Abstract
Materials and Methods A 6-year retrospective analysis of 111 patients treated for maxillofacial fractures in Davangere, Karnataka from January 2004 to December 2009 was performed. Variables like age, gender, occupation, type of fracture and mechanism of injury, concomitant injury, mode of treatment, and complications were recorded and assessed.
Results Men between 21 and 30 years were mostly affected (male-to-female ratio = 10:1; age range = 17.60 years; mean 31.7 ± 9.8 [standard deviation]). Most fractures were caused by road traffic accidents (RTAs; 74.7%), followed by interpersonal violence (IPV; 15.8%), falls (4.2%), industrial hazards and animal attacks (2.1% each), and self-inflicted injury (1.1%). Forty-two cases were isolated zygomaticomaxillary complex (ZMC) fractures. The total number of facial fractures documented was 316, of which 222 were purely related to the ZMC; however, 11 were confined only to the midface. Fifty-three cases had concomitant lower jaw fractures, totaling 83. Ophthalmic injuries occurred in 30.52% of cases. Ninety-two cases were treated with open reduction and internal fixation (ORIF), and three cases were managed conservatively. The complication rate observed was 25.26%.
Conclusion RTA continues to be the chief etiological factor in maxillofacial injury with males being affected predominantly. IPV and falls next contribute significantly to the incidence of such injuries. Concomitant injuries, however, require prompt recognition and appropriate management. ORIF still remains the mainstay of treatment; however, fixation devices are constantly being improved upon in an attempt to reduce immobilization time thereby facilitating early return to function with minimal morbidity. Nevertheless, future advances in maxillofacial trauma diagnosis and management are likely to reduce associated morbidity.
Keywords: maxillofacial trauma, zygomaticomaxillary fractures, mid-face, mandibular fractures, ORIF
The maxillofacial region is most prone to fracture owing to its prominent position.1,2 The anatomic location and pattern of such fractures are determined by the mechanism of injury and direction of impact. In addition to being anatomically complex, its exposure to the external environment is maximal in comparison with the rest of the human body; such injuries therefore require precise evaluation and treatment. The incidence and etiologies of facial fractures are chiefly influenced by race and country development. Other attributes include geography, culture, social and religious traditions, economic status and level of education, and mode of travel.
The World Health Organization statistics indicate that 1 million people die and between 15 and 20 million are injured annually in road traffic accidents (RTAs).3 Investigators in countries such as Jordan,4 Singapore,5 Nigeria,6,7 New Zealand,8 Denmark,9 and Japan10 have found that RTAs represent the most common cause of maxillofacial fractures in those countries; in Finland,11 the United States,12 and Sweden,13 assault has been reported as the most common etiological factor.
Facial fractures can have long-term residual effects both functionally and esthetically, regardless of nature and accuracy of treatment. It has also been observed that techniques for the treatment of facial fractures have evolved over the years to minimize if not preclude associated morbidity. The purpose of this study is to determine the etiology, pattern, and distribution of maxillofacial fractures in Central Karnataka and review the treatment methods employed in the management of such fractures. We also suggest, based on our experience, an all-inclusive algorithm that may have relevance in contemporary maxillofacial practice.
Patients and Methods
A total of 111 patients reported between January 2004 to December 2009 for treatment in the Department of Oral & Maxillofacial Surgery, College of Dental Sciences & Hospital, Davangere, but we were able to retrieve and review the oral and maxillofacial records of only 95 patients. The data were categorized under etiology, age and gender, site, month and day the incident occurred, treatment performed, and complications recognized.
