Abstract
Campylobacter jejuni is the most common bacterium that causes diarrhea worldwide, and chickens are considered the main reservoir of this pathogen. This study investigated the effects of serial truncation of lipooligosaccharide (LOS), a major component of the outer membrane of C. jejuni, on its bile resistance and intestinal colonization ability in chickens. Genes encoding manno-heptose synthetases or glycosyltransferases were inactivated to generate isogenic mutants. Serial truncation of the LOS core oligosaccharide caused a stepwise increase in susceptibilities of two C. jejuni strains, NCTC 11168 and 81-176, to bile acids. Inactivation of hldE, hldD, or waaC caused severe truncation of the core oligosaccharide, which greatly increased the susceptibility to bile acids. Both wild-type strains grew normally in chicken intestinal extracts, whereas the mutants with severe oligosaccharide truncation were not detected 12 h after inoculation. These mutants attained viable bacterial counts in the bile acid-free extracts 24 h after inoculation. The wild-type strain 11-164 was present in the cecal contents at >107 CFU/g on 5 days after challenge infection and after this time period, whereas its hldD mutant was present at <103 CFU/g throughout the experimental period. Trans-complementation of the hldD mutant with the wild-type hldD allele completely restored the in vivo colonization level to that of the wild-type strain. Mutants with a shorter LOS had higher hydrophobicities. Thus, the length of the LOS core oligosaccharide affected the surface hydrophobicity and bile resistance of C. jejuni as well as its ability to colonize chicken intestines.
Introduction
Campylobacter are curved-to-spiral shaped, flagellated gram-negative rods that grow under microaerophilic or anaerobic conditions [1]. Of the 25 species in the genus [2], C. jejuni and its close relative C. coli are the most important foodborne pathogens (hereafter collectively referred to as Campylobacter). Campylobacter is one of the most common bacterial causes of diarrhea in industrialized and developing countries, with approximately 400 million cases per year worldwide [3]. The annual economic burden of Campylobacter infections, based on medical costs and productivity loss in the USA, was estimated to be 1.5–8.0 billion dollars [4]. Campylobacteriosis is a typical self-limited enteritis, although C. jejuni strains with specific lipooligosaccharide (LOS) structures are known causative agents of an acute neuromuscular paralysis, Guillain–Barré syndrome, which develops 1–2 weeks after infections [5]. Although Campylobacter bacteremia is uncommon, systemic C. jejuni infections have been reported in the elderly, infants younger than 12 months, and patients with underlying conditions such as liver cirrhosis, human immunodeficiency virus disease, and therapy-induced immunosuppression [6], [7].
C. jejuni colonizes the intestinal tracts of various wild and domestic animals, and it persists in untreated and adequately treated aquatic environments. Avian species such as poultry and wild birds are considered the main reservoir of C. jejuni [8]–[11]. Most cases of campylobacteriosis are associated with the consumption of contaminated raw or undercooked poultry meat or other foods contaminated by these items through preparations [12]. An ice water immersion chilling step is suspected to be a major cause of fecal contamination during chicken meat processing [13]. The reduction of C. jejuni contamination in the food chain is an important step in the control of campylobacteriosis. One approach is to prevent C. jejuni colonization of broiler chickens. To successfully colonize chicken intestinal tracts, C. jejuni needs to tolerate various environmental stresses such as pH variation, low oxygen, nutrient limitation, elevated osmotic pressure, and digestive fluids including bile acids [14]. Understanding these stress resistance mechanisms may help to develop novel measures to control Campylobacter colonization in chickens.
In humans, bile is produced in the liver and stored in the gall bladder. After the ingestion of food, bile is secreted from the gall bladder into the duodenum, which helps digestion and absorption of dietary fats and fat-soluble vitamins. Bile consists of bile acids, pigments, phospholipids, and cholesterol. Bile acids are synthesized from cholesterol via a multienzyme process and promote fat absorption by producing polymolecular aggregates known as micelles [15]. Bile acids display antimicrobial activity by inducing membrane damage and oxidative stress to bacterial DNA [16], [17]. To overcome the antimicrobial effect of bile acids, enteric bacteria have evolved multiple mechanisms including active efflux, modulation of the synthesis of lipopolysaccharide (LPS) and porins, and production of bile acid hydrolase [16], [17]. Active efflux by the CmeABC system is a well-characterized bile resistance mechanism in C. jejuni. Functional disruption of this system results in substantial decreases in C. jejuni resistance to various antimicrobials including bile acids [18] and the loss of its ability to colonize chicken intestinal tracts [19]. The relationship between outer membrane integrity and bile resistance of C. jejuni remains unclear.
LOS is a major component of the outer membrane of gram-negative bacteria, including the genera Neisseria, Haemophilus, Bordetella, Branhamella, and Campylobacter [20]. Unlike LPS, LOS lacks the repeating polysaccharide O antigen and is composed of covalently linked domains, i.e., lipid A, a hydrophobic anchor, and a core oligosaccharide (OS) that consists of inner and outer core regions. More specifically, two 3-deoxy-d-manno-octulosonic acid (Kdo) residues are linked to lipid A and two l-glycero-d-manno-heptose residues are linked to Kdo in the inner core region of LOS in C. jejuni strains for which the LOS structure has been determined previously. Kdo is highly conserved in gram-negative bacteria and is essential for cell growth [21], whereas l-glycero-d-manno-heptose is not [22]. Malfunctioning of ADP-l-glycero-d-manno-heptose synthetases or heptosyltransferases that truncate the inner core region of C. jejuni reduces virulence and increases the susceptibility of the microbe to several types of detergents [22]–[24]. Jeon et al. reported that mutation in waaF, a gene encoding a heptosyltransferase, in C. jejuni reduced minimum inhibitory concentration (MIC) of polymyxin B and sodium dodecyl sulfate (SDS), whereas the mutant showed no changes in MIC of choleate [23]. Naito et al. showed that a waaF mutant exhibited significantly reduced intestinal colonization in mice [25]. However, the effect of structural changes in LOS on the C. jejuni susceptibility to bile acids remains unclear.
In this study, we constructed C. jejuni mutants with serial LOS OS truncations and compared their susceptibilities to bile acids with those of the wild-type strains. Colonization of the chicken intestinal tract by the mutants was also compared with that by the wild-type strains. This work provides a greater understanding of the minimum LOS core structures in C. jejuni that facilitate the tolerance of this pathogen to bile acids and promote its colonization of chicken intestinal tracts.
Results
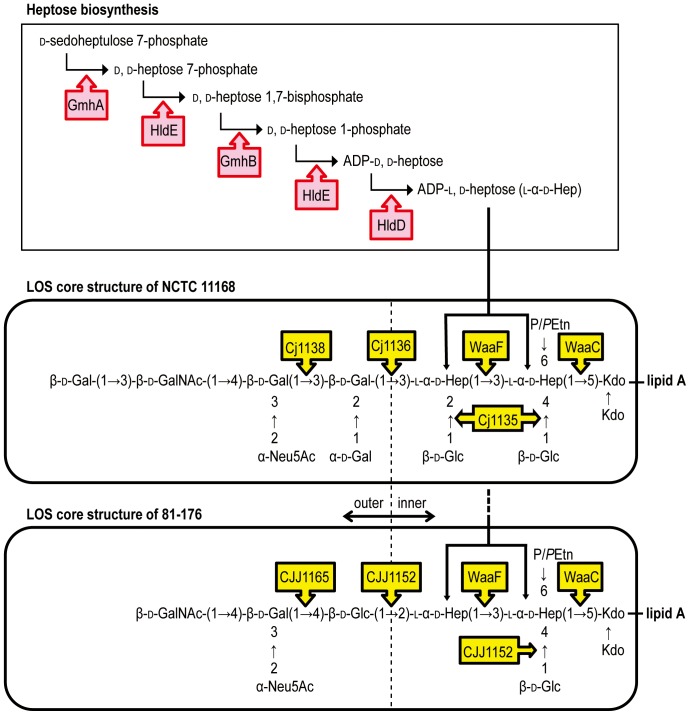
LOS mobilities of C. jejuni strains determined by tricine-SDS-PAGE
Isogenic mutants of the following genes were constructed: gmhA (cj1149), hldE (cj1150), hldD (cj1151), waaC (cj1133), waaF (cj1148), cj1135, cj1136, and cj1138 in C. jejuni NCTC 11168; and gmhA, hldE, hldD, waaC, waaF, cjj1152, and cjj1165 in C. jejuni 81-176 (Table 1). These genes were predicted to code for manno-heptose synthetases or glycosyltransferases, as indicated in Fig. 1 [25]–[27]. gmhB (cj1152) is essential for C. jejuni [22] and therefore was not inactivated in either of the strains used in this study. Complementations were performed for all LOS-truncated mutants.
