Abstract
Colonic volvulus is a common cause of large bowel obstruction worldwide. It can affect all parts of the colon, but most commonly occurs in the sigmoid and cecal areas. This disease has been described for centuries, and was studied by Hippocrates himself. Currently, colonic volvulus is the third most common cause of large bowel obstruction worldwide, and is responsible for ∼15% of large bowel obstructions in the United States. This article will discuss the history of colonic volvulus, and the predisposing factors that lead to this disease. Moreover, the epidemiology and diagnosis of each type of colonic volvulus, along with the various treatment options will be reviewed.
Keywords: volvulus, decompression, resection, cecopexy, fixation
Objectives: Upon completion of this article, the reader should be able to summarize the different types of colonic volvuli and understand the various treatment options.
History of Volvulus
The term “volvulus” originates from the Latin volvere, or “to twist.” In the case of colonic volvulus, the term refers to the twisting of colon, most often the sigmoid, in a manner leading to obstruction, possibly leading to ischemia and gangrene. The cecum and transverse colon can also be affected. This affliction has been described for thousands of years, as have rudimentary therapies. The Papyrus Ebers, ca. 1550 BC, described the natural course of volvulus to be spontaneous reduction or “rotting” of the intestines.1 In Hippocrates' Affections, treatment for volvulus involved injecting a large quantity of air into the intestines via the anus.1 Furthermore, In the Diseases, Hippocrates advocated the insertion of a suppository 10 digits long, or ∼22 cm.1 Modern proctoscopic decompression requires similar instrument length.
The first mention of volvulus in Western literature appeared in 1841, when von Rokitansky described it as a cause of intestinal strangulation.2 Modern Western therapy began to evolve with Gay's publication of transanal volvulus reduction on the cadaver of a patient with sigmoid volvulus.1 In 1883, Atherton described surgical laparotomy and lysis of adhesions for treatment of volvulus.3 Eventually, three surgical approaches were employed for treatment of volvulus including detorsion and plication of the mesentery, colonic resection and primary anastomosis, and lastly, the Hartmann procedure. Surgical management was the mainstay of treatment through the mid-20th century.
The requirement for laparotomy in the face of volvulus was challenged by Brusgaard in 1947. He described decompression via sigmoidoscopy and placement of a rectal tube in patients without peritonitis. He reported successful decompression with a rigid proctoscope in 91 patients with sigmoid volvulus, accompanied by a mortality rate of only 14%.4,5 However, without eventual operative management, recurrence was common. After successful nonoperative decompression, there is a well-recognized propensity for recurrence, which is reportedly as high as 90%, with an attendant mortality of up to 40%.6
This approach signaled the start of transanal reduction of sigmoid volvulus, which is used today. With the improvement of technology, the surgeon has the option of not only detorsion with a rigid proctoscope, but also the introduction of the flexible sigmoidoscope. Many authors have reported success in its use to decompress volvulus not only in the sigmoid, but also in other anatomic locations, and advocate its use in patients unable to tolerate laparotomy.7,8,9,10,11 Because of high rates of recurrence, endoscopic decompression is considered a temporizing measure.
Worldwide, colonic volvulus is the third leading cause of large bowel obstruction. Populations most affected reside in the “Volvulus Belt” of Africa, the Middle East, India, and Russia. In these regions, the average age is younger than Western countries, ranging from 40 to 50 years and in generally better health.4,12 In the United States, colonic volvulus accounts for 10 to 15% of all colon obstructions,13 ranking behind cancer and diverticulitis, and between 1 to 20% of all intestinal obstructions.13 It occurs when a mobile portion of the colon twists around a fixed base, causing obstruction of a segment of colon at the point of maximal torsion. In effect, it is a closed-loop obstruction. In a study of 546 cases of colonic volvulus, it is most often found in the sigmoid (60.9%), followed by the cecum (34.5%), the transverse colon (3.6%), and splenic flexure (1%).1 It is often seen in the elderly, in patients with neuropsychiatric disorders, and those in nursing care facilities. Predisposing factors include previous episodes of volvulus, previous abdominal operations, institutionalization, megacolon, and chronic constipation.
Sigmoid Volvulus
Volvulus of the sigmoid colon is the most common form of volvulus in the United States and Western Europe, though overall it is a rare form of colonic obstruction. In other parts of the world, including Asia, Africa, and less-developed regions, it can account for 20 to 50% of intestinal obstruction.14 Lower percentages of obstruction related to sigmoid volvulus in the Western world compared with other locations could be due to the low-fiber diet consumed in Western countries leading to higher incidences of diverticulosis and colorectal cancer, leading etiologies for obstruction. Also, high-fiber diets consumed in other parts of the world can lead to elongation of the colon. This can be a predisposing factor for volvulus.