Results
Etiology versus Percentage of Cases
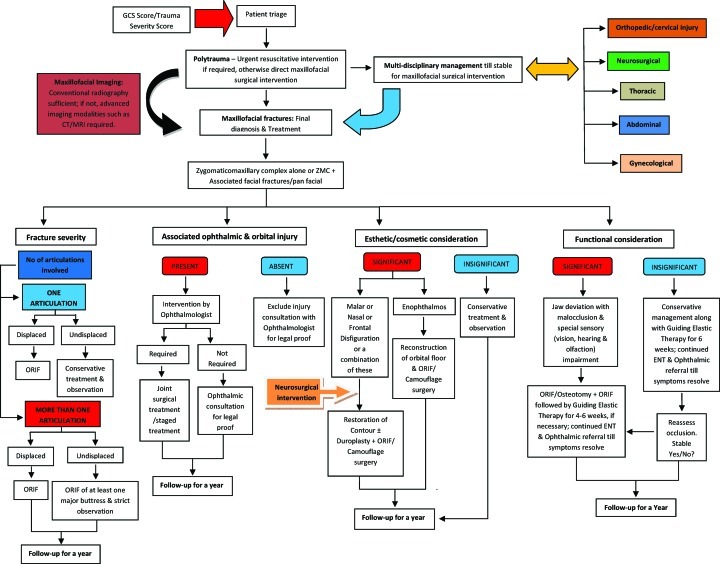
We observed the commonest cause of maxillofacial injuries to be RTA (74.7%), followed by interpersonal violence (IPV; 15.8%), falls (4.2%), animal attacks (2.1%), industrial hazards (2.1%), and self-inflicted injury (1.1%; Fig. 1).
Figure 1.
Etiology versus percentage of cases. RTA, road traffic accident.
Etiology, Age, and Gender Distribution
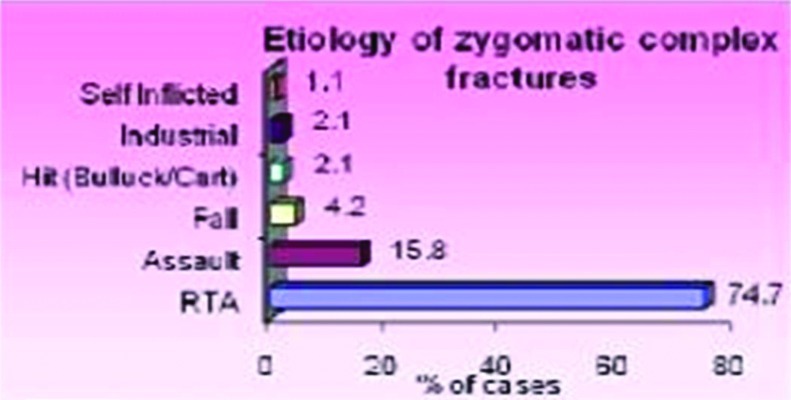
RTA was the most common cause for etiology accounting for 71 (74.7%; Figs. 2 and 3). Males were more frequently affected, accounting for 90.5% (86) of the study sample, and females accounted for 9.5% (9).The age group of 21 to 30 years (43.2%) was predominantly affected followed by the 31- to 40-year age group (32.6%). The age group of 21 to 30 years accounted for 41.8% of the age range.
Figure 2.
Etiology, age, and gender distribution. RTA, road traffic accident.
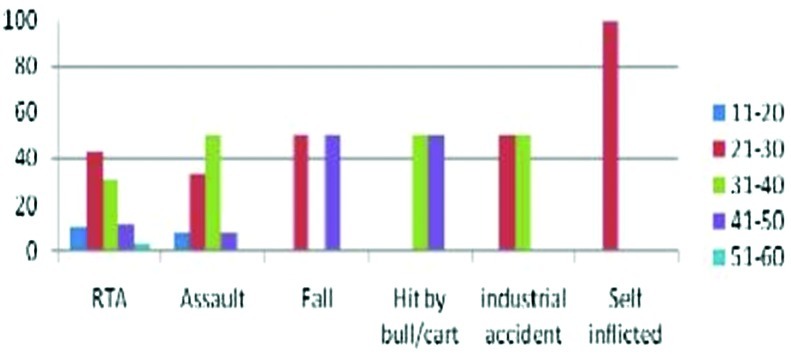
Figure 3.
Etiology, age, and gender distribution. RTA, road traffic accident.
Month and Day Distribution
March and December (16.8%) had the highest number of cases of maxillofacial injuries, followed by November (12.6%; Table 1). However, the least number was seen in April and September (3.2%).The day that had the highest number of casualties was Monday (17.9%) followed by Sunday (16.8%). However, the least number of cases was observed on Saturday (10.5%).
Table 1. RTA Number in Terms of Two-Wheeler and non-Two-Wheeler Population, with the Incidence of Wearing Crash Helmet.
| Road Traffic Accident Number by Vehicle Type | |||
|---|---|---|---|
| Two-wheelers | 53 | Total | 53 (74.65%) |
| Crash helmet wearing | 0 | ||
| Non-two-wheelers [(bullock cart, HMV, auto rickshaw, hit and run by MV (L&H)] | Total | 18 (25.35%) | |
| Case total | 71 | ||
HMV, heavy motor vehicles; LMV, light motor vehicles; L&H, light & heavy.
