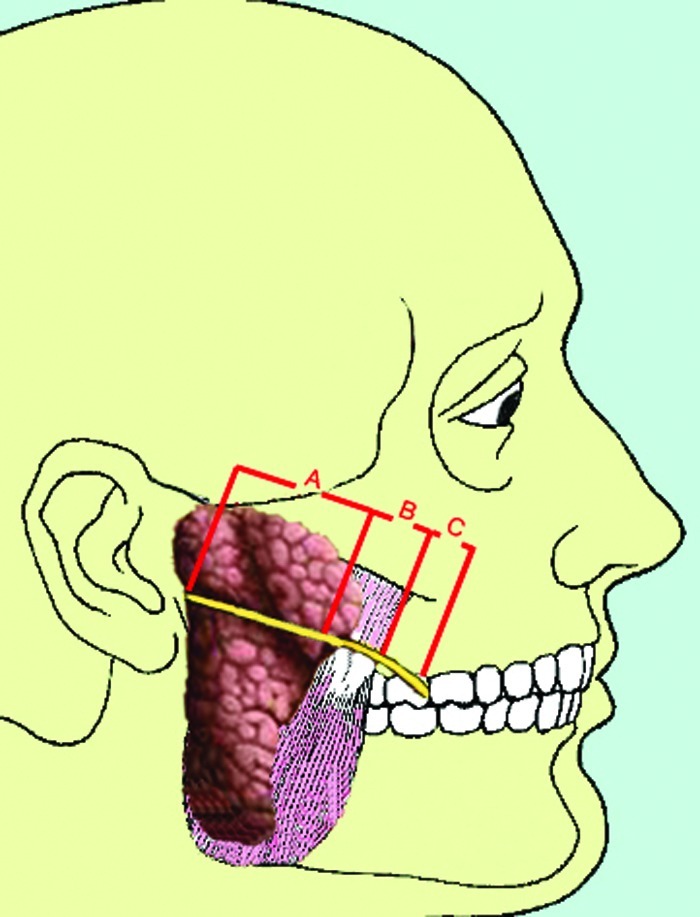
Parotid duct is divided in three distinct sites. Site A corresponds to the most proximal part of the duct. Site B corresponds to the part of the duct which is located superficial to the masseter muscle. Site C corresponds to the part of the duct located anterior to the masseter muscle.
The facial nerve emerges from the stylomastoid foramen, passes between the stylohyoid muscle and the posterior belly of digastric muscle and within the substance of the gland it subdivides into a temporofacial and a cervicofacial trunk. These trunks give rise to five major branches: temporal, zygomatic, buccal, mandibular, and cervical. Buccal and zygomatic branches of the facial nerve form an anastomotic loop over the parotid duct.7 It is absolutely essential to evaluate the function of the facial nerve whenever there is trauma to the parotid gland or duct.
External carotid artery ascends superiorly posterior to the mandible and enters the parotid gland through its inferior aspect. Within the gland it divides into the superficial temporal and the internal maxillary arteries. The transverse facial artery arises from the superficial artery within the gland. The retromandibular vein also arises within the gland. It is formed by the junction of the superficial temporal vein and the internal maxillary vein.4,7 It descends superficial to the external carotid artery. Any penetrating trauma to the parotid gland carries the risk of injuring these vascular structures which need to be ligated. It becomes clear that the parotid region is a complex region. The clinician who is called to treat parotid gland injuries must have a thorough understanding of the anatomy of surrounding structures.
Diagnosis
Evaluation of the patient must always begin by obtaining as much information as possible by the patient or the family. As in every trauma, mechanism and time interval between injury and presentation are vital information that can lead the clinician to a proper treatment plan. Patient's medical history is always necessary. When trauma to the salivary glands is suspected, the clinician should also ask when the patient ate his last meal4 because eating stimulates salivary gland function and if the patient had his last meal after the trauma, it is more possible to notice saliva coming out of the wound or producing parotid swelling.
The next step is to clinically evaluate the patient. If a penetrating injury exists along a line joining the tragus of the ear and the midportion of the upper lip, then there is a great chance that either the parotid gland or the parotid duct or both have been injured (Figs. 2 and 3).2 Another useful landmark is the anterior border of masseter muscle. Any injury behind it should be thoroughly inspected.4 An easy way to diagnose the presence of injury to the parotid gland is by palpating and massaging the gland to express saliva into the field. If there is injury to the ductal structures, saliva will be seen pooling in the wound. This is a simple maneuver, but occasionally it does not help to come to safe conclusions. Another simple way to confirm the presence of ductal injury is to cannulate the duct from its distal oral opening with a pediatric intravenous catheter after dilating it with a lacrimal probe and inject saline or methylene blue. If the injected liquid does not appear in the wound, the ductal system is intact. Despite this, it is advised to keep the catheter for at least 1 week to prevent obstruction of the duct due to edema.
Figure 2.