The sigmoid colon, with attachments in close proximity at its junction with the descending colon and rectum, make it a prime location for twist when elongated. In addition, an elongated mesentery can also be a predisposing factor. This was described by Treves in the 19th century: “The arrangement of the gut that is necessary for the production of a volvulus is the following: The loop must be of considerable length, the mesocolon must be long and very narrow at its parietal attachment, so that the two ends of the loop may be brought as close together as possible.”15 Treves also understood that sigmoid volvulus is generally not congenital, but “The commonest cause…is, without doubt, chronic constipation.”15 In the 1875 Handfield-Jones' Manual of Pathological Anatomy, the author states “Abnormal length of the mesentery probably predisposes to these affections.”16
The typical sigmoid volvulus patient in Treves' time was between the ages of 40 to 60, explained as “(this) circumstance of age has been explained by the greater frequency of constipation in those past middle life, and by the possibility that the condition of the gut that favors volvulus may require some years for preparation.”14 Given the increased longevity in the Western world, and low-fiber diet, it is often a disease of the elderly, and often those in institutions. Nowadays, the typical patient is elderly, living in a nursing home, often on psychotropic medications. Chronic constipation is common. Previous abdominal surgery and its subsequent adhesions, laxative abuse, and diabetes have also been cited.14,17
In the younger population, sigmoid volvulus is more often associated with megacolon and its etiologies, most often from Hirschsprung disease or Chagas disease.14 In children, age of presentation can range from 4 hours to 18 years, more commonly in boys. Symptoms can be acute or chronic, and generally are manifested by abdominal pain, distention, and vomiting.18
Adult patients will typically present with abdominal pain and distention. But as mentioned previously, the typical patient is in the hands of caregivers, who will remark that the patient has not had a bowel movement, appears distended, or is obtunded. On physical exam, the patient will be grossly distended, with or without peritoneal signs. About 30 to 41% of patients report previous episodes of gross distention.13 Symptoms may be present for up 42.5 hours in more elderly patients.19 Abdominal x-rays alone can be diagnostic in 60 to 75% of cases.19,20 Classic findings on radiology include the “bent inner tube” or “coffee bean” signs, which show a massively distended colon. In the presence of an incompetent ileocecal valve, there will also be distention of the small bowel. If additional radiologic studies are necessary, computed tomography (CT) scan or barium enema may be obtained. Barium enema along with plain films can increase diagnostic accuracy to up to 100%.21 As the appearance of dilated colon on radiographs can also be indications of neoplasm or megacolon, such diagnoses need to be ruled out. Subsequent endoscopic decompression can identify neoplasms. The presence of megacolon may alter the surgical approach, as the presence of megacolon in a patient with sigmoid volvulus leads to the greater possibility of recurrence after sigmoid colectomy.22
Treatment
Since the introduction of endoscopic detorsion in the 1940s, this approach, along with subsequent resection, has become the primary therapeutic modality. Detorsion can be performed via barium enema, rigid proctoscopy, flexible sigmoidoscopy, or colonoscopy. Some reports reveal better results with a flexible approach.23 It has been reported that 24% of sigmoidoscopic approaches will not find the site of torsion, encouraging the use of colonoscopy.10 Overall, decompression has been found to be successful in 70 to 80% of cases.14 If gangrenous bowel is encountered, the patient should be brought for emergent exploration and resection. If detorsion is successful and no ischemia or gangrenous bowel is encountered, a rectal tube is left and elective resection is scheduled. Care should be taken in the selection of patients for endoscopic detorsion. Patients with signs and symptoms of sepsis, fever, leukocytosis, and peritonitis should be taken directly to the operating room (OR) for exploration.
Whatever the technique, once the point of torsion has been passed, the surgeon should expect a rush of stool and gas. At this point, a rectal tube should be placed to avoid recurrence and secured in place. The patient should then be resuscitated, as many will be dehydrated and perhaps have electrolyte abnormalities. No time to resection has been standardized, but 48 hours for bowel preparation and resuscitation have been found to be safe.24 A formal colonoscopy should be performed to rule out malignancy, and the patient taken to the OR for resection. Although some sigmoid volvuli will not recur after decompression, as was seen in 75% of patients in a small series,13 patients can be managed successfully with multiple decompressions.25 Most evidence suggests recurrence is common and occurs in up to 90% of patients after endoscopic detorsion.6
Standard surgical practice has been exploration, with resection of the sigmoid colon. But given the age and comorbidities of the affected population, resection has been considered highly risky. That said, with advances in anesthesia and critical care technology, resection has become more feasible and safe. At the same time, other less-invasive techniques have been described. Endoscopic rectopexy, extraperitonealization of the entire sigmoid colon, laparoscopic rectopexy, and mesosigmoidoplasty have been shown to be reliable methods in both acute and elective settings.26,27,28,29,30 Laparoscopic approaches to resection have been successfully utilized. Liang reported that patients who presented with sigmoid volvulus and underwent detorsion and bowel prep were treated successfully with laparoscopic sigmoid resections. In this series, the cost versus conventional laparotomy was found to be higher.31 Another small series by Cartwright-Terry also found a laparoscopic approach to sigmoid volvulus to be safe after detorsion.32
Patients who fail endoscopic decompression, have gangrenous bowel identified on endoscopy, or who exhibit signs and symptoms of sepsis should be prepared for surgery in an expeditious fashion. The patient should be resuscitated, started on broad-spectrum antibiotics, and ingest nothing orally. If the patient is hemodynamically unstable, no further imaging or tests should be ordered and the patient should go to the OR. Exploration should be performed in a midline incision. Once the volvulus is identified, it should be assessed for viability. If the bowel appears healthy or only mildly compromised, it can be reduced and the aforementioned surgical options can be considered. If resection is indicated, the decision to create a primary anastomosis should be based on general surgical principles: the patient's nutritional status, adequacy of blood supply, presence of tension, presence of purulent or fecal peritonitis, and hemodynamic status. If there are any factors that may threaten the viability of a primary anastomosis, a Hartmann procedure should be performed. In emergent situations, the usual preoperative evaluation for stoma placement cannot be performed, but attention should be paid to the location of the stoma, as in elderly patients the likelihood is that the stoma will be permanent. The surgeon may also encounter dilated bowel, necessitating a larger incision. These patients may have a greater incidence of parastomal hernias.33 In selected patients, primary resection with anastomosis can be considered over a Hartmann procedure.