Site and Etiology Distribution of Fractures of Zygomaticomaxillary Complex Alone and Those Associated with Other Facial Fractures
Number of RTAs in terms of two-wheeler and non-two-wheeler population, with the incidence of crash helmet wearing, is indicated (Table 2). Of the total, 42 cases were isolated zygomaticomaxillary (ZM) complex fractures; 53 were associated with other facial fractures (Table 3). In ZM complex, the site and number of fractures involving these particular locations were variable. A relationship between the etiology and the site of fracture could be established: the fronto-zygomatic (FZ) suture and ZM buttress were most frequently involved in 84.5% of the cases caused by RTA, 80% caused by IPV, and 75% caused by falls. The overall involvement was 84.2%, irrespective of etiology and gender. Thus, it can be inferred that the FZ suture and ZM buttress appear the commonest sites of fracture (75 to 100%). However, the incidence of fractures of the infraorbital rim and arch was relatively lower (i.e., 37.9% and 27.4%, respectively).
Table 2. Month and Day Distribution.
| Month | No. of Cases | % | Day | No. of Cases | % |
|---|---|---|---|---|---|
| January | 4 | 4.2 | Monday | 17 | 17.9 |
| February | 9 | 9.5 | Tuesday | 14 | 14.7 |
| March | 16 | 16.8 | Wednesday | 14 | 14.7 |
| April | 3 | 3.2 | Thursday | 13 | 13.7 |
| May | 5 | 5.3 | Friday | 11 | 11.6 |
| June | 6 | 6.3 | Saturday | 10 | 10.5 |
| July | 8 | 8.4 | Sunday | 16 | 16.8 |
| August | 6 | 6.3 | |||
| September | 3 | 3.2 | |||
| October | 7 | 7.4 | |||
| November | 12 | 12.6 | |||
| December | 16 | 16.8 | |||
| Total | 95 | 100.0 | Total | 95 | 100.0 |
Table 3. Site and Etiology Distribution of Fractures of ZM Complex Alone and Those Associated with Other Facial Fractures.
| ZM Complex Only | ZM Complex + Associated Fractures | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case No. | Etiology | FZ Suture | ZM Buttress | Infraorbital Rim | Arch | LeFort 1 | LeFort 2 | LeFort 3 | Others | |||
| U/L | B/L | U/L | B/L | U/L | B/L | |||||||
| 71 | RTA | 60 (84.5%) | 60 (84.5%) | 30 (42.3%) | 20 (28.3%) | 3 (27.2%) | 4 (36%) | — | 4 (36%) | — | — | 53 (63.8%) |
| 15 | Assault/IPV | 12 (80.0%) | 12 (80.0%) | 4 (26.7%) | 5 (33.3%) | — | — | — | — | — | — | 14 (16.8%) |
| 4 | Fall | 3 (75.5%) | 3 (75.5%) | — | 1 (25%) | — | — | — | — | — | — | 10 (12%) |
| 2 | Hit (bull/cart) | 2 (100%) | 2 (100%) | — | — | — | — | — | — | — | — | 2 (2.4%) |
| 2 | Industry-related | 2 (100%) | 2 (100%) | 1 (50%) | — | — | — | — | — | — | — | 2 (2.4%) |
| 1 | Self-inflicted | 1 (100%) | 1 (100%) | 1 (100%) | — | — | — | — | — | — | — | 2 (2.4%) |
| Total = 95 | Total fractures (n = 316) | 80 (84.2%) | 80 (84.2%) | 36 (37.9%) | 26 (27.4%) | 3 (27.2%) | 4 (36%) | — | 4 (36%) | — | — | 83 (26.2%) |
| 222 (70.4%) | 11 (3.4%) | 83 (26.2%) | ||||||||||
| Total cases by category (n = 95) | 42 (44.2%) | 53 (55.8%) | ||||||||||
RTA, road traffic accident; IPV, interpersonal violence; ZM, zygomaticomaxillary; U/L, unilateral; B/L, bilateral.