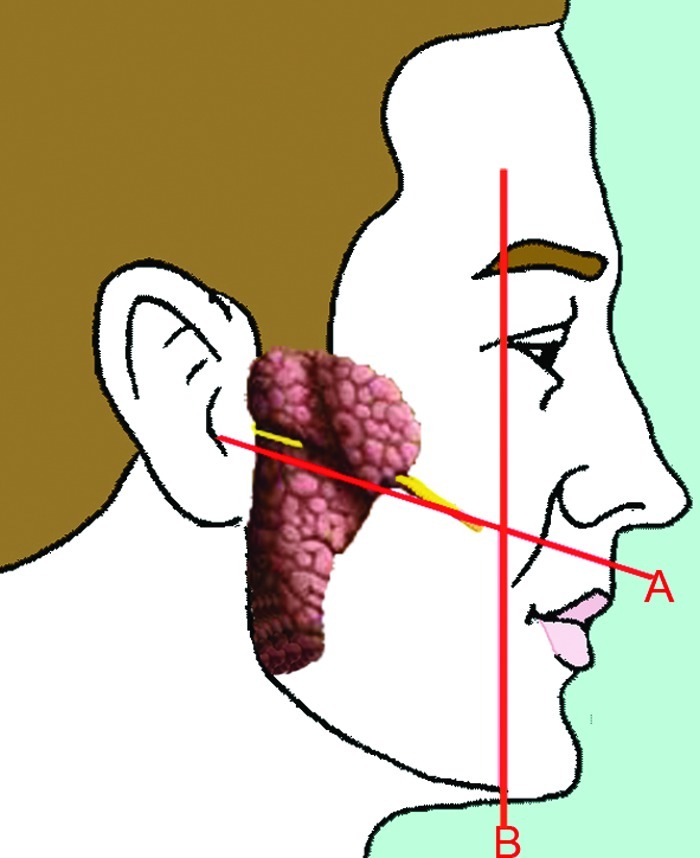
If the penetrating injury is located across a line joining the midline of the upper lip with the tragus of the ear, a great chance of injuring to the parotid duct or gland and the facial nerve exists. Another useful landmark is a line joining the upper canthus with the mental foramen. Any injuries behind this imaginary line must be explored.
Figure 3.

Photograph of a patient with a deep penetrating trauma of his left cheek.
If the liquid appears in the wound, it is safe to conclude that a ductal injury exists and needs to be repaired.4 Toluidine blue may discolor the field and pose difficulties in the subsequent maneuvers.2 That is why a very limited quantity should be injected or it should be diluted in saline before injecting.
Whenever there is a penetrating trauma over the parotid region, adjacent structures should also be examined. If the patient is awake, facial nerve integrity should be evaluated by asking the patient to raise his eyebrows, close his eyes, blow his cheeks, and show his teeth. Facial nerve injury occurs in 20% of patients with isolated gland injuries and in more than half of the patients with Stensen duct injuries.11 The buccal branch of the facial nerve is most commonly injured because it courses parallel with the duct superficial to the masseter muscle and sometimes may even cross the duct. Lacerations to the facial nerve or parotid duct should be repaired at the initial time of laceration closure. Injury to the duct may be accompanied by injury to the buccal branch of the facial nerve. In that case the patient presents with weakness of the upper lip when trying to animate.2 Electroneurography and electromyography are also important adjuncts to evaluate nerve recovering.4 The general rule dictates that when the facial nerve injury is located anterior to an imaginary line that unites the outer canthus with the gonial notch of the mandible repair of the facial nerve is not necessary. For nerve injuries posterior to this line, identification and primary repair of the nerve stumps is indicated.
Vascular injury is often easily diagnosed because it produces hemorrhage or leads to the formation of large hematomas, but it may also be obscure leading to the formation of pseudoaneurysms. Formation of a pseudoaneurysm is suspected when a palpating or audible bruit is present.4 Pressure is applied to control the hemorrhage until a more thorough exploration of the wound in the operating room can be achieved. The main vessels that course through the parotid gland are located deep to the branches of the facial nerve thus blind and uncareful attempts to ligate these vessels may lead to permanent facial nerve injuries.12 Moreover, external auditory canal may also be involved and in that case otorrhagia is present. Abnormal mandibular movements may indicate temporomandibular joint trauma. Jaw movements and proper occlusion should always be examined when trauma over the parotid region is evaluated.4
Diagnosis of parotid trauma is more of a clinical conclusion. Мagnetic resonance imaging and computed tomography are not useful in assessing parotid trauma. Sialography can confirm ductal system integrity but it is helpful in chronic obstructions. In the acute setting it does not offer much more than the clinical assessment, although some authors argue that it can delineate the exact injury location offering several advantages to the subsequent treatment.11,13 However, it is helpful when ductal injury has been overlooked or to evaluate patency of salivary duct after treatment.14 Sialoendoscopy offers more accurate information concerning intraductal anatomy,15 but it is usually not necessary as there are simpler methods to confirm ductal injuries. Vascular injury can be evaluated by angiography, magnetic resonance angiogram and Doppler.16 Angiography, although more invasive, is the gold standard and can be combined with embolization of the bleeding vessel, if it is needed.