Emergent operations for colonic volvulus carry significant morbidity and mortality. In an evaluation of 106 patients who were taken to the OR without decompression or bowel prep, the overall mortality was 6.6%, and in the presence of gangrenous bowel increased to 11%.34
In a study of patients at Veterans Affairs (VA) hospitals, the mortality rate was 24% for those undergoing emergency operations for sigmoid volvulus, versus 6% for elective procedures with antecedent decompression. Mortality was correlated with emergent surgery (p < 0.01) and necrotic colon (p < 0.05).5 In a large series from Turkey, overall mortality for patients presenting with sigmoid volvulus was 15.8%, while the complication rate was 37.2%. In patients with gangrenous bowel, they found a similar mortality rate with primary anastomosis versus the Hartmann procedure of 21.6% versus 19.2%, respectively. However, when combined with operative colonic cleansing, the mortality rate for anastomosis dropped to 9.3%.35
Cecal Volvulus
The cecum is the second most common site for volvulus. The incidence of cecal volvulus is reported to range from 2.8 to 7.1 per million people per year.36 It accounts for 1 to 1.5% of all the adult intestinal obstructions and 25 to 40% of all volvulus involving the colon. Anatomically, this diagnosis involves the terminal ileum, cecum, and proximal right colon. There are two variants of cecal volvulus: the axial rotation of the proximal right colon, the cecum, and the terminal ileum around their mesentery, generally clockwise (Fig. 1A); and the anterosuperior folding of the cecum without axial rotation, commonly known as “cecal bascule” (Fig. 1B).33 Cecal bascule presents less commonly than true rotational volvulus, is less likely to cause vascular compromise, and occurs more frequently in younger female patients.37 In a Japanese study evaluating cecal volvulus,38 patients treated before 1988 showed two peaks in ages at presentation. The first spike was at 10 to 29 years of age with another at 60 to 79 years of age. In younger patients, volvulus can be caused by mesenterium commune (a common mid-dorsally attached mesentery for small and large intestine) intestinal malformation, or excessive exercise. In older patients, cecal volvulus was associated with chronic constipation, distal colon obstruction, or senile dementia. Interestingly, between 1999 and 2008, there was a change in incidence with a single peak at 70 to 79 years of age.
Figure 1.
(A) Cecal volvulus. Source: Consorti and Liu.36 (B) Cecal bascule. Reproduced with permission from Consorti and Liu.36
Patients' ages at presentation are presumably affected by cultural and dietary influences and their effects on intestinal motility, resulting in highly variable peak ages of presentation from various geographic regions, where the average age of patients reported in India is 33 years as compared with 53 years in reports from Western countries.37
The etiology of cecal volvulus is likely related to late embryogenesis; the cecum rotates counterclockwise from the left side of the abdomen to the right lower quadrant. As this occurs, the mesentery of the right colon fixates to retroperitoneal structures. If the patient has incomplete fixation, there is risk of cecal volvulus formation. Based on the autopsy of 125 cadavers, 11.2% of right colons examined were freely mobile with complete common ileocolonic mesenterium, 25.6% were found to have cecum capable of “folding,” adding up to 36.8% of cadavers potentially at risk for cecal volvulus to occur.13 Given the relatively lower incidence of cecal volvulus, other factors must be at play. Reports have shown that 23 to 53% of patients presenting with cecal volvulus have had prior abdominal surgery.36 This could be because adhesions secondary to abdominal surgery form a point of fixation for the mobile right colon to rotate about, causing the twist that leads to bowel compromise.37 Chronic constipation, distal colon obstruction, high-fiber diets, ileus, prior colonoscopy, and late pregnancy have also been identified as factors important in the development of cecal volvulus.39,40,41,42,43
Presentation is marked by either intermittent or acute obstruction. Distention may occur, although often less dramatic than in more distal volvuli. Patients will often have pain, obstipation, nausea, and vomiting. These may resolve spontaneously and recur in an intermittent pattern, known as the “mobile cecum syndrome.”44 These patients will present with intermittent right lower quadrant pain. Symptoms will improve with passage of flatus. Patients with acute obstructive or fulminant patterns will present in a similar fashion to small bowel obstruction, with obstipation, abdominal pain, and if the patient's body habitus permits, a right lower quadrant mass. If the volvulus progresses to intestinal strangulation, patients will exhibit increasing abdominal pain to peritonitis and sepsis.
If a patient's clinical presentation is suspicious for cecal volvulus, diagnosis can be ascertained with plain abdominal films. As in sigmoid volvulus, the classic finding is the “coffee bean” sign—an axial view of dilated cecum with air and fluid generally pointing to the left upper quadrant, is present in roughly half of patients. Radiographs, however, will clearly diagnose the condition in less than 20% of patients.33,37 Barium enema may be employed when diagnosis is in doubt. Characteristic finding is a “bird's beak” sign—the progressive tapering of afferent and efferent bowel loops ending at the site of torsion in the right colon. The accuracy of a barium enema and has been shown to be up to 88%. CT of the abdomen and pelvis in stable patients is another option. Like plain films, CT may reveal the coffee bean and bird beak signs, as well as the whirl sign, which is the radiographic interpretation of a soft tissue mass containing swirling strands of soft tissue and fat attenuation. A gas-filled appendix may also be seen.36
In pregnant patients, the enlarged uterus may displace a mobile cecum out of the pelvis, and obstruction may occur from the kinking of the colon at a fixed point. The now-distended colon may displace superiorly, producing torsion. Diagnosis is often delayed by the denial of usual radiographic techniques in fear of damage to the fetus. This occurs despite the feasibility of prudent use of abdominal x-rays and CT scans.45 Patients will often go to surgery without a full workup and diagnosis is made in the operating room.46