Table 1. Plasmids and bacterial strains used in this study.
| Plasmid or strain | Description | Source or reference |
| Plasmids | ||
| pGem-T Easy | PCR cloning vector, Ampr | Promega |
| pUOA18 | E. coli-C. jejuni shuttle vector, Cmr | [38] |
| pUOA18Km | pUOA18 modified to replace cat with kan | This study |
| pUOA18Km-hldE | pUOA18Km with hldE (cj1150) | This study |
| pUOA18Km-hldD | pUOA18Km with hldD (cj1151) | This study |
| pUOA18Km-waaC | pUOA18Km with waaC (cj1133) | This study |
| pUOA18Km-waaF | pUOA18Km with waaF (cj1148) | This study |
| pUOA18Km-cj1135 | pUOA18Km with cj1135 | This study |
| pUOA18Km-cj1136 | pUOA18Km with cj1136 | This study |
| pUOA18Km-cj1138 | pUOA18Km with cj1138 | This study |
| pUOA18Km-cjj1152 | pUOA18Km with cjj1152 | This study |
| pUOA18Km-cjj1165 | pUOA18Km with cjj1165 | This study |
| pRK2013 | helper plasmid for triparental mating, Kmr | [41] |
| Strains | ||
| C. jejuni parental strains | ||
| NCTC 11168 | Wild type; human isolate | [28] |
| 81-176 | Wild type; human isolate | [55] |
| 11-164 | Wild type; chicken isolate, Nalr | This study |
| C. jejuni mutant strains | ||
| 168gmhA | NCTC 11168 derivative; gmhA mutant | This study |
| 168hldE | NCTC 11168 derivative; hldE mutant | This study |
| 168hldD | NCTC 11168 derivative; hldD mutant | This study |
| 168waaC | NCTC 11168 derivative; waaC mutant | This study |
| 168waaF | NCTC 11168 derivative; waaF mutant | This study |
| 168cj1135 | NCTC 11168 derivative; cj1135 mutant | This study |
| 168cj1136 | NCTC 11168 derivative; cj1136 mutant | This study |
| 168cj1138 | NCTC 11168 derivative; cj1138 mutant | This study |
| 168kpsS | NCTC 11168 derivative; kpsS mutant | This study |
| 168hldEc | 168hldE/pUOA18Km-hldE | This study |
| 168hldDc | 168hldD/pUOA18Km-hldD | This study |
| 168waaCc | 168waaC/pUOA18Km-waaC | This study |
| 168waaFc | 168waaF/pUOA18Km-waaF | This study |
| 168cj1135c | 168cj1135/pUOA18Km-cj1135 | This study |
| 168cj1136c | 168cj1136/pUOA18Km-cj1136 | This study |
| 168cj1138c | 168cj1138/pUOA18Km-cj1138 | This study |
| 817gmhA | 81-176 derivative; gmhA mutant | This study |
| 817hldE | 81-176 derivative; hldE mutant | This study |
| 817hldD | 81-176 derivative; hldD mutant | This study |
| 817waaC | 81-176 derivative; waaC mutant | This study |
| 817waaF | 81-176 derivative; waaF mutant | This study |
| 817cjj1152 | 81-176 derivative; cjj1152 mutant | This study |
| 817cjj1165 | 81-176 derivative; cjj1165 mutant | This study |
| 817kpsS | NCTC 11168 derivative; kpsS mutant | This study |
| 817hldEc | 817hldE/pUOA18Km-hldE | This study |
| 817hldDc | 817hldD/pUOA18Km-hldD | This study |
| 817waaCc | 817waaC/pUOA18Km-waaC | This study |
| 817waaFc | 817waaF/pUOA18Km-waaF | This study |
| 817cjj1152c | 817cjj1152/pUOA18Km-cjj1152 | This study |
| 817cjj1165c | 817cjj1165/pUOA18Km-cjj1165 | This study |
| 164hldE | 11-164 derivative; hldE mutant | This study |
| 164hldD | 11-164 derivative; hldD mutant | This study |
| 164waaC | 11-164 derivative; waaC mutant | This study |
| 164waaF | 11-164 derivative; waaF mutant | This study |
| 164hldDc | 164hldD/pUOA18Km-hldD | This study |
| E. coli DH5α | cloning strain | Takara |
Figure 1. Hypothetical pathways of LOS biosynthesis in C. jejuni NCTC 11168 and 81-176.
The enzymes are indicated by arrow boxes. Abbreviations: GalNAc, N-acetylgalactosamine; Neu5Ac, N-acetylneuraminic acid; Gal, galactose; Glc, glucose; Hep, heptose; P/PEtn, phosphate or pyrophosphoethanolamine; Kdo, 2-keto-3-deoxy-d-manno-octulosonic acid.
To confirm LOS truncations in each mutant, LOS samples were analyzed by tricine-SDS-PAGE, followed by silver staining (Fig. 2A). LOS produced by each mutant constructed in this study migrated more quickly than that produced by wild-type strains, with the exceptions of 168gmhA and 817gmhA. A previous whole genome analysis showed that NCTC 11168 contained two copies of the heptose isomerase gene: gmhA (cj1149 located in the LOS gene cluster) and gmhA2 (cj1424 located in the Capsular polysaccharide (CPS) gene cluster) [28]. Karlyshev et al. [26] reported that mutations in either gene in NCTC 11168 did not affect LOS and CPS expression, whereas mutation in both gmhA and gmhA2 resulted in the loss of CPS 6-O-methylheptose and LOS truncation.
Figure 2. LOS profiles and LOS OS structures of the C. jejuni wild-type strains (NCTC 11168 and 81-176) and mutants.
(A) LOS samples were analyzed by tricine-SDS-PAGE using 16% tricine gels and visualized by silver staining. The positions of the protein size markers are indicated on the left of each panel. (B) The LOS structures of 168hldE, 168hldD, 168cj1135, 168cj1136, 168cj1138, 817hldE, and 817hldD were analyzed by MALDI-TOF MS and GC-MS in this study. The wild-type strains and other mutants with asterisks have structures similar to those determined in previous studies [24]–[26], [52]–[54]. Abbreviations, refer to the legend of Fig. 1.
Glycosyltransferase mutants, i.e., 168waaC, 168waaF, 168cj1135, 168cj1136, 168cj1138, 817waaC, 817waaF, 817cjj1152, and 817cjj1165, exhibited increased LOS mobility in a stepwise manner, as reported previously [25], [26]. The mobility of LOS produced by the hldE and hldD mutants was identical and was slightly lower than that of LOS produced by the waaC mutant derived from NCTC 11168 and 81-176. The LOS bands of 168waaC and 817waaC were faint compared with those of other strains. Thus, the surface properties of these strains may be different from those of other strains. The LOS migration characteristics of all complemented strains were identical to those of their wild-type strains.