Site and Etiology Distribution of Fractures of the Lower Jaw
Fifty-three cases had concomitant lower jaw fractures, totaling 83; the parasymphysis (28 fractures) and condyle (11 fractures) were most affected by RTA (Table 4). Seven parasymphysis fractures were a result of IPV; however, the angle had lesser predilection (four fractures). The symphysis (four fractures) was maximally affected by falls, followed by the parasymphysis, body, and condyle (two each). Conversely, with an etiology site correlation, RTA accounted for 53 fractures of the lower jaw, followed by IPV and falls (i.e., 14 and 10, respectively).
Table 4. Site and Etiology Distribution of Fractures of the Lower Jaw.
| Etiology | Mandibular Fractures | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| Symphysis | Parasymphysis | Body | Angle | Ramus | Condyle | Coronoid | ||
| RTA | 3 | 28 | 2 | 9 | 0 | 11 | 0 | 53 |
| IPV | 1 | 7 | 0 | 4 | 0 | 2 | 0 | 14 |
| Fall | 4 | 2 | 2 | 0 | 0 | 2 | 0 | 10 |
| Hit (bull/cart) | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 2 |
| Industry-related | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 2 |
| Self-inflicted | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 2 |
| Total No. of fractures | 83 | |||||||
RTA, road traffic accident; IPV, interpersonal violence.
Incidence of Ophthalmic Injuries in Patients with Maxillofacial Fractures
Twenty-six cases (26.82%) had subconjunctival hemorrhage followed by microhyphema in three cases (3.7%; Table 5).
Table 5. Incidence of Ophthalmic Injuries in Patients with Maxillofacial Fractures.
| Type of Injury | n (%) |
|---|---|
| Subconjunctival hemorrhage | 26 (26.82%) |
| Iritis | 0 (0%) |
| Iris sphincter tear | 0 (0%) |
| Corneal abrasion | 0 (0%) |
| Commotio retinae | 0 (0%) |
| Microhyphema | 3 (3.70%) |
| Total | 29 (30.52%) |
Associated Injuries in Patients with Maxillofacial Injury
Eighty males and 15 females had associated major injuries that required specialist intervention (Table 6). According to category, 58 patients (53 males and 5 females) had isolated maxillofacial injuries. Twelve patients each had head and orthopedic injuries (nine males and three females, respectively). Five (three males and two females) had sustained injury to the cervical spine, and eight patients (six males and two females) had sustained thoracic and abdominal injuries. From Table 6, it can be inferred that males engage in outdoor activities more often than their counterparts, combined with an aim of meeting deadlines and lack of observation of traffic rules and regulations. Also, impatience coupled with aggressive behavior influences sex-etiology incidence.
Table 6. Associated Injuries in Patients with Maxillofacial Injury.
| Site | Sex | No. of Patients (%) | |
|---|---|---|---|
| Male | Female | ||
| Isolated maxillofacial injuries | 53 | 5 | 58 (61%) |
| Head injury | 9 | 3 | 12 (12.6%) |
| Orthopedic injury | 9 | 3 | 12 (12.6%) |
| Cervical spine injury | 3 | 2 | 5 (5.3%) |
| Abdomen/thoracic injury | 6 | 2 | 8 (8.4%) |
| Total | 80 | 15 | 95 |
Complications Associated following Operative Intervention of Maxillofacial Fractures
The most frequent complications encountered were infection and occlusal disharmony (six cases each) following operative intervention (Table 7). Three cases each of residual swelling and nerve paresthesia were observed. Residual scars resulted in four cases and wound dehiscence in two patients. However, the overall complication rate observed in our study was 25.26%.
Table 7. Complications Associated Following Operative Intervention of Maxillofacial Fractures.
| Complication | n (%) |
|---|---|
| Infection | 6 (6.32%) |
| Residual swelling | 3 (3.16%) |
| Residual scars | 4 (4.21%) |
| Wound dehiscence | 2 (2.11%) |
| Infraorbital nerve paresthesia | 3 (3.16%) |
| Occlusal disharmony | 6 (6.32%) |
| Total | 24 (25.26%) |
Discussion
Factors such as geographical location, culture and socioeconomic status, and the way people are transported in a given country influence the causes and incidence of maxillofacial fractures.14 However, current knowledge of an injury or a disease is important if diagnosis is to be accurate and treatment optimal. Owing to its prominent position in the upper facial skeleton, the cheekbone appears most susceptible to injury when an impact is directed laterally upon the upper face, but a centrally directed impact does result in varying degrees of LeFort skeletal injuries. On the other hand, the mandible, owing to its prominent size and position, is more often affected when the impact is directed to the lower face. The shape of the face is influenced largely by bone scaffold, and therefore the ZM complex and arch present as important structures in facial contour.15 The brittle anatomic architecture of the midfacial region makes it the most liable to injury, causing considerable disruption in skeletal integrity, simultaneously dissipating some of the high-energy forces to the adjacent rigid zygoma and along its articulations. Hence, the cheekbone appears to bear the brunt of impact, directly or indirectly. Similarly, the lower facial skeleton exhibits such character despite its seemingly rigid constitution.