Treatment of Parotid Injuries
Parotid injuries may involve the gland itself or parotid duct or both. It is very useful to divide injuries into the following: (1) those that involve only the parenchyma of the gland, (2) those that involve the parotid duct, and (3) those that involve both. This classification is correlated with prognosis and with the incidence of complications.17 Optimal outcome can be assured by early recognition and treatment of these injuries. One study refers to 19 untreated injuries of parotid region. Among them 10 patients suffered from late complications such as sialoceles or fistulas.5 Although the majority of these complications eventually heal conservatively, they pose a great concern both to the patient and to the surgeon. Whenever a ductal injury is found at the initial surgical exploration of the wound, it is better but not mandatory to perform primary closure of the duct.9,18
Treatment of Parotid Gland Injuries
Sometimes parotid gland may be injured and parotid duct may be left intact. This scenario is the most convenient for the surgeon. The wound must be carefully cleansed and the lacerated parotid capsule must be sutured with resorbable sutures. It is rather imperative to apply a pressure dressing for 48 hours to minimize the risk of sialocele formation.19 Epker and Burnette9 advocates to remove the dressing in 24 hours and reapply a new one. This allows evaluation of wound healing. Extensive laceration will cause extensive edema of the parotid region. Cannulation of the duct for a period of 2 weeks is advocated to maintain the lumen of the duct open. Otherwise, obliteration of the duct due to edema may occur leading to sialadenitis.19 Parenchyma injuries generally heal faster than parotid duct injuries and lead to fewer complications.13 Close follow-up of the patient is mandatory.
Treatment of Parotid Duct Injuries
Parotid duct course corresponds to a line connecting tragus and the medial surface of the upper lip. Whenever a penetrating trauma which involves this imaginary line exists, a parotid duct injury must be suspected. Following gentle irrigation and debridement of the wound, the surgeon should attempt to cannulate the duct with a 16-Gauge intravenous catheter and inject saline or methylene blue to confirm the presence of duct laceration. If saline or the dye is seen in the wound, laceration of the duct is confirmed. Methylene blue should be injected with caution because it can discolor the surgical field and make identification of the facial nerve very difficult. The next step is to identify both ductal stumps (Figs. 4 and 5). The distal stump has been already identified rather easily by cannulating the duct through its intraoral orifice. Identification of the proximal stump may be copious. The surgeon can approximate wound edges and follow the direction of the probe to search for the proximal ductal end.19 Another maneuver is to exert pressure on the parotid gland and look for saliva flow. Saliva comes out of the distal stump. Nevertheless sometimes identification of both stumps is impossible especially in avulsed wounds. Partial transection of the duct has a better prognosis than complete transection as healing time is significantly shorter.13
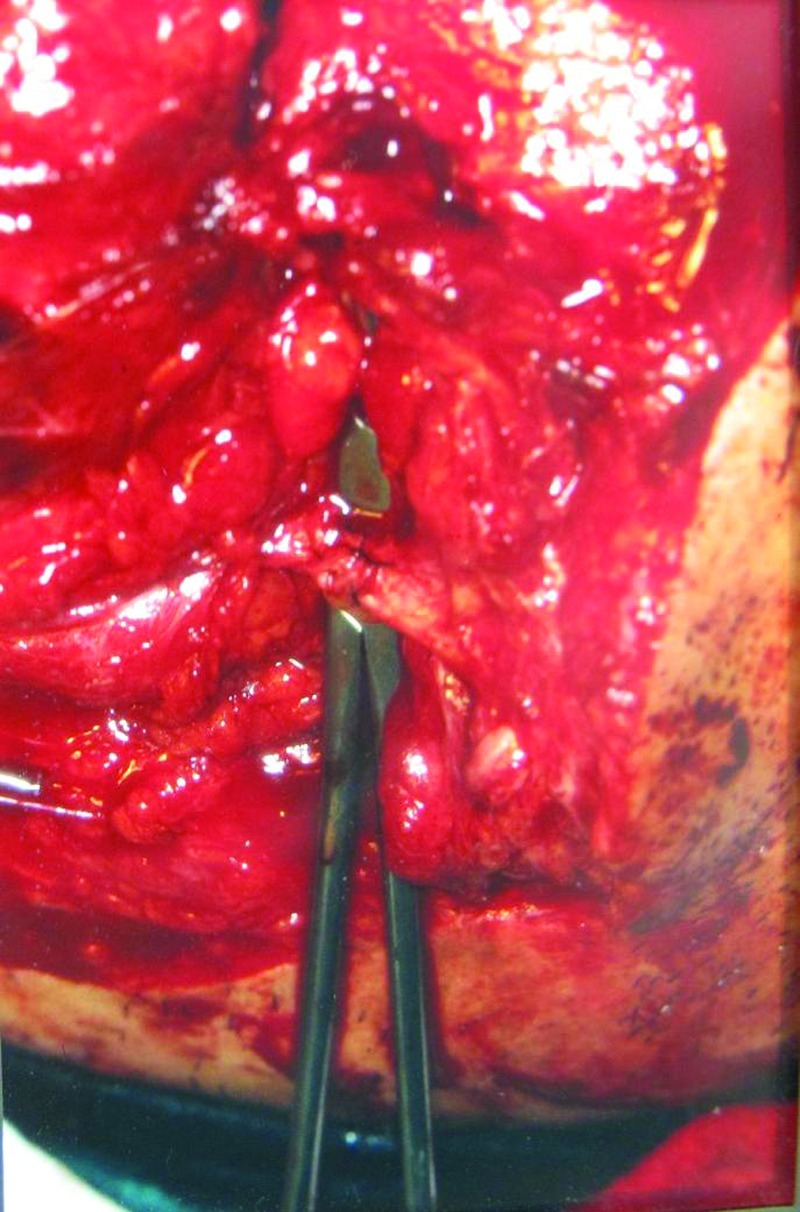
Figure 4.