LOS structures of C. jejuni mutants determined by mass spectrometry
The LOS structures of 168hldE, 168hldD, 168cj1135, 168cj1136, 168cj1138, 817hldE, and 817hldD were determined by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) and gas chromatography-mass spectrometry (GC-MS) for the first time in the present study and are shown in Fig. 2B. OS produced by 168cj1138 had an intact inner core with one galactose residue, whereas OS produced by 168cj1136 lacked all residues on the outer core. 168cj1135 contained no glucose or galactose residues in its OS, and the truncated molecule comprised heptose, Kdo, and phosphate or pyrophosphorylethanolamine (P/PEtn) (Table S1). The MALDI-TOF MS spectra of the intact LOS produced by the hldE (168hldE and 817hldE) and hldD (168hldD and 817hldD) mutants contained four intense ions, with one ion corresponding to the lipid A fragment ([M-H-H2O] at m/z 1904), and the intervals were observed at Δm/z 219–222 (Table S2). Only Kdo was detected in the GC mass spectra, whereas l-glycero-d-manno-heptose and d-glycero-d-manno-heptose were not observed in the OS samples obtained from the mutants.
Effects of LOS truncations on antimicrobial resistance
As shown in Table 2, MICs of cholic acid, deoxycholic acid, and taurocholic acid for 168waaF, 168cj1135, 168cj1136, and 168cj1138 were ≥2-fold smaller than those for NCTC 11168 and 168gmhA, while no difference was observed for other bile acids. MICs of the five bile acids used in this study for 168hldE, 168hldD, and 168waaC were 4- to >32-fold lower than those for NCTC 11168 and 168gmhA. The results obtained for C. jejuni 81-176 and its mutants were similar to those obtained for NCTC 11168 and its mutants, although 817waaF showed a 2- to >16-fold increase in its susceptibility to all five bile acids. Some of the LOS-truncated mutants had increased susceptibilities to erythromycin (1- to 8-fold), rifampin (1- to 2-fold), polymyxin B (2-fold), or SDS (1- to 2-fold). No difference was observed in the susceptibility to the other antimicrobials tested. The susceptibilities of 168gmhA and 817gmhA, and all complemented strains to bile acids and other antimicrobials were the same as those of the wild-type strains.
Table 2. Antimicrobial susceptibility of C. jejuni.
| Antimicrobiala | MIC (µg/ml)b | |||||||
| NCTC 11168 | 81-176 | |||||||
| Ia | IIa | IIIa | IVa | Ib | IIb | IIIb | IVb | |
| (wild-type, 168gmhA) | (168cj1136, 168cj1138) | (168waaF, 168cj1135) | (168hldE, 168hldD, 168waaC) | (wild-type, 817gmhA) | (817cjj1152, 817cjj1165) | (817waaF) | (817hldE, 817hldD, 817waaC) | |
| Ox gall | 25,000 | 25,000 | 25,000 | 6,250 | 12,500 | 12,500 | 6,250 | 6,250 |
| Ox bile extract | 12,500 | 12,500 | 12,500 | 3,130 | 6,250 | 6,250 | 3,130 | 3,130 |
| Cholic acid | 6,250 | 3,130 | 3,130 | 1,560 | 3,130 | 3,130 | 780 | 780 |
| Deoxycholic acid | >10,000 | 10,000 | 5,000 | 313 | >10,000 | 10,000 | 625 | 313 |
| Taurocholic acid | >100,000 | 100,000 | 100,000 | 12,500 | >100,000 | 100,000 | 12,500 | 12,500 |
| SDS | 100 | 100 | 100 | 50 | 50 | 50 | 25 | 25 |
| Ampicillin | >50 | >50 | >50 | >50 | 3.13 | 3.13 | 3.13 | 3.13 |
| Cefsulodin | 25 | 25 | 25 | 25 | 12.5 | 12.5 | 12.5 | 12.5 |
| Gentamicin | 0.313 | 0.313 | 0.313 | 0.313 | 0.313 | 0.313 | 0.313 | 0.313 |
| Tetracycline | <0.2 | <0.2 | <0.2 | <0.2 | 6.25 | 6.25 | 6.25 | 6.25 |
| Erythromycin | 0.5 | 0.125 | 0.125 | 0.0625 | 0.125 | 0.125 | 0.0625 | 0.0313 |
| Trimethoprim | 500 | 500 | 500 | 500 | 250 | 250 | 250 | 250 |
| Nalidixic acid | 10 | 10 | 10 | 10 | 2.5 | 2.5 | 2.5 | 2.5 |
| Enrofloxacin | 0.0625 | 0.0625 | 0.0625 | 0.0625 | 0.0313 | 0.0313 | 0.0313 | 0.0313 |
| Rifampin | 200 | 200 | 200 | 100 | 100 | 100 | 50 | 50 |
| Polymyxin B | 5 | 2.5 | 2.5 | 2.5 | 2.5 | 1.25 | 1.25 | 1.25 |
Bold-faced types indicate that the differences in MICs observed between NCTC 11168 or 81-176 wild-type strain and any mutant.
The NCTC 11168 or 81-176 wild-type strain and mutants were divided into four groups (Ia–IVa or Ib–IVb) on the basis of MICs. The strains belonging to the same group showed identical MIC values for all of the antimicrobials tested.
The multi-drug resistance system, CmeABC, is known to play an important role in bile resistance in C. jejuni [19]. The nucleotide sequences of cmeABC and its promoter region in the LOS-truncated mutants, 168cj1136, 168waaF, and 168hldD, were identical to those of the wild-type strain NCTC 11168, which suggested that CmeABC was functional in these mutants. CPS was detected by Alcian blue staining in all LOS-truncated strains constructed in this study and the wild-type strains (Fig. S1). However, inactivation of kpsS (cj1413) encoding the CPS export protein did not affect bile resistance in both NCTC 11168 and 81-176; MICs of ox gall, ox bile extract, cholic acid, deoxycholic acid, and taurocholic acid were identical in the kpsS mutants and wild-type strains.
Effects of LOS truncations on resistance to chicken intestinal extracts
The growth of the wild-type strains and mutants in intestinal extracts and cholestyramine-treated extracts were investigated to determine whether the bile acids in chicken intestinal extracts affected the viability of Campylobacter. Total bile acid concentrations in the jejunal and ileal extracts were 8.5 and 4.9 mM, respectively. After cholestyramine treatment, bile acid concentrations in the jejunal and ileal extracts were reduced to 1.8 mM, and 1.6 mM, respectively. The wild-type strain NCTC 11168 grew normally in both intestinal extracts, but the mutant strains, i.e., 168hldE, 168hldD, and 168waaC, were not detectable in the jejunal and ileal extracts 6 and 12 h after inoculation, respectively (Fig. 3A and 3B). In both intestinal extracts, the other mutants derived from NCTC 11168 were detectable 24 h after inoculation; however, the viable bacterial counts were lower than those of the wild-type strain 6 h after inoculation. In contrast, the 168hldE, 168hldD, and 168waaC mutants were detectable at all time points in the cholestyramine-treated extracts, and their viable bacterial counts were >1 log unit lower than those of the other strains 24 h after inoculation (Fig. 3C and 3D). Results obtained for the wild-type strain 81-176 and its mutants were similar to those obtained for NCTC 11168 and its mutants, except the 817waaF. This strain was not detectable 12 and 24 h after inoculation in the jejunal and ileal extracts, respectively (Fig. 3E and 3F), whereas 168waaF, the corresponding mutant derived from NCTC 11168, was detectable until 24 h after inoculation in both extracts.
Figure 3. Growth of C. jejuni strains in chicken intestinal extracts.
C. jejuni NCTC 11168 wild-type strain and its mutants were grown in chicken jejunal extract (A), chicken ileal extract (B), chicken jejunal extract pretreated with cholestyramine (C), and chicken ileal extract pretreated with cholestyramine (D). C. jejuni 81-176 wild-type strain and its mutants were also grown in chicken jejunal extract (E), chicken ileal extract (F), chicken jejunal extract pretreated with cholestyramine (G), and chicken ileal extract pretreated with cholestyramine (H). Each point represents the mean value obtained from triplicate wells in 96-well microtiter plates. The detection limit for the assay was 0.4 log10 CFU/ml.