Apart from the several causes of maxillofacial trauma mentioned in the world literature, most analysts regard RTAs as the predominant etiology, followed by IPV. Other causes include industrial or occupational hazards, falls, sports accidents, and animal attacks. We observed the commonest cause of injury to be RTA (74.7%), followed by IPV (15.8%) and falls (4.2%; Fig. 1). A vast majority of RTAs involved two-wheel riders, suggesting motorbikes as the predominant mean of conveyance in this district. None of the riders were in the habit of wearing a crash helmet despite strict legislation (Table 1). Subhashraj et al reported that RTA accounted for 85% of all maxillofacial injuries; falls accounted for 7% and assault for 93% of the total.16 In a survey by Luce et al in the United States, 65% of injuries were caused by RTA and 35% by assaults, falls, or sports-related accidents.17 Vetter et al demonstrated RTA as the cause in 40% of cases with IPV almost as prevalent (i.e., 37%).15 The remaining incidents were caused by falls, sports, and work-related accidents. Gassner et al reported that 38% of facial trauma was caused by daily activity, 31% by sports, and12% by RTA.2 Fasola et al, in Nigeria, observed facial injuries to be chiefly related to vehicular crashes.18 In Sweden, alcohol or narcotic involvement in facial fracture has been reported to be as high as 56%, and most of the cases associated with violence (79%) are linked to alcohol abuse.13 A peak incidence of cases was seen in March and December, followed by November (Table 2). Scorching summers, unscheduled load-shedding, and the celebration of major festivals particularly during the latter two months of the year all contributed to an increase in case number. By week, Sundays and Mondays saw the maximum case number. Social drinking and partying on general holidays coupled with changing social lifestyles contributed to the case peak. Our pattern seemed similar to that observed in a study by Subhashraj et al.16
As for age and sex distribution, males were more frequently affected, accounting for 90.5% (86), and females accounted for just 9.5% (9), almost attaining a male-to-female ratio of 10:1.The age group of 21 to 30 years (43.2%) was predominantly affected followed by the 31- to 40-year age group (32.6%; Figs. 2 and 3). The age group of 21 to 30 years overall accounted for 41.8% of the sample age range. According to the etiology and sex distribution, men constituted the majority of victims in RTA and IPV. However, an equal incidence of falls was seen between the sexes. The age range of the sample was 17.6 years, and the average age was 31.7 ± 9.8 (standard deviation). Vetter et al observed that males attained the majority (74%), and females accounted for 26%, making the ratio nearly 3:1. The average age was 29.7 years with a range of 4 to 82 years.15 Subhashraj et al also observed that males attained the majority (78.7%) with females accounting for 21.3% of the sample and the 20- to 29-year-old age group were maximally affected (31%). The male-to-female ratio was 3.7:1, and a higher incidence of fractures was noted among the men than women, the ratio being 3 to 6.1:1.16 Iida et al, who analyzed 1502 patients with facial fractures, demonstrated a male majority of 73.9%, with females accounting for the rest. A total of 665 patients (44.3%) were between 15 and 24 years of age, and the largest subgroup was 10 to 19 years for both the sexes.19 It can be observed that our results almost concur with those of previous studies.