Nonsurgical treatment for cecal volvulus via endoscopy is generally considered limited and relatively ineffective. Success rates have been reported at ∼30%.36 Given the higher rate of ischemia, ineffectiveness and technical difficulty with endoscopy, colonoscopy is generally not recommended and surgical management should be the primary modality.47,48 Findings at laparotomy will dictate the surgical course. Initially, the viability of the bowel must be assessed. If gangrene is encountered, which can occur in 23 to 100% of cases, resection is mandatory.49 If the patient's ability to heal is compromised by malnutrition, anemia, chronic steroids, or other conditions, resection with ileostomy, with or without mucous fistula should be performed. Otherwise, right hemicolectomy with resection of gangrenous tissue and creation of a well-perfused anastomosis can be performed. If a gangrenous, twisted volvulus is encountered, untwisting of the affected portion is not recommended, as septic shock may result from the introduction of toxins from gangrenous loops.50 Overall mortality in patients undergoing resection for cecal volvulus is between 0 to 32%.49
If the surgeon encounters viable bowel, resection may not always be necessary. Detorsion of the bowel is possible; however, recurrence rates can reach 25 to 70%49 Other techniques include detorsion and cecopexy and/or placement of a cecostomy tube. The former procedure is performed by making a flap of peritoneum from the right paracolic gutter and affixing it to the serosa of the anterior right colon. Cecostomy entails the placement of a tube within the cecum – this both vents the distended colon and anchors it to the abdominal wall. In a large study evaluating surgical options for treating cecal volvulus, detorsion with cecopexy was found the have complication, mortality, and recurrence rates of 15%, 10%, and 13%, respectively.37 This same study found rates of complications (52%), mortality (22%), and recurrence (14%) after cecostomy. This, along with other reports of poor outcomes, suggests cecostomy as an alternative procedure for cecal volvulus should be abandoned.37 A retrospective analysis of surgical options found high mortality after detorsion and cecostomy (14.2% and 66.6%, respectively) compared with cecal resection (7.2%).37 In the final analysis, the choice of operation, whether resection or fixation, should be based on the individual's expertise, the status of the involved bowel, the patient's overall physiologic status, and an evaluation of the patient's potential for perioperative complications. Although some authors contend detorsion and fixation is a viable alternative to resection, improved perioperative anesthesia and postoperative care has made resection the preferred treatment, as it leaves the patient with no chance of recurrence.36,49,51 Given the evidence, we recommend resection.
Transverse Colon and Splenic Flexure Volvulus
Transverse colon and splenic flexure volvulus have rarely been recorded. In a study of Olmstead County, Minnesota, of reported episodes of colonic volvulus, ∼2% are splenic and 3% are of the transverse colon.1 Older reports suggest that up to 30% of cases of colonic volvulus occur in the transverse colon in Eastern European and Scandinavian countries of the Volvulus Belt, where high-residue diets are consumed.4 Patients with transverse or splenic flexure volvuli are generally younger, often in the second or third decades of life, and more likely female.14 Factors that predispose to transverse colon volvulus include distal impediment to defecation, like distal obstruction or chronic constipation, elongation and redundancy of the colon, and the narrowing of the mesenteric attachments causing the flexures to be in closer proximity, as well as absence of, or malfixation of the mesenteries, and, like other forms of volvulus, a fixed point around which the bowel can twist.52,53 Risk factors for splenic flexure volvulus include constipation, probably due to elongation of the colon, as well as prior abdominal surgery. Chilaiditi syndrome, marked by the transposition of a loop of colon, usually transverse, between the diaphragm and liver, has been cited as a potential risk factor.14 An elongated and hypermobile colon with a long mesentery is an important predisposing factor for Chilaiditi syndrome, as it is in volvulus of the transverse colon, and the surgeon should have greater clinical suspicion for volvulus should a patient present with symptoms.54,55
Patients with transverse or splenic flexure volvulus will present with symptoms akin to a large bowel obstruction. Patients will experience abdominal pain, nausea, vomiting, and constipation, either acutely or with intermittent chronic symptoms. These symptoms may be acute or chronic. In the acute setting, the patient may experience less distention but the clinical condition will worsen. In the chronic setting, the patient's overall condition will not deteriorate quickly, but may present with more abdominal distension, as with repeated episodes the colon may elongate.
Radiographic identification of transverse colon volvulus begins with abdominal plain films. The criteria for diagnosis includes (1) a markedly dilated, air-filled colon with an abrupt termination at the anatomic splenic flexure; (2) two widely separated air-fluid levels, one in the transverse colon and the other in the cecum; (3) an empty descending and sigmoid colon; and (4) a characteristic beak at the anatomic splenic flexure at a barium enema examination.56 A twist in the transverse colon may be visible as a U-shaped loop or “bent inner tube” of bowel in the upper abdomen.
However, the diagnosis is difficult, and is usually not made preoperatively. This may lead to a delay in surgical intervention, or futile attempts at endoscopic decompression with the misdiagnosis of sigmoid volvulus. Delay in definitive surgical care, as there is no conservative modality to treat transverse colon volvulus, leads to a higher rate of mortality than sigmoid or cecal volvulus. One report revealed overall mortality as 33%.53
Although endoscopic decompression is possible with transverse colon and splenic flexure volvulus, the risk of recurrence and the difficulty of detorsion make it an ineffective and possibly dangerous modality. Surgical management includes detorsion, with or without colopexy, or resection. Like other forms of volvulus, if gangrenous bowel is encountered, resection is mandatory. And in cases where viable bowel is encountered, given the risk of recurrence, the consensus holds that an extended right hemicolectomy or transverse colectomy should be undertaken. In Ballantyne et al, all patients with transverse colon volvulus died after mere detorsion.13 The decision to create a stoma should be based on feasibility of reanastomosis, the presence of fecal contamination, and the clinical condition of the patient.