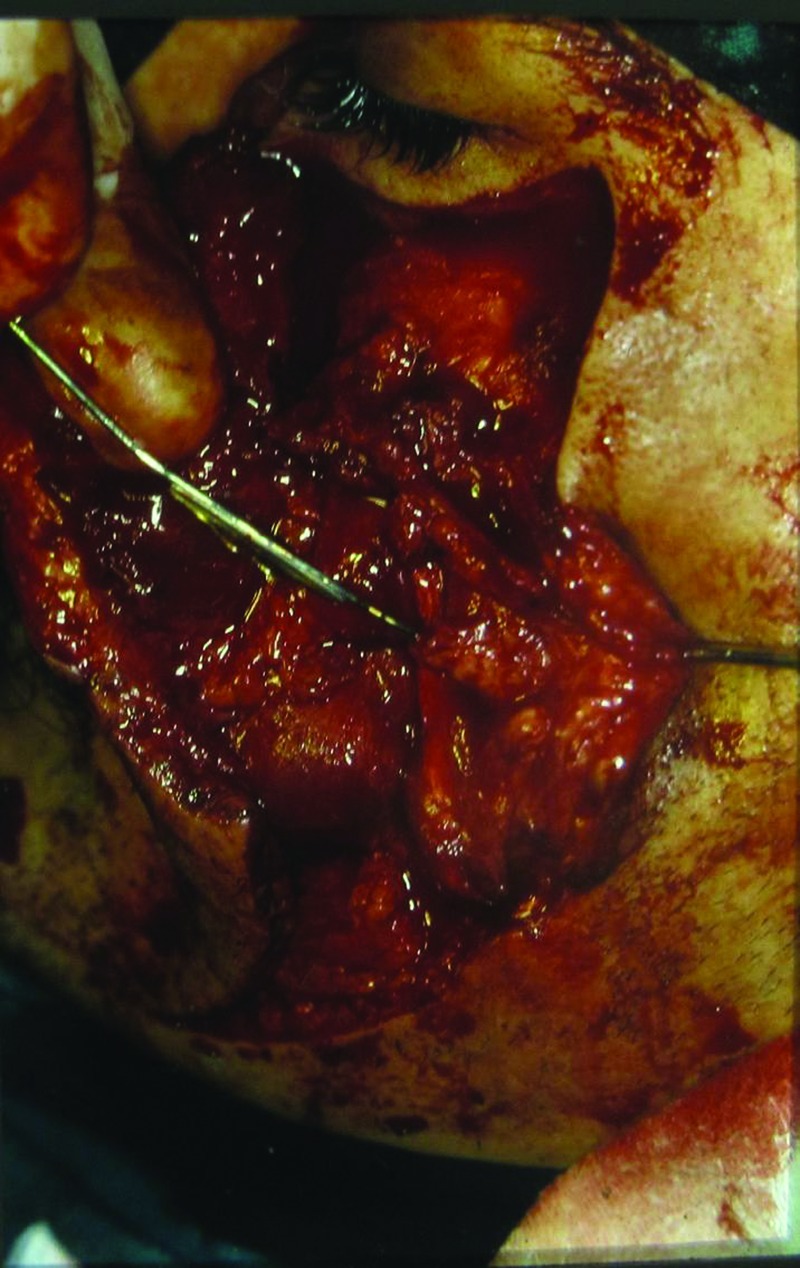
The proximal stump of the left transected parotid duct is identified with a lacrimal probe.
Figure 5.
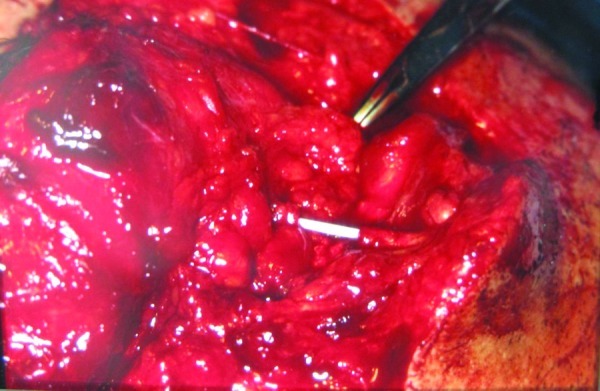
The transected stumps of the left parotid duct are identified and cannulated with a fine intravenous catheter.