With regard to fracture pattern, 44.2% of cases were isolated ZM complex fractures, and the remaining had associated facial fractures (Table 3). The total number of fractures documented was 316, of which 222 were purely related to the ZM complex; however, 11 were confined only to the midface. RTA and IPV appeared to be leading causes of injury with a strong male predilection. Females, owing to age, relative physical weakness, and lesser agility, appeared more susceptible to falls. Fifty-three cases had concomitant lower jaw fractures, totaling 83 (Table 4); the parasymphysis (28 fractures) and condyle (11 fractures) were most affected by RTA. We had seven parasymphysis fractures as a result of IPV; however, the angle had lesser predilection (four fractures). The symphysis (four fractures) was maximally affected by falls, followed by the parasymphysis, body, and condyle (two each). Conversely, with an etiology-site correlation, RTA accounted for 53 fractures of the lower jaw, followed by IPV and falls (i.e., 14 and 10, respectively). Ophthalmic injuries, including subconjunctival hemorrhage (26.82%) and microhyphema, occurred in 30.52% of the sample and were managed conservatively under expert medical supervision (Table 5). Jamal et al analyzed 96 patients with ZM complex fractures and observed a 55% incidence of subconjunctival hemorrhage in 66.6% of the study sample.20 However, diplopia or traumatic optic neuropathy was not observed in any of our patients. The reason for such a huge discrepancy in the incidence of subconjunctival hemorrhage may be that a vast majority of midface fractures involved the ZM complex frequently at the FZ suture. Also, despite superior driving conditions and conformity to traffic rules and regulations, such fractures appear more frequently than others.
In general, the protocol for treating all maxillofacial fractures is open reduction and internal fixation (ORIF) to maximally achieve pretrauma occlusion and esthetics and optimally restore function. This holds true even for fractures of the ZM complex. Addressing these fractures is important because this bone chiefly imparts an esthetically appealing contour to the face, apart from protecting the globe of the eye. Intact sensory perception over the cheek is also necessary. Occlusion is of considerable importance as it influences not only lower facial height and appearance but also speech and deglutition. Mastication is an important consideration in addressing these fractures as it could affect general nutrition and well-being. However, there are some situations that may not warrant ORIF, such as undisplaced fractures involving either the rim or the buttress without the involvement of the FZ suture, together with the absence of pain on clenching and visual impairment. In case of the lower jaw, undisplaced fractures with intact occlusion are amenable to conservative treatment.
Ninety-two cases were treated with ORIF under general anesthesia. Incisions to the midface included the intraoral (vestibular), lateral brow, and transconjunctival combined with lateral canthotomy. Adjunctive procedures such as frontolateral wire suspension, Gillies' temporal approach, and transpalatal wiring (for midpalatal splits) were indicated as and when necessary. Two cases with fracture of the arch were treated with Gillies' temporal approach; one patient, however, required just soft tissue debridement and closure. Orbital charts were maintained following operative intervention on the ZM complex. Parameters assessed were pain, pupillary size and responses, proptosis, and visual acuity every 15 minutes for the first 2 hours, then every 30 minutes for the next 2 hours, and then every hour over the next 12 hours.
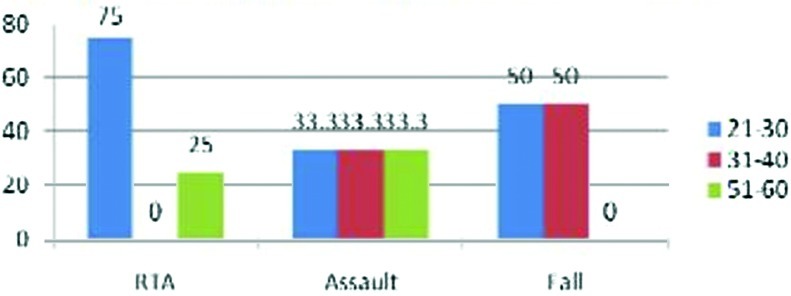
Incisions used to approach the mandible were mainly intraoral combined with extraoral, where the condyles needed to be addressed in terms of either being removed or reduced and fixed. A vast majority of the fractures were treated by ORIF, with the exception of the condyles that were favorable to closed treatment. Sixty-eight fractures of the mandible were subjected to ORIF. Of the 15 condyles fractured, three had to be removed in the event of bilateral occurrence or gross malocclusion despite unilateral involvement. However, none of the 95 cases had residual deformities at the time of presentation that required osteotomy or camouflage surgery to restore occlusion or esthetics. Standard analgesic-antibiotic regimens were followed postoperatively in all 95 cases. Major orthopedic and neurological injuries were managed by multidisciplinary approach (Table 6). Follow-up for all the patients ranged between 1 and 3 months (mean = 1.5 months). Additionally, for patients with concomitant mandibular fractures, guiding elastic therapy for 4 to 6 weeks postoperatively was advocated. Figure 4 presents an algorithm that summarizes the comprehensive management of maxillofacial fractures.