Ileosigmoid Knotting
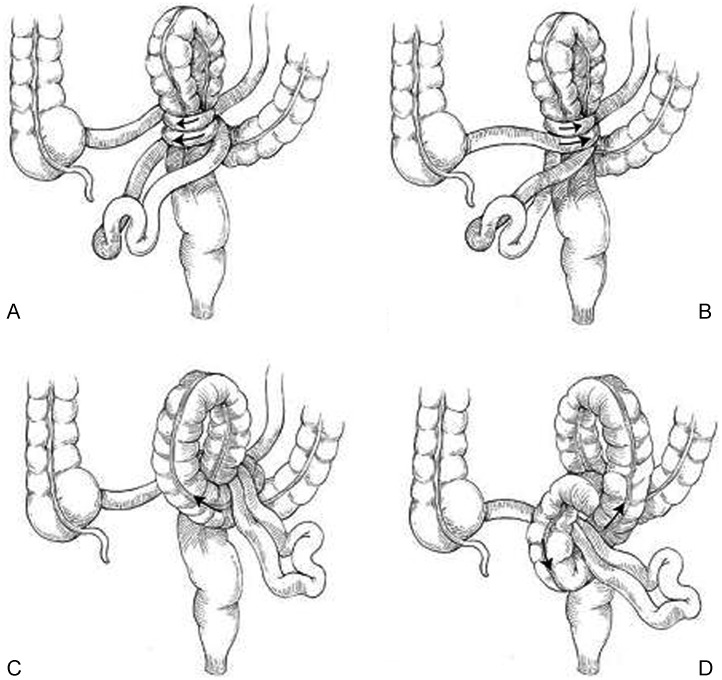
Ileosigmoid knotting—“compound volvulus” or “double volvulus”—is a rare entity and more often seen in the Middle East, Asia, and Africa than in Western countries. First described by Parker in 1845,57 only 280 cases have been described in the literature.58 Patients who develop this condition are generally younger, often 40 to 50 years of age; it is more common in men.59,60 It can progress quickly and cause gangrene of not only the sigmoid colon, but also the terminal ileum. Factors leading to this form of volvulus include a mobile small bowel on long mesentery; a redundant sigmoid colon on a narrow pedicle, and a diet high in bulk and carbohydrates with a large volume of concurrent liquid ingestion. Development of an ileosigmoid knot may also be related to the consumption of a single meal per day, as was seen in a study of the Bagandans of Uganda.61 Four specific patterns of this type of volvulus have been described in the literature. The most common is the encirclement of the sigmoid colon by the ileum in a clockwise manner. Theoretically, this form of volvulus occurs when a high-bulk, high-volume meal reaches the proximal jejunum, the increased weight in the intestine drops it into the left lower quadrant. Empty and hypermobile distal segments of jejunum and ileum then twist in a clockwise rotation around the pedicle of the sigmoid colon. As the gut peristalses, the heavy loop rotates, causing knot formation and closed loops form in the sigmoid colon and small bowel. Less commonly, the ileum wraps counterclockwise around the sigmoid colon, or the sigmoid colon wraps around the ileum in a clockwise or counterclockwise fashion. Internal herniation can cause or happen concurrently with ileosigmoid knotting. When they occur, most internal hernias are transmesenteric, through the Treves fold. They can also be transomental, intersigmoidal, pericecal, and wrap around the omphalomesenteric fibrous cord (Fig. 2).62,63
Figure 2.
Ileosigmoid knot. These schematic illustrations indicate the four forms of knotting. The active ileum may rotate around the sigmoid colon in either a clockwise (A) or counterclockwise (B) direction. Much more infrequently, the sigmoid colon may act as the active loop and rotate in either a clockwise (C) or counterclockwise (D) direction around the ileum. Source: From Beck DE, Rombeau JL, Stamos MJ, Wexner SD, eds. The ASCRS Manual of Colon and Rectal Surgery. 1st ed. New York: Springer; 2009: 426. Reprinted here with permission.
Patients will present with nausea and vomiting, abdominal distension, and pain. Chronic constipation or previous episodes will generally not be part of the history. They will usually present in worse clinical condition than other forms of volvulus, with sepsis, dehydration, acidosis, hypotension, and tachycardia. Because of the rarity of this condition, diagnosis may be delayed. Abdominal x-rays may reveal distended sigmoid in the right abdomen and a proximal small bowel obstruction in the left.64 But combined large and small bowel obstructions are not always seen.60,65 A CT scan of the abdomen may show a dilated loop of the sigmoid colon with a thinned-out wall, medially deviated distal descending colon and cecum, whirl sign, and thin, fluid-filled ileal loops with nonenhancing walls.66 A diagnostic triad consisting of a clinical evidence of small bowel obstruction in the presence of a radiographic colon obstruction and the failure of endoscopic detorsion of a suspected sigmoid volvulus was proposed in an Indian study.67 However, diagnosis is made in less than 20% of patients, and greater than 70% of patients will have gangrenous bowel at surgery.33
These patients should be resuscitated, have acid/base imbalances corrected, and urgently taken to the OR for exploration. Intraoperative options range from detorsion of the small and large bowel loops to en bloc resection. The choice of operation should depend upon anatomic variant and state of the bowel, the patient's overall operative risk, the surgeon's expertise, and facilities at hand. If the small and large bowel segments are gangrenous, these should be resected en bloc with healthy margins. Prior detorsion of gangrenous bowel puts the patient at risk of perforation and resulting fecal peritonitis and shock. If one segment is gangrenous and the other viable, resection of the dead segment may facilitate detorsion and preservation of the healthy loop. To facilitate the untying of the knot and possibly lessening the chance of recurrence, sigmoidectomy regardless of viability has been suggested.60,63,66 Deflation of the distended segments can aid in detorsion and reduce the risk of perforation.1,61,68 The Hartmann procedure is often advocated in the presence of gangrenous sigmoid colon,63,66 though coloproctostomy can be appropriate if the surgeon believes the anastomosis will be viable.33,60,63,66 In cases of resection of the ileum, anastomosis can be reestablished between viable ends. If < 10 cm of terminal ileum is viable, anastomosis should be made between the distal stump of ileum and right colon in an end-to-side fashion.60,63,66 If the cecum or right colon appear threatened, these portions should be included in the specimen and appropriate anastomosis made.60,63 Mortality for ileosigmoid knotting is high, ranging from 15 to 73%.60 Mortality is decreased if the colon is not gangrenous. Septic shock is a major cause of death. Mortality rates appear lower for younger patients without comorbidities, and though some studies show an inverse relationship between duration, symptoms, and mortality,63 others do not.33 This discrepancy can be explained by patients with severe symptoms seeking medical attention earlier. Postoperatively, adequate nutritional and metabolic support should be given.65
Greater suspicion for ileosigmoid knotting should be held by surgeons in patients with acute abdomens in countries making up the Volvulus Belt, as prompt resuscitation and laparotomy are essential for survival.