Van Sickels has proposed a classification of parotid duct trauma depending on site of injury. Site A injury corresponds to the part of the duct which is located intraglandulary and in that case treatment involves only closure of the lacerated parotid capsule. No effort is made to anastomose the duct because these injuries have a lower complication rate and healing usually occurs fast and uneventfully.5 Site B injury corresponds to the part of the gland overlying masseter muscle. In that case direct anastomosis of the ductal stumps is recommended. Site C injuries correspond to the portion of the gland anterior to the masseter muscle. Again anastomosis of ductal ends is recommended but it is more difficult to achieve. If anastomosis is not feasible creation of an intraoral drainage is recommended by suturing the proximal stump to an artificial mucosal opening (oral reimplantation).10
When an injury site B or C exists and both ductal ends are identified, they must be sutured together without tension. Initially, a small silicone catheter or a probe is inserted through both ends and the stumps are brought together and sutured over the catheter to prevent suturing the anterior wall of the one stump with the posterior wall of the other. However, experienced surgeons may not need intraductal catheter placement and still have good results.20,21 It is recommended that the catheter is sutured to the buccal mucosa and left in place for 2 weeks to prevent stenosis and allow unobstructed salivary flow.21 In one literature survey of reports, Dumpis and Feldmane conclude that long-term stenting has significantly better results than short-term stenting.22 Suturing is performed either with nylon 9–0 or 10–0 or with silk 7–0 or 8–019 and at least three sutures are needed (Fig. 6). Nonresorbable sutures are preferred to resorbable sutures because resorbable sutures tend to produce massive scarring in comparison with ductal size and may lead to secondary ductal stenosis or obstruction.22 If the two stumps cannot be sutured without tension or cannot be approximated, an autogenous vein graft can be used. Experimental studies on dogs have published contradictory results concerning success of vein grafts.22,23 The catheter is left in place for 10 to 14 days to prevent stenosis of the duct. During this time antisialagogues and antibiotics are recommended.10 External pressure is applied over the parotid region for 2 days. Postoperatively, sialoendoscopy may be used to examine the patency of the duct15 (Figs. 7 and 8).
Figure 6.
The stumps are sutured together with 9–0 Prolene suture material.
Figure 7.

Intraoral photograph of the same patient 1 month later. Parotid gland functions normally and saliva can be seen exiting from the orifice of the duct.
Figure 8.
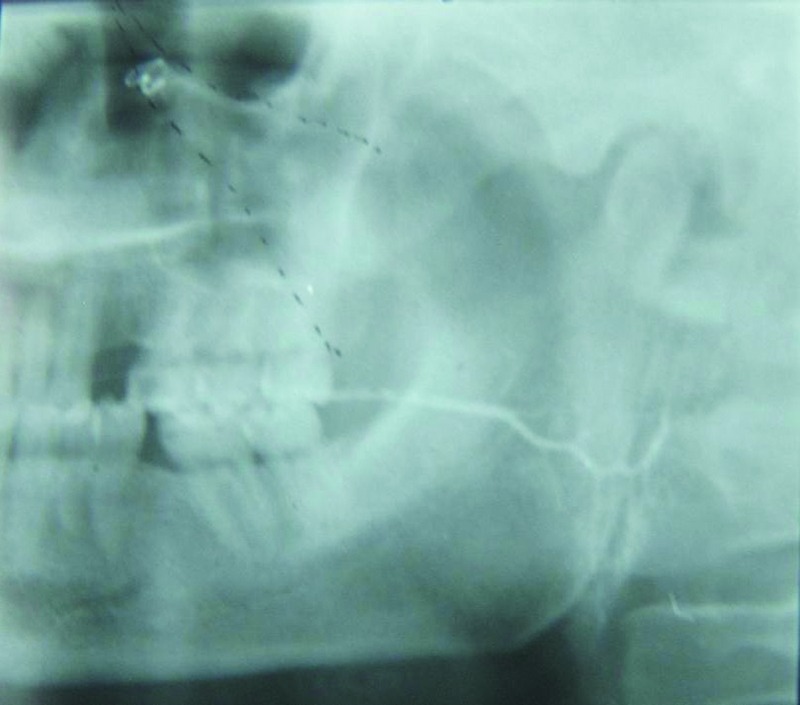
Sialography of the same patient 1 month later. The excretory system of the left parotid gland functions normally. No stenosis of the parotid duct is noticed.