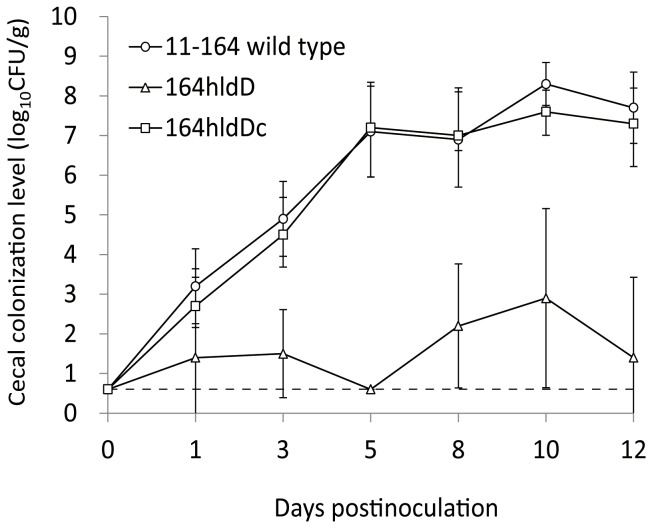
Effects of LOS truncations on chick cecum colonization
To evaluate the effects of LOS truncation on chick cecum colonization, we used strain 11-164 as the wild-type because colonization was better with this strain compared with strains NCTC 11168 and 81-176 in our preliminary experiments (data not shown). The hldE, hldD, waaC, and waaF mutants were constructed from strain 11-164 by natural transformation, and these mutants were used in the in vitro experiments including LOS analysis by mass spectrometry, LOS mobility, antimicrobial susceptibility, and surface hydrophobicity. All results were similar to those obtained with mutants of NCTC 11168 and 81-176. Inactivation of hldE, hldD, or waaC produced severe LOS truncations, which greatly increased the susceptibility of the strains to bile acids (Tables S2 and S3 and Fig. S2A).
Of these, 164hldD and the hldD-complemented strain, 164hldDc, were used in the chick colonization experiments. In 164hldD, the MALDI-TOF MS spectra of the intact LOS contained four intense ions, while only Kdo was detected in the GC mass spectra of the OS sample, as well as strains 168hldD and 817hldD (Table S2). No significant differences were observed among the strains in terms of their growth curves in Mueller–Hinton (MH) broth (Becton Dickinson and Company, Sparks, MD, USA) and the resistance to low pH stress (Fig. S3). In addition, the motilities of all LOS-truncated mutants of 11-164, including 164hldD, were identical to those of the wild-type strains in 0.4% soft MH agar (Becton Dickinson and Company) (Fig. S2B).
As shown in Fig. 4, 11-164 and 164hldDc colonized chickens as early as 1 day after inoculation, and the viable bacterial counts were >107 CFU/g on 5 days after inoculation and after this time period. The mutant strain 164hldD was also detected 1 day after inoculation, although the viable bacterial counts were <103 CFU/g throughout the experimental period. 164hldD was not detected constantly in the cecal contents, whereas 11-164 and 164hldDc were detected in all samples recovered during this experiment.
Figure 4. Colonization of chickens by the C. jejuni 11-164 wild-type strain and its isogenic hldD mutant.
Each point represents the mean log10 CFU/g in the cecal contents of chickens in each group. Standard deviations are indicated by error bars. The dashed line indicates the lower limit of detection (0.7 log10 CFU/g).
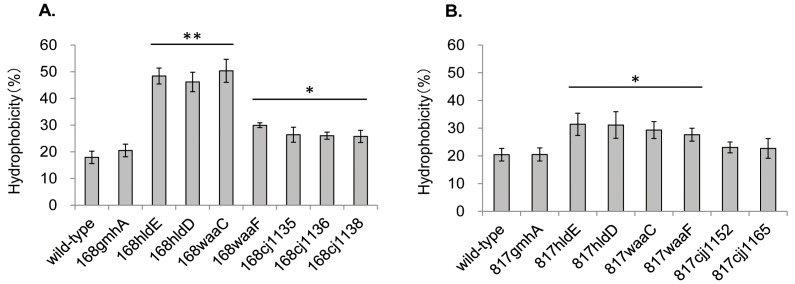
Effects of LOS truncations on cell surface hydrophobicity
It was reported that the surface hydrophobicity of the waaF mutant constructed from strain NCTC 11168 was significantly higher than that of the wild-type strain [23]. To test whether serial truncations of LOS OSs caused a stepwise elevation in the surface hydrophobicity, we conducted a bacterial adherence to hydrocarbon (octane) assay with the LOS-truncated mutants and their wild-type strains.
As shown in Fig. 5A, the surface hydrophobicities of 168hldE, 168hldD, and 168waaC were 2.6- to 2.8-fold higher, while those of the other derivatives were 1.4- to 1.7-fold higher than the surface hydrophobicities of NCTC 11168. The surface hydrophobicities of 817hldE, 817hldD, 817waaC, and 817waaF were 1.4- to 1.5-fold higher than those of the wild-type strain, 81-176, and the difference was significant (Fig. 5B). The surface hydrophobicities of strains 168gmhA, 817gmhA, 817cjj1152, and 817cjj1165 were comparable to those of their wild-type strains (Fig. 5). Complementation restored hydrophobicity in all LOS-truncated mutants (data not shown).
Figure 5. Effect of LOS truncations on the cell surface hydrophobicity of C. jejuni NCTC 11168 (A) and 81-176 (B).
The percentage hydrophobicity of the bacterial surface was calculated as follows: (1−final OD600 of the aqueous phase/initial OD600 of the cell suspension)×100. Standard deviations are indicated by error bars. *Significantly different from wild-type, **significant differences from both the wild-type and LOS mutants are labeled with an asterisk (P<0.05).
Elevation of the surface hydrophobicity was also observed in mutants constructed from strain 11-164, which was used in the chicken colonization experiments; the surface hydrophobicity of 164hldE, 164hldD, 164waaC, and 164waaF was 1.6- to 1.9-fold higher than that of the wild-type strain (Fig. S2C).
Discussion
The involvement of bacterial LPS in bile resistance has been reported [15], [16]. Deep rough mutants of Escherichia coli and Vibrio cholerae showed an increased susceptibility to bile acids [29], [30]. However, the relationship between the LPS/LOS OS structure and bile resistance in gram-negative bacteria remains largely unknown. Recently, Javed et al. [31] reported that the cj1136 mutant of the hyperinvasive wild-type strain 01/51 had an increased susceptibility to sodium taurocholate and a reduced ability to colonize 1-day-old chicks. However, they did not test any other mutants with LOS OS truncations.
In this study, we constructed multiple C. jejuni mutants with serial LOS OS truncations and showed that differences in LOS OS length of one or two saccharides affected bile resistance in the mutants (Table 2). In addition, the hldE, hldD, and waaC mutants of NCTC 11168 and 81-176, which lacked all LOS sugars except Kdo, had greatly increased susceptibilities to bile acids. The susceptibility of the waaF mutant derived from 81-176 to bile acids was comparable to that of mutants that lacked all sugars except Kdo, although LOS of this strain contained a heptose and P/PEtn in addition to Kdo [25]. In contrast, the waaF mutant derived from NCTC 11168, which contained an additional glucose linked to a heptose, was more resistant to bile acids than the mutants derived from 81-176 (Table 2 and Fig. 2). The differences in the susceptibilities to bile acids of the waaF mutants derived from 81-176 and NCTC 11168 were reflected in their growth in chicken intestinal extracts (Fig. 3). In addition to a heptose linked to a Kdo in LOS of C. jejuni, one or more sugars might be essential for bile acid tolerance.
The migration of LOS produced by the isogenic hldE and hldD mutants on SDS-PAGE was slightly slower than that of LOS produced by the waaC mutant derived from NCTC 11168 and 81-176 (Fig. 2A). The hldE and hldD mutants were expected to lack the ability to generate ADP-l-glycero-d-manno-heptose. In the rfaD (a homolog of hldD) mutants of E. coli and H. influenzae, d-glycero-d-manno-heptose is incorporated into the inner core instead of l-glycero-d-manno-heptose, although the sugar chains are not extended further [32], [33]. GC-MS analysis showed that LOS produced by the isogenic hldE and hldD mutants contained Kdo residues, whereas other possible inner core components, including l-glycero-d-manno-heptose and d-glycero-d-manno-heptose, were not detected in this study. MALDI-TOF MS analysis in the negative ion linear mode showed that three residues were incorporated into LOS (Table S2), and the mass differences between the observed ions at approximately Δm/z 220 suggested that the residues were Kdo. The results of SDS-PAGE and GC-MS analysis suggested that there were some modifications to the Kdo2-lipid A structure in the isogenic hldE and hldD mutants, such as a third Kdo addition, although future detailed analyses are necessary to determine the LOS OS structures of these mutants.