Conclusion
Volvulus of the colon is a common cause of large bowel obstruction. It is a potentially fatal condition whose etiology has been recognized for centuries. It can occur at different points in the colon, in patients of all ages, and risk factors include a high-fiber diet. Technological advances in imaging have assisted surgeons in making the diagnosis. Although some conservative measures can be applied to ameliorate the symptoms caused by volvulus, surgical resection is the most definitive approach in treating this condition, regardless of location.
References
- 1.Ballantyne G H. Review of sigmoid volvulus: history and results of treatment. Dis Colon Rectum. 1982;25(5):494–501. doi: 10.1007/BF02553666. [DOI] [PubMed] [Google Scholar]
- 2.von Rokitansky C. Wien, Germany: Braumüller u. Seidel; 1841. Handbuch der Pathologischen Anatomie. Vol. I, Anatomie. [Google Scholar]
- 3.Case by Dr. Atherton. Boston Med Surg J. 1883;CVIII(24):553. [Google Scholar]
- 4.Bruusgaard C. Volvulus of the sigmoid colon and its treatment. Surgery. 1947;22(3):466–478. [PubMed] [Google Scholar]
- 5.Grossmann E M, Longo W E, Stratton M D, Virgo K S, Johnson F E. Sigmoid volvulus in Department of Veterans Affairs Medical Centers. Dis Colon Rectum. 2000;43(3):414–418. doi: 10.1007/BF02258311. [DOI] [PubMed] [Google Scholar]
- 6.Hines J R, Geurkink R E, Bass R T. Recurrence and mortality rates in sigmoid volvulus. Surg Gynecol Obstet. 1967;124(3):567–570. [PubMed] [Google Scholar]
- 7.Orchard J L, Mehta R, Khan A H. The use of colonoscopy in the treatment of colonic volvulus: three cases and review of the literature. Am J Gastroenterol. 1984;79(11):864–867. [PubMed] [Google Scholar]
- 8.Anderson M J Sr, Okike N, Spencer R J. The colonoscope in cecal volvulus: report of three cases. Dis Colon Rectum. 1978;21(1):71–74. doi: 10.1007/BF02586552. [DOI] [PubMed] [Google Scholar]
- 9.Joergensen K, Kronborg O. The colonoscope in volvulus of the transverse colon. Dis Colon Rectum. 1980;23(5):357–358. doi: 10.1007/BF02586847. [DOI] [PubMed] [Google Scholar]
- 10.Brothers T E, Strodel W E, Eckhauser F E. Endoscopy in colonic volvulus. Ann Surg. 1987;206(1):1–4. doi: 10.1097/00000658-198707000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghazi A, Shinya H, Wolfe W I. Treatment of volvulus of the colon by colonoscopy. Ann Surg. 1976;183(3):263–265. doi: 10.1097/00000658-197603000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heis H A, Bani-Hani K E, Rabadi D K. et al. Sigmoid volvulus in the Middle East. World J Surg. 2008;32(3):459–464. doi: 10.1007/s00268-007-9353-3. [DOI] [PubMed] [Google Scholar]
- 13.Ballantyne G H, Brandner M D, Beart R W Jr, Ilstrup D M. Volvulus of the colon. Incidence and mortality. Ann Surg. 1985;202(1):83–92. doi: 10.1097/00000658-198507000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hellinger M D Steinhagen R M Colonic volvulus 1st ed. New York: Springer; 2009286–298. [Google Scholar]
- 15.Treves F. Philadelphia, PA: HC Lea's Son & Co.; 1884. Intestinal obstruction; p. 135. [Google Scholar]
- 16.Jones C H, Sieveking E H. Philadelphia, PA: Lindsay; 1875. The mouth-faces-the teeth-the pharynx- esophagus-the peritoneum-stomach-intestinal canal-the intestinal contents; p. 578. [Google Scholar]
- 17.Friedman J D, Odland M D, Bubrick M P. Experience with colonic volvulus. Dis Colon Rectum. 1989;32(5):409–416. doi: 10.1007/BF02563694. [DOI] [PubMed] [Google Scholar]
- 18.Salas S, Angel C A, Salas N, Murillo C, Swischuk L. Sigmoid volvulus in children and adolescents. J Am Coll Surg. 2000;190(6):717–723. doi: 10.1016/s1072-7515(00)00270-2. [DOI] [PubMed] [Google Scholar]
- 19.Atamanalp S S, Ozturk G. Sigmoid volvulus in the elderly: outcomes of a 43-year, 453-patient experience. Surg Today. 2011;41(4):514–519. doi: 10.1007/s00595-010-4317-x. [DOI] [PubMed] [Google Scholar]
- 20.Mangiante E C, Croce M A, Fabian T C, Moore O F III, Britt L G. Sigmoid volvulus. A four-decade experience. Am Surg. 1989;55(1):41–44. [PubMed] [Google Scholar]
- 21.Ballantyne G H. Sigmoid volvulus: high mortality in county hospital patients. Dis Colon Rectum. 1981;24(7):515–520. doi: 10.1007/BF02604311. [DOI] [PubMed] [Google Scholar]
- 22.Chung Y F, Eu K W, Nyam D C, Leong A F, Ho Y H, Seow-Choen F. Minimizing recurrence after sigmoid volvulus. Br J Surg. 1999;86(2):231–233. doi: 10.1046/j.1365-2168.1999.01034.x. [DOI] [PubMed] [Google Scholar]