When both ends of the lacerated duct cannot be found or cannot be sutured due to extensive lacerations, identification and ligation of the proximal end are recommended. This is done with the intention to promote atrophy of the gland and to reduce the risk of sialocele or fistula formation.10,11,19 This maneuver can be combined with pressure dressings and antisialagogues to further reduce salivary flow. No noticeable asymmetry occurs following unilateral atrophy of the parotid gland.19
Some studies recommend performing oral reimplantation when the proximal stump is identified but end-to-end anastomosis cannot be performed. The proximal stump is transported through buccinator muscle and through an opening of the oral mucosa which is created by the surgeon behind the orifice of Stensen duct and is sutured to the oral mucosa. By creating this oral fistula, diversion of salivary flow to the oral cavity is achieved.24
Complications
The most common complications following trauma in the parotid region are sialoceles and fistulas. Prognosis depends on the extent and site of injury as glandular injuries heal faster than ductal injuries and partial duct transection heals faster than complete duct transection.9,19 Treatment depends on timing of their appearance but it generally follows two directions: diversion of parotid secretions into the mouth and depression of parotid secretion.19
Sialoceles
Sialoceles are formed due to accumulation of saliva which cannot be drained intraorally. They are cysts filled with a collection of mucoid saliva in the tissues surrounding parotid gland. They manifest themselves as soft swellings over the parotid region which can be misdiagnosed as hematomas or infections. Diagnosis is usually established by aspiration. Aspiration reveals a fluid that resembles to saliva but, if doubts still exist, the fluid must be sent for measuring amylase levels, which will be found to exceed 100,000 U/L.19
Treatment depends on whether sialocele is an immediate or a late complication. It is prudent to reopen and reexplore the wound if the sialocele appears immediately or a few days after wound closure. Reexploring the wound may reveal a laceration of parotid gland parenchyma or a laceration of the parotid duct. In the first case the surgeon must clean the wound and suture the lacerated parotid capsule. In the second case, the surgeon must make every effort to recognize both ends of the salivary duct and suture them together. Sometimes this is not possible especially if duct laceration is located anterior to the masseter muscle. In that case, the sialocele must be drained intraorally via a catheter which is led intraorally usually behind the papilla.19
If the sialocele appears as a late complication, conservative treatment is advocated. Repeated aspirations with external pressure dressings usually have a successful outcome especially if trauma is located to parenchyma rather than to the ductal system.5 Antisialagogue medications are also helpful because they reduce salivary flow. Further reduction in autonomic gland stimulation can be achieved if the patient refrains from oral intake. Feeding via nasogastric tube is indicated when dealing with chronic sialoceles or fistulas.4,15 Botulinum toxin has been used to treat sialoceles. It is injected right into the lesion and it has been stated that it gradually causes sialocele regression.25,26 Botulinum toxin type A affects presynaptic neurons inhibiting release of acetylcholine. This blockage of parasympathetic neurons innervating the secretory system of parotid gland will reduce salivary flow. Injection of 0.1 to 0.2 mL of a solution of 25 mU/0.1 mL botulinum toxin in the parotid gland preferably with sonographic assistance is recommended. Without having major complications, this protocol succeeds in reducing salivary production in a few weeks.27,28
Rarely sialoceles do not resolve with these conservative measures. Only if conservative measures have proved unsuccessful, the surgeon may proceed to radiotherapy10 or operative treatment such as parotidectomy.19,21 However, it should be stated that parotidectomy is performed in a compromised bed with scar and granulation tissue and carries a high risk of damaging the facial nerve. Radiation induces fibrosis and atrophy of the gland. Today it has been abandoned because more than 6 weeks is required to achieve atrophy of the gland. Moreover, radiation increases the potential of malignancy.7
Fistulas
A fistula is a communication between the skin and the parotid gland or the parotid duct that allows external drainage of saliva through the skin (Fig. 9). Sometimes a long-standing sialocele may convert to a fistula due to rupture of the skin overlying the sialocele.19 Treatment depends on the time that fistula appeared compared with the time of injury. When fistula appears as an immediate complication, surgical reexploration is advocated. Trauma to gland parenchyma is treated with cleansing and suturing of the parotid capsule. Trauma to the parotid duct is best treated by anastomosing its ends. If both ends cannot be found, ligation of the proximal end and placement of an intraoral drainage is the best solution. When fistula appears as a late complication, it is more convenient to treat it conservatively with external pressure and anticholinergic drugs.19 In one study 17 fistulas were treated. Of these, three of them originated from the parotid gland and they were resolved quickly. The rest originated from parotid duct. These were treated by surgical anastomosis of the ductal ends, by saphenous vein grafting when ductal ends could not be approximated and by parotidectomy.29
Figure 9.

Photograph of a fistula developed after a penetrating trauma of the parotid region.