CPS is detectable on the surface of C. jejuni and is known to play an important role in serum resistance, epithelial cell invasion, and the onset of diarrheal disease [34]. In this study, CPS was detected in all LOS-truncated mutants, and bile resistance of CPS mutants was comparable to that of wild-type strains. These results suggest that CPS is not essential for bile resistance in C. jejuni, which was previously suggested by Jeon et al. [23].
Bile acids are surface active detergents with potent antimicrobial activities [15]. The binding of bile acids to membrane lipids is correlated to their hydrophobicities. Increased hydrophobicity may facilitate the accessibility of bile acids to membrane lipids, thus leading to membrane damage. The increased susceptibilities to bile acids due to severe truncations of LOS OS may have been observed because of the higher hydrophobicities conferred by the shorter LOS chains, which made the microbe more susceptible to bile acids (Table 2 and Fig. 5).
The bile acid concentration in chicken intestines varies at different detection sites. The bile acid concentration in jejunal contents is >10 mM, which is lethal to many non-enteric bacteria [35]. The concentration in the upper gastrointestinal tract is higher than that in the lower part. Lin et al. reported that the bile acid concentration in jejunal and cecal extracts were 14.0 mM and 0.17 mM, respectively [19]. This may explain why C. jejuni mainly colonizes the lower intestines of chickens [36]. In this study, the bile acid concentrations of the jejunal and ileal extracts were 8.5 mM and 4.9 mM, respectively. These bile acid concentrations did not affect the growth of NCTC 11168 and 81-176 in the extracts, although these strains were poor colonizers of chicken intestines in our laboratory. Thus, these experiments showed that jejunal and ileal extracts did not accurately replicate the intestinal environments of chickens. However, it has been shown that these systems can be used to evaluate the tolerance of C. jejuni strains to bile acids by simulating the conditions in intestinal tracts of chickens.
Inactivation of hldE, hldD, and waaC greatly increased the susceptibility to jejunal and ileal extracts from chickens in this study (Fig. 3). The hldD mutant derived from 11-164 can be killed or damaged by high concentration of bile acids in the jejunum and ileum of chickens, while colonization of the lower intestine by this mutant was lower than that by the wild-type strain. Overall, this study demonstrated that the addition of more than one sugar to Kdo facilitated bile acid tolerance and promoted the colonization of chicken intestinal tracts. These data should be useful for developing novel control measures to prevent C. jejuni colonization of chicken intestines. Inhibitors of the C. jejuni enzymes, bifunctional d-glycero-d-manno-heptose 7-phosphate kinase/d-glycero-d-manno-heptose 1-phosphate adenylyltransferase (HldE), ADP-d-glycero-d-manno-heptose epimerase (HldD), and heptosyltransferase I (WaaC), might act as potent anti-Campylobacter agents.
Materials and Methods
Bacterial strains, plasmids, and culture conditions
The bacterial strains and plasmids used in this study and their sources are listed in Table 1. MH broth and MH agar were used to grow the C. jejuni strains at 42°C under microaerophilic conditions, which were generated using AnaeroPack (Mitsubishi Gas Chemical Company, Inc., Tokyo, Japan) in an enclosed jar. E. coli DH5α was grown in Luria–Bertani broth or on LB agar (Becton Dickinson and Company) with or without ampicillin (100 µg/ml) and kanamycin (30 µg/ml) at 37°C.
PCR
The PCR primers used in this study are shown in Table S4. PCR was performed in a volume of 50 µl containing 200 µM of each of the four deoxynucleoside triphosphates, 2 or 1 mM of MgCl2, 250 nM of primers, 50 ng of template DNA, and 1.25 U of Ex Taq DNA polymerase (Takara Bio Inc., Otsu, Japan) or Pyrobest DNA polymerase (Takara Bio). Amplifications were performed using iCycler (Bio-Rad Laboratories, Hercules, CA, USA). The cycling conditions varied depending on the estimated annealing temperatures of the primers and the expected size of the products. The size of the PCR products was confirmed by agarose gel electrophoresis.
Construction of LOS mutants of C. jejuni
Isogenic mutants were constructed using a nonpolar chloramphenicol cassette [37]. The upstream and downstream regions of each target gene and the cat gene encoding chloramphenicol resistance from pUOA18 [38] were amplified independently and used as templates for overlapping extension PCR to join the three fragments [39]. The fragments produced were cloned into the pGEM-T Easy vector (Promega Corporation, Madison, WI, USA) to generate suicide vectors. Each suicide vector was introduced into NCTC 11168 or 81-176 by electroporation using a MicroPulser electroporator (Bio-Rad Laboratories), according to the manufacturer's instructions. Transformants were selected on MH agar containing 6 µg/ml chloramphenicol.
The construction of complemented strains of LOS-truncated mutants was based on a previous study [40]. Each target gene encoding the biosynthetic enzyme and promoter region of cmeABC was amplified independently and used as a template for overlapping extension PCR. The fragments produced were digested with EcoRI and BamHI and cloned into pUOA18Km. Each vector was introduced into the corresponding LOS-truncated mutant via triparental mating using Dh5α harboring the helper plasmid pRK2013 [41]. The complemented strain 164hldDc was selected using MH agar plates containing kanamycin (30 µg/ml) and chloramphenicol (6 µg/ml).
The genomic DNA from C. jejuni 168hldE, 168hldD, 168waaC, and 168waaF were used to transform C. jejuni 11-164 in order to generate the 164hldE, 164hldD, 164waaC, and 164waaF as described previously [42]. hldD was cloned into pUOA18Km and transformed into 164hldD for trans-complementation.
Isolation of LOS and the OS fraction
LOS was obtained from each strain by hot phenol extraction followed by RNase, DNase, and protease treatments, as reported previously [43]. LOS samples were separated by tricine-SDS-PAGE [44] using a 16% (w/v) polyacrylamide separating gel and visualized by silver staining [45].
LOS samples were prepared for MALDI-TOF MS analyses using the following procedure. Each LOS band was excised from the separating gel of tricine-SDS-PAGE, ground, and homogenized using a spatula. Five volumes of distilled water was added to one volume of homogenate, and then incubated overnight at room temperature with shaking. After centrifugation at 5,000×g for 10 min, LOS was filtered from the supernatant through a 0.45-µm membrane filter (Toyo Roshi Kaisha, Ltd., Tokyo, Japan) and precipitated by performing two sets of centrifugation at 284,000×g for 8 h.
OS was released from LOS samples by mild acid hydrolysis in 1.5% acetic acid at 100°C for 2 h [46] and lyophilization. Lipid A was removed with CHCl3/MeOH/H2O (12∶8∶1) [47].
LOS analysis by mass spectrometry
The structures of LOS and OS were analyzed by MALDI-TOF MS in the negative ion mode using a 4800 plus MALDI TOF/TOF analyzer (AB Sciex, Framingham, MA, USA). The ion-accelerating voltage was set at 20 kV. Freeze-dried LOS or OS was dissolved in 30% methanol and desalted with a few grains of a cation exchange resin, i.e., Dowex 50W-X2 (H+ form) (Wako Pure Chemical Industries, Ltd., Osaka, Japan). The solution (0.5 µl) was deposited on the target and covered with the same amount of the matrix solution containing 20 mg/ml of 2,5-dihydroxybenzoic acid (DHB, Bruker Daltonics Inc., Billerica, MA, USA) in 30% methanol with 0.1 M citric acid [48]. The mass spectrometer was tuned and calibrated using commercially available standard peptides in the reflector mode and proteins in the linear mode (Bruker Daltonics; Peptide calibration standard I containing angiotensin II, angiotensin I, substance P, bombesin, ACTH clip 1–17, ACTH clip 18–39, somatostatin 28; and Protein calibration standard I containing insulin, ubiquitin, cytochrome C, and myoglobin).