Figure 4.
Algorithm that summarizes the comprehensive management of maxillofacial fractures. GCS, Glasgow Coma Scale; CT, computed tomography; MRI, magnetic resonance image; ZMC, zygomaticomaxillary complex; ORIF, open reduction and internal fixation; ENT, ear, nose, and throat.
Complications were observed in 24 cases (Table 7); these include infection secondary to hardware rejection or poor oral hygiene leading to plate exposure at the operated site in six cases; residual swelling in the affected region in three cases; residual scars from cut/lacerated wounds and wound dehiscence (most frequent at the FZ suture, presumably due to dust contamination) in six cases. Infraorbital nerve paresthesia was seen in three cases but resolved over time with (medical) nerve-regenerative therapy. Pain radiating to temporal or infratemporal regions on the side of the fracture was evident during the immediate postoperative period in a majority of the cases but reduced over time with nonsteroidal anti-inflammatory drug therapy. Ophthalmic injuries under expert supervision resolved in all of the 29 patients. With regard to occlusal stability, we encountered problems relating to postoperative occlusion in six cases (6.32%) following surgical intervention. O'Sullivan et al reported an occlusal disharmony incidence of 8% of 100 cases.21 In view of the total number of fractures recorded and treated, the complication rate is rather disturbing. The reason of course may be many. It may well be that methods of sterilization and asepsis as also the antibiotic therapy protocols and quality of postoperative care might vary between units. Although implant materials designed for ORIF may exhibit considerable variation in physical, chemical, and mechanical properties, technical expertise and precision are also known to influence complication rates, as noted in most studies. Moreover, consistency in follow-up and documentation significantly influence such rates. Last, racial phenotype and genotype and levels of immunity differ globally and thus probably account for such variations, as observed in maxillofacial trauma units across the world.
Conclusion
In conclusion, RTAs continue to be the chief etiological factor in maxillofacial injury with males being affected predominantly. Despite improved driving conditions such as well-constructed roads, adequate illumination, appropriate guideposts and automated traffic signaling, authorized speed breaking or speed governing (in developing countries), and highway patrolling, RTAs continue to occur. IPV and falls next contribute significantly to the incidence of maxillofacial fractures. However, injuries concomitant with those of the maxillofacial region require prompt recognition and appropriate management.
As emphasized previously, the strict observance of road safety legislation and lane discipline, the prohibitive use of cellular phones while driving, legal forbiddance of drunken driving, and the incorporation of high-tech protective devices (e.g., airbags, shatterproof glass, seat belts, and collapsible steering assemblies) appear to dramatically reduce the incidence of maxillofacial injuries, particularly in developed countries.
ORIF remains the method of choice in the management of these fractures in most cases. However, advances in fixation systems have resulted in reduced immobilization time, early return to function, and minimal morbidity. Yet, complications do occur regardless of nature and accuracy of intervention. Several factors known to influence such rates are indicated in earlier studies. Nevertheless, future advances in the diagnosis, investigation, and management of maxillofacial trauma are likely to further reduce morbidity.