If conservative measures fail to treat the fistula, other treatment modalities have been advocated. Tympanic neurectomy involves drilling into the temporal bone and disruption of tympanic nerve, which carries parasympathetic secretory nerve fibers to the parotid gland.30,31 This technique aims at reducing salivary flow and causing spontaneous fistula resolution. However, the results were disappointing probably because with time reinnervation of the gland tends to occur. Although popular in the past, this method tends to be abandoned due to short-term and poor results.32
Submandibular Gland: Anatomy
Submandibular gland is the second largest salivary gland. It secretes both serous and mucous saliva, although it is predominantly serous secreting. It consists of a superficial and a deep part. The superficial part occupies most of the posterior portion of the submandibular triangle. The gland folds around the posterior border of the mylohyoid muscle so that a portion of the gland (deep portion) lies in the oral cavity between the hyoglossus muscle and the mandible. The submandibular duct exits from the deep portion of the gland, lies in the floor of the mouth along the sublingual gland, and empties at the sublingual papilla. Along its course the lingual nerve crosses the duct twice.4,7
Submandibular Gland Trauma
Penetrating trauma to the floor or the mouth or beneath the mandible can damage the submandibular or sublingual glands. However, trauma to the submandibular gland is very rare because the gland is protected from the body of the mandible. In fact there are only case reports of submandibular gland trauma in the literature.33,34 Penetrating or gunshot injuries or associated mandibular fractures can traumatize submandibular gland or its duct. Other causes of submandibular gland injury involve lacerations of the floor of the mouth that may involve Wharton duct and blunt trauma with fracture of the gland that is usually found in motor vehicle accidents.7 If trauma to the submandibular gland is identified during surgical exploration of the wound, removal of the gland is recommended as it is an easy procedure with a low complication rate. If trauma to the submandibular gland is not diagnosed during wound exploration, a submandibular fistula or a slowly expanding submandibular mass is likely to appear later. In that case conservative treatment with antisialagogues, pressure bandages and aspiration is followed and usually leads to fistula resolution. If conservative measures prove unsuccessful, the surgeon should not hesitate to proceed to gland removal. Injuries to the duct of the submandibular gland should be treated with marsupialization of the gland in a more distal location to avoid stricture formation.35
References
- 1.Nicoladoni C. Über Fisteln des Ductus Stenonianus. Verh Dtsch Ges Chir. 1896;25:81–83. [Google Scholar]
- 2.Sickels J E Van. Management of parotid gland and duct injuries. Oral Maxillofac Surg Clin North Am. 2009;21(2):243–246. doi: 10.1016/j.coms.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 3.Singh B, Shaha A. Traumatic submandibular salivary gland fistula. J Oral Maxillofac Surg. 1995;53(3):338–339. doi: 10.1016/0278-2391(95)90237-6. [DOI] [PubMed] [Google Scholar]
- 4.Haller J R. Trauma to the salivary glands. Otolaryngol Clin North Am. 1999;32(5):907–918. doi: 10.1016/s0030-6665(05)70181-x. [DOI] [PubMed] [Google Scholar]
- 5.Lewis G, Knottenbelt J D. Parotid duct injury: is immediate surgical repair necessary? Injury. 1991;22(5):407–409. doi: 10.1016/0020-1383(91)90107-p. [DOI] [PubMed] [Google Scholar]
- 6.Tachmes L, Woloszyn T, Marini C. et al. Parotid gland and facial nerve trauma: a retrospective review. J Trauma. 1990;30(11):1395–1398. doi: 10.1097/00005373-199011000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Norton N S. Philadelphia: Elsevier; 2007. Parotid bed and gland; p. 196. [Google Scholar]
- 8.Hallock G G. Microsurgical repair of the parotid duct. Microsurgery. 1992;13(5):243–246. doi: 10.1002/micr.1920130509. [DOI] [PubMed] [Google Scholar]
- 9.Epker B N, Burnette J C. Trauma to the parotid gland and duct: primary treatment and management of complications. J Oral Surg. 1970;28(9):657–670. [PubMed] [Google Scholar]
- 10.Sickels J E Van. Parotid duct injuries. Oral Surg Oral Med Oral Pathol. 1981;52(4):364–367. doi: 10.1016/0030-4220(81)90330-3. [DOI] [PubMed] [Google Scholar]
- 11.Landau R, Stewart M. Conservative management of post-traumatic parotid fistulae and sialoceles: a prospective study. Br J Surg. 1985;72(1):42–44. doi: 10.1002/bjs.1800720117. [DOI] [PubMed] [Google Scholar]
- 12.Youngs R P, Walsh-Waring G P. Trauma to the parotid region. J Laryngol Otol. 1987;101(5):475–479. doi: 10.1017/s0022215100102038. [DOI] [PubMed] [Google Scholar]