- 23.Turan M, Sen M, Karadayi K. et al. Our sigmoid colon volvulus experience and benefits of colonoscope in detortion process. Rev Esp Enferm Dig. 2004;96(1):3. doi: 10.4321/s1130-01082004000100005. [DOI] [PubMed] [Google Scholar]
- 24.Tsai M S, Lin M T, Chang K J, Wang S M, Lee P H. Optimal interval from decompression to semi-elective operation in sigmoid volvulus. Hepatogastroenterology. 2006;53(69):354–356. [PubMed] [Google Scholar]
- 25.Theuer C, Cheadle W G. Volvulus of the colon. Am Surg. 1991;57(3):145–150. [PubMed] [Google Scholar]
- 26.Choi D, Carter R. Endoscopic sigmoidopexy: a safer way to treat sigmoid volvulus? J R Coll Surg Edinb. 1998;43(1):64. [PubMed] [Google Scholar]
- 27.Bhatnagar B N, Sharma C L. Nonresective alternative for the cure of nongangrenous sigmoid volvulus. Dis Colon Rectum. 1998;41(3):381–388. doi: 10.1007/BF02237496. [DOI] [PubMed] [Google Scholar]
- 28.Miller R, Roe A M, Eltringham W K, Espiner H J. Laparoscopic fixation of sigmoid volvulus. Br J Surg. 1992;79(5):435. doi: 10.1002/bjs.1800790521. [DOI] [PubMed] [Google Scholar]
- 29.Akgun Y. Mesosigmoplasty as a definitive operation in treatment of acute sigmoid volvulus. Dis Colon Rectum. 1996;39(5):579–581. doi: 10.1007/BF02058715. [DOI] [PubMed] [Google Scholar]
- 30.Subrahmanyam M. Mesosigmoplasty as a definitive operation for sigmoid volvulus. Br J Surg. 1992;79(7):683–684. doi: 10.1002/bjs.1800790731. [DOI] [PubMed] [Google Scholar]
- 31.Liang J T, Lai H S, Lee P H. Elective laparoscopically assisted sigmoidectomy for the sigmoid volvulus. Surg Endosc. 2006;20(11):1772–1773. doi: 10.1007/s00464-005-0665-9. [DOI] [PubMed] [Google Scholar]
- 32.Cartwright-Terry T, Phillips S, Greenslade G L, Dixon A R. Laparoscopy in the management of closed loop sigmoid volvulus. Colorectal Dis. 2008;10(4)(Issue 4):370–372. doi: 10.1111/j.1463-1318.2007.01340.x. [DOI] [PubMed] [Google Scholar]
- 33.Rakinic J Colonic volvulus 2nd ed. New York: Springer; 2011395–406. [Google Scholar]
- 34.Kuzu M A, Aşlar A K, Soran A, Polat A, Topcu O, Hengirmen S. Emergent resection for acute sigmoid volvulus: results of 106 consecutive cases. Dis Colon Rectum. 2002;45(8):1085–1090. doi: 10.1007/s10350-004-6364-0. [DOI] [PubMed] [Google Scholar]
- 35.Oren D, Atamanalp S S, Aydinli B. et al. An algorithm for the management of sigmoid colon volvulus and the safety of primary resection: experience with 827 cases. Dis Colon Rectum. 2007;50(4):489–497. doi: 10.1007/s10350-006-0821-x. [DOI] [PubMed] [Google Scholar]
- 36.Consorti E T, Liu T H. Diagnosis and treatment of caecal volvulus. Postgrad Med J. 2005;81(962):772–776. doi: 10.1136/pgmj.2005.035311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rabinovici R, Simansky D A, Kaplan O, Mavor E, Manny J. Cecal volvulus. Dis Colon Rectum. 1990;33(9):765–769. doi: 10.1007/BF02052323. [DOI] [PubMed] [Google Scholar]
- 38.Katoh T, Shigemori T, Fukaya R, Suzuki H. Cecal volvulus: report of a case and review of Japanese literature. World J Gastroenterol. 2009;15(20):2547–2549. doi: 10.3748/wjg.15.2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tejler G, Jiborn H. Volvulus of the cecum. Report of 26 cases and review of the literature. Dis Colon Rectum. 1988;31(6):445–449. doi: 10.1007/BF02552614. [DOI] [PubMed] [Google Scholar]
- 40.Montes H, Wolf J. Cecal volvulus in pregnancy. Am J Gastroenterol. 1999;94(9):2554–2556. doi: 10.1111/j.1572-0241.1999.01394.x. [DOI] [PubMed] [Google Scholar]
- 41.Alinovi V, Herzberg F P, Yannopoulos D, Vetere P F. Cecal volvulus following cesarean section. Obstet Gynecol. 1980;55(1):131–134. [PubMed] [Google Scholar]
- 42.Anderson J R, Spence R A, Wilson B G, Hanna W A. Gangrenous caecal volvulus after colonoscopy. Br Med J (Clin Res Ed) 1983;286(6363):439–440. doi: 10.1136/bmj.286.6363.439-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Radin D R, Halls J M. Cecal volvulus: a complication of colonoscopy. Gastrointest Radiol. 1986;11(1):110–111. doi: 10.1007/BF02035046. [DOI] [PubMed] [Google Scholar]
- 44.Rogers R L, Harford F J. Mobile cecum syndrome. Dis Colon Rectum. 1984;27(6):399–402. doi: 10.1007/BF02553011. [DOI] [PubMed] [Google Scholar]
- 45.Hogan B A, Brown C J, Brown J A. Cecal volvulus in pregnancy: report of a case and review of the safety and utility of medical diagnostic imaging in the assessment of the acute abdomen during pregnancy. Emerg Radiol. 2008;15(2):127–131. doi: 10.1007/s10140-007-0642-9. [DOI] [PubMed] [Google Scholar]