References
- 1.Motamedi M HK. An assessment of maxillofacial fractures: a 5-year study of 237 patients. J Oral Maxillofac Surg. 2003;61:61–64. doi: 10.1053/joms.2003.50049. [DOI] [PubMed] [Google Scholar]
- 2.Gassner R, Tuli T, Hächl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003;31:51–61. doi: 10.1016/s1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 3.Geneva, Switzerland: WHO; 1992. Statistics Annual WHO. 1992. [Google Scholar]
- 4.Bataineh A B. Etiology and incidence of maxillofacial fractures in the north of Jordan. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:31–35. doi: 10.1016/s1079-2104(98)90146-9. [DOI] [PubMed] [Google Scholar]
- 5.Tay A G, Yeow V K, Tan B K, Sng K, Huang M H, Foo C L. A review of mandibular fractures in a craniomaxillofacial trauma centre. Ann Acad Med Singapore. 1999;28:630–633. [PubMed] [Google Scholar]
- 6.Olasoji H O, Tahir A, Arotiba G T. Changing picture of facial fractures in northern Nigeria. Br J Oral Maxillofac Surg. 2002;40:140–143. doi: 10.1054/bjom.2001.0716. [DOI] [PubMed] [Google Scholar]
- 7.Oji C. Jaw fractures in Enugu, Nigeria, 1985–95. Br J Oral Maxillofac Surg. 1999;37:106–109. doi: 10.1054/bjom.1997.0083. [DOI] [PubMed] [Google Scholar]
- 8.Kieser J, Stephenson S, Liston P N, Tong D C, Langley J D. Serious facial fractures in New Zealand from 1979 to 1998. Int J Oral Maxillofac Surg. 2002;31:206–209. doi: 10.1054/ijom.2002.0208. [DOI] [PubMed] [Google Scholar]
- 9.Marker P, Nielsen A, Bastian H L. Fractures of the mandibular condyle. Part 1: patterns of distribution of types and causes of fractures in 348 patients. Br J Oral Maxillofac Surg. 2000;38:417–421. doi: 10.1054/bjom.2000.0317. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka N, Tomitsuka K, Shionoya K. et al. Aetiology of maxillofacial fracture. Br J Oral Maxillofac Surg. 1994;32:19–23. doi: 10.1016/0266-4356(94)90166-x. [DOI] [PubMed] [Google Scholar]
- 11.Oikarinen K, Ignatius E, Kauppi H, Silvennoinen U. Mandibular fractures in northern Finland in the 1980s—a 10-year study. Br J Oral Maxillofac Surg. 1993;31:23–27. doi: 10.1016/0266-4356(93)90092-b. [DOI] [PubMed] [Google Scholar]
- 12.Ogundare B O, Bonnick A, Bayley N. Pattern of mandibular fractures in an urban major trauma center. J Oral Maxillofac Surg. 2003;61:713–718. doi: 10.1053/joms.2003.50118. [DOI] [PubMed] [Google Scholar]
- 13.Strom C, Nordenram A, Fischer K. Jaw fractures in the country of Kopparberg and Stockholm 1979–1988—a retrospective comparative study of frequency and cause with special reference to assault. Swed Dent. 1991;15:285–289. [PubMed] [Google Scholar]
- 14.Gomes P P, Passeri L A, Barbosa J R. A 5-year retrospective study of zygomatico-orbital complex and zygomatic arch fractures in Sao Paulo State, Brazil. J Oral Maxillofac Surg. 2006;64:63–67. doi: 10.1016/j.joms.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 15.Vetter J D, Topazian R G, Goldberg M H, Smith D G. Facial fractures occurring in a medium-sized metropolitan area: recent trends. Int J Oral Maxillofac Surg. 1991;20:214–216. doi: 10.1016/s0901-5027(05)80177-8. [DOI] [PubMed] [Google Scholar]
- 16.Subhashraj K, Nandakumar N, Ravindran C. Review of maxillofacial injuries in Chennai, India: a study of 2748 cases. Br J Oral Maxillofac Surg. 2007;45:637–639. doi: 10.1016/j.bjoms.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 17.Luce E A, Tubb T D, Moore A M. Review of 1,000 major facial fractures and associated injuries. Plast Reconstr Surg. 1979;63:26–30. doi: 10.1097/00006534-197901000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Fasola A O, Lawoyin J O, Obiechina A E, Arotiba J T. Inner city maxillofacial fractures due to road traffic accidents. Dent Traumatol. 2003;19:2–5. doi: 10.1034/j.1600-9657.2003.00073.x. [DOI] [PubMed] [Google Scholar]
- 19.Iida S, Kogo M, Sugiura T, Mima T, Matsuya T. Retrospective analysis of 1502 patients with facial fractures. Int J Oral Maxillofac Surg. 2001;30:286–290. doi: 10.1054/ijom.2001.0056. [DOI] [PubMed] [Google Scholar]
- 20.Jamal B T, Pfahler S M, Lane K A. et al. Ophthalmic injuries in patients with zygomaticomaxillary complex fractures requiring surgical repair. J Oral Maxillofac Surg. 2009;67:986–989. doi: 10.1016/j.joms.2008.12.035. [DOI] [PubMed] [Google Scholar]
- 21.O'Sullivan S T, Snyder B J, Moore M H, David D J. Outcome measurement of the treatment of maxillary fractures: a prospective analysis of 100 consecutive cases. Br J Plast Surg. 1999;52:519–523. doi: 10.1054/bjps.1999.3159. [DOI] [PubMed] [Google Scholar]