- 13.Parekh D, Glezerson G, Stewart M, Esser J, Lawson H H. Post-traumatic parotid fistulae and sialoceles. A prospective study of conservative management in 51 cases. Ann Surg. 1989;209(1):105–111. doi: 10.1097/00000658-198901000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steinberg M J, Herréra A F. Management of parotid duct injuries. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99(2):136–141. doi: 10.1016/j.tripleo.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 15.Nahlieli O Baruchin A M Sialoendoscopy: three years' experience as a diagnostic and treatment modality J Oral Maxillofac Surg 1997559912–918., discussion 919–920 [DOI] [PubMed] [Google Scholar]
- 16.Roon A J, Christensen N. Evaluation and treatment of penetrating cervical injuries. J Trauma. 1979;19(6):391–397. doi: 10.1097/00005373-197906000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Betts N J, Cotrell K R. St. Louis, Missouri: Elsevier Saunders; 2005. Diagnosis and management of traumatic salivary gland injuries; pp. 865–867. [Google Scholar]
- 18.Morel A S, Firestein A. Repair of traumatic fistulas of the parotid duct. Arch Surg. 1963;87:623–626. doi: 10.1001/archsurg.1963.01310160085015. [DOI] [PubMed] [Google Scholar]
- 19.Lewkowicz A A, Hasson O, Nahlieli O. Traumatic injuries to the parotid gland and duct. J Oral Maxillofac Surg. 2002;60(6):676–680. doi: 10.1053/joms.2002.33118. [DOI] [PubMed] [Google Scholar]
- 20.Sparkman R S. Laceration of parotid duct further experiences. Ann Surg. 1950;131(5):743–754. doi: 10.1097/00000658-195005000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stevenson J H. Parotid duct transection associated with facial trauma: experience with 10 cases. Br J Plast Surg. 1983;36(1):81–82. doi: 10.1016/0007-1226(83)90019-x. [DOI] [PubMed] [Google Scholar]
- 22.Dumpis J, Feldmane L. Experimental microsurgery of salivary ducts in dogs. J Craniomaxillofac Surg. 2001;29(1):56–62. doi: 10.1054/jcms.2000.0190. [DOI] [PubMed] [Google Scholar]
- 23.Chudakov O, Ludchik T. Microsurgical repair of Stensen's & Wharton's ducts with autogenous venous grafts. An experimental study on dogs. Int J Oral Maxillofac Surg. 1999;28(1):70–73. [PubMed] [Google Scholar]
- 24.Neuhaus R W, Baylis H I. Parotid duct injury as a complication of differential seventh nerve ablation. Am J Ophthalmol. 1982;93(1):124–125. doi: 10.1016/0002-9394(82)90714-0. [DOI] [PubMed] [Google Scholar]
- 25.Vargas H, Galati L T, Parnes S M. A pilot study evaluating the treatment of postparotidectomy sialoceles with botulinum toxin type A. Arch Otolaryngol Head Neck Surg. 2000;126(3):421–424. doi: 10.1001/archotol.126.3.421. [DOI] [PubMed] [Google Scholar]
- 26.Guntinas-Lichius O, Sittel C. Treatment of postparotidectomy salivary fistula with botulinum toxin. Ann Otol Rhinol Laryngol. 2001;110(12):1162–1164. doi: 10.1177/000348940111001214. [DOI] [PubMed] [Google Scholar]
- 27.Marchese-Ragona R, De Filippis C, Staffieri A, Restivo D A, Restino D A. Parotid gland fistula: treatment with botulinum toxin. Plast Reconstr Surg. 2001;107(3):886–887. doi: 10.1097/00006534-200103000-00048. [DOI] [PubMed] [Google Scholar]
- 28.von Lindern J J, Niederhagen B, Appel T, Bergé S, Reich R H. New prospects in the treatment of traumatic and postoperative parotid fistulas with type A botulinum toxin. Plast Reconstr Surg. 2002;109(7):2443–2445. doi: 10.1097/00006534-200206000-00041. [DOI] [PubMed] [Google Scholar]
- 29.Ananthakrishnan N, Parkash S. Parotid fistulas: a review. Br J Surg. 1982;69(11):641–643. doi: 10.1002/bjs.1800691104. [DOI] [PubMed] [Google Scholar]
- 30.Chitre V V, Premchandra D J. Recurrent parotitis. Arch Dis Child. 1997;77(4):359–363. doi: 10.1136/adc.77.4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vasama J P. Tympanic neurectomy and chronic parotitis. Acta Otolaryngol. 2000;120(8):995–998. doi: 10.1080/00016480050218762. [DOI] [PubMed] [Google Scholar]
- 32.Mandour M A, El-Sheikh M M, El-Garem F. Tympanic neurectomy for parotid fistula. Arch Otolaryngol. 1976;102(6):327–329. doi: 10.1001/archotol.1976.00780110039002. [DOI] [PubMed] [Google Scholar]
- 33.de Geus J J, Maisels D O. A traumatic fistula of the submandibular gland. Br J Plast Surg. 1976;29(2):196–198. doi: 10.1016/0007-1226(76)90051-5. [DOI] [PubMed] [Google Scholar]
- 34.Traiger J. Laceration of a minor salivary gland. A complicating factor in a fracture of the mandible in a child. Oral Surg Oral Med Oral Pathol. 1963;16:783–785. doi: 10.1016/0030-4220(63)90314-1. [DOI] [PubMed] [Google Scholar]
- 35.Feinberg S E. Philadelphia: Lippincott Company; 1992. The diagnosis and surgical management of salivary gland disorders; pp. 841–879. [Google Scholar]