Sugar compositions of LOS and OS were determined as their alditol acetates by GC-MS [46].
Susceptibility tests
MICs of the antimicrobials shown in Table 2 were determined by the standard microtiter broth dilution method using MH broth containing an inoculum of 106 CFU/well, as described previously [49]. Bacterial growth was assessed after incubating the microtiter plates for 48 h at 42°C under microaerobic conditions. The MIC experiments were repeated three times using each strain tested in this study and each of the different antimicrobials, and the results of one representative experiment are shown.
Growth assay using chicken intestinal extracts
Chicken intestinal extracts were prepared as described by Lin et al. [19]. In brief, jejunal and ileal contents of six 28-day-old chickens were obtained and pooled. Each sample was mixed with the same volume of MH broth and centrifuged at 10,000×g at 4°C for 30 min. The supernatant was filtered through a 0.45-µm membrane filter (Toyo Roshi Kaisha). To sequestrate bile acids, each chicken intestinal extract was pretreated with 5% (w/v) cholestyramine resin (Sigma-Aldrich Co., St. Louis, MO, USA) at room temperature for 1 h with intermittent vortexing [50]. After incubation, cholestyramine was removed by centrifugation and filtration. Filtration was performed using a 0.2-µm membrane filter (Toyo Roshi Kaisha). Total bile acid concentrations in each intestinal extract and cholestyramine-treated extracts were measured using the colorimetric Total Bile Acid Test Kit (Diazyme Laboratories, San Diego, CA, USA), according to the manufacturer's instruction. Bile acid concentrations were recorded as the arithmetic means of three independent analyses.
The growth of C. jejuni strains in the chicken intestinal extracts and cholestyramine-treated extracts was measured using the following procedure. Thirty microliters of the C. jejuni strain (approximately 5×108 CFU/ml) and 300 µl of a 1∶10 dilution of each extract were mixed in a 96-well plate (in triplicate) and incubated at 42°C under microaerophilic conditions for 24 h. During incubation, 50 µl of the mixture was removed from each well at different time points (0, 6, 12, and 24 h after inoculation), serially diluted, and plated onto MH agar to enumerate the Campylobacter colonies in each sample. With each strain tested in this study, the growth assay was repeated three times with each of the chicken intestinal extract and the results of one representative experiment are shown.
Chicken colonization experiments
To analyze the effect of hldD mutation on intestinal colonization by C. jejuni, hldD mutant and complementary strain were constructed using C. jejuni 11-164. The resistant strain 11-164 was selected using MH agar plates containing 100 µg/ml nalidixic acid and used as the wild-type strain to construct the mutant and complementary strains. The nalidixic acid-resistant phenotype of this strain facilitated the enumeration of viable C. jejuni cells in the cecal contents of experimentally infected chicks.
Newly hatched 1-day-old chicks were obtained from Nisseiken Co. Ltd. (Ome, Japan). Before use, these chicks were screened for Campylobacter by culturing cloacal swabs on MH agar plates containing Campylobacter-specific growth supplements (SR232E and SR117E; Oxoid Ltd., Basingstoke, UK). All chicks tested negative for Campylobacter. To compare colonization of strains, 54 three-day-old chicks were assigned to three groups (18 chicks/group). Each group was challenged with 106 CFU of 11-164 wild type, 164hldD, or 164hldDc. Three chicks from each group were sacrificed at 1, 3, 5, 8, 10, and 12 days after inoculation, and their cecal contents were collected, serially diluted, and spread on MH agar plates supplemented with nalidixic acid. Plates were incubated at 42°C under microaerophilic conditions for 48 h, and Campylobacter colonies formed on each plate were counted.
These experiments were carried out in strict accordance with the guidelines of animal experimentation defined by the National Institute of Animal Health (NIAH) of Japan. The protocol was approved by the committee on the Ethics of Animal Experiments of the NIAH (Permit Number 10-027).
Hydrophobicity test
Bacterial adherence to hydrocarbons was tested as described by Rosenberg et al. [51]. In brief, freshly grown C. jejuni cells on MH agar plates were harvested and washed twice using phosphate-buffered saline (PBS), centrifuged, and resuspended in the same buffer to produce an optical density (OD) of 0.5 at 600 nm. One milliliter of the suspension and 1 ml of n-octane (Wako Pure Chemical Industries) were placed in a borosilicate glass tube and mixed using a vortex mixer for 120 s. After 15 min of standing, the aqueous phase was transferred to a cuvette and OD600 was measured. The surface hydrophobicity (%) of the bacteria was calculated as follows: (1−final OD600 of the aqueous phase/initial OD600 of the cell suspension)×100. All tests were performed in triplicate.
Statistical analysis
Differences in the results were tested using the two-tailed unpaired Student's t test. P<0.05 was considered statistically significant. The results of chicken colonization experiments and hydrophobicity tests are expressed as the means with error bars denoting the standard deviations of the means.
Supporting Information
CPS profiles of the C. jejuni wild-type strains (NCTC 11168 and 81-176) and mutants. CPS samples were obtained from each strain by hot phenol extraction followed by RNase, DNase, and protease treatments. CPS samples were separated on a 4–20% Tris-glycine SDS-PAGE gel and visualized by Alcian blue staining.
(TIF)
LOS profiles, motility, and cell surface hydrophobicity of the wild-type 11-164 and mutants. (A) LOS samples were analyzed by tricine-SDS-PAGE using 16% tricine gels and visualized by silver staining. The positions of the protein size markers are indicated on the left of each panel. (B) Zones of motility of wild-type 11-164 and mutants in 0.4% soft MH agar. (C) Effect of LOS truncations on the cell surface hydrophobicity of the wild-type 11-164 and mutants. The percentage hydrophobicity of the bacterial surface was calculated as follows: (1−final OD600 of the aqueous phase/initial OD600 of the cell suspension)×100. Three independent experiments were performed using the same strains and conditions. The standard deviations are indicated by error bars.
(TIF)
Growth properties in MH broth and survival in MH broth at pH 4.0 of the wild-type 11-164, 164hldD, and 164hldDc. (A) To compare the growth kinetics of the mutants of 11-164 with that of the wild-type strain, the cultures were inoculated separately into MH broth at an initial cell density of 5×10 CFU/ml. The cultures were incubated at 42°C under microaerobic conditions. Aliquots of the cultures were collected at different time points (0, 8, 24, 32, 48, and 72 h), serially diluted, and plated onto MH agar plates to enumerate the bacterial colonies. Three independent experiments were performed using the same strains and conditions. (B) Bacterial cultures were inoculated separately into MH broth (pH 4.0) at an initial cell density of 1×108 CFU/ml and incubated at 42°C under microaerobic conditions. Aliquots of the cultures were collected at different time points (0, 0.5, 1, and 2 h), serially diluted, and plated onto MH agar plates to enumerate the bacterial colonies. Three independent experiments were performed using the same strains and conditions.
(TIF)
Major ions in the negative reflectron mode MALDI-TOF mass spectra and the proposed compositions of the OS chains of 168cj1135, 168cj1136, and168cj1138.
(DOCX)
Major ions in the negative linear mode MALDI-TOF mass spectra and the proposed compositions of the intact LOS chains of 168hldE, 168hldD, 817hldE, 817hldD, and 164hldD.
(DOCX)
Antimicrobial susceptibility of wild-type 11-164 and mutants.
(DOCX)
Primers used in this study.
(DOCX)
Acknowledgments
We thank Dr. Qijing Zhang for providing the plasmid pUOA18 and C. jejuni strains NCTC 11168 and 81-176.
Funding Statement
This work was supported in part by a Grant-in-Aid from the Ministry of Agriculture, Forestry, and Fisheries of Japan (Research project for ensuring food safety from farm to table DI-5101). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. No additional external funding received for this study.