- 46.Chase D M, Sparks D A, Dawood M Y, Perry E. Cecal volvulus in a multiple-gestation pregnancy. Obstet Gynecol. 2009;114(2 Pt 2):475–477. doi: 10.1097/AOG.0b013e3181989578. [DOI] [PubMed] [Google Scholar]
- 47.Friedman J D, Odland M D, Bubrick M P. Experience with colonic volvulus. Dis Colon Rectum. 1989;32(5):409–416. doi: 10.1007/BF02563694. [DOI] [PubMed] [Google Scholar]
- 48.Renzulli P, Maurer C A, Netzer P, Büchler M W. Preoperative colonoscopic derotation is beneficial in acute colonic volvulus. Dig Surg. 2002;19(3):223–229. doi: 10.1159/000064217. [DOI] [PubMed] [Google Scholar]
- 49.Madiba T E, Thomson S R, Church J M. The management of cecal volvulus. DCR. 2002;45(2):264–267. doi: 10.1007/s10350-004-6158-4. [DOI] [PubMed] [Google Scholar]
- 50.Tuech J J, Becouarn G, Cattan F, Arnaud J P. Volvulus of the right colon. Plea for right hemicolectomy. Apropos of a series of 23 casesxd. J Chir (Paris) 1996;133(6):267–269. [PubMed] [Google Scholar]
- 51.Ostergaard E, Halvorsen J F. Volvulus of the caecum. An evaluation of various surgical procedures. Acta Chir Scand. 1990;156(9):629–631. [PubMed] [Google Scholar]
- 52.Zinkin L D, Katz L D, Rosin J D. Volvulus of the transverse colon: report of case and review of the literature. Dis Colon Rectum. 1979;22(7):492–496. doi: 10.1007/BF02586939. [DOI] [PubMed] [Google Scholar]
- 53.Loke K L, Chan C S. Case report: transverse colon volvulus: unusual appearance on barium enema and review of the literature. Clin Radiol. 1995;50(5):342–344. doi: 10.1016/s0009-9260(05)83431-2. [DOI] [PubMed] [Google Scholar]
- 54.Orangio G R, Fazio V W, Winkelman E, McGonagle B A. The Chilaiditi syndrome and associated volvulus of the transverse colon. An indication for surgical therapy. Dis Colon Rectum. 1986;29(10):653–656. doi: 10.1007/BF02560330. [DOI] [PubMed] [Google Scholar]
- 55.Kurt Y, Demirbas S, Bilgin G. et al. Colonic volvulus associated with Chilaiditi's syndrome: report of a case. Surg Today. 2004;34(7):613–615. doi: 10.1007/s00595-004-2751-3. [DOI] [PubMed] [Google Scholar]
- 56.Mindelzun R E, Stone J M. Volvulus of the splenic flexure: radiographic features. Radiology. 1991;181(1):221–223. doi: 10.1148/radiology.181.1.1887035. [DOI] [PubMed] [Google Scholar]
- 57.Parker E. Case of intestinal obstruction: sigmoid flexure strangulated by the ileum. Edinb Med Surg J. 1845;64:306–308. [Google Scholar]
- 58.Machado N O. Ileosigmoid knot: a case report and literature review of 280 cases. Ann Saudi Med. 2009;29(5):402–406. doi: 10.4103/0256-4947.55173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Akgun Y. Management of ileosigmoid knotting. Br J Surg. 1997;84(5):672–673. [PubMed] [Google Scholar]
- 60.Kotisso B, Bekele A. Ilio-sigmoid knotting in Addis Ababa: a three-year comprehensive retrospective analysis. Ethiop Med J. 2006;44(4):377–383. [PubMed] [Google Scholar]
- 61.Shepherd J J. Ninety-two cases of ileosigmoid knotting in Uganda. Br J Surg. 1967;54(6):561–566. doi: 10.1002/bjs.1800540615. [DOI] [PubMed] [Google Scholar]
- 62.Alver O, Oren D, Tireli M, Kayabaşi B, Akdemir D. Ileosigmoid knotting in Turkey. Review of 68 cases. Dis Colon Rectum. 1993;36(12):1139–1147. doi: 10.1007/BF02052263. [DOI] [PubMed] [Google Scholar]
- 63.Alver O, Oren D, Apaydin B, Yiğitbaşi R, Ersan Y. Internal herniation concurrent with ileosigmoid knotting or sigmoid volvulus: Presentation of 12 patients. Surgery. 2005;137(3):372–377. doi: 10.1016/j.surg.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 64.Young W S, White A, Grave G F. The radiology of ileosigmoid knot. Clin Radiol. 1978;29(2):211–216. doi: 10.1016/s0009-9260(78)80241-4. [DOI] [PubMed] [Google Scholar]
- 65.Puthu D, Rajan N, Shenoy G M, Pai S U. The ileosigmoid knot. Dis Colon Rectum. 1991;34(2):161–166. doi: 10.1007/BF02049992. [DOI] [PubMed] [Google Scholar]
- 66.Baheti A D, Patel D, Hira P, Babu D. Ileosigmoid knot: A case report. Indian J Radiol Imaging. 2011;21(2):147–149. doi: 10.4103/0971-3026.82301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Raveenthiran V. The ileosigmoid knot: new observations and changing trends. Dis Colon Rectum. 2001;44(8):1196–1200. doi: 10.1007/BF02234644. [DOI] [PubMed] [Google Scholar]
- 68.Kedir M, Kotisso B, Messele G. Ileosigmoid knotting in Gondar teaching hospital north-west Ethiopia. Ethiop Med J. 1998;36(4):255–260. [PubMed] [Google Scholar]