References
- 1. Penner JL (1988) The genus Campylobacter: a decade of progress. Clinical Microbiology Reviews 1: 157–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Euzeby JP (1997) List of Bacterial Names with Standing in Nomenclature: a folder available on the Internet. International Journal of Systematic Bacteriology 47: 590–592. [DOI] [PubMed] [Google Scholar]
- 3. Coker AO, Isokpehi RD, Thomas BN, Amisu KO, Obi CL (2002) Human campylobacteriosis in developing countries. Emerging Infectious Diseases 8: 237–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Buzby JC, Allos BM, Roberts T (1997) The economic burden of Campylobacter-associated Guillain-Barre syndrome. J Infect Dis 176 Suppl 2: S192–197. [DOI] [PubMed] [Google Scholar]
- 5. Yuki N, Odaka M (2005) Ganglioside mimicry as a cause of Guillain-Barre syndrome. Current Opinion in Neurology 18: 557–561. [DOI] [PubMed] [Google Scholar]
- 6. Fernandez-Cruz A, Munoz P, Mohedano R, Valerio M, Marin M, et al. (2010) Campylobacter bacteremia: clinical characteristics, incidence, and outcome over 23 years. Medicine 89: 319–330. [DOI] [PubMed] [Google Scholar]
- 7. Pigrau C, Bartolome R, Almirante B, Planes AM, Gavalda J, et al. (1997) Bacteremia due to Campylobacter species: clinical findings and antimicrobial susceptibility patterns. Clin Infect Dis 25: 1414–1420. [DOI] [PubMed] [Google Scholar]
- 8. Baker J, Barton MD, Lanser J (1999) Campylobacter species in cats and dogs in South Australia. Aust Vet J 77: 662–666. [DOI] [PubMed] [Google Scholar]
- 9. Buswell CM, Herlihy YM, Lawrence LM, McGuiggan JT, Marsh PD, et al. (1998) Extended survival and persistence of Campylobacter spp. in water and aquatic biofilms and their detection by immunofluorescent-antibody and -rRNA staining. Appl Environ Microbiol 64: 733–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Newell DG, Fearnley C (2003) Sources of Campylobacter colonization in broiler chickens. Appl Environ Microbiol 69: 4343–4351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Horrocks SM, Anderson RC, Nisbet DJ, Ricke SC (2009) Incidence and ecology of Campylobacter jejuni and coli in animals. Anaerobe 15: 18–25. [DOI] [PubMed] [Google Scholar]
- 12. Wilson DJ, Gabriel E, Leatherbarrow AJ, Cheesbrough J, Gee S, et al. (2008) Tracing the source of campylobacteriosis. PLoS Genet 4: e1000203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Smith DP, Cason JA, Berrang ME (2005) Effect of fecal contamination and cross-contamination on numbers of coliform, Escherichia coli, Campylobacter, and Salmonella on immersion-chilled broiler carcasses. J Food Prot 68: 1340–1345. [DOI] [PubMed] [Google Scholar]
- 14. Louis P, O'Byrne CP (2010) Life in the gut: microbial responses to stress in the gastrointestinal tract. Science Progress 93: 7–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Begley M, Gahan CG, Hill C (2005) The interaction between bacteria and bile. FEMS Microbiol Rev 29: 625–651. [DOI] [PubMed] [Google Scholar]
- 16. Gunn JS (2000) Mechanisms of bacterial resistance and response to bile. Microbes Infect 2: 907–913. [DOI] [PubMed] [Google Scholar]
- 17. Merritt ME, Donaldson JR (2009) Effect of bile salts on the DNA and membrane integrity of enteric bacteria. J Med Microbiol 58: 1533–1541. [DOI] [PubMed] [Google Scholar]
- 18. Lin J, Michel LO, Zhang Q (2002) CmeABC functions as a multidrug efflux system in Campylobacter jejuni . Antimicrob Agents Chemother 46: 2124–2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lin J, Sahin O, Michel LO, Zhang Q (2003) Critical role of multidrug efflux pump CmeABC in bile resistance and in vivo colonization of Campylobacter jejuni . Infect Immun 71: 4250–4259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Preston A, Mandrell RE, Gibson BW, Apicella MA (1996) The lipooligosaccharides of pathogenic gram-negative bacteria. Crit Rev Microbiol 22: 139–180. [DOI] [PubMed] [Google Scholar]
- 21. Raetz CR, Reynolds CM, Trent MS, Bishop RE (2007) Lipid A modification systems in gram-negative bacteria. Annual Review of Biochemistry 76: 295–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Marsden GL, Li J, Everest PH, Lawson AJ, Ketley JM (2009) Creation of a large deletion mutant of Campylobacter jejuni reveals that the lipooligosaccharide gene cluster is not required for viability. J Bacteriol 191: 2392–2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jeon B, Muraoka W, Scupham A, Zhang Q (2009) Roles of lipooligosaccharide and capsular polysaccharide in antimicrobial resistance and natural transformation of Campylobacter jejuni . J Antimicrob Chemother 63: 462–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kanipes MI, Papp-Szabo E, Guerry P, Monteiro MA (2006) Mutation of waaC, encoding heptosyltransferase I in Campylobacter jejuni 81–176, affects the structure of both lipooligosaccharide and capsular carbohydrate. J Bacteriol 188: 3273–3279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Naito M, Frirdich E, Fields JA, Pryjma M, Li J, et al. (2010) Effects of sequential Campylobacter jejuni 81–176 lipooligosaccharide core truncations on biofilm formation, stress survival, and pathogenesis. J Bacteriol 192: 2182–2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Karlyshev AV, Champion OL, Churcher C, Brisson JR, Jarrell HC, et al. (2005) Analysis of Campylobacter jejuni capsular loci reveals multiple mechanisms for the generation of structural diversity and the ability to form complex heptoses. Mol Microbiol 55: 90–103. [DOI] [PubMed] [Google Scholar]
- 27. Szymanski CM, Logan SM, Linton D, Wren BW (2003) Campylobacter–a tale of two protein glycosylation systems. Trends Microbiol 11: 233–238. [DOI] [PubMed] [Google Scholar]
- 28. Parkhill J, Wren BW, Mungall K, Ketley JM, Churcher C, et al. (2000) The genome sequence of the food-borne pathogen Campylobacter jejuni reveals hypervariable sequences. Nature 403: 665–668. [DOI] [PubMed] [Google Scholar]
- 29. Picken RN, Beacham IR (1977) Bacteriophage-resistant mutants of Escherichia coli K12 with altered lipopolysaccharide. Studies with concanavalin A. J Gen Microbiol 102: 319–326. [DOI] [PubMed] [Google Scholar]
- 30. Nesper J, Schild S, Lauriano CM, Kraiss A, Klose KE, et al. (2002) Role of Vibrio cholerae O139 surface polysaccharides in intestinal colonization. Infect Immun 70: 5990–5996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Javed MA, Cawthraw SA, Baig A, Li J, McNally A, et al. (2012) Cj1136 is required for lipooligosaccharide biosynthesis, hyperinvasion, and chick colonization by Campylobacter jejuni . Infect Immun 80: 2361–2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Coleman WG (1983) The rfaD gene codes for ADP-L-glycero-D-mannoheptose-6-epimerase. An enzyme required for lipopolysaccharide core biosynthesis. J Biol Chem 258: 1985–1990. [PubMed] [Google Scholar]
- 33. Nichols WA, Gibson BW, Melaugh W, Lee NG, Sunshine M, et al. (1997) Identification of the ADP-L-glycero-D-manno-heptose-6-epimerase (rfaD) and heptosyltransferase II (rfaF) biosynthesis genes from nontypeable Haemophilus influenzae 2019. Infect Immun 65: 1377–1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bacon DJ, Szymanski CM, Burr DH, Silver RP, Alm RA, et al. (2001) A phase-variable capsule is involved in virulence of Campylobacter jejuni 81-176. Mol Microbiol 40: 769–777. [DOI] [PubMed] [Google Scholar]
- 35. Green J, Kellogg TF (1987) Bile acid concentrations in serum, bile, jejunal contents, and excreta of male broiler chicks during the first six weeks posthatch. Poultry Science 66: 535–540. [DOI] [PubMed] [Google Scholar]
- 36. Meinersmann RJ, Rigsby WE, Stern NJ, Kelley LC, Hill JE, et al. (1991) Comparative study of colonizing and noncolonizing Campylobacter jejuni . Am J Vet Res 52: 1518–1522. [PubMed] [Google Scholar]
- 37. Akiba M, Lin J, Barton YW, Zhang Q (2006) Interaction of CmeABC and CmeDEF in conferring antimicrobial resistance and maintaining cell viability in Campylobacter jejuni . J Antimicrob Chemother 57: 52–60. [DOI] [PubMed] [Google Scholar]
- 38. Wang Y, Taylor DE (1990) Chloramphenicol resistance in Campylobacter coli: nucleotide sequence, expression, and cloning vector construction. Gene 94: 23–28. [DOI] [PubMed] [Google Scholar]
- 39. Hansen CR, Khatiwara A, Ziprin R, Kwon YM (2007) Rapid construction of Campylobacter jejuni deletion mutants. Lett Appl Microbiol 45: 599–603. [DOI] [PubMed] [Google Scholar]
- 40. Oakland M, Jeon B, Sahin O, Shen Z, Zhang Q (2011) Functional characterization of a lipoprotein-encoding operon in Campylobacter jejuni . PLoS One 6: e20084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Miller WG, Bates AH, Horn ST, Brandl MT, Wachtel MR, et al. (2000) Detection on surfaces and in Caco-2 cells of Campylobacter jejuni cells transformed with new gfp, yfp, and cfp marker plasmids. Appl Environ Microbiol 66: 5426–5436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wang Y, Taylor DE (1990) Natural transformation in Campylobacter species. J Bacteriol 172: 949–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Inzana TJ, Glindemann G, Cox AD, Wakarchuk W, Howard MD (2002) Incorporation of N-acetylneuraminic acid into Haemophilus somnus lipooligosaccharide (LOS): enhancement of resistance to serum and reduction of LOS antibody binding. Infect Immun 70: 4870–4879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Schagger H, von Jagow G (1987) Tricine-sodium dodecyl sulfate-polyacrylamide gel electrophoresis for the separation of proteins in the range from 1 to 100 kDa. Anal Biochem 166: 368–379. [DOI] [PubMed] [Google Scholar]
- 45. Hitchcock PJ, Brown TM (1983) Morphological heterogeneity among Salmonella lipopolysaccharide chemotypes in silver-stained polyacrylamide gels. J Bacteriol 154: 269–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. York WS, Darvill AG, McNeil M, Albersheim P (1985) 3-deoxy-d-manno-2-octulosonic acid (KDO) is a component of rhamnogalacturonan II, a pectic polysaccharide in the primary cell walls of plants. Carbohydrate Research 138: 109–126. [Google Scholar]
- 47. Gudlavalleti SK, Forsberg LS (2003) Structural characterization of the lipid A component of Sinorhizobium sp. NGR234 rough and smooth form lipopolysaccharide. Demonstration that the distal amide-linked acyloxyacyl residue containing the long chain fatty acid is conserved in rhizobium and Sinorhizobium sp. J Biol Chem 278: 3957–3968. [DOI] [PubMed] [Google Scholar]
- 48. Therisod H, Labas V, Caroff M (2001) Direct microextraction and analysis of rough-type lipopolysaccharides by combined thin-layer chromatography and MALDI mass spectrometry. Analytical Chemistry 73: 3804–3807. [DOI] [PubMed] [Google Scholar]
- 49.Sahm DF, Washington JA (1991) Antimicrobial susceptibility test: dilution methods. In: Balows A, Hausler WJ, Herrmann KL Jr, Isenberg HD, Shadomy HJ, editors. Manual of clinical microbiology, 5th ed. Washington, DC: American Society for Microbiology. pp. 1105–1116. [Google Scholar]
- 50. Edwards AD, Slater NK (2009) Protection of live bacteria from bile acid toxicity using bile acid adsorbing resins. Vaccine 27: 3897–3903. [DOI] [PubMed] [Google Scholar]
- 51. Rosenberg M, Gutnick D, Rosenberg E (1980) Adherence of bacteria to hydrocarbons: A simple method for measuring cell-surface hydrophobicity. FEMS Microbiology Letters 9: 29–33. [Google Scholar]
- 52. Guerry P, Szymanski CM, Prendergast MM, Hickey TE, Ewing CP, et al. (2002) Phase variation of Campylobacter jejuni 81-176 lipooligosaccharide affects ganglioside mimicry and invasiveness in vitro. Infect Immun 70: 787–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Oldfield NJ, Moran AP, Millar LA, Prendergast MM, Ketley JM (2002) Characterization of the Campylobacter jejuni heptosyltransferase II gene, waaF, provides genetic evidence that extracellular polysaccharide is lipid A core independent. J Bacteriol 184: 2100–2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Szymanski CM, Michael FS, Jarrell HC, Li J, Gilbert M, et al. (2003) Detection of conserved N-linked glycans and phase-variable lipooligosaccharides and capsules from campylobacter cells by mass spectrometry and high resolution magic angle spinning NMR spectroscopy. J Biol Chem 278: 24509–24520. [DOI] [PubMed] [Google Scholar]
- 55. Black RE, Levine MM, Clements ML, Hughes TP, Blaser MJ (1988) Experimental Campylobacter jejuni infection in humans. J Infect Dis 157: 472–479. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CPS profiles of the C. jejuni wild-type strains (NCTC 11168 and 81-176) and mutants. CPS samples were obtained from each strain by hot phenol extraction followed by RNase, DNase, and protease treatments. CPS samples were separated on a 4–20% Tris-glycine SDS-PAGE gel and visualized by Alcian blue staining.
(TIF)
LOS profiles, motility, and cell surface hydrophobicity of the wild-type 11-164 and mutants. (A) LOS samples were analyzed by tricine-SDS-PAGE using 16% tricine gels and visualized by silver staining. The positions of the protein size markers are indicated on the left of each panel. (B) Zones of motility of wild-type 11-164 and mutants in 0.4% soft MH agar. (C) Effect of LOS truncations on the cell surface hydrophobicity of the wild-type 11-164 and mutants. The percentage hydrophobicity of the bacterial surface was calculated as follows: (1−final OD600 of the aqueous phase/initial OD600 of the cell suspension)×100. Three independent experiments were performed using the same strains and conditions. The standard deviations are indicated by error bars.
(TIF)
Growth properties in MH broth and survival in MH broth at pH 4.0 of the wild-type 11-164, 164hldD, and 164hldDc. (A) To compare the growth kinetics of the mutants of 11-164 with that of the wild-type strain, the cultures were inoculated separately into MH broth at an initial cell density of 5×10 CFU/ml. The cultures were incubated at 42°C under microaerobic conditions. Aliquots of the cultures were collected at different time points (0, 8, 24, 32, 48, and 72 h), serially diluted, and plated onto MH agar plates to enumerate the bacterial colonies. Three independent experiments were performed using the same strains and conditions. (B) Bacterial cultures were inoculated separately into MH broth (pH 4.0) at an initial cell density of 1×108 CFU/ml and incubated at 42°C under microaerobic conditions. Aliquots of the cultures were collected at different time points (0, 0.5, 1, and 2 h), serially diluted, and plated onto MH agar plates to enumerate the bacterial colonies. Three independent experiments were performed using the same strains and conditions.
(TIF)
Major ions in the negative reflectron mode MALDI-TOF mass spectra and the proposed compositions of the OS chains of 168cj1135, 168cj1136, and168cj1138.
(DOCX)
Major ions in the negative linear mode MALDI-TOF mass spectra and the proposed compositions of the intact LOS chains of 168hldE, 168hldD, 817hldE, 817hldD, and 164hldD.
(DOCX)
Antimicrobial susceptibility of wild-type 11-164 and mutants.
(DOCX)
Primers used in this study.
(DOCX)